Escolar Documentos
Profissional Documentos
Cultura Documentos
Atelectasis. Mechanisms, Diagnosis and Management (Peroni, 2000)
Enviado por
Renato Li SoldevillaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Atelectasis. Mechanisms, Diagnosis and Management (Peroni, 2000)
Enviado por
Renato Li SoldevillaDireitos autorais:
Formatos disponíveis
PAEDIATRIC RESPIRATORY REVIEWS (2000) 1, 274278
doi: 10.1054/prrv.2000.0059, available online at http://www.idealibrary.com on
MANAGEMENT
Atelectasis: mechanisms, diagnosis and management
D. G. Peroni and A. L. Boner*
Clinica Pediatrica, University of Verona, Verona and Istituto Pio XII, Misurina, Italy
KEYWORDS
atelectasis, children,
asthma, cystic fibrosis,
mucus plugs
Summary The term atelectasis describes a state of collapsed and non-aerated region
of the lung parenchyma, which is otherwise normal.This pathological condition is usually
associated with several pulmonary and chest disorders and represents a manifestation of
the underlying disease, not a disease per se. Atelectasis may occur in three ways: (i) airway obstruction; (ii) compression of parenchyma by extrathoracic, intrathoracic, chest
wall processes; and (iii) increased surface tension in alveoli and bronchioli. Chest radiographs using both the anterior-posterior and lateral projections are mandatory to document the presence of atelectasis. Differentiation from lobar consolidation may be a
clinical dilemma.The treatment of atelectasis varies depending on duration and severity
of the causal disease from chest physiotherapy to postural drainage, bronchodilator
and anti-inflammatory therapy. Persistent mucous plugs should be removed by bronchoscopy. 2000 Harcourt Publishers Ltd
INTRODUCTION
The developing lung is particularly predisposed to atelectasis once airway obstruction develops: in early childhood the
airways are smaller and more collapsable, the chest wall is
more compliant, and the collateral ventilation through intraalveolar and bronchiole-alveolar pores is not completely
developed. Atelectasis is influenced by pulmonary surfactant deficiency, such as in hyaline membrane disease (HMD)
of prematurity and by surfactant dysfunction, in neardrowning, and in the acute respiratory distress syndrome
(ARDS). Surfactant can directly modify alveolar tension with
the changes of lung volumes, preventing collapse of small
alveoli at low lung volumes and facilitating collapse at high
lung volumes. The surfactant components (phospholipids,
lipids, four surfactant-associated proteins, and calcium) may
explain the properties of surfactant which are required for
the normal function of peripheral gas exchange apparatus.1
PATHOPHYSIOLOGY
Air trapping and hyperinflation are produced by partial
airway obstruction, atelectasis by complete obstruction.
*Address for correspondence: Prof. Attilio Boner, Clinica
Pediatrica Universita di Verona, Policlinico GB Rossi, Via
Menegone 37134 Verona, Italy. Tel: 39 045 8074615, Fax: 39 045
8200993, E-mail: boner@borgoroma.univr.it
15260550/00/030274 + 05 $35.00/0
The gases trapped by complete occlusion are absorbed
by the blood perfusing that region of the lung. The rate of
gas absorption depends on the gas solubility: respirable
air nitrogen and helium are absorbed in 23 h, 100% oxygen within a few min. For these reasons atelectases are
more common in HMD and in the postoperative period,
when high concentrations of oxygen are administered to
the patient. If alveoli are collapsed a greater effort is
required to reinflate them than when they are filled with
air; an even greater effort is required to expand lung tissue which has been collapsed for days rather than for
hours. Atelectasis produces alveolar hypoxia and pulmonary vasoconstriction to prevent ventilation-perfusion
mismatching and to minimize arterial hypoxia. The vascular response is less effective when a large part of the lung
is collapsed; if the blood cannot be diverted, it flows
through the atelectatic non-ventilated region and produces intrapulmonary shunting.2,3
CAUSES OF ATELECTASIS
The causes of atelectasis in childhood are summarized in
Table 1. Atelectasis may occur mainly in three ways: (i)
airway obstruction; (ii) compression of parenchyma by
extrathoracic, intrathoracic, chest wall processes; and (iii)
increased surface tension in alveoli and bronchioli due to
surfactant deficiency or dysfunction.
2000 Harcourt Publishers Ltd
ATELECTASIS: MECHANISMS, DIAGNOSIS AND MANAGEMENT
Table 1 Causes of atelectasis in childhood.
1. Airway obstruction
(a) Exogenous
Foreign body
Recurrent aspiration
Histoplasmosis
(b) Endogenous
Polyps
Papilloma
Adenomas
Granulomas
Mucus plugs in
cystic fibrosis
asthma
bronchopulmonary dysplasia
bronchiectasis
pneumonia
immobile cilia syndromes
2. Compression of parenchyma
(a) Extrinsic bronchial compression
Tumors
Metastasis,
Lymph nodes
Cardiomegaly
(b) Intrathoracic compression
Chilothorax
Hemothorax
Pneumothorax
(c) Chest wall defects and Neuromuscular diseases
Abnormalities of diaphragm
Spinal muscular atrophy
WerdnigHoffmann disease
Muscular dystrophies
GuillainBarre syndrome
3. Surfactant deficiency or dysfunction
Hyaline membrane disease
Pneumonia
Pulmonary oedema
Near-drowning
Adult respiratory distress syndrome (ARDS)
Most of the causes of atelectasis in childhood are due
to airway obstruction: the obstruction leads to a non-ventilation of the distal airways; the gas residing in that region
is completely absorbed by pulmonary blood flowing
through that area. Compression of the parenchyma
and increased surface tension produce an extrusion of
the gas out of the alveoli and reduce the capability of the
involved parenchyma to reinflate.
Intrabronchial obstruction may be exogenous (foreign
body, histoplasmosis, etc.) or endogenous (polyps, papillomas, adenomas, granulomas, mucous plugs due to
asthma, cystic fibrosis (CF), bronchopulmonary dysplasia,
or bronchiectasis). The poor clearance of inflammatory
debris, smooth muscle constriction and oedema of the
bronchial wall in asthma and CF produce atelectasis by
occluding the lumen of the airways; bronchiectasis causes
275
an inadequate bronchial wall integrity, which may lead to
obstruction.
Extrinsic bronchial compression may cause a compression of the adjacent bronchi: the more common process
involved is enlargement of the hilar or mediastinal lymphnodes by a disease such as tubercolosis, sarcoidosis,
immunodeficiency syndrome, lymphomas, or metastases
in, for example, Wilms tumour, neuroblastoma or retinoblastoma. Cardiomegaly in congenital heart disease
could produce atelectasis, especially of the left upper
bronchus, left main bronchus and middle bronchus.3
Different disorders which occupy space in the mediastinum, such as chylothorax, haemothorax, and pneumothorax may cause compression of normal lung.
Congenital abnormalities of the diaphragm (hernia, eventration, etc.) may produce atelectasis by occluding
bronchi by the displaced viscera.
Neuromuscular diseases such as spinal muscular atrophy or WerdnigHoffmann disease, the muscular dystrophies and the Guillain-Barre syndrome, characterized by
weakness of the diaphragm, are more rare causes of
atelectasis.
Surfactant deficiency or dysfunction causes increased
alveolar surface tension with consequent diffuse atelectasis; the most common cause is HMD, but pneumonia or
pulmonary oedema may affect surfactant dysfunction.
Surfactant insufficiency or inactivation are typical causes
of atelectasis in ARDS. ARDS in childhood may be precipitated by shock, sepsis, trauma, aspiration or inhalation
injury; these all produce surfactant dysfunction, which
leads to an increase in surface tension.
Presentation of atelectasis
The signs and symptoms of atelectasis are often non-specific: the disease, which leads to the obstruction, may
cause fever, cough, tachypnoea, wheezing, ronchi, and
chest pain. Furthermore, in the case of infections such as
bronchiolitis, bronchitis, pneumonia and tuberculosis and
with tumours, asthma and CF, the presence of atelectasis
does not change the clinical picture unless the obstructed
area is large. Suggestive signs of atelectasis are localized
reduced breath sounds or a constant wheeze. There may
also be reduced chest wall expansion. If the obstruction
involves a main bronchus, wheeze can be heard and
cyanosis and asphyxia may be present, with mediastinal
and cardiac displacement and elevation of the diaphragm.
Aspiration of a foreign body in a previously well child is
an acute respiratory emergency. If a large bronchus is
present immediate intervention is mandatory. If the foreign body is lodged in a smaller airway there may be a
symptom-free period, followed by infection in the area of
atelectasis causing fever, malaise and cough.
A full medical history and specific clinical characteristics may help to identify the aetiology of the atelectasis.
The patient with bronchopulmonary dysplasia exhibits a
276
D.G. PERONI AND A.L. BONER
neonatal history of HMD and mechanical ventilation;4 the
patient with CF may present with failure to and steatorrhea, but persistent wheezing may give a clue to the presence of atelectasis.5 Frequent vomiting or cough during
and immediately after feeding, especially in young babies,
suggests recurrent aspiration or gastroesophageal reflux.6
In asthma the presence of bronchial inflammation producing cellular debris and mucus plugs may cause airway
obstruction, which is particularly frequent in the right middle
lobe, leading to the so-called right middle lobe syndrome;
this characterizes most cases of persistent atelectasis in
childhood.7 The right middle lobe bronchus is longer than
other bronchi, starting at the bronchus intermedius after a
sharp angle, leading to retention of intrabronchial secretions.
The occurrence of migrating or rotating atelectasis
may be an early manifestation of neuromuscular diseases
such as WerdnigHoffman disease.8 Another rare cause
of intrabronchial obstruction with ensuing persistent
atelectasis, often accompanied by pneumonitis resistant
to therapy (with wheeze, and haemoptysis), is a bronchial
carcinoid tumour.9
Diagnosis of atelectasis
Once the diagnosis of atelectasis is suspected, chest radiographs using both the anterior-posterior and lateral projections are mandatory to document the presence, extent,
and distribution of the atelectasis (Fig. 1). Radiographically,
there can be problems differentiating atelectasis from simple lobar consolidation (Table 2).10 With consolidations the
alveoli are full of exudates and there is no significant loss of
lung volume. However, as the pneumonia clears, atelectasis
may develop because of mucus plugs or surfactant dysfunction. A more marked loss of volume in one lobe and compensatory emphysema in an accompanying lobe indicates
the presence of atelectasis. The difficulty in diagnosis is best
exemplified by atelectasis of the right middle lobe. In this
case, the loss of volume is so small it may appear as a dense
band, suggesting pleural thickening rather than an atelectatic
lobe.10 In atelectasis associated with greater loss of volume,
other radiographic findings may be useful (Table 2). With
loss of volume, the mediastinum shifts towards the involved
lung: with volume gain, such as a pleural effusion or a large
unilateral chest mass, it moves away from the involved lung.
The presence of a unilateral elevated diaphragm may also
suggest atelectasis, whereas it is unaffected in lobar pneu-
Figure 1 Chest X-rays using the antero-posterior and lateral
projections document the presence and distribution of atelectasis.
monia. With a pleural effusion the diaphragm may be displaced downwards and flattened on the side of the effusion. Ultrasonography may be useful in determining
whether the opacity represents fluid or collapsed lung.10
Differentiating atelectasis from lobar consolidation is a
common dilemma in the assessment of respiratory infections in children (Table 3). Viral infections commonly
cause lower respiratory tract infections in childhood,
whilst bronchial asthma causes atelectasis secondary to
mucous plugging; in some patients radiographic differentiation of atelectasis and pneumonia is very difficult, and in
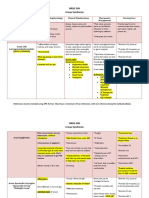
Table 2 Radiographic differences between atelectasis versus consolidation.
Lung volume loss
Compensatory emphysema
Mediastinum shift
Diaphragm position
Atelectasis
Consolidation
Marked
++
Toward lesion
Unilateral elevated
Not significant
Not significant
ATELECTASIS: MECHANISMS, DIAGNOSIS AND MANAGEMENT
277
Table 3 Radiological differentiation of atelectasis versus
consolidation: the pulmonary infiltrate patterns.
Type of infiltrate
Virus
Tuberculosis
Fungi (actinomycosis)
Pneumocystis carinii
Mycoplasma
Pertussis
Pneumococcus
Staphylococcus
Haemophilus
Aspiration pneumonia
Pulmonary haemorrhage
Asthma
Cystic fibrosis
Atelectasis
Consolidation
+++
+++
+
+++
+
+++
+++
+++
+
+
+/
+++
+/
+++
++
+++
++
+
+
+
such cases a clinical history is helpful. Coryza, nasal congestion and mild fever generally accompany viral infections; in asthma the consolidation is almost always due to
atelectasis, since bacterial pneumonia seldom precipitate
an acute asthma attack. If confusion remains, chest radiographic follow-up may be useful to demonstrate rapid
resolution, which is more rapid with atelectasis.
Peripheral atelectasis may be mistaken for a tumour
mass, in which case a CT scan is helpful.
Atelectasis may occur in any lobe or segment of the
lung, but the right and left lower lobes are the most frequently involved. The right middle lobe is vulnerable from
enlargement of the hilar lymph nodes and is also the most
commonly affected in asthma (Fig. 2).
In recurrent aspiration syndrome (usually caused by
milk aspiration in infants), the most frequently affected
lobes are the posterior areas of the upper and lower
lobes, because the infants lie supine for much of the day.
In toddlers or older children, who spend more time vertical, the lower lobes the lingula and the right middle lobe
are more frequently affected.6
Treatment of atelectasis
The treatment of atelectasis varies depending on the
cause, the duration and the severity. Respiratory infections are common causes of atelectasis in childhood, but
are generally transient (except TB) with resolution within
3 months following antimicrobial therapy.3 If the atelectasis does not resolve, bronchodilator inhalation and physiotherapy are performed.3 Aerosol therapy by inhalation
of jet-nebulized saline increases sputum volume and
clearance compared with physiotherapy alone.11 The use
of inhaled 2-agonists in patients with CF and bronchiectasis should be reserved for those who have demonstrated a clinical or lung function response to
bronchodilator.12
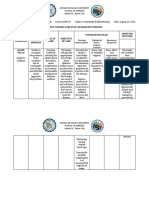
Figure 2 Atelectasis of the right middle lobe caused by extrinsic bronchial compression determined by enlargement of hylar
lymph nodes.
Chest physiotherapy is commonly used in paediatric
respiratory diseases: the benefit is thought to be due to
mobilization of secretions by huffing and coughing from
the smaller to the more central airways. Patients with
chronic pulmonary diseases, such as CF and ciliary dyskinesia, usually improve with antibiotics and regular home
chest physiotherapy. If atelectasis occurs in the intensive
care unit, in the postoperative period or during mechanical ventilation, postural drainage and chest percussion,
together with bronchodilator therapy, may help. When
atelectasis persists, bronchoscopy should be used to
investigate and remove the cause of the obstruction.
Resistant atelectases have been successfully treated by
positive pressure ventilation using a flexible bronchoscope inserted into a subsegmental bronchus
with a small balloon cuff at the distal end of the scope.13
The use of nebulized recombinant human Dnase I
(rhDNase), which hydrolyses bacterial and cellular DNA
present in sputum plugs, has been described in the management of a mechanically ventilated child with
asthma.14 It has also been used in patients with cystic
fibrosis.15 The diagnosis and early management of
atelectasis in children is important so as to optimize resolution and prevent permanent atelectasis with the possibility of irretrievable lung damage.
PRACTICE POINTS
In early childhood the airways are smaller and
more collapsible.
The signs and symptoms of atelectasis are often
non-specific.
The presence of atelectasis does not change the
clinical picture unless the obstructed area is
large.
In the case of persisting atelectasis, bronchoscopy should be considered.
278
RESEARCH DIRECTIONS
Differential diagnosis of migrating or rotating
atelectasis.
Greater understanding of mechanisms of surfactant insufficiency or inactivation.
Evaluation of chest physiotherapy programs.
Application of positive pressure ventilation via
flexible bronchoscope.
REFERENCES
1. Lung growth and development. In: Phelan, Olinsky, Robertson R
(eds). Respiratory illness in children. Oxford: Blackwell, 1994;
17.
2. Redding GJ. Atelectasis in childhood. Ped Clin North America 1984;
31: 891907.
3. Hazinski TA. Atelectasis. In: Chernick and Boat (eds). Kendigs disorders of the respiratory tract in children. Philadelphia: Saunders Co,
1998; 634641.
4. Kennedy SD. Lung function outcome in children of premature birth.
J Paediatr Child Health 1999; 35: 516521.
5. Ruzal-Shapiro C. Cystic fibrosis: an overview. Radiol Clin North Am
1998; 36: 143161.
D.G. PERONI AND A.L. BONER
6. Pulmonary complications of inhalation. In: Phelan, Olinsky,
Robertson R (eds) Respiratory illness in children. Oxford: Blackwell,
1994; 252268.
7. De Boeck K, Willems T, Van Gysel D, Corbeel L, Eeckels R.
Outcome after right middle lobe syndrome. Chest 1995; 108:
150152.
8. Leistikow EA, Jones NE, Josephson KD, de Sierra TM. Migrating
atelectasis in Werdnig-Hoffmann disease: pulmonary manifestations
in two cases of spinal muscular atrophy type 1. Pediatr Pulmonol
1999; 28: 149153.
9. Wang LT, Wilkins EW, Bode HH. Bronchial carcinoid tumors in
pediatric patients. Chest 1993; 103: 14261428.
10. Swischhuk LE, John SD. Differential diagnosis in pediatric radiology
Baltimore: Williams and Wilkins, 1995; 6478.
11. Conway J, Fleming JS, Perring S, Holgate ST. Humidification as an
adjunct to chest physiotherapy in aiding tracheo-bronchial clearance in patients with bronchiectasis. Respir Med 1992; 86:
109114.
12. Eber E, Oberwaldner B, Zach M. Airway obstruction and airway
wall instability in cystic fibrosis: the isolated and combined effect of
theophylline and sympathomimetics. Pediatr Pulmonol 1988; 4:
205212.
13. Krell WS, Prakash UB. Therapeutic bronchoscopy. In: Prakash UB
(ed). Bronchoscopy. New York: Raven Press, 1994.
14. Greally P. Human recombinant Dnase for mucus plugging in status
asthmaticus. Lancet 1995; 346: 14231442.
15. Harms H, Matouk E, Tournier G. Multicenter, open-label study of
recombinant human Dnase in cysti fibrosis patients with moderate
lung disease. Dnase International Study Group. Ped Pulmonol 1998;
26: 155161.
Você também pode gostar
- Neurodermatitis (Lichen Simplex Chronic)Documento26 páginasNeurodermatitis (Lichen Simplex Chronic)Yusran Ady FitrahAinda não há avaliações
- Timebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisNo EverandTimebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisNota: 3.5 de 5 estrelas3.5/5 (2)
- Batuk Kronik BerulangDocumento24 páginasBatuk Kronik BerulangHameldo Andika PattinasaranyAinda não há avaliações
- Ventikular Septal Defect FixDocumento18 páginasVentikular Septal Defect FixPutri Sari DewiAinda não há avaliações
- Walking Pneumonia, (Mycoplasma Pneumonia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandWalking Pneumonia, (Mycoplasma Pneumonia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- MeningitisDocumento20 páginasMeningitisAmalia Tri UtamiAinda não há avaliações
- Kuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)Documento17 páginasKuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)DillaAinda não há avaliações
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- Jurnal BronkiolitisDocumento10 páginasJurnal BronkiolitisAmi WilliamsAinda não há avaliações
- Hurler Syndrome (Biochem Repot)Documento5 páginasHurler Syndrome (Biochem Repot)Kristine Abegail CantillerAinda não há avaliações
- G IN A: Lobal Itiative For SthmaDocumento66 páginasG IN A: Lobal Itiative For SthmaNerissaArvianaShintaraAinda não há avaliações
- Pneumoconiosis PDFDocumento10 páginasPneumoconiosis PDFAnonymous lF3962RA1cAinda não há avaliações
- Overview of The Mucopolysaccharidoses: RheumatologyDocumento9 páginasOverview of The Mucopolysaccharidoses: RheumatologyLaura Orjuela MateusAinda não há avaliações
- Children With Henoch Schonlein Purpura 2.0Documento13 páginasChildren With Henoch Schonlein Purpura 2.0soniaAinda não há avaliações
- Gnaps EmedicineDocumento13 páginasGnaps Emedicineharyanti lupitaAinda não há avaliações
- Severe Acute Respiratory SyndromeDocumento11 páginasSevere Acute Respiratory SyndromeNick Arngel CorporalAinda não há avaliações
- Referat Kulit KakayDocumento26 páginasReferat Kulit KakayRezky Dwiputra FellanysAinda não há avaliações
- TB MeningitisDocumento11 páginasTB MeningitisMontserrat ÁlvarezAinda não há avaliações
- Pathogenesis of Systemic Sclerosis Scleroderma UpToDateDocumento27 páginasPathogenesis of Systemic Sclerosis Scleroderma UpToDateLê Hạ Long HảiAinda não há avaliações
- Pediatrics in Review-2013-Sahai-216-27Documento14 páginasPediatrics in Review-2013-Sahai-216-27Facu GuerreroAinda não há avaliações
- Pneumocystis Carinii PneumoniaDocumento16 páginasPneumocystis Carinii PneumoniaHera HeraAinda não há avaliações
- NRSG 206 Croup SyndromeDocumento3 páginasNRSG 206 Croup SyndromeGirlwithnonameAinda não há avaliações
- Pediatric Lupus NephritisDocumento9 páginasPediatric Lupus NephritisOtilia FrasinariuAinda não há avaliações
- Meningitis Pada AnakDocumento14 páginasMeningitis Pada AnakRayhanun MardhatillahAinda não há avaliações
- Jurnal RabiesDocumento19 páginasJurnal RabiesjenifermtAinda não há avaliações
- Sepsis Induced CholestasisDocumento12 páginasSepsis Induced CholestasisYusuf Hakim AjiAinda não há avaliações
- LimfadenitisDocumento24 páginasLimfadenitisrahmah ningsihAinda não há avaliações
- Gagal Napas: Pembimbing Dr. Ngakan Putu Parsama Putra, SPP (K) Presenter Dr. Muli YamanDocumento20 páginasGagal Napas: Pembimbing Dr. Ngakan Putu Parsama Putra, SPP (K) Presenter Dr. Muli YamanAdlan BinharyantoAinda não há avaliações
- 2017 Tubulointerstitial Nephritis, Diagnosis, Treatment, and MonitoringDocumento11 páginas2017 Tubulointerstitial Nephritis, Diagnosis, Treatment, and MonitoringbrufenAinda não há avaliações
- Penyakit Respirasi Pada AnakDocumento29 páginasPenyakit Respirasi Pada AnakyudhaAinda não há avaliações
- KriptorkismusDocumento14 páginasKriptorkismusMutiara Prima DianaAinda não há avaliações
- Acute Pulmonary Edema - NEJMDocumento4 páginasAcute Pulmonary Edema - NEJMSuzika Dewi0% (1)
- Neonatal JaundiceDocumento12 páginasNeonatal JaundiceGiska T PutriAinda não há avaliações
- Overview of Mallory - Weiss SyndromeDocumento3 páginasOverview of Mallory - Weiss SyndromeLeslyAgredaNavarroAinda não há avaliações
- Sindroma Metabolik Dislipidemia Dan ObesitasDocumento45 páginasSindroma Metabolik Dislipidemia Dan ObesitasLaurentius Juan WicaksonoAinda não há avaliações
- Pneumokoniosis ReferatDocumento7 páginasPneumokoniosis Referatbella yolandaAinda não há avaliações
- PPT DIARHEA IN CHILDRENDocumento31 páginasPPT DIARHEA IN CHILDRENRifka AnisaAinda não há avaliações
- Intermediate UveitisDocumento33 páginasIntermediate UveitismitaamayAinda não há avaliações
- K21-Fever With RashDocumento76 páginasK21-Fever With RashMarisa Perucana SinambelaAinda não há avaliações
- Japanese EncephalitisDocumento14 páginasJapanese EncephalitisMuhammad Rafli AkbarAinda não há avaliações
- Congenital Rubella Syndrome-Case ReportDocumento4 páginasCongenital Rubella Syndrome-Case ReportErlina WahyuAinda não há avaliações
- Drug EruptionDocumento46 páginasDrug EruptionSyahDikaAinda não há avaliações
- Respiratory Support For PneumoniaDocumento25 páginasRespiratory Support For Pneumoniamarte robiul saniAinda não há avaliações
- Management of Diabetic Ketoacidosis in Children and AdolescentsDocumento8 páginasManagement of Diabetic Ketoacidosis in Children and AdolescentsnurlatifahAinda não há avaliações
- DEN GU E: DengueDocumento53 páginasDEN GU E: Denguerose OAinda não há avaliações
- Neonatal SepsisDocumento17 páginasNeonatal SepsisDhilla Feroh Kesuma TAinda não há avaliações
- Cerebral Toxoplasmosis: Diagnosis & ManagementDocumento32 páginasCerebral Toxoplasmosis: Diagnosis & ManagementShinta DianAinda não há avaliações
- Daftar Kode Diagnosa & TindakanDocumento7 páginasDaftar Kode Diagnosa & Tindakannovi andriyaniAinda não há avaliações
- Asma - SansanDocumento15 páginasAsma - SansanAloysia SandraAinda não há avaliações
- TBC KutisDocumento37 páginasTBC KutisNycoAinda não há avaliações
- Hipertiroid HarrisonDocumento8 páginasHipertiroid HarrisonravenskaAinda não há avaliações
- Referat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Documento14 páginasReferat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Ahmad Fari Arief LopaAinda não há avaliações
- Anemi Aplastik Dan MielodisplasiaDocumento34 páginasAnemi Aplastik Dan MielodisplasiaRoby KieranAinda não há avaliações
- Topical Treatment of Common Superficial Tinea InfectionsDocumento8 páginasTopical Treatment of Common Superficial Tinea InfectionsColate LocoAinda não há avaliações
- Kuliah ADENOMYOSISDocumento38 páginasKuliah ADENOMYOSISmarajuuAinda não há avaliações
- Adrenal DisordersDocumento32 páginasAdrenal DisordersJyoti ChadhaAinda não há avaliações
- Patogenesis Patofisiologi Gejala KlinikDocumento4 páginasPatogenesis Patofisiologi Gejala KlinikAdrian KuswantoAinda não há avaliações
- Impacts of Antibiotic ResistanceDocumento3 páginasImpacts of Antibiotic ResistanceSajid RahimAinda não há avaliações
- Herpes Zoster PDFDocumento19 páginasHerpes Zoster PDFNicolás LaverdeAinda não há avaliações
- Phcist Letter Sept 2006Documento52 páginasPhcist Letter Sept 2006MichelAinda não há avaliações
- Learnin G Objectiv ESDocumento54 páginasLearnin G Objectiv ESKirk Matthew ZhuAinda não há avaliações
- DR - Thompsons CBC-RBC Indices Guide - A Guide To Red Blood Cell IndicesDocumento54 páginasDR - Thompsons CBC-RBC Indices Guide - A Guide To Red Blood Cell IndicesYohana SetiawanAinda não há avaliações
- Amisulprid 2Documento5 páginasAmisulprid 2Robert MovileanuAinda não há avaliações
- Basic First Aid NotesDocumento9 páginasBasic First Aid NotesPaul SealyAinda não há avaliações
- Dmso Natures Best HealerDocumento2 páginasDmso Natures Best HealerJan Pran100% (1)
- Prevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenDocumento10 páginasPrevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenRiszki_03Ainda não há avaliações
- Renal and Perinephric AbscessDocumento11 páginasRenal and Perinephric AbscessYusak DpAinda não há avaliações
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedDocumento12 páginasAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanAinda não há avaliações
- Antimalarial DrugsDocumento7 páginasAntimalarial DrugsHilmanAinda não há avaliações
- Hypertensive Crisis: - Alexter John C. Fajardo M.DDocumento49 páginasHypertensive Crisis: - Alexter John C. Fajardo M.DAlexter John Cabalonga FajardoAinda não há avaliações
- APFCB - Slides - Adrenal TestsDocumento61 páginasAPFCB - Slides - Adrenal TestsGPNAinda não há avaliações
- KSC WSSforKSCCQIDocumento34 páginasKSC WSSforKSCCQILệnhHồXungAinda não há avaliações
- FNCP - Inadequate Exercise & Breeding Site For MosquitoesDocumento2 páginasFNCP - Inadequate Exercise & Breeding Site For MosquitoesGwyneth Fisher100% (1)
- EmergencyDocumento7 páginasEmergencymedodiabAinda não há avaliações
- Initial Antimicrobial Management of Sepsis: Review Open AccessDocumento11 páginasInitial Antimicrobial Management of Sepsis: Review Open AccessblanquishemAinda não há avaliações
- Icra Longterms CareDocumento19 páginasIcra Longterms CareFajarRachmadiAinda não há avaliações
- Crohn Vs ColitisDocumento5 páginasCrohn Vs Colitiswbarnes7Ainda não há avaliações
- Laporan Jaga 5Documento44 páginasLaporan Jaga 5Dila AuAinda não há avaliações
- (Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDocumento490 páginas(Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDanalachi Adrian100% (2)
- Accesiblities of Accadamic For Students With Dis AblitiesDocumento8 páginasAccesiblities of Accadamic For Students With Dis AblitiesGuutaa DirbabaaAinda não há avaliações
- A Psychosomatic Perspective On Endometriosis - A MDocumento18 páginasA Psychosomatic Perspective On Endometriosis - A MsilsilviasilAinda não há avaliações
- Neck Pain ManagementDocumento35 páginasNeck Pain ManagementNur Elisaa100% (1)
- Postpartum Haemorrhage Dr. G. Al-ShaikhDocumento51 páginasPostpartum Haemorrhage Dr. G. Al-ShaikhRaphzid InurfaceAinda não há avaliações
- Virulence Factors of Streptococcus PyogenesDocumento6 páginasVirulence Factors of Streptococcus PyogenesAmador GielasAinda não há avaliações
- Obstetrics & Gynecologyc MnemonicsDocumento12 páginasObstetrics & Gynecologyc MnemonicsMuhammad Luqman Nul HakimAinda não há avaliações
- Liver BiopsyDocumento4 páginasLiver BiopsyLouis FortunatoAinda não há avaliações
- KetorolacDocumento2 páginasKetorolacDayanaj OngAinda não há avaliações
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (30)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (60)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (45)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNo EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNota: 4 de 5 estrelas4/5 (95)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)