Escolar Documentos
Profissional Documentos
Cultura Documentos
Medoralv10suppl2 I p154
Enviado por
Neira N SakinahTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Medoralv10suppl2 I p154
Enviado por
Neira N SakinahDireitos autorais:
Formatos disponíveis
Ciruga Bucal / Oral Surgery
Central odontogenic fibroma
Central odontogenic fibroma: A case report
Ugo Covani (1), Roberto Crespi (2), Nicola Perrini (3), Antonio Barone (2)
(1) Associate Professor and Chairman of Oral Pathology and Medicine School of Dental Medicine and Nanoworld Institute - University of
Genova, Italy
(2) Visiting Professor - Chair of Oral Pathology and Medicine School of Dental Medicine and Nanoworld Institute - University of Genova,
Italy
(3) Centro di Odontoiatria e Stomatologia F. Perrini - Pistoia, Italy
Correspondencia / Address:
Dott. Antonio Barone
Piazza Diaz 10
55041 Camaiore (Lu)
Italy
Fax: +39 0584 985334
Tel: +39 0584 98531
E-mail : barosurg@libero.it
Indexed in:
-Index Medicus / MEDLINE / PubMed
-EMBASE, Excerpta Medica
-Indice Mdico Espaol
-IBECS
Recibido / Received: 24-03-2005 Aceptado / Accepted: 18-05-2005
Covani U, Crespi R, Perrini N, Barone A. Central odontogenic
fibroma: A case report. Med Oral Patol Oral Cir Bucal 2005;10
Suppl2:E154-7.
Medicina Oral S. L. C.I.F. B 96689336 - ISSN 1698-4447
ABSTRACT
Objective: The aim of this case report was to analyze clinical and
histological features of a central odontogenic fibroma followed
up for 6 years after surgical excision.
Methods: A 26-year old Caucasian female was referred, reporting a painless gingival swelling in the buccal area of the
maxillary right canine. There were no other symptoms and no
recent history of pain. Her medical history was non-contributory.
Radiographic evaluation showed the presence of a radiolucent
area with well-defined margins. The lesion was surgically removed and histologically analysed.
Results: Histologic analysis showed a cellular fibroblastic tissue characterized by interwoven bundles of collagen densely
packed and absence of odontogenic epithelium. The surgical
site was monitored for 6 years after surgery with no signs of
recurrence.
Conclusion: The central odontogenic fibroma here reported
displayed a prominent quantity of collagen and absence of
odontogenic epithelium. The surgically removed lesion had a
favourable prognosis and no recurrence for the 6 year followup period.
Key words: Central odontogenic fibroma, endodontic disease/
diagnosis, oral tumors.
INTRODUCTION
The central odontogenic fibroma (COF) is a rare and benign
neoplasm that could appear very similar to the endodontic lesions and/or to the other odontogenic tumors (1, 2). This lesion
is considered to be derived from the mesenchymal tissue of
dental origin such as periodontal ligament, dental papilla, or
dental follicle. The central odontogenic fibroma consists of collagenous fibrous connective tissue containing varying amounts
of odontogenic epithelium (3). Connective tissue proliferation
can have different localizations and there exist both intraosseous (central) and gingival (peripheral) lesions designated as
odontogenic fibroma. While peripheral odontogentic fibroma
clearly represents a periodontal lesion, the central odontogenic
fibroma usually resembles an endodontic lesion and it is reported
in endodontic or oral pathology journals (4, 5).
Some authors in an international classification of oral tumors
have reported that some COF could contain varying amounts
of hard tissue resembling dysplastic cementum or bone (6).
Clinically, the central odontogenic fibroma could appear as
an asymptomatic expansion of the buccal or lingual cortical
plate, occurring in the mandible and in the maxilla with equal
frequency. In the maxilla the lesion appears frequently to involve
the anterior region, whereas in the mandible the lesion tends to
be located in the posterior area, involving the premolar and molar
areas. The radiological examinations of this lesion appear as an
area of radiolucency or as an area with a mixed radiodensity,
most of the time the lesions have well-defined boarders (7). The
central odontogenic fibroma has been described as a unilocular
(8, 9) or a multi-locular radiolucent lesion (10), root resorption
and displacement have also been reported in cases of more
severe lesions.
The aim of this case report was to analyze clinical and histological features of a central odontogenic fibroma, occurring in the
area of the maxillary canine and followed up for 6 years after
surgical excision.
154
Med Oral Patol Oral Cir Bucal 2005;10 Suppl2:E154-7.
CASE REPORT
A 26-year old Caucasian female was referred to us with a chief
compliant of painless gingival swelling in the buccal area of
the maxillary right canine. The patient reported slow growth
of the lesion during the last two years; she believed that the
small diastema present between the maxillary right canine and
lateral incisor was increasing. There were no other symptoms
and no recent history of pain. Her medical history was noncontributory.
The oral examination showed the presence of an enlargement
of the buccal maxillary right canine region, extending to the
area of the canine and first premolar. The overlaying mucosa
and gingiva were of normal colour and smooth in texture. The
canine appeared to have been slightly displaced by the lesion.
The mass was firm, raised, not tender and no fluctuation was
evident on manual palpation. All the teeth in the area were positive to thermal testing; percussion and palpation tests were within
normal limits. The needle biopsy did not give any result.
Radiographic evaluation showed the presence of a unilocular
radiolucent area between the maxillary right canine and first
premolar. The radolucency did not appear to involve the teeth
apices. The margins of the lesion appeared to be well-defined
(Fig. 1).
A comprehensive explanation was given to the patient, who
signed an informed consent.
An intrasulcular incision and two vertical releasing incisions
were made in order to better mobilize the full thickness flap
and a buccal flap was raised to give access to the lesion. An
absence of buccal cortical bone was observed, the limits of the
lesion were identified. The lesion, which was white and of stiffelastic consistency, was removed and enucleated intact. After
lesion removal a horizontal bone defect with no bony walls
was observed. The residual bone defect was vigorously and
thoroughly curretted and the exposed root surfaces were scaled
and planed with ultrasonic and hand instruments. The bone
defect did not reach the root apex areas of the adjacent teeth.
The mucoperiosteal flap was repositioned and primary closure
was achieved using 3/0 silk sutures. The patient was prescribed
amoxicillin, 2 gr, at the time of surgery, then 500 mg, 3 times
daily, for 5 days. The patient used chlorhexidine as a postoperative oral rinse for 30 days. Sutures were removed at 7 days after
surgery. Instructions were given to the patient to neither brush
nor floss the surgical area for the first 4 weeks and to continue
the chlorhexidine application to the surgical area.
The surgical site was monitored for 6 years after surgery with
no signs of recurrence and with a complete soft and hard tissue
healing (Fig. 2).
Histological examination of the lesion was carried out as follows:
the specimen was fixed in phosphate-buffered neutral formalin
for 1 day, subsequently, 5 micron paraffin sections were obtained
and stained with hematoxylin and eosin.
Histologic analysis of the tissue obtained from the specimen
showed a cellular fibroblastic tissue characterized by densely
packed interwoven bundles of collagen. The fibroblastic cells
were slightly elongated with thin and fusiform nuclei, which
appeared intensely stained. Many areas of the lesion showed a
Central odontogenic fibroma
random distribution of fibroblastic cells (Fig. 3), whereas some
other areas showed a distribution resembling an elongated rete
ridge. The lesion had a component of reactive hyperplastic collagen, which contributed to the overall size of the lesion.
Fig. 1. Periapical radiograph showing a radiolucent area with well-defined
margins in the maxillary right canine area.
Fig. 2. Periapical radiograph 6 years following surgical excision.
155
Ciruga Bucal / Oral Surgery
Fig. 3. Histologic features of biopsy specimen showing a cellular fibroblastic
tissue characterized by interwoven bundles of collagen densely packed and
absence of odontogenic epithelium. (Hematoxylin-eosin stain; original magnification X 150).
DISCUSSION
Although the Central Odontogenic Fibroma is a rare lesion of the
periodontium, general dentists and periodontists should consider
the presence of COF because this lesion closely resembles the
endodontic lesions. The COF lesion is often diagnosed in the
second and third decade of life.
In international literature a considerable age range was noted.
Some authors reported a distribution related to gender with a 2.2
to 1 ratio of women to men (11). The most frequently observed
sign was swelling and, moreover, several clinical cases showed
the presence of slowly-growing diastema, due to the dislocation of the adjacent teeth. Clinical symptoms such as pain and
paresthesia were uncommon.
The radiographic features of the central odontogenic fibroma
were compatible with radiolucent lesions with well-defined
boarders. The radiographic unilocular or multilocular aspect
of the lesions seemed to be dependent on the dimension of
the lesion. Small fibromas (about 2 cm) had a radiographic
unilocular appearance, whereas large lesions (about 4 cm) had
a radiographic multilocular appearance (12).
Many clinical cases of odontogenic fibroma showed a dislocation of adjacent teeth and, sometimes, root resorption. The case
reported in this study showed a unilocular radiolucent area with
well-defined boarders associated with the dislocation of adjacent
teeth without any sign of root resorption (13).
The radiographic features of the COF are similar to other peripheral odontogenic tumors such as traumatic bone cyst, ameloblastoma, odontogenic cyst and central giant cell granuloma (14). It
was originally thought that most of these lesions have multilocular radiolucencies, but the current reports showed that there were
more unilocular than multilocular radiolucencies ( 14).
The histologic differential diagnosis is based on the presence
of the reactive fibrous hyperplastic tissue, which may contain
occasional inactive odontogenic cells. A variety of mineralised
Central odontogenic fibroma
tissues such as bone, dentinoid or even cementum-like material may be found, sometimes associated with the odontogenic
epithelium.
According to the latest classification of odontogenic tumours
reported by Gardner (15), the odontogenic fibroma (OF) is
classified as a benign lesion derived from odontogenic ectomesenchyme with or without odontogenic epithelium. This
classification has been applied to various types of lesions,
characterized by the presence of connective tissue containing
islands and strands of odontogenic epithelium, and sometimes
associated with the presence of dystrophic calcification. The
author (15) reviewed the information concerning the central
odontogenic fibroma identifying lesions with two different histologic patterns. The first type, classified as simple, contained
fibrous tissue with various amounts of collagen and the second
type, which has been referred to as the WHO type or complex
type, contained fibrous tissue with myxoid area associated to
odontogenic epithelium. Moreover, dysplastic dentin and cementum-like material could be found.
Daniels has reported a case of central odonotgenic fibroma of
the right molar region of the mandible in a 30-year-old female
patients (16). The case being reported here occurred in the maxillary right canine region in a 26-year-old female. This case
report showed a lesion with cellular fibrous connective tissue
and collagen fibers arranged in interlacing bundles and absence
of odontogenic epithelium.
The central odontogenic fibroma is usually easily removed, not
showing any adherence to bone and/or to tooth structure. As seen
in the clinical case here reported, the lesion is slow-growing and
typical conservative surgical intervention including enucleation
and curettage has often proved to be successful. It should be
noted that, depending on the extent of the residual defect, the
bone regenerative procedure must be considered. In this case,
the morphology of the residual bone defect, which was filled
by a blood clot, did not require any guided bone regeneration.
Despite the fact that no regenerative procedures were performed,
a complete bone healing was observed, as shown by the radiographic examinations at the follow-up visits. Moreover, the
clinical examination showed a normal alignment of the teeth
previously dislocated. Few clinical cases reported in literature
had a recurrence which required more extensive surgical excision (3). Some other authors reported a clinical case which
had recurrence 9 years after surgery (17); in an another clinical
study the authors found recurrence of 2 cases out of 15 (18).
In conclusion, the clinical, radiological and histological aspects
of the case reported here were consistent with the diagnosis of
central odontogenic fibroma from periodontal ligament. The
lesion was surgically removed, the prognosis was favourable
and no recurrence of the lesion was observed until the 6 year
follow-up visit.
The periapical radiolucent lesions of non-endodontic origin
sometimes occur, and a proper diagnosis must be made. A
wrong initial diagnosis may delay or preclude the rendering of
proper treatment. Therefore, dentists must be aware of periapical lesions of non-endodontic origin. The clinical examination
should give serious consideration to the pulp vitality tests and
the radiographs should be diligently observed.
156
Med Oral Patol Oral Cir Bucal 2005;10 Suppl2:E154-7.
Central odontogenic fibroma
The findings from this case report point out the importance of
recommending to the patient periodic clinical and radiographic
examinations, and the importance of adequate pathological
expertise for histological examination of fibrous lesion of the
maxilla.
REFERENCES
1. Gardner DG. The peripheral odontogenic fibroma: an attempt at clarification.
Oral Surg Oral Med Oral Pathol 1982;54:40-8.
2. Dunlap CL. Odontogenic fibroma. Semin Diagn Pathol 1999;16:293-6.
3. Allen CM, Hammond HL, Stimson PG. Central odontogenic fibroma, WHO
type. A report of three cases with an unusual associated giant cell reaction.
Oral Surg Oral Med Oral Pathol 1992;73:62-6.
4, Gardner DG, Baker DC. Fibromatous epulis in dogs and peripheral odontogenic fibroma in human beings: two equivalent lesions. Oral Surg Oral Med
Oral Pathol 1991;71:317-21.
5. Huey MW, Bramwell JD, Hutter JW, Kratochvil FJ. Central odontogenic
fibroma mimicking a lesion of endodontic origin. J Endod 1995;21:625-7.
6. Kramer IR, Pindborg JJ, Shear M. The WHO Histological Typing of Odontogenic Tumours. A commentary on the Second Edition. Cancer 1992;70:
2988-94.
7. Kaffe I, Buchner A. Radiologic features of central odontogenic fibroma.
Oral Surg Oral Med Oral Pathol 1994;78:811-8
8. Hamner JE, Gamble JW, Gallegos GJ. Odontogenic fibroma: report of two
cases. Oral Surg Oral Med Oral Pathol 1966;21:113-9.
9. Scofield ID. Central odontogenic fibroma: report of case. J Oral Surg
1981;39:218-20.
10. Regezi JA, Sciubba JJ. Oral Pathology clinical-pathologic correlations. 3rd
edn. Philadelphia: WB Saunders 1993:383-5.
11. Neville BW, Damm DD, Allen CM, Bouquet JE. Oral and Maxillofacial
Pathology. 2nd ed. Philadelphia: WB Saunders; 2001.
12. Regezi JA. Odontogenic cysts, odontogenic tumors, fibroosseous, and giant
cell lesions of the jaws. Mod Pathol 2002;15:331-41.
13. Hwang E-H, Lee S-R. Central odontogenic fibroma of the simple type.
Korean J Oral Maxillofac Rad 2002;32:227-30.
14. Ramer M, Buonocore P, Krost B. Central Odontogenic fibroma- report of a
case and review of the literature. Periodont Clin Invest 2002;24:27-40.
15. Gardner DG. Central odontogenic fibroma: current concepts. J Oral Pathol
Med 1996;25:556-61.
16. Daniels JS. Central odontogenic fibroma of mandible: a case report and
review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2004;98:295-300.
17. Heimedal A, Isaacson G, Nilsson L. Recurrent odontogenic fibroma. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 1980;50:140-5.
18. Svirsky JA, Abbey LM, Kaugars GE. A clinical review of central odontogenic fibroma: with addition of 3 new cases. J Oral Med 1986;41:51-4.
157
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Neira Contemporary GTDocumento4 páginasNeira Contemporary GTNeira N SakinahAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Periodontal TerapiDocumento1 páginaPeriodontal TerapiNeira N SakinahAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Rats Molar ToothDocumento1 páginaRats Molar ToothNeira N SakinahAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Acute Necrotizing Ulcerative GingivitisDocumento4 páginasAcute Necrotizing Ulcerative GingivitisNeira N SakinahAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Quaternary Protoberberine Alkaloids (Must Read)Documento26 páginasQuaternary Protoberberine Alkaloids (Must Read)Akshay AgnihotriAinda não há avaliações
- Entrepreneurship Project On Jam, Jelly & PicklesDocumento24 páginasEntrepreneurship Project On Jam, Jelly & Picklesashish karshinkarAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Coleman Product PageDocumento10 páginasColeman Product Pagecarlozz_96Ainda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Organizing Small Items with Glass Bottle OrganizersDocumento70 páginasOrganizing Small Items with Glass Bottle OrganizersDy SaiAinda não há avaliações
- VA TearDownDocumento5 páginasVA TearDownfaj_larcfave5149Ainda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- 2 Scour VentDocumento8 páginas2 Scour VentPrachi TaoriAinda não há avaliações
- Chemistry Implementation: Name: Rasheed Campbell School: Kingston College Candidate #.: Centre #: 100057Documento12 páginasChemistry Implementation: Name: Rasheed Campbell School: Kingston College Candidate #.: Centre #: 100057john brownAinda não há avaliações
- Chain Surveying InstrumentsDocumento5 páginasChain Surveying InstrumentsSachin RanaAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- FP-XH PGRG eDocumento936 páginasFP-XH PGRG ebvladimirov85Ainda não há avaliações
- 1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFDocumento274 páginas1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFRobert Klitzing100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Chapter 16 - Energy Transfers: I) Answer The FollowingDocumento3 páginasChapter 16 - Energy Transfers: I) Answer The FollowingPauline Kezia P Gr 6 B1Ainda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Home Brewing Log Sheet PDFDocumento2 páginasHome Brewing Log Sheet PDFStefanita0% (1)
- GIS AccidentsDocumento5 páginasGIS Accidentsali110011Ainda não há avaliações
- AI Model Sentiment AnalysisDocumento6 páginasAI Model Sentiment AnalysisNeeraja RanjithAinda não há avaliações
- Indian Patents. 232467 - THE SYNERGISTIC MINERAL MIXTURE FOR INCREASING MILK YIELD IN CATTLEDocumento9 páginasIndian Patents. 232467 - THE SYNERGISTIC MINERAL MIXTURE FOR INCREASING MILK YIELD IN CATTLEHemlata LodhaAinda não há avaliações
- Cs8791 Cloud Computing Unit2 NotesDocumento37 páginasCs8791 Cloud Computing Unit2 NotesTeju MelapattuAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Letter of MotivationDocumento4 páginasLetter of Motivationjawad khalidAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Clean Milk ProductionDocumento19 páginasClean Milk ProductionMohammad Ashraf Paul100% (3)
- Ro-Buh-Qpl: Express WorldwideDocumento3 páginasRo-Buh-Qpl: Express WorldwideverschelderAinda não há avaliações
- TIA Selection Tool: Release Notes V2022.05Documento10 páginasTIA Selection Tool: Release Notes V2022.05Patil Amol PandurangAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Proposal Anguria Pasta NewDocumento24 páginasProposal Anguria Pasta NewNOOR IRDINA HAFIZAH BT TAUPISAinda não há avaliações
- IEQ CompleteDocumento19 páginasIEQ Completeharshal patilAinda não há avaliações
- Lesson 2 Socio Anthropological View of The SelfDocumento12 páginasLesson 2 Socio Anthropological View of The SelfAilyn RamosAinda não há avaliações
- Retaining Wall-Masonry Design and Calculation SpreadsheetDocumento6 páginasRetaining Wall-Masonry Design and Calculation SpreadsheetfarrukhAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Tds G. Beslux Komplex Alfa II (25.10.19)Documento3 páginasTds G. Beslux Komplex Alfa II (25.10.19)Iulian BarbuAinda não há avaliações
- Innovative Food Science and Emerging TechnologiesDocumento6 páginasInnovative Food Science and Emerging TechnologiesAnyelo MurilloAinda não há avaliações
- Troubleshooting Hydraulic Circuits: Fluid PowerDocumento32 páginasTroubleshooting Hydraulic Circuits: Fluid PowerMi LuanaAinda não há avaliações
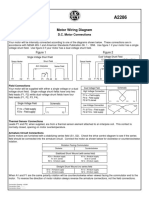
- Motor Wiring Diagram: D.C. Motor ConnectionsDocumento1 páginaMotor Wiring Diagram: D.C. Motor Connectionsczds6594Ainda não há avaliações
- Sri Radhakrishna SwamijiDocumento43 páginasSri Radhakrishna SwamijiNarayana IyengarAinda não há avaliações
- B. Pharmacy 2nd Year Subjects Syllabus PDF B Pharm Second Year 3 4 Semester PDF DOWNLOADDocumento25 páginasB. Pharmacy 2nd Year Subjects Syllabus PDF B Pharm Second Year 3 4 Semester PDF DOWNLOADarshad alamAinda não há avaliações