Escolar Documentos
Profissional Documentos
Cultura Documentos
Ap3 1465 W Wiedermann
Enviado por
andaanda4660 notas0% acharam este documento útil (0 voto)
7 visualizações2 páginasthanks
Título original
Ap3 1465 w Wiedermann
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentothanks
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
7 visualizações2 páginasAp3 1465 W Wiedermann
Enviado por
andaanda466thanks
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 2
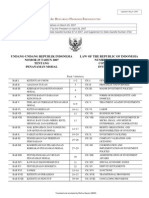
Introduction
Objective:
Has there been quality improvement?
Long-term trends of quality indicators in 58 Swiss
hospitals
Wolfgang Wiedermann a,b
Dirk Wiedenhfer c
Barbara Eckl c
Ulrich Frick a,d,e
Method:
a) Research Institute on Public Health and Addiction, University of Zurich, Switzerland
b) Faculty of Psychology, University of Vienna, Austria
c) Health Care Research Institute AG, Zurich, Switzerland
d) Psychiatric University Hospital, University of Regensburg, Germany
e) Dept. Health Care Management, Carinthia University of Applied Sciences, Austria
To determine the potential impact of annual quality reports on
service delivery.
Analysis of long-term trends in incidence of pressure ulcer (PU),
anesthesia complications (AC) and patients or after caring
institutions discharge dissatisfaction (DD).
Clinical and sociodemographic data were reported to an
independent data centre between 2001 and 2011.
PU (n = 179,256; 58 hospitals) and AC (n = 69,899; 53 hospitals) were
registered via expert judgments. DD (n = 15,116; 31 hospitals) was
registered via self-administered questionnaires.
Statistical Analysis: Multilevel modelling approach (2 levels of
variables: patient and hospital characteristics; + historical time).
Pressure Ulcer:
Introduction
Objective:
pressure ulcer rates (relative frequencies)
Results
Decline in crude rates from 2.6% to 1.6%
Observation period: 2004 2010
To determine the potential impact of annual quality reports on
service delivery.
Analysis of long-term trends in incidence of pressure ulcer (PU),
anesthesia complications (AC) and patients or after caring
institutions discharge dissatisfaction (DD).
Patients age, gender, LOS, degree of health impairment,
and health insurence coverage beyond legal minimum (HIC)
were significantly related to PU risk (+ seasonal component).
Adjusted PU risk declined during the 6 yrs (OR = 0.998 per
month) & significant differences across hospitals and time
trends (age, LOS, and HIC proportion related to PU risk).
Anesthesia Complications:
Method:
Clinical and sociodemographic data were reported to an
independent data centre between 2001 and 2011.
PU (n = 179,256; 58 hospitals) and AC (n = 69,899; 53 hospitals) were
registered via expert judgments. DD (n = 15,116; 31 hospitals) was
registered via self-administered questionnaires.
Statistical Analysis: Multilevel Modeling (incl. patient and hospital
characteristics and historical time).
Intended increase in AC rates (2% vs. 6% since 2006)
due to a more sensitive documentation form.
Since 2006: Decrease in AC risk suggests quality
improvement (OR = 0.997 per quarter).
Significant hospital differences after adjusting for
gender, HIC, intubation, seasonal components and ASA
risk-score.
Discharge Dissatisfaction:
Stable DD proportions over 5 yrs (~ 30%).
Patients age, LOS, involvement of GP and/or after caring
institutions as well as emegency admissions were
significantly related to DD risk.
Additionally significant differences across wards.
After Adjustment: Larger hospitals display higher DD risks.
only 44 observations
Take Home Messages
Take Home Messages
Service delivery can be supported by annual quality
reports across hospitals.
Quality indicators under control of health professionals
(such as PU or AC) seem more sensitive for quality
change.
Complex and uncontrollable indicator (patient reported
outcomes) seem less sensitive for quality change.
Patient reported outcomes seem useful for identifying
hospital differences (bechmarking, best-practice
models).
Service delivery can be supported by annual quality
reports across hospitals.
Quality indicators under control of health professionals
(such as PU or AC) seem more sensitive for quality
change.
Complex and uncontrollable indicator (patient reported
outcomes) seem less sensitive for quality change.
Patient reported outcomes seem useful for identifying
hospital differences (bechmarking, best-practice
models).
Definition of PU
Definition of AC
Stage 0: no pressure ulcer
Stage 1: intact skin with nonblanchable redness
Stage 2: Partial thickness loss of dermis
Stage 3: Full thickness tissue loss of dermis
Stage 4: Full thickness tissue loss of dermis with exposed bone,
tendon, muscle; necrosis
2001 2005:
Unplaned ventilation after surgery
Re-intubation within one hour after primary extubation
Injuries of skin or nerves
Medication errors
Other injuries due to anesthesia
Hypothermia < 35 C
A) Existing PU with deterioration
Stage at admission > 1.
Stage increases > 0.
B) Incidence of PU
Additionally since 2006:
Nausea in recovery room
Dental injuries
Perioperative pressure ulcers
Multilevel Modelling: PU
Level 1
log[p/(1 p)] = 0 + 1 nursing home + 2 LOS + 3 age
+ 4 gender + 5 emergency admission + 6 HIC
+ 7 time + 8 QM-participation
+ 9 discharging ward + 10 GP + 11 month
Level 2
0 = 00 + 01 mean LOS + 02 prop. females
+ 03 mean age + 04 bed-capacity + u00
Random Intercept
1 = 10
2 = 20
k = k0 + k1 mean LOS + uk0
Random Slope
6 = 60
7 = 70
Você também pode gostar
- Clinical case in the emergency room of a patient with an ischemic strokeNo EverandClinical case in the emergency room of a patient with an ischemic strokeAinda não há avaliações
- Nursing care process in patients with chronic obstructive pulmonary diseaseNo EverandNursing care process in patients with chronic obstructive pulmonary diseaseAinda não há avaliações
- 158 Nausea - Vomiting ScaleDocumento9 páginas158 Nausea - Vomiting ScaleMas Indra ShuAinda não há avaliações
- Predictive RuleDocumento7 páginasPredictive RuleRci Club BucurestiAinda não há avaliações
- Journal Club: Dr. Shereen S. LucmanDocumento36 páginasJournal Club: Dr. Shereen S. LucmanShereen DS LucmanAinda não há avaliações
- Recurrent Tonsillitis in Adults: MedicineDocumento7 páginasRecurrent Tonsillitis in Adults: MedicineAnnizada Intan PratiwiAinda não há avaliações
- The Readmission Rate and Medical Cost of PatientsDocumento42 páginasThe Readmission Rate and Medical Cost of PatientsZulvikar UmasangadjiAinda não há avaliações
- Prevalence of Preoperative Anxiety and Its Relationship With Postoperative Pain in Foot Nail Surgery: A Cross-Sectional StudyDocumento10 páginasPrevalence of Preoperative Anxiety and Its Relationship With Postoperative Pain in Foot Nail Surgery: A Cross-Sectional StudyburhanAinda não há avaliações
- Chronic Pain and Quality of Life After Inguinal HerniaDocumento13 páginasChronic Pain and Quality of Life After Inguinal HerniaWilliam SonyoAinda não há avaliações
- Effect of A Pediatric Early Warning System On All-Cause Mortality in Hospitalized Pediatric PatientsDocumento35 páginasEffect of A Pediatric Early Warning System On All-Cause Mortality in Hospitalized Pediatric PatientsabdfaqihAinda não há avaliações
- Wound Closure Technique and Acute Wound Complication in Gastric Surgery For Morbid ObesityDocumento13 páginasWound Closure Technique and Acute Wound Complication in Gastric Surgery For Morbid ObesitywhcaoAinda não há avaliações
- The Influence of Perioperative Care and Treatment On The 4-Month Outcome in Elderly Patients With Hip FractureDocumento12 páginasThe Influence of Perioperative Care and Treatment On The 4-Month Outcome in Elderly Patients With Hip FractureResti LovitaAinda não há avaliações
- 10 1016@j Jmig 2018 08 005Documento24 páginas10 1016@j Jmig 2018 08 005Putri Tamara DasantosAinda não há avaliações
- UnsafeDocumento60 páginasUnsafejose ramosAinda não há avaliações
- ICU Orientation ManualDocumento107 páginasICU Orientation Manualhery100% (2)
- The Readmission Rate and Medical Cost of PatientsDocumento42 páginasThe Readmission Rate and Medical Cost of PatientsZulvikar UmasangadjiAinda não há avaliações
- Highlight Bubu 2Documento7 páginasHighlight Bubu 2soniAinda não há avaliações
- 2 General Principles of Research Design and AnalysisDocumento6 páginas2 General Principles of Research Design and AnalysisMohamed Elprince AdelAinda não há avaliações
- Bjs 11477Documento11 páginasBjs 11477sidraAinda não há avaliações
- The Value of Preoperative Pulmonary Assessment in Predicting Postoperative Pulmonary ComplicationsDocumento47 páginasThe Value of Preoperative Pulmonary Assessment in Predicting Postoperative Pulmonary ComplicationsDr. Hadika Pramana, SpPDAinda não há avaliações
- Ifferential Iagnosis: in This SectionDocumento11 páginasIfferential Iagnosis: in This SectionKiana TehraniAinda não há avaliações
- The Haematology Patient ICU - BP PDFDocumento34 páginasThe Haematology Patient ICU - BP PDFAnonymous Chb8DdaAinda não há avaliações
- GIQLIDocumento7 páginasGIQLIMazyAinda não há avaliações
- Pandini Et Al., 2016Documento6 páginasPandini Et Al., 2016mackenzie.lacey28Ainda não há avaliações
- Participating in The Surviving Sepsis Campaign: How It Can Help You!Documento41 páginasParticipating in The Surviving Sepsis Campaign: How It Can Help You!Tahira ZartashtAinda não há avaliações
- File Jurnal VertigoDocumento12 páginasFile Jurnal VertigoChris JohnAinda não há avaliações
- A Follow Up Study of Psychological Problems After StrokeDocumento1 páginaA Follow Up Study of Psychological Problems After StrokeJodiMBrownAinda não há avaliações
- Blunt Trauma AbdomenDocumento2 páginasBlunt Trauma AbdomenPadmaja DurgaAinda não há avaliações
- EC EBM Presentation Template-ExpandedDocumento28 páginasEC EBM Presentation Template-ExpandedErgon ÇoçajAinda não há avaliações
- Bjs 11477Documento12 páginasBjs 11477angelAinda não há avaliações
- Perception and Use of The Results of Patient Satisfaction Surveys by Care Providers in A French Teaching HospitalDocumento6 páginasPerception and Use of The Results of Patient Satisfaction Surveys by Care Providers in A French Teaching HospitalSagor AhmedAinda não há avaliações
- Tese SnotDocumento16 páginasTese SnotCaio GonçalvesAinda não há avaliações
- Pattern MiningDocumento22 páginasPattern MiningShameek GhoshAinda não há avaliações
- Prospective Study of Pain, Quality of Life and The Economic Impact of Open Inguinal Hernia RepairDocumento7 páginasProspective Study of Pain, Quality of Life and The Economic Impact of Open Inguinal Hernia RepairkaisalanaafidaAinda não há avaliações
- British Journal of Surgery - 2020 - Small - Acute Postoperative Pain ManagementDocumento11 páginasBritish Journal of Surgery - 2020 - Small - Acute Postoperative Pain ManagementkyleAinda não há avaliações
- Astrology and Mental Health Outcomes or Why Data Mining Is SuspectDocumento52 páginasAstrology and Mental Health Outcomes or Why Data Mining Is Suspectjbeebe2Ainda não há avaliações
- Aldrete 4Documento7 páginasAldrete 4Widhiasmara BawaAinda não há avaliações
- Endocarditis InfecciosaDocumento12 páginasEndocarditis InfecciosaJavier Agustín Holloway Sahli100% (1)
- Antibiotics 02 00001Documento10 páginasAntibiotics 02 00001Jenny AlmagroAinda não há avaliações
- Delirium in Mechanized PacientsDocumento10 páginasDelirium in Mechanized PacientsGabrielSteffenAinda não há avaliações
- Community-Acquired Pneumonia (CAP) : Why FocusDocumento4 páginasCommunity-Acquired Pneumonia (CAP) : Why FocusYoni KomalasariAinda não há avaliações
- Final Edit Synopsis RUPS PDFDocumento20 páginasFinal Edit Synopsis RUPS PDFAMSP IPGMERAinda não há avaliações
- Are Hospital Process Quality Indicators PDFDocumento7 páginasAre Hospital Process Quality Indicators PDFJOMAR HIJAPON PACINIOAinda não há avaliações
- Clinical Decision Support Systems: Syed Tirmizi, M.DDocumento94 páginasClinical Decision Support Systems: Syed Tirmizi, M.DgopiAinda não há avaliações
- Understanding Patient Provider Conversations: What Are We Talking About?Documento1 páginaUnderstanding Patient Provider Conversations: What Are We Talking About?drartzAinda não há avaliações
- VISION Study 2018Documento8 páginasVISION Study 2018Pia Shiela BadongAinda não há avaliações
- Eliminating Hospital Acquired Infections: Is It Possible? Is It Sustainable? Is It Worth It?Documento33 páginasEliminating Hospital Acquired Infections: Is It Possible? Is It Sustainable? Is It Worth It?drive_yugoAinda não há avaliações
- How, in Principle, Should Quality of Care Be Measured?Documento4 páginasHow, in Principle, Should Quality of Care Be Measured?Feronika ekaAinda não há avaliações
- Medical AuditDocumento6 páginasMedical Auditanantarao100% (1)
- Background: Information About Critically Ill Patients WithDocumento19 páginasBackground: Information About Critically Ill Patients WithamochiteamoAinda não há avaliações
- Adherence To Surgical Care Improvement Project Measures and The Association With Postoperative InfectionsDocumento7 páginasAdherence To Surgical Care Improvement Project Measures and The Association With Postoperative InfectionsBayu SunaryoAinda não há avaliações
- ModifiedDocumento18 páginasModifiedHrishikeshAinda não há avaliações
- Jurnal 5Documento9 páginasJurnal 5raraAinda não há avaliações
- EJHC Volume 13 Issue 1 Pages 528-545Documento18 páginasEJHC Volume 13 Issue 1 Pages 528-545Anna IndriastutiAinda não há avaliações
- Population HealthDocumento20 páginasPopulation HealthtiffylolaAinda não há avaliações
- Hospital Quality IndicatorsDocumento32 páginasHospital Quality Indicatorsakhtarulmunim2279Ainda não há avaliações
- Death and DischargeDocumento18 páginasDeath and DischargeBala GaneshAinda não há avaliações
- PCT SistemikfgDocumento7 páginasPCT SistemikfgAndi BintangAinda não há avaliações
- POCT Pros and ConsDocumento15 páginasPOCT Pros and ConsScientist Bernard EkhatorAinda não há avaliações
- EbpDocumento44 páginasEbpapi-356127291Ainda não há avaliações
- Internal Change Request FormDocumento2 páginasInternal Change Request Formandaanda466Ainda não há avaliações
- Module 1 PDFDocumento42 páginasModule 1 PDFandaanda466Ainda não há avaliações
- Contoh JurnalDocumento8 páginasContoh Jurnalreza_bustamiAinda não há avaliações
- Water SupplyDocumento30 páginasWater Supplysofianina05Ainda não há avaliações
- COW Water Jan2011Documento7 páginasCOW Water Jan2011LWYenAinda não há avaliações
- Klasifikasi GastritisDocumento15 páginasKlasifikasi Gastritisroropuji0% (1)
- Routine Data in German Hospitals: Jürgen Stausberg, MD, PHDDocumento31 páginasRoutine Data in German Hospitals: Jürgen Stausberg, MD, PHDandaanda466Ainda não há avaliações
- Universitas Sumatera UtaraDocumento2 páginasUniversitas Sumatera UtaraYosdim Si SulungAinda não há avaliações
- Ipi 267375Documento7 páginasIpi 267375andaanda466Ainda não há avaliações
- Gujarat SuratDocumento5 páginasGujarat Suratandaanda466Ainda não há avaliações
- IND-ENG-UU 25-2007 Penanaman ModalDocumento41 páginasIND-ENG-UU 25-2007 Penanaman ModalVelliana TanayaAinda não há avaliações
- PDF Vol 14-01-06Documento9 páginasPDF Vol 14-01-06Sulistyawati WrimunAinda não há avaliações
- Jurnal Manajemen Pelayanan Kesehatan: Artikel PenelitianDocumento6 páginasJurnal Manajemen Pelayanan Kesehatan: Artikel PenelitiankevinrestuAinda não há avaliações
- Group 11 Research ReportDocumento18 páginasGroup 11 Research ReportjoesayikAinda não há avaliações
- Principles of Anatomy and Physiology Tortora 14th Edition Test BankDocumento11 páginasPrinciples of Anatomy and Physiology Tortora 14th Edition Test BankTeri Thompson100% (30)
- Homemade Detox Drinks That WorkDocumento1 páginaHomemade Detox Drinks That WorkPure-Detox100% (1)
- Accredited ClinicsDocumento40 páginasAccredited ClinicsatescandorAinda não há avaliações
- Blood Cold ChainDocumento74 páginasBlood Cold Chainشريف عبد المنعمAinda não há avaliações
- VRPIN 01843 PsychiatricReportDrivers 1112 WEBDocumento2 páginasVRPIN 01843 PsychiatricReportDrivers 1112 WEBeverlord123Ainda não há avaliações
- Renal Function TestsDocumento31 páginasRenal Function TestsPhysiology by Dr RaghuveerAinda não há avaliações
- Mosquitoe Repellent Plants Final 31 AugustDocumento48 páginasMosquitoe Repellent Plants Final 31 AugustHomero SilvaAinda não há avaliações
- Digestive SystemDocumento41 páginasDigestive Systemhorace hernandez0% (1)
- Sleep Apnea: Dr. Goldfried P. Sianturi, SP.SDocumento4 páginasSleep Apnea: Dr. Goldfried P. Sianturi, SP.SDyanAqshaAinda não há avaliações
- FileVT0310 PR HorneCEDocumento6 páginasFileVT0310 PR HorneCEHassim M H SAinda não há avaliações
- Surgical Sutures-10Documento25 páginasSurgical Sutures-10badar_aqAinda não há avaliações
- A Group Analysis Evaluation of The Class Insecta in Terms of Known Materia MedicaDocumento163 páginasA Group Analysis Evaluation of The Class Insecta in Terms of Known Materia MedicaYASIR KHANAinda não há avaliações
- Locate Us Disclaimer: DSC ClinicDocumento2 páginasLocate Us Disclaimer: DSC ClinichanchiangAinda não há avaliações
- Roots, Prefix, Suffix Relative Meaning Sample WordDocumento27 páginasRoots, Prefix, Suffix Relative Meaning Sample WordChandramouli PathanjaliAinda não há avaliações
- Job Responsibilities of Medical Officer and Other StaffDocumento18 páginasJob Responsibilities of Medical Officer and Other StaffAlpit Gandhi100% (4)
- Dental Office Incident ReportDocumento2 páginasDental Office Incident ReportXYZAinda não há avaliações
- Physiologic Transition From Intrauterine To Extrauterine LifeDocumento12 páginasPhysiologic Transition From Intrauterine To Extrauterine Lifeyhojar PisfilAinda não há avaliações
- Rashtriya Bal Swasthya Karykram (RBSK) : Answer All QuestionsDocumento4 páginasRashtriya Bal Swasthya Karykram (RBSK) : Answer All Questionspvaibhav08Ainda não há avaliações
- Quality Control in Homoeopathy: DefinitionDocumento3 páginasQuality Control in Homoeopathy: Definition11 Isha ChitnisAinda não há avaliações
- Healthpoint SeptemberDocumento4 páginasHealthpoint SeptemberngochasfAinda não há avaliações
- Bear 1000Documento2 páginasBear 1000elabsAinda não há avaliações
- Anatomy and Physiology of Animals/Body Organisation: Read BookDocumento10 páginasAnatomy and Physiology of Animals/Body Organisation: Read BookIni UsenAinda não há avaliações
- Msds Asam MefenamatDocumento6 páginasMsds Asam MefenamatKristal Resa Diena RAinda não há avaliações
- Running Head: Normal Saline vs. Heparin 1Documento9 páginasRunning Head: Normal Saline vs. Heparin 1MaureenAmilcaAinda não há avaliações
- Neoplasia ExamDocumento9 páginasNeoplasia ExamYheng Gaosaii100% (1)
- Insurance Implications of DSM-5: Frequently Asked QuestionsDocumento4 páginasInsurance Implications of DSM-5: Frequently Asked QuestionszaneaxtenAinda não há avaliações
- Australian Pharmacy Council LTD Intern Written Exam Sample 2Documento61 páginasAustralian Pharmacy Council LTD Intern Written Exam Sample 2Chidi Njoku100% (3)
- Polarity Farming EnglishDocumento13 páginasPolarity Farming EnglishPere SubiranaAinda não há avaliações
- Sickle CellDocumento21 páginasSickle CellLeon0% (1)