Escolar Documentos
Profissional Documentos
Cultura Documentos
Afib Flowchart 1-21 SLW
Enviado por
Indra WijayaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Afib Flowchart 1-21 SLW
Enviado por
Indra WijayaDireitos autorais:
Formatos disponíveis
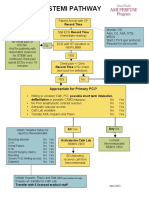
ED observation protocol for hemodynamically stable atrial fibrillation
Consider differential diagnosis for afib: PE, thyroid disease, intoxication, withdrawal, valvular disease,
infection. Evaluate and treat associated conditions as indicated.
Excluded from ED pathway:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Known intracardiac thrombus*
Signs of heart failure*
Known EF<30%*
Angina
Acute MI within 4 weeks
Stroke/TIA within 3 months
Renal dysfunction
CHA2DS2-VASC score 5
Other comorbid conditions that
require admission
*Consider bedside echo
Yes
No
Hospital admission
Consider CBC
Consider BMP
TSH if new diagnosis
INR if on warfarin
Echo if no recent echo and possible to obtain
OR can get echo as an outpatient
Appropriate for
immediate
cardioversion?
Appropriate for cardioversion after
observation period:
AF<48 hours at end of planned obs
period AND
Need to address other issue prior
to CV
OR for pill in pocket strategy (3)
OR for rate control and monitoring
for spontaneous cardioversion
AF Continues
at 8 hours
Initiate AC
Rate control (2)
Expert consultation as
needed
Utilize CDU if appropriate
Cardioversion
Rate control (HR<100) and
pt asymptomatic
Continued AF
Discharge
Cardiovert ,
assess need
for AC(1), and
discharge
Rate control strategy
desired
Sinus rhythm:
- Assess need for AC (1)
- Early PCP F/U
- consider arranging
cards F/U
Yes
Symptomatic or not
rate controlled
Admit
-monitor 1-2 hours, ambulate
patient
-Home AC and rate control
meds
- Early PCP F/U
- consider arranging cards
F/U
Discharge
1. Calculate CHA2DS2-VASc Score:
CHF
1
1
Hypertension
Age >/= 75
Diabetes Mellitus
History of stroke or TIA
Vascular disease (prior MI, PAD,
or aortic plaque)
1
1
Age 65-74 years
Female gender
0: Reasonable to omit antithrombotic therapy
1: No anticoagulation OR aspirin OR oral anticoagulation may be considered
>/= 2: Oral anticoagulation
Consider contraindications to AC
Preferred anticoagulants in patients without severe renal dysfunction (CrCl<30) are
apixaban and rivaroxaban. Options below adapted from MMC/MaineHealth Clinical
Guideline for Anticoagulation in Atrial Fibrillation:
Age <80 years:
Weight
60-100kg**
Apixaban 5mg bid
>50 mL/min
Rivaroxaban 20 mg daily
Dabigatran 150mg bid
Warfarin
Apixaban 2.5mg bid*
Apixaban 5mg bid*
30-50 mL/min
Rivaroxaban 15 mg daily
Rivaroxaban 15 mg daily
Warfarin
Dabigatran 150mg bid
Warfarin
<30 mL/min
Warfarin; not appropriate for ED management protocol, consider
admission
*Apixaban MAY be preferred in lower weight patients and those with poor renal function due
to increased bleeding risk but data is very limited; rivaroxaban may be chosen in these
patients if preferable for other reasons
CrCl
<60 kg
Apixaban 5mg bid*
Rivaroxaban 20 mg daily
Warfarin
**Clinical trials of NOACs did not include large numbers of patients with body weight
>100kg, thus their efficacy in AF patients is not well understood; Pharmacokinetic studies
demonstrated no definitive alterations in drug concentrations of dabigatran, rivaroxaban, and
apixaban in patients up to 110kg, 140kg, and 120kg, respectively.
Please refer to MMC Clinical Guideline for Anticoagulation in Atrial Fibrillation for further
guidance in patients >80 years old and special cases. Consider consultation with MMC
anticoagulation pharmacy specialist if needed: 741-7933.
2. Initial treatment with IV beta-blocker or nondihydropyridine calcium channel blocker, then
convert to long acting medications:
IV
PO
Timing
Metoprolol 5mg IV q
15 minutes
Metoprolol succinate
XL 25-50 mg daily
Give PO at same time
as first IV dose
Diltiazem10-20 mg IV
push over 10-20 min
Diltiazem LA 120-240
mg po daily
Give po dose if initial
IV dose achieves rate
control and infusion is
not planned
Diltiazem infusion 5-15
mg /hr
IV rate
PO dose
2.5mg/h
120mg
Turn off IV infusion 1
hour after PO dose is
given
5mg/h
180mg
7.5mg/h
240mg
10mg/h
300mg
12.5mg/h
360mg
15mg/h
480mg
Notes
Diltiazem is preferred
for patients with
asthma or COPD
Goal HR is < 100. After this has been achieved, monitor patient for 1-2 more hours and ensure
patient can ambulate prior to discharge
Short acting medications may be chosen if there are severe financial constraints: metoprolol 50 mg
po bid, diltiazem 30 mg po tid. Strongly consider involving care management/pharmacy as long
acting medications are preferable.
2. Pill-in-pocket strategy:
a. AVOID in patients with known structural heart disease including history of MI,
congenital abnormalities, NICM. Consider discussion with cardiology consultant if
unsure about appropriateness for pill-in-pocket strategy
b. Administer flecainide 200 mg po if <70 kg, 300 mg if 70 kg
c. Success rates for cardioversion are reported at 58-95%
d. Patients should be monitored for 8 hours after drug administration on telemetry.
Transient aflutter with rapid ventricular rate occurs in about 1% of patients.
Você também pode gostar
- Af NoteDocumento6 páginasAf NoteMohammed SadoonAinda não há avaliações
- CCU HandoverDocumento9 páginasCCU Handoverapi-192342497Ainda não há avaliações
- Afib Protocol Exclusion CriteriaDocumento3 páginasAfib Protocol Exclusion CriteriaJesse M. MassieAinda não há avaliações
- Anticoagulant Pocket GuideDocumento8 páginasAnticoagulant Pocket GuideDrew John Minardi100% (2)
- Atrial Fibrillation 2022Documento29 páginasAtrial Fibrillation 2022daniel mitikuAinda não há avaliações
- UHS Anticoagulation Therapy Guideline Y12 04Documento7 páginasUHS Anticoagulation Therapy Guideline Y12 04staylor235Ainda não há avaliações
- Deep Vein ThrombosisDocumento4 páginasDeep Vein ThrombosisStefania CristinaAinda não há avaliações
- 2014 AHA/ACC/HRS Guideline For The Management of Patients With Atrial Fibrillation: Executive SummaryDocumento32 páginas2014 AHA/ACC/HRS Guideline For The Management of Patients With Atrial Fibrillation: Executive SummaryprobowurAinda não há avaliações
- Mini Warfarin GuidelinesDocumento2 páginasMini Warfarin GuidelinesPeunn NattaphatAinda não há avaliações
- 1210 DIASTOLIC HypertensionDocumento44 páginas1210 DIASTOLIC HypertensionBoysz TheBestAinda não há avaliações
- Anticoagulation Protocol For PostDocumento8 páginasAnticoagulation Protocol For PostMohammed IbrahimAinda não há avaliações
- Acute Myocardial Infarction: Recognition and AssessmentDocumento7 páginasAcute Myocardial Infarction: Recognition and AssessmentHasnainKhimjiAinda não há avaliações
- Atrial Fibrillation: Anish DhakalDocumento33 páginasAtrial Fibrillation: Anish DhakalDrjawadhussain HussainAinda não há avaliações
- Anticoagulants: Julene FunkDocumento25 páginasAnticoagulants: Julene FunkJulieAinda não há avaliações
- Dokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedDocumento54 páginasDokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedMahmoud FathyAinda não há avaliações
- Anticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveDocumento3 páginasAnticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveShoyeb KhanAinda não há avaliações
- Cardiovascular Center Pocket Guide Use of Warfarin in Thrombotic Cardiovascular DiseaseDocumento2 páginasCardiovascular Center Pocket Guide Use of Warfarin in Thrombotic Cardiovascular Diseasemicheal1960Ainda não há avaliações
- Chapter 3: Perioperative ManagementDocumento14 páginasChapter 3: Perioperative ManagementpoddataAinda não há avaliações
- Vit KguidelinesDocumento2 páginasVit KguidelinesMayer Rosenberg100% (1)
- AnticogulationDocumento58 páginasAnticogulationRudhra Dharshan ThiyagarajanAinda não há avaliações
- Aha/Asa 2018 Guidelines For The Early Management of Patients With Acute Ischemic StrokeDocumento4 páginasAha/Asa 2018 Guidelines For The Early Management of Patients With Acute Ischemic StrokeFrancisco PuenteAinda não há avaliações
- ACLS DrugsDocumento16 páginasACLS Drugstostc100% (1)
- Anticoag GuidelinesDocumento22 páginasAnticoag Guidelinesyusuf100% (1)
- QRG AntithromboticDocumento6 páginasQRG AntithromboticthapanAinda não há avaliações
- Procoagulantes Guias PDFDocumento30 páginasProcoagulantes Guias PDFtsntbAinda não há avaliações
- Guidelines For The Management of Atrial Fibrillation Part-IIIDocumento82 páginasGuidelines For The Management of Atrial Fibrillation Part-IIIJamil Muqtadir BhattiAinda não há avaliações
- Stroke Secondary Prevention Guideline September 2021Documento5 páginasStroke Secondary Prevention Guideline September 2021aniqahmed6565Ainda não há avaliações
- Pharmacology CardiovascularDocumento86 páginasPharmacology Cardiovascularamasoud96 amasoud96Ainda não há avaliações
- Clozapine Monitoring GuidelinesDocumento3 páginasClozapine Monitoring GuidelinesAntoine JusticeAinda não há avaliações
- Name of The Medicinal Product: Prescribing Information Coumadin TabletsDocumento13 páginasName of The Medicinal Product: Prescribing Information Coumadin Tabletsddandan_2Ainda não há avaliações
- NOAC ChartDocumento2 páginasNOAC Chartsgod34Ainda não há avaliações
- Anticoagulatio N Asra Guidelines: Sravya VemuriDocumento62 páginasAnticoagulatio N Asra Guidelines: Sravya VemuriSiva Prasad AspAinda não há avaliações
- Management of ArrhythmiasDocumento4 páginasManagement of ArrhythmiasAray Al-AfiqahAinda não há avaliações
- 6 - Fahad Class 6 Cardiac AnesthesiaDocumento18 páginas6 - Fahad Class 6 Cardiac AnesthesiaOne ClickAinda não há avaliações
- Guidelines For The Management of Atrial Fibrillation Part-IIDocumento66 páginasGuidelines For The Management of Atrial Fibrillation Part-IIJamil Muqtadir BhattiAinda não há avaliações
- Protocol of Management of Acute Heart FailureDocumento5 páginasProtocol of Management of Acute Heart FailureMc inloveAinda não há avaliações
- Medicine ManagementsDocumento87 páginasMedicine ManagementsMohamed LibanAinda não há avaliações
- MANAGEMENT of ACUTE HF IN EDDocumento4 páginasMANAGEMENT of ACUTE HF IN EDagar agarAinda não há avaliações
- Cardiology Pharmacist Guide to Acute Coronary SyndromeDocumento38 páginasCardiology Pharmacist Guide to Acute Coronary SyndromeAnonymous100% (1)
- Antihypertensive Agents that Reduce Uric Acid and Migraines or Cause GynecomastiaDocumento53 páginasAntihypertensive Agents that Reduce Uric Acid and Migraines or Cause GynecomastiaDian ParamitaAinda não há avaliações
- VernakalantDocumento15 páginasVernakalantAkif AhamadAinda não há avaliações
- UFH LMWH Fonda - 06september2020Documento7 páginasUFH LMWH Fonda - 06september2020gabrimarteAinda não há avaliações
- Atrial Fibrillation Pharmacologic OptionsDocumento2 páginasAtrial Fibrillation Pharmacologic OptionshebaAinda não há avaliações
- ACLS Simulation ScenariosDocumento14 páginasACLS Simulation ScenariosVanessa HermioneAinda não há avaliações
- LMWH QML 06Documento7 páginasLMWH QML 06pd7qmlAinda não há avaliações
- Main Stroke Protocol - Use For All Suspected Stroke-TIA PatientsDocumento2 páginasMain Stroke Protocol - Use For All Suspected Stroke-TIA PatientsRivulet1Ainda não há avaliações
- New Oral Anticoagulants Guidelines: Kai YapDocumento23 páginasNew Oral Anticoagulants Guidelines: Kai YapMuhammad Reza FirdausAinda não há avaliações
- Xarelto 2.5mg tablets for ACS preventionDocumento182 páginasXarelto 2.5mg tablets for ACS preventionadrip234Ainda não há avaliações
- Current Clinical Strategies: Handbook of AnesthesiologyDocumento180 páginasCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaAinda não há avaliações
- Management of Symptomatic Bradycardia and TachycardiaDocumento55 páginasManagement of Symptomatic Bradycardia and TachycardiaDewintha Airene NoviantiAinda não há avaliações
- ECMO Management Lecture 5Documento39 páginasECMO Management Lecture 5dnafredyAinda não há avaliações
- PDF Pulmonary Oedema ProtocolDocumento1 páginaPDF Pulmonary Oedema ProtocolHanan FathyAinda não há avaliações
- Guidelines For The Management of Atrial Fibrillation Part-IVDocumento56 páginasGuidelines For The Management of Atrial Fibrillation Part-IVJamil Muqtadir BhattiAinda não há avaliações
- Managing Heart Failure with Drug TherapyDocumento8 páginasManaging Heart Failure with Drug TherapyAbdallahMousaAinda não há avaliações
- Pathway StemiDocumento2 páginasPathway StemiIntan Nurulita SariAinda não há avaliações
- Asthma PathwayDocumento42 páginasAsthma PathwayVhony Purnamasari HAinda não há avaliações
- An Update Management of Acute Ischemic Stroke: SurotoDocumento36 páginasAn Update Management of Acute Ischemic Stroke: SurotoShinta DianAinda não há avaliações
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingAinda não há avaliações
- Clinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2No EverandClinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Ainda não há avaliações
- NAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)No EverandNAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)Nota: 4.5 de 5 estrelas4.5/5 (3)
- Hari2 4 Cita210413Documento45 páginasHari2 4 Cita210413Indra WijayaAinda não há avaliações
- Medication Safety ReconciliationDocumento117 páginasMedication Safety ReconciliationIndra WijayaAinda não há avaliações
- Medication Reconciliation: Opportunity To Improve Patient SafetyDocumento11 páginasMedication Reconciliation: Opportunity To Improve Patient SafetyEvelinne MayAinda não há avaliações
- 4 High Alert Medication FinalDocumento4 páginas4 High Alert Medication Finalrini setyawatiAinda não há avaliações
- Complication of Enteral Nutrition PDFDocumento3 páginasComplication of Enteral Nutrition PDFIndra WijayaAinda não há avaliações
- Drug RekonsiliationDocumento4 páginasDrug RekonsiliationIndra WijayaAinda não há avaliações
- Langkah Ke 7-Cegah Cedera Melalui Implementasi Keselamatan PasienDocumento79 páginasLangkah Ke 7-Cegah Cedera Melalui Implementasi Keselamatan PasienSepti MayandariAinda não há avaliações
- 1000 519 High Alert High Risk Hazardous Look Alike Sound Alike Medications FRLORIDA HOSPITALDocumento7 páginas1000 519 High Alert High Risk Hazardous Look Alike Sound Alike Medications FRLORIDA HOSPITALrini setyawatiAinda não há avaliações
- High Alert Medications OB Inpatient UnitsDocumento37 páginasHigh Alert Medications OB Inpatient UnitsHari Mas Kuncoro100% (1)
- High Alert MedicationsDocumento1 páginaHigh Alert MedicationsOctaviana SimbolonAinda não há avaliações
- Automatic Stop Order Univ Kentucky hospitalPH04-04 PDFDocumento1 páginaAutomatic Stop Order Univ Kentucky hospitalPH04-04 PDFNahjarAinda não há avaliações
- Clinical Safety Automatic Stop OrdersDocumento3 páginasClinical Safety Automatic Stop OrdersindraAinda não há avaliações
- Protocols Pocket Card StJosephDocumento2 páginasProtocols Pocket Card StJosephAnonymous dPns6kdGuAinda não há avaliações
- Pemateri Paralel SimposiumDocumento8 páginasPemateri Paralel SimposiumIndra WijayaAinda não há avaliações
- Complikasi NutrisiDocumento3 páginasComplikasi NutrisiIndra WijayaAinda não há avaliações
- Shock: GeneralDocumento2 páginasShock: GeneralIndra WijayaAinda não há avaliações
- 1230 2569 1 SM PDFDocumento7 páginas1230 2569 1 SM PDFArifMugiSetiawanAinda não há avaliações
- Rundown BLSDocumento1 páginaRundown BLSIndra WijayaAinda não há avaliações
- Range Extender SettingsDocumento1 páginaRange Extender SettingsIndra WijayaAinda não há avaliações
- Prevention and Management of Procedural Pain in The Neonate An U 2016Documento13 páginasPrevention and Management of Procedural Pain in The Neonate An U 2016Indra WijayaAinda não há avaliações
- Pubmed ResultDocumento1 páginaPubmed ResultIndra WijayaAinda não há avaliações
- Preeclampsia management obstetric anaesthesiaDocumento21 páginasPreeclampsia management obstetric anaesthesiaIndra WijayaAinda não há avaliações
- Automatic Stop Order Univ Kentucky hospitalPH04-04 PDFDocumento1 páginaAutomatic Stop Order Univ Kentucky hospitalPH04-04 PDFNahjarAinda não há avaliações
- ME10!03!003 MMC Pathway2Documento2 páginasME10!03!003 MMC Pathway2Indra WijayaAinda não há avaliações
- JfpromDocumento23 páginasJfpromik4_bpS3077Ainda não há avaliações
- Sda PDFDocumento1 páginaSda PDFIndra WijayaAinda não há avaliações
- Sda PDFDocumento1 páginaSda PDFIndra WijayaAinda não há avaliações
- ACLS Study Guide for IU Health ClassDocumento18 páginasACLS Study Guide for IU Health ClassZarah Jane Rull NateAinda não há avaliações
- Acute Heart Failure SyndromeDocumento1 páginaAcute Heart Failure SyndromeIndra WijayaAinda não há avaliações
- Construction Safety Plan GuideDocumento13 páginasConstruction Safety Plan Guideemmanueloboh92% (24)
- SSC DWDocumento4 páginasSSC DWsanketpavi21Ainda não há avaliações
- Sri Lanka's Economic Crisis Explained: Depleting Reserves, Food InflationDocumento11 páginasSri Lanka's Economic Crisis Explained: Depleting Reserves, Food InflationRohan PachunkarAinda não há avaliações
- Demeclocycline Effective for Treating SIADHDocumento4 páginasDemeclocycline Effective for Treating SIADHSally TareqAinda não há avaliações
- Learning Strand I - EnglishDocumento19 páginasLearning Strand I - EnglishMaricel MaapoyAinda não há avaliações
- Rotex Brochure PDFDocumento4 páginasRotex Brochure PDFestramilsolutionAinda não há avaliações
- All India Test Series (2023-24)Documento22 páginasAll India Test Series (2023-24)Anil KumarAinda não há avaliações
- Engineer Course - Plumbing I PDFDocumento359 páginasEngineer Course - Plumbing I PDFfanatickakashiAinda não há avaliações
- Expectations:: Good Manners and Right Conduct (GMRC)Documento3 páginasExpectations:: Good Manners and Right Conduct (GMRC)Jae Mae Moral BubanAinda não há avaliações
- 7 HO Clearance Consent FormDocumento2 páginas7 HO Clearance Consent FormzanehfncbusinessAinda não há avaliações
- Bio Brain Review Q S PDFDocumento22 páginasBio Brain Review Q S PDFtehilashiftehAinda não há avaliações
- Role of Victims in Commission of CrimeDocumento16 páginasRole of Victims in Commission of CrimeBEST OF ONE PIECEAinda não há avaliações
- Event Service AgreementDocumento5 páginasEvent Service AgreementPNC ChoraleAinda não há avaliações
- Republic of The Philippines: Cavite State University Don Severino de Las Alas CampusDocumento5 páginasRepublic of The Philippines: Cavite State University Don Severino de Las Alas CampusRobin EscosesAinda não há avaliações
- Varicella Zoster VirusDocumento11 páginasVaricella Zoster VirusJayaram SAinda não há avaliações
- Holistic NursingDocumento7 páginasHolistic NursingSharmila Laxman DakeAinda não há avaliações
- Bams 1st Rachna Sharir Joints and Their Classification 16-05-2020Documento15 páginasBams 1st Rachna Sharir Joints and Their Classification 16-05-2020Sanjana SajjanarAinda não há avaliações
- Astm C 125-03 PDFDocumento4 páginasAstm C 125-03 PDFArnold EspinozaAinda não há avaliações
- CWU Psychiatry 1.1Documento8 páginasCWU Psychiatry 1.1Codillia CheongAinda não há avaliações
- Flood Risk Mitigation Adis Ababa UNI PDFDocumento100 páginasFlood Risk Mitigation Adis Ababa UNI PDFshucayb cabdiAinda não há avaliações
- Littelfuse TVS Diode 5 0SMDJ Datasheet PDFDocumento6 páginasLittelfuse TVS Diode 5 0SMDJ Datasheet PDFAnonymous BTGRlmuWsAinda não há avaliações
- A Safety Alert Maintenance 1 IADCDocumento10 páginasA Safety Alert Maintenance 1 IADCVeeramuthu SundararajuAinda não há avaliações
- Mass XL Workout Plan by Guru Mann PDFDocumento4 páginasMass XL Workout Plan by Guru Mann PDFSaptarshi BiswasAinda não há avaliações
- Presented By: Bhagyashree KaleDocumento58 páginasPresented By: Bhagyashree KaleSupriya JajnurkarAinda não há avaliações
- UntitledDocumento10 páginasUntitledGuia Charish SalvadorAinda não há avaliações
- Event Details Report - Algoma SteelDocumento66 páginasEvent Details Report - Algoma SteelThe NarwhalAinda não há avaliações
- Play and Communication TheoryDocumento21 páginasPlay and Communication Theoryroberto100% (2)
- Hawaii Hotel Performance by WeekDocumento1 páginaHawaii Hotel Performance by WeekHonolulu Star-AdvertiserAinda não há avaliações
- Shipping Instructions For US ImportsDocumento7 páginasShipping Instructions For US ImportsRichard LimAinda não há avaliações
- Abolish SlaveryDocumento1 páginaAbolish SlaverySiyeon (Sean) LeeAinda não há avaliações