Escolar Documentos
Profissional Documentos
Cultura Documentos
Bronkiektasis
Enviado por
Halida Batik AlunaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Bronkiektasis
Enviado por
Halida Batik AlunaDireitos autorais:
Formatos disponíveis
Residents Section Pat tern of the Month
Cantin et al.
Bronchiectasis
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Residents Section
Pattern of the Month
Residents
inRadiology
Luce Cantin1
Alexander A. Bankier
Ronald L. Eisenberg
Cantin L, Bankier AA, Eisenberg RL
Bronchiectasis
Bronchiectasis is a relatively frequent condition in the United States, with an estimated
prevalence of 4.2 per 100,000 persons 1834 years old and 272 per 100,000 persons 75 years
or older. It is defined as an irreversible localized or diffuse dilatation, usually resulting from
chronic infection, proximal airway obstruction, or congenital bronchial abnormality. On
chest radiographs, bronchiectasis manifests as tram tracks, parallel line opacities, ring opacities, and tubular structures. However, chest radiographs lack sensitivity for detecting mild or
even moderate disease. CT is substantially more sensitive than chest radiography for showing
bronchiectasis, which is characterized by lack of bronchial tapering, bronchi visible in the
peripheral 1 cm of the lungs, and an increased bronchoarterial ratio producing the so-called
signet-ring sign. According to appearance and severity, bronchiectasis can be classified as
cylindric, varicose, or cystic (Fig. 1). The wide differential diagnosis of bronchiectasis can be
substantially narrowed by considering both the anatomic location and the distribution of this
pathology (Fig 2).
Keywords: airway obstruction, bronchiectasis
DOI:10.2214/AJR.09.3053
Received May 15, 2009; accepted after revision
May 26, 2009.
1
All authors: Department of Radiology, Beth Israel
Deaconess Medical Center, Harvard Medical School, 330
Brookline Ave., Boston, MA 02215. Address correspondence to R. L. Eisenberg (rleisenb@bidmc.harvard.edu).
WEB
This is a Web exclusive article.
AJR 2009; 193:W158W171
Fig. 1Categories of bronchiectasis.
AD, Normal bronchus (arrow) (A), cylindric bronchiectasis with lack of bronchial tapering (arrow) (B), varicose
bronchiectasis with string-of-pearls appearance (arrow) (C), and cystic bronchiectasis (arrow) (D).
(Fig. 1 continues on next page)
0361803X/09/1933W158
American Roentgen Ray Society
W158
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
Fig. 1 (continued)Categories of bronchiectasis.
AD, Normal bronchus (arrow) (A), cylindric bronchiectasis with lack of bronchial tapering (arrow) (B), varicose
bronchiectasis with string-of-pearls appearance (arrow) (C), and cystic bronchiectasis (arrow) (D).
Detection of bronchiectasis
Focal bronchiectasis
Congenital bronchial atresia
Extrinsic compression
Endobronchial malignancy
Foreign body
Broncholithiasis
Airway stenosis
Upper lung
predominance
Cystic fibrosis
Sarcoidosis
Postradiation fibrosis
Diffuse bronchiectasis
Peripheral
predominance
Lower lung
predominance
Idiopathic
Postinfectious
Repeated aspiration
Fibrotic lung disease
Posttransplant rejection
Hypogammaglobulinemia
Central
predominance
Right middle lobe and
lingula predominance
Allergic bronchopulmonary aspergillosis
Mounier-Kuhns syndrome
Williams-Campbell syndrome
Atypical mycobacterial infection (MAI)
Immotile cilia syndrome
Fig. 2Flowchart shows algorithm for evaluation of bronchiectasis. MAI = Mycobacterium avium-intracellulare.
Focal Bronchiectasis
Any cause of airway obstruction can lead to focal bronchiectasis (Fig. 3). In contrast to
diffuse bronchiectasis, focal bronchiectasis requires diagnostic bronchoscopy in almost all
patients.
Bronchial Atresia
The most common cause of congenital focal bronchiectasis is bronchial atresia, characterized by obliteration of a bronchus with distal bronchiectasis, mucoid impaction, and air trapping that is most commonly seen in the left upper lobe (Fig. 4). In this rare lesion, the bronchial tree peripheral to the point of obliteration is patent and the lung parenchyma is overinflated because of collateral air drift.
AJR:193, September 2009
W159
Cantin et al.
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Fig. 3Focal
bronchiectasis
(idiopathic) in left lower
lobe (arrow).
Fig. 4Bronchial atresia.
A, Transverse image of focal bronchiectasis (arrow) distal to bronchial atresia associated with hyperlucency
and hyperexpansion of left lung.
B, Coronal image shows proximal mucoid impaction (arrow), distal bronchiectasis (arrowhead), and widespread
air trapping of left lung.
Extrinsic Compression
Extrinsic compression is an acquired cause of focal bronchiectasis, most commonly caused
by lymphadenopathy, usually from previous granulomatous exposure. Less frequent causes
include sarcoidosis, hilar mass, and metastatic lymphadenopathy.
Endoluminal Obstruction by Tumor
Most carcinoid tumors are primarily endobronchial lesions, occurring in the central, main,
or segmental bronchi (Fig. 5). Some small tumors are located entirely within the lumen. How-
W160
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
Fig. 5Carcinoid. This predominantly endobronchial tumor, arising before bifurcation of left upper and lower
lobe bronchi, causes distal bronchiectasis.
A and B, Transverse images of tumor (arrow, A) and distal bronchiectasis (arrows, B).
C and D, Coronal oblique image (C) and volume-rendering reformation (D) in similar orientation as A and B show
central carcinoid tumor (arrows) and distal bronchiectasis (arrowheads, C).
ever, some display a dominant extraluminal component with only a small part of the tumor
lying within the airway (iceberg lesion). A variety of other benign and malignant neoplasms
can also result in obstruction leading to focal bronchiectasis.
Foreign Body
Aspirated foreign material can result in focal bronchiectasis. Persistence of a noncalcified
foreign body, such as a vegetable fiber, within a bronchus for a prolonged period of time can
serve as a nidus for calcium deposition.
Broncholithiasis
Calcified or ossified material within the bronchial lumen can cause focal bronchiectasis.
By far the most common cause of broncholithiasis is erosion by and extrusion of a calcified
AJR:193, September 2009
W161
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Cantin et al.
Fig. 6Broncholithiasis.
AC, Calcified left upper lobe endobronchial
broncholithiasis (arrow) from previous tuberculosis
exposure is seen on transverse image (A), minimumintensity-projection reformation in coronal oblique
plane (B), and volume-rendering reformation (C)
in similar orientation. In C, arrow points to distal
bronchiectasis.
C
adjacent lymph node, usually associated with a long-standing focus of necrotizing granulomatous lymphadenitis, especially after tuberculosis (Fig. 6). Nevertheless, the frequency of
broncholithiasis complicating granulomatous infection is quite low. The most common sites
are the proximal right middle lobe bronchus and the origin of the anterior segmental bronchus
of the upper lobes because of airway anatomy and lymph node distribution.
Airway Stenosis
Airway stenosis causing focal bronchiectasis (Fig. 7) can result from a broad spectrum of
entities including infection, intubation stricture, healing of a tracheostomy stoma, tracheobronchopathia osteochondroplastica, amyloidosis, relapsing polychondritis, sarcoidosis, and
fibrosing mediastinitis.
Diffuse Bronchiectasis: Upper Predominance
Cystic Fibrosis
The most common cause of congenital upper-lung-predominant bronchiectasis is cystic
fibrosis, commonly associated with enlarged lung volumes and interstitial alterations (Fig. 8).
An autosomal recessive genetic disorder causing ineffective clearance of secretions, cystic
fibrosis presents with recurrent pneumonias, sinusitis, pancreatic insufficiency, and infertility.
Milder forms of cystic fibrosis, however, can remain unrecognized until adulthood (Fig. 9).
W162
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
C
Fig. 7Congenital stenosis of left mainstem bronchus.
A and B, Transverse images show stenosis (arrow, A), distal bronchiectasis, and mucoid impaction (arrows, B).
C, Coronal reformation image shows bronchial stenosis (arrow).
Sarcoidosis
Parenchymal involvement by sarcoidosis can lead to upper and mid lung fibrosis and traction bronchiectasis, typically associated with multiple nodules in a perilymphatic distribution
(Fig. 10). Mediastinal and bilateral symmetric lymphadenopathy is common, although it can
regress as the interstitial disease worsens.
Postradiation Fibrosis
Another important cause of upper-lung-predominant bronchiectasis is postradiation fibrosis, in which traction bronchiectasis is usually limited to the radiation port (Fig. 11). A straight
interface between the irradiated field and normal lung is often seen. This does not respect
anatomic borders, such as fissures and lobes. Postradiation fibrosis may also be bilateral after
mediastinal radiation for lymphoma.
AJR:193, September 2009
W163
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Cantin et al.
A
Fig. 8Cystic fibrosis.
A and B, Transverse (A) and coronal (B) images show
upper lobe predominance of cystic bronchiectasis
(arrows) and volume loss, enlarged lung volumes, and
diffuse heterogeneous attenuation.
Fig. 9Adult cystic fibrosis. In this milder case, there is upper lobe predominance of cylindric bronchiectasis
(white arrows) and bronchiolitis (black arrows).
W164
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
B
Fig. 10Sarcoidosis.
A and B, Transverse images show fibrosis and traction bronchiectasis (arrows, B) that predominantly involve
upper lobes.
Diffuse Bronchiectasis: Lower Predominance
Lower-lung-predominant bronchiectasis, which is the most frequent pattern, is most commonly idiopathic (Fig. 12). However, some cases have known causes.
Recurrent Childhood Infections
Postinfectious bronchiectasis is a frequent cause of lower-lung-predominant bronchiectasis. It is less seen today because of better control of tuberculosis, earlier treatment of pneumonia, and immunization. However, recurrent infections still remain a frequent cause of bronchiectasis in immune-suppressed patients.
Aspiration
Any predisposition for repeated aspiration is associated with an increased risk of developing bibasilar bronchiectasis. Common causes include a large hiatal hernia with gastroesophageal reflux, scleroderma (Fig. 13) and other causes of a patulous esophagus, and esophageal
motility disorders.
AJR:193, September 2009
W165
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Cantin et al.
Fig. 11Postradiation fibrosis.
A and B, Right paramediastinal fibrotic changes, which developed after treatment of lung cancer, are
associated with traction bronchiectasis (arrows).
Fig. 12Lower lobe predominance of bronchiectasis.
A, Subtle idiopathic bibasilar cylindric bronchiectasis
shows signet-ring sign (arrows).
B, In another patient, there is marked idiopathic left
lower bronchiectasis with volume loss, bronchial wall
thickening, and diffuse opacity.
Fibrotic Lung Disease
Bronchiectasis predominantly involving lung bases is a common finding in fibrotic lung
disease. In usual interstitial pneumonia (UIP), coarse reticulation, honeycombing, parenchymal distortion, and traction bronchiectasis are typically predominant in a subpleural and
W166
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
Fig. 13Scleroderma. There is patulous esophagus (white arrow), recurrent aspiration with subsequent
bibasilar bronchiectasis, and chronic ground-glass opacities. Black arrow points to bronchus visible in
peripheral 1 cm of lung.
Fig. 14Usual interstitial pneumonia. Bibasilar and subpleural reticulation and traction bronchiectasis are
seen in areas of fibrosis (arrows).
bibasilar distribution with geographic heterogeneity (Fig. 14). Although often idiopathic, UIP
occurs in asbestosis, drug toxicity, and collagenvascular disease. Nonspecific interstitial
pneumonia has almost the same differential diagnosis but typically occurs in younger patients
and carries a better prognosis. Ground-glass opacity is more frequent than in UIP and honeycombing usually remains minimal.
Rare Causes
Bronchiolitis obliterans from posttransplantation rejection is a rare cause of bronchiectasis
associated with patchy mosaic perfusion, air trapping, and bronchiolar obstruction (Fig. 15).
Hypogammaglobulinemia can also be a cause of lower-lung-predominant bronchiectasis,
most often caused by recurrent infections.
AJR:193, September 2009
W167
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Cantin et al.
Fig. 15Bronchiolitis obliterans after lung transplantation.
A and B, Transverse images of right lung in deep inspiration (A) and end expiration (B) show subtle basilar
cylindric bronchiectasis (arrows, A) and widespread air trapping (arrows, B).
Fig. 16Mycobacterium avium-intracellulare infection. Bronchiectasis (arrows) predominantly involves right
middle lobe and lingula.
Diffuse Bronchiectasis: Middle Lobe and Lingula Predominance
Nontuberculous Mycobacterial Infection
The most common acquired cause of bronchiectasis predominantly involving the right
middle lobe and lingula is nontuberculous mycobacterial infection, such as Mycobacterium
avium-intracellulare (MAI). This infection, typically seen in women over 60 years old, presents with chronic infection, bronchiectasis, mucoid impaction, and bronchiolitis (Fig. 16).
The disease often has an indolent but progressive course requiring long-term antibiotics.
Immobile Cilia Syndrome
This rare congenital cause of bronchiectasis, which primarily involves the middle lung, is
characterized by ineffective clearing of secretions, causing bronchiectasis, recurrent pneumonias, sinusitis, and infertility. In 50% of cases, total situs inversus is present, a condition
known as Kartageners syndrome (Fig. 17).
W168
AJR:193, September 2009
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Bronchiectasis
Fig. 17Kartageners syndrome.
A, Chest radiograph shows cardiomegaly, dextrocardia, left middle lobe bronchiectasis, and volume loss.
Arrow points to wrong-sided left marker.
B, Transverse CT image confirms dextrocardia (asterisk is in left ventricle) and bronchiectasis (arrows) that
predominantly affects midportion of lungs.
Fig. 18Allergic bronchopulmonary aspergillosis.
A, Chest radiograph shows central bronchiectasis
and mucoid impaction, so-called finger-in-glove
appearance (arrows).
B, Transverse CT image shows central
bronchiectasis, mucoid impaction (large arrow), and
distal bronchiolitis (small arrow).
B
AJR:193, September 2009
W169
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Cantin et al.
B
Fig. 19Mounier-Kuhns syndrome.
A, Enlarged trachea (arrow).
B, Enlarged mainstem bronchi (black arrows) and distal bronchiectasis (white arrows).
Fig. 20Williams-Campbell syndrome. There is mostly varicose and cystic central bronchiectasis (arrows).
W170
AJR:193, September 2009
Bronchiectasis
Downloaded from www.ajronline.org by 36.81.19.190 on 11/22/14 from IP address 36.81.19.190. Copyright ARRS. For personal use only; all rights reserved
Diffuse Bronchiectasis: Central Predominance
Allergic Bronchopulmonary Aspergillosis
Allergic bronchopulmonary aspergillosis is an immune reaction to Aspergillus species that
damages the bronchial wall, causing central bronchiectasis and mucous plugs that contain
fungus and inflammatory cells. On chest radiography, this produces a characteristic finger-inglove appearance. On CT, central bronchiectasis and mucoid impactions are often associated
with areas of peripheral bronchiolitis, manifesting as bronchiolar nodules or tree-in-bud
opacities (Fig. 18).
Cartilage-Deficiency Disorders
Several rare disorders characterized by cartilage deficiency can cause bronchiectasis that
primarily involves the central regions of the lung. One is tracheobronchomegaly, also known as
Mounier-Kuhns syndrome, which manifests as diffuse enlargement of the trachea and mainstem bronchi with more distal bronchiectasis (Fig. 19).
An even rarer cartilage deficiency disorder is the Williams-Campbell syndrome, in which
central bronchiectasis, mimicking the appearance of parenchymal cysts, is associated with
widespread air trapping (Fig. 20).
Suggested Reading
1. Barker AF. Bronchiectasis. New Engl J Med 2002; 346:13831393
2. Baydarian M, Walter RN. Bronchiectasis: introduction, etiology, and clinical features. Dis Mon 2008;
54:516526
3. Hansell DM, Bankier AA, MacMahon TC, McLoud TC, Mller NL, Remy J. Fleischner Society: glossary
of terms for thoracic imaging. Radiology 2008; 246:697722
4. Javidan-Nejad C, Bhalla S. Bronchiectasis. Radiol Clin North Am 2009; 47:289306
5. Kim JS, Mller NL, Park CS, Grenier P, Herold CJ. Cylindrical bronchiectasis: diagnostic findings on thinsection CT. AJR 1997; 168:751754
6. ODonnell AE. Bronchiectasis. Chest 2008; 134:815823
7. Quast TM, Self AR, Browning radiofrequency: diagnostic evaluation of bronchiectasis. Dis Mon 2008;
54:527539
8. Reid LM. Reduction in bronchial subdivision in bronchiectasis. Thorax 1950; 5:233247
AJR:193, September 2009
W171
Você também pode gostar
- Art:10.1007/s00247 005 1559 7 PDFDocumento12 páginasArt:10.1007/s00247 005 1559 7 PDFHalida Batik AlunaAinda não há avaliações
- Critical ThinkingDocumento2 páginasCritical ThinkingMwagaVumbiAinda não há avaliações
- Bronkiektasis PDFDocumento14 páginasBronkiektasis PDFHalida Batik AlunaAinda não há avaliações
- Neuro BlastomaDocumento7 páginasNeuro BlastomaHalida Batik AlunaAinda não há avaliações
- A Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportDocumento3 páginasA Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportHalida Batik AlunaAinda não há avaliações
- A Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportDocumento3 páginasA Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportHalida Batik AlunaAinda não há avaliações
- Review Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageDocumento12 páginasReview Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageHalida Batik AlunaAinda não há avaliações
- Journal Cystic Abdominal Masses PDFDocumento16 páginasJournal Cystic Abdominal Masses PDFHalida Batik AlunaAinda não há avaliações
- Review Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageDocumento12 páginasReview Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageFika Tri NandaAinda não há avaliações
- Jurnal PneumoniaDocumento12 páginasJurnal PneumoniaHalida Batik AlunaAinda não há avaliações
- Journal Cystic Abdominal MassesDocumento16 páginasJournal Cystic Abdominal MassesHalida Batik AlunaAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Strategies For StartupDocumento16 páginasStrategies For StartupRoshankumar BalasubramanianAinda não há avaliações
- Shopping Mall: Computer Application - IiiDocumento15 páginasShopping Mall: Computer Application - IiiShadowdare VirkAinda não há avaliações
- Paper 4 (A) (I) IGCSE Biology (Time - 30 Mins)Documento12 páginasPaper 4 (A) (I) IGCSE Biology (Time - 30 Mins)Hisham AlEnaiziAinda não há avaliações
- Oxgen Sensor Cat WEBDocumento184 páginasOxgen Sensor Cat WEBBuddy Davis100% (2)
- WWW - Commonsensemedia - OrgDocumento3 páginasWWW - Commonsensemedia - Orgkbeik001Ainda não há avaliações
- Copula and Multivariate Dependencies: Eric MarsdenDocumento48 páginasCopula and Multivariate Dependencies: Eric MarsdenJeampierr Jiménez CheroAinda não há avaliações
- Cableado de TermocuplasDocumento3 páginasCableado de TermocuplasRUBEN DARIO BUCHELLYAinda não há avaliações
- Fast Aldol-Tishchenko ReactionDocumento5 páginasFast Aldol-Tishchenko ReactionRSLAinda não há avaliações
- The Smith Generator BlueprintsDocumento36 páginasThe Smith Generator BlueprintsZoran AleksicAinda não há avaliações
- United-nations-Organization-uno Solved MCQs (Set-4)Documento8 páginasUnited-nations-Organization-uno Solved MCQs (Set-4)SãñÂt SûRÿá MishraAinda não há avaliações
- Essential Rendering BookDocumento314 páginasEssential Rendering BookHelton OliveiraAinda não há avaliações
- 202112fuji ViDocumento2 páginas202112fuji ViAnh CaoAinda não há avaliações
- Joining Instruction 4 Years 22 23Documento11 páginasJoining Instruction 4 Years 22 23Salmini ShamteAinda não há avaliações
- Arta Kelmendi's resume highlighting education and work experienceDocumento2 páginasArta Kelmendi's resume highlighting education and work experienceArta KelmendiAinda não há avaliações
- Analyze and Design Sewer and Stormwater Systems with SewerGEMSDocumento18 páginasAnalyze and Design Sewer and Stormwater Systems with SewerGEMSBoni ClydeAinda não há avaliações
- Process Financial Transactions and Extract Interim Reports - 025735Documento37 páginasProcess Financial Transactions and Extract Interim Reports - 025735l2557206Ainda não há avaliações
- Why Choose Medicine As A CareerDocumento25 páginasWhy Choose Medicine As A CareerVinod KumarAinda não há avaliações
- Allan S. Cu v. Small Business Guarantee and FinanceDocumento2 páginasAllan S. Cu v. Small Business Guarantee and FinanceFrancis Coronel Jr.Ainda não há avaliações
- Form 709 United States Gift Tax ReturnDocumento5 páginasForm 709 United States Gift Tax ReturnBogdan PraščevićAinda não há avaliações
- Tutorial 1 Discussion Document - Batch 03Documento4 páginasTutorial 1 Discussion Document - Batch 03Anindya CostaAinda não há avaliações
- SEC QPP Coop TrainingDocumento62 páginasSEC QPP Coop TrainingAbdalelah BagajateAinda não há avaliações
- (123doc) - Chapter-24Documento6 páginas(123doc) - Chapter-24Pháp NguyễnAinda não há avaliações
- Typical T Intersection On Rural Local Road With Left Turn LanesDocumento1 páginaTypical T Intersection On Rural Local Road With Left Turn Lanesahmed.almakawyAinda não há avaliações
- Reading Comprehension Exercise, May 3rdDocumento3 páginasReading Comprehension Exercise, May 3rdPalupi Salwa BerliantiAinda não há avaliações
- Srimanta Sankaradeva Universityof Health SciencesDocumento3 páginasSrimanta Sankaradeva Universityof Health SciencesTemple RunAinda não há avaliações
- Link Ratio MethodDocumento18 páginasLink Ratio MethodLuis ChioAinda não há avaliações
- Dance Appreciation and CompositionDocumento1 páginaDance Appreciation and CompositionFretz Ael100% (1)
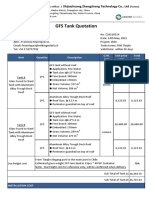
- GFS Tank Quotation C20210514Documento4 páginasGFS Tank Quotation C20210514Francisco ManriquezAinda não há avaliações
- Key Fact Sheet (HBL FreedomAccount) - July 2019 PDFDocumento1 páginaKey Fact Sheet (HBL FreedomAccount) - July 2019 PDFBaD cHaUhDrYAinda não há avaliações
- Build A Program Remote Control IR Transmitter Using HT6221Documento2 páginasBuild A Program Remote Control IR Transmitter Using HT6221rudraAinda não há avaliações