Escolar Documentos
Profissional Documentos
Cultura Documentos
Thyroid Rebuttal
Enviado por
Sachin MakhijaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Thyroid Rebuttal
Enviado por
Sachin MakhijaDireitos autorais:
Formatos disponíveis
Thyroid Science 4(3):C1-12, 2009
www.ThyroidScience.com
Criticism
Stability, Effectiveness, and Safety of
Desiccated Thyroid vs Levothyroxine:
A Rebuttal to the British Thyroid Association
Dr. John C. Lowe*
*Director of Research, Fibromyalgia Research Foundation
Contact: Dr. John C. Lowe drlowe@drlowe.com
R eceived: February 16, 2009
Accepted: February 23, 2009
Abstract. In 2007, an Executive Committee (the Committee) of the British Thyroid Association (BTA)
published a document in which it concluded that levothyroxine is safer, more stable, and more effective than
Armour Thyroid. By extension, the conclusion also applies to other desiccated thyroid products, such as Erfa
Thyroid. Enough evidence is available, however, to conclude that T4 /T3 therapies with either synthetic hormones or desiccated thyroid are safer and more effective than T4 replacement, and that desiccated thyroid is
more stable than levothyroxine products. The Committee mentioned clinical trials that directly bear on its conclusions, but it did not include any of these in the reference section of its document. Instead, it referenced a review of the clinical trials by Escobar-Morreale et al. and a meta-analysis of the trials by Grozinsky-Glasberg
et al. These two publications, however, deal with synthetic T4 /T3 therapies, not desiccated thyroid. Both publications contain factual errors and unbalanced presentations of data, excluding or limiting data favorable to
T4 /T3 therapies. Specific examples from the publications are included in this rebuttal. The unbalanced data presentations and factual errors of Escobar-Morreale et al. and Grozinsky-Glasberg et al. may have influenced
the Committees conclusions. Nonetheless, the Committees document contains false statements and unbalanced
presentations of data independent from those in the other authors publications. Specific examples are included
in this rebuttal. The Committee, the BTA, Escobar-Morreale et al., and Grozinsky-Glasberg et al. are all called
upon to correct their false statements of fact as well as their unbalanced presentations of data relevant to their
conclusions.
Keywords. Armour Thyroid British Thyroid Association Levoxyl Desiccated thyroid Erfa Thyroid FDA
Levothyroxine Synthroid
Introduction: Attacks on
Desiccated Thyroid
In February 2007, an Executive Committee of
the British Thyroid Association (the Committee) published a document in which it denounced Armour
Thyroid (Armour). Armour Thyroid is a brand of
natural desiccated thyroid that contains four parts T4
to one part T3, that is, a ratio of 4 to 1 (4:1). Whether
the Committee intended it or not, its arguments against Armour also apply to other brands of desiccated thyroid, including Erfa Thyroid. Because the
arguments apply to all such products, in this rebuttal
I subsume and refer to all such brands as desiccated
thyroid except when particular passages are specific
to Armour. In its document, the Committee, as well
as opposing the use of desiccated thyroid, also advocated T4 replacement as the preferable treatment
for hypothyroidism.
The basic issues raised by the Committee were
(1) the stability of desiccated thyroid, and (2) its safety and (3) effectiveness as a form of treatment for hypothyroid patients. Considerable evidence that bears
on these issues is readily available. Yet the Committee cited virtually none of it. In this rebuttal, I cite
the evidence they left out of their document. When
faced squarely and considered without prejudice, that
evidence leads to conclusions diametrically opposed
to those of the Committee.
The medical literature contains at least twenty reports of studies in which researchers compared the
effectiveness and safety of different thyroid hormone
therapies.[7][10][1 5 ][16][22][23][24][25][26][29][31][32][33][36][39][40][41
][42][44][45]
Among the therapies compared in the studies
were T4 alone, desiccated thyroid, and combined
synthetic T4 /T3 . Instead of referencing these studies,
2 Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
however, the Committee cited only two papers in
which authors reviewed the most recent studies that
compared T4 monotherapy to synthetic T4/T3. One of
those papers is a review of the studies by EscobarMorreale et al.,[17] and the other is a report of a metaanalysis by Grozinsky-Glasberg et al.[18]
In this paper, I critically dissect relevant parts of
the two papers cited by the Committee. I also show
that both papers contain errors that misinform readers who take the authors statements at face value.
Members of the Executive Committee appear to be
among the misinformed. I include citations below that
indicate that the Committee accepted without question and reiterated false statements of the authors of
the two papers. Possibly as a result of this, but apparently for other reasons, the Committees document
contains falsehoods that I cite below. As will be obvious to readers, only if the falsehoods were true
could the Committee validly deduce its conclusions
about T4 replacement and desiccated thyroid. But the
evidence I present shows that the falsehoods are
indeed false.
and T4 /T3 replacement, are not effective for many patients and because of this, potentially harmful to
them.
Because of its documented ineffectiveness for
many patients and consequent potential harm, T4 replacement should be abandoned as the thyroid hormone therapy of choice. Clinicians should preferably
most often prescribe desiccated thyroid, synthetic
T4 /T3 , of synthetic T3 alone; and the dosages should
best be larger than replacement dosages.
I base this recommendation on several findings:
(1) hypothyroid patients have long used desiccated
thyroid safely and effectively, (2) many studies show
desiccated thyroid to be at least as effective as T 4 replacement, and (3) two studies showed that patients
who used T4 /T3 therapy in a 5:1 ratio (close to the
4:1 ratio in desiccated thyroid) had no adverse effectswhile patients using T4 alone have adverse
effects!and were more satisfied with the combination therapy than with T4 alone (see Figures 1 and
2).
Issues Raised by the Committee
of the British Thyroid Association (BTA)
The Committee contends that T4 is more stable,
safer, and more effective than desiccated thyroid.
This proposition, however, is a mere presumption,
one that is refuted by evidence that I present below.
The Committee bulwarks its proposition only with an
unbalanced presentation of some evidence, and false
laims about other relevant evidence.
As I document below, contrary to the conclusions
of the Committee, the evidence shows that compared
to desiccated thyroid, T 4 is actually less stable.
Moreover, thyroid hormone replacement therapies
(dosages of thyroid hormone that keep the patients
levels of the TSH within its currentbut often revisedreference range), including T4 replacement
Invalid Conclusion
When Bunevicius et al. reported improvement in
cognitive function after patients substituted 12.5 g
of T3 for 50 g of their T4 dosage,[7] other researchers
quickly conducted four studies in which they compared the effectiveness of T4 replacement to T4 /T3 replacement. The ratio of T4 to T3 that patients in the
studies used was far higher than the 4:1 ratio in Armour and Erfa Thyroid. One aim in the studies was
to keep patients TSH levels within the reference
range, which makes the tested T4 /T3 treatments a
form of replacement.
No difference was found between the two types
of replacement therapies. Based on this finding, the
endocrinologists who conducted the studies,[23][24][25]
others,[26] and endocrinologists who wrote editorials
about the studies,[30][43] made a logical error. By using
incorrect universal propositions rather than correct
singular ones, they sweepingly denounced as no more
Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
effective than T4 replacement each and all T4 /T3 therapiesnot just the T4 /T3 replacement tested in the
studies.
They did not bother to note that the T4 /T3 therapy
they studied was not the T4 /T3 therapy long used by
clinicians who have reported treatment results superior to those of T4 replacement. That superior treatment was the use of desiccated thyroid and synthetic
T4 /T 3 products with a T4 /T3 ratio of 4:1 or lower. I
first reported this logical error of the endocrinology
researchers and editorialists in 2003 and again in
2006.[8] But to this date none of them have responded.
I hope that the British Thyroid Association (BTA)
will not be similarly silent. (For a detailed description
of the endocrinologists logical error, see my critique
of the first four T4 vs T4 /T3 studies that followed the
1999 Bunevicius study.[8,pp.2-4])
The Committee made the same error as the researchers who conducted the T4 replacement vs T4 /
T3 replacement studies and the endocrinologists who
wrote editorials about them. I would like to remind
the Committee of the words of one of their countrymen who was one of the greatest intellects in history,
Lord Bertrand Russell: I do like clarity and exact
thinking, and I believe that very important to mankind. Because, when you allow yourself to think inexactly, your prejudices, your bias, your self interest
come in in ways you dont notice, and you do bad
things without knowing that youre doing them. Self
deception is very easy. So I do think exact thinking
immensely important.[5]
Instability of T4 Products
Eric P. Duffy, PhD is Director, Division of PostMarketing Evaluation Office of New Drug Quality
Assessment, OPS, FDA. In 2006, he presented a
slide presentation titled Stability Of Levothyroxine
Sodium Products.[2] On slide 8, Dr. Duffy wrote:
Levothyroxine Tablet Stability: Levothyroxine sodium (T4 ) is labile to [prone to reduced potency by]
the following: Heat, moisture, oxidative conditions,
chemical reactions. These conditions typically occur
during levothyroxine formulation, tableting, packaging, and storage. He then wrote, Many levothyroxine drug products have exhibited: history of sub-optimal stability profile, significant loss of potency over
shelf life, [and] inconsistent stability profiles within
an individual manufacturers drug product line. (Italics mine.)
Another FDA scientist, Steven B. Johnson,
Pharm.D., is with the Division of Pharmaceutical
Evaluation II of the FDA. In a 2003 slide presenta-
tion, he said, Levothyroxine degrades quickly with
exposure to light, moisture, oxygen, and carbohydrate excipients.[3,slide 5] He noted that over the years,
companies worked to improve the stability of their levothyroxine products, and significant changes occurred.[3,slide 6] Obviously, stability was a problem; why
else would companies work to improve stability? In
fact, the stability problem has been so substantial
that until the FDA stopped the practice, many companies engaged in stability overage; that is, the
companies would add more than 100% of the T4 designated on the product label. They did so because
they assumed that potency would be lost, and they
compensated for the loss by packing extra T4 into the
tablets.[2,slide 9][3,slide 5]
The instability of levothyroxine tablets is noteworthy, especially in view of the Committees claim
that levothyroxine products are more stable than desiccated thyroid products. Dr. Johnson cited the noteworthy FDA recall record of levothyroxine: Between 1990 and 1997: 10 recalls, 150 lots, and 100
million tablets.[3,slide 5] (Italics mine.) The reasons for
the FDA recalls are also noteworthy: Content uniformity, sub-potency, and stability failures.[3,slide 5]
Whether intentional or not, the BTAs Executive
Committee painted a grossly imbalanced picture of
the comparative stability of desiccated thyroid and levothyroxine. The Committee clearly cast an unfavorable light on desiccated thyroid by presenting the
meager evidence against it, while failing to disclose
the copious evidence against T4 . The fact is that the
stability of levothyroxine has been far more in question at the FDA than has that of desiccated thyroid.
Stability of Natural Desiccated Thyroid
According to the Committee: The concentration
of thyroid hormones in Armour Thyroid USP is regulated by the manufacturer to United States Food and
Drug Administration (FDA) standards. Despite this,
there have been significant problems with the stability of Armour Thyroid in recent years, prompting
a massive recall of tablets. (Italics mine.) The Committee also wrote, An FDA enforcement removed
more than half a million bottles of Armour Thyroid
from US pharmacies in 2005 due to unstable concentrations of thyroid hormone in the preparation.[1]
Indeed, batches of the product were recalled in
2005.[9] But the Committee mentions problems with
the stability . . . in recent years. (Italics mine.) This
suggests that the FDA has repeatedly recalled Armour batches in two or more years. But the Committee cites only the 2005 recall; I cannot find doc-
4 Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
umentation for others.
The Committees purpose in citing the Armour
recall appears to have been to implicitly argue that
levothyroxine products (levothyroxine sodium, thyroxine, and T4 ) are more stable than desiccated thyroid products. If so, the Committee engaged in cardstacking of evidence, as it failed to disclose a highly
relevant fact: the T4 products Synthroid and Levoxyl
have been recalled far more often than Armour, Erfa
Throid, and other desiccated thyroid hormone products.
Anyone with Internet access can view the public
record at www.fda.gov/search.html. Searches show
that the many recalls of T4 products dwarf the few
recalls of desiccated thyroid.
Clinicians and patients interested in the relative
merits and demerits of T4 and desiccated thyroid
should be aware that desiccated thyroid products are
not carelessly produced. The Committee failed to
note that manufacturers of desiccated thyroid take
proper steps to ensure its potency before the products
are shipped to pharmacies. For example, manufacturer of USP Thyroid tablets take appropriate steps
to ensure consistent potency from tablet-to-tablet and
lot-to-lot. The manufacturer not only performs analytical tests on the raw material (Thyroid USP
powder), but also on the tablets (finished products) to
measure actual T 4 and T3 activity.[11] As a result of
this attention to quality, only two recallsvoluntary
oneshave occurred in the past eight years. These
recalls included fewer than one hundred bottles. The
recalls were for a labeling problem, not for instability
or potency variability as with levothyroxine products.
Ineffectiveness of T4
Replacement for Many Patients
The endocrinology specialty has long claimed
that T4 replacement is effective for most hypothyroid
patients, and that patients need no other treatment
such as T4 /T3 therapy. However, as I wrote in a 2006
review (and in 2003) of four T4 vs T4 /T3 studies
published in 2003, T4 replacement is ineffective for
many hypothyroid patients.[8,p.14] At that time, at least
six studies had shown this to be true.[7][15][16][23][24]
[25][26][27][28]
As I said above, in the 1999 Bunevicius
[7]
study patients who had been on T4 replacement
substituted 12.5 g of T3 for 50 g of their usual T4
dosages. The neuropsychological function of patients
who added T3 to their treatment improved. It is obvious but worth emphasizing that from the patients
improved neuropsychological function, it follows that
their previous T4 monotherapy had failed to provide
them the higher level of function that T4 /T3 provided.
In a large, community-based questionnaire study
in 2002,[27] researchers evaluated the health status of
hypothyroid patients using T4 replacement therapy.
Compared to matched control patients, hypothyroid
patients on adequate dosages of T4 had a higher reported incidence of four diseases: depression, hypertension, diabetes, and heart disease. Hypothyroid patients on inadequate T4 replacement (their TSH levels
were elevated) also had a higher incidence of strokes.
In addition, hypothyroid patients chronically used
more prescription drugs, especially for diabetes, cardiovascular disease, and gastrointestinal conditions.
Patients on T4 replacement had scores 21% higher
(worse) than controls on the General Health Questionnaire. The researchers wrote, This communitybased study is the first evidence to indicate that
patients on thyroxine replacement even with a normal
TSH display significant impairment in psychological
well-being compared to controls of similar age and
sex.[27,p.577]
In the study by Cassio et al.,[26] researchers treated infants who had congenital hypothyroidism with
either T4 or T4 /T3 replacement therapy. The infants
had scores on psychological tests that were lower
than those of infants who were not hypothyroid. The
two replacement therapies did not improve the scores
of the hypothyroid infants, so their psychological impairment presumably persisted.
To take part in the Sawka et al. study,[24] patients
on T4 replacement had to have test evidence of depression: that is, they had to have, . . . evidence of
depressive symptoms as defined by a score of more
than 5 on the 30-item General Health Questionnaire
. . . on 2 occasions, at least 2 wk apart.[24,p.4551] The
researchers found that replacement therapies were not
effective for the patients and, again, presumably left
them depressed.
In the Walsh et al. study,[23] typical symptoms
suffered by hypothyroid patients who were dissatisfied with their T4 replacement included tiredness,
impaired well-being, or weight gain.[23,p.4544] The
study showed that replacement therapies were ineffective for these patients and left them suffering from
their symptoms.
In addition to the four studies I just mentioned,
two other studies also showed the ineffectiveness of
T4 replacement.[15][16] The study by Escobar-Morreale
et al.[15] is especially informative. The researchers reported that patients on both T4 and T4 /T3 replacement
performed worse than controls in the time score and
Visual Scanning Test . . . .[15,p.420] But patients who
used a 5:1 ratio of T4 and T3 did not perform worse
than the healthy control subjects. Also, patients on T4
and T4/T3 replacement therapies did worse than healthy
controls on two other tests (isovolumic relaxation
Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009 5
time and brainstem evoked potentials), but patients
who used T 4 and T3 in a 5:1 ratio did not do worse
than controls.[15,p.420] This positive result for 5:1 T4 /T3
therapy is evidence from Escobar-Morreale et al. that
the therapy was more effective than the two forms of
replacement therapy.
False Reporting by the Committee,
Escobar-Morreale et al., and GrozinskyGlasberg et al.
In this rebuttal to the Committee of the BTA, I
cite incidences of unbalanced presentation of data
that deny readers an accurate understanding of the
research concerning the relative stability, safety, and
effectiveness of desiccated thyroid as comparted to
synthetic T4 products. In the pursuit of scientific
truth, these instances of unbalanced presentation are
lamentable. However, the Committee, Escobar-Morreale et al., and Grozinsky-Glasberg et al. gave false
reports concerning the research data that are an even
more egregious departure from accurate reporting.
The Committees extrapolation that T4 /T3
therapies provide no benefits
The Committee of the BTA wrote, Since this initial study, [the 1999 Bunevicius et al. study[7]] there
have been a further [sic] seven rigorously conducted
(randomized, double-blind, placebo-controlled)
studies . . . . None of the subsequent studies showed
a beneficial effect of combined T4 /T3 therapy on
measures of wellbeing, health and mental functioning. (Italics mine.)
The Committee then concluded, . . . combined
T4 /T3 cannot be recommended because of a lack of
benefit . . . . The studies of T4 /T3 therapy the
Committee referred to involved synthetic hormones,
none of which were used in the 4:1 T4/T3 ratio as
contained in desiccated thyroid. But in its document,
the Committee implies by extrapolation that desiccated thyroid, too, cannot be recommended because
of a lack of benefit. This is a clear-cut non sequitur.
I request that the Committee reconcile its conclusion, at the very least, with the evidence I cite in
this section. This evidence directly contradicts the
Committees conclusion. Older studies show that
T4 /T3 in the form of desiccated thyroid was at least as
effective as synthetic T4 . As Cobb and Jackson wrote
in a drug therapy review, desiccated thyroid products
are equipotent to T4 alone in treating hypothyroidism.[19,p.53] This was determined by a study of the potency of desiccated thyroid using an antigoitrogenic
assay in rats.[13] Most studies of T4/T3 therapy have
not been of desiccated thyroid itself, although at least
12 studies did directly compare desiccated thyroid to
T4 alone.[4][29][31][32][33][35][37][38][39][40][42][45] The Committee, however, did not cite these studies; instead, it extrapolated to desiccated thyroid from studies that
compared synthetic T4 to synthetic T4 /T3 combinations. Reading the same studies the Committee referred to makes clear that its claim of a lack of benefit
of desiccated thyroid is false.
First Bunevicius study. In a study published
in 1999, Bunevicius et al.[7] included 26 hypothyroid
women. Eleven had autoimmune thyroiditis and 15
had been treated for thyroid cancer. Patients either
continued their usual dose of T4 , or they substituted
12.5 g of T3 for 50 g of their usual dosage of T4 .
Bunevicius et al. later wrote that when patients
were undergoing T4 /T3 therapy, they had clear improvements in both cognition and mood, the latter
changes being greater. [21,p.167] The researchers also
wrote, The patients who had been treated for thyroid
cancer showed more mental improvement than the
women with autoimmune thyroiditis . . . .[21,p.167]
However, patients in both groups improved on some
measures.[21,pp.169-171]
This is important to note because in the review
paper that the Committee cited, Escobar-Morreale et
al. falsely reported that only thyroid cancer patients
improved. Specifically, they wrote, . . . the presumed benefits of T3 substitution were restricted to
athyreotic thyroid cancer patients . . . .[17,p.4949] Consider, however, what Bunevicius and Prange actually
reported: Referring to visual analog scales, they
wrote, The advantages [improvements] for combined treatment were statistically significant in the . . .
[autoimmune thyroiditis] group on 4 scales, in the
. . . [thyroid cancer] group on 6 scales.[21,p.170] Table
5 in Bunevicius and Pranges report shows this to be
true.[21,p.172] Escobar-Morreale et al., then, are guilty
of false reporting.
Second Bunevicius study. In the second Bunevicius study,[22] patients were hypothyroid from thyroidectomy for Graves disease. The patients substituted 10 g of T3 for 50 g of their usual T4 monotherapy dose. In their first study, Bunevicius et al.
substituted 12.5 g of T3 for 50 g of T4.[7] Despite
the more modest substitution dose of 10 g of T3 in
the second study, the results indicated that patients
improved with T4 /T3 therapy.
Compared to baseline scores when patients were
using T4 replacement, the patients had statistically
significant improvement on three measures.[22,p.130]
Allowing for a slightly larger significance level (p =
0.06), the patients using T4 also improved on one
other measurea total of four measures. Similarly,
when patients used T4 and T3, they significantly improved on three measures. But allowing for slightly
6 Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
larger significance levels (p = 0.06 to 0.08), these patients also improved on four more measuresa total
of seven measures. This means that with T4 alone,
patients improved on four measures, while on T4 /T3 ,
they improved on seven. With the slightly expanded
significance levels, then, patients improved more with
T4 and T3 combined than they did on T4 alone.
Bunevicius et al. wrote: Thus, to a statistically
significant degree, the substitution of 10 g of T3 reduced the concentration of free T4 , as well as the
symptoms of hypothyroidism and subjective tension,
while improving pairs recalled on the Digit Symbol
Test. In addition, it tended to reduce the symptoms of
hyperthyroidism, to improve mood on the Beck Depression Inventory, as well as feelings of confusion
on the Visual Analog Scale, and to improve the raw
score on the Digit Symbol Test and forward recall on
the Digit Span Test.[22,pp.131-132]
In the 2005 Saravanan study,[14] patients substituted 10 g of T3 for 50 g of their T4 dosages. The
researchers wrote that patients on the different therapies had no differences in a number of test scores.
However, patients who used T4 /T3 had some improvements compared to patients who used T4 alone.
The researchers reported, . . . a significantly greater
reduction in psychiatric caseness [patients who met
the criteria for different disorders] was seen in the T 3
group compared with T4 alone . . . . Improvement
was also seen in the HADS anxiety score [the
Hospital Anxiety and Depression questionnaire] at 3
months.[14,p.807] (Italics mine.)
Patients preference for T4/T3 therapy. The Committee wrote that in two studies in which researchers
compared T4 to T4 /T3 therapy, patients preferred
T4 /T3 therapy. This is a factual error by the Committee. Actually, patients preferred or were more satisfied with T4 /T3 therapy in five studies.[7][15][16][22][36]
In each of the five studies, far more patients pre-
ferred T4/T3 therapy over T4 replacement. Combining
the preference data from the five studies, of 236
patients, 110 patients had no preference. Only 27 pa-
tients preferred T4 replacement while 99 preferred
some form of T4 /T3 therapy. (See Figure 3.)
In two studies,[15][16] patients used T4 /T3 in a ratio
of both 10:1 and 5:1. Of the 61 patients involved, 31
preferred the 10:1 ratio; 30 preferred the 5:1 ratio.
One of the five studies was published in 1999,[7]
another in 2002,[22] and three other studies were published in 2005[15][16][36]all well before the 2007
Committee document published by the British Thyroid Association.[1] Despite this, the Committee failed
to mention that patients preferred T4/T3 therapies.
Perhaps this neglect of the Committee was due to its
dependence on the reviews by Escobar-Morreale et
al.[17] and Grozinsky-Glasberg et al.[18] rather than the
original study reports the reviewers purportedly analyzed. In any case, neglecting this important finding
constitutes an unbalanced presentation of data that
favors T4 replacement over T4 /T3 therapies.
The 1999 and 2002 studies that the Committee
did not reference were the first and second Bunevicius et al. studies.[7][22] At the end of the 1999 study,
the researchers asked patients about their preferences
for a particular form of treatment. The researchers
wrote, When asked at the end of the study whether
they preferred the first or second treatment, 20 patients preferred thyroxine plus triiodothyronine, 11
had no preference, and 2 preferred thyroxine alone (p
= 0.001).[7,p.427] (See Figure 4.)
At the end of the 2002 study, the researchers
asked patients about their preferences. Six patients,
they wrote, preferred combined treatment, reporting
increased energy, better performance, and decreased
tension in the eyes. Two preferred monotherapy with
T4 , and two found no difference.[22,p.132] (See Figure 5.)
In the Applehof et al. study, patients who used
T4 /T3 therapy were more satisfied with the treatment.
In fact, the researchers found a linear relationship between the use of T3 and the number of patients preferring treatment: In the T4 monotherapy group, only
29.2% were satisfied with the treatment; in the group
who used T4 /T3 therapy in a 10:1 ratio, 41.3% were
Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009 7
satisfied; and in the group that used T4 /T3 therapy in
a 5:1 ratio, 52.2% were satisfied. (See Figure 1.)
Escobar-Morreale et al.[15] and Rodriquez et al.[36]
also reported more satisfaction with T 4/T3 therapies
(see Figures 2 and 6). Unfortunately, GrozinskyGlasberg et al., for all practical purposes, gave no attention to patients preference for T4 /T3 therapies. To
their credit, Escobar-Morreale et al. did mention patients preference for T4/T 3 in their abstract, the body
of their review, and in their conclusion section.[15]
In some studies, researchers did not inquire about
patients satisfaction with tested therapies. In the
Walsh et al.[23] study the researchers did inquire, and
there was no difference in patients preferences.
The Committees parroting of false
statements by Escobar-Morreale et al.
and Grozinsky-Glasberg et al.
The Committee wrote, There is no evidence to
favour the prescription of Armour Thyroid in the
treatment of hypothyroidism over the prescription of
thyroxine sodium.[1] The Committee appears to have
argued against desiccated thyroid by appropriately
including it among T4 /T3 therapies. Its claim of no
benefit of these therapies over T4 replacement, however, is false. It is possible that the source of the
Committees erroneous conclusions are false statements by Escobar-Morreale et al. and GrozinskyGlasberg et al. in their reviews of the studies testing
T4 alone vs T4 /T3 therapies.
As Figures 1 through 6 show, patients satisfaction is a benefit often provided by T4 /T3 therapies. In
their meta-analysis of the T4 vs T4/T3 studies, Grozinsky-Glasberg et al. side-stepped this important
finding. They merely included the term satisfaction
in a table,[16,p.2594] and they briefly mentioned patients
dissatisfied with T4 replacement.[16,p.2597] They did not
include the words prefer or preferred in their paper, and they did not include the data from the five
studies in which patients by far preferred T4 /T3 therapies.
Keep in mind that Applehof et al. reported that
weight loss with T4 /T 3 therapy correlated with patients satisfaction with the treatment.[16,p.2672] But
Grozinsky-Glasberg et al. were so dismissive of
weight loss from T4 /T3 therapy that they contradicted
themselves on different pages of their report: In their
results section under Weight Changes they wrote,
The weight in the combination group was lower at
the end of the study, and this difference reached statistical significance . . . .[18,p.2596] (Italics mine.) Yet
in their abstract they wrote, No difference was
found in . . . body weight . . . .[18,p.2592] And in their
discussion section, they wrote . . . there was no significant difference in terms of weight change.[18,p.2597]
Grozinsky-Glasberg et al. also falsely reported
the outcome of Bunevicius and Pranges reanalysis of
their data from their 1999 study.[21] Grozinsky-Glasberg et al. wrote: Only one trial found significant
benefit of combination therapy over the monotherapy.
It was later suggested that this benefit was associated with the cause of hypothyroidism and that
only athyreotic [without a thyroid gland or endogenously produced thyroid hormone] thyroid cancer
patients benefited from the combination therapy,
whereas patients with autoimmune thyroiditis did
not.[18,p.2597] (Italics mine.) Yet clearly, Bunevicius
and Pranges report of their reanalysis shows this
statement to be patently false. In Table 5 of Bunevicius and Pranges report, they showed improvement
on visual analog scales among thyroiditis patients.
Compared to the patients baseline measures (when
they were on T4 replacement), testing when they were
using T4 /T3 therapy revealed statistically significant
(p = 0.02) reductions in sadness, confusion, fearfulness, and irritability.[21,p.172]
In their report, Bunevicius and Prange wrote,
Table 5 shows results on the visual analogue scales.
For each diagnostic group [thyroid cancer and autoimmune thyroiditis patients] on all 8 scales, there was
at least a tendency for improvement after T4 plus T3
compared to T4 alone.[21,p.170] They then wrote, The
advantages for combined treatment were statistically
8 Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
significant in the AT [autoimmune thyroiditis] group
on 4 scales, in the TC [thyroid cancer] group on 6
scales. (All italics mine.) These statements by Bunevicius and Prange and Table 5 in their report show
that in their meta-analysis paper, Grozinsky-Glasberg
et al. falsely reported the results of the Bunevicius
and Prange reanalysis.
Maybe the mistake of Grozinsky-Glasberg et al.
was in taking at face value what Escobar-Morreale et
al. stated in a review of T4 vs T4 /T3 studies. (Grozinsky-Glasberg et al. cited the review paper at the end
of their false statement about the result of the Bunevicius and Prange reanalysis.[18,p.2597]) Escobar-Morreale et al. wrote, A subsequent reanalysis of the
data, removing from the initial study the data from
the two men, from four depressed women, and from
a woman who presented with increased serum TSH
levels at baseline, revealed that the findings originally reported were maintained only in the subset of
athyreotic patients and not in women with autoimmune thyroiditis.[17,p.4949] (Italics mine.) Thus, Escobar-Morreale et al. may be the source of false statements about Bunevicius and Pranges finding. Unfortunately, other researchers have reiterated the false
statements.[36]
Eleven Studies Have Compared
T4 -Replacement to Natural Desiccated
Thyroid: Factual Error of the Committee
Referring to T4 and desiccated thyroid, the Committee wrote, There has never been a direct comparison of these two treatments. (Italics mine.) When
I read this, I immediately turned in my desk chair and
pulled from a filing cabinet 12 published reports of
direct comparison of these two forms of treatment.[4][29][31][32][33][35][37][38][39][40][42][45] Researchers reported
using Armour per se in three of the studies.[4]
[39][40]
One study was published in 1972.[39] The researchers wrote, The present study was designed to
compare the effects of desiccated thyroid and monosodium l-thyroxine [T4 ], administered by mouth, on
serum lipids in a group of hypothyroid patients. The
researchers reported, . . . a cholesterol-lowering
effect was manifested by the time of first testing after
institution of desiccated thyroid or l-thyroxine treatment. They wrote further, The magnitude of the hypolipidemic [fat lowering] effects were [sic] similar
when desiccated thyroid and l-thyroxine were give [sic]
orally in therapeutic [sic] equivalent doses.[39,p.1047]
Another direct comparison was published in
1978.[40] The researchers wrote, The biologic effect of
the two therapies was compared by estimating by interpolation the dose of thyroid hormone that caused the
peak serum TSH after TRH to fall to 5 U/ml.[40,p.1518]
They concluded, . . . a daily dose of 100 mcg of T4 was
on average equal in biologic activity to 101 mg of
desiccated thyroid; 60 mg of desiccated thyroid was
equal to 60 mcg of T4 .[40,p.1518]
Two other research groups showed that the 60 mg
of desiccated thyroid had the effect of 100 g of T4 in
raising the basal metabolic rate.[29][42] A number of other researchers have made direct comparison of desiccated thyroid and T4 .[4][31][32][33][34][37][38] These studies
show that the Committees statement that Armour (and
by extension, similar desiccated thyroid products) has
not been directly compared to T4 was an ex cathedra
pronouncement, one that is clearly false.
Necessity of retractions. In the interest of precision and accuracy in the science of thyroidologyin
fact, in the interest of its credibilityEscobar-Morreale et al., Grozinsky-Glasberg et al., and the Executive Committee of the BTA are compelled to correct
their false reports of Bunevicius and Pranges actual
study results. Also, the Committee is compelled to correct its false statement that no studies have compared T4
to desiccated thyroid.
As the statements of these groups of authors stand,
they drive the body of scientific information in clinical
thyroidology away from the goal of accuracy and truth.
Regarding Escobar-Morreale et al. and GrozinskyGlasberg et al., we have to look no further than the
Committees document to confirm that their incorrect
and inexact reports send ripples of falsehood through
the sea of beliefs within the field of clinical thyroidology
and of its decision-makers. Setting off such ripples is
contrary to the traditional aims of science and is not a
worthy legacy of these authors. On the grounds of science ethics, they are obligated to rectify their errors.
Harmful Ineffectiveness of T4 Therapy
It appears that when the Committee was writing its
document, it had the impression that research had unequivocally established the safety and effectiveness of
T4 replacement. The Committee wrote, The BTA committee [sic] cannot recommend a treatment with possible side-effects [sic], [such as desiccated thyroid],
when a safe and equally-well established treatment
[T 4 replacement] exists.[1] (Italics mine.) The proposition that T4 replacement is safe and effective for all
patients, however, is simply false. Studies show that for
many people, the therapy is harmful by virtue of its ineffectiveness.
In 2000, Bunevicius and Prange wrote: It is conventional to provide replacement treatment with T4
alone, in the belief that each tissue will make sufficient
quantities of T3 (the more potent hormone) for its own
needs. Nevertheless, it has long been noted that after
Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009 9
treatment with T4 alone not all patients are entirely
well.[21,p.167] (Italics mine.) Here they reference a report
by Taylor et al.[44] published in 1970. Today, 39 years
later, studies are still showing that T4 replacement is
ineffective for many patients, subjecting them to the
ravages of deficient thyroid hormone regulation of cell
function. This is indicated by patients who were stable on T4 replacement: (1) still suffering from hypothyroid symptoms and having various abnormal test
scores,[23][24][26][27] (2) entering a study hoping they
would feel better on another thyroid hormone therapy,[25] (3) having disorders plausibly explained by too
little thyroid hormone regulation,[10][16][27][36] (4) gaining
and not being able to lose weight,[12][20] and (5) suffering
potentially-fatal diseases associated with untreated or
undertreated hypothyroidism and using more medications for those diseases.[27]
Inadequate regulation of cell function by thyroid
hormone in patients using T4 replacement can cause
them to not only suffer, but to potentially die earlier
than otherwise. It can also greatly increase medical and
societal costs. Because of these harmful effects, it is
reasonable to conclude that T4 replacementin which
the TSH is kept within the reference rangeis injurious
to many hypothyroid patients and to society at large.
Adverse effects in studies of T4 and T4/T3 therapies. The Committee wrote in its document, Three of
the seven studies show harmful or undesirable effects of
the T4 /T3 combination.[1] One might assume from the
Committees statement that desiccated thyroid and
other T4/T3 therapies are likely to cause adverse effects.
But it would have been obvious that this is not true had
the Committee accurately reported what was found in
the three studies.[15][16][22]
In one of the studies, Escobar-Morreale et al.
compared T4 and T4/T3 replacement to T4/T3 therapy in
a 5:1 ratio. After the study ended they wrote, No adverse effects were reported with any of the treatments.[15,p.420] They also reported the proportion of
patients who had increased heart rates. They defined
increased rates as higher than 120 beats/min in daytime
and higher than 100 beats/min at night. Of 420 patients
on T4 replacement, 13 had raised heart rates. Of 376
patients using T4 /T3 replacement, 13 had increased
rates. But of 377 patients using T 4/T 3 therapy in a 5:1
ratio, only 7 had increased heart rates.[15,p.420] The researchers reported, however, that the groups did not
differ statistically.
In the study by Appelhof et al.,[16] patients who used
T4 /T3 therapy in a 5:1 ratio had no adverse effects. In
contrast, patients who used T4 and T4 /T3 replacement
did have adverse effects. Appelhof et al. wrote of adverse effects in the study: One participant (5:1 [T4 /T3 ]
group) withdrew because of unexpected travel abroad
for family matters and was excluded from all analyses.
Seven patients withdrew because of side effects, four in
the LT4 group and three in the 10:1 [T4 /T3 ] group.
Various side effects were mentioned (e.g. fatigue, muscle aches, dizziness, irritability), but no specific complaints could be identified for those on combination
therapy.[16,p.2668] (see Figure 7).
In the second Bunevicius et al study,[22] the researchers compared T 4 to T4 /T3 replacement. More
patients were satisfied with T4 /T3 than with T4 replacement. (Figure 5) Perhaps the lack of satisfaction
of patients using T4 replacement resulted from the
adverse effects they experienced: two patients reported
that they experienced sensitiveness of the heart, and
one reported hand tremor.[22,p.132]
Of most relevance to desiccated thyroid, studies of
patients who used T4 /T3 therapy in a ratio close to that
of desiccated thyroid had no adverse effects. The Committee failed to report this, just as it failed to report that
patients in studies of T4 replacement have had adverse
effects. By failing to report accurately, the Committee
cast an unjustified shadow of doubt over T4/T3 therapies, including desiccated thyroid, and it flooded T4
replacement with an indefensible light of safety.
Conclusions
In its document on desiccated thyroid and T4 /T3
therapies, the Executive Committee of the British Thyroid Association presented a grossly unbalanced picture of the stability of levothyroxine sodium, Armour
Thyroid, and by extension, other prescription desiccated thyroid products such as Erfa Throid. The Committee also reiterated false statements about T4/T3 therapies contained in reports by other researchers. Furthermore, the Committee did this without mentioning or
accounting for the other researchers variances from
the facts.
In addition, in its denouncement of desiccated
thyroid, the Committee failed to account for the outcome of two highly relevant studies.[15][16] In these
studies, treatment with T4 and T3 in a 5:1 ratio (close to
10 Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009
the 4:1 ratio in desiccated thyroid) was more effective
in some ways than was T4 replacement and T4 /T3 replacement.
While warning of adverse effects from desiccated
thyroid, the Committee failed to disclose the complete
lack of adverse effects among patients who used T4 and
T3 in a 5:1 ratio.[15][16] It also failed to disclose that
patients using T4 replacement and T4 /T3 replacement
(in 10:1 to 15:1 ratios) had adverse effects.[16]
Moreover, the Committee failed to account for
three harmful effects from T4 replacement. These are:
(1) continued suffering from hypothyroid symptoms by
patients who are restricted to T4 replacement therapy[7][15][16][23][24][25][26][27][28]in as high a percentage as
50%,[27] (2) a higher incidence in these patients of diseases associated with hypothyroidism,[27] and (3) the
use of more drugs by the patients.[27]
At the top of its homepage, the BTA once indicated
that it is Encouraging the Highest Sandards [sic] of
Research and Patient Care. I trust that the BTAs integrity is such that it will conduct itself in accord with
this statement. Hence, I also expect that its Executive
Committee will revise its document on desiccated thyroid based on a careful reading of the original reports of
the studies to which they refer, taking note of the
findings I have described. As the Committee does so,
the scientific and humanitarian imperatives are that it
abide by the advice of one of the United Kingdomsindeed, historysmost eminent logicians:
When you are studying any matter or considering any
philosophy, ask yourself only what are the facts, and
what is the truth that the facts bear out. Never let yourself be diverted either by what you wish to believe, or by
what you think would have beneficent social effects if
it were believed. But look only and surely at what are
the facts.[6]
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
References
1. The British Thyroid Association Executive Committee
Armour Thyroid (USP) and combined thyroxine/ triiodothyronine as thyroid hormone replacement: a
statement from February 2007. http://www.british
thyroidassociation.org/armour_statement_2007.pdf
2. Duffy, E.P.: Stability of levothyroxine sodium products, 2006. http://www.fda.gov/ohrms/dockets/ac/06
/slides/2006-4228S1-01-04-Eric%20Duffy%20 slides
.pdf
3. Johnson, S.B.: Endogenous substance bioavailability
and bioequivalence: levothyroxine sodium tablets,
March 13, 2003. http://www.fda.gov/ohrms/dockets
/ac/03/slides/3926S2_07_Johnson.ppt
4. LeBoff, M.S., Kaplan, M.M., Silva, J.E., et al.: Bioavailability of thyroid hormones from oral replacement preparations. Metabolism, 31(9):900-905, 1982.
16.
17.
18.
Russell, B.:1959 Interveiw of Bertrand Russell by J.F.
McDonald. http://www.youtube.com/watch?v=LUa
S O9WDcng
Russell, B: Bertrand Russell, BBC interview, 1959.
http://www.youtube.com/watch?v=L7I9pgqiLo0&
feature=related
Bunevicius, R., Kazanavicius, G., Zalinkevicius, R., et
al.: Effects of thyroxine as compared with thyroxine
plus triiodothyronine in patients with hypothyroidism.
N. Engl. J. Med., 340:424-429, 1999.
Lowe, J.C.: Thyroid hormone replacement therapies:
ineffective and harmful for many hypothyroid patients.
Thyroid Science, 1(1):C1-21, 2006. http://www
.thyroidscience.com/Criticism/lowe.dec.2006/t4%2
0vs%20t4t3%20studies.htm
FDA: Recalls and Field Corrections: DrugsClass II,
May 11, 2005. www.fda.gov/bbs/topics/enforce/2005
/ENF00899.html
Siegmund, W., Spieker, K., Weike, A.I., et al.: Replacement therapy with levothyroxine plus triiodothyronine (bioavailable molar ratio 14:1) is not superior to
thyroxine alone to improve well-being and cognitive
performance in hypothyroidism. Clin. Endocrinol.
(Oxf), 60(6):750-757, 2004.
Western Research Labs, 2007. http://www.wes-throid.
com/vs.asp
Tigas, S., Idiculla, J., Beckett, G., et al.: Is excessive
weight gain after ablative treatment of hyperthyroidism due to inadequate thyroid hormone therapy? Thyroid, 10(12):1107-1111, 2000.
Mangieri, C.N. and Hund, M.H.: Potency of United
States Pharmacopeia desiccated thyroid tablets as determined by the antigoitrogenic assay in rats. J. Clin.
Endocrinol. Metab., 30:102-104, 1970.
Saravanan, P., Simmons, D.J., Greenwood, R., et al.:
Partial substitution of thyroxine (T4) with tri-iodothyronine in patients on T4 replacement therapy: results of
a large community-based randomized controlled trial.
J. Clin. Endocrinol. Metab., 90(2):805-812, 2005.
Escobar-Morreale, H.F., Botella-Carretero, J.I.,
Gmez-Bueno, M., et al.: Thyroid hormone replacement therapy in primary hypothyroidism: a randomized trial comparing L-thyroxine plus liothyronine
with L-thyroxine alone. Ann. Intern. Med., 142(6):
412-424, 2005.
Appelhof, B.C., Fliers, E., Wekking, E.M., et al.:
Combined therapy with levothyroxine and liothyronine in two ratios, compared with levothyroxine monotherapy in primary hypothyroidism: a double-blind,
randomized, controlled clinical trial. J. Clin. Endocrinol. Metab., 90(5):2666-2674, 2005.
Escobar-Morreale, H.F., Botella-Carretero, J.I., Escobar del Rey, F., et al.: Review: Treatment of hypothyroidism with combinations of levothyroxine plus
liothyronine. J. Clin. Endocrinol. Metab., 90(8):49464954, 2005.
Grozinsky-Glasberg, S., Fraser, A., Nahshoni, E., et
al.: Thyroxine-triiodothyronine combination therapy
versus thyroxine monotherapy for clinical hypothy-
Lowe, J.C.: Stability, effectiveness, and safety of desiccated thyroid . . . . Thyroid Science 4(3):C1-12, 2009 11
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
roidism: meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab., 91:2592-2599, 2006.
Cobb, W.E. and Jackson, I.M.: Drug therapy reviews:
management of hypothyroidism.Am. J. Hosp. Pharm.,
35(1):51-58, 1978.
Bastemir, M., Akin, F., Alkis, E., et al.: Obesity is associated with increased serum TSH level, independent
of thyroid function. Swiss. Med. Wkly., 137(29-30):
431-434, 2007.
Bunevicius, R. and Prange, A.J.: Mental improvement
after replacement therapy with thyroxine plus triiodothyronine: relationship to cause of hypothyroidism. Int. J. Neuropsychopharmacol., 3(2):167174, 2000.
Bunevicius, R., Jakubonien, N., Jurkevicius, R., et al.:
Thyroxine vs thyroxine plus triiodothyronine in
treatment of hypothyroidism after thyroidectomy for
Graves disease. Endocrine, 18(2):129-133, 2002.
Walsh, J.P., Shiels, L., Mun Lim, E.E., et al.: Combined thyroxine/liothyronine treatment does not improve well-being, quality of life, or cognitive function
compared to thyroxine alone: a randomized controlled
trial in patients with primary hypothyroidism. J. Clin.
Endocrinol. Metab., 88(10):4543-4550, 2003.
Sawka, A.M., Gerstein, H.C., Marriott, M.J., et al.:
Does a combination regimen of thyroxine (T4) and
3,5,3-triiodothyronine improve depressive symptoms
better than T4 alone in patients with hypothyroidism?
Results of a double-blind, randomized, controlled trial.
J. Clin. Endocrinol. Metab., 88(10):4551-4555,
2003.
Clyde, P.W., Harari, A.E., Getka, E.J., and Shakir,
K.M.M.: Combined levothyroxine plus liothyronine
compared with levothyroxine alone in primary hypothyroidism: a randomized controlled trial. J.A.M.A.,
290:2952-2958, 2003.
Cassio, A., Cacciari, E., Cicgnani, A., et al.: Treatment of congenital hypothyroidism: thyroxine alone or
thyroxine plus triiodothyronine? Pediatrics, 111(5):
1055-1060, 2003.
Saravanan, P., Chau, W.F., Roberts, N., et al.: Psychological well-being in patients on adequate doses
of L-thyroxine: results of a large, controlled community-based questionnaire study. Clin. Endocrinol.
(Oxf.), 57(5):577-585, 2002.
Walsh, J.P.: Dissatisfaction with thyroxine therapy:
could the patients be right? Curr. Opin. Pharmacol.,
2:717722, 2002.
Lavietes, P.H. and Epstein, F.H.: Thyroid therapy of
myxedema: A comparison of various agents with a
note on the composition of thyroid secretion in man.
Ann. Intern. Med., 60:79-87, 1964.
Cooper, D.S.: Combined T4 and T3 therapyback to
the drawing board. J.A.M.A., 290:3002-3004, 2003.
Gorowski, T., Pucilowska, J., and Wernic, K.: Comparative effects of desiccated thyroid gland and sodium
salt of L-thyroxine in the treatment of hypothyroidism.
Pol. Tyg. Lek., 44(32-33):768-770, 1989.
32. Krenning, E.P., Docter, R., Visser, T.J., et al.: Replacement therapy with L-thyroxine: serum thyroid
hormone and thyrotropin levels in hypothyroid patients changing from desiccated thyroid to pure thyroxine substitution therapy. Neth. J. Med., 28(1):1-5,
1981.
33. Felt, V. and Nedvidkova, J.: Comparison of treatment
with L-thyroxine and a dried thyroid gland preparation
in patients with hypothyroidism. Vnitr. Lek., 28
(11):1067-1073, 1982.
34. Cobb, W.E. and Jackson, I.M.: Drug therapy reviews:
management of hypothyroidism. Am.J. Hosp. Pharm.,
35(1):51-58, 1978.
35. Wartofsky, L.: Combined levotriiodothyronine and
levothyroxine therapy for hypothyroidism: are we a
step closer to the magic formula? Thyroid, 14(4):247248, 2004.
36. Rodriguez, T., Lavis, V.R., Meininger, J.C., et al.:
Substitution of liothyronine at a 1:5 ratio for a portion
of levothyroxine: effect on fatigue, symptoms of depression, and working memory versus treatment with
levothyroxine alone. Endocr. Pract., 11:223233,
2005.
37. Kosowicz, J., Horst-Sikorska, W., Lacka, K., et al.:
Outcome of treating hypothyroidism with thyreoideum. Pol. Tyg. Lek, 48(27-28):599-602, 1993.
38. Warszawie, C.M.K.P.: Treatment of hypothyroidism
with L-thyroxine. Pol. Tyg. Lek, 48(27-28):605-608,
1993.
39. Singh, S.P., Feldman, E.B., and Carter, A.C.: Desiccated thyroid and levothyroxine in hypothyroidism:
comparison in replacement therapy. N.Y. State J.
Med., 72(9):1045-1048, 1972.
40. Sawin, C.T., Hershman, J.M., Fernandez-Garcia, R.,
et al.: A comparison of thyroxine and desiccated thyroid in patients with primary hypothyroidism. Metabolism, 27(10):1518-1525, 1978.
41. Smith, R.N., Taylor, S.A., and Massey, J.C.: Controlled clinical trial of combined triiodothyronine and
thyroxine in the treatment of hypothyroidism. Brit.
Med. J., 4:145-148, 1970.
42. McGavack, T.H. and Reckendorf, H.K.: Therapeutic
activity of desiccated thyroid substance, sodium Lthyroxine and D, L-triiodothyronine: a comparative
study. Am. J. Med., 20:774-777, 1956.
43. Kaplan, M.M., Sarne, D.H., and Schneider, A.B.:
Editorial: In search of the impossible dream? Thyroid
hormone replacement therapy that treats all symptoms
in all hypothyroid patients J. Clin. Endocrinol. Metab., 88(10):4540-4542, 2003.
44. Taylor, S., Kapur, M., and Adie, R.: Combined thyroxine and triiodothyronine for thyroid replacement
therapy. Brit. Med. J., 2:270-271, 1970.
45. Baisier, W.V., Hertoghe, J., and Eeckhaut, W.:
Thyroidinsufficiency: is thyroxine the only valuable
drug? J. Nutr. Environ. Med., 11:159-166, 2001.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- PEBC Application Pharmacist Document EvaluationDocumento2 páginasPEBC Application Pharmacist Document EvaluationmcarthooAinda não há avaliações
- 8 CPSDocumento2 páginas8 CPSpharmacist2000Ainda não há avaliações
- GSK Pakistan-Annual Report 2007Documento74 páginasGSK Pakistan-Annual Report 2007Bassanio BrokeAinda não há avaliações
- Gandanta - Junction of Fire & WaterDocumento4 páginasGandanta - Junction of Fire & WaterVaraha Mihira0% (1)
- Ashtakvarga and Transits - An Article by MurtyDocumento4 páginasAshtakvarga and Transits - An Article by MurtySachin MakhijaAinda não há avaliações
- Relationships With ParentsDocumento2 páginasRelationships With ParentsVaraha Mihira100% (1)
- Retrograde Planets AIA PDFDocumento28 páginasRetrograde Planets AIA PDFSachin MakhijaAinda não há avaliações
- Planetary Astrology of Human Affairs PDFDocumento114 páginasPlanetary Astrology of Human Affairs PDFSachin MakhijaAinda não há avaliações
- Notes On Medical AstrologyDocumento14 páginasNotes On Medical AstrologySachin Makhija50% (2)
- ProgenyNotes-An Article by Ventak RamanaDocumento7 páginasProgenyNotes-An Article by Ventak RamanaSachin MakhijaAinda não há avaliações
- ManusmritiDocumento244 páginasManusmritiSachin MakhijaAinda não há avaliações
- Kalam ChartDocumento3 páginasKalam ChartSachin MakhijaAinda não há avaliações
- Effects of CombustionsDocumento1 páginaEffects of CombustionsSachin MakhijaAinda não há avaliações
- 3 Nakshatra Chintamani R BhattDocumento29 páginas3 Nakshatra Chintamani R BhattSachin Makhija100% (1)
- YantrasDocumento12 páginasYantrasSachin Makhija100% (1)
- 2 Nakshatra Chintamani R BhattDocumento22 páginas2 Nakshatra Chintamani R BhattSachin MakhijaAinda não há avaliações
- 1 Nakshatra Chintamani R BhattDocumento31 páginas1 Nakshatra Chintamani R BhattSachin MakhijaAinda não há avaliações
- Skin Cancer and Nanoscience Case StudyDocumento1 páginaSkin Cancer and Nanoscience Case StudySachin MakhijaAinda não há avaliações
- Prasana Shastra or Horary Astrology B S Rao S2Documento100 páginasPrasana Shastra or Horary Astrology B S Rao S2Sachin MakhijaAinda não há avaliações
- Rajesh Potdar Profile PQS-4Documento3 páginasRajesh Potdar Profile PQS-4DeepakAinda não há avaliações
- 20 Encapsulation of Fragrances and Flavours: A Way To Control Odour and Aroma in Consumer ProductsDocumento2 páginas20 Encapsulation of Fragrances and Flavours: A Way To Control Odour and Aroma in Consumer ProductsKashif RehanAinda não há avaliações
- 2014 - Pharmaceuticals and Healthcare Q214 Round Up (BMI)Documento33 páginas2014 - Pharmaceuticals and Healthcare Q214 Round Up (BMI)SamAinda não há avaliações
- Konduktometri Jurnal KaiDocumento9 páginasKonduktometri Jurnal Kaianggihalfiantara_178Ainda não há avaliações
- IVMS ID High Yield Microbiology Antimicrobial Pharmacology and IDDocumento58 páginasIVMS ID High Yield Microbiology Antimicrobial Pharmacology and IDiahmed3000100% (1)
- Quality Risk Management Ich Q9Documento57 páginasQuality Risk Management Ich Q9prakash deshmukhAinda não há avaliações
- Phyllanthus Niruri PhytochemistryDocumento11 páginasPhyllanthus Niruri PhytochemistryAlvian Rahman Ssyah100% (1)
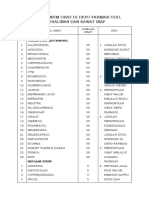
- Stok Minimum Obat Di Depo Farmasi Ugd, Persalinan Dan Rawat InapDocumento2 páginasStok Minimum Obat Di Depo Farmasi Ugd, Persalinan Dan Rawat InapsumalataAinda não há avaliações
- Dosis Obat Untuk Anak: No. Nama Obat Frekuensi Dosis Dosis Maksimal Sediaan SumberDocumento1 páginaDosis Obat Untuk Anak: No. Nama Obat Frekuensi Dosis Dosis Maksimal Sediaan SumberAbikbaeAinda não há avaliações
- Generic Name: Classification: IndicationDocumento2 páginasGeneric Name: Classification: IndicationKristine YoungAinda não há avaliações
- Pharmaceutical Calculation I - Pharmaceutical CalculationDocumento39 páginasPharmaceutical Calculation I - Pharmaceutical Calculationlili fitrianiAinda não há avaliações
- Truth in AdvertisingDocumento3 páginasTruth in AdvertisingClyde TanAinda não há avaliações
- PharmaBiotech Flyer 105x210mm Low 140312Documento16 páginasPharmaBiotech Flyer 105x210mm Low 140312Yaqoob AliAinda não há avaliações
- Drug Study For AsthmaDocumento3 páginasDrug Study For AsthmaDianne MaeAinda não há avaliações
- DendrimersDocumento8 páginasDendrimersAjaya BhattaraiAinda não há avaliações
- Regional Anaesthesia in Patients On Antithrombotic.4 PDFDocumento33 páginasRegional Anaesthesia in Patients On Antithrombotic.4 PDFsatyanarayana reddyAinda não há avaliações
- Nihms579455 PDFDocumento78 páginasNihms579455 PDFMASIEL AMELIA BARRANTES ARCEAinda não há avaliações
- Practice Test # 01 (Past Year PPSC Paper) : JOIN IS at WHATSAPP +92 333 2243031Documento19 páginasPractice Test # 01 (Past Year PPSC Paper) : JOIN IS at WHATSAPP +92 333 2243031Saima ShehzadAinda não há avaliações
- Randoxintl8 PDFDocumento23 páginasRandoxintl8 PDFdatitoxAinda não há avaliações
- Minoxidil 10%, Finasteride 0.1%, Biotin 0.2%, and Caffeine Citrate 0.05% Hydroalcoholic SolutionDocumento5 páginasMinoxidil 10%, Finasteride 0.1%, Biotin 0.2%, and Caffeine Citrate 0.05% Hydroalcoholic SolutionJafar HerizAinda não há avaliações
- United States Food and Drug Administration (Usfda)Documento50 páginasUnited States Food and Drug Administration (Usfda)Hyma RamakrishnaAinda não há avaliações
- TABLE 56-4 - Neurological Side Effects of Antipsychotic DrugsDocumento1 páginaTABLE 56-4 - Neurological Side Effects of Antipsychotic DrugsDragutin PetrićAinda não há avaliações
- 6 Sept 23 LKDocumento178 páginas6 Sept 23 LKDurrah Zati YumnaAinda não há avaliações
- Solubility Enhancement of Nitazoxanide Using SolidDocumento15 páginasSolubility Enhancement of Nitazoxanide Using SolidErick SalgadoAinda não há avaliações
- 16 10 25 Decarboxylation of THCA To Active THC PDFDocumento3 páginas16 10 25 Decarboxylation of THCA To Active THC PDFRafael Ignacio Leal QuijónAinda não há avaliações
- Lasa High Alert FarmasiDocumento10 páginasLasa High Alert FarmasiUlfa ErviliaAinda não há avaliações
- University of San Carlos Department of Business Administration School of Business and EconomicsDocumento4 páginasUniversity of San Carlos Department of Business Administration School of Business and EconomicsDaisy KetchAinda não há avaliações