Escolar Documentos
Profissional Documentos
Cultura Documentos
Gapo Syndrome (Mckusick 23074) - A Connective Tissue Disorder
Enviado por
Attar RahaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Gapo Syndrome (Mckusick 23074) - A Connective Tissue Disorder
Enviado por
Attar RahaDireitos autorais:
Formatos disponíveis
American J o u r n a l of Medical Genetics 37:213-223 (1990)
GAPO Syndrome (McKusick 23074)-A Connective
Tissue Disorder: Report on Two Affected Sibs and on the
Pathologic Findings in the Older
Anita Wajntal, Celia P. Koiffmann, Berenice B. Mendonqa, Dorina Epps-Quaglia, Myriam Nacagami
Sotto, Patricia B.M. Rati, and John M. Opitz
Genetic Counseling Unit, Department of Biology, Institute of Biosciences (A. W., C.P.K.), Endocrinology Unit of the
Faculty of Medicine (B.B.M., D.E.-Q.),Pathology Department of the Faculty of Medicine (M.N.S., P.B.M.R.),
University of ,960Paulo, Sao Paulo, Brazil; Shodair Childrens Hospital, Helena, Montana (J.M.O.)
GAPO syndrome was described in 12 patients
from 7 families. Constant manifestations include dwarfism, alopecia, pseudoanodontia,
and a peculiar, geriatric facial appearance.
We describe the autopsy findings and all
available clinical data on one deceased patient and his living affected sister, previously
reported as short abstracts (Epps et al.: Cienc
Cult 29(Suppl):740, 1977; Wajntal et al.: Cienc
Cult 34(Suppl):705, 1982). Both had the characteristic anomalies of this syndrome but optic atrophy was absent; instead, they had
glaucoma and keratoconus; hypogonadism
was present in both patients. Biopsy and autopsy findings show that the GAPO syndrome
is a dyshistogenetic sequence due to accumulation of extracellular material and thus
should be called GAPO dysplasia. We suggest
that the basic defect in this autosomal recessive disorder is possibly related to a lack of
breakdown of the extracellular components,
perhaps due to an enzyme deficiency involved
in the metabolism of extracellular matrix.
KEY WORDS: collagen and ground substance accumulation, hypogonadism, autosomal recessive inheritance
Twelve patients from 7 different families have been reported [Andersen and Pindborg, 1947; Epps et al., 1977;
Fuks et al., 1978; Gorlin et al., 1978; Shapira et al., 1982;
Wajntal et al., 1982; Gagliardi et al., 1984; Silva, 1984;
hpton and Gorlin, 1984; Manouvrier-Hanu et al., 19871.
We give detailed reports of the same patients previously
reported by Epps et al. [19771 and Wajntal et al. [19821
and mentioned in Freire-Maia and Pinheiro [1984].
FAMILY HISTORY
The family is of Brazilian ancestry, from the state of
Ceara (northern Brazil), and lives in Sao Paulo, Brazil.
The patients have been followed a t the Hospital das
Clinicas, University of Sao Paulo, for the last 23 years.
Their parents are multiply consanguineous (Fig. 1).In
1976, when they were referred for genetic evaluation,
the mother (IV-10) was 53 years old, the father (IV-9)
was 56 years old, patient 1 07-41 was 27 years old, and
patient 2 (V-8)was 20 years old. Both parents were short
(mother 143 cm, father 155 cm) and, except for the sensorineural hypoacusia of the mother, they were normal.
Three of the maternal sisters have hearing deficits and 2
have short stature. One of the patients sisters is also
short (137 cm). Both father and mother are the product
of a consanguineous marriage, but the exact degree of
consanguinity could not be established between the fathers parents. Thus the patients have a minimum coefficient of inbreeding of 1/16 (Fig. 1).
CLINICAL REPORTS
Patient 1
INTRODUCTION
History. Patient 1 (V-4, ADA) was born at term
GAPO is an acronym coined by Tipton and Gorlin
after a n uneventful pregnancy and home delivery. His
[19841 to refer to a syndrome of growth retardation (G),
alopecia (A),pseudoanodontia (P),and optic atrophy (0). birth weight and length were not recorded but were
similar to those of his normal sibs. At birth his skin was
thick and he had generalized atrichia. His teeth never
erupted. There was initial delay in motor development,
Received for publication June 28,1989; revision received Novembut
school performance was normal. The available
ber 20, 1989.
growth data are: when he was 12 years old (Fig. 2a), his
Address reprint requests to Anita Wajntal, Unidade de Aconselhamento Genetico, Departamento de Biologia, Instituto de Bio- height was 108 cm (<3rd centile), weight 18,300 g (<3rd
cihcias, Universidade de Sao Paulo, Caixa Postal 11461-CEP centile), OFC 51.5 cm (<50th centile), and he had a bone
05499, S&o Paulo, S.P., Brazil.
age of 7 years. When he was 14 years old his height was
0 1990 Wiley-Liss, Inc.
214
Wajntal et al.
I
/I
II I
I
O A
10
I V
10
21-28
11-20
V
I
Fig. 1. Pedigree
Fig. 2. Patient 1 at 12 years old (a)and 27 years old (b).(Photo b reproduced from Freire-Maia and
Pinheiro, 1984, with permission of the publisher.)
G A P 0 Syndrome: A Connective Tissue Disorder
122 cm (<<3rd centile). Puberty occurred spontaneously at age 13 years.
When reexamined a t 27 years old (Fig. 2b), his height
was 138 cm (<<5th centile) and weight was 32 kg. He
had a gerodermic facial appearance, prominent supraorbital ridges, bilateral keratoconus and ptosis of upper
lids, lagophthalmos, absence of eyebrows and eyelashes,
a n inner canthal distance of 4 cm, interpupillary distance of 8 cm, depressed nasal bridge, protruding lips
with ptosis of the lower lip, pseudoanodontia without
alveolar ridges; high palate and micrognathia; redundant, hyperelastic skin with poor wound healing, depressed scars, depigmented areas, unusual wrinkles,
nodules especially on scalp and some on face (Fig. 3a,b),
neck, and trunk; hyperextensibility of fingers and hyperconvexity of nails, a palpable liver 8 cm below the
right costal margin; normal genitalia, penis measuring
12 x 2.5 cm and testes (right 5 x 3.5 cm, left 5 x 4 cm).
Pubic and axillary hair were absent. When 34 years old,
the patient had recurrent ear, eye, and respiratory infections; he died of bronchopneumonia and respiratory
acidosis at age 35 years.
Skin biopsy and sweat test. At age 12 years skin
Fig. 3. Patient 1 (on the right) at 32 years old and patient 2 a t 25
years old. a: Frontal view. b Lateral view.
215
biopsies of scalp and axillae were performed. Scalp biopsy showed a thin epidermis with lack of epithelial
ridges. The papillary dermis contained clumps of homogeneous amorphous hyaline material and collagen fibers. Residual hair follicles were surrounded or filled
with homogeneous eosinophilic material. Axillary skin
showed the characteristic dermis with sparse hair follicles and normal apocrine glands with areas of the same
amorphous material in papillary dermis. The described
hyaline material was periodic acid-Schiff (PAS)positive,
diastase resistant, and was not stained by the Congo red
stain for amyloid. The elastic fibers, evaluated by resorcin-fuchsin stain, were almost absent in the reticular
dermis where the eosinophilic material was present.
When palm sweating was induced a t age 12 years there
was absence of sweat production. Reduced sweating was
present on the 2nd and 5th phalanges.
Radiologic manifestations
Head. Reduced density of calvaria and sclerosis of
the cranial base. Absence of pneumatization of the maxillary sinuses. Apneumatic hypoplasia of mastoid apophysis and facial sinuses with a marble-like aspect (Fig.
4a,b). Planigraphic cuts showed clouding of the median
ear which was small. Nasal cavities were of diminished
caliber because of excess soft tissue, but permeability
was preserved bilaterally.
Chest. Demineralization of vertebral bodies, alteration of the discal surface with Schmorls nodules, disc
calcification of Cg and Cg reduced intervertebral distance.
Pelvis. Small with normal articulation.
Long bones. Reduced density, bowing of diaphyses,
and elongation of distal metaphyses, especially in femora and tibiae (Fig. 5a,b).
Hands and feet. Short metacarpals, metatarsals,
and phalanges with wide diaphyses (Fig. 6).
Autopsy, Macroscopic findings showed a thickened
arachnoid membrane over the brain convexity and
thickened pericardium with a verrucous appearance,
coarse and whitish, similar to grated coconut. This
coarse material was also present on the epicardium (Fig.
7) along the coronary vessels. There was atrial dilatation with elongated pectineus muscles and prolapse of
the 3 tricuspid valve leaflets and of the 2 mitral valve
leaflets (Fig. 8). There were hardened plaques in the
coronary lumen narrowing i t up to 10% of its original
size in the anterior descending and the circumflex arteries. On the visceral pleurae there was the same material as on the epicardium and pericardium. The peritoneum was also thickened with whitish lumps on the
liver and the spleen; the liver had a thickened capsule
and widening of the portal spaces, which were joined by
whitish septa.
Microscopic examination using hematoxylin and eosin staining showed a n increase of a n amorphous hyaline substance in all organs and interstitia. In the
hepatic parenchyma, this substance was responsible for
the thickening of the portal spaces, forming bridges
which joined the portal spaces. The same changes were
present in the lymph nodes, spleen, entire digestive
tract, gallbladder, mesentery, and the endocrine gland
216
Wajntal et al.
Fig. 4. Skull roentgenograms of patient 1. a: Frontal view. b: Lateral view.
Fig. 5. Long bone roentgenograms of patient 1. a: Ulna and radius. b: Tibia
interstitia (hypophysis, thyroid, adrenals, pancreas,
and testes) (Fig. 9). In the kidneys, besides the interstitial widening caused by the amorphous material, there
was hyalinization of the subcapsular glomeruli; in the
heart there was valvular dysplasia characterized by
valvular fibroelastic proliferation and amorphous material storage in the interstitium of the myocardium.
Study of the ocular globe showed hypophoria, retino-
schisis, and hypermature cataract; there was no optic
nerve atrophy but there was a thickened dura surrounding the optic nerves (Fig. 10a,b) and atrophy of the
ganglion cells of the retina.
In the bones there was delay of bone maturation with
a great quantity of primary trabecules and accumulation of the amorphous and hyaline material.
In the skin (Fig. lla-d) there was severe atrophy of
G A P 0 Syndrome: A Connective Tissue Disorder
217
Fig. 8. Patient 1,necropsy of heart showing section of right ventricle
with prolapse of the tricuspid valve leaflets (arrowheads).
Fig. 6. Hand roentgenograms of patient 1.
epidermis and of cutaneous adnexa which were surrounded and frequently replaced by the amorphous material and collagen. The dermis studied with resorcinfuchsin staining showed a small number of elastic fibers.
The fibrous and hyaline material, which replaced the
cutaneous adnexa, was strongly stained by Masson trichromic and was PAS positive and diastase resistant.
The thin fibrillar amorphous material, which was present in the papillary dermis, between the thickened collagen fibers and also next to the cutaneous adnexa,
showed metachromasia when stained by toluidine blue
a t pH 7.0, being composed of mucine and probably hyaluronic acid. This material was almost completely digested by hyalozyme, suggesting the presence of hyaluronic acid in this material. Congo red staining was
negative, thus excluding a n amyloid origin of the hyaline storage. Staining with scarlet-R was equally negative, excluding a fatty origin of this material.
Dermatoglyphics
Digits: left hand: WD (131, A", L" (5),L" (121, Ws (8);
right hand: WD(141, A", L" (51,L" (8), L" (13). Mainline
formula: left hand: 9.-7-9.9.5'. 13.t'-A.A/LR.0.L.W",
right hand: 9.-9.9. 7.5' -5'.13.t'-A.A./LR.L.L.L.
There
was a n incomplete simian crease on both hands.
Fig. 7. Patient 1, necropsy of heart showing the presence of verrucous coarse material on the epicardium (arrows).
Patient 2
History. Patient 2 (V-8, MMA), the sister of patient
1,was first seen when 4 years old. She was born a t term
after a n uneventful pregnancy and home delivery. Her
birth weight and length were not recorded, but were said
to be normal. Neuromotor development was normal and
she had normal black hair on her scalp, which she lost
progressively after age one year; there was complete
alopecia a t age 2 years. She had choanal stenosis which
caused respiratory problems. Breast development and
menarche occurred a t age 15;her menstrual cycles have
always been irregular with amenorrheic episodes of 2 or
3 months and, later, for up to 12 months; she has not had
menses for 3 years and is receiving hormone replacement.
218
Wajntal et al.
Fig. 9. Patient 1 necropsy, showing increase of hyaline amorphous substance in the testis interstitia
(arrowheads). Hematoxylin and eosin. x 1000.
Fig. 10. Patient 1necropsy, showing optic nerve. a:normal histology of the nerve (open arrow) Hematoxylin and eosin. x 250. b: Optic nerve (open arrow) surrounded by thickened dura (arrowheads).Hematoxylin and eosin. x 50.
When 20 years old (Fig. 12a,b)she complained of pain
in her eyes. She was found to have bilateral glaucoma
and keratoconus. When 25 years old she was 123 cm tall
and weighed 29,200 g; she had a gerodermic face, depressed nasal bridge, protruding lips, pseudoanodontia,
and micrognathia; pale, edematous, redundant, hairless
skin with the same cicatricial changes as her brother;
hyperextensibility of fingers and hyperconvexity of
nails, hypoplastic breasts at Tanner stage 111, and normal female external genitalia without axillary or pubic
hair; her liver and spleen were both palpable 4 cm below
the costal margins.
Radiologic investigation. There was a diffused osteopenia (Fig. 13), hypoplasia of the maxilla, normal
G A P 0 Syndrome: A Connective Tissue Disorder
219
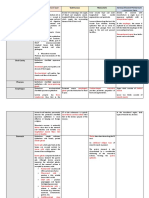
Fig. 11. Patient 1,necropsy of skin. a: Severe atrophy of epidermis (arrow) and cutaneous adnexa with
storage of amorphous material. Hematoxlyin and eosin. x 40. b: Sebaceous glands and hair follicles
partially replaced by fibrous material (arrowheads).Hematoxylin and eosin. x 100.c: Hair follicle completely replaced by fibrous and hyaline material (open arrow). Hematoxylin and eosin. x 100. d Fibrillar
and amorphous material present in reticular dermis. Hematoxylin and eosin. x 250.
mandible and sella turcica (Fig. 141, square vertebral
bodies with a n anterior concavity (Fig. 15), short iliac
bones, deformed femoral head and neck, bilateral coxa
vara, and wide ribs and clavicles. Computerized tomography of the cranium disclosed hypodense areas in the
brain and a normal ventricular system.
Skin biopsy. Skin biopsies were done at age 19
years and 27 years. The first showed a preserved epidermis with storage of a n amorphous and hyaline material in the papillary dermis; this material surrounded
the hair follicles which were atrophic. Sweat glands
were preserved. The second biopsy, 8 years later, showed
severe atrophy in the epidermis, with increase of the
hyaline material, and hair follicle atrophy. Many follicles were totally replaced by fibrous material. Resorcinfuchsin staining disclosed elastic fibers only a t the
deeper reticular dermis. They were absent where the
amorphous material was stored.
Dermatoglyphics
Digits: left hand: WD (lo), A", A", LR(61, L" (4);right
hand: L" (6), As, L" (3), L" (61, L" (4).Mainline formula:
220
Wajntal et al.
Fig. 12. Patient 2 when 20 years old. a:Frontal view. (Reproduced from Reire-Maia and Pinheiro, 1984,
with permission of the publisher.) b: Lateral view.
hand: 9.9.5"-4.13
.t '-A.0.0.
L.V., right hand:
9.9.-9.5".5'.13.t-t'-LU.O.O.L.L.
There was a n incomplete
left
simian crease on both hands.
Fig. 13. Long bone roentgenograms of patient 2.
Additional tests (patients 1 and2). Results of routine hematologic and urine tests, total protein level, and
protein electrophoresis were normal, except for prothrombin time that was reduced to 66% in patient 1 and
60% in patient 2, and corrected by vitamin K in both
patients. Acid mucopolysaccharide levels were normal
in urine and blood. Buhot cells were absent in bone
marrow and there was no vacuolization in leukocytes.
Patient 1 had oligoasthenospermia with 30,000,000
spermatozoa in a total volume of 1 ml of ejaculate and
50% of dead spermatozoa one hour after ejaculation.
Basal thyroid hormone levels were normal as was the
function of the adenohypophysis (Table I). Patient 1had
a discrete primary gonadal lesion suggested by oligoasthenospermia and slight elevation of basal folliclestimulating hormone (FSH)levels with conserved function of Leydig cells (basal testosterone = 368 ng/dl and
397 ngidl; after stimulation with hCG = 1,228ngidl).
Patient 2 had high levels of gonadotropin. Chromosomes
were normal in both patients. Electron microscopic
studies of collagen from cultured fibroblasts of patient 2
did not show any collagen abnormalities.
GAPO Syndrome: A Connective Tissue Disorder
221
Fig. 14. Skull roentgenogram of patient 2.
Fig. 15. Square vertebral bodies with anterior concavities observed
on patient 2 roentgenogram.
DISCUSSION
Our patients have manifestations of the GAPO syndrome (except for absence of optic atrophy), presence of
bilateral keratoconus, and signs of hypogonadism. Optic
atrophy is not a constant manifestation, as 6 of the 12
reported patients did not have this manifestation. In 2
instances a n apparent thickening of the optic nerve was
evident by CT scan of the 3 brothers studied by Gag-
liardi et al. [19841. In the present case autopsy studies
showed the optic nerve surrounded by a thickened dura
mater. We interpret the reduced number of retinal ganglion cells found in patient 1 as secondary to physical
compression of the nerve. It is possible that the optic
atrophy found in 50% of the patients may be as well
secondary to nerve constriction.
Hormonal evaluation showed normal pituitary reserve, but both patients had altered gonadal function. In
patient 1,there was oligospermia and a n increased response of luteinizing hormone (LH) and FSH after luteinizing hormone-releasing hormone (LH-RH) stimulation, and in patient 2 a primary gonadal lesion was
characterized by menopause gonadotropin levels. Those
alterations are probably secondary to the extracellular
matrix accumulation in the gonads, leading to hypogonadism and gonadal failure. Besides our patients, the
only 2 other postpubertal patients described also had
evidence of hypogonadism: the patient described by
Silva [ 19841had amenorrhea and hypoplasia of breasts,
labia major,, and clitoris, and the patient of Andersen
and Pindborg [1947] had irregular menses which began
a t 18 years [Tipton and Gorlin, 19841. Thus, the hypogonadism found in our patients is probably a common
manifestation in adults with GAPO syndrome.
Only one other autopsy has been reported. The patient
studied by Andersen and Pindborg [19471 as reported by
Tipton and Gorlin [19841 died a t age 39 years and autopsy showed polycystic kidneys and nephrocalcinosis;
interstitial fibrosis of spleen, liver, kidneys, pericardium, myocardium, pancreas, adrenals, and ovaries;
and atherosclerotic changes in arteries of spleen, liver,
lungs, kidneys, and brain.
In our patient, kidneys were not abnormal, but atherosclerotic changes were present and there was collagen and ground substance deposition in skin, on the
222
Wajntal et al.
TABLE I Results of Functional Studies of t h e Adenohypophysis
Patient 1
Patient 2
Normal basal values
Blood glucose
(mgidl)
-~
B
P
~
~~
94
62
60-100
Cortisol
(kgidl)
GH
(ngiml)
__
B
P
~
~~
34
32
19
34
5-25
27
69
20-40
1,5
2,8
0-5
25
25
>7
PRL
(ngiml)
B
P
-
34
53
5,25
167
84
LH
FSH
TSH
(mIUiml)
B
P
~-
mIUiml)
B
P
( FIUiml)
~~
116
6,3
5-20
921
99
200
6,8
42
4,4
0-7
18
8,7
8-25
135
20
5-20
Abbreviations B basal value FSH follicle stimulating hormone G H , growth hormone, LH luteinizing hormone P peak value dftel stimulation PRL
prolactin TSH thyroid-stimulating hormone
P - After intravenous infusion with insulin tO 1-0 2 U kgl thyrotropin releasing hormone (200 pgl and luteinuing hormone-releaqing hormone I100 pgi
surface and interstitium of all the examined organs, and
in all serosal membranes.
All of the manifestations present in the GAPO syndrome can be explained by a n excess of extracellular
connective tissue matrix that accumulates during life
and interferes with the normal function of tissues and
organs. This can be inferred from the fact that some of
the patients described were normal a t birth, as was our
patient 2, and progressive deterioration was observed.
Thus, in patient 2 scalp hair started to disappear when
she was 2 years old and her skin biopsies, as well a s those
of her brother, show the gradual disappearance of the
skin adnexa with accumulation of the extracellular matrix components. Autopsy data of patient 1also showed
gross alterations of the skin with substitution of the
parenchymatous elements by extracellular elements.
The increase in extracellular components can be due
to different mechanisms causing either 1)overproduction or 2) decreased breakdown of one or more of the
components.
All overproduction mechanisms will be due to dominant mutations: any mutation that modifies a structural gene in such a way that its product is no longer
recognized by the normal enzymes involved with its
breakdown must be dominant. A constitutive mutation
of a structural gene, increased stability of the messenger RNA or a modified repressor, or increased amount of
an activator should also be dominantly inherited.
Should the basic alteration be related to overproduction
of any one of the components, a feedback mechanism
must be postulated to account for the increased amount
of the remaining material.
Decreased breakdown mechanisms can be due to any
mutation causing a decreased activity of any one of the
enzymes related to normal breakdown of the extracellular components and would be recessive as in other inherited errors of metabolism. The GAPO syndrome is inherited as a n autosomal recessive mutation, as implied by
the observed consanguinity and normal phenotype of
obligate heterozygotes, even though skin biopsies have
not been performed on the heterozygotes. Thus, the mutation present in GAPO syndrome seems to be related to
a n abnormal breakdown of the extracellular components rather than to their overproduction.
Alteration in enzymes that are related to normal
breakdown of extracellular components has been described. There is hyperactive collagenase in epidermolysis bullosa dystrophica, Hallopeau-Siemens type
[McK 22660, McKusick, 1988; Bauer, 19771. To our
knowledge, a hypoactive collagenase has not been described. Hyaluronidase is present in body fluids and
certainly plays a n important role in turnover of hyaluronic acid and derivatives. The elastases are powerful proteases that can hydrolyze numerous proteins and
might be responsible for the turnover of some of the
extracellular components. Further studies will be necessary to disclose the basic pathways involved in this
pathogenetic mechanism, but at this time, we think that
one of the enzymes involved in the breakdown of the
extracellular components is responsible for the manifestations in the GAPO syndrome.
The histologic data presented here on GAPO syndrome show that this condition should be reclassified as
GAPO dysplasia.
ACKNOWLEDGMENTS
We thank Dr. Consuelo Junqueira for specific collagen
staining studies. Our thanks to Miss Luceleni da Silva
for secretarial assistance. Our special thanks to the Scientific Documentation Department of the Faculty of
Medicine, University of Sao Paulo.
This work was partially supported by the Conselho
Nacional de Desenvolvimento Cientifico e Tecnologico
(CNPq), Brazil.
REFERENCES
Andersen TH, Pindborg JJ (1947): Et tilfaelde at total pseudoanodonti i forbindelse med kranie deformitet, dvaergvaekst og ektodermal dysplasi. Odontol Tilster 55:484-493.
Bauer EA (1977): Recessive dystrophic epidermolysisbullosa: Evidence
for an altered collagenase in fibroblast cultures. Proc Natl Acad Sci
USA 74:4646-4650.
Epps DR, Mendonqa BB, Olazabal LC, Billerbeck AEC, Wajntal A
(1977): Poiquiloderma conghito familiar (S. de RothmundThompson). Cienc Cult 29(Suppl):740.
Freire-Maia N, Pinheiro M (1984):Ectodermal Dysplasias-A Clinical and Genetic Study. New York: Alan R. Liss, pp 98-100.
Fuks A, Resenman A, Chosack A (1978): Pseudoanodontia, cranial
deformity, blindness, alopecia and dwarfism: A new syndrome. J
Dent Child 45:155-157.
Gagliardi ART, Gonzalez CH, Pratesi R (1984): GAPO syndrome: Report of three affected brothers. Am J Med Genet 19217-223.
Gorlin RJ, Tipton RE, Langer LO J r (1978):Pseudoanodontia, growth
retardation and alopecia: A syndrome. Paper presented at Annual
Meeting of American Academy of Oral Pathology, Fort Lauderdale,
FL, 26 April 1978.
Manouvrier-Hanu S, Largilliere C, Benalioua M, Farriaux JP, Fontaine G (1987): Brief clinical report: The GAPO syndrome. Am J
Med Genet 26:683-688.
McKusick VA (1988): Mendelian Inheritance in Man. Catalogs of
Autosomal Dominant, Autosomal Recessive and X-Linked Phe-
GAPO Syndrome: A Connective Tissue Disorder
notypes. 8th ed. Baltimore: The Johns Hopkins University Press,
pp 951.
Shapira Y, Yatziv S, Deckelbaum R (1982): Growth retardation,
alopecia, pseudoanodontia and optic atrophy. Synd Ident, case report 85, VIIk14-16.
Silva EO (1984): Dwarfism, alopecia, pseudoanodontia and other
anomalies: Report of a case. Rev Bras Genet 7:743-747.
223
Tipton RE, Gorlin R J (1984): Growth retardation, alopecia, pseudoanodontia, and optic atrophy-the GAPO syndrome. Am J Med Genet
19:209-216
Wajntal A, E P P ~DR, M e n d o w BB, Billerbeck AEC (1982): Nova
Sindrome de displasia ectodermica: Nanismo, alopecia, anodontia e
laxa. Cienc
34(supp1):705
Você também pode gostar
- Nursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFDocumento7 páginasNursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFNyeweh Sia Yomba67% (15)
- MedTech Recall NotesDocumento27 páginasMedTech Recall NotesIsniharah Pangandaman100% (2)
- GI Tract Histology SummaryDocumento5 páginasGI Tract Histology SummaryFluffy_iceAinda não há avaliações
- Sammito1988Documento7 páginasSammito1988Aling AyenAinda não há avaliações
- Osteopathia Striata With Cranial SclerosisDocumento5 páginasOsteopathia Striata With Cranial SclerosisritvikAinda não há avaliações
- Dyscephalia Mandibulo-Oculo-FacialisDocumento5 páginasDyscephalia Mandibulo-Oculo-FacialisReyes Ivan García CuevasAinda não há avaliações
- Mca/Mr: New Syndrome?Documento3 páginasMca/Mr: New Syndrome?JoAinda não há avaliações
- Al Ghamdi1997Documento5 páginasAl Ghamdi1997JohnnyAinda não há avaliações
- Letter To The Editor: Midline Field Defects and Hirschsprung DiseaseDocumento2 páginasLetter To The Editor: Midline Field Defects and Hirschsprung DiseaseAraAinda não há avaliações
- Brief Clinical Report: The Floating Harbor Syndrome With Cardiac Septa1 DefectDocumento3 páginasBrief Clinical Report: The Floating Harbor Syndrome With Cardiac Septa1 DefectSarly FebrianaAinda não há avaliações
- Loss of The N-Myc Oncogene in A Patient With A Small Interstitial Deletion of The Short Arm of ChromosomeDocumento5 páginasLoss of The N-Myc Oncogene in A Patient With A Small Interstitial Deletion of The Short Arm of ChromosomeantonioopAinda não há avaliações
- Smith 1999Documento8 páginasSmith 1999smithl25Ainda não há avaliações
- Aphallia Associate Fistula RectouretraDocumento3 páginasAphallia Associate Fistula Rectouretraeni nadzhifahAinda não há avaliações
- Apparently New Syndrome of Congenital Cataracts, Sensorineural Deafness, Down Syndrome-Like Facial Appearance, Short Stature, and Mental RetardationDocumento5 páginasApparently New Syndrome of Congenital Cataracts, Sensorineural Deafness, Down Syndrome-Like Facial Appearance, Short Stature, and Mental Retardationjahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Confirmation of The Catania Brachydactylous Type of Acrofacial DysostosisDocumento4 páginasConfirmation of The Catania Brachydactylous Type of Acrofacial DysostosisSergioFernandezAinda não há avaliações
- Reish 1996Documento5 páginasReish 1996jahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Somorin SsDocumento8 páginasSomorin SsChikezie OnwukweAinda não há avaliações
- Himmelhoch 09 03Documento4 páginasHimmelhoch 09 03andreAinda não há avaliações
- Cherubism Combined With EpilepsyDocumento7 páginasCherubism Combined With EpilepsywwhhjAinda não há avaliações
- HSS Clinical Pronostic ConsiderationDocumento4 páginasHSS Clinical Pronostic ConsiderationReyes Ivan García CuevasAinda não há avaliações
- Plomp 1998Documento7 páginasPlomp 1998dad dzd adaAinda não há avaliações
- Ben-Bassat, Casper, Kaplan Laron, Petah-Tikva, Israel: MacrodactylyDocumento6 páginasBen-Bassat, Casper, Kaplan Laron, Petah-Tikva, Israel: MacrodactylyYuni Kurnia PrajawatiAinda não há avaliações
- Sindrom PatauDocumento12 páginasSindrom PatauIoana PaulaAinda não há avaliações
- Magini 2012Documento5 páginasMagini 2012rossibAinda não há avaliações
- 1 s2.0 S2213576621002852 MainDocumento6 páginas1 s2.0 S2213576621002852 Mainafri pakalessyAinda não há avaliações
- (Sici) 1096 8628 (19981228) 80:5 454::aid Ajmg4 3.0.co 2 o PDFDocumento5 páginas(Sici) 1096 8628 (19981228) 80:5 454::aid Ajmg4 3.0.co 2 o PDFJaymel MaigueAinda não há avaliações
- Terminal Deletion of The Long Arm Chromosome (46,, De1 (3) (427 Qter) LDocumento4 páginasTerminal Deletion of The Long Arm Chromosome (46,, De1 (3) (427 Qter) LantonioopAinda não há avaliações
- Labrune 1997Documento6 páginasLabrune 1997dad dzd adaAinda não há avaliações
- Le Mire 2004Documento2 páginasLe Mire 2004Fapuw ParawansaAinda não há avaliações
- AMS PublishedDocumento4 páginasAMS PublishedAyanawAinda não há avaliações
- Wieczorek 2003Documento5 páginasWieczorek 2003ladybieibiAinda não há avaliações
- Cla Eys 1997Documento6 páginasCla Eys 1997jahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Ichthyosis-Characteristic: Appearance-Mental Retardation Syndrome With Distinct Histological Skin AbnormalitiesDocumento4 páginasIchthyosis-Characteristic: Appearance-Mental Retardation Syndrome With Distinct Histological Skin AbnormalitiesJoAinda não há avaliações
- Phleboliths and The Vascular Maxillofacial LesionDocumento4 páginasPhleboliths and The Vascular Maxillofacial LesionVinay KumarAinda não há avaliações
- Gracile Bone Dysplasia (American Journal of Medical Genetics, Vol. 75, Issue 1) (1998)Documento6 páginasGracile Bone Dysplasia (American Journal of Medical Genetics, Vol. 75, Issue 1) (1998)mgAinda não há avaliações
- 631-Article Text-2378-1-10-20180830Documento6 páginas631-Article Text-2378-1-10-20180830azizhamoudAinda não há avaliações
- Ijcpd 05 203Documento5 páginasIjcpd 05 203yanyangAinda não há avaliações
- Enf Heck Caso Imagen de HistoloDocumento3 páginasEnf Heck Caso Imagen de Histolocarmen espinozaAinda não há avaliações
- Sorge 1996Documento4 páginasSorge 1996jahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Saethre-Chotzen Syndrome, Pro136His TWIST Mutation, Hearing Loss, and External and Middle Ear Structural Anomalies: Report On A Brazilian FamilyDocumento5 páginasSaethre-Chotzen Syndrome, Pro136His TWIST Mutation, Hearing Loss, and External and Middle Ear Structural Anomalies: Report On A Brazilian FamilyLeti MouraAinda não há avaliações
- Teebi 1996Documento4 páginasTeebi 1996JohnnyAinda não há avaliações
- Rheumatology Case Report Hand Abnormalities FeatDocumento1 páginaRheumatology Case Report Hand Abnormalities FeatAlberto Sifuentes GiraldoAinda não há avaliações
- Archdisch01563 0108Documento6 páginasArchdisch01563 0108jharmandoAinda não há avaliações
- Complete Trisomy 17p Syndrome in A Girl With Der (14) T (14 17) (p11.2 p11.2)Documento8 páginasComplete Trisomy 17p Syndrome in A Girl With Der (14) T (14 17) (p11.2 p11.2)AldunIdhunAinda não há avaliações
- Anancephaly 2Documento3 páginasAnancephaly 2Metta SariAinda não há avaliações
- Treatment of Prepubertal Periodontitis: Case ReportDocumento7 páginasTreatment of Prepubertal Periodontitis: Case ReportRut ViodettaAinda não há avaliações
- 121-Article Text-369-3-10-20160627Documento4 páginas121-Article Text-369-3-10-20160627rosangelaAinda não há avaliações
- Chondro-Osseous Respiratory Epithelial Adenomatoid Hamartomas in 3 DogsDocumento4 páginasChondro-Osseous Respiratory Epithelial Adenomatoid Hamartomas in 3 DogsfisheirAinda não há avaliações
- JURNALDocumento4 páginasJURNALrahastuti drgAinda não há avaliações
- Marby SXDocumento7 páginasMarby SXSantiago Basto CruzAinda não há avaliações
- Ijcmr 3499Documento4 páginasIjcmr 3499AlfirahmatikaAinda não há avaliações
- Histoid Hansens - The Current PerspectiveDocumento6 páginasHistoid Hansens - The Current PerspectiveIOSRjournalAinda não há avaliações
- Proteus SyndromeDocumento6 páginasProteus SyndromeAnshul JainAinda não há avaliações
- International Journal of Pediatric OtorhinolaryngologyDocumento5 páginasInternational Journal of Pediatric OtorhinolaryngologyAmmy ContrerasAinda não há avaliações
- Gorlins SyndromeDocumento6 páginasGorlins SyndromeAnupama NagrajAinda não há avaliações
- SAMS: Provisionally Unique Multiple CongenitalDocumento5 páginasSAMS: Provisionally Unique Multiple Congenitaljahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Three-Generation Family With Resemblance To Townes-Brocks Syndrome and Goldenhar/Oculoauriculovertebral SpectrumDocumento6 páginasThree-Generation Family With Resemblance To Townes-Brocks Syndrome and Goldenhar/Oculoauriculovertebral SpectrumAndjela RoganovicAinda não há avaliações
- Autosomal Dominant Microcephaly With Normal Intelligence, Short Palpebral Fissures, and Digital AnomaliesDocumento6 páginasAutosomal Dominant Microcephaly With Normal Intelligence, Short Palpebral Fissures, and Digital Anomaliesjahfdfgsdjad asdhsajhajdkAinda não há avaliações
- Ajmg A 36442Documento4 páginasAjmg A 36442Narjes Sharif AskariAinda não há avaliações
- Multiple Bilateral Taurodontism. A Case ReportDocumento3 páginasMultiple Bilateral Taurodontism. A Case ReportJing XueAinda não há avaliações
- Bahan Pagets Disease of MaxillaDocumento3 páginasBahan Pagets Disease of MaxillayuniAinda não há avaliações
- Diagnosis and Treatment of Vestibular DisordersNo EverandDiagnosis and Treatment of Vestibular DisordersSeilesh BabuAinda não há avaliações
- Accept-Hastal Hasili PDFDocumento1 páginaAccept-Hastal Hasili PDFAttar RahaAinda não há avaliações
- PhysicsElectromagnetismAH tcm4-726384Documento51 páginasPhysicsElectromagnetismAH tcm4-726384Attar RahaAinda não há avaliações
- Teaching Philosophy of Science To Scientists: Why, What and HowDocumento23 páginasTeaching Philosophy of Science To Scientists: Why, What and HowAttar RahaAinda não há avaliações
- (Page 16-30) Teaching Strategies For Promoting Higher Order Thinking Skills - No 2 PDFDocumento15 páginas(Page 16-30) Teaching Strategies For Promoting Higher Order Thinking Skills - No 2 PDFAttar RahaAinda não há avaliações
- Jurnal Mi 01Documento14 páginasJurnal Mi 01Attar RahaAinda não há avaliações
- Ipi22162 PDFDocumento6 páginasIpi22162 PDFAttar RahaAinda não há avaliações
- Jurnal Utama ImaDocumento20 páginasJurnal Utama ImaAttar RahaAinda não há avaliações
- Datarc eDocumento5 páginasDatarc eAttar RahaAinda não há avaliações
- Wardani 2017 J. Phys.: Conf. Ser. 895 012152Documento7 páginasWardani 2017 J. Phys.: Conf. Ser. 895 012152Attar RahaAinda não há avaliações
- Fhsstphy PDFDocumento397 páginasFhsstphy PDFAttar RahaAinda não há avaliações
- Intro Physics 1 ReviewDocumento608 páginasIntro Physics 1 ReviewImran RashidAinda não há avaliações
- 13 OCTOBER, 2021 Wednesday Biology Transport SystemDocumento12 páginas13 OCTOBER, 2021 Wednesday Biology Transport SystemOyasor Ikhapo AnthonyAinda não há avaliações
- Integumentary System: Skin and Accessory Structures Hair NailsDocumento117 páginasIntegumentary System: Skin and Accessory Structures Hair NailsSunita RaniAinda não há avaliações
- 5043 14437 1 PB PDFDocumento9 páginas5043 14437 1 PB PDFvivi hutabaratAinda não há avaliações
- Todentj 9 250 PDFDocumento7 páginasTodentj 9 250 PDFRSU DUTA MULYAAinda não há avaliações
- Cavity Preparation in Deciduous Teeth: Sum M AryDocumento8 páginasCavity Preparation in Deciduous Teeth: Sum M AryNabilla FaralizaAinda não há avaliações
- Erickson Kurol (CT Study)Documento9 páginasErickson Kurol (CT Study)Srishti SyalAinda não há avaliações
- Final Case Study (Hernia)Documento52 páginasFinal Case Study (Hernia)Kingfer Garcia Ignacio II63% (16)
- Brain Understanding Interpretation of CT and MriDocumento67 páginasBrain Understanding Interpretation of CT and MriStefan StefAinda não há avaliações
- Tissues of The Human BodyDocumento39 páginasTissues of The Human BodyCarmen MaldonadoAinda não há avaliações
- 72 HR ReviewerDocumento8 páginas72 HR ReviewerAstrid AmadorAinda não há avaliações
- Chugh2010 Brodie PDFDocumento7 páginasChugh2010 Brodie PDFLudy Jiménez ValdiviaAinda não há avaliações
- 00004Documento8 páginas00004api-3710948Ainda não há avaliações
- Life Science Class X V2Documento159 páginasLife Science Class X V2Surya Narayan DasAinda não há avaliações
- Softcopy For Teachers PDFDocumento199 páginasSoftcopy For Teachers PDFMithalina AfiqahAinda não há avaliações
- Blood Transfusion NotesDocumento1 páginaBlood Transfusion NotesShreyas WalvekarAinda não há avaliações
- Bisecting and Parelling TechniqueDocumento32 páginasBisecting and Parelling TechniqueArka Saha100% (1)
- Section - 026 - Immediate DenturesDocumento12 páginasSection - 026 - Immediate DenturesMuli Maroshi100% (1)
- The EyesDocumento9 páginasThe EyesEmmanuel JohnsonAinda não há avaliações
- Prevalence of Third Molar Impaction in Patient With Mandibular Anterior Teeth CrowdingDocumento5 páginasPrevalence of Third Molar Impaction in Patient With Mandibular Anterior Teeth CrowdingArina Al-KhaqAinda não há avaliações
- A Clinical Case Report/ Oral Diagnosis On Lichenoid ReactionDocumento7 páginasA Clinical Case Report/ Oral Diagnosis On Lichenoid ReactionJu WenAinda não há avaliações
- Excretory System (Excercise)Documento17 páginasExcretory System (Excercise)Shadab HanafiAinda não há avaliações
- Meninges: Consist of Three LayersDocumento23 páginasMeninges: Consist of Three LayersShantu ShirurmathAinda não há avaliações
- Arteries, Vein, Nerve... LarynxDocumento3 páginasArteries, Vein, Nerve... LarynxShafiqah AbdullahAinda não há avaliações
- Breast and Development of UGDocumento8 páginasBreast and Development of UGkamie155Ainda não há avaliações
- Reflection Paper Phy108Documento8 páginasReflection Paper Phy108VshamVijayAinda não há avaliações
- Tooth Origin and Formation - by Bugnariu Paul, Buterchi Codrut, Chit-Stinean AdonisDocumento73 páginasTooth Origin and Formation - by Bugnariu Paul, Buterchi Codrut, Chit-Stinean AdonisVlad FlaviusAinda não há avaliações
- Guided Notes Respiratory SystemDocumento3 páginasGuided Notes Respiratory Systemapi-280337641Ainda não há avaliações