Escolar Documentos
Profissional Documentos
Cultura Documentos
tmp9B90 TMP
Enviado por
FrontiersTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
tmp9B90 TMP
Enviado por
FrontiersDireitos autorais:
Formatos disponíveis
International Journal of Scientific Reports
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
http://www.sci-rep.com
pISSN 2454-2156 | eISSN 2454-2164
DOI: http://dx.doi.org/10.18203/issn.2454-2156.IntJSciRep20163397
Original Research Article
Factors influencing atherogenic indices in type 2 diabetic
women in northwestern Algeria
Mustapha Diaf*, Boumediene Mghit Khaled
Department of Biology, Faculty of Natural and Life Sciences, Djillali Liabes University, Sidi-bel-Abbes, Algeria
Received: 30 July 2016
Accepted: 31 August 2016
*Correspondence:
Dr. Mustapha Diaf
E-mail: diafmustapha@gmail.com
Copyright: the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Type 2 diabetic women are at higher risk of developing atherogenic dyslipidemia. The major possible
risk factors are obesity, abdominal fat accumulation and poor glycaemic control. However, menopause-related
changes could be another determinant. The aim of this study was to evaluate the interrelationships of these risk factors
and their independent effects on atherogenic indices in type 2 diabetes women.
Methods: A prospective, cross-sectional study, which includes 160 women agreed to participate in this study.
Anthropometrics, biochemical parameters and blood pressure were measured. Atherogenic indices - total cholesterolto-high-density lipoprotein cholesterol ratio (TC/HDL) and apolipoprotein (apo) B-to-apo A1 ratio, were calculated.
Individual risk factors were examined in relationship to these atherogenic indices using correlation tests and logistic
regression.
Results: 23.12% of the participants were normal weight and 76.87% were overweight/obese. The overall mean age
was 57.7011.16 years. Diabetes duration (5years), anthropometric parameters, poor glycaemic control, high apo B
and high level of low-density lipoprotein (LDL) were found to be significant determinants of atherogenic indices
changes. The TC/HDL ratio was weakly associated with both BMI and waist circumference. However, the apo B/apo
A1 ratio provided positive correlations with anthropometric parameters, especially with waist circumference
(p=0.185, r=0.108, r2=0.012), and this, in both pre and post-menopausal type 2 diabetic women.
Conclusions: The atherogenic risk, estimated by TC/HDL and apo B/apo A1 ratios, becomes more severe with higher
anthropometric parameters (BMI and waist circumference), diabetes duration and poor glycaemic control in type 2
diabetes women and this during both premenopausal and postmenopausal periods.
Keywords: Type 2 diabetes, Atherogenic indices, Risk factors, Women, Anthropometric parameters
INTRODUCTION
Type 2 diabetes (T2D) has now become a global public
health burden affecting all strata of societies in both
developed and developing countries, it is a well-known
risk factor in the incidence of cardiovascular disease
(CVD) and atherogenic dyslipidemia.1 The atherogenic
dyslipidemia, a common metabolic disorder, is
characterized by elevated very low density lipoprotein
(VLDL), small dense low density lipoprotein (LDL) and
low high density lipoprotein (HDL) levels, which
constitute the lipid triad and are considered as traditional
risk factors for cardiovascular events.2 Recently,
lipoproteins and apolipoproteins (apo) ratios have also
been found as consistent predictors of atherogenic risk
than lipids alone.3 Therefore, the mosaic of modifiable
CVD risk issues imply some physiological factors which
include the untreated hypertension and high toal
cholesterol level, as well as the increased prevalence of
sedentary, the overall and/or abdominal obesity and
insulin-resistant, these latter may also vary according to
ethnicity, age and gender.3,4
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 258
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
In women, comparing to men, manifest symptoms of
CVD are generally delayed by approximately 10 to 15
years.5 Scientists suggest that women benefit from the
protective effects of ovarian hormones during the
premenopausal period, however, men are more likely to
be engaged in health-damaging behaviours.6
Biochemical, structural and physiological changes are
due to the decreased in oestrogen levels during and after
menopause, which alter the general health status of the
woman. Oestrogen is known as an anti-atherogenic that
could protect females against coronary artery disease
during the premenopausal period. The post-menopausal
women have less cardiovascular friendly lipid profiles
than premenopausal ones.7
Hence, the aim of the present study was to assess the
powerful factors that may influence on atherogenic
indices (total cholesterol/HDL and apo B/apo A1) in type
2 diabetic women. We investigated the correlations
between anthropometric parameters and atherogenic
indices during both pre- and post-menopausal states.
METHODS
is tightened around the patients abdomen, above the line
passing through the navel, without depressing the skin.
Blood pressure measurement
The morning blood pressure was evaluated using
OMRON M3 Digital Automatic Blood Pressure Monitor
(Omron Healthcare., Ltd. Kyoto, Japan), this
sphygmomanometer can determine systolic blood
pressures between 3-24 cm Hg, diastolic 1-21 cm Hg and
heart rate 40-200 beats per minute.
Laboratory data
Fasting blood samples (12 h after an overnight fast) were
collected under aseptic conditions by venopuncture from
the antecubital vein, into sterile plain tubes. The serum
was used for the analysis of fasting glycaemia, total
cholesterol (TC), HDL, LDL and triglycerides (TG) using
the enzymatic colorimetric methods (Spinreact Reagents,
Spain). Apo A1 and Apo B were quantified by
turbidimetric tests (Spinreact Reagents, Spain). However,
the glycosylated haemoglobin (HbA1c) concentration
value was determined on fasting plasma samples using an
ion exchange resin separation method.
Patients data
Statistical analysis
One hundred sixty adult female subject with confirmed
T2D for at least six months were recruited from April to
September 2015, at the level of the Public Establishment
of Proximity Health in Sidi-Bel-Abbes city (Northwestern Algeria).
Informed consent was obtained from all participants and
ethical clearance was obtained from the relevant
authority. We randomly solicited all adult women who
met the inclusion criteria, that is, aged more than twenty,
having T2D duration of less than fifteen years and
exclusively under diet or oral anti-diabetic treatment, to
participate in the study. However, pregnant and
breastfeeding women as well as female patients with
primary hyperlipidaemia, hypothyroidism, a confirmed
cardiovascular disease, renal impairment or liver
dysfunction were excluded from our study. Likewise,
women using lipid-lowering drugs or who were treated
with insulin have also been excluded.
Anthropometric measurements were taken during
mornings according to the recommendations of the World
Health Organization (WHO).8 The electronic balance TS2003A:360 lb (capacity: 180 kg, graduations 0.1 kg) was
used for evaluating body weight (in kilograms) and the
Seca 206 body meter (measuring range 0-220 cm,
graduation length 1 mm) was employed for height
measurement. The body mass index (BMI) was
calculated as weight (kg)/height2 (m2).
The waist circumference was measured with a measuring
tape (maximum: 150 cm, graduation length: 1 mm) which
All data were processed and analysed through SPSS 23.0
(Statistical Package for the Social Sciences, IBM
Corporation; Chicago, IL. March 2015). Results are
expressed as meanstandard deviations, the independent
student t-test was used for comparing results between
groups according to the women corpulence.
Binary logistic regression was used in order to determine
the factors associated with atherogenic indices, results are
presented using odds ratios with a 95% confidence
interval (95% CI). A p-value lower than 0.05 was
considered statistically significant for all statistical tests.
Relationships between lipids, apolipoproteins ratios and
anthropometric parameters were studied using Pearson
correlation tests and simple linear regression tests with a
confidence interval of 95%.
RESULTS
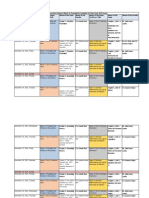
Table 1 displays the subjects characteristics. Amongst all
patients, 23.12% were normal weight and 76.87% were
either overweight or obese. The overall mean age was
57.7011.16 years (56.0014.20 years in normal weight
and 58.2411.57 years in overweight/obese), with no
significant differences between the two groups. However,
we noted a high significant difference of height and waist
circumference (p <0.01). No differences between the two
groups was observed with respect to age, diabetes
duration, blood pressure and all the studied conventional
biochemical parameters. Comparing TC/HDL and apo
B/apo A1 ratios between normal weight and overweight/
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 259
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
obese women, no significant differences were noted.
Nevertheless, an exception was found for TC/HDL ratio
during the pre-menopausal period (p =0.005). As
illustrated in Table 2, we investigated risk factors
associated with elevated TC/HDL ratio (3) levels.
The performed logistic regression analysis indicated that
the pathological atherogenic index (TC/HDL 3) was
significantly associated with diabetes duration (5 years),
overweight, poor glycaemic control (HbA1c 7%), and
high apo B and LDL levels.
Table 1: Characteristics of the studied cases.
Variables
All patients
160
N (%)
57.7011.16
Age (Years), MeansS.D
7.043.85
Duration of diabetes
(years), MeansS.D
Anthropometric characteristics, (MeansS.D)
73.8411.82
Weight (kg)
160.916.80
Height (cm)
97.7814.14
Waist circumference (cm)
28.494.43
BMI (kg/m2)
Overweight, obesity
duration (years)
Blood pressure, MeansS.D
Systolic pressure (mmHg)
12.901.48
Diastolic pressure (mmHg)
7.600.98
Menopausal status, n (%)
Pre-menopause
49 (30.6)
Oestrogen use (yes)
39 (24.35)
Oestrogen use (no)
10 (6.24)
Post-menopause
111 (69.4)
Menopausal age (years)
Pre-menopause
45.559.70
Post-menopause
63.066.66
Biochemical parameters (g/L)
1.530.61
Fasting glycaemia
2.260.96
Postprandial glycaemia
7.701.30
HbA1c
1.700.35
Fasting TC
0.400.11
Fasting HDL-c
1.070.32
Fasting LDL-c
1.500.76
Fasting TG
1.330.36
Apo A1
0.990.46
Apo B
4.521.47
TC/HDL-c
TC/HDL-c during pre4.381.62
menopause
TC/HDL-c during post4.591.40
menopause
0.770.35
Apo B/Apo A1
Apo B/Apo A1 during pre0.710.32
menopause
Apo B/Apo A1 during
0.790.36
post-menopause
Normal
weight
37 (23.12)
56.0014.20
6.273.79
Overweight/obese
123 (76.87)
58.2411.57
6.714.01
P value for Student ttest*
0.381
0.579
63.596.07
164.136.01
86.2010.37
23.561.20
-
69.687.39
159.607.36
95.939.93
27.101.38
9.316.25
<0.001
0.002
<0.001
<0.001
12.621.18
7.541.02
13.091.60
7.601.01
0.123
0.760
12 (7.5)
12 (7.5)
25 (15.6)
37 (23.1)
27 (16.85)
10 (6.25)
86 (53.8)
40.0012.52
63.686.41
47.357.99
62.886.76
0.021
0.604
1.470.54
2.330.92
7.961.39
1.720.31
0.390.13
1.160.29
1.440.82
1.260.27
0.920.32
4.892.00
1.580.65
2.260.93
7.641.29
1.660.36
0.400.11
1.040.33
1.450.72
1.380.40
1.000.52
4.421.27
0.419
0.696
0.255
0.466
0.695
0.092
0.922
0.150
0.418
0.101
5.622.25
3.831.05
0.005
4.491.77
4.611.32
0.761
0.750.29
0.780.36
0.691
0.810.41
0.640.28
0.168
0.710.21
0.790.39
0.380
*Comparison of means, between normal weight patients and overweight/obese ones. BMI: body mass index. HbA1c: glycosylated
haemoglobin. TC: total cholesterol. HDL-c: high density lipoprotein cholesterol. LDL-c: low density lipoprotein cholesterol. TG:
triglycerides. Apo: apolipoproteins.
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 260
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
Table 2: Crude odds ratio of risk factors associated with TC/HDL levels.
Risk factors
Age
<40 years
40-60 years
>60 years
Diabetes duration
< 5 years
5-10 years
10 years
BMI
<25 kg/m2
25-29.9 kg/m2
30 kg/m2
Waist circumference
80 cm
80 cm
Menopausal status
Pre-menopause
Post-menopause
HbA1c level
7% (53.01mmol/mol)
7% (53.01mmol/mol)
Apo B level (0.9 g/L)
Normal range
Below normal range
LDL-c level (0.8 g/L)
Normal range
Below normal range
Odd ratio
(95% CI OR)
TC/HDL-c < 3
TC/HDL-c 3
Number (%)
Number (%)
3 (1.9)
11 (6.9)
9 (5.6)
7 (4.4)
58 (36.2)
72 (45.0)
Reference
0.200 [0.017-2.303]
0.687 [0.147-3.215]
0.197
0.633
5 (3.1)
13 (8.1)
5 (3.1)
43 (26.9)
49 (30.6)
45 (28.1)
Reference
1.500 [0.304-7.409]
0.590 [0.159-2.193]
0.019
0.431
6 (3.8)
11 (6.9)
6 (3.8)
31 (19.4)
58 (36.2)
48 (30.0)
Reference
1.098 [0.118-10.226]
0.972 [0.264-3.578]
0.034
0.966
5 (3.1)
18 (11.2)
20 (12.5)
117 (73.1)
Reference
0.605 [0.071-5.144]
0.645
10 (6.2)
13 (8.1)
39 (24.4)
98 (61.2)
Reference
1.021 [0.201-4.969]
0.865
1 (0.6)
22 (13.8)
52 (32.5)
85 (53.1)
Reference
1.257 [0.155-10.978]
0.018
18 (11.2)
5 (3.1)
61 (38.1)
76 (47.5)
Reference
1.227 [1.067-1.770]
0.017
18 (11.2)
5 (3.1)
55 (34.4)
82 (51.2)
Reference
1.231 [1.071-1.746]
0.014
P*
*multivariate logistic regression significant at p=0.05. CI: confidence interval. OR: odd ratio. BMI: body mass index. TC: total
cholesterol. HbA1c: glycosylated haemoglobin. Apo B: apolipoproteine B. LDL-c: low-density lipoprotein cholesterol.
The odds ratios of having a high TC/HDL ratio were
1.098 [0.0118-10.226] and 1.000 [0.201-4.969] in
overweight and post-menopausal women, respectively.
Female subjects with poor glycaemic control (HbA1c
7%) were 1.257 [0.155-10.978] times more at risk of
having a higher atherogenic index (TC/HDL).
Our results about risk factors associated with high apo
B/apo A1 ratio (0.7) are summarised in Table 3. The
logistic regression analysis showed that higher apo B/apo
A1 ratios are associated with diabetes duration (5
years), abdominal obesity, poor glycaemic control
(HbA1c 7%), post-menopausal period and high LDL
levels. The odds ratios of having an apo B/apo A1 7 was
1.504 [0.528-4.284] in patients with more than five years
of diabetes, 1.976 [0.538-7.259] in those suffering from
abdominal obesity and 1.239 [0.364-4.219] in postmenopausal women.
As depicted in Figure 1, the TC/HDL ratio was weakly
associated with both BMI and waist circumference.
However, the apo B/apo A1 ratio provided positive
correlations with anthropometric parameters, especially
with waist circumference (p =0.185, r =0.108, r2 =0.012)
in both pre- and post-menopausal type 2 diabetic women.
DISCUSSION
The association between altered lipid profile and
atherosclerotic cardiovascular events is becoming more
accepted in postmenopausal women, despite that some
observed metabolic/physiological changes may occur as
results of aging.9,10 However, menopause tends to be
associated with an increased risk of general obesity,
abdominal fat distribution and associated health risk
factors.11
In the present study, we aimed to assess factors
influencing atherogenic indices in T2D women, during
premenopausal and postmenopausal periods. Furthermore, to investigate correlations between overall obesity
(estimated by BMI), abdominal fat accumulation
(estimated by waist circumference) and atherogenic
indices (TC/HDL and apo B/apo A1).
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 261
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
Table 3: Crude odds ratio of risk factors associated with Apo B/Apo A1 levels.
Risk factors
Age
<40 years
40-60 years
>60 years
Diabetes duration
< 5 years
5-10 years
10 years
BMI
<25 kg/m2
2
25-29.9 kg/m
2
30 kg/m
Waist circumference
80 cm
80 cm
Menopausal status
Pre-menopause
Post-menopause
HbA1c level
7% (53.01mmol/mol)
7% (53.01mmol/mol)
Apo B level (0.9 g/L)
Normal range
Below normal range
LDL-c level (0.8g/L)
Normal range
Below normal range
Odd ratio
(95% CI OR)
Apo B/Apo A1 < 0.7
Apo B/Apo A1 0.7
Number (%)
Number (%)
6 (3.8)
37 (23.1)
41 (25.6)
4 (2.5)
32 (20.0)
40 (25.0)
Reference
0.588 [0.080-4.327]
0.776 [0.271-2.227]
0.602
0.637
22 (13.8)
37 (23.1)
25 (15.6)
26 (16.2)
25 (15.6)
25 (15.6)
Reference
1.504 [0.528-4.284]
0.555 [0.215-1.430]
0.045
0.223
20 (12.5)
17 (10.6)
Reference
37 (23.1)
32 (20.0)
0.638 [0.184-2.215]
0.479
27 (16.9)
27 (16.9)
0.780 [0.315-1.931]
0.591
14 (8.8)
70 (43.8)
11 (6.9)
65 (40.6)
Reference
1.976 [0.538-7.259]
0.030
29 (18.1)
55 (34.4)
20 (12.5)
56 (35.0)
Reference
1.239 [0.364-4.219]
0.731
26 (16.2)
58 (36.2)
27 (16.9)
49 (30.6)
Reference
1.042 [0.469-2.315]
0.020
62 (38.8)
22 (13.8)
17 (10.6)
76 (47.5)
Reference
0.079 [0.034-0.183]
<0.001
46 (28.8)
38 (23.8)
27 (16.9)
49 (30.6)
Reference
1.327 [1.242-1.144]
0.015
P*
*multivariate logistic regression significant at p=0.05. CI: confidence interval. OR: odd ratio. BMI: body mass index. Apo A1:
apolipoproteine A1. HbA1c: glycosylated haemoglobin. Apo B: apolipoproteine B. LDL-c: low-density lipoprotein cholesterol.
Results from this study revealed higher levels of TC/HDL
and apo B/apo A1 in all female subjects, indicating that
all of our patients are prone to an increased
cardiovascular risk. Furthermore, when adapting our apo
B/apo A1 data with AMORIS and INTERHEART
thresholds, almost 36% of all participants were at high
myocardial infarction risk.12,13
In our female subjects, the TC/HDL ratio was
significantly influenced by overall obesity, poor
glycaemic control, apo B and LDL levels. According to
Stpie et al, in patients with T2D, the TC/HDL ratio is
considered as a cumulative marker of cardiovascular
risk.14 However, this ratio is not stable, it is modified by
several factors including BMI, food intake and the time
of blood sampling.15 Despite that the BMI is a good
indicator of body fat degree, it however does not capture
body fat distribution, which the waist circumference
dose. Intriguingly, the apo B/apo A1 ratio was more
likely to be associated with abdominal obesity, poor
glycaemic control and LDL level. According to many
studies, the apo B/apo A1 seems to be an effective
predictor of coronary heart disease risk in overweight and
obese individuals.12,13,16,17
The apolipoproteins are slightly influenced by meals and
biological variables, unlike the ordinary lipid parameters,
which fluctuate widely depending on food intake. 3
Therefore, measurement of apolipoproteins does not
require fasting blood samples, which represent a main
advantage.
In T2D patients, glycaemic control via the HbA1c is
considered as the backbone in the management of
diabetes.18 An increase of one percent in HbA1c level
above the accepted threshold of 7% is equivalent to a
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 262
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
change of about 30 mg/dl in mean plasma glucose. 19
Thus, the cardio-metabolic risk of our patients is
compounded by the problem of poor glycaemic control.
Regarding menopausal status, our results indicate that the
post-menopausal stage is associated with increased
atherogenic indices (TC/HDL and apo B/apo A1) without
however being significant.
During the transition from pre-menopause to menopause
and post-menopause, the central deposition of fat is
determined by specific genetic factors and leads to
metabolic correlated changes, including the risk of
cardiovascular diseases. The oestrogenic depletion after
menopause is associated with changes in body fat
distribution. As a result, a decrease in sex hormone
binding globulin is noted, and an increase of free
androgen level leads to higher androgenicity.20 Hormone
Replacement Therapy can prevent the central distribution
of fat, which explains the role of sex hormones.
The correlation tests through this investigation noticeably
showed, during both premenopausal and postmenopausal
periods, that the apo B/apo A1 ratio was marginally
related to the BMI (r2 =0.002, F =0.320, p =0573).
However, although not significant, the apo B/apo A1 was
positively correlated with waist circumference (r 2 =0.012,
F =1.770, p =0.185). On the other hand, the TC/HDL
ratio was faintly associated to anthropometric parameters
in both pre and post-menopausal women.
Figure 1: Association between TC/HDL-c and Apo B/Apo A1 ratios and body parameters according to the
menopausal status.
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 263
Diaf M et al. Int J Sci Rep. 2016 Oct;2(10):258-264
9.
CONCLUSION
The atherogenic risk, one of the CVD risk factors,
estimated by index ratios (TC/HDL and apo B/apo A1),
becomes more severe with higher anthropometric
parameters including BMI and more specifically the
waist circumference. However, the poor glycaemic
control depicts another parameter that could influence the
atherogenicity in T2D women and this during both
premenopausal and postmenopausal periods. As
apolipoproteins can be analysed in non-fasting samples, it
is of great practical advantage for patients and doctors to
use apo B/apo A1 ratio as an indicator of atherosclerosis.
It could be very helpful to use a single ratio for risk
prediction instead of referring to a larger number of lipid
ratios. The apo B/apo A1 ratio is more correlated to waist
circumference than BMI, this last depends upon the
individuals physical activity and lifestyle conditions.
Funding: No funding sources
Conflict of interest: None declared
Ethical approval: The study was approved by the
institutional ethics committee
10.
11.
12.
13.
14.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
Bener A, Zirie M, Daghash MH, Al-Hamaq AO,
Daradkeh G, Rikabi A. Lipids, lipoprotein (a)
profile and HbA1c among Arabian Type 2 diabetic
patients. Biomedical Research. 2007;18(2):97-102.
Habib SS. Cardiovascular disease in diabetes: An
enigma
of dyslipidemia,
thrombosis
and
inflammation. Basic Research Journal of Medicine
and Clinical Sciences. 2012;1(3):33-42.
Diaf M, Khaled BM, Sellam F. Impact of
corpulence parameters and haemoglobin A1c on
metabolic control in type 2 diabetic patients:
comparison of apolipoprotein B/A-I ratio with
fasting and postprandial conventional lipid ratios.
Libyan J Med. 2015;10:27400.
Snijder MB, Van Dam RM, Visser M, Seidell JC.
What aspects of body fat are particularly hazardous
and how do we measure them?. Int J Epidemiol.
2006;35(1):83-92.
Von Der Lohe E. Coronary heart disease in women.
Prevention. Diagnosis. Therapy. 1st ed. Berlin
Heidelberg: Springer-Verlag; 2003: 17-21.
Wingard DL, Suarez L, Barrett-Connor E. The sex
differential in mortality from all causes and
ischemic heart disease. Am J Epidemiol.
1983;117(2):165-72.
Nwagha UI, Ikekpeazu EJ, Ejezie FE, Neboh EE,
Maduka IC. Atherogenic index of plasma as useful
predictor
of
cardiovascular
risk
among
postmenopausal women in Enugu, Nigeria. Afr
Health Sci. 2010;10(3):248-52.
World Health Organization (WHO). The WHO
STEPwise approach to chronic disease risk factor
surveillance. Switzerland; Geneva: World Health
Organization; 2005.
15.
16.
17.
18.
19.
20.
Samanta B. Serum cholesterol in healthy
postmenopausal women. Indian J Med Sci.
1998;52(5):191-5.
Pasquali R, Casimirri F, Pascal G, Tortelli O,
Morselli Labate A, Bertazzo D, et al. Influence of
menopause on blood cholesterol levels in women:
the role of body composition, fat distribution and
hormonal milieu. Virgilio Menopause Health
Group. J Intern Med. 1997;241(3):195-203.
Lovejoy JC. The menopause and obesity. Prim
Care. 2003;30(2):317-25.
Walldius G, Jungner I, Holme I, Aastveit AH, Kolar
W, Steiner E. High apolipoprotein B, low
apolipoprotein A-I, and improvement in the
prediction of fatal myocardial infarction (AMORIS
study):
a
prospective
study.
Lancet.
2001;358(9298):2026-33.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A,
Lanas F, et al. Effect of potentially modifiable risk
factors associated with myocardial infarction in 52
countries (the INTERHEART study): case-control
study. Lancet. 2004;364(9438):937-52.
Stpie A, Stpie M, Wlaze RN, Paradowski M,
Banach M, Rysz J. Assessment of the relationship
between lipid parameters and obesity indices in nondiabetic obese patients: a preliminary report. Med
Sci Monit. 2014;20:2683-8.
Diaf M, Khaled MB, Sellam F. Correlation between
dietary fat intake and atherogenic indices in normal,
overweight and obese adults with or without type 2
diabetes. Romanian Journal of Diabetes Nutrition
and Metabolic Diseases. 2015;22(4):347-60.
Van Der Steeg WA, Boekholdt SM, Stein EA, ElHarchaoui K, Stroes ES, Sandhu MS, et al. Role of
the apolipoprotein B-apolipoprotein A-I ratio in
cardiovascular risk assessment: a case-control
analysis in EPIC-Norfolk. Ann Intern Med.
2007;146(9):640-8.
Dunder K, Lind L, Zethelius B, Berglund L, Lithell
H. Evaluation of a scoring scheme, including
proinsulin and the apolipoprotein B/apolipoprotein
A1 ratio, for the risk of acute coronary events in
middle-aged men: Uppsala Longitudinal Study of
Adult
Men
(ULSAM).
Am
Heart
J.
2004;148(4):596-601.
Rohlfing CL, Wiedmeyer HM, Little RR, England
JD, Tennill A, Goldstein DE. Defining the
relationship between plasma glucose and HbA(1c):
analysis of glucose profiles and HbA(1c) in the
Diabetes Control and Complications Trial. Diabetes
Care. 2002;25(2):275-8.
Elley CR, Kenealy T, Robinson E, Drury PL.
Glycated haemoglobin and cardiovascular outcomes
in people with Type 2 diabetes: a large prospective
cohort study. Diabet Med. 2008;25(11):1295-301.
Chang CJ, Wu CH, Yao WJ, Yang YC, Wu JS, Lu
FH. Relationships of age, menopause and central
obesity on cardiovascular disease risk factors in
Chinese women. Int J Obes Relat Metab Disord.
2000;24(12):1699-704.
Cite this article as: Diaf M, Khaled BM. Factors
influencing atherogenic indices in type 2 diabetic
women in northwestern Algeria. Int J Sci Rep
2016;2(10):258-64.
International Journal of Scientific Reports | October 2016 | Vol 2 | Issue 10 Page 264
Você também pode gostar
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionAinda não há avaliações
- ADA Scientific 2000Documento6 páginasADA Scientific 2000Rahmah Gadis Wartania PutriAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 18: PsychiatryNo EverandComplementary and Alternative Medical Lab Testing Part 18: PsychiatryNota: 5 de 5 estrelas5/5 (1)
- Prevalence of Hypertension Among Obese and Non-Obese Patients With Coronary Artery DiseaseDocumento4 páginasPrevalence of Hypertension Among Obese and Non-Obese Patients With Coronary Artery DiseasePrinceTumbuktooAinda não há avaliações
- Are The Associations of Plasma Leptin and Adiponectin With Type 2 Diabetes Independent of Obesity in Older Chinese Adults?Documento6 páginasAre The Associations of Plasma Leptin and Adiponectin With Type 2 Diabetes Independent of Obesity in Older Chinese Adults?bogdansoroAinda não há avaliações
- Analysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Documento9 páginasAnalysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Aleksa CopicAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsNo EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsAinda não há avaliações
- Jcem 2952Documento9 páginasJcem 2952parta anantamaAinda não há avaliações
- Duracion de La Obesidad PDFDocumento7 páginasDuracion de La Obesidad PDFGuillermo CalderaroAinda não há avaliações
- ,content, 31,2,361 FullDocumento2 páginas,content, 31,2,361 FullMilka MimingAinda não há avaliações
- Impact of Diet Composition On Blood GlucDocumento51 páginasImpact of Diet Composition On Blood GlucNarasimha Pavan BAinda não há avaliações
- NAFLDDocumento17 páginasNAFLDJirran CabatinganAinda não há avaliações
- 24 Obesity and Inflamation 2016-With-Cover-Page-V2Documento8 páginas24 Obesity and Inflamation 2016-With-Cover-Page-V2Uswatun HasanahAinda não há avaliações
- Plasma Lipids: Optimal Levels for HealthNo EverandPlasma Lipids: Optimal Levels for HealthAmerican Health FoundationAinda não há avaliações
- H Amruth Et AlDocumento6 páginasH Amruth Et AlInternational Journal of Clinical and Biomedical Research (IJCBR)Ainda não há avaliações
- 05 Iajps05062017Documento6 páginas05 Iajps05062017Baru Chandrasekhar RaoAinda não há avaliações
- Adua Et Al-2017-Clinical and Translational MedicineDocumento11 páginasAdua Et Al-2017-Clinical and Translational MedicineSam Asamoah SakyiAinda não há avaliações
- Pathophysiology of Obesity-Induced Health ComplicationsNo EverandPathophysiology of Obesity-Induced Health ComplicationsParamjit S. TappiaAinda não há avaliações
- Paper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsDocumento7 páginasPaper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsNike Dwi Putri LestariAinda não há avaliações
- PHD Thesis: University of Medicine and Pharmacy CraiovaDocumento10 páginasPHD Thesis: University of Medicine and Pharmacy CraiovapaulAinda não há avaliações
- 10 12 16 Journal Club ExampleDocumento52 páginas10 12 16 Journal Club ExampleSandra BaiAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 4: VascularNo EverandComplementary and Alternative Medical Lab Testing Part 4: VascularAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 8: UrologyNo EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyNota: 3 de 5 estrelas3/5 (1)
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderAinda não há avaliações
- Lu 2014Documento6 páginasLu 2014Yanet FrancoAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 7: EndocrineNo EverandComplementary and Alternative Medical Lab Testing Part 7: EndocrineAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 13: DermatologyNo EverandComplementary and Alternative Medical Lab Testing Part 13: DermatologyNota: 5 de 5 estrelas5/5 (4)
- Clinical Study Regarding The Effect of NDocumento7 páginasClinical Study Regarding The Effect of NcolceardoinaAinda não há avaliações
- 7decaf9c Cb18 4623 Bced Ecef2197e451Documento25 páginas7decaf9c Cb18 4623 Bced Ecef2197e451PrabhuAinda não há avaliações
- Metabolic Evaluation of Young Women With Congenital Adrenal HyperplasiaDocumento7 páginasMetabolic Evaluation of Young Women With Congenital Adrenal HyperplasiaOnysapto PramanaAinda não há avaliações
- Accepted Manuscript: MaturitasDocumento26 páginasAccepted Manuscript: MaturitasAlpha17 MedicsteenAinda não há avaliações
- HOMA Medicion EJIM2003Documento6 páginasHOMA Medicion EJIM2003Dr Dart05Ainda não há avaliações
- Metabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreNo EverandMetabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreNota: 4.5 de 5 estrelas4.5/5 (2)
- Research ArticleDocumento93 páginasResearch Articlearyan batangAinda não há avaliações
- NorthAmJMedSci 2015 7 7 310 161246Documento8 páginasNorthAmJMedSci 2015 7 7 310 161246Amany SalamaAinda não há avaliações
- Sindroma MetabolikDocumento7 páginasSindroma MetabolikainindyaAinda não há avaliações
- 4_2015Serum lipoprotein (a) concentrations are inversely associated with T2D, prediabetes, and insulin resDocumento10 páginas4_2015Serum lipoprotein (a) concentrations are inversely associated with T2D, prediabetes, and insulin resjef5525Ainda não há avaliações
- IDWG marker BP, nutrition, survival HDDocumento6 páginasIDWG marker BP, nutrition, survival HDAnthonyJohanAinda não há avaliações
- Salt and Metabolic Syndrome 2007Documento6 páginasSalt and Metabolic Syndrome 2007irene hoffmannAinda não há avaliações
- Nurul ArfinaDocumento9 páginasNurul ArfinaNurul ArfinaAinda não há avaliações
- Berri No 2014Documento7 páginasBerri No 2014Panji Agung KhrisnaAinda não há avaliações
- Diabetes Treatment Literature ReviewDocumento7 páginasDiabetes Treatment Literature Reviewafmzatvuipwdal100% (1)
- Article AmalDocumento16 páginasArticle Amalsaliha mharchiAinda não há avaliações
- 4CM14AD2021 RojasMontañezKathia PartesdelArtículoCientíficoDocumento8 páginas4CM14AD2021 RojasMontañezKathia PartesdelArtículoCientíficoKathiaAinda não há avaliações
- Abstracts For The Website - pdf1441898071Documento166 páginasAbstracts For The Website - pdf1441898071Radu MiricaAinda não há avaliações
- JAPI Body FatDocumento6 páginasJAPI Body FatBhupendra MahantaAinda não há avaliações
- Glycemic index, glycemic load, and blood pressure meta-analysisDocumento15 páginasGlycemic index, glycemic load, and blood pressure meta-analysisLisiane PerinAinda não há avaliações
- 5 Revathi EtalDocumento5 páginas5 Revathi EtaleditorijmrhsAinda não há avaliações
- Significance of Serum Uric Acid Level in Patients of Stroke With Diabetes MellitusDocumento4 páginasSignificance of Serum Uric Acid Level in Patients of Stroke With Diabetes MellitusIOSR Journal of PharmacyAinda não há avaliações
- Contribution of Lifestyle and Obesity To The Incidence of Pre-DiabetesDocumento7 páginasContribution of Lifestyle and Obesity To The Incidence of Pre-DiabetesRicky BooyAinda não há avaliações
- Non-Cephalic Presentation in Late Pregnancy: EditorialsDocumento2 páginasNon-Cephalic Presentation in Late Pregnancy: EditorialsNinosk Mendoza SolisAinda não há avaliações
- Dia Care 2014 Espeland 2548 56Documento9 páginasDia Care 2014 Espeland 2548 56Fikih Diah KusumasariAinda não há avaliações
- البحثDocumento43 páginasالبحثحسين علي ذيبان عليAinda não há avaliações
- Nej Mo A 1304501aasDocumento12 páginasNej Mo A 1304501aasHadiyana Arief HafizAinda não há avaliações
- Metabolic cardiovascular disease risk factors and their clustering in subclinical hypothyroidismDocumento7 páginasMetabolic cardiovascular disease risk factors and their clustering in subclinical hypothyroidismMaria Alice BourneufAinda não há avaliações
- Da QingDocumento18 páginasDa QingAlina PopaAinda não há avaliações
- 1 s2.0 S0002870320302143 MainDocumento9 páginas1 s2.0 S0002870320302143 MaindeepAinda não há avaliações
- Clinical and Epidemiological Profile of Diabetes Mellitus in Pregnancy, Isle of Youth, 2008Documento6 páginasClinical and Epidemiological Profile of Diabetes Mellitus in Pregnancy, Isle of Youth, 2008nunki aprillitaAinda não há avaliações
- tmp80F6 TMPDocumento24 páginastmp80F6 TMPFrontiersAinda não há avaliações
- tmpCE8C TMPDocumento19 páginastmpCE8C TMPFrontiersAinda não há avaliações
- tmpEFCC TMPDocumento6 páginastmpEFCC TMPFrontiersAinda não há avaliações
- tmp3CAB TMPDocumento16 páginastmp3CAB TMPFrontiersAinda não há avaliações
- tmpF178 TMPDocumento15 páginastmpF178 TMPFrontiersAinda não há avaliações
- tmpE7E9 TMPDocumento14 páginastmpE7E9 TMPFrontiersAinda não há avaliações
- tmpFFE0 TMPDocumento6 páginastmpFFE0 TMPFrontiersAinda não há avaliações
- Tmp1a96 TMPDocumento80 páginasTmp1a96 TMPFrontiersAinda não há avaliações
- tmpF407 TMPDocumento17 páginastmpF407 TMPFrontiersAinda não há avaliações
- tmp6F0E TMPDocumento12 páginastmp6F0E TMPFrontiersAinda não há avaliações
- tmpF3B5 TMPDocumento15 páginastmpF3B5 TMPFrontiersAinda não há avaliações
- Tmpa077 TMPDocumento15 páginasTmpa077 TMPFrontiersAinda não há avaliações
- tmpE3C0 TMPDocumento17 páginastmpE3C0 TMPFrontiersAinda não há avaliações
- tmpC0A TMPDocumento9 páginastmpC0A TMPFrontiersAinda não há avaliações
- tmp6382 TMPDocumento8 páginastmp6382 TMPFrontiersAinda não há avaliações
- tmp60EF TMPDocumento20 páginastmp60EF TMPFrontiersAinda não há avaliações
- Tmp75a7 TMPDocumento8 páginasTmp75a7 TMPFrontiersAinda não há avaliações
- tmp72FE TMPDocumento8 páginastmp72FE TMPFrontiersAinda não há avaliações
- tmp37B8 TMPDocumento9 páginastmp37B8 TMPFrontiersAinda não há avaliações
- tmp998 TMPDocumento9 páginastmp998 TMPFrontiersAinda não há avaliações
- tmp8B94 TMPDocumento9 páginastmp8B94 TMPFrontiersAinda não há avaliações
- tmpB1BE TMPDocumento9 páginastmpB1BE TMPFrontiersAinda não há avaliações
- tmpC30A TMPDocumento10 páginastmpC30A TMPFrontiersAinda não há avaliações
- tmp4B57 TMPDocumento9 páginastmp4B57 TMPFrontiersAinda não há avaliações
- tmpD1FE TMPDocumento6 páginastmpD1FE TMPFrontiersAinda não há avaliações
- tmp9D75 TMPDocumento9 páginastmp9D75 TMPFrontiersAinda não há avaliações
- tmpA0D TMPDocumento9 páginastmpA0D TMPFrontiersAinda não há avaliações
- tmp27C1 TMPDocumento5 páginastmp27C1 TMPFrontiersAinda não há avaliações
- tmp3656 TMPDocumento14 páginastmp3656 TMPFrontiersAinda não há avaliações
- tmp2F3F TMPDocumento10 páginastmp2F3F TMPFrontiersAinda não há avaliações
- Black BeautyDocumento70 páginasBlack BeautyMeryem DevirgenAinda não há avaliações
- Infineum Ilsa Gf-6 API SP e JasoDocumento28 páginasInfineum Ilsa Gf-6 API SP e JasoDanielAinda não há avaliações
- Understanding Urbanization & Urban Community DevelopmentDocumento44 páginasUnderstanding Urbanization & Urban Community DevelopmentS.Rengasamy89% (28)
- Lewis Carrol: Birth: DeathDocumento21 páginasLewis Carrol: Birth: DeathmarialuvsjeffAinda não há avaliações
- Harajuku: Rebels On The BridgeDocumento31 páginasHarajuku: Rebels On The BridgeChristian Perry100% (41)
- Cbydp Draft SK BaracbacDocumento13 páginasCbydp Draft SK BaracbacLikey PromiseAinda não há avaliações
- Class 9 - Half Yearly Examination - 2023 - Portions and BlueprintDocumento16 páginasClass 9 - Half Yearly Examination - 2023 - Portions and BlueprintSUBRAMANI MANOHARANAinda não há avaliações
- Corporate Subsidies On A Massive ScaleDocumento2 páginasCorporate Subsidies On A Massive ScaleBurchell WilsonAinda não há avaliações
- Cytogenectics Reading ListDocumento2 páginasCytogenectics Reading ListHassan GillAinda não há avaliações
- Stress-Busting Plan for Life's ChallengesDocumento3 páginasStress-Busting Plan for Life's Challengesliera sicadAinda não há avaliações
- Armitage Tutorial for Cyber Attack ManagementDocumento54 páginasArmitage Tutorial for Cyber Attack Managementworkmumbai3870Ainda não há avaliações
- Flow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorDocumento15 páginasFlow Through Pipes: Departmentofcivilengineering Presidency University, Bangalore-64 BY Santhosh M B Asstistant ProfessorSanthoshMBSanthuAinda não há avaliações
- Hci01 HumanComputerInteraction OverviewDocumento140 páginasHci01 HumanComputerInteraction OverviewAlexSpiridonAinda não há avaliações
- Nurses Week Program InvitationDocumento2 páginasNurses Week Program InvitationBenilda TuanoAinda não há avaliações
- Specification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VDocumento2 páginasSpecification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VJavierAinda não há avaliações
- Strategicmanagement Finalpaper 2ndtrisem 1819Documento25 páginasStrategicmanagement Finalpaper 2ndtrisem 1819Alyanna Parafina Uy100% (1)
- Plant Processes: Lesson 3Documento3 páginasPlant Processes: Lesson 3Kayla Ta’jaeAinda não há avaliações
- Purnanandalahari p3D4Documento60 páginasPurnanandalahari p3D4anilkumar100% (1)
- Ultra Slimpak G448-0002: Bridge Input Field Configurable IsolatorDocumento4 páginasUltra Slimpak G448-0002: Bridge Input Field Configurable IsolatorVladimirAinda não há avaliações
- Plano Electrico 785CDocumento2 páginasPlano Electrico 785CLuis MartínezAinda não há avaliações
- Material Safety Data Sheet: Development Associates, IncDocumento3 páginasMaterial Safety Data Sheet: Development Associates, IncDedi MulyadiAinda não há avaliações
- Lambika YogaDocumento2 páginasLambika Yogavsyamkumar100% (3)
- Caribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDocumento37 páginasCaribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDarrion BruceAinda não há avaliações
- 1ST Periodical Test ReviewDocumento16 páginas1ST Periodical Test Reviewkaren rose maximoAinda não há avaliações
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsDocumento10 páginasChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHIAinda não há avaliações
- Bread Machine Sunbeam 5891Documento44 páginasBread Machine Sunbeam 5891Tyler KirklandAinda não há avaliações
- Curriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: ObjectiveDocumento1 páginaCurriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: Objectivebhupal shresthaAinda não há avaliações
- The Filipino FamilyDocumento11 páginasThe Filipino FamilyTiger Knee97% (37)
- Transactionreceipt Ethereum: Transaction IdentifierDocumento1 páginaTransactionreceipt Ethereum: Transaction IdentifierVALR INVESTMENTAinda não há avaliações
- To Be African or Not To Be: An Autoethnographic Content Analysis of The Works of Dr. Asa Grant Hilliard, III (Nana Baffour Amankwatia, II) - by Qiana M. CuttsDocumento283 páginasTo Be African or Not To Be: An Autoethnographic Content Analysis of The Works of Dr. Asa Grant Hilliard, III (Nana Baffour Amankwatia, II) - by Qiana M. Cutts☥ The Drop Squad Public Library ☥100% (1)