Escolar Documentos
Profissional Documentos
Cultura Documentos
Knowledge and Disclosure of Hiv Status Among Adolescents Accra Ghana
Enviado por
Obadele KambonDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Knowledge and Disclosure of Hiv Status Among Adolescents Accra Ghana
Enviado por
Obadele KambonDireitos autorais:
Formatos disponíveis
Kenu et al.
BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
RESEARCH ARTICLE
Open Access
Knowledge and disclosure of HIV status among
adolescents and young adults attending an
adolescent HIV clinic in Accra, Ghana
Ernest Kenu1,3*, Adjoa Obo-Akwa1,2, Gladys B Nuamah1, Anita Brefo1, Miriam Sam1 and Margaret Lartey1,2
Abstract
Background: In Ghana it is estimated that 1.2% of HIV infections occur in young people aged 15-24 but the
representation in our clinics is small. Adherence to treatment, appointment keeping and knowledge of HIV status
remains a challenge. Disclosure has been shown to result in better adherence to therapy, good clinical outcomes,
psychological adjustment and reduction in the risk of HIV transmission when the young person becomes sexually
active. A baseline study was conducted to ascertain if adolescents and young adults knew their HIV status and their
knowledge on HIV. Informed consent and assent were obtained from willing participants. Self-administered
questionnaires on general knowledge of HIV, HIV treatment and disclosure were collected and analyzed.
Results: Thirty-four young persons participated in the study. The mean age was 16.9 SD 2.5 and 62% (21/32)
were female. All of them were still in school. Eighty-five percent were aware that young people their age could fall
sick, 91% had heard of HIV, 70% knew someone with HIV and 45% thought that adolescents were not at risk of HIV.
On modes of HIV transmission, 66.7% knew HIV was transmitted through sex and 63.6% knew about mother to
child transmission. Fifty three percent (18/34) knew their HIV status, 50% (17/34) were on antiretroviral and 35%
(6/17) of them admitted to missing ARV doses. One person who said he was HIV negative and another who did
not know his status were both on ARVs.
Conclusion: Disclosure of HIV status to adolescents and young people is dependent on a complex mix of factors
and most practitioners recommend an age and developmentally appropriate disclosure. Thus it is highly individualized.
The knowledge and awareness of HIV was 91% compared to 97% of adults in the most recent Ghana Demographic
and Health Survey however only about two thirds had acceptable in depth knowledge on HIV. Only half knew their
HIV status which was not the best considering their ages. There is the need to strengthen education to young persons
with HIV, support adhere to ARVs for better outcomes and assist care givers to disclose HIV status to them.
Keywords: Knowledge, Disclosure adolescents/young adults, HIV
Background
Children under 15 years of age account for approximately
3.3 million of the people living with human immune virus
(HIV)/acquired immune deficiency syndrome (AIDS)
worldwide, and almost 90% of all HIV infected children
live in sub-Saharan Africa including Ghana [1]. In Ghana
the prevalence of HIV in young people from 15-24 years is
* Correspondence: Ernest_kenu@yahoo.com
1
Korle-Bu Teaching Hospital, Accra, Ghana
3
Department of Epidemiology and Disease Control, School of Public Health,
College of Health Sciences, University of Ghana, P.O. Box LG 13, Legon,
Ghana
Full list of author information is available at the end of the article
1.2% [2]. Currently, children infected with HIV through
mother-to-child transmission once diagnosed and in care,
live longer and reach adolescence because of greater access
to antiretroviral therapy (ART) in the past decade in West
Africa [3,4]. Thus, with the start of national programme
for providing care and free highly active antiretroviral therapy (HAART) to children, there has been a significant reduction in morbidity and mortality of HIV infected
children and more of them are surviving through childhood into adolescence with improved quality of life [3].
Along with the increased survival of children infected
with HIV, disclosure of HIV status to children remains a
complex and a critical clinical issue in the care of HIV
2014 Kenu et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Kenu et al. BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
infected children [4]. World Health organization (WHO)
and American Academy of Pediatrics (AAP) strongly encourage disclosing HIV infection status to school aged
children and younger children. They should be informed
incrementally to accommodate their cognitive skills and
emotional maturity [5,6]. Telling children and adolescents about their HIV infection is a challenging dilemma
because children are often asymptomatic in the early
stages of HIV infection, yet require daily medications
and close monitoring [7].
Caregivers and healthcare workers are presented with
group of challenges around disclosure, including deciding on what is in the childs best interest and when, why
and how information about his/her HIV positive status
should be shared with him/her. Caregivers are reluctant
to disclose the HIV positive status to their children for
fear of social rejection and isolation, parental sense of
guilt, and fear that the child would not keep diagnosis to
themselves [8,9]. Disclosure of HIV status helps HIV infected adolescents to understand their status and the need
for treatment, thereby promoting their participation and
responsibility for their care [10]. The rate of disclosure remains low especially in resource limited countries despite
the growing evidence of the benefits of disclosure [11].
The inability of most caregivers to handle disclosure has
defined the three main patterns of disclosure: complete,
partial, and non-disclosure. Complete disclosure of HIV
status has been associated with improved adherence to
ART [12]. Whereas partial and non-disclosure can strain
the relationship between the caregiver and the child. In
such situations, force and persuasion are often used to get
the child to adhere to treatment; these may results in purposeful rebellion and non-adherence by the child [12].
There is a lot of controversy about what and when to
tell children living with HIV about their diagnosis. Many
families do not think their children can handle the information and they do not want to upset them because
they have already been through so much [8]. Several
studies have documented the benefits of disclosure of
HIV positive status to HIV infected children and adolescents, including psychological benefits as well as positive
effects on the clinical course of the disease [6-9]. The
American Academy of Pediatrics recommends that children and adolescents with HIV should be told their diagnosis [6]. However, published rates of disclosure in
children from resource rich countries vary widely, from
18 to 77% [6-9,12], partly due to the lack of conclusive
guidelines on when and how to disclose the diagnosis of
HIV to children.
Though limited, studies available on rates and effects
of HIV disclosure on children are mainly from resource
rich countries. There is paucity of data on disclosure from
resource limited settings, where the majority of HIV
infected children live. Moreover, studies from resource
Page 2 of 6
limited settings have mainly been qualitative in design
with small samples sizes making it difficult to generalize
the findings. This study found out the knowledge and disclosure of HIV status among adolescents and young adults
attending adolescent HIV clinic.
Methods
A cross-sectional study was carried out in July 2013
among HIV infected adolescent and young adults attending an adolescent club meeting in Accra. The Adolescent
HIV Care programme at Fevers unit of Korle-Bu Teaching
Hospital was established in June 2012 and provides comprehensive HIV/AIDS care and management of opportunistic infections. The Unit serves as the national referral
centre for HIV-infected patients. Ever since the first case
of HIV was diagnosed in Ghana in 1986, the Unit has provided care and support to persons living with HIV/AIDS.
Provision of comprehensive HIV/AIDS care and treatment started at the Unit in December 2003 in line with
the scale-up of access to treatment by the National AIDS
Control Programme (NACP) and her partners.
Patients are referred from the paediatric HIV clinic to
the adult clinic at age twelve. Thus the adult clinic serves
both adolescents and adults. An adolescent clinic was
started as best practice when it was recognized that their
needs and expectations were not being met at the adult
clinic. The clinic was supported by adult physicians since
it proved difficult to get the paediatricians to come on
board.
The adolescents and young adults referred to the clinic
present with the following modes of diagnosis: have
mothers known to be HIV seropositive during pregnancy
through the programme for the prevention of mother-tochild transmission (PMTCT), others are discovered to be
infected with HIV after presenting with an AIDS-defining
illness, or are diagnosed after either a symptomatic sibling
or parent was found to be HIV positive. Majority of them
were infected perinatally. At the time of the study, the
adolescent clinic was 13 months old and had about 70
HIV infected adolescents and young adults.
Korle-Bu Teaching Hospital gave the approval for the
formation of the adolescent group as well as the study.
All the young people recruited into the study received
medical care for their HIV infection through the clinic
and were all invited to voluntarily participate in a general survey on HIV infection at one of the club meetings
(Self-selection). Following the self-selection, written informed consent was obtained from those aged 16 years
and above and assent and permission from care givers
for those less than 16 years after briefing on the purpose,
use, and significance of the study. Those who did not
consent were excluded from the survey but continued to
participate in the fun games, music and dance.
Kenu et al. BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
A structured questionnaire was then used to collect
data. The questionnaire was anonymous and solicited information on respondents background as well as their
general knowledge on the causes, mode of transmission of
HIV, HIV treatment and disclosure. The questionnaire
had three parts. The first part was closed ended and contained questions on the background of the respondents.
The second part contained questions on general knowledge and awareness of HIV/AIDS found in HIV/AIDS
awareness leaflets used by the Ghana AIDS Commission
for information, education and communication. The final
part of the questionnaire sought respondents views on
HIV status, disclosure and treatment. Here, information
was collected on disclosure status, age at disclosure, treatment compliance, and socio-demographic data, family
type (biologic parents, adoptive/foster, extended), and
care- givers HIV status. Service providers and care givers
were independently interviewed in a focused group discussion on HIV disclosure. The data collected was entered
and analyzed using Statistical Package for the Social
Sciences (SPSS; IBM Corporation, Armonk, NY, USA)
version 16 with the key issues being presented in summary
frequency tables as descriptive statistics.
Results
Demography of respondents
A total of thirty-four (34) young persons living with HIV
from age 13 to 22 were self-recruited to participate in the
study out of 36 at the adolescent meeting. Thirty four adolescents and young adults did not attend the adolescent
meeting. The mean age of respondents was 16.91 2.5, of
which 61.8% (21/34) were females. All participants were
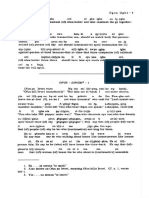
still in school and the distribution is showed in Figure 1.
In relation to religion, 94% (32/34) were Christians and
6% (2/34) were Muslims. The demographic characteristics
of the absentees from the meeting were similar to those
who attended. Of the 8 care givers in the FGD 7 were females and 1 male whereas 75% (6/8) of the service providers in the FGD were females.
Figure 1 Educational level of respondents.
Page 3 of 6
HIV knowledge
Eighty-five percent (29/34) of respondents were aware that
young people of their age could fall sick whilst 5.8% (2/34)
thought otherwise and 8.8% (3/34) did not give any response. Over 91% (31/34) of adolescents had heard of
HIV as compared to 8.8% (3/34) who had no clue. Moreover, 70.6% (24/34) knew someone with HIV whilst the
remaining 29.4% (10/34) did not. Forty-five percent
thought that adolescents were not at risk of getting HIV.
Fifteen percent (5/34) were not sure whether infected patients could continue with their education. Sub-analysis
did not show any statistical difference in HIV knowledge
in terms age, sex and educational status.
Modes of transmission
Majority of the respondents 90.4% (multiple responses)
were able to correctly identify one or more mode of HIV
of transmission with the remaining 9.6% were not able to
provide any correct answers. Out of those who correctly
identified the modes of transmission, 66.7% knew that
HIV could be transmitted through unprotected sexual
intercourse with infected persons and 63.6% knew about
mother to child transmission. Twenty three percent (19/
83 multiple responses) said HIV can be transmitted by
sharing sharp needles/syringes with infected persons.
Overall, 29% (10/34) participants think HIV can be transmitted through physical contact.
The prevalence of HIV disclosure and antiretroviral
therapy
HIV disclosure status rate was 52.9% (18/34), 20.6% (7/
34) said they did not have HIV, 20.6% (7/34) did not
know whether they had it or not and 5.9% (2/34) did not
give any specific answer. Ninety three percent (13/14) of
those who did not know their HIV status were between
13 to 15 years. Fifty percent (17/34) of the respondents
were on antiretroviral whilst 5.9% (2/34) were not, however 26.5% (9/34) did not know whether they were on
ARVs or not. One person who said he was HIV negative
Kenu et al. BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
but was on ARVs and 17.6% (6/34) did not give any response. In general, 35% (6/17) of the respondents who
knew they were on ARVs admitted missing some of their
doses Figure 2.
From the FGDs, most of the disclosures happened after
ART initiation and were planned. The persons involved in
this process varied across individual families. It was sometimes disclosed by family members, particularly care givers
or parents after an interview between the latter and a
psychologist. None of the respondents did find out their
status by chance or through unplanned events.
Limitation
The study was carried out in a single adolescent clinic
with a small sample size which may affect generalizability
of our findings.
Discussion
Knowledge of HIV
The study revealed that 90.4% were able to correctly
identify one or more mode of HIV transmission with the
remaining 9.6% not able to provide any correct answer.
The fact that 10% of respondents were ignorant on
mode of HIV transmission even when they were HIV
positive poses serious threats to HIV/AIDS prevention
and control in this age group. It was however not clear
whether this was just ignorance or denial. This study is
in line with findings from other studies done in developing countries such as South Africa and Ethiopia as only
about half knew much about their HIV including their
status even when on anti-retroviral therapy which was
quiet poor [13].
The key to HIV awareness hinges on knowledge of what
HIV and AIDS is, and what exposures and risky behaviors
can potentially lead to contracting the virus. Knowledge of
Figure 2 ART patients knowledge on the type of medication
they are taking.
Page 4 of 6
HIV among infected adolescents and young adults is
therefore crucial not only in preventing the spread of the
virus, but also in addressing the threats posed by HIV/
AIDS. There is the need to strengthen education to young
persons on HIV as well as support care givers to disclose
HIV status and to support young people to adhere to
ARVs for better outcomes.
Status of disclosure
The prevalence of disclosure among our study population was 52.9% (18/34). This is however within the middle bounds of the range (1877%) reported in studies
from resource rich countries. Our finding is consistent
but slightly higher than the reported prevalence of disclosure from Thailand, Zambia, and Uganda of 30.1%,
31.8%, and 29%, respectively [6,7,12,14]. Of the children
who did not know their HIV positive status, more than
two third reportedly were being told of other related
diagnosis like TB, malaria, cholera and the rest did not
have any clue at all about their illness. Reasons cited by
the caregivers for not disclosing HIV status to their
wards were consistent with that of studies in resourcelimited countries; namely stigmatization and isolation,
parental sense of guilt and fear that the child would not
keep diagnosis to themselves [10,15]. As part of standard
of care, disclosure is made to adolescents before transfer
to the adult clinic. We are unable to tell if these were
missed, disclosure was made but not accepted or that
adolescents and care givers were still in denial. Interestingly, some caregivers for fear of stigma reverse what
healthcare providers say as soon as they leave the presence of healthcare providers. However, several studies
from both resource rich and resource limited countries
suggest that the disclosure of HIV status to HIV infected
adolescents and young adults has immense psychological
benefits and positive effects on the clinical course of the
disease [5,12,16,17].
Our findings and that of other studies in the subregion of low rate of disclosure underscore the need for
a systematic review of the hurdles to disclosure and implementation of locally and culturally sensitive interventions programs to promote disclosure.
Nearly a third of the caregivers expected the healthcare providers alone to disclose the HIV status of their
children. This is contrary to European study where majority of caregivers believed that as parents it was their
responsibility to disclose the diagnosis to the child [14].
This may be partly due to the cultural differences in relation to communication between parents and children
on issues and the lack of disclosure skills. The healthcare
providers agreed that disclosure is the prerogative of the
caregivers and children should be told their HIV status.
These contrasting views are consistent with that of studies from resource rich countries [14]. The expectation of
Kenu et al. BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
some caregivers that healthcare providers should disclose
the HIV status to the HIV infected adolescents may lead
to unnecessary delays in disclosure. As reiterated by the
healthcare providers, training in disclosure counseling and
a disclosure program adopted by the clinic would allow
healthcare providers to better advice caregivers on how to
disclose. With caregivers who lack disclosure skills, a
counselor assisted or supported disclosure session may
suffice [10].
Transmission of HIV/AIDS
Ninety percent of respondents were able to clearly point
out that HIV/AIDS may be transmitted through having
unprotected sex with an infected partner, being born to
a mother who is infected with HIV, or through the infected mothers breast milk. Which is similar to the 2008
Ghana Demographic and Health survey (GDHS) report
of 97% adult knowledge on HIV transmission [18]. Almost
all the adolescents and young adults were also aware that
using unsterilized instruments or sharing personal items
like toothbrushes could lead to acquiring the virus. Their
awareness has a positive impact on prevention of HIV/
AIDS considering that sharing items like blades, toothbrushes, pins and needles, cooking and pocket knives, hair
and nail clippers, and other sharp objects is a major cause
of transmission in less developed countries [16].
The small proportion (10/34) of participants believed
that physical contact with infected persons or sharing public space with infected persons could be a source of transmission of HIV/AIDS. This might explain the relatively
high stigmatization and discrimination against PLWHA by
their colleagues within some communities in Sub Saharan
Africa [4]. This is in sharp contrast to the content of educational materials and information provided by the Ghana
AIDS Commission, National HIV/AIDS Control Program,
and the mass media on HIV/AIDS transmission. These
materials clearly explain that it is a scientifically proven fact
that physical contact, without the exchange of bodily fluids
with an infected person, cannot transmit the virus. In fact,
a lot of HIV/AIDS awareness messages in Ghana focus on
this point because of the realization that poor awareness of
this fact leads to high stigmatization, seclusion, and discrimination of PLWHA. Such perceptions also explain the
case made by World Bank that PLWHA in rural areas and
less developed countries are sometimes denied access to
public transport, swimming in public pools, fetching water
from public standpipes, engaging in contact sports, and
other activities that involve physical proximity [19].
Believing that physical contact and sharing public space
can lead to HIV infection may result in the adolescent and
young person self-isolation and self-stigmatization. He or
she may not want to socialize and interact for fear of
transmitting the virus or becoming infected. These leads
to poor social skills, lack of support and subsequently
Page 5 of 6
affect adherence and also school work. If such perceptions
are still being held by some people, then prevention and
even management of new and existing cases of HIV/AIDS
may be seriously hindered.
Conclusions
In conclusion, 47% of HIV infected adolescents in the study
were not aware of their HIV status, though strong beneficial
effect of HIV disclosure on retention in care after ART initiation beyond the age of ten is known. Disclosure of HIV
status to adolescents and young people is dependent on a
complex mix of factors and most practitioners recommend
an age and developmentally appropriate disclosure thus it
is highly individualized. The knowledge and awareness of
HIV was 91% compared to 97% of adults in the most recent
Ghana demographic and health Survey. There is the need
to support care givers to disclose HIV status and to support
young people to adhere to ARVs for better outcomes.
Consent
Written informed consent was obtained from the patients
guardian/parent/next of kin for the publication of this
report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
Conceived and designed the study: EK, ML, GBN, AOA, MS and AB Performed
the experiments: EK, ML, GBN, AOA, AB and MS. Analyzed the data: ML, EK,
GBN and AOA. Wrote the paper: GBN, EK and ML. All authors read and
approved the final manuscript.
Acknowledgments
We would like to thank study participants and the staff of Adolescents/young
adult clinic for their participation in this study.
Author details
1
Korle-Bu Teaching Hospital, Accra, Ghana. 2Department of Medicine and
Therapeutics, University of Ghana Medical School, Accra, Ghana. 3Department
of Epidemiology and Disease Control, School of Public Health, College of
Health Sciences, University of Ghana, P.O. Box LG 13, Legon, Ghana.
Received: 16 July 2014 Accepted: 18 November 2014
Published: 26 November 2014
References
1. Global summary of the AIDS epidemic. http://www.unaids.org/sites/
default/files/en/media/unaids/contentassets/documents/epidemiology/
2013/gr2013/201309_epi_core_en.pdf.
2. National AIDS/STI Control Programme, Ghana Health Service: HIV Sentinel
Survey Report. 2013.
3. Foster C, Fidler S: Optimizing antiretroviral therapy in adolescents with
perinatally acquired HIV-1 infection. Expert Rev Anti Infect Ther 2010,
8:14031416. doi:10.1586/eri.10.129. View Article PubMed/NCBI Google
Scholar.
4. Eng E, Maman S, Tshikandu T, Behets F, Vaz LM: Telling children they have
HIV: lessons learned from findings of a qualitative study in sub-Saharan
Africa. AIDS Patient Care STDS 2010, 24:247256.
5. World Health Organization: Guideline on HIV disclosure counselling for
children up to 12 years of age. 2011. http://whqlibdoc.who.int/
publications/2011/9789241502863_eng.pdf.
Kenu et al. BMC Research Notes 2014, 7:844
http://www.biomedcentral.com/1756-0500/7/844
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
Page 6 of 6
American Academy of Pediatrics Committee on Pediatrics AIDS: Disclosure
of illness status to children and adolescents with HIV infection.
Pediatrics 2010, 103:164166.
Menon A, Glazebrook C, Campain N, Ngoma M: Mental health and
disclosure of HIV status in Zambian adolescents with HIV infection:
implications for peer-support programs. J Acquir Immune Defic Syndr 2007,
46:349354.
Lee CL, Johann-Liang R: Disclosure of the diagnosis of HIV/ AIDS to
children born of HIV-infected mothers. AIDS Patient Care STDS 1999,
13:4145.
Vaz L, Corneli A, Dulyx J, Rennie S, Omba S, Kitetele F, Behets F, AD
Research Group: The process of HIV status disclosure to HIV-positive
youth in Kinshasa, Democratic Republic of the Congo. AIDS Care 2008,
20:842852.
Bachanas PJ, Kullgren KA, Schwartz KS, Lanier B, McDaniel JS, Smith J,
Nesheim S: Predictors of psychological adjustment in school-age children
infected with HIV. J Pediatr Psychol 2001, 26:343352.
Mahloko JM, Madiba S: Disclosing HIV diagnosis to children in Odi district,
South Africa: reasons for disclosure and non-disclosure. Afr J Prm Health
Care Fam Med 2012, 4:17.
Bikaako-Kajura W, Luyirika E, Purcell DW, Downing J, Kaharuza F, Mermin J,
Malamba S, Bunnell R: Disclosure of HIV status and adherence to daily
drug regimens among HIV- infected children in Uganda. AIDS Behav
2006, 10:S85S93.
Demmer C: Experiences of families caring for an HIV-infected child in
KwaZulu-Natal, South Africa: an exploratory study. AIDS Care 2011,
23:873879.
Thorne C, Newell ML, Peckham CS: Disclosure of diagnosis and planning
for the future in HIV-affected families in Europe. Child Care Health Dev
2000, 26:2940.
Moore AR, Williamson D: Disclosure of childrens positive serostatus to
family and nonfamily members: informal caregivers in Togo, West Africa.
AIDS Res Treat 2011, 2011:595301.
Ferris M, Burau K, Schweitzer AM, Mihale S, Murray N, Preda A, Ross M, Kline
M: The influence of dis-closure of HIV diagnosis on time to disease
progression in a cohort of Romanian children and teens. AIDS Care 2007,
19:10881094.
Siu GE, Bakeera-Kitaka S, Kennedy CE, Dhabangi A, Kambugu A: HIV serostatus
disclosure and lived experiences of adolescents at the Transition Clinic of
the Infectious Diseases Clinic in Kampala, Uganda: a qualitative study.
AIDS Care 2012, 24:606611.
Ghana Demographic Health Survey Report. 2008.
World Bank: HIV/AIDS prevention and Care Strategies for HIV; 2010. Retrieved
from http://siteresources.worldbank.org/EDUCATION/Resources/2782001099079877269/547664-1099080042112/Edu_HIVAIDS_window_hope.pdf.
doi:10.1186/1756-0500-7-844
Cite this article as: Kenu et al.: Knowledge and disclosure of HIV status
among adolescents and young adults attending an adolescent HIV
clinic in Accra, Ghana. BMC Research Notes 2014 7:844.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Você também pode gostar
- Evolving EarthDocumento38 páginasEvolving EarthObadele KambonAinda não há avaliações
- Wadi Al-JarfDocumento22 páginasWadi Al-JarfObadele KambonAinda não há avaliações
- Wadi Al-JarfDocumento22 páginasWadi Al-JarfObadele KambonAinda não há avaliações
- Sandro Capo Chichi: (Texte)Documento34 páginasSandro Capo Chichi: (Texte)Obadele KambonAinda não há avaliações
- 1st African Regional Martial Arts CongressDocumento8 páginas1st African Regional Martial Arts CongressObadele KambonAinda não há avaliações
- Remarks On A Few "Polyplural" Classes in Bantu: Africa & Asia, No 3, 2003, PP 161-184Documento24 páginasRemarks On A Few "Polyplural" Classes in Bantu: Africa & Asia, No 3, 2003, PP 161-184Obadele KambonAinda não há avaliações
- Egyptian, Hieroglyphs, In, Five, Weeks, A, Crash, Course, In, The, Script, And, Language, Of, The, Ancient, Egyptians, IDocumento2 páginasEgyptian, Hieroglyphs, In, Five, Weeks, A, Crash, Course, In, The, Script, And, Language, Of, The, Ancient, Egyptians, IObadele KambonAinda não há avaliações
- ACTFLProficiencyGuidelines2012 FINALDocumento53 páginasACTFLProficiencyGuidelines2012 FINALObadele KambonAinda não há avaliações
- Inherent Complement Verbs - Sampson KorsahDocumento26 páginasInherent Complement Verbs - Sampson KorsahObadele Kambon100% (1)
- Ghana Beads HandoutDocumento2 páginasGhana Beads HandoutObadele KambonAinda não há avaliações
- Ifa Divination PDFDocumento2 páginasIfa Divination PDFObadele KambonAinda não há avaliações
- Radical Caribbean Social Thought: Race, Class Identity and The Postcolonial NationDocumento19 páginasRadical Caribbean Social Thought: Race, Class Identity and The Postcolonial NationObadele KambonAinda não há avaliações
- Anubis - The God's Manifestation in The Iconographical and Literary Sources of The Pharaonic PeriodDocumento140 páginasAnubis - The God's Manifestation in The Iconographical and Literary Sources of The Pharaonic PeriodObadele Kambon100% (1)
- Wiley Ethics - Guidelines - 7.06.17 PDFDocumento29 páginasWiley Ethics - Guidelines - 7.06.17 PDFObadele KambonAinda não há avaliações
- Ife 6 Year ProjectDocumento193 páginasIfe 6 Year ProjectObadele Kambon100% (2)
- Cifar: Connecting The Best Minds For A Better WorldDocumento1 páginaCifar: Connecting The Best Minds For A Better WorldObadele KambonAinda não há avaliações
- AASR Bulletin 45 - 2 PDFDocumento101 páginasAASR Bulletin 45 - 2 PDFObadele KambonAinda não há avaliações
- Bantoid Languages in KoelleDocumento1 páginaBantoid Languages in KoelleObadele KambonAinda não há avaliações
- 2010 Ptolemaic HieroglyphsDocumento11 páginas2010 Ptolemaic HieroglyphsShihab EldeinAinda não há avaliações
- Pankhurst Richard Italian Fascist War CrimesDocumento59 páginasPankhurst Richard Italian Fascist War CrimesObadele KambonAinda não há avaliações
- Ifa Divination PDFDocumento2 páginasIfa Divination PDFObadele KambonAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- 2021-2022 Business French BCAD 108-Detailed Course OutlineDocumento5 páginas2021-2022 Business French BCAD 108-Detailed Course OutlineTracy AddoAinda não há avaliações
- Chapter 8Documento5 páginasChapter 8Bernadette PononAinda não há avaliações
- Cumberland Youth Football Registration 2021Documento3 páginasCumberland Youth Football Registration 2021api-293704297Ainda não há avaliações
- Field Experience Assignment #1: Become Familiar With The SchoolDocumento6 páginasField Experience Assignment #1: Become Familiar With The Schoolapi-511543756Ainda não há avaliações
- The V ttaRatnaKara and The ChandoMañjarī. Patgiri Ritamani, 2014Documento154 páginasThe V ttaRatnaKara and The ChandoMañjarī. Patgiri Ritamani, 2014Srinivas VamsiAinda não há avaliações
- Daily Time Record Daily Time Record: Saturday SundayDocumento13 páginasDaily Time Record Daily Time Record: Saturday Sundaysingle ladyAinda não há avaliações
- Roya Abdoly ReferenceDocumento1 páginaRoya Abdoly Referenceapi-412016589Ainda não há avaliações
- Course Outline Pre-Calc Math 12Documento2 páginasCourse Outline Pre-Calc Math 12api-709173349Ainda não há avaliações
- Modified Double Glove TechniqueDocumento1 páginaModified Double Glove TechniqueSohaib NawazAinda não há avaliações
- EappDocumento19 páginasEappdadiosmelanie110721Ainda não há avaliações
- Translation Services in Hong KongDocumento12 páginasTranslation Services in Hong KongAnjali ukeyAinda não há avaliações
- Critical Thinking QuestionsDocumento2 páginasCritical Thinking QuestionsJulie Ann EscartinAinda não há avaliações
- Unit 5 Mock Paper1Documento78 páginasUnit 5 Mock Paper1SahanNivanthaAinda não há avaliações
- Rubric Shom Art Exploration Shoe DrawingDocumento1 páginaRubric Shom Art Exploration Shoe Drawingapi-201056542100% (1)
- Project Proposal I. Project Title II. Theme Iii. Ifp Goal IV. Implementation Date V. VenueDocumento7 páginasProject Proposal I. Project Title II. Theme Iii. Ifp Goal IV. Implementation Date V. VenueJay Frankel PazAinda não há avaliações
- Dolphin Readers Level 1 Number MagicDocumento19 páginasDolphin Readers Level 1 Number MagicCharles50% (2)
- Anurag Goel: Principal, Business Consulting and Advisory at SAP (Among Top 0.2% Global SAP Employees)Documento5 páginasAnurag Goel: Principal, Business Consulting and Advisory at SAP (Among Top 0.2% Global SAP Employees)tribendu7275Ainda não há avaliações
- Handout Sa Personal Development G 11Documento2 páginasHandout Sa Personal Development G 11Alecks Luis JacobeAinda não há avaliações
- Lesson 3 - A Person You AdmireDocumento6 páginasLesson 3 - A Person You AdmireBen English TVAinda não há avaliações
- Why Women Wash DishesDocumento9 páginasWhy Women Wash Dishesmoodswingss100% (1)
- Assignment 1Documento3 páginasAssignment 1SourabhBharatPanditAinda não há avaliações
- The Reaction Paper, Review, and CritiqueDocumento16 páginasThe Reaction Paper, Review, and CritiqueChristian PapaAinda não há avaliações
- On Your Date of Joining, You Are Compulsorily Required ToDocumento3 páginasOn Your Date of Joining, You Are Compulsorily Required Tokanna1808Ainda não há avaliações
- Chapter 1 Research PaperDocumento5 páginasChapter 1 Research PaperMae DeloriaAinda não há avaliações
- Trainee'S Record Book: Muñoz National High SchoolDocumento8 páginasTrainee'S Record Book: Muñoz National High SchoolGarwin Rarama OcampoAinda não há avaliações
- Proverbs 1: Prov, Christ's Death in TheDocumento24 páginasProverbs 1: Prov, Christ's Death in TheO Canal da Graça de Deus - Zé & SandraAinda não há avaliações
- TestAS-Economic-2017 (Second Edition)Documento16 páginasTestAS-Economic-2017 (Second Edition)Thanh VuAinda não há avaliações
- Les FHW 10Documento17 páginasLes FHW 10Parvez TuhenAinda não há avaliações
- Steps in Successful Team Building.: Checklist 088Documento7 páginasSteps in Successful Team Building.: Checklist 088Sofiya BayraktarovaAinda não há avaliações