Escolar Documentos
Profissional Documentos
Cultura Documentos
Lung Protective Mechanical Ventilation Strategies
Enviado por
Anne Julia AgustinDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Lung Protective Mechanical Ventilation Strategies
Enviado por
Anne Julia AgustinDireitos autorais:
Formatos disponíveis
International Journal of General Medicine
Dovepress
open access to scientific and medical research
ORIGINAL RESEARCH
International Journal of General Medicine downloaded from https://www.dovepress.com/ by 192.30.84.235 on 16-Nov-2016
For personal use only.
Open Access Full Text Article
Lung protective mechanical ventilation strategies
in cardiothoracic critical care: a retrospective
study
This article was published in the following Dove Press journal:
International Journal of General Medicine
11 November 2016
Number of times this article has been viewed
Vasileios Zochios 13
Matthew Hague 3,4
Kimberly Giraud 5
Nicola Jones 3
1
Department of Intensive Care
Medicine, Queen Elizabeth Hospital
Birmingham, University Hospitals
Birmingham NHS Foundation
Trust, 2Institute of Inflammation
and Ageing, College of Medical
and Dental Sciences, University
of Birmingham, 3Department of
Anesthesia and Intensive Care
Medicine, Papworth Hospital NHS
Foundation Trust, Papworth Everard,
Cambridge, 4Department of Medicine,
Colchester Hospital University NHS
Foundation Trust, Colchester General
Hospital, Colchester, 5Research and
Development Department, Papworth
Hospital NHS Foundation Trust,
Papworth Everard, Cambridge, UK
Correspondence: Vasileios Zochios
Department of Intensive Care Medicine,
Queen Elizabeth Hospital Birmingham,
University Hospitals Birmingham
NHSFoundation Trust, Birmingham,
B152GW, UK
Tel +44 121 627 2000
Email vasileioszochios@doctors.org.uk
Introduction
Positive pressure mechanical ventilation (MV) can lead to ventilator associated lung
injury (VALI) due to cyclic alveolar atelectasis and strain. Risk factors for VALI in
patients without acute respiratory distress syndrome (ARDS) include high tidal volume
(Vt >6 mL/kg predicted body weight [PBW]), acidemia, blood product transfusion,
and restrictive lung disease.1 A randomized controlled trial (RCT) of low tidal volume
ventilation in patients with mild ARDS (the term acute lung injury has been replaced
with mild ARDS: 26.6 kPa < partial pressure of arterial oxygen (PaO2)/fraction of
inspired oxygen (FiO2) 40 kPa),24 carried out by the ARDS Network, demonstrated
an 8.8% absolute reduction in short term mortality.35
There is a body of evidence supporting the use of low tidal volume (Vt 68 mL/kg
PBW) in slowing progression to ARDS in patients with normal lungs.4 Gajic et al
demonstrated that 24% of intensive care unit (ICU) patients with noninjured lungs,
who received MV for 2 days or longer, developed ARDS within the first 5 days of
MV. A multivariate analysis revealed an increased risk of developing ARDS with the
use of volumes >6 mL/kg PBW (odds ratio [OR] 1.3 for every 1 mL >6 mL/kg PBW,
P<0.001). A large database analysis of over 3,000 mechanically ventilated ICU patients
without ARDS showed that ARDS developed in 6.2% of patients after 48 hours of MV.
A multivariate analysis revealed that the use of a Vt >700 mL was associated with an
OR of 2.66 for the development of ARDS (P<0.001).1,4,5
415
submit your manuscript | www.dovepress.com
International Journal of General Medicine 2016:9 415418
Dovepress
2016 Zochios et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
php and incorporate the Creative Commons Attribution Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work
you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
http://dx.doi.org/10.2147/IJGM.S122204
Powered by TCPDF (www.tcpdf.org)
Abstract: A body of evidence supports the use of low tidal volumes in ventilated patients
without lung pathology to slow progress to acute respiratory distress syndrome (ARDS) due
to ventilator associated lung injury. We undertook a retrospective chart review and tested the
hypothesis that tidal volume is a predictor of mortality in cardiothoracic (medical and surgical) critical care patients receiving invasive mechanical ventilation. Independent predictors of
mortality in our study included: type of surgery, albumin, H+, bilirubin, and fluid balance. In
particular, it is important to note that cardiac, thoracic, and transplant surgical patients were
associated with lower mortality. However, our study did not sample equally from The Berlin
Definition of ARDS severity categories (mild, moderate, and severe hypoxemia). Although our
study was not adequately powered to detect a difference in mortality between these groups, it
will inform the development of a large prospective cohort study exploring the role of low tidal
volume ventilation in cardiothoracic critically ill patients.
Keywords: lung protective ventilation, cardiothoracic critical care, acute respiratory distress
syndrome, invasive mechanical ventilation
Dovepress
International Journal of General Medicine downloaded from https://www.dovepress.com/ by 192.30.84.235 on 16-Nov-2016
For personal use only.
Zochios et al
The use of lung damaging ventilation strategies (large
Vts and high plateau pressures) in patients who develop
subclinical lung injury during surgery, which involves large
pulmonary resection or cardiopulmonary bypass (CPB), can
contribute to ARDS in noninjured lungs.6,7
Based on the current evidence and understanding of MV
and ARDS, it would seem reasonable to use lung protective
ventilation (Vt 68 mL/kg PBW, low plateau pressures and
positive end-expiratory pressure [PEEP]) in all patients,
whether they are at risk of ARDS or not.17 However, use of
least damaging ventilation settings is not always feasible.
Patients with airway obstruction (chronic obstructive
airway disease, asthma) who may have increased intrinsic
PEEP or patients with interstitial lung disease who have
restrictive lung disease and poor lung compliance may
require higher plateau pressures to ensure adequate gas
exchange.
Patients undergoing cardiac surgery are particularly
sensitive to lung damage due to prolonged MV, multiple
comorbidities, and pro-inflammatory cofactors such as CPB,
transfusions, and ischemia/reperfusion.8,9
Aims and objectives
The aim of our study was to test the hypothesis that tidal
volume is a predictor of mortality in the cohort of cardiothoracic critically ill patients.
Additional aims of this project were 1) to identify the
commonly used ventilatory modes and parameters in our
cardiothoracic ICU (postoperative and nonsurgical patients),
2) to identify whether certain components of lung protective
ventilation care bundles are followed by our institutions
cardiac intensivists at the onset of MV, 3) to help develop
a ventilatory guideline within our cardiac ICU and cardiac
recovery unit and integrate a ventilator bundle in checklist format in our electronic clinical information system,
and 4) to organize teaching sessions on lung protective
strategies for all ICU medical, nursing, and allied health
professionals.
Methodology
We performed a retrospective database analysis of patients
>18 years admitted to tertiary center high volume cardiothoracic ICU between 01/01/2015 and 15/08/2015 requiring MV
for 48 hours (n=189).
Exclusions were made for:
Patients who did not require invasive MV.
Patients who required strict PaCO2 control (eg, in post cardiac arrest syndrome goal directed ventilatory strategy).
416
Powered by TCPDF (www.tcpdf.org)
submit your manuscript | www.dovepress.com
Dovepress
Patients for whom ICU electronic daily charts are
unavailable.
Predictor variables in the first 24 hours extracted from
clinical information system included sequential organ failure assessment (SOFA) score at the onset of MV, ventilator
mode, Vt, respiratory rate, PEEP, FiO2, pH, PaO2, arterial
partial pressure of carbon dioxide (PaCO2), peak airway
pressure, compliance, PaO2/FiO2 ratio, albumin, bilirubin,
fluid balance, [H+], and types of surgery (cardiac/thoracic,
transplant, and nonsurgical). Outcome variables included
ICU and 90-day mortality.
This project has been reviewed and approved by the
Research and Development Unit of Papworth Hospital
NHS Foundation Trust it has no material ethical issues.
The Research and Development Unit on behalf of Papworth
Hospital NHS Foundation Trust has reviewed this project and
did not require written informed consent be obtained from
the participants, as this was a retrospective study and service
evaluation, and all data was anonymous.
Statistical analysis
Statistical software Stata/SE 13.1 for Mac was used (StataCorp, 2013, Stata Statistical Software: Release 13, StataCorp LP, College Station, TX, USA). Univariate logistic/
linear regressions identified predictor variables to include
in multivariate regressions (reduce risk of overfitting) at
P<0.20. Multiple logistic/linear regressions, adjusting for
covariates, identified independent significant predictors for
outcome variables.
Results
Overall, 129 patients were identified according to the inclusion criteria. Twenty-nine percent were female and 71% were
male. Sixty-four percent were admitted to ICU following
cardiac/thoracic or transplant surgery, 25% for nonsurgical
reasons (cardiothoracic medical pathologies) and 11% were
patients who were readmitted in the postoperative period.
Of all patients, 7% were admitted following coronary artery
bypass grafting surgery, 9% following valve replacement/
repair, 16% following combined valve and other procedure,
14% following heart and/or lung transplant, and 0.8% following video-assisted thoracoscopic surgery. All patients
included in the study were mechanically ventilated on
Siemens Servo-I ventilators. Summary statistics for initial
choice of ventilator mode are demonstrated in Table 1. Mean
SOFA score at onset of MV was 132.5 (standard deviation).
Predictor variables (in the first 24 hours) retained for
inclusion in multiple regression model: gender, type of
International Journal of General Medicine 2016:9
Dovepress
Ventilating the cardiothoracic critically ill
International Journal of General Medicine downloaded from https://www.dovepress.com/ by 192.30.84.235 on 16-Nov-2016
For personal use only.
Table 1 Summary statistics of initial ventilator mode for each
patient in sample
Ventilator mode
Patients
(N=129), n (%)
SIMV (PRVC) + pressure support
Volume control
SIMV (pressure control) + pressure support
Pressure control
PRVC
Pressure support/CPAP
SIMV (volume control) + pressure support
CMV (volume control)
57 (44)
36 (28)
11 (9)
11 (9)
10 (8)
2 (2)
1 (1)
1 (1)
Abbreviations: CMV, continuous mandatory ventilation; CPAP, continuous positive
airway pressure; PRVC, pressure regulated volume control; SIMV, synchronized
intermittent mandatory ventilation.
surgery, admission type, Vt, FiO2, PaO2, PaO2/FiO2 ratio,
PaCO2, albumin, platelet count, H+, total bilirubin, and fluid
balance. When controlling for covariates, Vt and other ventilator variables did not independently predict mortality in
our model, despite best evidence suggesting that they should
(Tables 24).
Discussion
When controlling for covariates, Vt and other ventilator
variables did not independently predict mortality in our
model, despite best evidence suggesting that they should.
Table 2 Ninety-day mortality
90-day mortality
Regression
coefficient (95% CI)
P-value
Mean PaO2/FiO2 ratio
0.0025812
(0.005, 0.010)
0.8039421
(1.375, 0.233)
0.2022619
(0.320, 0.085)
0.0744572
(0.002, 0.146)
0.0219693
(0.001, 0.043)
0.0007785
(0.00151, 0.0000376)
0.0010963
(0.002, 0.005)
0.0040282
(0.002, 0.010)
0.0822255
(0.094, 0.259)
0.4574553
(1.186, 0.271)
0.4365685
(1.546, 0.673)
0.520
Surgery type
Mean albumin (g/L)
Mean H+
Mean bilirubin
Mean fluid balance
Mean platelet count
Mean Vt (mL)
Mean PaO2 (kPa)
Mean PaCO2 (kPa)
Gender
0.006
0.001
0.044
0.039
0.039
0.579
CCA mortality
Regression coefficient
(95% CI)
P-value
Mean PaO2/FiO2 ratio
Surgery type
Mean albumin (g/L)
0.0012962 (0.012, 0.009)
2.06707 (3.15, 0.984)
0.188557 (0.324, 0.053)
0.0767531 (0.009, 0.162)
0.0233401 (0.002, 0.048)
0.0000732 (0.001, 0.0009)
0.808
0.000
0.006
0.078
0.067
0.877
0.0023714 (0.008, 0.003)
0.0026183 (0.005, 0.011)
0.0938601 (0.125, 0.312)
0.0468157 (0.930, 0.836)
0.0823749 (1.263, 1.428)
0.378
0.521
0.400
0.917
0.904
Mean H+
Mean bilirubin
Mean fluid
balance
Mean platelet count
Mean Vt (mL)
Mean PaO2 (kPa)
Mean PaCO2 (kPa)
Gender
Abbreviations: CI, confidence interval; CCA, critical care area; PaO2, partial
pressure of arterial oxygen; FiO2, fraction of inspired oxygen; PaCO2, arterial partial
pressure of carbon dioxide.
Table 4 Summary statistics of ARDS severity in sample
ARDS
severity
ICU mortality
90-day mortality
Yes (%)
No (%)
Yes (%)
No (%)
None
Mild
Moderate
Severe
23/99 (23)
44/99 (44)
27/99 (27)
5/99 (5)
12/30 (40)
8/30 (27)
10/30 (33)
0/30 (0)
18/83 (22)
36/83 (43)
24/83 (29)
5/83 (6)
17/46 (37)
16/46 (35)
13/46 (28)
0/46 (0)
Total
35/129 (27)
52/129 (40)
37/129 (29)
5/129 (4)
Abbreviations: ARDS, acute respiratory distress syndrome; ICU, intensive care unit.
Independent predictors of mortality in our study included:
type of surgery, albumin, H+, bilirubin, and fluid balance.
In particular, it is important to note that cardiac, thoracic,
and transplant surgical patients were associated with lower
mortality. This could reflect the expertise of our institution
as a cardiothoracic center in ensuring the best outcomes for
these patients. The Berlin Definition of ARDS severity10
categorizes patients on their degree of hypoxemia (mild,
moderate, and severe based on PaO2:FiO2 ratio) which should
predict mortality. However as demonstrated in Table 3, we did
not sample equally from each of these groups. As a result,
our study was not adequately powered to detect a difference
in mortality between these groups and therefore our results
are not definitive. Further study of this sample would add
the required power or use subgroup analyses to determine
all factors contributing to death.
0.214
0.361
0.218
0.441
Abbreviations: CI, confidence interval; PaO2, partial pressure of arterial oxygen;
FiO2, fraction of inspired oxygen; PaCO2, arterial partial pressure of carbon dioxide.
International Journal of General Medicine 2016:9
Table 3 CCA mortality
Acknowledgment
An abstract of this paper was presented as a poster at the Critical Care Canada Forum on 2nd November 2016 at Sheraton
Centre Toronto Hotel, Toronto, ON, Canada.
Disclosure
The authors report no conflicts of interest in this work.
submit your manuscript | www.dovepress.com
Dovepress
Powered by TCPDF (www.tcpdf.org)
417
Dovepress
Zochios et al
International Journal of General Medicine downloaded from https://www.dovepress.com/ by 192.30.84.235 on 16-Nov-2016
For personal use only.
References
1. Neto AS, Cardoso SO, Manetta JA, et al. Association between use of
lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a
meta-analysis. JAMA. 2012;308(16):16511659.
2. Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in
patients without acute lung injury at the onset of mechanical ventilation.
Crit Care Med. 2004;32(9):1817.
3. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT,
Wheeler A. Ventilation with lower tidal volumes as compared with
traditional tidal volumes for acute lung injury and the acute respiratory
distress syndrome. The acute respiratory distress syndrome network. N
Engl J Med. 2000;342(18):13011308.
4. Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A.Ventilator
settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31(7):922926.
5. Petrucci N, De Feo C. Lung protective ventilation strategy for the
acute respiratory distress syndrome. Cochrane Database Syst Rev.
2013;(2):CD003844.
6. Putensen C, Theuerkauf N, Zinserling J, Wrigge H, Pelosi P. Metaanalysis: ventilation strategies and outcomes of the acute respiratory
distress syndrome and acute lung injury. Ann Intern Med. 2009;151(8):
566576.
7. Zupancich E, Paparella D, Turani F, Munch C, Rossi A, Massaccesi S,
Ranieri VM. Mechanical ventilation affects inflammatory mediators
in patients undergoing cardiopulmonary bypass for cardiac surgery:
a randomized clinical trial. J Thorac Cardiovasc Surg. 2005;130(2):
378383.
8. Lipes J, Bojmehrani A, Lellouche F. Low tidal volume ventilation in
patients without acute respiratory distress syndrome: a paradigm shift
in mechanical ventilation. Crit Care Res Pract. 2012;2012:41686.
9. Schreiber JU, Lanc MD, de Korte M, Artmann T, Aleksic I, KrankeP.
The effect of different lung-protective strategies in patients during cardiopulmonary bypass: a meta-analysis and semiquantitative
review of randomized trials. J Cardiothorac Vasc Anesth. 2012;26(3):
448454.
10. Ranieri VM, Rubenfeld GD, Thompson BT, et al; The ARDS Definition
Task Force. Acute respiratory distress syndrome: the Berlin definition.
JAMA. 2012;307(23):25262533.
Dovepress
International Journal of General Medicine
Publish your work in this journal
The International Journal of General Medicine is an international,
peer-reviewed open-access journal that focuses on general and internal
medicine, pathogenesis, epidemiology, diagnosis, monitoring and treatment protocols. The journal is characterized by the rapid reporting of
reviews, original research and clinical studies across all disease areas.
The manuscript management system is completely online and includes
a very quick and fair peer-review system, which is all easy to use. Visit
http://www.dovepress.com/testimonials.php to read real quotes from
published authors.
Submit your manuscript here: https://www.dovepress.com/international-journal-of-general-medicine-journal
418
Powered by TCPDF (www.tcpdf.org)
submit your manuscript | www.dovepress.com
Dovepress
International Journal of General Medicine 2016:9
Você também pode gostar
- Neuro Clinical Pocket GuideDocumento334 páginasNeuro Clinical Pocket Guidesayles4174100% (2)
- Arterial Line Arterial LineDocumento13 páginasArterial Line Arterial LineLinamaria Lozano100% (1)
- Lung Mechanics and Ventilation-Lecture NotesDocumento16 páginasLung Mechanics and Ventilation-Lecture NotesCarlos Eduardo LinaresAinda não há avaliações
- Lifestyle DiseasesDocumento44 páginasLifestyle Diseaseskyro draxAinda não há avaliações
- TEMPLATE Clinical Reasoning Case Study2Documento10 páginasTEMPLATE Clinical Reasoning Case Study2Ianne MerhAinda não há avaliações
- Thoracic Injury Management Jan 08Documento39 páginasThoracic Injury Management Jan 08Uday PrabhuAinda não há avaliações
- Valvular Heart DiseaseDocumento27 páginasValvular Heart DiseaseOwen J. WieseAinda não há avaliações
- Thesis Epidural Labor Analgesia Using BupivacianeDocumento157 páginasThesis Epidural Labor Analgesia Using BupivacianeShuaib Bin Aboobacker100% (1)
- Key Nursing SkillsDocumento359 páginasKey Nursing Skillsmordanga100% (6)
- SOPDocumento16 páginasSOPjerome marquezAinda não há avaliações
- AIR Conditioner: Owner'S ManualDocumento52 páginasAIR Conditioner: Owner'S Manualashley diazAinda não há avaliações
- Underground Equipment SelectionDocumento44 páginasUnderground Equipment SelectionCherotich Silas cheboseiAinda não há avaliações
- Noncardiogenic Pulmonary EdemaDocumento12 páginasNoncardiogenic Pulmonary EdemaIrina DuceacAinda não há avaliações
- Cerebral Venous ThrombosisDocumento15 páginasCerebral Venous ThrombosisValentina RobuAinda não há avaliações
- Approach To Septic ShockDocumento16 páginasApproach To Septic ShockRaja EllysyaAinda não há avaliações
- Spinal TuberculosisDocumento46 páginasSpinal TuberculosisAbby Austero100% (1)
- Respiratory and Renal ReviewDocumento39 páginasRespiratory and Renal ReviewTony PadAinda não há avaliações
- Respiratory Failure (1) .Documento36 páginasRespiratory Failure (1) .Ibrahim HemdanAinda não há avaliações
- Post Op CardiacDocumento7 páginasPost Op CardiacsimplyputmonicAinda não há avaliações
- Chest PhysiotherapyDocumento88 páginasChest Physiotherapy私 シャーロットAinda não há avaliações
- Arterial LinesDocumento9 páginasArterial LinesRei IrincoAinda não há avaliações
- COPD Acute Management ABCDEDocumento11 páginasCOPD Acute Management ABCDESSAinda não há avaliações
- Managing Mechanical VentilationDocumento7 páginasManaging Mechanical VentilationArden QuiambaoAinda não há avaliações
- Pulmonary SequestrationDocumento15 páginasPulmonary SequestrationEmily EresumaAinda não há avaliações
- Acute Severe AsthmaDocumento5 páginasAcute Severe AsthmaRizsa Aulia DanestyAinda não há avaliações
- Dr. G.N. Prabhu Associate Professor Cardiothoracic Surgery SRM MCH & RCDocumento60 páginasDr. G.N. Prabhu Associate Professor Cardiothoracic Surgery SRM MCH & RCNithya SekarAinda não há avaliações
- Inotropic Agents: Submitted ToDocumento87 páginasInotropic Agents: Submitted Toraman kumariAinda não há avaliações
- Ventricular Assist DeviceDocumento12 páginasVentricular Assist DevicesamadonyAinda não há avaliações
- Cardiac Enzyme StudiesDocumento4 páginasCardiac Enzyme StudiesDara VinsonAinda não há avaliações
- Critical Care - Improving OutcomesDocumento81 páginasCritical Care - Improving OutcomeshimanshuAinda não há avaliações
- Use of Vasopressors and InotropesDocumento14 páginasUse of Vasopressors and InotropesEdwin VargasAinda não há avaliações
- Blue Bloaters and Pink PuffersDocumento2 páginasBlue Bloaters and Pink PuffersAlmir SaraciAinda não há avaliações
- Pneumonia Management ProtocolDocumento2 páginasPneumonia Management Protocolsky nuts100% (1)
- Interstitial Lung DiseaseDocumento26 páginasInterstitial Lung DiseaseEnimia ShyAinda não há avaliações
- Maxilofacial Trauma: Presenter: - Wisnu Adiputra (07120080072) - Nofilia Citra Candra (07120090066)Documento97 páginasMaxilofacial Trauma: Presenter: - Wisnu Adiputra (07120080072) - Nofilia Citra Candra (07120090066)Nofilia Citra CandraAinda não há avaliações
- PacemakersDocumento19 páginasPacemakersAswathy RCAinda não há avaliações
- Acuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiesDocumento16 páginasAcuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiessamuelAinda não há avaliações
- Newborn Respiratory Distress 11.28.2011Documento41 páginasNewborn Respiratory Distress 11.28.2011Emily EresumaAinda não há avaliações
- Mechanical VentilationDocumento40 páginasMechanical VentilationPratik SahooAinda não há avaliações
- Approach To Ventricular ArrhythmiasDocumento18 páginasApproach To Ventricular ArrhythmiasDavid CruzAinda não há avaliações
- Kidney TransplantDocumento11 páginasKidney TransplantPrincess Xzmae RamirezAinda não há avaliações
- Congenital Heart Disease - Cynotic AcynoticDocumento34 páginasCongenital Heart Disease - Cynotic Acynoticvruttika parmarAinda não há avaliações
- Restrictive Lung DiseaseDocumento32 páginasRestrictive Lung DiseaseSalman Khan100% (1)
- Pulmonary HTNDocumento51 páginasPulmonary HTNMuhammad HaekalAinda não há avaliações
- What Is ICU PsychosisDocumento6 páginasWhat Is ICU PsychosisAngelicaMarieRafananAinda não há avaliações
- Class Presentation ON Acute Tubular NecrosisDocumento39 páginasClass Presentation ON Acute Tubular NecrosisDeeksha RajputAinda não há avaliações
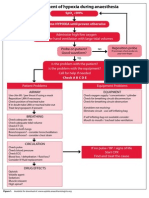
- Management of Hypoxia During AnaesthesiaDocumento5 páginasManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Blood Gas Analysis For Bedside DiagnosisDocumento6 páginasBlood Gas Analysis For Bedside DiagnosisMuhamad Wirawan AdityoAinda não há avaliações
- Adam Low - CLABSI Best Practice and BundlesDocumento34 páginasAdam Low - CLABSI Best Practice and Bundlesvera indrawatiAinda não há avaliações
- Defining Hemodynamic InstabilityDocumento9 páginasDefining Hemodynamic InstabilitynadyajondriAinda não há avaliações
- Idiopathic Pulmonary Fibrosis: Optimizing The Diagnosis and Multi-Disciplinary Decision MakingDocumento4 páginasIdiopathic Pulmonary Fibrosis: Optimizing The Diagnosis and Multi-Disciplinary Decision MakingAnna LiachenkoAinda não há avaliações
- Essential Hypertension ManagementDocumento5 páginasEssential Hypertension Managementspicychips7Ainda não há avaliações
- Cardiac AsthmaDocumento12 páginasCardiac AsthmaNeupane KsabAinda não há avaliações
- Clinical Examination of Respiratory SystemDocumento37 páginasClinical Examination of Respiratory SystemDipienshu BhatAinda não há avaliações
- Lung AuscultationDocumento62 páginasLung AuscultationOlea CroitorAinda não há avaliações
- INOTROPIC SUPPORT (Autosaved)Documento23 páginasINOTROPIC SUPPORT (Autosaved)Bindhu RaniAinda não há avaliações
- Fulminant Hepatic FailureDocumento12 páginasFulminant Hepatic Failureafghansyah arfiantoAinda não há avaliações
- Platelet DisordersDocumento12 páginasPlatelet Disordersopi nean100% (1)
- Use of Vasopressors and Inotropes - UpToDateDocumento18 páginasUse of Vasopressors and Inotropes - UpToDateAlbertoMarteAinda não há avaliações
- Clinical ECG RoundsDocumento2 páginasClinical ECG RoundsKai Siang ChanAinda não há avaliações
- Chest Trauma FinalDocumento50 páginasChest Trauma FinalAsim Siddiq VineAinda não há avaliações
- Cardiac AssessmentDocumento48 páginasCardiac AssessmentRatheesh NathAinda não há avaliações
- Surviving Sepsis Campaign 2016 Guidelines Presentation FinalDocumento60 páginasSurviving Sepsis Campaign 2016 Guidelines Presentation FinalCocosul Cocosului CocosaruluiAinda não há avaliações
- Invasive Devices On CXRDocumento1 páginaInvasive Devices On CXRLaurensia Erlina NataliaAinda não há avaliações
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Medical MneumonicsDocumento139 páginasMedical MneumonicsdrtpkAinda não há avaliações
- GINA 2022 Whats New SlidesDocumento52 páginasGINA 2022 Whats New SlidesYulia DevinaAinda não há avaliações
- 3E - Agustin, Anne Julia - Group 1 - Case 7,8Documento5 páginas3E - Agustin, Anne Julia - Group 1 - Case 7,8Anne Julia AgustinAinda não há avaliações
- Neuro Exam Ret Demo SET ADocumento2 páginasNeuro Exam Ret Demo SET AAnne Julia AgustinAinda não há avaliações
- Clinical Nutrition B Guide SY 2nd Sem 2022-2023 2Documento156 páginasClinical Nutrition B Guide SY 2nd Sem 2022-2023 2Anne Julia AgustinAinda não há avaliações
- Clinical Nutrition B Guide SY 2nd Sem 2022-2023 2Documento156 páginasClinical Nutrition B Guide SY 2nd Sem 2022-2023 2Anne Julia AgustinAinda não há avaliações
- ACAQ Crit Care Nursing CurriculumDocumento91 páginasACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- General Practice Physical Activity QuestionnaireDocumento1 páginaGeneral Practice Physical Activity QuestionnaireAnne Julia Agustin100% (1)
- Rules of A Godly WomanDocumento3 páginasRules of A Godly WomanAnne Julia AgustinAinda não há avaliações
- Management of EpilepsyDocumento41 páginasManagement of EpilepsyThilina SasankeAinda não há avaliações
- Gpaq enDocumento3 páginasGpaq engitaparamanandhiAinda não há avaliações
- Exam Cram Cheet SheetDocumento2 páginasExam Cram Cheet SheetSheila Stenson-Roberts100% (1)
- Reviewer For 2nd LEDocumento21 páginasReviewer For 2nd LEAnne Julia AgustinAinda não há avaliações
- CDH Advanced Physiology and CareDocumento9 páginasCDH Advanced Physiology and CareAnne Julia AgustinAinda não há avaliações
- Diaphragmatic-Hernia Repair and After CareDocumento4 páginasDiaphragmatic-Hernia Repair and After CareAnne Julia AgustinAinda não há avaliações
- Waiver NS4 FieldworkDocumento1 páginaWaiver NS4 FieldworkAnne Julia AgustinAinda não há avaliações
- NS4-04 Sed RocksDocumento5 páginasNS4-04 Sed RocksAnne Julia AgustinAinda não há avaliações
- 04no4 1Documento10 páginas04no4 1snipper007Ainda não há avaliações
- NY Scheme For Geo RocksDocumento2 páginasNY Scheme For Geo RocksAnne Julia AgustinAinda não há avaliações
- Attia General Surgery Review ManualDocumento158 páginasAttia General Surgery Review Manualbphage100% (2)
- Comm. 3 Reference Book PDFDocumento193 páginasComm. 3 Reference Book PDFAnne Julia AgustinAinda não há avaliações
- Cancer Predisposition in Diabetics: Risk Factors Considered For Predictive Diagnostics and Targeted Preventive MeasuresDocumento8 páginasCancer Predisposition in Diabetics: Risk Factors Considered For Predictive Diagnostics and Targeted Preventive MeasuresAnne Julia AgustinAinda não há avaliações
- NY Scheme For Geo RocksDocumento2 páginasNY Scheme For Geo RocksAnne Julia AgustinAinda não há avaliações
- N11 - OxygenationDocumento3 páginasN11 - OxygenationAnne Julia AgustinAinda não há avaliações
- Antifungal Written ReportDocumento4 páginasAntifungal Written ReportAnne Julia AgustinAinda não há avaliações
- Multiple Sclerosis - Managing A Complex Neurological DiseaseDocumento10 páginasMultiple Sclerosis - Managing A Complex Neurological DiseaseAnne Julia AgustinAinda não há avaliações
- Carved I LolDocumento3 páginasCarved I LolAnne Julia AgustinAinda não há avaliações
- Stroke PicDocumento1 páginaStroke PicAnne Julia AgustinAinda não há avaliações
- Project ReportDocumento14 páginasProject ReportNoah100% (7)
- Adaptive Reuse Architecture Documentation and Analysis 2168 9717 1000172Documento9 páginasAdaptive Reuse Architecture Documentation and Analysis 2168 9717 1000172Komal HundiaAinda não há avaliações
- Blue Modern Company Profile PresentationDocumento15 páginasBlue Modern Company Profile PresentationjaneAinda não há avaliações
- Kinder DLL Week 8Documento15 páginasKinder DLL Week 8Jainab Pula SaiyadiAinda não há avaliações
- Case 445Documento4 páginasCase 445ForomaquinasAinda não há avaliações
- Test09 Eoc Algebra2 ReducedDocumento33 páginasTest09 Eoc Algebra2 ReducedkristymadimikeAinda não há avaliações
- VavDocumento8 páginasVavkprasad_56900Ainda não há avaliações
- Esterification Oil of WintergreenDocumento8 páginasEsterification Oil of WintergreenMaria MahusayAinda não há avaliações
- Segmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewDocumento10 páginasSegmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewRainata PutraAinda não há avaliações
- Climbing FormworkDocumento4 páginasClimbing FormworkAshwin B S RaoAinda não há avaliações
- Chapter 7 - Stress - TransformationsDocumento21 páginasChapter 7 - Stress - TransformationsroselleAinda não há avaliações
- Multi Organ Dysfunction SyndromeDocumento40 páginasMulti Organ Dysfunction SyndromeDr. Jayesh PatidarAinda não há avaliações
- Arts Class: Lesson 01Documento24 páginasArts Class: Lesson 01Lianne BryAinda não há avaliações
- Minimalist KWL Graphic OrganizerDocumento2 páginasMinimalist KWL Graphic OrganizerIrish Nicole AlanoAinda não há avaliações
- Precision CatalogDocumento256 páginasPrecision CatalogImad AghilaAinda não há avaliações
- Science Magazine February 2020Documento133 páginasScience Magazine February 2020Elena González GonzálezAinda não há avaliações
- Coding Decoding Sheet - 01 1678021709186Documento9 páginasCoding Decoding Sheet - 01 1678021709186Sumit VermaAinda não há avaliações
- 988611457NK448908 Vehicle Scan ReportDocumento5 páginas988611457NK448908 Vehicle Scan ReportVictor Daniel Piñeros ZubietaAinda não há avaliações
- Statics: Vector Mechanics For EngineersDocumento39 páginasStatics: Vector Mechanics For EngineersVijay KumarAinda não há avaliações
- Ap, Lrrsisal of Roentgenograph, Ic: I SsayDocumento30 páginasAp, Lrrsisal of Roentgenograph, Ic: I SsayMindaugasStacevičiusAinda não há avaliações
- Solar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power GeneratorDocumento4 páginasSolar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power Generatorluis fernandoAinda não há avaliações
- 2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticeDocumento40 páginas2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticebbAinda não há avaliações
- Daftar PustakaDocumento3 páginasDaftar PustakaMel DaAinda não há avaliações
- Anderson, Poul - Flandry 02 - A Circus of HellsDocumento110 páginasAnderson, Poul - Flandry 02 - A Circus of Hellsgosai83Ainda não há avaliações
- Optical Scattering of Gold NanosphereDocumento24 páginasOptical Scattering of Gold NanosphereParas KumarAinda não há avaliações
- Las Tech Drafting 3Q WKDocumento13 páginasLas Tech Drafting 3Q WKClemenda TuscanoAinda não há avaliações
- Kimi No Na Wa LibropdfDocumento150 páginasKimi No Na Wa LibropdfSarangapani BorahAinda não há avaliações