Escolar Documentos
Profissional Documentos
Cultura Documentos
Diazepam Drug Study: Effects, Uses, Interactions
Enviado por
Cheezy BreadDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Diazepam Drug Study: Effects, Uses, Interactions
Enviado por
Cheezy BreadDireitos autorais:
Formatos disponíveis
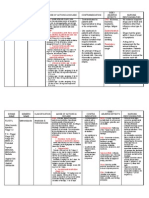
Diazepam Drug Study
Diazepam
Brand Name: Apo-Diazepam (CAN), Diastat, Diazemuls (CAN),
Diazepam Intensol, Valium, Vivol (CAN)
Pregnancy Category D, C-IV controlled substance
Drug classes: Benzodiazepine, Antianxiety agent, Antiepileptic agent,
Skeletal muscle relaxant, centrally acting
Therapeutic actions
Exact mechanisms of action not understood; acts mainly at the limbic
system and reticular formation; may act in spinal cord and
at supraspinal sites to produce skeletal muscle relaxation; potentiates the
effects of GABA, an inhibitory neurotransmitter; anxiolytic effects occur at
doses well below those necessary to cause sedation, ataxia; has little effect
on cortical function.
Indications
Management of anxiety disorders or for short-term relief of symptoms
of anxiety
Acute alcohol withdrawal; may be useful in symptomatic relief of
acute agitation, tremor, delirium tremens, hallucinosis
Muscle relaxant: adjunct for relief of reflex skeletal muscle spasm due
to local pathology (inflammation of muscles or joints) or secondary to
trauma; spasticity caused by upper motoneuron disorders (cerebral
palsy and paraplegia); athetosis, stiff-man syndrome
Treatment of tetanus (parenteral)
Antiepileptic: adjunct in status epilepticus and severe recurrent
convulsive seizures (parenteral); adjunct in convulsive disorders (oral)
Preoperative: relief of anxiety and tension and to lessen recall in
patients prior to surgical procedures, cardioversion,
and endoscopic procedures (parenteral)
Management of selected, refractory patients with epilepsy who
require intermittent use to control bouts of increased seizure activity
(rectal)
Unlabeled use: treatment of panic attacks
Contraindications
Contraindicated with hypersensitivity to benzodiazepines; psychoses,
acute narrow-angle glaucoma, shock, coma, acute alcoholic
intoxication; pregnancy (cleft lip or palate, inguinal hernia, cardiac
defects, microcephaly, pyloric stenosis when used in first trimester;
neonatal withdrawal syndrome reported in newborns); lactation.
Adverse effects
Transient, mild drowsiness initially; sedation, depression, lethargy, apathy,
fatigue, light-headedness, disorientation, restlessness, confusion, crying,
delirium, headache, slurred speech, dysarthria, stupor, rigidity,
tremor, dystonia, vertigo, euphoria, nervousness, difficulty in concentration,
vivid dreams, psychomotor retardation, extrapyramidal symptoms; mild
paradoxical excitatory reactions, during first 2 wk of treatment, visual and
auditory disturbances, diplopia, nystagmus, depressed hearing, nasal
congestion
Bradycardia, tachycardia, CV collapse, hypertension and hypotension,
palpitations, edema
Drug dependence with withdrawal syndrome when drug is discontinued
(common with abrupt discontinuation of higher dosage used for longer than
4 mo); IV diazepam: 1.7% incidence of fatalities; oral benzodiazepines
ingested alone; no well-documented fatal overdoses
Urticaria, pruritus, skin rash, dermatitis
Constipation; diarrhea, dry mouth; salivation; nausea; anorexia; vomiting;
difficulty in swallowing; gastric disorders; elevations of blood enzymes--LDH,
alkaline phosphatase, AST, ALT; hepatic dysfunction; jaundice
Incontinence, urinary retention, changes in libido, menstrual irregularities
Decreased hematocrit, blood dyscrasias
Phlebitis and thrombosis at IV injection sites, hiccups, fever,
diaphoresis, paresthesias, muscular disturbances, gynecomastia; pain,
burning, and redness after IM injection
Drug Interactions:
Increased CNS depression with alcohol, omeprazole
Increased pharmacologic effects of diazepam if combined
with cimetidine, disulfiram, hormonal contraceptives
Decreased effects of diazepam with theophyllines, ranitidine
Nursing considerations
Do not administer intra-arterially; may produce arteriospasm,
gangrene.
Change from IV therapy to oral therapy as soon as possible.
Do not use small veins (dorsum of hand or wrist) for IV injection.
Reduce dose of narcotic analgesics with IV diazepam; dose should be
reduced by at least one-third or eliminated.
Carefully monitor P, BP, respiration during IV administration.
Maintain patients receiving parenteral benzodiazepines in bed for 3
hr; do not permit ambulatory patients to operate a vehicle following an
injection.
Monitor EEG in patients treated for status epilepticus; seizures may
recur after initial control, presumably because of short duration of drug
effect.
Monitor liver and kidney function, CBC during long-term therapy.
Taper dosage gradually after long-term therapy, especially in epileptic
patients.
Arrange for epileptic patients to wear medical alert ID indicating that
they are epileptics taking this medication.
Discuss risk of fetal abnormalities with patients desiring to become
pregnant.
Você também pode gostar
- NaloxoneDocumento3 páginasNaloxoneTracyAinda não há avaliações
- Tetracycline HCl study drugDocumento4 páginasTetracycline HCl study drugCheezy BreadAinda não há avaliações
- Piroxicam Drug Study: NSAIDs Reduce InflammationTITLE Ciprofloxacin Antibiotic Treats Bacterial Infections TITLE Salbutamol Nebulizer Relieves Asthma SymptomsDocumento3 páginasPiroxicam Drug Study: NSAIDs Reduce InflammationTITLE Ciprofloxacin Antibiotic Treats Bacterial Infections TITLE Salbutamol Nebulizer Relieves Asthma SymptomsBheiatriz de VeraAinda não há avaliações
- Drug Study: Nursing DepartmentDocumento1 páginaDrug Study: Nursing Departmentgiselle chloe100% (1)
- Gentamicin Pedia Drug StudyDocumento3 páginasGentamicin Pedia Drug StudyGong AllenaAinda não há avaliações
- Dextromethorphan HydrobromideDocumento2 páginasDextromethorphan Hydrobromideapi-3797941Ainda não há avaliações
- DemerolDocumento1 páginaDemerolCassie100% (1)
- Drug Study AminophyllineDocumento1 páginaDrug Study Aminophyllinejunie100% (3)
- Nursing responsibilities for bleomycin administrationDocumento1 páginaNursing responsibilities for bleomycin administrationkyawAinda não há avaliações
- ZonisamideDocumento2 páginasZonisamideRo-anne AkuAinda não há avaliações
- Drug Study - Tamiflu, FlagylDocumento2 páginasDrug Study - Tamiflu, Flagylmark_gain100% (1)
- Atracurium BesylateDocumento4 páginasAtracurium BesylateStill DollAinda não há avaliações
- Fluconazole Dose Indications Side Effects Nursing TeachingDocumento2 páginasFluconazole Dose Indications Side Effects Nursing Teachingryan100% (1)
- Beclomethasone Dipropionate (Drug Study)Documento2 páginasBeclomethasone Dipropionate (Drug Study)Franz.thenurse6888100% (1)
- Effects of Midazolam and Diazepam drug studyDocumento10 páginasEffects of Midazolam and Diazepam drug studyAbie Jewel Joy Roque100% (1)
- BetamethasoneDocumento3 páginasBetamethasoneMichael KuzbytAinda não há avaliações
- MIDAZOLAM DRUG STUDYDocumento5 páginasMIDAZOLAM DRUG STUDYShara Lailanie A. AzisAinda não há avaliações
- Brand Name: Bactrim Generic Name: Sulfamethoxazole, Trimethoprim, Co-Trimoxazole Drug ClassificationDocumento2 páginasBrand Name: Bactrim Generic Name: Sulfamethoxazole, Trimethoprim, Co-Trimoxazole Drug Classificationianecunar100% (2)
- Terbutaline SulfateDocumento2 páginasTerbutaline SulfateRhoellet VenzonAinda não há avaliações
- Metronidazole drug information summaryDocumento4 páginasMetronidazole drug information summaryKaloy AnneAinda não há avaliações
- Drug StudyDocumento9 páginasDrug StudyJonica CamposAinda não há avaliações
- AeknilDocumento2 páginasAekniljaycey24Ainda não há avaliações
- Drug StudyDocumento6 páginasDrug StudyArdrina SappariAinda não há avaliações
- Generic Name: Brand Name:: ClassificationsDocumento2 páginasGeneric Name: Brand Name:: ClassificationsbillyktoubattsAinda não há avaliações
- DiphenhydramineDocumento10 páginasDiphenhydramineFebry Dian SinagaAinda não há avaliações
- StreptomycinDocumento1 páginaStreptomycinDemilyn Fat100% (2)
- Nalbuphine (Nubain)Documento2 páginasNalbuphine (Nubain)Adrianne Bazo100% (1)
- NeostigmineDocumento4 páginasNeostigmineDonna Lyn B. DizonAinda não há avaliações
- Lansoprazole Drug Study SummaryDocumento2 páginasLansoprazole Drug Study SummaryGeorley Lobrido100% (1)
- Drug Study Bsn3aDocumento3 páginasDrug Study Bsn3aEmuelle GanAinda não há avaliações
- 4th Rot Drug StudyDocumento3 páginas4th Rot Drug StudyAaron GarciaAinda não há avaliações
- Drug StudyDocumento8 páginasDrug StudyAnne Lorraine RodriguezAinda não há avaliações
- Oxymetazoline 2Documento8 páginasOxymetazoline 2Febry Dian SinagaAinda não há avaliações
- Diazepam (Valium) Drug StudyDocumento1 páginaDiazepam (Valium) Drug StudyEmika Dizon100% (7)
- Drug Classification Action of Drug Indication and Contraindication Side Effect Nursing ConsiderationDocumento2 páginasDrug Classification Action of Drug Indication and Contraindication Side Effect Nursing ConsiderationDanica Kate GalleonAinda não há avaliações
- OfloxacinDocumento2 páginasOfloxacinCarla Arciaga100% (1)
- Drug Study AmpicillinDocumento6 páginasDrug Study AmpicillinDgjj Compuiter100% (1)
- Ofloxacin Drug StudyDocumento4 páginasOfloxacin Drug StudyMikko Anthony Pingol Alarcon100% (1)
- Fentanyl Citrate Drug StudyDocumento1 páginaFentanyl Citrate Drug StudyArthur Christopher CorpuzAinda não há avaliações
- Cefprozil (Drug Study)Documento2 páginasCefprozil (Drug Study)Franz.thenurse6888Ainda não há avaliações
- Valium Drug AnalysisDocumento1 páginaValium Drug AnalysisFerdinand Sherwin MorataAinda não há avaliações
- Generic Name:: Drug Name Mechanism of Action Indications Contraindi-Cation Adverse Effects Nursing ResponsibilitiesDocumento1 páginaGeneric Name:: Drug Name Mechanism of Action Indications Contraindi-Cation Adverse Effects Nursing ResponsibilitiesmaemalabonAinda não há avaliações
- AtracuriumDocumento2 páginasAtracuriumFederico Andales50% (2)
- Drug Study CardinalDocumento21 páginasDrug Study CardinalDrei LanuzoAinda não há avaliações
- Drug Study MethotrexateDocumento1 páginaDrug Study MethotrexatekyawAinda não há avaliações
- Chlorpheniramine MaleateDocumento17 páginasChlorpheniramine MaleateMaria Abegail Gomez100% (1)
- ORDocumento7 páginasORMay EvelynAinda não há avaliações
- Phenergan (Promethazine)Documento1 páginaPhenergan (Promethazine)E100% (1)
- Clomid Drug StudyDocumento3 páginasClomid Drug StudySheen Ivashkov-BelikovAinda não há avaliações
- Diazepam Medication Guide: Uses, Side Effects and Nursing CareDocumento2 páginasDiazepam Medication Guide: Uses, Side Effects and Nursing CaregoyaAinda não há avaliações
- DRUGSTUDY3DIAZEDocumento1 páginaDRUGSTUDY3DIAZEEryn_Casaclang_6640Ainda não há avaliações
- Drug StudyDocumento4 páginasDrug StudySytrose MoralesAinda não há avaliações
- Anticonvulsants NotesDocumento19 páginasAnticonvulsants NotesPIRENAAinda não há avaliações
- CNS: Drowsiness, Fatigue, Ataxia, Confusion, Paradoxic RageDocumento4 páginasCNS: Drowsiness, Fatigue, Ataxia, Confusion, Paradoxic RageYanna N. CuakiAinda não há avaliações
- Drug PresentationDocumento32 páginasDrug PresentationManisha ShakyaAinda não há avaliações
- Drug Study 2Documento8 páginasDrug Study 2rey_tengAinda não há avaliações
- Dosage and effects of midazolam hydrochlorideDocumento3 páginasDosage and effects of midazolam hydrochlorideEricka Jordan AberinAinda não há avaliações
- Drug Study ShenDocumento12 páginasDrug Study ShenLass KazeAinda não há avaliações
- Drug Study On DiazepamDocumento1 páginaDrug Study On DiazepamMaya Acosta BiruarAinda não há avaliações
- Brand Name: Intravenous (IV)Documento4 páginasBrand Name: Intravenous (IV)Ian Jeff Landingin DumayasAinda não há avaliações
- Nifedepine Drug StudyDocumento2 páginasNifedepine Drug StudyCheezy BreadAinda não há avaliações
- Nystatin Drug StudyDocumento2 páginasNystatin Drug StudyCheezy BreadAinda não há avaliações
- Nitroglycerine Drug StudyDocumento3 páginasNitroglycerine Drug StudyCheezy BreadAinda não há avaliações
- Benadryl Drug StudyDocumento3 páginasBenadryl Drug StudyCheezy BreadAinda não há avaliações
- Benicar Drug StudyDocumento2 páginasBenicar Drug StudyCheezy BreadAinda não há avaliações
- Lansoprazole Drug StudyDocumento2 páginasLansoprazole Drug StudyCheezy Bread100% (1)
- Benadryl Drug StudyDocumento3 páginasBenadryl Drug StudyCheezy BreadAinda não há avaliações
- Ofloxacin Drug StudyDocumento2 páginasOfloxacin Drug StudyCheezy Bread100% (1)
- Risperidone Drug StudyDocumento2 páginasRisperidone Drug StudyCheezy Bread100% (1)
- Penicillin Drug StudyDocumento2 páginasPenicillin Drug StudyCheezy BreadAinda não há avaliações
- Phenobarbital Drug StudyDocumento3 páginasPhenobarbital Drug StudyCheezy Bread100% (1)
- Phenytoin Drug StudyDocumento3 páginasPhenytoin Drug StudyCheezy Bread100% (1)
- Potassium Salts Drug StudyDocumento2 páginasPotassium Salts Drug StudyCheezy BreadAinda não há avaliações
- Ramipril Drug StudyDocumento3 páginasRamipril Drug StudyCheezy Bread0% (1)
- Prednisone Drug StudyDocumento2 páginasPrednisone Drug StudyCheezy Bread67% (3)
- Ranitidine Drug StudyDocumento2 páginasRanitidine Drug StudyCheezy BreadAinda não há avaliações
- Warfarin Drug StudyDocumento3 páginasWarfarin Drug StudyCheezy Bread100% (2)
- Simvastatin Drug StudyDocumento3 páginasSimvastatin Drug StudyCheezy BreadAinda não há avaliações
- Theophylline Drug StudyDocumento3 páginasTheophylline Drug StudyCheezy Bread100% (5)
- Simvastatin Drug StudyDocumento3 páginasSimvastatin Drug StudyCheezy BreadAinda não há avaliações
- Warfarin Drug StudyDocumento3 páginasWarfarin Drug StudyCheezy Bread100% (2)
- Tramadol HCL Drug StudyDocumento2 páginasTramadol HCL Drug StudyCheezy BreadAinda não há avaliações
- CVADocumento116 páginasCVAkathy100% (1)
- Verapamil HCL Drug StudyDocumento3 páginasVerapamil HCL Drug StudyCheezy Bread100% (1)
- Cerebrovascular AccidentDocumento108 páginasCerebrovascular AccidentCarl Elexer Cuyugan Ano94% (16)
- Losartan Drug StudyDocumento2 páginasLosartan Drug StudyCheezy Bread100% (1)
- Cytotoxins Pose Risks for Healthcare WorkersDocumento2 páginasCytotoxins Pose Risks for Healthcare WorkersMaria Nesen NuezAinda não há avaliações
- Atopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)Documento289 páginasAtopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)NguyenDinh NinhAinda não há avaliações
- FIKY NISWATI YUSLIHAH P17250193025 (Morning Breafing)Documento3 páginasFIKY NISWATI YUSLIHAH P17250193025 (Morning Breafing)Fiky NiswatiAinda não há avaliações
- Classification of FracturesDocumento26 páginasClassification of FracturesHoney May Rollan VicenteAinda não há avaliações
- National Mental Health ProgrammeDocumento9 páginasNational Mental Health ProgrammeSharika sasi0% (1)
- Daftar Pustaka AsihDocumento5 páginasDaftar Pustaka AsihKhansaAinda não há avaliações
- Changes in Central Corneal Thickness in Healthy Pregnant Women-A Clinical StudyDocumento3 páginasChanges in Central Corneal Thickness in Healthy Pregnant Women-A Clinical StudyIJAR JOURNALAinda não há avaliações
- Cns 765 Final Case StudyDocumento10 páginasCns 765 Final Case Studyapi-581708536Ainda não há avaliações
- Ethical Counselling and Medical Decision-Making in The Era of Personalised Medicine A Practice-Oriented Guide PDFDocumento129 páginasEthical Counselling and Medical Decision-Making in The Era of Personalised Medicine A Practice-Oriented Guide PDFEddyYuristoAinda não há avaliações
- Lazy Leucocyte SyndromeDocumento2 páginasLazy Leucocyte SyndromeDragos BourosAinda não há avaliações
- Update On Importance of Diet in Gout: ReviewDocumento6 páginasUpdate On Importance of Diet in Gout: ReviewIoana IonAinda não há avaliações
- Lincomycin: Drug Information: ALERT: US Boxed WarningDocumento12 páginasLincomycin: Drug Information: ALERT: US Boxed WarningsadiaAinda não há avaliações
- Dr. Ayesha Latif's Guide to Airway ManagementDocumento32 páginasDr. Ayesha Latif's Guide to Airway ManagementAyesha LatifAinda não há avaliações
- Drummond Methods For The Economic Evaluation of Health Care Programmes PDFDocumento461 páginasDrummond Methods For The Economic Evaluation of Health Care Programmes PDFGerman Camilo Viracacha Lopez80% (10)
- Community Pharmacy Management CH 3 Prescription and Prescription Handlind NotesDocumento9 páginasCommunity Pharmacy Management CH 3 Prescription and Prescription Handlind Notesi.bhoomi12Ainda não há avaliações
- Goals and principles of community health nursingDocumento4 páginasGoals and principles of community health nursingNoemiAinda não há avaliações
- Electrocardiography for Healthcare ProfessionalsDocumento6 páginasElectrocardiography for Healthcare ProfessionalsOasisBogo Med0% (1)
- Prasugrel and RosuvastatinDocumento7 páginasPrasugrel and RosuvastatinMohammad Shahbaz AlamAinda não há avaliações
- Organization of NICU ServicesDocumento45 páginasOrganization of NICU ServicesMonika Bagchi84% (64)
- 2018 Conference AbstractsDocumento155 páginas2018 Conference AbstractsBanin AbadiAinda não há avaliações
- List of Books For PurchaseDocumento23 páginasList of Books For Purchasepavans25Ainda não há avaliações
- Krok 2 2002-2003 TherapyDocumento41 páginasKrok 2 2002-2003 TherapyAli ZeeshanAinda não há avaliações
- Hypnotherapy Scripts 6 Steve G Jones Ebook PDFDocumento66 páginasHypnotherapy Scripts 6 Steve G Jones Ebook PDFjohannes2212100% (10)
- Psychiatric Assessment ToolDocumento53 páginasPsychiatric Assessment ToolLori100% (4)
- Case Digest 01Documento4 páginasCase Digest 01Jazz SolisAinda não há avaliações
- CV April Geo Savulescu WordDocumento9 páginasCV April Geo Savulescu Wordmiagheorghe25Ainda não há avaliações
- Evidence Based Practice in Nursing BinuDocumento51 páginasEvidence Based Practice in Nursing BinuBinu Joshva100% (2)
- Four Humors Theory in Unani MedicineDocumento4 páginasFour Humors Theory in Unani MedicineJoko RinantoAinda não há avaliações
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementDocumento10 páginasMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahAinda não há avaliações
- Surgery and Surgical NursingDocumento193 páginasSurgery and Surgical NursingFan Eli100% (4)