Escolar Documentos
Profissional Documentos
Cultura Documentos
Journal Cystic Abdominal Masses PDF
Enviado por
Halida Batik AlunaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Journal Cystic Abdominal Masses PDF
Enviado por
Halida Batik AlunaDireitos autorais:
Formatos disponíveis
Residents Section Pat tern of the Month
Ranganath et al.
Abdominal Masses in Children
Residents Section
Pattern of the Month
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Residents
Focal Cystic Abdominal
inRadiology Masses in Pediatric Patients
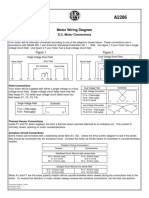
Shashi H. Ranganath1,2 TABLE 1: Focal Cystic Abdominal
F
ocal abdominal cystic masses are
Edward Y. Lee1 common in pediatric patients. Af- Masses in Children
Ronald L. Eisenberg2 fected patients present with vari- Solid organ of origin
ous symptoms and physical find- Hepatobiliary system
Ranganath SH, Lee EY, Eisenberg RL ings depending on size, location, and mass Hepatic cyst
effect on the adjacent abdominal structures.
Hepatic abscess
The symptoms in these patients can be ab-
dominal pain, early satiety, bowel obstruction, Hydatid infection
or fever if the underlying cause of the mass is Mesenchymal hamartoma
infection. The physical signs are abdominal Choledochal cyst
distention or a palpable mass. Kidney
The sites of origin of focal cystic masses are Hydronephrosis
from various abdominal organs and mesentery in
Ureteropelvic junction obstruction
pediatric patients (Table 1). For the purpose of
evaluation and diagnosis, focal abdominal cystic Ureterovesicular junction obstruction
masses in children can be divided into three cat- Ureteropelvic duplication (Weigert-
egories on the basis of their region of origin: Meyer rule)
solid organs (liver, kidney, pancreas, spleen, Prune belly syndrome
and adrenal gland), mesentery, and bowel. Renal abscess
Although ultrasound is the imaging modality Multicystic dysplastic kidney
of choice for initial evaluation of focal abdomi-
Multilocular cystic nephroma
nal cystic masses, CT or MRI is often subse-
Cystic Wilms tumor
quently obtained for confirmation and further
characterization of focal abdominal cystic Rhabdoid tumor
masses in pediatric patients. Understanding the Pancreas
Keywords: abdominal cystic masses, children, pediatric characteristic imaging findings of focal cystic Pancreatic pseudocyst
abdominal masses that can be symptomatic or Pancreatic cystadenoma
DOI:10.2214/AJR.11.6642
incidental findings in pediatric patients can im-
Spleen
Received February 3, 2011; accepted after revision prove pediatric patient care by guiding the next
Splenic cyst
November 7, 2011. appropriate step in management.
Splenic abscess
1
Department of Radiology, Childrens Hospital Boston, Solid Organ of Origin Vascular malformation
Harvard Medical School, Boston, MA.
Hepatobiliary System Adrenal gland
2
Department of Radiology, Beth Israel Deaconess Hepatic cystHepatic cysts in pediatric pa- Adrenal hemorrhage
Medical Center, Harvard Medical School, 330 Brookline tients can be congenital or acquired. Whereas
Ave, Boston, MA 02215. Address correspondence to
Cystic neuroblastoma
congenital hepatic cysts occur when an intra-
R. L. Eisenberg (rleisenb@bidmc.harvard.edu).
hepatic biliary duct fails to involute, acquired Mesentery
hepatic cysts result from trauma or infection in Mesenteric cyst/lymphatic malformation
WEB
This is a Web exclusive article. the pediatric population. On histology, hepatic CSF collection (CSFoma)
cysts consist of a layer of simple cuboidal epi- Abscess
AJR 2012; 199:W1W16 thelium. In pediatric patients, hepatic cysts are Cystic teratoma
0361803X/12/1991W1
usually benign and do not require follow-up
Bowel
imaging evaluation. On ultrasound, a hepatic
American Roentgen Ray Society cyst is an anechoic round or oval lesion with Duplication cyst
AJR:199, July 2012 W1
Ranganath et al.
increased posterior through-transmission and
without mural nodularity.
Although subsequent imaging study is not
necessary for further evaluation of hepatic
cysts once the diagnosis is made with ultra-
sound, hepatic cysts also can be incidental
findings on cross-sectional imaging studies,
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
such as CT or MRI, obtained for other indica-
tions. On CT and MRI with contrast adminis-
tration, a hepatic cyst is a nonenhancing well-
defined homogeneous water-attenuation le-
sion with an imperceptible wall (Fig. 1). Ad-
ministration of IV contrast material is helpful
for differentiating simple hepatic cysts from
other low attenuation on CT or signal inten-
sity on hepatic lesions found on T1-weighted
Fig. 1Hepatic cyst. Enhanced axial CT image
imaging. Hepatic cysts are typically solitary of 1-year-old boy who presented with increasing
but can be multiple. The presence of more abdominal distention shows nonenhancing well-
than 10 hepatic cysts in a child should sug- defined homogeneous water-attenuation mass
gest the possibility of associated polycystic (arrows) with imperceptible wall.
kidney disease. Hepatic cysts in children can
be complicated by hemorrhage or infection, but simple cysts without complication require no
further imaging follow-up or treatment.
Hepatic abscessA hepatic abscess is a localized collection of pus in the hepatic parenchyma,
which can result from bacterial, fungal, amebic, or parasitic infection. On ultrasound, the echoge-
nicity and margins of hepatic abscess vary depending on the stage of the infectious process. At the
early stage of the infectious process, hepatic abscesses are hypoechoic to anechoic lesions with
ill-defined borders. They become more echogenic with well-defined margins as the abscesses be-
come more organized at the later stage of the infectious process (Fig. 2A). Hepatic abscesses may
also contain internal air-fluid levels, septations, gas, or debris. Although diagnosis of hepatic ab-
scess can be obtained with ultrasound in pediatric patients who present with typical clinical signs
and symptoms, such as fever, elevated WBC count, and upper abdominal pain, a cross-sectional
imaging study, such as CT, may be necessary for confirmation and assessment of extent of disease,
particularly before interventional procedure, such as a percutaneous drainage catheter placement.
On CT, a hepatic abscess typically appears as a complex fluid collection, which is hypodense
centrally and shows peripheral rim enhancement (Fig. 2B). The best diagnostic clue for a pyogenic
A B
Fig. 2Hepatic abscess in 13-year-old boy with right upper quadrant pain, fever, and elevated liver function
tests. Culture of drainage fluid was positive for Escherichia coli.
A, Transverse ultrasound image of liver shows large cystic mass (arrows) with internal mobile echogenic debris (D).
B, Contrast-enhanced axial CT image shows complex fluid collection (arrows) with internal septations of
varying thickness in right hepatic lobe.
W2 AJR:199, July 2012
Abdominal Masses in Children
hepatic abscess is the cluster sign, in which
a group of small pyogenic abscesses coalesc-
es into a single large cavity that often has in-
ternal septations (Fig. 2B). Although small
hepatic abscesses may be treated with antibi-
otics alone, a large hepatic abscess (> 5 cm)
typically requires percutaneous catheter or
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
surgical drainage.
Hydatid infectionHydatid disease is
caused by infection with Echinococcus tape-
worm (E. granulosus or E. multilocularis).
E. granulosus is the most common form of
hydatid disease in humans, and the liver is
the primary site of infection. Hepatic hydatid
infection is characterized by a large well-
defined cystic hepatic mass with multiple pe-
Fig. 3Hydatid infection in 4-year-old boy with
fever, chills, and right upper quadrant pain. Serology ripheral daughter cysts. Daughter cysts can
cultures were positive for Echinococcus granulosus float freely within the mother cyst, and a
infection. Contrast-enhanced axial CT image shows change in their position with alterations in
well-defined cystic mass with several internal
endocyst membranes (arrows). (Courtesy of Ali
patient position can confirm the diagnosis of
Yikilmaz) hepatic hydatid infection. Hydatid cysts are
typically large, averaging 5 cm in size, and
they can potentially grow 23 cm annually. These lesions may appear as simple cysts but
sometimes contain endocyst membranes (Fig. 3). CT is helpful for evaluation of the dense
peripheral calcification of a hydatid cyst, which is usually seen during the healing phase of
echinococcal hepatic infection.
Mesenchymal hamartomaHepatic mesenchymal hamartoma is a benign hamartomatous
growth of mesenchymal tissue in the liver of unknown cause. It occurs in infants and young
children less than 2 years old. Histopathologically, mesenchymal hamartoma of the liver is
characterized by the admixture of epithelial structures in a loose connective stroma with fluid
accumulation suggestive of lymphangiomatous channels. Ultrasound frequently shows a com-
plex cystic mass containing both cystic and solid components (Fig. 4A). The CT features of
hepatic mesenchymal hamartoma depend on the amount of stromal tissue, which shows con-
trast enhancement whereas the cystic component does not enhance (Fig. 4B). Although there
are reported cases of spontaneous regression of mesenchymal hamartomas with conservative
management in children, surgical resection is usually the preferred choice of management
A B
Fig. 4Hepatic mesenchymal hamartoma in 15-month-old girl with progressively increasing abdominal
distention and palpable right upper quadrant mass.
A, Transverse ultrasound image of liver shows large mass with areas of cystic (C) and solid (arrows)
components.
B, Contrast-enhanced axial CT image of liver shows large mass with multiple cysts (C) of variable size and solid
components (arrows).
AJR:199, July 2012 W3
Ranganath et al.
because an increased risk of malignancy and, particularly in symptomatic patients, mass effect
from large lesions.
Choledochal cystCholedochal cysts are a spectrum of congenital developmental abnor-
malities of the biliary system in which there is fusiform dilatation of the extrahepatic and
intrahepatic bile ducts. The Todani classification of choledochal cysts is as follows:
Type 1: Segmental or diffuse fusiform dilatation of the common bile duct (most frequent)
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Type 2: Diverticulum of an extrahepatic duct
Type 3: Choledochocele
Type IVa: Multiple extrahepatic bile duct cysts with intrahepatic biliary involvement
Type IVb: Multiple extrahepatic bile duct cysts alone
Type 5: Cystic dilatation of the intrahepatic bile ducts (Caroli disease)
Pediatric patients with choledochal cysts typically present with jaundice, abdominal pain,
and a mass. Ultrasound and MRI are the two best imaging modalities to detect and character-
ize choledochal malformations in children. MRI using an MRCP protocol with thick-slab
T2-weighted turbo spin-echo (TSE) and HASTE in the coronal, coronal oblique, and axial
planes is the MRI protocol for evaluating choledochal cysts. The findings can show a chole-
dochal cyst that is separate from the gallbladder but communicates with the biliary ducts and
shows abrupt changes in caliber at the junction between the dilated segment and normal ducts
(Fig. 5). Dilatation of multiple intrahepatic bile ducts is typically seen in Caroli disease (Fig.
6). Typical complications of choledochal cysts include infection, stone formation, and bile
duct carcinomas. The current treatment of choice is surgical resection.
Kidney
HydronephrosisHydronephrosis, characterized by a dilated renal pelvis that communi-
cates with dilated calyces, is the most frequent abdominal mass in neonates and infants. Im-
A B
Fig. 5Choledochal cyst in 9-year-old boy who
presented with epigastric mass and jaundice.
A, Transverse ultrasound image of liver in region of
porta hepatis shows large fusiform dilatation of bile
duct (C). Also noted is adjacent gallbladder (GB).
B, Contrast-enhanced axial T1-weighted MR image
shows nonenhancing large mass (C) in region of
porta hepatis with mass effect on adjacent liver
parenchyma. Also noted is adjacent gallbladder (GB).
C, Coronal MRCP image shows large cystic mass (C)
corresponding well with findings seen on ultrasound
image in A).
C
W4 AJR:199, July 2012
Abdominal Masses in Children
Fig. 6Caroli disease in 9-month-old girl who
presented with increasing abdominal distention and
vomiting.
A, Transverse ultrasound image of liver shows
multiple cystic dilatations of intrahepatic bile ducts
(arrows).
B, Contrast-enhanced axial CT image shows
multiple areas of low-attenuation cystic dilatation of
intrahepatic bile ducts (arrows). Also noted is ascites.
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
C, Axial T2-weighted image of liver shows cystic
dilatation of multiple intrahepatic bile ducts (arrows).
B C
aging evaluation plays an important role by differentiating a marked hydronephrosis that may
mimic a true intrarenal cystic mass. In the pediatric population, the three most frequent
causes of hydronephrosis are ureteropelvic junction (UPJ) obstruction, ureterovesicular junc-
tion obstruction, and renal duplication. Additionally, patients with prune belly syndrome can
also present with bilateral varying degrees of hydronephrosis and hydroureters.
UPJ obstruction is the most frequent cause of hydronephrosis in the pediatric population.
UPJ obstruction typically produces severe hydronephrosis, which ends abruptly at the UPJ
and is associated with a normal caliber of the downstream ureter (Fig. 7). In severe cases of
UPJ obstruction, the renal pelvis is disproportionately enlarged compared with the calyces.
Theoretic causes for UPJ obstruction include abnormal smooth muscle arrangement of the
proximal ureter that impairs distensibility, abnormal innervation of the proximal ureter im-
pairing peristalsis, and a crossing vessel or fibrous scar at the UPJ. UPJ obstruction can be
evaluated with ultrasound and 99mTc-MAG3 (mercaptoacetyltriglycine) renography. Ultra-
sound can show structural dilatation of the renal collecting system, whereas 99mTc-MAG3
renography provides functional information of renal excretion in patients with UPJ obstruc-
tion. After injection of 99mTc-MAG3, sequential images of the kidney are obtained. In cases
of UPJ obstruction, there is no drainage from the dilated renal collecting system into ureter
and bladder despite hydration and diuretic washout. The current treatment of choice for UPJ
obstruction is pyeloplasty to resect the narrowed segment at the UPJ or to reroute the crossing
vessel. In pediatric patients with UPJ obstruction, pyeloplasty is indicated when there is persis-
tent or worsening renal collecting system obstruction or deteriorating renal function on serial
follow-up studies, such as ultrasound and 99mTc-MAG3 renography.
Another cause of hydronephrosis in pediatric patients is ureterovesicular junction obstruction.
Megaureter is the most frequent type of ureterovesicular junction obstruction, in which the renal
collecting system and ureter are dilated because of a functional aperistalsis of the distal ureter at the
juxtavesical ureteral segment. Other less frequent causes of ureterovesicular junction obstruction
include ureterocele and distal ureteral stricture. The amount of hydroureteronephrosis depends
AJR:199, July 2012 W5
Ranganath et al.
on the degree of obstruction. Ultrasound and
voiding cystourethrography (VCUG) are the
two complementary imaging modalities for di-
agnosing ureterovesicular junction obstruction
in pediatric patients. Ultrasound shows dilata-
tion of the renal collecting system and ureter,
and VCUG shows no vesicoureteral reflux.
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Duplication of the collecting system of the
kidney is characterized by the presence of
two separate pelvocaliceal collecting sys-
tems in one kidney. Two draining ureters
may join above the bladder (partial duplica-
tion) or insert into the bladder separately
(complete duplication). The ureter draining
the upper pole tends to insert in the bladder
inferior and medial to the ureter draining the
Fig. 7Newborn girl with prenatal diagnosis of
lower pole (Weigert-Meyer rule). The upper ureteropelvic junction obstruction. Longitudinal
pole ureter, which develops later than the ultrasound image of right kidney shows
lower pole ureter with a normal anatomic lo- marked hydronephrosis. Renal pelvis (RP) is
cation of insertion into the bladder, is often disproportionately enlarged compared with calyces
(C). Left kidney was normal and there was no
ectopic and associated with ureterocele. Al- dilatation of ureters.
though the dysplastic upper pole collecting
system tends to distend, the lower pole collecting system tends to have vesicoureteral reflux.
On ultrasound, a band of renal cortex crossing the medullary portion of the kidney, which
separates the upper and lower pole collecting systems, is typically seen (Fig. 8). There may
be associated hydronephrosis, especially if there is obstruction (Fig. 8). Chronic obstruction,
infection, and scarring in children with untreated renal duplication may lead to long-term
complications, such as hypertension and renal insufficiency.
The prune belly syndrome is a congenital disorder of the urinary system, characterized by a
triad of hypoplastic or absent abdominal wall musculature, urinary tract anomalies, and cryptor-
chidism. The incidence of the prune belly syndrome is approximately one in 40,000 births and
occurs almost exclusively in male infants (97%). Although the underlying cause of the prune
belly syndrome is unknown, high-grade urethral obstruction from a posterior urethral valve or
urethral atresia, a primary defect in the mesoblast, and a complex chromosomal mutation have
been implicated. Affected patients typically present with bilateral varying degrees of hydrone-
phrosis and hypoperistaltic, tortuous hydroureters (Fig. 9). Other less frequent findings in pa-
tients with the prune belly syndrome include a dilated posterior urethra or prostatic utricle.
A B
Fig. 8Ureteropelvic duplication in 19-day-old girl with prenatal diagnosis of hydronephrosis and duplex kidney.
A, Longitudinal ultrasound image of right kidney shows markedly dilated upper pole (UP) moiety and mildly dilated
lower pole (LP) moiety. Dilated upper pole ureter (UU) and lower pole ureter (LU) are also seen. Upper pole and
lower pole collecting systems are separated by band of renal cortex (arrow).
B, Longitudinal ultrasound image of bladder (BL) shows upper pole ureter terminating in bladder as ureterocele (UC).
W6 AJR:199, July 2012
Abdominal Masses in Children
Renal abscessRenal abscess is character-
ized by a collection of pus related to suppura-
tive necrosis in the kidney. Most renal ab-
scesses are the result of inadequately treated
renal infection that ultimately liquefies. Less
frequently, renal abscesses can occur from the
direct spread of an infectious process from
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
other adjacent organs, trauma, or surgery. Im-
munocompromised pediatric patients are at
risk for developing renal abscesses, similar to
adult patients. Imaging characteristics of renal
abscess are similar to those seen in other or-
gans, with ultrasound showing an avascular
lesion of varying echogenicity and wall thick-
ening (Fig. 10A). Renal abscess may be asso-
ciated with low-level internal echoes that
Fig. 9Prune belly syndrome in 1-day-old boy with
prenatal diagnosis of bilateral hydronephrosis and move with changes in patient position, dirty
oligohydramnios. Transverse ultrasound image of posterior shadowing characteristic of internal
left kidney shows marked hydronephrosis (HN) and gas, or internal septations. On CT, a renal ab-
dilated ureter (DU). Right hydroureteronephrosis was
also detected (not shown).
scess often shows internal septations and a rim
sign (enhancement of the abscess wall with a
central low density within the collection) (Fig. 10B). Mass effect, adjacent inflammation of the
perinephric or renal sinus fat, or mild dilatation of the renal pelvis and ureter may also be present.
The current management of renal abscess in children includes antibiotic treatment, with or with-
out aspiration, and follow-up imaging to confirm abscess resolution.
Multicystic dysplastic kidneyMulticystic dysplastic kidney is a nonhereditary developmen-
tal renal dysplasia. The underlying cause of multicystic dysplastic kidney is believed to be early
in utero urinary tract obstruction. On pathology, there are noncommunicating cysts of varying
sizes that represent the dilated collecting system. These cysts are separated by primitive dysplas-
tic renal tissues that are nonfunctional. Unlike autosomal-dominant polycystic kidney disease,
which is the most frequent hereditary cystic kidney disease involving both kidneys, multicystic
dysplastic kidney almost always involves a unilateral kidney. Approximately 2050% of patients
with multicystic dysplastic kidney also have a concomitant contralateral renal abnormality, in-
cluding vesicoureteral reflux, UPJ obstruction, and primary megaureter.
The imaging features of multicystic dysplastic kidney parallel the underlying pathologic fea-
tures. On imaging studies, there are multiple cystic masses of variable size and shape in a random
distribution with absent or dysplastic renal parenchyma (Fig. 11). Additionally, an identifiable
renal pelvis or sinus is absent.
A B
Fig. 10Renal abscess in 15-year-old boy who presented with fever, elevated WBC count, and right flank pain.
A, Transverse ultrasound image of right kidney shows avascular heterogeneous area in upper and mid zones.
B, Contrast-enhanced axial CT image shows heterogeneous lesion with multiple internal septations of varying
thickness in right kidney.
AJR:199, July 2012 W7
Ranganath et al.
Multilocular cystic nephromaA multi-
locular cystic nephroma is a rare nonheredi-
tary benign cystic renal neoplasm. It typi-
cally occurs in boys between 3 months and 2
years old, or in women between 40 and 50
years old. Multilocular cystic nephromas can
range in size from a few centimeters to a
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
mean of approximately 10 cm. In children,
multilocular cystic nephroma typically pres-
ents as a palpable abdominal mass (Fig.
12A). On ultrasound, the lesion is usually a
well-defined multiloculated anechoic mass
with echogenic internal septa (Fig. 12B). Al-
though CT is not usually necessary after ul-
trasound detection, multilocular cystic ne-
phroma may be incidentally detected on CT
Fig. 11Mutlicystic dysplastic kidney in 2-week-
obtained for other reasons. On CT, it appears old boy with prenatal diagnosis of cystic right
as a cystic mass with water attenuation, well- renal mass. Transverse ultrasound image of right
circumscribed margins, and internal septa- kidney shows numerous cysts (C) of various sizes
tions (Fig. 12C). Because imaging studies without recognizable normal renal corticomedullary
architecture.
cannot reliably distinguish multilocular cys-
tic nephroma from a multilocular cystic renal cell carcinoma or cystic Wilms tumor (Fig. 13),
surgical excision is the currently accepted management of choice.
Cystic Wilms tumorWilms tumor is the most frequent primary renal neoplasm in the pe-
diatric population. It accounts for approximately 95% of all pediatric renal malignancies and
typically occurs in children younger than 5 years old. Pediatric patients with Wilms tumor
Fig. 12Multilocular cystic nephroma in 10-month-
old boy who presented with palpable left-sided
abdominal mass.
A, Abdominal radiograph shows opacity (M) centered
in left side of abdomen that produces mass effect on
adjacent colon (arrow).
B, Transverse ultrasound image of left kidney shows
cystic mass (C) with echogenic septa (arrow). Blood
flow within these echogenic septa is also seen.
C, Contrast-enhanced axial CT image shows large
water-attenuation mass with well-circumscribed
borders and mildly enhancing internal septations
(arrows).
A
B C
W8 AJR:199, July 2012
Abdominal Masses in Children
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
A B
Fig. 13Cystic Wilms tumor in 1-year-old boy who presented with rapidly enlarging right-sided abdomen and
increasing irritability.
A, Transverse ultrasound image of right kidney shows large cystic mass (C) arising from right kidney (arrows).
B, Contrast-enhanced axial CT image shows large cystic mass (C) with well-circumscribed borders and without
internal solid components arising from right kidney (arrows).
A B
Fig. 14Rhabdoid tumor in 1-year-old girl who
initially presented with low-grade fever, symptoms
of prolonged upper respiratory tract infection,
decreased oral intake, and increased fatigue. On
admission, initial physical examination revealed
palpable mass in left-sided abdomen.
A, Longitudinal ultrasound image of left kidney shows
large left renal mass with subcapsular fluid collection
(SF) containing internal debris. K = kidney.
B, Contrast-enhanced axial CT image shows large
subcapsular fluid collection (SF) within intact left
renal capsule (arrow). Also noted is left kidney (K).
C, Contrast-enhanced coronal CT image better shows
relationship among tumor (T), left kidney (K), and
subcapsular fluid collection (SF).
C
present with a palpable abdominal mass, pain, hematuria, or hypertension. Wilms tumor may
be associated with clinical syndromes or anomalies, including Beckwith-Wiedemann syn-
drome, Drash syndrome, hemihypertrophy, cryptorchidism, and sporadic aniridia. Approxi-
mately 510% of children with Wilms tumors have bilateral or multicentric tumors. Although
AJR:199, July 2012 W9
Ranganath et al.
the majority of Wilms tumors are solid renal masses, a small percentage may be purely cystic,
referred to as cystic Wilms tumor.
On ultrasound, cystic Wilms tumors are anechoic intrarenal masses (Fig. 13A). Although
the diagnosis of cystic Wilms tumor and vascular extension can be made on ultrasound, CT
may be used to confirm the renal origin of the tumor, its margins, and the local and distant
metastases (Fig. 13B). The current management of Wilms tumor involves multimodal thera-
py, including surgery, chemotherapy, and radiation therapy for selected patients. Such multi-
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
modal therapy results in dramatic improvement in outcome in children with Wilms tumor,
with overall 5-year survival rates of 90%.
Rhabdoid tumorMalignant rhabdoid tumor is a rare and aggressive renal neoplasm in chil-
dren. It is often associated with early onset of local and distant metastases as well as resistance
to chemotherapy. The most frequent sites of metastases are lungs, abdominal lymph nodes, liver,
brain, and bone. Although there is no pathognomonic imaging feature of malignant rhabdoid
tumor of the kidney in children, it typically presents as a large renal mass composed of both
cystic and solid components. The most helpful imaging feature is a peripheral subcapsular cres-
cent-shaped fluid collection, which may be due to either hemorrhage or necrosis (Fig. 14). How-
ever, the definitive diagnosis of rhabdoid tumor is only made by histologic examination. Treat-
ment includes both surgery and chemotherapy, but the prognosis is generally poor.
Pancreas
Pancreatic pseudocystA pancreatic pseudocyst is a collection of pancreatic fluid and in-
flammatory exudates encapsulated by fibrous tissue. It usually develops as a result of posttrau-
matic or inflammatory injury to the pancreas, when unabsorbed fluid collections organize and
form a fibrous capsule within 46 weeks after initial injury. On ultrasound, pancreatic pseudo-
cysts are usually well-circumscribed unilocular smooth-walled cystic masses, often with irregu-
larly thickened walls (Fig. 15A). They are most frequently located in the body or tail of the
pancreas. Pancreatic pseudocysts can sometimes be complicated by hemorrhage or infection,
which is manifested by septations, internal echoes, and fluid-debris levels on imaging studies. On
CT, pancreatic pseudocysts are typically round or oval homogeneously hypodense lesions with
near-water attenuation (Fig. 15B). However, the attenuation and complexity of the lesion can
increase when there is associated hemorrhage or superimposed infection. In pediatric patients,
ultrasound is usually used to follow pancreatic pseudocysts, which may require surgical decom-
pression if they continue to grow and cause symptoms.
Pancreatic cystadenomaPancreatic cystadenoma is a benign neoplasm arising from acinar
cells of the pancreas. It is composed of numerous small cysts that contain proteinaceous fluid
and are separated by septa of connective tissue. Depending on the size of the individual cysts,
pancreatic cystadenoma can have a variable appearance on ultrasound and CT. On ultrasound,
A B
Fig. 15Pancreatic pseudocyst in 17-year-old girl with history of pancreatitis who presented with new onset
of epigastric pain.
A, Longitudinal ultrasound image of epigastric region shows large cystic mass (C) with irregular walls (arrows).
B, Contrast-enhanced axial CT image shows large cystic mass (C) arising from pancreas. Mild surrounding
inflammatory changes and fluid (arrows) are also seen adjacent to this large pancreatic pseudocyst.
W10 AJR:199, July 2012
Abdominal Masses in Children
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
A B
Fig. 16Mucinous cystadenoma of pancreas in 17-year-old girl who presented with epigastric pain.
A, Transverse ultrasound image of pancreas shows large cystic mass with multiple internal septations (arrows)
in pancreatic body and tail.
B, Contrast-enhanced axial CT image shows large low-attenuation cystic mass with several mildly enhancing
internal septations (arrows) arising from body and tail of pancreas.
numerous small cysts can appear as solid, partially solid, or multicystic with septations (Fig.
16A). CT shows similar findings and can show enhancement of the septa separating numerous
small cysts (Fig. 16B). For small cystadenomas in asymptomatic patients, conservative manage-
ment with follow-up imaging is sufficient. However, large cystadenomas that cause common
bile duct obstruction or atrophy of the pancreas distal to the tumor require complete surgical
excision and follow-up.
Spleen
Splenic cystSplenic cysts can be either congenital or acquired, although they appear
identical on imaging studies. Congenital splenic cysts (true or epidermoid cysts) contain an
inner cellular lining. Acquired splenic cysts (false or pseudocysts) are usually posttraumatic
and due to liquefactive necrosis. Both congenital and acquired splenic cysts usually appear as
anechoic round lesions with imperceptible walls on ultrasound, although they can show inter-
nal echoes if they contain debris or hemorrhage. Posttraumatic splenic cysts often have thick-
er walls that may be calcified, unlike the imperceptible walls of congenital cysts. There is no
internal enhancement on contrast-enhanced CT images (Fig. 17).
Splenic abscessA splenic abscess is a collection of pus within the splenic parenchyma.
On ultrasound, it is typically a hypoechoic lesion containing low-level internal echoes that
represent debris and internal septations. On CT, splenic abscesses typically appear as com-
plex fluid collections that are often associated with internal septations, peripheral contrast
rim enhancement, and surrounding inflammatory changes (Fig. 18). Splenic abscesses can be
divided into microabscesses ( 1.5 cm), which are often due to fungal infection (Fig. 19), and
larger abscesses (> 1.5 cm), which are typically due to bacterial infection (Fig. 18). Splenic
abscesses in children also can be due to cat scratch disease, which is a regional, infectious
lymphadenitis caused by a pleomorphic gram-negative bacillus. Children affected with cat
scratch disease may present with multiple hypoechoic lesions on ultrasound in the spleen or
hypoattenuating lesions on CT of the spleen, representing underlying granulomatous inflam-
mation with abscess formation. Imaging evaluation with ultrasound or CT can be helpful in
pediatric patients with splenic abscess for guiding surgical drainage procedures in managing
large splenic abscesses, particularly when the abscesses are not responding to medical man-
agement with either antibacterial or antifungal medications.
Vascular malformationSplenic vascular malformations are characterized by abnormal
vascular channels lined with a single layer of dysplastic endothelium. Capillary and venous
malformations of the spleen have a similar imaging appearance and may be solitary or multi-
ple. Multiple vascular malformations in the spleen often occur in patients with Klippel-Tre-
naunay-Weber or Beckwith-Wiedemann syndrome. For assessment of the underlying vascular
AJR:199, July 2012 W11
Ranganath et al.
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Fig. 17Simple splenic cyst in 10-year-old girl who Fig. 18Splenic abscess in 11-year-old boy with
presented with right lower quadrant pain. Contrast- fever, elevated WBC count, and left flank pain.
enhanced axial CT image of abdomen obtained for Contrast-enhanced axial CT image shows large
possible appendicitis shows well-circumscribed complex fluid collection with internal septations
round splenic cystic lesion (arrows) without contrast (straight arrows) and perisplenic inflammatory
enhancement. Follow-up imaging study showed change (curved arrow). Fluid culture obtained
interval stability of this incidentally detected lesion. after drainage catheter placement was positive for
Staphylococcus aureus infection.
component of splenic vascular malformation, Doppler ultrasound is a helpful imaging tech-
nique. Splenic vascular malformation may be an incidental finding on CT performed for other
reasons in pediatric patients. On CT, splenic vascular malformations are often multiple, homo-
geneous, and hypodense and are sometimes associated with central or peripheral calcification.
Lymphatic malformations are rare benign cystic splenic lesions that can be solitary or
multiple. On contrast-enhanced CT images, they typically have low attenuation and do not
enhance (Fig. 20).
Adrenal Gland
Adrenal hemorrhageAdrenal hemorrhage, which typically occurs in infants during the
perinatal period, is usually due to birth trauma, anoxia, neonatal sepsis, or dehydration. The
right adrenal gland is more often affected than the left. Left adrenal gland hemorrhage is as-
sociated with renal vein thrombosis. Clinical findings of neonatal adrenal hemorrhage in-
clude a palpable mass, anemia, and jaundice due to underlying hyperbilirubinemia.
Fig. 19Splenic abscess in 15-year-old girl with Fig. 20Lymphatic malformation. Contrast axial
leukemia who presented with fever. Contrast- CT image in 18-year-old girl shows multiple low-
enhanced axial CT image shows multiple small low- attenuation cystic lesions of varying size in spleen.
attenuation splenic lesions (arrows). Blood culture
was positive for Candida albicans infection.
W12 AJR:199, July 2012
Abdominal Masses in Children
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
A B
Fig. 21Neonatal adrenal hemorrhage in 5-day-old boy with prenatal diagnosis of cystic mass of right upper
quadrant.
A, Longitudinal ultrasound image of suprarenal region shows cystic mass with internal debris (arrow), likely
representing blood product and consistent with adrenal hemorrhage. K = kidney.
B, Follow-up ultrasound image obtained 3 months later shows interval decrease in size of adrenal hemorrhage
(arrows). K = kidney.
The imaging appearance depends on the stage of the hemorrhage. On ultrasound, acute adre-
nal hemorrhage typically presents as a suprarenal cystic mass with variable echogenicity and
complexity. In the subacute stage, adrenal hemorrhage becomes more hypoechoic because of
liquefaction of the hemorrhage (Fig. 21). Later, adrenal hemorrhage becomes hyperechoic as the
clot retracts and calcification develops. Follow-up ultrasound is helpful for documenting interval
resolution of adrenal hemorrhage in neonates because sonographic differentiation between neo-
natal adrenal hemorrhage and neuroblastoma can be difficult or impossible. In contrast to neona-
tal adrenal hemorrhage, which decreases in size within 12 weeks, neuroblastoma remains stable
or increases in size on follow-up ultrasound.
Cystic neuroblastomaNeuroblastoma is the most frequent malignant tumor in infancy and
most often originates from the adrenal gland. Although cystic neuroblastoma, which can arise
from the adrenal gland or any neural crest element of the abdomen, is a rare form of this neoplasm,
it should be considered in the differential diagnosis of a cystic adrenal mass, particularly in neo-
nates. On ultrasound, cystic neuroblastoma typically presents as an anechoic or complex echo-
genic suprarenal mass that may have associated calcification (Fig. 22). Because the imaging ap-
pearance of cystic neuroblastoma is often very similar to that of adrenal hemorrhage in neonates,
follow-up ultrasound is currently recommended for management. Although adrenal hemorrhage
rapidly decreases in size and usually resolves within several weeks, cystic neuroblastoma in the
neonate is unlikely to show any substantial interval change in size on follow-up ultrasound.
Mesentery
Mesenteric Cyst or Lymphatic Malformation
A mesenteric lymphatic malformation, also known as mesenteric cyst, arises from the small
or large bowel mesentery. It develops from a proliferation of lymphatic tissue that fails to com-
municate with the central lymphatic system. A mesenteric cyst can range in size from a few milli-
meters to 40 cm. On imaging studies, mesenteric lymphatic malformations can be unilocular or
multilocular cystic lesions. They sometimes show thin septations, fine calcifications, and vari-
able attenuation or internal echogenicity depending on the composition of the internal fluid (Fig.
23). Complications of mesenteric lymphatic malformations include hemorrhage and infection.
CSF Collection
A collection of CSF at the distal end of a ventriculoperitoneal shunt is termed a CSFoma and
typically occurs secondary to adhesion of the ventriculoperitoneal shunt catheter in the perito-
neal cavity and subsequent blockage of peritoneal absorption of the shunted CSF. Children with
CSFomas typically present with abdominal distention or shunt malfunction, which manifests as
increased intracranial pressure. The diagnosis can be made by ultrasound or CT, which typically
AJR:199, July 2012 W13
Ranganath et al.
show an anechoic abdominal cystic mass lo-
cated near the tip of the ventriculoperitoneal
shunt catheter (Fig. 24). Although CSFomas
sometimes resolve spontaneously, shunt revi-
sion or aspiration of the lesion should be con-
sidered as other treatment options, particu-
larly in symptomatic children.
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Abscess
Mesenteric abscesses are localized collec-
tions of pus within the mesentery. In chil-
dren, they are often secondary to infectious
or inflammatory processes of the large and
small bowel, such as inflammatory bowel
disease or ruptured appendicitis. Ultrasound
and CT can show a fluid collection that is of-
Fig. 22Cystic neuroblastoma. Longitudinal
ten complex with internal gas, air-fluid level, ultrasound in 2-year-old boy shows complex
or septations (Fig. 25). suprarenal cystic mass (arrows). Also noted is mild
pelvocaliectasis of right kidney.
Cystic Teratoma
Intraabdominal mesenteric cystic teratomas are extremely rare. Radiographs often show a
large abdominal opacity that displaces bowel loops. Calcifications associated with mesenteric
cystic teratoma can sometimes be seen. On ultrasound, the mass has variable cystic and solid
components (Fig. 26A). CT shows similar imaging findings, but this modality better shows the
fat and calcifications that are often associated with an intraabdominal mesenteric cystic tera-
toma (Fig. 26B).
Bowel
Duplication Cyst
Enteric duplication cyst is a rare focal congenital cystic malformation of the gastrointesti-
nal tract. They can occur anywhere along the mesenteric border of the bowel but most fre-
quently involve the jejunum or ileum. Although affected patients may be asymptomatic, the
typical clinical presentation includes a palpable abdominal mass, abdominal distention, vom-
iting (secondary to bowel obstruction), or hemorrhage (secondary to peptic ulceration due to
the presence of gastric mucosa in some patients). Pathologically, duplication cysts are charac-
terized by a well-developed coat of smooth muscle, epithelial lining that represents some part
of the alimentary tract, and contiguity with some part of the alimentary tract.
A B
Fig. 23Mesenteric cyst in 14-year-old girl who presented with abdominal pain.
A, Transverse ultrasound image of midabdomen shows large anechoic cystic mass (C) with imperceptible wall.
B, Contrast-enhanced axial CT image shows well-circumscribed cystic mass (C) without enhancement in
midabdomen.
W14 AJR:199, July 2012
Abdominal Masses in Children
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Fig. 24CSF collection (CSFoma) in 16-year-old Fig. 25Mesenteric abscess in 2-year-old boy who
boy with ventriculoperitoneal shunt catheter placed presented with fever, elevated WBC count, increased
after posterior fossa dermoid tumor resection who irritability, and decreased appetite. Contrast-
presented with abdominal pain and headache. enhanced axial CT image shows complex fluid
Transverse ultrasound image of midabdomen collection (straight arrows) with air-fluid level. Note
shows loculated fluid collection in midabdomen. appendicolith (curved arrow) within complex fluid
Ventriculoperitoneal shunt catheter (arrow) lies collection. BL = bladder.
within CSFoma.
A B
Fig. 26Mesenteric cystic teratoma in 9-month-old girl who presented with palpable abdominal mass.
A, Longitudinal ultrasound image of midabdomen shows complex mass composed of cystic (C) and solid
(arrows) components.
B, Contrast-enhanced axial CT image shows cystic component (C), fat component (F), and calcification (arrow).
On ultrasound, duplication cysts typically have a spherical, ovoid, or dumbbell shape (Fig.
27). They have a characteristic bowel wall signature, which includes echogenic mucosa, hy-
poechoic muscular layer, and echogenic serosa (Fig. 27). On CT, gastrointestinal duplication
cysts typically appear as round masses with water attenuation and a mildly enhancing wall
(Fig. 28). Information regarding complications of gastrointestinal duplication cysts is limited,
particularly in the pediatric population. However, reported complications include perforation,
intussusception, bowel obstruction, and volvulus. The current treatment of choice for gastro-
intestinal duplication cysts in symptomatic pediatric patients is surgical excision, whereas
there is currently no standardized evidence-based guideline for managing incidentally de-
tected gastrointestinal duplication cysts in asymptomatic pediatric patients.
Conclusion
Focal cystic abdominal masses are frequent disorders that can be symptomatic or inciden-
tal findings in pediatric patients. Imaging evaluation can provide precise information regard-
AJR:199, July 2012 W15
Ranganath et al.
Downloaded from www.ajronline.org by 36.73.111.48 on 09/01/14 from IP address 36.73.111.48. Copyright ARRS. For personal use only; all rights reserved
Fig. 27Duplication cyst of ileum in 9-month-old Fig. 28Colonic duplication cyst. Contrast-
boy who presented with increasing abdominal enhanced axial CT image in 2-year-old boy with
distention and crying. Transverse ultrasound image right lower quadrant pain to evaluate of possible
of right lower quadrant shows spherical cystic mass appendicitis shows round cystic mass (C) within right
with echogenic mucosa (long arrow), hypoechoic colon surrounded by oral contrast material.
muscular layer (short arrow), and echogenic serosa
(curved arrow). This complex of findings represents
gut signature.
ing their location, appearance, size, and mass effect on adjacent abdominal structures. This
information is crucial for early and correct diagnosis, which, in turn, can lead to optimal pa-
tient management.
Selected Reading pearance of cystic masses of the liver. Radio-
1. Berrocal T, Pajares MP, Zubillaga AF. Pancreatic Graphics 1989; 9:307322
cystosis in children and young adults with cystic 9. Niron EA, Ozer H. Ultrasound appearances of liver
fibrosis: sonographic, CT, and MRI findings. AJR hydatid disease. Br J Radiol 1981; 54:335338
2005; 184:13051309 10. Prieto ML, Casanova A, Delgado J, Zabalza R.
2. Chung CJ, Lorenzo R, Rayder S, et al. Rhabdoid Cystic teratoma of the mesentery. Pediatr Radiol
tumors of the kidney in children: CT findings. 1989; 19:439
AJR 1995; 164:697700 11. Roitberg BZ, Tomita T, McLone DG. Abdominal
3. Decter RM. Renal duplication and fusion anoma- cerebrospinal fluid pseudocyst: a complication of
lies. Pediatr Clin North Am 1997; 44:13231341 ventriculoperitoneal shunt in children. Pediatr
4. Elsayes KM, Menias CO, Dillman JR, et al. Vas- Neurosurg 1998; 29:267273
cular malformation and hemangiomatosis syn- 12. Ros PR, Olmsted WW, Moser RP Jr, et al. Mesen-
dromes: spectrum of imaging manifestations. teric and omental cysts: histologic classification with
AJR 2008; 190:12911299 imaging correlation. Radiology 1987; 164:327332
5. Han TI, Kim MJ, Yoon HK, et al. Rhabdoid tu- 13. Rypens F, Dubois J, Garel L, et al. Percutaneous
mour of the kidney: imaging findings. Pediatr drainage of abdominal abscesses in pediatric
Radiol 2001; 31:233237 Crohns disease. AJR 2007; 188:579585
6. Horton KM, Bluemke DA, Hruban RH, et al. CT 14. Strife JL, Souza AS, Kirks DR, et al. Multicystic
and MR imaging of benign hepatic and biliary dysplastic kidney in children: ultrasound follow-
tumors. RadioGraphics 1999; 19:431451 up. Radiology 1993; 186:785788
7. Koumanidou C, Vakaki M, Papadaki M, et al. 15. Todani T, Watanabe Y, Narusue M, Tabuchi K,
New sonographic appearance of hepatic mesen- Okajima K. Congenital bile duct cysts: classifica-
chymal hamartoma in childhood. J Clin Ultra- tion, operative procedures, and review of thirty-
sound 1999; 27:164167 seven cases including cancer arising from the
8. Murphy BJ, Casillas J, Ros PR, et al. The CT ap- choledochal cyst. Am J Surg 1977; 134:263269
W16 AJR:199, July 2012
Você também pode gostar
- Critical ThinkingDocumento2 páginasCritical ThinkingMwagaVumbiAinda não há avaliações
- Bronkiektasis PDFDocumento14 páginasBronkiektasis PDFHalida Batik AlunaAinda não há avaliações
- Neuro BlastomaDocumento7 páginasNeuro BlastomaHalida Batik AlunaAinda não há avaliações
- Review Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageDocumento12 páginasReview Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageHalida Batik AlunaAinda não há avaliações
- Art:10.1007/s00247 005 1559 7 PDFDocumento12 páginasArt:10.1007/s00247 005 1559 7 PDFHalida Batik AlunaAinda não há avaliações
- Review Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageDocumento12 páginasReview Article: Differentiating Between Hemorrhagic Infarct and Parenchymal Intracerebral HemorrhageFika Tri NandaAinda não há avaliações
- A Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportDocumento3 páginasA Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportHalida Batik AlunaAinda não há avaliações
- A Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportDocumento3 páginasA Rare Cause of Reversible Unilateral Breast Swelling: A Case ReportHalida Batik AlunaAinda não há avaliações
- Journal Cystic Abdominal MassesDocumento16 páginasJournal Cystic Abdominal MassesHalida Batik AlunaAinda não há avaliações
- Jurnal PneumoniaDocumento12 páginasJurnal PneumoniaHalida Batik AlunaAinda não há avaliações
- BronkiektasisDocumento14 páginasBronkiektasisHalida Batik AlunaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Juan Martin Garcia System Dynamics ExercisesDocumento294 páginasJuan Martin Garcia System Dynamics ExercisesxumucleAinda não há avaliações
- Progibb LV Plus PGR - Low Voc FormulationDocumento2 páginasProgibb LV Plus PGR - Low Voc FormulationDodik Novie PurwantoAinda não há avaliações
- Library Dissertation in Community DentistryDocumento9 páginasLibrary Dissertation in Community DentistryPayForPaperCanada100% (1)
- Elements of ClimateDocumento18 páginasElements of Climateእኔ እስጥፍAinda não há avaliações
- 24.postpartum Period-Physiological Changes in The MotherDocumento16 páginas24.postpartum Period-Physiological Changes in The MotherHem KumariAinda não há avaliações
- Apollo TyresDocumento78 páginasApollo TyresADITYA33% (3)
- Hyperbaric WeldingDocumento17 páginasHyperbaric WeldingRam KasturiAinda não há avaliações
- Space DynamicsDocumento37 páginasSpace Dynamicspurushottam KashyapAinda não há avaliações
- SRS Design Guidelines PDFDocumento46 páginasSRS Design Guidelines PDFLia FernandaAinda não há avaliações
- Chemistry Implementation: Name: Rasheed Campbell School: Kingston College Candidate #.: Centre #: 100057Documento12 páginasChemistry Implementation: Name: Rasheed Campbell School: Kingston College Candidate #.: Centre #: 100057john brownAinda não há avaliações
- Problem SolutionsDocumento5 páginasProblem SolutionskkappaAinda não há avaliações
- A Study On Customer Satisfaction Towards Honda Bikes in CoimbatoreDocumento43 páginasA Study On Customer Satisfaction Towards Honda Bikes in Coimbatorenkputhoor62% (13)
- Features Integration of Differential Binomial: DX BX A X P N MDocumento4 páginasFeatures Integration of Differential Binomial: DX BX A X P N Mابو سامرAinda não há avaliações
- LSUBL6432ADocumento4 páginasLSUBL6432ATotoxaHCAinda não há avaliações
- Stability Calculation of Embedded Bolts For Drop Arm Arrangement For ACC Location Inside TunnelDocumento7 páginasStability Calculation of Embedded Bolts For Drop Arm Arrangement For ACC Location Inside TunnelSamwailAinda não há avaliações
- Motor Wiring Diagram: D.C. Motor ConnectionsDocumento1 páginaMotor Wiring Diagram: D.C. Motor Connectionsczds6594Ainda não há avaliações
- Final Decision W - Cover Letter, 7-14-22Documento19 páginasFinal Decision W - Cover Letter, 7-14-22Helen BennettAinda não há avaliações
- Proposal Anguria Pasta NewDocumento24 páginasProposal Anguria Pasta NewNOOR IRDINA HAFIZAH BT TAUPISAinda não há avaliações
- VivsayamDocumento87 páginasVivsayamvalarumsakthi100% (2)
- Casio AP-80R Service ManualDocumento41 páginasCasio AP-80R Service ManualEngkiong Go100% (1)
- Virchow TriadDocumento6 páginasVirchow Triadarif 2006Ainda não há avaliações
- Is.4162.1.1985 Graduated PipettesDocumento23 páginasIs.4162.1.1985 Graduated PipettesBala MuruAinda não há avaliações
- Background of The Study Statement of ObjectivesDocumento4 páginasBackground of The Study Statement of ObjectivesEudelyn MelchorAinda não há avaliações
- Monster of The Week Tome of Mysteries PlaybooksDocumento10 páginasMonster of The Week Tome of Mysteries PlaybooksHyperLanceite XAinda não há avaliações
- 9600 DocumentDocumento174 páginas9600 Documentthom38% (13)
- APLICACIONES PARA AUTOS Y CARGA LIVIANADocumento50 páginasAPLICACIONES PARA AUTOS Y CARGA LIVIANApancho50% (2)
- Fake News Poems by Martin Ott Book PreviewDocumento21 páginasFake News Poems by Martin Ott Book PreviewBlazeVOX [books]Ainda não há avaliações
- 12 Week Heavy Slow Resistance Progression For Patellar TendinopathyDocumento4 páginas12 Week Heavy Slow Resistance Progression For Patellar TendinopathyHenrique Luís de CarvalhoAinda não há avaliações
- Are Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDocumento5 páginasAre Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDr Chevyndra100% (1)
- VA TearDownDocumento5 páginasVA TearDownfaj_larcfave5149Ainda não há avaliações