Escolar Documentos
Profissional Documentos
Cultura Documentos
Monitoring During Anaesthesia
Enviado por
Jim Jose AntonyDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Monitoring During Anaesthesia
Enviado por
Jim Jose AntonyDireitos autorais:
Formatos disponíveis
(9) Monitoring During Anesthesia
Leader: Moody A. Almarshad
Done by: Ghadah Alharbi
Revised by: Shatha Al-Shanqeeti
Monitoring During Anesthesia 1
Anesthesia Teamwork 432
Doctor's note Team's note Not important Important 431 teamwork
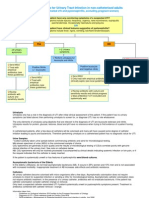
Noninvasive Arterial
Blood Pressure
Monitoring
ASA Standards for
Basic Anaesthetic
Monitoring
Invasive Arterial
Blood Pressure
Monitoring
Cardiovascular
Monitoring
ECG
Central Venous
Catheterization
Pulse Oximetry
Respiratory
Capnography
Monitoring During Monitoring
Anaesthesia
Stethoscope
Neurological
EEG
Monitors
Temperature
Urine Output
Peripheral Nerve
Stimulation
Monitoring During Anesthesia 2
Anesthesia Teamwork 432
Perioperative Management and Monitoring in Anesthesia
Inadequate monitoring Constitutes 10% of anesthesia related deaths.
Vital signs should always be monitored in order to have proper standardized anesthesia.
Monitoring Recommendations of the Association of Anesthetists of Great Britain and Ireland:
Essential Monitoring:
Circulation: ECG, non-invasive measurements of systemic blood pressure, clinical observation.
Respiration: Capnography, pulse oximetry, clinical observation.
Body Temperature: Temperature probe.
Available Monitoring:
If muscle relaxants are used: Nerve stimulator.
If volatile anesthetics are used: Inspiratory and expiratory anesthetic concentration.
Assessing the Depth of Anesthesia:
Craniofacial electromyography
Respiratory sinus arrhythmia
Heart rate variability
Electroencephalogram derivatives:
Spectral edge frequency
Median power frequency
Power band ratios
Evoked responses:
P300
Middle latency evoked responses
Auditory steady state response
Coherent frequency of the auditory steady state response
Guidelines for Pediatric Perioperative Anesthesia Environment:
ECG
Blood pressure
Pulse oximetry
Capnography
FiO2
Anesthetic gas concentration
Temperature
The emphasis is on the temperature and the respiratory system (They usually die of
respiratory failure).
Monitoring During Anesthesia 3
Anesthesia Teamwork 432
Practice Guidelines for Postanesthetic Care
Immediately available
ASA Standards for Basic Anesthetic Monitoring
Standard I: Qualified anesthesia personnel shall be present in the room throughout
the conduct of all general anesthetics, regional anesthetics and monitored anesthesia
care.
Standard II: During all anesthetics, the patients oxygenation, ventilation, circulation
and temperature shall be continually evaluated. (This is called the Minimum
Mandatory Monitoring (MMM))
Monitoring During Anesthesia 4
Anesthesia Teamwork 432
Oxygenation Ventilation Circulation Temperature
Inspired gas: ECG (Continuos Temperature probe
Auscultation of
Oxygen display)
breath sounds,
analyzer observation of
(measures the patient, Arterial blood Monitor tempreture when
FiO2 and observation of pressure and changes are intended,
FeO2) the resivior bag. heart rate anticipated, or suspected.
(record every 5
minutes)
Blood Capnography
oxygenation: (Carbon dioxide
Pulse Oximetry monitoring) Evaluation of circulation:
Plapation of pulse,
auscultation of heart
sounds, pulse
plethysmography, pulse
oximetry, intrarterial
pressure tracing (Only
when needed).
Monitoring During Anesthesia 5
Anesthesia Teamwork 432
1. Cardiovascular Monitoring (1)
A. Noninvasive Arterial Blood Pressure Monitoring
The use of any anesthetic is an indication for arterial blood pressure monitoring. The
techniques and frequency of pressure determination depend on the patients
condition and the type of surgical procedure. The results should be viewed as an
indicator of organ transfusion. Blood pressure cuff are best avoided in extremities
with vascular abnormalities or intravenous line, or in cases of burns.
Arterial blood pressure can be measured by: palpation, doppler probe, oscillometry,
and arterial tonometry.
B. Invasive Arterial Blood Pressure Monitoring
It allows continuous beat-to-beat blood pressure measurements. The radial artery is
commonly cannulated. Allens test is a simple, non reliable method of assessing the
safety of radial artery.
Types:
Swan Ganz Catheter, PiCCO System (Pulse Contour Cardiac Output),
Advanced PAC: SVO2, CCO, REF, EDV, TEE.
Indications for Invasive Blood Pressure Monitoring:
A. Patient-dependent factors
Hemodynamic instability (shock)
Cardiac disease
Respiratory insufficiency (ABG monitoring in COPD patients)
Increased intracranial pressure
Polytrauma
Risk factors of complications
B. Type of Surgery are: Prolonged cannulation,
hyperlipidemia, repeated
Cardiac surgery insertion attempts, female
Craniotomy gender, and the use of large
Major thoracic surgery catheters in small vessels and
Major abdominal surgery the use of vasopressors.
Complications of intra-arterial monitoring include: Arterial laceration, hematoma,
bleeding, loss of distal perfusion to the hand, vasospasm, arterial thrombosis, air
embolism, pseudoaneurysm, nerve damage, infection, and necrosis of skin overlying
the catheter, errors in monitoring, failed attempt.
Monitoring During Anesthesia 6
Anesthesia Teamwork 432
1. Cardiovascular Monitoring (1)
- Arterial Waveform Evaluation:
Tf- Foot: onset of ejection, systole.
T1- First shoulder: peak flow.
T2- Second Shoulder: peak pressure.
Ti- Dichotic Notch: end of ejection, closure
of aortic valve, precedes the onset of
diastole.
Tt- Pulse Duration.
Non-invasive Methods vs. Arterial Cannulation:
NIBP Arterial Cannulation
Pros Healthy Patients Continuous BP
Sick patients
Short case Difficult cases
ABG monitoring
Cons Bladder cuff size Thrombosis / Ischemia
Flow dependant
Motion Hematoma formation
Interruption of IV infusion Infection
Injury
Cuff deflation rate Nerve dysfunction
Hydrostatic errors
Monitoring During Anesthesia 7
Anesthesia Teamwork 432
1. Cardiovascular Monitoring (1)
C. Electrocardiogram ECG:
All patients should have intraoperative ECG
monitoring.
What to expect from the ECG: rate, rhythm,
propagation of the excitation wave, heart
position, muscle hypertrophy, and regional
ischemia.
It gives NO information about pump function.
P wave represents atrial contraction Atrial
depolarization. The QRS complex represents
ventricular contraction depolarization
following the 120-200 msec atrioventricular
nodal delay, it can be prolonged in patients with cardiomyopathies and heart failure.
T wave represents ventricular repolarization, prolongation of the QT interval is
secondary to electrolytes imbalance or drugs which could lead to life-threatening
arrhythmias.
Lead Selection:
The electrical axis of lead II is parallel to the electrical axis of the atria, this orientation
enhances the diagnosis of arrhythmias by detecting inferior wall ischemia Lead II is
the most common lead used for monitoring but it is not the optimal monitoring lead.
Lead V5 can detect ST-T changes (anterior and lateral wall ischemia).
Monitoring During Anesthesia 8
Anesthesia Teamwork 432
1. Cardiovascular Monitoring (1)
D. Central Venous Catheterization:
CVC is indicated for monitoring of the central venous pressure, administration of
fluids to treat hypovolemia and shock, infusion of caustic drugs and total parenteral
nutrition, aspiration of air emboli and gaining venous access in patients with poor
peripheral veins. Usually we choose the right internal jugular vein subclavian vein
cannulation is associated with increased risk of pneumothorax during insertion but a reduced risk for
other complications during prolonged cannulations (e.g. in critically ill patients).
Contraindications: Patient refusal, tumors, clots or tricuspid valve vegetations, severe
coagulopathy, infection at site, previous failed attempts at specific site, hematoma and
unusual anatomy, bundle branch block (relative contraindication).
The risks are: infections, air or thrombus embolism, arrhythmias, hematoma,
pneumothorax, hemothorax, cardiac perforations and tamponade, trauma to the
nerves and arteries, and thrombosis.
Central Line Techniques:
Sterile techniques should be used for all central line cannulation
Surgical scrub with Sterile gown and gloves
Sterile prep of skin and surgical drapes.
Local anesthetic should be used for central catheters in awake patients
Success may be improved by using ultrasound guidance
Techniques of gaining access include:
Catheter over needle
Catheter through needle
Seldinger technique
Surgical cut-down is surgical technique as last resort.
Monitoring During Anesthesia 9
Anesthesia Teamwork 432
1. Cardiovascular Monitoring (1)
Anatomy of Central Access:
Internal jugular vein
Right sided access preferred because apical pleura does not rise as
high on right and avoids thoracic duct
Patient positioned head down to engorge the vein
In the low approach triangle formed by two heads of
sternomastoid and clavicle identified
Cannula aimed down and lateral towards ipsilateral nipple
Subclavian vein
Usually approached from below clavicle
Patient positioned head down
Needle inserted below junction of medial 2/3 and lateral 1/3 of the
clavicle
Needle aimed towards suprasternal notch
Passes immediately behind clavicle
Vein encountered after 4-5 cm
Normal CVP Waveform:
- A wave: due to the increased atrial
pressure during right atrial
contraction correlates with P wave
on EKG.
- C wave: caused by slight elevation
of the tricuspid valve into the right
atrium during early ventricular
contraction correlated with the end
of QRS complex.
- X descent: caused by downward movement of the ventricular during
systolic contraction, occurred before the T wave in EKG.
- V wave: arises from the pressure produced when the blood filling the
right atrium comes up against a closed tricuspid valve correlated with
the end of T wave.
- Y descent: produced by the opening of tricuspid valve in diastole with
the blood flowing into the right ventricle, it occurs before the P wave in
EKG.
Monitoring During Anesthesia 10
Anesthesia Teamwork 432
2. Respiratory Monitoring (1)
A. Pulse Oximetry
Pulse oximeter is mandatory for all anesthetic, including cases of moderate sedation. It
measures the oxygen saturation in arterial blood. In addition to SpO2, pulse oximeters
provide an indication of tissue perfusion (pulse amplitude) and measure heart rate, and
provide rapid diagnosis of hypoxia. Clinically detectable cyanosis requires 5 g of
desaturated hemoglobin and SpO2 less than 80%.
B. Capnography
Determination of end-tidal CO2 (ETCO2) concentration to confirm adequate ventilation
is mandatory during all anesthetic procedures, but particularly so for general
anesthesia. A rapid fall in ETCO2 is a sensitive indicator of air embolism.
C. Stethoscope
Used with the placement of endotracheal tube to hear the breath sounds clearly with
with the delivery of oxygen into the ET tube with correct placement, it can be used in
placement of nasogastric (NG) tube.
Monitoring During Anesthesia 11
Anesthesia Teamwork 432
3. Neurological Monitors (1)
A. Electroencephalogram EEG
The electroencephalogram is occasionally used during cerebrovascular surgery to
confirm the adequacy of cerebral oxygenation. It is a recording of electrical potentials
generated by cells in the cerebral cortex.
- Normal EEG waves (2,3):
Beta waves: frequency greater than 13
Hz, seen in all age groups, normally
found when you are alert or have taken
high doses of certain medications like
benzodiazepines and barbiturates.
Alpha waves: frequency 8-13 Hz, seen in
all age group but commonly in adults,
present only in the waking state when
your eyes are closed but mentally alert.
They disappear with attention (stress,
opening eyes).
Theta waves: frequency 3.5-7.5 Hz, they
are normally found when you are sleeping
or in young children. Theta and delta
waves are known collectively as slow
waves.
Delta waves: frequency 3 Hz or less, seen
normally in deep sleep in adults as well as
in infants and children.
Wakefulness is indicated by bispectral
index (BIS), used to prevent awareness
during anesthesia.
Monitoring During Anesthesia 12
Anesthesia Teamwork 432
4. Temperature (1)
Postoperative temperature is used as a quality anesthesia indicator. Hypothermia is
associated with delayed drug metabolism, increased blood glucose, vasoconstriction,
impaired coagulation, and impaired resistance to surgical infections.
Hyperthermia have deleterious effects perioperatively, leading to tachycardia,
vasodilation, and neurological injury.
The temperature is measured using thermistor or thermocouple.
5. Urine Output (1)
Urinary bladder catheter is the only reliable method for monitoring urinary output.
Insertion of a urinary catheter is indicated in patients with congestive heart failure,
renal failure, advanced hepatic disease, or shock.
It is a routine in some surgical procedures such as cardiac and aortic surgeries, renal
vascular surgery, major abdominal surgery, or procedures in which large fluid shifts are
expected.
It should not be done in patients with high risk of infections.
6. Peripheral Nerve Stimulation (1)
Neuromuscular function should be monitored in all patients receiving intermediate or
long-acting neuromuscular blocking agents. Peripheral nerve stimulation is helpful in
assessing paralysis during rapid sequence induction or during continuous infusion of
short-acting agents, also in locating peripheral nerves for regional anesthesia.
Indications for Neuromuscular Monitoring:
1. Use of long-acting muscle relaxants
2. Abnormal pharmacokinetics of muscle relaxants (sever liver or kidney disease, severe
illness, extreme of age) Prolonged action of muscle relaxants
3. Patients with neuromuscular disease
4. Situations in which antagonizing muscle-relaxants should be avoided e.g. severe heart
disease or bronchial asthma
5. Situations in which postoperative respiratory muscle power must be maximal e.g. sever
pulmonary disease or marked obesity
6. Lengthy surgery
7. Continuous infusion of neuromuscular blocking drug
Monitoring During Anesthesia 13
Anesthesia Teamwork 432
Summary
- Monitoring of oxygenation: pulse oximeter, and make sure that you have
exposed the patient adequately to assess the color.
- Monitoring of ventilation: capnogram, chest excursion, breath sounds
auscultation, and observation of the reservoir breathing bag.
- Monitoring of circulation: noninvasive arterial blood pressure, ECG, and
heart rate.
- Monitoring of temperature: temperature probe.
- Monitoring of urine output: urinary bladder catheter.
- Monitoring of neurological function: EEG.
- Monitoring of neuromuscular function: peripheral nerve stimulation.
References
1. Morgan and Mikhails Clinical Anaesthesiology, 5th Edition.
2. Normal EEG Waveforms: http://emedicine.medscape.com/article/1139332-overview#a2
3. Electroencephalogram (EEG): http://www.webmd.com/epilepsy/electroencephalogram-eeg-
21508?page=3
For mistakes or feedback
Anesthesiateam432@hotmail.com
Monitoring During Anesthesia 14
Anesthesia Teamwork 432
Você também pode gostar
- 6min English Kids at Home PDFDocumento5 páginas6min English Kids at Home PDFJim Jose AntonyAinda não há avaliações
- 6min English Electricity PDFDocumento5 páginas6min English Electricity PDFJim Jose AntonyAinda não há avaliações
- India Today 29 June 2020 PDFDocumento76 páginasIndia Today 29 June 2020 PDFJim Jose AntonyAinda não há avaliações
- Optha: NeuroDocumento13 páginasOptha: NeuroJim Jose AntonyAinda não há avaliações
- Ocular EmergenciesDocumento4 páginasOcular EmergenciesJim Jose AntonyAinda não há avaliações
- Urinary Tract Infection in Children: Dr. Alia Al-Ibrahim Consultant Pediatric Nephrology Clinical Assistant ProfessorDocumento11 páginasUrinary Tract Infection in Children: Dr. Alia Al-Ibrahim Consultant Pediatric Nephrology Clinical Assistant ProfessorJim Jose AntonyAinda não há avaliações
- Dr. Elham Bukhari: Aediatri Nfectious IseaseDocumento56 páginasDr. Elham Bukhari: Aediatri Nfectious IseaseJim Jose AntonyAinda não há avaliações
- Ortho Team FinalDocumento221 páginasOrtho Team FinalJim Jose AntonyAinda não há avaliações
- Immunization in Children: Fahad Al ZamilDocumento44 páginasImmunization in Children: Fahad Al ZamilJim Jose AntonyAinda não há avaliações
- Common Cutaneous Infections and InfestationsDocumento28 páginasCommon Cutaneous Infections and InfestationsJim Jose AntonyAinda não há avaliações
- Acne Vulgaris and Acne Related DisordersDocumento12 páginasAcne Vulgaris and Acne Related DisordersJim Jose AntonyAinda não há avaliações
- Strabismus, Amblyopia Management and LeukocoriaDocumento19 páginasStrabismus, Amblyopia Management and LeukocoriaJim Jose AntonyAinda não há avaliações
- Hair Disorders and Pigmented Skin ConditionsDocumento8 páginasHair Disorders and Pigmented Skin ConditionsJim Jose AntonyAinda não há avaliações
- Acute Visual LossDocumento10 páginasAcute Visual LossJim Jose AntonyAinda não há avaliações
- Refractive ErrorsDocumento7 páginasRefractive ErrorsJim Jose AntonyAinda não há avaliações
- MCQ Questions May 2006Documento10 páginasMCQ Questions May 2006Jim Jose AntonyAinda não há avaliações
- Chronic Visual LossDocumento7 páginasChronic Visual LossJim Jose AntonyAinda não há avaliações
- Pleural EffusionDocumento10 páginasPleural EffusionJim Jose Antony100% (1)
- Orthopedic History Taking: DR - Kholoud Al-ZainDocumento30 páginasOrthopedic History Taking: DR - Kholoud Al-ZainJim Jose AntonyAinda não há avaliações
- Investigations of Lung DiseasesDocumento14 páginasInvestigations of Lung DiseasesJim Jose AntonyAinda não há avaliações
- GoutDocumento1 páginaGoutJim Jose AntonyAinda não há avaliações
- COPD and BronchiectasisDocumento20 páginasCOPD and BronchiectasisJim Jose AntonyAinda não há avaliações
- Diagnostic Criteria For Urinary Tract InfectionDocumento2 páginasDiagnostic Criteria For Urinary Tract InfectioncandyslibioAinda não há avaliações
- Medicine Annotated Multiple ChoiceDocumento20 páginasMedicine Annotated Multiple ChoiceJim Jose AntonyAinda não há avaliações
- Cardiology Disease List PDFDocumento139 páginasCardiology Disease List PDFJim Jose AntonyAinda não há avaliações
- Anatomy of The Nose Nasopharynx and Paranasal Sinuses PDFDocumento7 páginasAnatomy of The Nose Nasopharynx and Paranasal Sinuses PDFJim Jose AntonyAinda não há avaliações
- History and Physical Exam of Depressed College StudentDocumento6 páginasHistory and Physical Exam of Depressed College StudentJim Jose AntonyAinda não há avaliações
- Paranasal SinusesDocumento7 páginasParanasal SinusesJim Jose AntonyAinda não há avaliações
- Motor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistDocumento36 páginasMotor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistJim Jose Antony100% (1)
- Pediatric History FormDocumento2 páginasPediatric History FormJim Jose AntonyAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Preventing Mosquito BitesDocumento1 páginaPreventing Mosquito BitesmkumAinda não há avaliações
- Glossary of Terms 2nd PartDocumento2 páginasGlossary of Terms 2nd Part2DJoyce D.N CapacieteAinda não há avaliações
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDocumento17 páginasRajiv Gandhi University of Health Sciences, Bangalore, KarnatakayashramawatAinda não há avaliações
- Nakshatra DhanishtaDocumento7 páginasNakshatra DhanishtaANTHONY WRITER100% (3)
- COVID-19 Vaccination Certificate from India's Ministry of HealthDocumento1 páginaCOVID-19 Vaccination Certificate from India's Ministry of Healthbliss bAinda não há avaliações
- Klenner Protocol For 2013Documento10 páginasKlenner Protocol For 2013jcoppala4476Ainda não há avaliações
- Deficiency Diseases InformationDocumento4 páginasDeficiency Diseases InformationJasvinder SinghAinda não há avaliações
- 3911515Documento1 página3911515Gemmelle CangcoAinda não há avaliações
- 7 Vs 14days Gram Negative SepsisDocumento8 páginas7 Vs 14days Gram Negative SepsisPavan KumarAinda não há avaliações
- You Might Need SomebodyDocumento11 páginasYou Might Need SomebodyHans georg NeyAinda não há avaliações
- Manual of TB and Leprosy in TanzaniaDocumento132 páginasManual of TB and Leprosy in TanzaniaYovanRivanzahAinda não há avaliações
- Pharmacographia IndicaDocumento615 páginasPharmacographia IndicaSatish Vaidya100% (1)
- Review on Ayurvedic Concept of Srotas ChannelsDocumento4 páginasReview on Ayurvedic Concept of Srotas ChannelsmikikiAinda não há avaliações
- Paediatric Examination Handbook 2015Documento66 páginasPaediatric Examination Handbook 2015Ulfa Rahmadanti SetiawanAinda não há avaliações
- Setting up MRI Scan CentresDocumento86 páginasSetting up MRI Scan CentresGokilavani RajagopalAinda não há avaliações
- 2021-07-31 New Scientist International EditionDocumento62 páginas2021-07-31 New Scientist International EditionDuc Anh DinhAinda não há avaliações
- Report On Etiology, Epidemiology, Clinic, DD, Treatment, Profilaxis of Typhoid Fever & ParathyphoidDocumento3 páginasReport On Etiology, Epidemiology, Clinic, DD, Treatment, Profilaxis of Typhoid Fever & ParathyphoidAdnan Akram, MD (Latvia)Ainda não há avaliações
- Safety and Health Risk Register v1 6Documento17 páginasSafety and Health Risk Register v1 6Tri SubaktiAinda não há avaliações
- Effect of Intravenous Pamidronate Treatment in Children With Osteogenesis ImperfectaDocumento5 páginasEffect of Intravenous Pamidronate Treatment in Children With Osteogenesis Imperfectavikash singhAinda não há avaliações
- Kertas Kerja PinjamanDocumento18 páginasKertas Kerja PinjamanWan AzmanAinda não há avaliações
- Full Download High Acuity Nursing 6th Edition Wagner Test BankDocumento18 páginasFull Download High Acuity Nursing 6th Edition Wagner Test Bankassapancopepodmhup100% (38)
- ArthropodaDocumento36 páginasArthropodatapas kunduAinda não há avaliações
- Diabetic KetoacidosisDocumento7 páginasDiabetic KetoacidosisetengAinda não há avaliações
- The Neuro Metabolic Summit - TranscriptsDocumento35 páginasThe Neuro Metabolic Summit - TranscriptsIONUT GRIGOROVAinda não há avaliações
- Clinical Tips by MastersDocumento48 páginasClinical Tips by MastersShah NoorAinda não há avaliações
- November 2, 2012 Strathmore TimesDocumento32 páginasNovember 2, 2012 Strathmore TimesStrathmore TimesAinda não há avaliações
- DNA RepairDocumento35 páginasDNA RepairAbid Al RezaAinda não há avaliações
- 1536106348Documento144 páginas1536106348Saman SarKoAinda não há avaliações
- Druid Spell ChecklistDocumento5 páginasDruid Spell Checklistfedorable1Ainda não há avaliações