Escolar Documentos
Profissional Documentos
Cultura Documentos
Afina Thara P - UNAIR
Enviado por
Thara Pitaloka Vreundschap0 notas0% acharam este documento útil (0 voto)
38 visualizações6 páginasini merupakan contoh literature review
Título original
Afina Thara P_UNAIR
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoini merupakan contoh literature review
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
38 visualizações6 páginasAfina Thara P - UNAIR
Enviado por
Thara Pitaloka Vreundschapini merupakan contoh literature review
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 6
Indonesia International (Bio)Medical Students Congress
2017
Intravenous delivery of bone marrow-derived
mesenchymal stem cells (BM-MSCs) enhances
functional recovery and brain repair markers in
ischemic stroke
Afina Thara Pitaloka*, Ramadhanti Salma Ulwanda** and Nuzula Fikrin
Nabila***
* Third Year Medical Student, Universitas Airlangga, (finapitaloka@gmail.com)
** Third Year Medical Student, Universitas Airlangga, (ulwanda@gmail.com)
*** Third Year Medical Student, Universitas Airlangga,
(fkrnnabila@gmail.com)
Correspondent author : Afina Thara Pitaloka (+628983887521, Faculty of
Medicine, Airlangga University, Mayjen Prof. Dr. Moestopo 47, Surabaya,
finapitaloka@gmail.com)
Abstract
Stroke is a major contributor to the noncommunicable diseases worldwide. As one of
the neurodegenerative diseases, stroke causes loss of brain parenchyma and neurons,
astrocytes, oligodendrocytes and endothelial cells. Ischemic strokes as one of the
types of stroke account for about 80-85% of all strokes. Nowadays, there is a lack of
effective treatment to promote tissue repair and functional recovery after the
ischemic attack. Thus, strategies such as cell-based therapies with mesenchymal
stem cells (MSCs) pave the way for new treatment options for stroke. Bone marrow-
derived mesenchymal stem cells (BM-MSCs) therapy is one of the most promising
methods to treat and promote recovery from ischemic stroke. This literature review
aims to evaluate the therapeutic potential of BM-MSCs in ischemic stroke. Studies
showed that intravenous administration of BM-MSCs significantly improved
function and also increased the level of vascular endothelial growth factor (VEGF),
synaptophysin, oligodendrocyte (Olig-2) and neurofilament. Furthermore, MSCs
have many advantages. MSCs can be obtained, amplified, and stored for immediate
use after stroke. MSCs also do not express Major histocompatibility complex II
(MCH-II), so it could minimize the risk of rejection in patients.
Keywords: bone marrow; intravenous; ischemic stroke; mesenchymal stem cells.
Introduction types relevant to repair, modulate the
immune system, promote neurogenesis,
Stroke is a major contributor to the and secrete neuroprotective factors.1,3,4
global non-communicable diseases. Another research also suggests that the
About 15 million people suffer from reduction of inflammatory component
stroke, with approximately six millions complement 3 (C3) expression by
of deaths annually. In the US, 87% MSCs can help to alleviate ischemic
strokes account as ischemic stroke. brain damage, and can be used for a
Combining the expectation that the new neuroprotective strategy in stroke
number of people over the age of 65 therapy.4,5
will double by 2030, and that the risk
of suffering a stroke doubles for each This literature review aims to discuss
decade over the age of 55, will even the usage of BM-MSCs given
lead to a further increase in patient intravenously for the treatment of
numbers with permanent disabilities ischemic stroke.
and socioeconomic burden.1 Stroke
causes loss of brain parenchyma and Materials and Methods
neurons, astrocytes, oligodendrocytes
and endothelial cells.2,3 We have done a systematic literature
search for relevant clinical researches
Ischemic stroke is most frequently and reviews published between 2008
caused by thromboembolisms while and 2017 using Pubmed, ScienceDirect
hemorrhagic stroke most often results and Google Scholar. The search
from vessel wall pathology associated strategy consisted of MeSH (medical
with hypertension and subject heading) words and keywords
microaneurysms. This review will only related to the disease. Search words
focus on ischemic stroke as the main were 'bone marrow', 'intravenous' or
pathology. The specific therapies 'iv', 'ischemic stroke', and
currently used for ischemic stroke 'mesenchymal stem cells'. All studies
management are intervention to prevent about bone marrow mesenchymal stem
inappropriate coagulation, surgical cells were included. We excluded
procedures to repair vascular publications which were not in English.
abnormalities, and thrombolytic
therapy.2,4 Despite the high burden of Result and Discussion
stroke, there is still a lack of effective
treatment to promote tissue repair and Many studies, from preclinical to
functional recovery after the ischemic clinical, have evaluated the potency of
attack.2,3 BM-MSCs in many degenerative brain
diseases, including ischemic stroke.
Stem cell therapy is one of the most BM-MSCs contribute to the formation
promising methods to treat and of hematopoietic stem cells niche that
promote recovery from ischemic supports hematopoiesis. Within the
stroke. Many studies regarding the bone marrow, MSCs can be isolated
treatment of ischemic stroke have been from other BM cells due to their
using bone marrow-derived potency to adhere to tissue culture
mesenchymal stem cells (BM-MSCs). plastic. These cells have a spindle-
BM-MSCs are promising therapy after shaped fibroblast-like morphology and
ischemic stroke because of their can be expanded and enriched by
advantageous characteristic, such as culturing for 3 to 5 weeks.3,6,7
their ability to differentiate into cell
A study evaluated the effect of response to repair processes, and this
intravenously administered BM-MSCs could amplify trophic factor levels in
(2 106 cells) 30 minutes after the brain. A study found that BM-
permanent middle cerebral artery MSCs increased cellular proliferation
occlusion (pMCAO) to rats as the and modified brain repair markers
model of ischemic stroke at 24 hours levels.1,7,8
and 14 days. It showed that BM-MSCs
therapy reduced the number of Vascular endothelial growth factor
TUNEL+ cells in the peri-infarct area (VEGF) levels were significantly
which means decreased cell death. higher in the rat brain after BM-MSCs
According to this study, at 14 days, the therapy compared with the control
untreated group showed significantly group by 4.84 (A.U.) and 2.75 (A.U.)
more TUNEL+ cells than the BM- respectively. The levels of Olig-2
MSCs group, with number of labeling were also considerably higher
TUNEL+ cells 41 6.4 and 26 5.5 than in the control group after the BM-
respectively.1,7,8 MSCs treatment with the number 2.05
(A.U.) and 2.89 (A.U.) respectively.1,7
BM-MSCs also increased cellular
proliferation after pMCAO. Recovery after stroke is a dynamic
Quantitative analysis showed that the process, and the growth and trophic
infarct group displayed a significantly factors produced by BM-MSCs may
smaller decrease in the peri-infarct affect synaptogenesis in the ischemic
zone at 14 days after focal cerebral brain. Compared with the control
ischemia than did the BM-MSCs.1,7 group, synaptophysin (SYP) levels
were also significantly increased after
A study demonstrated that infarct size BM-MSCs administration with the
measured by MRI in rats with pMCAO number 2.15 (A.U.) and 3.14 (A.U.)
does not change after administration of respectively. Lastly, neurofilament (NF)
intravenous BM-MSCs, but some levels were significantly increased
previous studies showed a decrease.1,7,8 after the BM-MSCs treatment
compared with the control group by
The study also revealed that the BM- 2.10 (A.U.) and 1.18 (A.U.)
MSCs treated groups showed good respectively. The BDNF levels were
functional recovery at 24 hours and 14 also higher after BM-MSCs therapy,
days compared with the untreated but this increase did not reach
infarct group (Figure 1).1 statistical significance. The GFAP
levels were decreased significantly
This result is in line with other studies after BM-MSCs administration in
which also showed that administration comparison with the infarct group.1,7,8
of BM-MSCs in animal models
improved sensorimotor function. In ischemic stroke, BM-MSCs
Another study also found that BM- establishes neuronal protection through
MSCs enhanced synaptogenesis and inflammatory and immune response
nerve regeneration, while decreased modulation. BM-MSCs has been
tissue plasminogen activator (tPA)- shown to upregulate interleukin-6 (IL-
induced brain damage.6,9 6) expression in a mouse model, which
probably accounts for neuroprotective
Studies found that BM-MSCs secrete a effect. Soluble factors secreted from
wide array of neurotrophins, growth BM-MSCs, such as IL-6, IL-8,
factors, cytokines and other soluble chemokine ligand 2 (CCL2), VEGF,
factors such as VEGF or BDNF, in
hepatocyte growth factor, and bone by modified Rankin scale (mRS)
morphogenetic protein-4 (BMP-4) also (Figure 2). This clinical improvement
increase maturation and survival of is believed to be associated with serum
neuron. The same research also levels of stromal cell-derived factor-
suggests that neuroprotective effect of 1.12
MSCs in cerebral ischemia is
associated with the down-regulation of Conclusion
C3 expression.5,7
The use of BM-MSCs intravenously as
In particular, intravenously injected a therapy after an ischemic attack can
BM-MSCs enter the brain and reduce ischemic damage, significantly
stimulate local production of growth improved functional recovery, and
factors from endogenous cells like increase brain repair markers. Its
astrocytes and endothelial cells. These effects on the ischemic tissues can also
growth factors lead to angiogenesis promote angiogenesis and
and vascular stabilization. Intravenous synaptogenesis through the increase of
administration of BM-MSCs leads to a VEGF, SYP, Olig-2 and NF levels.
time-dependent release of Neuroprotective effects are achieved
neurotrophins and angiogenic growth through the modulation of
factors. The production of these inflammatory and immune response.
molecules all contributes to and likely MSCs is also advantageous for their
coordinates the improvement in obtainability and can be easily
neurological function post stroke.1,7,8 amplified and stored for immediate use
when needed after an attack. They also
The use of BM-MSCs for therapies are have minimal risk of rejection because
advantageous because they are easy to of the unexpressed MCH-II.
harvest, can be quickly isolated,
expanded and stored for a period, can Further studies are necessary to explain
be administered in various ways, are the beneficial effects, efficacy, and
relatively immune-privileged, and they safety related to MSCs therapy,
may be administered through different especially in the human model. But,
methods.9,10,11 the intravenous MSCs therapy remains
as one of the most promising methods
Furthermore, it is known that BM- to treat and promote recovery from
MSCs do not express major ischemic stroke.
histocompatibility complex II (MCH-
II), thus minimizing the risk of Acknowledgement
rejection in patients and facilitates their
allogeneic administration. It possibly We would like to acknowledge the
allows BM-MSCs from healthy donors support and guidance from all
to be stored in biobanks for the mentoring lecturers.
treatment of stroke patients during the
acute phase of the disease.7,9,10 Conflict of Interest
Clinical trials in ischemic stroke The authors declare that there is no
patients showed that administration of conflict of interest in this work.
intravenous BM-MSCs is safe and no
significant side effects were observed
References
during the treatment.11,12 A study also
found that BM-MSCs therapy
improves clinical outcome measured
1. Gutirrez-Fernndez M, 7. Liu X, Ye R, Yan T, et al. Cell
Rodrguez-Frutos B, Ramos- based therapies for ischemic
Cejudo J, et al. Effects of stroke: From basic science to
intravenous administration of bedside. Progress in
allogenic bone marrow- and Neurobiology. 2014;115:92-115.
adipose tissue-derived 8. Bang O. Clinical Trials of Adult
mesenchymal stem cells on Stem Cell Therapy in Patients
functional recovery and brain with Ischemic Stroke. Journal of
repair markers in experimental Clinical Neurology.
ischemic stroke. Stem Cell 2016;12(1):14.
Research & Therapy. 9. Bang O. Clinical Trials of Adult
2013;4(1):11. Stem Cell Therapy in Patients
2. Jeong C, Kim S, Lim J, et al. with Ischemic Stroke. 2017.
Mesenchymal Stem Cells 10. Tanna T, Sachan V.
Expressing Brain-Derived Mesenchymal Stem Cells:
Neurotrophic Factor Enhance Potential in Treatment of
Endogenous Neurogenesis in an Neurodegenerative Diseases.
Ischemic Stroke Model. BioMed Current Stem Cell Research &
Research International. Therapy. 2014;9(6):513-521.
2014;2014:1-10. 11. Friedrich M. Intra-Arterial
3. Dulamea A. The potential use of Infusion of Autologous Bone-
mesenchymal stem cells in stroke Marrow Mononuclear Cells in
therapyFrom bench to bedside. Patients with Moderate to Severe
Journal of the Neurological Middle-Cerebral-Artery Acute
Sciences. 2015;352(1-2):1-11. Ischemic Stroke. Cell
4. Gervois P, Wolfs E, Ratajczak J, Transplantation. 2012.
et al. Stem Cell-Based Therapies 12. Lee J, Hong J, Moon G, et al. A
for Ischemic Stroke: Preclinical Long-Term Follow-Up Study of
Results and the Potential of Intravenous Autologous
Imaging-Assisted Evaluation of Mesenchymal Stem Cell
Donor Cell Fate and Mechanisms Transplantation in Patients With
of Brain Regeneration. Medicinal Ischemic Stroke. STEM CELLS.
Research Reviews. 2010;28(6):1099-1106.
2016;36(6):1080-1126.
5. Jung H, Jeong S, Yang J, et al.
Neuroprotective effect of
mesenchymal stem cell through
complement component 3
downregulation after transient
focal cerebral ischemia in mice.
Neuroscience Letters.
2016;633:227-234.
6. Huang W, Mo X, Qin C, Zheng
J, Liang Z, Zhang C.
Transplantation of differentiated
bone marrow stromal cells
promotes motor functional
recovery in rats with stroke.
Neurological Research.
2013;35(3):320-328.
Long-Term Follow-Up Study of Intravenous Autologous
Appendixes
Mesenchymal Stem Cell Transplantation in Patients With
Ischemic Stroke. STEM CELLS. 2010;28(6):1099-1106.)
Fig. 1. Acute intravenous (i.v.)
administration of bone marrow-derived
mesenchymal (BM-MSC) cells
improved functional recovery at 24 h
and 14 d after permanent middle
cerebral artery occlusion (pMCAO). 1
(Gutirrez-Fernndez M, Rodrguez-Frutos B, Ramos-
Cejudo J, Teresa Vallejo-Cremades M, Fuentes B, Cerdn
S et al. Effects of intravenous administration of allogenic
bone marrow- and adipose tissue-derived mesenchymal
stem cells on functional recovery and brain repair markers
in experimental ischemic stroke. Stem Cell Research &
Therapy. 2013;4(1):11.)
Fig. 2. Proportion of patients in the
control and MSC group according to
the mRS at day 7 of admission and last
evaluation. 12 (Lee J, Hong J, Moon G, et al. A
Você também pode gostar
- AmrapDocumento128 páginasAmraphijackerAinda não há avaliações
- Critical Care Medicine An Algorithmic Approach 2023Documento335 páginasCritical Care Medicine An Algorithmic Approach 2023Ahmed AbusalabAinda não há avaliações
- Data CollectionDocumento9 páginasData Collectionapi-512131053Ainda não há avaliações
- Clinic Trăilă of StemDocumento22 páginasClinic Trăilă of StemRadu AvramAinda não há avaliações
- Among Mesenchymal Stem Cells For The Best Therapy After Ischemic StrokeDocumento3 páginasAmong Mesenchymal Stem Cells For The Best Therapy After Ischemic Strokeaburachman24Ainda não há avaliações
- BstractDocumento9 páginasBstractmerosaber622001Ainda não há avaliações
- 2021 Front. Cell Dev. Biol. Laundos TL Et Al.Documento15 páginas2021 Front. Cell Dev. Biol. Laundos TL Et Al.PerpetuaAinda não há avaliações
- Bone Marrow Mesenchymal Stem Cell-Derived ExosomesDocumento9 páginasBone Marrow Mesenchymal Stem Cell-Derived Exosomesiam_ca2Ainda não há avaliações
- Cell Therapy in Patients With Critical Limb IschemiaDocumento27 páginasCell Therapy in Patients With Critical Limb IschemiaAsep HrAinda não há avaliações
- Neuroasia 2023 28 (4) 857Documento10 páginasNeuroasia 2023 28 (4) 857B VeerendrasaiAinda não há avaliações
- Pharmaceuticals 13 00031Documento18 páginasPharmaceuticals 13 00031DwitaRiadiniAinda não há avaliações
- Xin 2013Documento5 páginasXin 2013Maximiliano PfannlAinda não há avaliações
- SCCAA 7820 Mesenchymal Stem Cells in The Treatment of Ischemic Stroke 111110Documento7 páginasSCCAA 7820 Mesenchymal Stem Cells in The Treatment of Ischemic Stroke 111110Nur FitriahAinda não há avaliações
- Bioengineering The Infarcted Heart by Applying Bio-Inspired MaterialsDocumento16 páginasBioengineering The Infarcted Heart by Applying Bio-Inspired MaterialsMhandu EsauAinda não há avaliações
- 506626v1 FullDocumento17 páginas506626v1 FullShourya SONI (11C)Ainda não há avaliações
- Stem Cell Implants Emerging Innovation For Stroke RecoveryDocumento14 páginasStem Cell Implants Emerging Innovation For Stroke RecoveryAthenaeum Scientific PublishersAinda não há avaliações
- Angoulvant Et Al. - 2011 - Mesenchymal Stem Cell Conditioned Media Attenuates in Vitro and Ex Vivo Myocardial Reperfusion InjuryDocumento8 páginasAngoulvant Et Al. - 2011 - Mesenchymal Stem Cell Conditioned Media Attenuates in Vitro and Ex Vivo Myocardial Reperfusion Injuryscribd mendeleyAinda não há avaliações
- Human Mesenchymal Stem Cell-Conditioned Medium Improves Cardiac Function Following Myocardial InfarctionDocumento9 páginasHuman Mesenchymal Stem Cell-Conditioned Medium Improves Cardiac Function Following Myocardial InfarctionSigit Harya HutamaAinda não há avaliações
- Brain HemorrhagesDocumento10 páginasBrain HemorrhagesRadu AvramAinda não há avaliações
- Cellular Therapies For Treating Pain Associated With Spinal Cord InjuryDocumento14 páginasCellular Therapies For Treating Pain Associated With Spinal Cord InjuryWinni FebriariAinda não há avaliações
- Mesenchymal Stromal Cells: Potential For Cardiovascular RepairDocumento19 páginasMesenchymal Stromal Cells: Potential For Cardiovascular RepairardhanputraAinda não há avaliações
- 2019 Article 73Documento10 páginas2019 Article 73Radu AvramAinda não há avaliações
- Stemcell CardiovascularDocumento29 páginasStemcell CardiovascularAdi WijayantoAinda não há avaliações
- Role of CiticolineDocumento20 páginasRole of CiticolinesylviaAinda não há avaliações
- Fneur 12 639315Documento13 páginasFneur 12 639315Muhammad Naqvi Al FarisiAinda não há avaliações
- Jurnal Stem CellDocumento11 páginasJurnal Stem CellprimaswariAinda não há avaliações
- NeuralRegenRes114559-8526593 234105Documento2 páginasNeuralRegenRes114559-8526593 234105JouleAlSBAinda não há avaliações
- Review Article: Neuroprotective Effects of Stem Cells in Ischemic StrokeDocumento7 páginasReview Article: Neuroprotective Effects of Stem Cells in Ischemic StrokesalmaAinda não há avaliações
- Skeletal MuscleDocumento11 páginasSkeletal MuscleStefania CristinaAinda não há avaliações
- Effect of The Conditioned Medium of Mesenchymal Stem Cells On The Expression Levels of P2X4 and P2X7 Purinergic Receptors in The Spinal Cord of Rats With Neuropathic PainDocumento8 páginasEffect of The Conditioned Medium of Mesenchymal Stem Cells On The Expression Levels of P2X4 and P2X7 Purinergic Receptors in The Spinal Cord of Rats With Neuropathic Painmatheus derocoAinda não há avaliações
- Annotated New20stem20how20method20be20to20heart20failureDocumento21 páginasAnnotated New20stem20how20method20be20to20heart20failureapi-583335284Ainda não há avaliações
- MachalDocumento5 páginasMachalMinh Vương NguyễnAinda não há avaliações
- Inflamation N StrokeDocumento30 páginasInflamation N StrokeNona Suci rahayuAinda não há avaliações
- Therapeutic Effect of Human Adipose-Derived Stem Cells and Their Secretome in Experimental Diabetic PainDocumento15 páginasTherapeutic Effect of Human Adipose-Derived Stem Cells and Their Secretome in Experimental Diabetic Painmatheus derocoAinda não há avaliações
- MSC Reduces Il-6 Gene Expression in AdDocumento16 páginasMSC Reduces Il-6 Gene Expression in AdFarhan Royan PermanahadiAinda não há avaliações
- Jurnal 6Documento11 páginasJurnal 6ichamarichaAinda não há avaliações
- Stem Cell For Cardiac RepairDocumento9 páginasStem Cell For Cardiac RepairAdi WijayantoAinda não há avaliações
- jcm-08-00537 YDA 7Documento11 páginasjcm-08-00537 YDA 7Muhammad Sandy Ali YafieAinda não há avaliações
- Therapeutic Cardiac Patches: BY Leah Sabu: 1Ms20Bt026 VIVEK T.R: 1MS20BT060Documento16 páginasTherapeutic Cardiac Patches: BY Leah Sabu: 1Ms20Bt026 VIVEK T.R: 1MS20BT060Vivek TRAinda não há avaliações
- 2023 - Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage - A Dose-Escalation Safety and Tolerability TrialDocumento11 páginas2023 - Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage - A Dose-Escalation Safety and Tolerability TrialOlga Manco GuzmánAinda não há avaliações
- Cell Tracking in Cardiac RepairDocumento16 páginasCell Tracking in Cardiac RepairdeadcorpsesAinda não há avaliações
- Mjms RtmsDocumento10 páginasMjms RtmsMuhammad Hafiz HanafiAinda não há avaliações
- Contemporary Biological Therapies For Cardiovascular Diseases MMH Nuri Ahmad YahyaDocumento6 páginasContemporary Biological Therapies For Cardiovascular Diseases MMH Nuri Ahmad YahyaHammad. A Rehan ACCAAinda não há avaliações
- 10 1126@scitranslmed Aah6510Documento14 páginas10 1126@scitranslmed Aah6510翁子貽Ainda não há avaliações
- Transcranial Photobiomodulation Therapy in The Cognitive - Photob.2019.4683Documento10 páginasTranscranial Photobiomodulation Therapy in The Cognitive - Photob.2019.4683Viviane MarquesAinda não há avaliações
- NIH Public AccessDocumento16 páginasNIH Public AccessJarmy BjAinda não há avaliações
- Protective Effect of MitoTEMPO Against Cardiac Dysfunction Caused by Ischemia Reperfusion MCAO Stroke Model StudyDocumento13 páginasProtective Effect of MitoTEMPO Against Cardiac Dysfunction Caused by Ischemia Reperfusion MCAO Stroke Model StudyyusranurparlakAinda não há avaliações
- Exosomes Derived From Mir-26A-Modified Mscs Promote Axonal Regeneration Via The Pten/Akt/Mtor Pathway Following Spinal Cord InjuryDocumento15 páginasExosomes Derived From Mir-26A-Modified Mscs Promote Axonal Regeneration Via The Pten/Akt/Mtor Pathway Following Spinal Cord Injuryelif.onsozAinda não há avaliações
- Secretome of Mesenchymal Stromal Cells As A Possible Innovative Therapeutic Tools in Facial Nerve Injury TreatmentDocumento7 páginasSecretome of Mesenchymal Stromal Cells As A Possible Innovative Therapeutic Tools in Facial Nerve Injury TreatmentIgor HermandoAinda não há avaliações
- Acupuncture Therapy in Ischemic Stroke RehabilitationDocumento12 páginasAcupuncture Therapy in Ischemic Stroke RehabilitationcocosinghAinda não há avaliações
- 04 Wang 2015Documento8 páginas04 Wang 2015Andrei BicanAinda não há avaliações
- Human Induced Pluripotent Stem Cell-Derived Cardiomyocytes: ReviewDocumento9 páginasHuman Induced Pluripotent Stem Cell-Derived Cardiomyocytes: ReviewCinsley GentillonAinda não há avaliações
- Profiling Mikrorna Post InjeksiDocumento4 páginasProfiling Mikrorna Post InjeksiHARIAinda não há avaliações
- Mesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)Documento25 páginasMesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)flying highAinda não há avaliações
- Ijms 23 03482 v2Documento26 páginasIjms 23 03482 v2Ravi Kant TripathiAinda não há avaliações
- Assingement#2 Stem CellDocumento6 páginasAssingement#2 Stem Cellhaseeb ShafaatAinda não há avaliações
- Wu Et Al-2007-Stem CellsDocumento12 páginasWu Et Al-2007-Stem CellsNinanu Nida-nnAinda não há avaliações
- Stem Cell Therapy For Ischemic Heart Diseases: Invited ReviewDocumento20 páginasStem Cell Therapy For Ischemic Heart Diseases: Invited ReviewChristian MollericonaAinda não há avaliações
- Bài Báo 1Documento9 páginasBài Báo 1doainhi28062002Ainda não há avaliações
- Tissue Engineering and Regeneration in Dentistry: Current StrategiesNo EverandTissue Engineering and Regeneration in Dentistry: Current StrategiesRachel J. WaddingtonAinda não há avaliações
- Multiple Sclerosis: Practical Comprehensive EssentialsNo EverandMultiple Sclerosis: Practical Comprehensive EssentialsAinda não há avaliações
- A Roadmap to Nonhematopoietic Stem Cell-Based Therapeutics: From the Bench to the ClinicNo EverandA Roadmap to Nonhematopoietic Stem Cell-Based Therapeutics: From the Bench to the ClinicNota: 5 de 5 estrelas5/5 (1)
- Kegawatan Pada Diare Dehidrasi BeratDocumento40 páginasKegawatan Pada Diare Dehidrasi BeratAkram BatjoAinda não há avaliações
- DVand Video ArthroscopesDocumento2 páginasDVand Video Arthroscopesapi-19808945Ainda não há avaliações
- Inflammatory Arthritis (SDD)Documento45 páginasInflammatory Arthritis (SDD)Fera MulidarAinda não há avaliações
- PIL 18047 LatestDocumento2 páginasPIL 18047 LatestWendy EscalanteAinda não há avaliações
- Silver Is The New BlackDocumento30 páginasSilver Is The New BlackSeptriyani KaswindiartiAinda não há avaliações
- Clinical Abstract FormDocumento1 páginaClinical Abstract FormHihiAinda não há avaliações
- Alprazolam Effect On ThyroidDocumento7 páginasAlprazolam Effect On ThyroidswatiAinda não há avaliações
- Obstruktive Sleep ApneaDocumento29 páginasObstruktive Sleep ApneaEfri SyaifullahAinda não há avaliações
- Perdarahan Intra Dan Extra AxialDocumento19 páginasPerdarahan Intra Dan Extra AxialFarmasi FKUNSAinda não há avaliações
- Immunity Mark SchemeDocumento6 páginasImmunity Mark SchemeDAinda não há avaliações
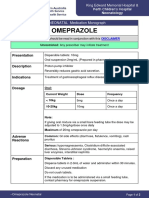
- OmeprazoleDocumento2 páginasOmeprazolephawphawphawAinda não há avaliações
- Bronchial AsthmaDocumento40 páginasBronchial Asthmasamson bd mokuntil100% (1)
- Pre-Diabetes:: Don't Let It Lead To Type-2Documento1 páginaPre-Diabetes:: Don't Let It Lead To Type-2ARIA MINDAinda não há avaliações
- Parts of The Body and Health ProblemDocumento13 páginasParts of The Body and Health ProblemSonia Tri AgustinaAinda não há avaliações
- Intestinal Malrotation and VolvulusDocumento14 páginasIntestinal Malrotation and VolvulusSaf Tanggo Diampuan100% (1)
- Homeopathic Remedies For Kidney Stones - HompathDocumento5 páginasHomeopathic Remedies For Kidney Stones - HompathBGAinda não há avaliações
- Précision P2D Par CalquesDocumento1 páginaPrécision P2D Par CalquesamineAinda não há avaliações
- Klinefelters SyndromeDocumento2 páginasKlinefelters SyndromeAlexandra Gabriella ZawisnyAinda não há avaliações
- Nursing Practice IDocumento45 páginasNursing Practice IWilmaBongotanPadawilAinda não há avaliações
- An Approach To The Management of Hyperbilirubinemia in The Preterm Infant Less Than 35 Weeks of GestationDocumento5 páginasAn Approach To The Management of Hyperbilirubinemia in The Preterm Infant Less Than 35 Weeks of Gestationberthad33Ainda não há avaliações
- 2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Documento16 páginas2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Jakob AndradeAinda não há avaliações
- DAFTAR PUSTAKA Rachel ParasianDocumento3 páginasDAFTAR PUSTAKA Rachel ParasianAnto TomodachiRent SusiloAinda não há avaliações
- 861 Drug Prescribing For Dentistry 2 Web 2 Email PDFDocumento94 páginas861 Drug Prescribing For Dentistry 2 Web 2 Email PDFRaphaela TravassosAinda não há avaliações
- Rose Pharmacy JaipurDocumento6 páginasRose Pharmacy JaipurAmit KochharAinda não há avaliações
- Neuropediatric ExaminationDocumento43 páginasNeuropediatric ExaminationShaniaAinda não há avaliações
- Duchenne Muscular DystrophyDocumento9 páginasDuchenne Muscular Dystrophyapi-306057885Ainda não há avaliações
- 1.halliwck Child Principios - Halliwick - en - Nino PDFDocumento7 páginas1.halliwck Child Principios - Halliwick - en - Nino PDFmuhammad yaminAinda não há avaliações
- WC500059147 PDFDocumento140 páginasWC500059147 PDFAnaStankovićAinda não há avaliações