Escolar Documentos
Profissional Documentos
Cultura Documentos
6
Enviado por
cliffwinskyDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
6
Enviado por
cliffwinskyDireitos autorais:
Formatos disponíveis
6.1.
Age
Patients belonging to younger age group have been found to be at higher risk for anti-TB-DIH [7].
However, several studies suggested that increasing age is a potential risk factor for anti- TB-DIH [53, 54].
One study reported that the rate of anti-TB-DIH ranges from 2 to 8% as age increases, with an average of
5% [55]. Other studies reported that hepatotoxicity ranges from 22 to 33% in patients older than 35 years
compared with a range from 8 to 17% in those younger than 35 years [22, 56]. Also, Mahmood et al.
(2007) reported that older age group was affected more than the younger age group for anti-TB-DIH (25.8
and 14.4%, respectively) [57]. Marazuki et al. (2008) reported no significant association between age and
the risk of developing anti-TB-DIH [58].
6.2. Sex
Anti-TB-DIH was found to be closely associated with female sex [59]. Though, some studies showed no
increased risk of anti-TB-DIH in women [60, 33]. Several studies report females at an increased risk of
anti-TB-DIH as compared to males [53, 54]. Mahmood et al. (2007) reported a higher incidence of anti-
TB-DIH in females than males (26.3% vs. 19.7%) [57]. Female gender was also considered to be one of
the potential risk factors contributing to the high incidence of anti-TB-DIH by Singh et al. (1996) [61].
Difference in DIH incidences between males and females is mainly attributed to slow acetylator status of
females, due to which, females are more predisposed to the risk of hepatotoxicity [62].
6.3. Malnutrition
Malnutrition (detected by Body Mass Index 18.5 kg/m2) is the leading risk factor globally in terms of the
burden of anti-TB-DIH [57, 55]. According to Saukkonen et al. (2006), patients with low BMI had
increased incidence of anti-TB-DIH [63]. A study in India showed that the incidence of anti-TB-DIH was
found to be three times higher in malnourished patients as compared to healthy controls [20].
6.4. Pre-existing liver disease
Pre-existing liver disease is also a potential risk factor for anti-TB-DIH. An increased risk of
hepatotoxicity during TB treatment was observed in patients with pre-existing liver disease (abnormal
baseline transaminases) [64, 65]. Hepatitis B virus (HBV) and/or hepatitis C virus (HCV) infections are
common causes of the chronic liver disease that is frequently seen in populations at risk for TB infection.
Several studies show that HBV and HCV co-infection increase the risk of anti-TB-DIH [28, 66]. A study
on 128 patients in Florida, showed that approximately 30% of HCV infected individuals developed anti-
TB-DIH compared with 11% among uninfected individuals and HCV infection was an independent risk
factor for the development of hepatotoxicity [52].
6.5. HIV/AIDS
HIV infection increases the risk of hepatotoxicity during standard multidrug treatment of TB [18].
Marzuki et al. (2008) found that HIV was a significant independent risk factor for developing anti-TB-
DIH [58]. Similarly, Ungo et al. (1998) observed that infection with HIV is responsible for increased risk
of anti-TB-DIH [52]. HIV patients with acute illnesses have altered activities of oxidative pathways,
which may partly explain their increased risk of anti-TB-DIH [67]. Concurrent therapy of TB/HIV co-
infection requires concomitant use of two to four different anti-TB drugs and at least three antiretroviral
drugs. Unfortunately, combined TB/HIV treatment is often complicated by overlapping toxicities and
drugdrug interactions [68]. The simultaneous use of antifungals (e.g. fluconazole) in HIV-infected
patients, is also a risk factor for anti-TB-DIH [69]. Increased risk of anti-TB-DIH in HIV patients may be
related to an underlying viral replication or the immunocompromised state [19]. Severe TB infection in
HIVinfected patients may be one of the reasons for their higher risk of anti-TB-DIH [20].
6.6. Anti-TB-DIH and oxidative stress
Studies have shown that anti-TB-DIH is primarily due to oxidative stress, caused by the drugs and
metabolites [70]. The role of oxidative stress in the mechanism of INH and RIF-induced hepatitis has also
been reported by Attri et al. (2000) [71]. In experimental rats oxidative stress has been proved a major
mechanism of hepatotoxicity due to anti-TB drugs [72]. According to Funde et al. (2013) oxidative stress
due to free radical generation and subsequent lipid peroxidation of membrane play a critical role in the
pathogenesis of drug induced liver injury [73].
Oxidative stress is an unbalanced state characterized by an increased production of reactive oxygen
species (ROS) and decreased level of antioxidants. In the liver, hepatotoxic metabolites of anti-TB drugs
induce increased ROS generation that activates intracellular antioxidant defence mechanisms including
antioxidants such as glutathione (GSH) and superoxide dismutase (SOD). The altered levels of
antioxidant enzymes critically influence the susceptibility of various tissues to oxidative stress and are
associated with the development of liver complications. [Figure-4].
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Reconstruction of Defects of The Posterior Pinna.15Documento4 páginasReconstruction of Defects of The Posterior Pinna.15cliffwinskyAinda não há avaliações
- Lesson Plan 3Documento4 páginasLesson Plan 3api-253402286Ainda não há avaliações
- 16.00 DR Neil Baldwin, Management of StrokeDocumento57 páginas16.00 DR Neil Baldwin, Management of Strokeamir ahmadAinda não há avaliações
- HIMSS EMRAM CriteriaDocumento2 páginasHIMSS EMRAM CriteriaReinhard Harianja100% (1)
- Aklan Polytechnic College: Performance Rating ScaleDocumento3 páginasAklan Polytechnic College: Performance Rating ScaleShane DamianAinda não há avaliações
- Perbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaDocumento5 páginasPerbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaTeguh_Yudha_Adi_WijaAinda não há avaliações
- Anaesthesia For Laparoscopic SurgeryDocumento4 páginasAnaesthesia For Laparoscopic SurgeryRubén Darío HerediaAinda não há avaliações
- Ni Hms 777674Documento13 páginasNi Hms 777674cliffwinskyAinda não há avaliações
- NFT 1Documento2 páginasNFT 1cliffwinskyAinda não há avaliações
- Tropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakaDocumento2 páginasTropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakacliffwinskyAinda não há avaliações
- FSFSFSDFDocumento7 páginasFSFSFSDFcliffwinskyAinda não há avaliações
- Kikel JurnalDocumento4 páginasKikel JurnalcliffwinskyAinda não há avaliações
- Lisence Agreement Fine CollegeDocumento2 páginasLisence Agreement Fine Collegedidididididididi1234Ainda não há avaliações
- Tropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakaDocumento2 páginasTropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakacliffwinskyAinda não há avaliações
- Perbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaDocumento5 páginasPerbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaTeguh_Yudha_Adi_WijaAinda não há avaliações
- Follow UpDocumento5 páginasFollow UpcliffwinskyAinda não há avaliações
- 3.05 Potential Cancer Risk IRSN PaperDocumento8 páginas3.05 Potential Cancer Risk IRSN PapercliffwinskyAinda não há avaliações
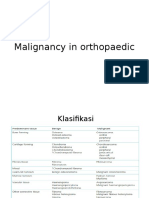
- Malignancy in OrthopaedicDocumento14 páginasMalignancy in OrthopaediccliffwinskyAinda não há avaliações
- Morning Report InternaDocumento14 páginasMorning Report InternacliffwinskyAinda não há avaliações
- 56 CBT For OCD 2007Documento9 páginas56 CBT For OCD 2007cliffwinskyAinda não há avaliações
- S0733861911X00026 S073386191000157X MainDocumento19 páginasS0733861911X00026 S073386191000157X MaincliffwinskyAinda não há avaliações
- Effect of Rosuvastatin On Cytokines After TraumaticDocumento7 páginasEffect of Rosuvastatin On Cytokines After TraumaticcliffwinskyAinda não há avaliações
- 3.05 Potential Cancer Risk IRSN PaperDocumento8 páginas3.05 Potential Cancer Risk IRSN PapercliffwinskyAinda não há avaliações
- Chest X Ray in CAPDocumento7 páginasChest X Ray in CAPsahatmanurungAinda não há avaliações
- Biology of Belief ReviewDocumento12 páginasBiology of Belief ReviewcliffwinskyAinda não há avaliações
- Chest X Ray in CAPDocumento7 páginasChest X Ray in CAPsahatmanurungAinda não há avaliações
- Cognitive Behavioral Therapy For Pediatric Obsessive CompulsivedisorderDocumento9 páginasCognitive Behavioral Therapy For Pediatric Obsessive CompulsivedisordercliffwinskyAinda não há avaliações
- Reconstruction of Defects of The Posterior PinnaDocumento11 páginasReconstruction of Defects of The Posterior PinnacliffwinskyAinda não há avaliações
- Varicella Fact Sheet PDFDocumento6 páginasVaricella Fact Sheet PDFgodeapAinda não há avaliações
- DFGHJKDocumento3 páginasDFGHJKcliffwinskyAinda não há avaliações
- 7.ipc Yemen Food Security Nutrition 2022june Report EnglishDocumento41 páginas7.ipc Yemen Food Security Nutrition 2022june Report EnglishSirajAinda não há avaliações
- Notice To Kettle Falls SDDocumento2 páginasNotice To Kettle Falls SDErin RobinsonAinda não há avaliações
- Harpreet ResumeDocumento3 páginasHarpreet Resumeapi-541342882Ainda não há avaliações
- Comparitive Study of Fifty Cases of Open Pyelolithotomy and Ureterolithotomy With or Without Double J Stent InsertionDocumento4 páginasComparitive Study of Fifty Cases of Open Pyelolithotomy and Ureterolithotomy With or Without Double J Stent InsertionSuril VithalaniAinda não há avaliações
- QuestionnaireDocumento6 páginasQuestionnaireRyan DaetAinda não há avaliações
- Updated Vaccination Card KNHSDocumento4 páginasUpdated Vaccination Card KNHSlemar aribalAinda não há avaliações
- Directory of Avma Listed Veterinary Colleges of The World: NangarharDocumento23 páginasDirectory of Avma Listed Veterinary Colleges of The World: NangarharMuneebAinda não há avaliações
- Middle East and North Africa Pharmaceutical Industry WhitepaperDocumento17 páginasMiddle East and North Africa Pharmaceutical Industry WhitepaperPurva ChandakAinda não há avaliações
- Medical Reimbursement Form-B & CDocumento3 páginasMedical Reimbursement Form-B & CDesiUrbanAinda não há avaliações
- Lejour Reduction MammoplastyDocumento6 páginasLejour Reduction MammoplastyMiguelito JohnsonAinda não há avaliações
- The CHIPS Randomized Controlled Trial (Control of Hypertension in Pregnancy Study)Documento7 páginasThe CHIPS Randomized Controlled Trial (Control of Hypertension in Pregnancy Study)Stephen AlexanderAinda não há avaliações
- Access To Childbirth CareDocumento67 páginasAccess To Childbirth CareemeAinda não há avaliações
- Prevention of Substance Use and Abuse (Gateway Drugs: Cigarette and AlcoholDocumento11 páginasPrevention of Substance Use and Abuse (Gateway Drugs: Cigarette and AlcoholYuki雪Ainda não há avaliações
- Traumatic Brain InjuryDocumento45 páginasTraumatic Brain InjuryShitaljit IromAinda não há avaliações
- Acrylic Removable Partial Denture (RPD)Documento6 páginasAcrylic Removable Partial Denture (RPD)israaAinda não há avaliações
- Transfusion RXNsDocumento67 páginasTransfusion RXNsSuha Abdullah100% (1)
- Cocci VexDocumento18 páginasCocci VexNona AlyAinda não há avaliações
- V-Gel Cleaning & User GuideDocumento3 páginasV-Gel Cleaning & User GuideInstrulife OostkampAinda não há avaliações
- Clinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyDocumento9 páginasClinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyGustavo BerrioAinda não há avaliações
- Ncpfdardrug Study NotesDocumento3 páginasNcpfdardrug Study NotesLuigi GeduqueAinda não há avaliações
- 07 DomingopjvmfinalDocumento9 páginas07 DomingopjvmfinalyumixxiAinda não há avaliações
- I Great Medi Care Pds enDocumento6 páginasI Great Medi Care Pds enainafaqeeraAinda não há avaliações
- CHN Q&aDocumento10 páginasCHN Q&aSweetyfe GabatanAinda não há avaliações
- KDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFDocumento102 páginasKDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFlucasnatalia21bAinda não há avaliações
- Essential GCP by Prof David Hutchinson 2017Documento78 páginasEssential GCP by Prof David Hutchinson 2017Luis Marcas VilaAinda não há avaliações
- Psychosocial Support For Parents of Extremely PretDocumento13 páginasPsychosocial Support For Parents of Extremely PretDag AraAinda não há avaliações