Escolar Documentos
Profissional Documentos
Cultura Documentos
Laparoscopic Abdominal Cerclage
Enviado por
putri rachelDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Laparoscopic Abdominal Cerclage
Enviado por
putri rachelDireitos autorais:
Formatos disponíveis
CASE REPORT
Laparoscopic Abdominal Cerclage
James F. Carter, MD, David E. Soper, MD
ABSTRACT INTRODUCTION
Abdominal cerclages are necessary when the standard The original abdominal cerclage was described by Benson
transvaginal cerclages fail or anatomical abnormalities and Durfee1 in 1965. The majority of patients diagnosed
preclude the vaginal placement. The disadvantage of the with incompetent cervix can be treated successfully with a
transabdominal approach is that it requires at least 2 transvaginal cerclage. A select group of patients who have
laparotomies with significant morbidity and hospital stays. failed the vaginal approach, or have extremely short cer-
We discuss a case of abdominal cerclage performed lapa- vices, anatomically deformed cervix, deeply lacerated cer-
roscopically. We feel it offers less morbidity and in the vices, or severely scarred from previous failed vaginal
proper hands eliminates or significantly shortens hospital cerclages may benefit from the transabdominal approach.
stays.
The disadvantage of the transabdominal approach is the
Key Words: Cerclage, Abdominal, Laparoscopy. necessity for 2 laparotomies. We describe a successful
laparoscopic placement and subsequent successful out-
come.
CASE REPORT
The patient is a 36-year-old African-American woman
(gravida 2, para 2, aborta 0, last menstrual period 4/1/03)
referred from our Maternal Fetal Medicine division for
consideration for laparoscopic cerclage. She had 2 prior
pregnancies that were lost despite McDonald cerclages.
Both pregnancies were lost in the second trimester. The
patient had a previous laparoscopy at age 20 with normal
findings.
On physical examination, the cervix was normal in ap-
pearance, the vagina was normal, and on bimanual exam-
ination the uterus was midposition and normal size, shape
and contour with some uterine descensus.
The patient was taken to the operating room after exten-
sive counseling as to possible laparotomy and bleeding
and underwent laparoscopic placement of an abdominal
cerclage using a 5-mm Mersilene band as is the usual
suture used by our Maternal Fetal Medicine (MFM) divi-
sion. This included placing the 5-mm Mersilene band
around the internal os of the cervix, tying the knots ante-
riorly, and suturing 2 0 silk suture to the cut Mersilene to
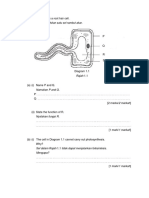
prevent any unraveling (Figure 1). We wanted to perform
Department of Obstetrics and Gynecology, Medical University of South Carolina,
Charleston, South Carolina, USA (all authors).
this procedure exactly as our MFM colleagues would do.
Address reprint requests to: James F. Carter, MD, Associate Professor of Ob/Gyn,
Department of Ob/Gyn, Medical University of South Carolina, 96 Jonathan Lucas St, RESULTS
Charleston, SC 29425, USA. E-mail: carterja@musc.edu
2005 by JSLS, Journal of the Society of Laparoendoscopic Surgeons. Published by The patient did well postoperatively and was pregnant
the Society of Laparoendoscopic Surgeons, Inc. approximately 3 months later. She had some first trimester
JSLS (2005)9:491 493 491
Laparoscopic Abdominal Cerclage, Carter JF et al.
Figure 1. (A) Placing suture; (B) tying the suture; (C) completed suture: Mersilene and silk; (D) showing posterior placement; (E) end
of case after irrigation.
492 JSLS (2005)9:491 493
bleeding at 8 weeks in which the vaginal ultrasound move these sutures through a colpotomy, most cannot)
confirmed cardiac activity. The patients prenatal course should the fetus succumb in the second trimester. We
was significant for chronic hypertension, an abnormal advocate the placement of the abdominal cerclage via the
glucose tolerance test that was diet controlled with fast- laparoscopic approach.
ings less than 100 and 2-hour postprandials consistently
The surgeon should have a skilled assistant and team. The
less than 120. She began kick counting at 28 weeks and
surgeons should have a thorough knowledge of the pelvic
Non Stress Tests2 were begun at 33 weeks. An elevated
anatomy. The ability to adapt to abnormal anatomy and
creatinine level was noted at 33 weeks and decreasing
bleeding difficulties cannot be overstated.6,7 One must
creatinine clearance was noted, for a diagnosis of pre-
always keep the patient and fetus health first, and if
eclampsia. The patient was brought to the Medical Uni-
unable to succeed laparoscopically, must be prepared to
versity of South Carolina for bedrest and evaluation at 34
perform the abdominal cerclage via laparotomy to com-
weeks. Her 24-hour urine test showed an elevated (1.27 g)
plete the procedure.
protein level. She was offered an amniocentesis at 35 0/7
weeks for lung maturity. She underwent a low transverse
References:
Cesarean delivery after lung maturity was confirmed, that
day delivering a 5 pound 12 ounce female infant, APGAR 1. Benson RC, Durfee RB. Transabdominal cervicouterine cer-
8/9. The patient tolerated the surgery well, and the infant clage during pregnancy for treatment of cervical incompetency.
and mother went home on postoperative day 3, doing Obstet Gynecol. 1965;25:145155.
well. Appropriate instructions and medications were 2. Moore TR, Piacquadio K. A prospective evaluation of fetal
given. movement screening to reduce the incidence of antepartum fetal
death. Am J Obstet Gynecol. 160(5 pt 1):10751080, 1989.
CONCLUSION 3. Novy MJ. Transabdominal cervicoisthmic cerclage: a reap-
Certainly, the usual treatment for women at risk for cer- praisal 25 years after its introduction. Am J Obstet Gynecol.
1991;164:16351642.
vical incompetence is a cerclage placed transvaginally.
When this approach has failed, or when this approach is 4. Cammarano CL, Herron MA, Parer JT. Validity of indications
not possible because of anatomic deformities, a transab- for transabdominal cerclage for cervical incompetence. Am J
dominal cerclage is a viable option. Obstet Gynecol. 1995;172:18711875.
Data clearly show an improved fetal survival rate com- 5. Leiman G, Harrison NA, Rubin A. Pregnancy following
pared with fetal survival in untreated pregnancies.35 The conization of the cervix. Complications related to cone size. Am J
Obstet Gynecol. 1980;136:14 18.
advantage of the abdominal approach is placement of the
suture at the internal os with decreased movement. No 6. Lesser KB, Childers JM, Surwit EA. Transabdominal cerclage:
foreign body enters the vagina. The band can be left in a laparoscopic approach. Obstet Gynecol. 1998;91:855 856.
place between pregnancies. The obvious disadvantage is 7. Carter JF, Soper DE. Laparoscopy in pregnancy. JSLS. 2004;
the need for 2 or even 3 laparotomies (although some 8:57 60.
skillful nonlaparoscopic surgeons have managed to re-
JSLS (2005)9:491 493 493
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- ACOG Practice Bulletin: Gestational Hypertension and Preeclampsia 2019.Documento25 páginasACOG Practice Bulletin: Gestational Hypertension and Preeclampsia 2019.Jean Paúl LópezAinda não há avaliações
- Abortion EssayDocumento10 páginasAbortion EssayRamizAinda não há avaliações
- Pathogenesis of Preterm LaborDocumento14 páginasPathogenesis of Preterm LaborAgung Sunarko PutraAinda não há avaliações
- Absent End-Diastolic Velocity in The Umbilical Artery and Its Clinical SignificanceDocumento12 páginasAbsent End-Diastolic Velocity in The Umbilical Artery and Its Clinical Significancejakob_saleanAinda não há avaliações
- Delivery Room E-Portfolio: Bartolaba, Lyca RDocumento17 páginasDelivery Room E-Portfolio: Bartolaba, Lyca RLRBAinda não há avaliações
- Pregnancy Simulation Scenario StudentDocumento3 páginasPregnancy Simulation Scenario StudentmarieAinda não há avaliações
- Hypoxic Ischemic EncephalopathyDocumento7 páginasHypoxic Ischemic EncephalopathyJennesse May Guiao IbayAinda não há avaliações
- Drug Therapy Across The LifespanDocumento34 páginasDrug Therapy Across The LifespanJSeasharkAinda não há avaliações
- Sheila C. Woodward. Fetal, Neonatal and Early Infant Experiences of Maternal Singing.Documento29 páginasSheila C. Woodward. Fetal, Neonatal and Early Infant Experiences of Maternal Singing.Юрий Семёнов100% (1)
- Drug Use During Pregnancy and LactationDocumento93 páginasDrug Use During Pregnancy and Lactation2012100% (2)
- MCN Ethical and Social Issues in Prenatal NursingDocumento26 páginasMCN Ethical and Social Issues in Prenatal NursingLhara Vhaneza CuetoAinda não há avaliações
- Obg Prenatal Period Golden Points: Nursing CrashDocumento9 páginasObg Prenatal Period Golden Points: Nursing CrashOmprakash SainiAinda não há avaliações
- MCN Finals NotesDocumento495 páginasMCN Finals NotesLeigh JiandAinda não há avaliações
- Notes On Maternal & Child Care (Pregnancy)Documento3 páginasNotes On Maternal & Child Care (Pregnancy)Oink TopusAinda não há avaliações
- REPRODocumento48 páginasREPROARVIND KUMAR YADAVAinda não há avaliações
- ISUOG Practice Guidelines Updated Performance CompressedDocumento17 páginasISUOG Practice Guidelines Updated Performance CompressedSaranya BalamuruganAinda não há avaliações
- Melody Doria - Chapter 20 ActivityDocumento3 páginasMelody Doria - Chapter 20 ActivityMelody MirandaAinda não há avaliações
- Lydia E Hall's Theory (Nov 06)Documento42 páginasLydia E Hall's Theory (Nov 06)soniya naik100% (2)
- Cognizant Previous Year Papers and Questions: (Green Marked Option Denotes The Correct OptionnDocumento316 páginasCognizant Previous Year Papers and Questions: (Green Marked Option Denotes The Correct OptionnHanuman Sai MajetiAinda não há avaliações
- Indications Contraindications Warnings PrecautionsDocumento3 páginasIndications Contraindications Warnings PrecautionsMelvin ValdezAinda não há avaliações
- The Thrifty Psychiatric PhenotypeDocumento3 páginasThe Thrifty Psychiatric Phenotypeeduardobar2000Ainda não há avaliações
- Charateristics of NewbornDocumento3 páginasCharateristics of NewbornRagupathyRamanjuluAinda não há avaliações
- Curs Pediatrie ENG 2013Documento362 páginasCurs Pediatrie ENG 2013cubixmuresAinda não há avaliações
- Rajah 1.1 Menunjukkan Satu Sel Rambut AkarDocumento29 páginasRajah 1.1 Menunjukkan Satu Sel Rambut AkarAzfar SyahmiAinda não há avaliações
- Maternity Nursing An Introductory Text 11th Edition Leifer Test BankDocumento25 páginasMaternity Nursing An Introductory Text 11th Edition Leifer Test BankJenniferNicholsonqknj100% (63)
- Early and Late Preeclamsia Are Characterized by High Cardiac Output, But in The Presence of Fetal Growth Restriction, Cardiac Output Is Low Insights From A Prospective Study PDFDocumento12 páginasEarly and Late Preeclamsia Are Characterized by High Cardiac Output, But in The Presence of Fetal Growth Restriction, Cardiac Output Is Low Insights From A Prospective Study PDFJustiawan NazwanAinda não há avaliações
- Best Practice & Research Clinical Obstetrics and GynaecologyDocumento13 páginasBest Practice & Research Clinical Obstetrics and GynaecologyRodrigoEscobedoAinda não há avaliações
- 2021 July HighlightedDocumento76 páginas2021 July HighlightedAu Cassie100% (5)
- Post Term PregnancyDocumento35 páginasPost Term PregnancyNishaThakuri100% (2)
- Final Why Abortion Should Be Legal.........Documento15 páginasFinal Why Abortion Should Be Legal.........haque163Ainda não há avaliações