Escolar Documentos
Profissional Documentos
Cultura Documentos
Drugs of Coagulation Disorders
Enviado por
Seff CausapinDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Drugs of Coagulation Disorders
Enviado por
Seff CausapinDireitos autorais:
Formatos disponíveis
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
Hemostasis - refers to the finely regulated dynamic process of red thrombi- venous clots tend to be more fibrin- rich, contain
maintaining fluidity of the blood, repairing vascular injury, and limiting large numbers of trapped red blood cells
blood loss while avoiding vessel occlusion (thrombosis) and inadequate
perfusion of vital organs
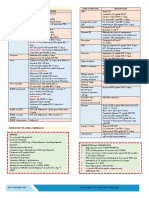
BLOOD COAGULATION CASCADE
Blood coagulates due to the transformation of soluble fibrinogen
MECHANISMS OF BLOOD COAGULATION into insoluble fibrin by the enzyme thrombin
vascular injury
endothelial cell layer rapidly undergoes a series of changes resulting in
a more pro- coagulant phenotype
Injury exposes reactive sub- endothelial matrix proteins such as
collagen and von Willebrand factor
platelet adherence and activation, and secretion and synthesis of
vasoconstrictors and platelet-recruiting and activating molecules
thromboxane A2 (TXA2) is synthesized from arachidonic acid within
platelets and is a platelet activator and potent vasoconstrictor.
adenosine diphosphate (ADP) and serotonin (5-HT)- products
secreted from the platelet granules
ADP- powerful inducer of platelet aggregation
Serotonin- stimulates aggregation and vasoconstriction
PLATELET PLUG FORMATION
Activation of platelets
conformational change in the IIbIII integrin (IIb/IIIa) receptor bind
fibrinogen
aggregation and formation of a platelet plug
Platelet- central to normal hemostasis and thromboembolic
disease, and is the target of many therapies
white thrombi- platelet- rich thrombi form in the high flow rate
and high shear force environment of arteries.
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
tissue factor (TF)-factor VIIa pathway- main initiator of blood BASIC PHARMACOLOGY OF THE ANTI- COAGULANT DRUGS
coagulation in vivo - prevent pathologic thrombosis and limit reperfusion injury, yet
- activates factors X and IX. allow a normal response to vascular injury and limit bleeding.
Factor Xa + factor Va prothrombinase complex on - all anticoagulants and fibrinolytic drugs have an increased
activated cell surfaces, which catalyzes the conversion of bleeding risk as their principle toxicity.
prothrombin (factor II) to thrombin (factor IIa)
Thrombin, in turn, activates upstream clotting INDIRECT THROMBIN INHIBITORS
factors, primarily factors V, VIII, and XI, resulting in - their anti- thrombotic effect is exerted by their interaction with
amplification of thrombin generation a separate protein, anti- thrombin.
Antithrombin (AT)- an endogenous anticoagulant and a member of - This includes unfractionated heparin (UFH), low- molecular-
the serine protease inhibitor (serpin) family; it inactivates the serine weight heparin (LMWH), and the synthetic pentasaccharide
proteases IIa, IXa, Xa, XIa, and XIIa (2, 9-12). fondaparinux that bind to antithrombin and enhance its
The endogenous anticoagulants protein C and protein S- attenuate inactivation of factor Xa
the blood clotting cascade by proteolysis of the two cofactors Va
and VIIIa
HEPARIN
A. Chemistry and MOA
Fibrinolysis - It s a heterogeneous mixture of sulfated mucopolysaccharides
- refers to the process of fibrin digestion by the fibrin- specific - binds to endothelial cell surfaces and a variety of plasma
protease, plasmin. proteins
- its biologic activity is dependent upon the endogenous
anticoagulant antithrombin
Antithrombin inhibits clotting factor proteases,
especially thrombin (IIa), IXa, and Xa, by forming
equimolar stable complexes with them
This is accelerated by heparin 1000 fold
- Commercial heparin has only about 1/3 having an accelerating
capacity, remainder lack the unique pentasaccharide sequence
needed for high- affinity binding to antithrombin
- MOA: active heparin molecules bind tightly to antithrombin
conformational changes in this inhibitor this exposes its
active site for more rapid interaction with the proteases (the
activated clotting factors)
- Heparin functions as a cofactor for the antithrombin-protease
reaction without being consumed
heparin is released intact for renewed binding to
more antithrombin once the antithrombin- protease
complex is formed.
antithrombin binding region of commercial unfractionated
heparin consists of repeating sulfated disaccharide units
composed of D-glucosamine-L-iduronic acid and D-
glucosamine- D-glucuronic acid
High-molecular-weight (HMW), also known as UFH has high
affinity for antithrombin and inhibit coagulation by inhibiting
all three factors esp. thrombin and factor Xa.
Shorter- chain low-molecular-weight (LMW) fractions of
heparin inhibit activated factor X but have less effect on
thrombin than the HMW species.
Tissue plasminogen activator, urokinase, and streptokinase all enoxaparin, dalteparin, and tinzaparin
activate the fibrinolytic system commercial heparin consists of a family of molecules of different
Aminocaproic acid- useful inhibitor of fibrinolysis molecular weights extracted from porcine intestinal mucosa and
Heparin and the oral anticoagulant drugs do not affect the bovine lung
fibrinolytic mechanism
Monitoring of Heparin Effect
- Close monitoring of the activated partial thromboplastin time
(aPTT or PTT) is necessary in patients receiving UFH
- Levels of UFH may also be determined by protamine titration
or anti-Xa units
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
- Therapeutic levels: Rivaroxaban- first oral factor Xa inhibitor to reach phase III clinical
0.20.4 unit/mL by protamine titration trials
0.30.7 unit/mL by anti- Xa units
0.51 unit/mL for twice-daily dosing LMW
Reversal of Heparin Action
1.5 units/mL for once-daily dosing LMW
B. TOXICITY
- When excessive anticoagulation action of heparin is treated
by discontinuance of the drug
a. Bleeding and Miscellaneous Effects
- Major effect of heparin is bleeding - protamine sulfate given when bleeding occurs
- Elderly women and patients with renal failure are more 100: 1 ratio (for every 100 units of heparin, 1 mg
prone to hemorrhage of protamine sulfate is given)
- Heparin is of animal origin allergy excess of protamine must also be avoided, it has
- Increased loss of hair and reversible alopecia have been also an anticoagulant effect.
reported - Protamine will not reverse the activity of fondaparinux
- Long-term heparin therapy is associated with - Excess danaparoid can be removed by plasmapheresis.
osteoporosis and spontaneous fractures and
mineralocorticoid deficiency.
- Heparin accelerates the clearing of postprandial lipemia
ORAL DIRECT FACTOR XA INHIBITORS
b. Heparin-Induced Thrombocytopenia - exert their anticoagulant effect by directly binding to the
- occurs in 14% of individuals treated with UFH for a active site of thrombin, thereby inhibiting thrombins
minimum of 7 days downstream effects.
- The risk of HIT may be higher in individuals treated with - Hirudin and bivalirudin- bivalent DTIs in that they bind at both
UFH of bovine origin compared with porcine heparin and the catalytic or active site of thrombin as well as at a
is lower in those treated exclusively with LMWH substrate recognition site.
- Morbidity and mortality in HIT are related to thrombotic - Argatroban and melagatran- small molecules that bind only
events commonly venous thrombosis at the thrombin active site.
- Platelet counts should be performed frequently;
- thrombocytopenia appearing in a time frame consistent PARENTERAL DIRECT THROMBIN INHIBITORS
with an immune response to heparin should be Hirudin
considered suspicious for HIT - A specific, irreversible thrombin inhibitor from leech saliva
that is now available in recombinant form as lepirudin
C. CONTRAINDICATIONS - Its action is independent of antithrombin, which means it can
- HIT, hypersensitivity to the drug, active bleeding, reach and inactivate fibrin-bound thrombin in thrombi.
hemophilia, significant thrombocytopenia, purpura, Lepirudin- has little effect on platelets or the bleeding time
severe hypertension, intracranial hemorrhage, infective - administered parenterally and is monitored by the
endocarditis, active tuberculosis, ulcerative lesions of aPTT.
the gastrointestinal tract, threatened abortion, visceral - use in patients with thrombosis related to HIT
carcinoma, or advanced hepatic or renal disease. - excreted by the kidney and should be used with
- Hx of present surgery of the brain, spinal cord, or eye, great caution in patients with renal insufficiency as
and in patients who are undergoing lumbar puncture or no antidote exists
regional anesthetic block Bivalirudin
- bivalent inhibitor of thrombin, is administered intravenously,
D. ADMINISTRATION AND DOSAGE with a rapid onset and offset of action
- 0.20.4 unit/mL by protamine titration - has a short half-life with clearance that is 20% renal
- 0.30.7 unit/mL by anti- Xa units - FDA-approved for use in percutaneous coronary angioplasty.
- Continuous intravenous administration of heparin is Argatroban
accomplished via an infusion pump - A small molecule thrombin inhibitor that is FDA-approved for
use in patients with HIT with or without thrombosis and
80100 units/kg- initial bolus injection
coronary angioplasty in patients with HIT
1522 units/ kg/h- continuous infusion - has a short half-life, is given by continuous IV infusion, and is
5000 units every 812 hours - Low-dose monitored by aPTT.
prophylaxis administered subQ - Metabolism is liver, dose reduction is required in patients
with liver disease
fondaparinux- avidly binds antithrombin with high specific activity,
resulting in efficient inactivation of factor Xa ORAL DIRECT THROMBIN INHIBITORS
- T1/2 is 15 hours - Advantages: predictable pharmacokinetics and bioavailability,
- Effective in the prevention and treatment of venous - these agents do not interact with P450-interacting drugs,
thromboembolism, and appears to not cross-react and their rapid onset and offset of action allow for immediate
with pathologic HIT antibodies in most individuals anticoagulation
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
Dabigatran etexilate mesylate is the first oral direct thrombin half-lives are:
inhibitor approved by the FDA factors VII 6 hrs,
- reduce risk of stroke and systemic embolism with factor IX 24 hrs
nonvalvular atrial fibrillation factor X 40 hrs
factor II 60 hrs
a. Pharmacology - The only difference among oral anticoagulants in producing
- dabigatran etexilate mesylate is converted to and maintaining hypoprothrombinemia is the half-life of each
dabigatran drug.
- the drug is a substrate for the P-glycoprotein efflux
pump; however, P-glycoprotein inhibitors or C. Toxicity
inducers do not have a significant effect on drug - Warfarin crosses the placenta readily and can cause a
clearance. hemorrhagic disorder in the fetus
- aketoconazole, amiodarone, quinidine, and - cause a serious birth defect characterized by abnormal bone
clopidogrel increases the effect of dabigatran formation (-carboxyglutamate residues)
- T = 1217 hours - with reduced protein C, it can cause cutaneous necrosis
- requires dose adjustment; the drug should be
avoided in patients with severe renal impairment. D. Administration & Dosage
b. Administration and Dosage - standard doses of 510 mg rather than the large loading
- prevention of stroke and systemic embolism in doses
nonvalvular atrial fibrillation, 150 mg should be - prothrombin time (PT) should be increased to a level
given bid to patients with creatinine clearance > representing a reduction of prothrombin activity to 25% of
30 mL/min normal and maintained there for long-term therapy
- for decreased creatinine clearance of 1530
mL/min, the dose is 75 mg bid E. Drug Interactions
- prolong the PTT and thrombin time - The most serious interactions with warfarin are those that
c. Toxicity increase the anticoagulant effect and the risk of bleeding.
- primary toxicity of dabigatran is bleeding - The most dangerous of these interactions are the
- no antidote for dabigatran pharmacokinetic interactions with the mostly obsolete
pyrazolones phenylbutazone and sulfinpyrazone.
WARFARIN & OTHER COUMARIN ANTICOAGULANTS Causes not only augmentation of hypoprothrombinemia but
A. Chemistry & Pharmacokinetics also inhibit platelet function and may induce peptic ulcer
- Warfarin is generally administered as the sodium salt and has disease
100% bioavailability - Metronidazole, fluconazole, and trimethoprim-
- bound to plasma albumin (99%) sulfamethoxazole inhibit the metabolic transformation of
- has a long half-life in plasma= 36 hours, and the lack of S-warfarin
urinary excretion of unchanged drug - amiodarone, disulfiram, and cimetidine inhibit metabolism
- used clinically is a racemic mixture composed of equal of both enantiomorphs of warfarin
amounts of two enantiomorphs - Aspirin, hepatic disease, and hyperthyroidism augment
levorotatory S-warfarin is four times more potent than the warfarins effects
dextrorotatory R-warfarin - Barbiturates and rifampin cause a marked decrease of the
B. Mechanism of Action anti- coagulant effect by induction of the hepatic enzymes
- blocks the -carboxylation of several glutamate residues in - ethanol, phenothiazines, benzodiazepines, acetaminophen,
prothrombin and factors VII, IX, and X as well as the opioids, indomethacin, and most antibiotics no significant
endogenous anticoagulant proteins C and S effect on anticoagulation therapy
this blockade results in incomplete coagulation factor
molecules that are biologically inactive Reversal of Warfarin Action
- protein carboxylation reaction is coupled to the oxidation of - reversed by stopping the drug and administering oral or
vitamin K parenteral vitamin K1 (phytonadione), fresh-frozen plasma,
- Warfarin prevents reductive metabolism of the inactive prothrombin complex concentrates such as Bebulin and
vitamin K epoxide back to its active hydroquinone form Proplex T, and recombinant factor VIIa (rFVIIa)
- There is an 8- to 12-hour delay in the action of warfarin
- anticoagulant effect results from a balance between partially
inhibited synthesis and unaltered degradation of the four
vitamin K-dependent clotting factors.
- The resulting inhibition of coagulation is dependent on their
degradation half-lives in the circulation
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
BASIC PHARMACOLOGY OF THE FIBRINOLYTIC DRUGS BASIC PHARMACOLOGY OF ANTIPLATELET AGENTS
- rapidly lyse thrombi by catalyzing the formation of the serine Three categories of substances that regulate platelet functions:
protease plasmin from its precursor zymogen, plasminogen 1. agents generated outside the platelet that interact with
platelet membrane receptors e.g. catecholamines, collagen,
Pharmacology thrombin, and prostacyclin
2. agents generated within the platelet that interact with
STREPTOKINASE
membrane receptors, eg, ADP, prostaglandin D2,
- is a protein synthesized by streptococci that combines with
prostaglandin E2, and serotonin
the proactivator plasminogen
3. agents generated within the platelet that act within the
- catalyzes the conversion of inactive plasminogen to active
platelet, eg, prostaglandin endoperoxides and thromboxane
plasmin
A2, the cyclic nucleotides cAMP and cGMP, and calcium ion
UROKINASE
- is a human enzyme synthesized by the kidney that directly
Several targets for platelet inhibitory drugs:
converts plasminogen to active plasmin
1. inhibition of prostaglandin synthesis (aspirin)
ANISTREPLASE
2. inhibition of ADP- induced platelet aggregation (clopidogrel,
- an anisoylated plasminogen streptokinase activator complex
prasugrel, ticlopidine)
- consists of a complex of purified human plasminogen and
3. blockade of glycoprotein IIb/IIIa receptors on platelets
bacterial streptokinase that has been acylated to protect the
(abciximab, tirofiban, and eptifibatide).
enzymes active site
Dipyridamole and cilostazol are additional antiplatelet drugs.
Tissue plasminogen activators (t-PAs)
- activates plasminogen preferentially that is bound to fibrin ASPIRIN
which confines fibrinolysis to the formed thrombus and - Prototype of the drug that antagonizes the prostaglandin
avoids systemic activation thromboxane A2 interfering with platelet aggregation in vitro
- manufactured as alteplase by means of recombinant DNA and prolong the bleeding time in vivo
technology - inhibits the synthesis of thromboxane A2 by irreversible
Reteplase- another recombinant human t-PA from which several acetylation of the enzyme cyclooxygenase
amino acid sequences have been deleted - approved: use of 325 mg/d aspirin for primary prophylaxis of
- less expensive to produce than t- PA because it lacks the myocardial infarction
major fibrin-binding domain, reteplase is less fibrin- specific
than t-PA TICLOPIDINE, CLOPIDOGREL, & PRASUGREL
Tenecteplase- a mutant form of t-PA that has a longer half-life, - a reduce platelet aggregation by inhibiting the ADP pathway
and it can be given as an intravenous bolus of platelets.
- Tenecteplase is slightly more fibrin-specific than t-PA - irreversibly block the ADP receptor on platelets
- have no effect on prostaglandin metabolism
Indications & Dosage a. Ticlopidine
IV administration- indicated in cases of pulmonary embolism with approved for prevention of stroke in patients with a history
hemodynamic instability, severe deep venous thrombosis such as of a transient ischemic attack (TIA) or thrombotic stroke,
the superior vena caval syndrome, and ascending and in combination with aspirin for prevention of coronary
thrombophlebitis of the iliofemoral vein with severe lower extremity stent thrombosis
edema. adverse effects: nausea, dyspepsia, and diarrhea in up to
Streptokinase is administered by intravenous infusion of a loading 20% of patients, hemorrhage in 5%, and, most seriously,
dose of 250,000 units, followed by 100,000 units/h for 2472 leukopenia in 1%
hours ingestion of ticlopidine thrombotic thrombocytopenic
Urokinase requires a loading dose of 300,000 units given over 10 purpura
minutes and a maintenance dose of 300,000 units/h for 12 hours. dosage: 250 mg twice daily
Alteplase (t-PA) is given by intravenous infusion of 60 mg over the the use of this drug for stroke prevention is restricted to
first hour and then 40 mg at a rate of 20 mg/h. those who are intolerant of or have failed aspirin therapy
Reteplase is given as two intravenous bolus injections of 10 units b. Clopidogrel
each, sepa- rated by 30 minutes. approved for patients with unstable angina or non-ST-
Tenecteplase is given as a single intravenous bolus of 0.5 mg/kg. elevation acute myocardial infarction (NSTEMI) in
Anistreplase (where available) is given as a single intravenous combination with aspirin; for patients with ST-elevation
injection of 30 units over 35 minutes. myocardial infarction (STEMI); or recent myocardial
infarction, stroke, or established peripheral arterial disease
adverse effects: fewer than ticlopedine, thrombotic
thrombocytopenic purpura
antithrombotic effects of clopidogrel are dose-dependent;
within 5 hours after an oral loading dose of 300 mg,
80% of platelet activity will be inhibited
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
the maintenance dose of clopidogrel is 75 mg/d, which - Once therapeutic effects of warfarin have been established,
achieves maximum platelet inhibition. therapy with warfarin is continued for a minimum of 36
the duration of the antiplatelet effect is 710 days months.
a prodrug that requires activation via the cytochrome P450
enzyme isoform CYP2C19 DRUGS USED IN BLEEDING DISORDERS
c. Prasugrel VITAMIN K
approved for patients with acute coronary syndromes - Two natural forms exist:
given as a 60-mg loading dose and then 10 mg/d in 1. K1- phytonadione, found in food
combination with aspirin 2. K2- menaquinone, found in human tissues and is
the major and minor bleeding risk was increased with synthesized by intestinal bacteria.
prasugrel. - Onset of effect is delayed for 6 hours but the effect is
Prasugrel is contraindicated in patients with history of TIA or complete by 24 hours when treating depression of
stroke because of increased bleeding risk. prothrombin activity by excess warfarin or vitamin K
deficiency
BLOCKADE OF PLATELET GLYCOPROTEIN IIB/IIIA RECEPTORS - IV administration of vitamin K1 should be slow, because rapid
infusion can produce dyspnea, chest and back pain, and
- used in patients with acute coronary syndromes
- drugs target the platelet IIb/IIIa receptor complex even death
- Ib/IIIa complex functions as a receptor mainly for fibrinogen - Vitamin K repletion is best achieved with intravenous or oral
administration
and vitronectin but also for fibronectin and von Willebrand
factor
PLASMA FRACTIONS
a. Abciximab
- Concentrated plasma fractions are available for the treatment
- a chimeric monoclonal antibody directed against the IIb/IIIa
complex including the vitronectin receptor of deficiencies such as hemophilia A dse and Christmas dse
- use in percutaneous coronary intervention and in acute Desmopressin acetate
coronary syndromes. - increases the factor VIII activity of patients with mild
b. Eptifibatide hemophilia A or von Willebrand disease
- analog of the sequence at the extreme carboxyl terminal of Cryoprecipitate
the delta chain of fibrinogen, which mediates the binding of - is a plasma protein fraction obtainable from whole blood.
fibrinogen to the receptor. - It is used to treat deficiencies or qualitative abnormalities of
c. Tirofiban fibrinogen, such as that which occurs with disseminated
- smaller molecule with similar properties intravascular coagulation and liver disease.
Eptifibatide and tirofiban inhibit ligand binding to the IIb/IIIa - A single unit of cryoprecipitate contains 300 mg of
receptor by their occupancy of the receptor but do not block the fibrinogen.
vitronectin receptor.
RECOMBINANT FACTOR VIIA
three agents described above are administered parenterally
- approved for treatment of inherited or acquired hemophilia A
or B with inhibitors, treatment of bleeding associated with
ADDITIONAL ANTIPLATELET-DIRECTED DRUGS
Dipyridamole- a vasodilator that also inhibits platelet function by invasive procedures in congenital or acquired hemophilia, or
factor VII deficiency
inhibiting adenosine uptake and cGMP phosphodiesterase activity.
- initiates activation of the clotting pathway by activating factor
- has little or no beneficial effect
IX and factor X in association with tissue factor
- therapeutic use of this agent is primarily in combination with
aspirin to prevent cerebrovascular ischemia - drug is given by bolus injection
- been widely used for off-label indications, including bleeding
- also be used in combination with warfarin for primary
prophylaxis of thromboemboli in patients with prosthetic with trauma, surgery, intracerebral hemorrhage, and warfarin
heart valves. toxicity
Cilostazol- newer phosphodiesterase inhibitor that promotes
FIBRINOLYTIC INHIBITORS: AMINOCAPROIC ACID
vasodilation and inhibition of platelet aggregation
- is used primarily to treat intermittent claudication. - chemically similar to the amino acid lysine, is a synthetic
inhibitor of fibrinolysis
CLINICALPHARMACOLOGYOF DRUGS USED TO PREVENT CLOTTING - competitively inhibits plasminogen activation
Tranexamic acid is an analog of aminocaproic acid and has the
Antithrombotic Management
same properties.
Heparin and warfarin may be used to prevent venous
- It is administered orally with a 15 mg/kg loading dose
thrombosis
followed by 30 mg/kg every 6 hours.
Subcutaneous administration of low-dose unfractionated
Clinical Uses of EACA:
heparin, LMWH, or fondaparinux provides effective
- as adjunctive therapy in hemophilia, as therapy for bleeding
prophylaxis
from fibrinolytic therapy, and as prophylaxis for rebleeding
unfractionated or LMWH- tx for established venous
from intracranial aneurysms
thrombosis, initiated for the first 5- 7 days
DRUGS USED IN DISORDERS OF COAGULATION seffcausapinmd
Adverse effects of the drug: include intravascular thrombosis from
inhibition of plasminogen activator, hypotension, myopathy, abdominal
discomfort, diarrhea, and nasal stuffiness.
should not be used in patients with disseminated intravascular
coagulation or genitourinary bleeding of the upper tract, eg,
kidney and ureters, because of the potential for excessive clotting
SERINE PROTEASE INHIBITORS: APROTININ
- serine protease inhibitor (serpin) that inhibits fibrinolysis by
free plasmin and may have other antihemorrhagic effects as
well.
- It also inhibits the plasmin-streptokinase complex in patients
who have received that thrombolytic agent.
- use of the drug was associated with an increased risk of
renal failure, heart attack, and stroke
-
Você também pode gostar
- Thyroid 2Documento58 páginasThyroid 2Seff CausapinAinda não há avaliações
- Disorders of The Female Reproductive System PDFDocumento4 páginasDisorders of The Female Reproductive System PDFSeff CausapinAinda não há avaliações
- Dem Tickler NotesDocumento1 páginaDem Tickler NotesSeff CausapinAinda não há avaliações
- 3 180824051636Documento45 páginas3 180824051636Seff CausapinAinda não há avaliações
- Disorders of The Female Reproductive System PDFDocumento4 páginasDisorders of The Female Reproductive System PDFSeff CausapinAinda não há avaliações
- Anterior Pituitary Tumor SyndromesDocumento10 páginasAnterior Pituitary Tumor SyndromesSeff CausapinAinda não há avaliações
- Hemostasissurgicalbleedingandtransfusion 130707035616 Phpapp02Documento42 páginasHemostasissurgicalbleedingandtransfusion 130707035616 Phpapp02Seff CausapinAinda não há avaliações
- Altitude IllnessDocumento4 páginasAltitude IllnessSeff CausapinAinda não há avaliações
- Anterior Pituitary Tumor SyndromesDocumento10 páginasAnterior Pituitary Tumor SyndromesSeff CausapinAinda não há avaliações
- Urinary Tract ObstructionDocumento2 páginasUrinary Tract ObstructionSeff CausapinAinda não há avaliações
- Glomerular Diseases: Pathogenesis of Glomerular Diseases Progression of Glomerular DiseasesDocumento6 páginasGlomerular Diseases: Pathogenesis of Glomerular Diseases Progression of Glomerular DiseasesSeff CausapinAinda não há avaliações
- Lumbar TapDocumento4 páginasLumbar TapSeff CausapinAinda não há avaliações
- Medicine (Dr. Pedroza) Copd 14 FEBRUARY 2018Documento3 páginasMedicine (Dr. Pedroza) Copd 14 FEBRUARY 2018Seff CausapinAinda não há avaliações
- Approach To Patient With Endocrine DisordersDocumento2 páginasApproach To Patient With Endocrine DisordersSeff CausapinAinda não há avaliações
- Peripheral Vascular System Physical DiagnosisDocumento3 páginasPeripheral Vascular System Physical DiagnosisSeff Causapin100% (1)
- Musculoskeletal System Physical DiagnosisDocumento4 páginasMusculoskeletal System Physical DiagnosisSeff Causapin100% (1)
- Complete Guide To Physical ExamDocumento19 páginasComplete Guide To Physical ExamSeff Causapin100% (2)
- Disorders of The MediastinumDocumento1 páginaDisorders of The MediastinumSeff CausapinAinda não há avaliações
- Approach To The PX With CancerDocumento7 páginasApproach To The PX With CancerSeff CausapinAinda não há avaliações
- Abdomen Physical DiagnosisDocumento3 páginasAbdomen Physical DiagnosisSeff CausapinAinda não há avaliações
- Disturbances in Respiratory FunctionDocumento6 páginasDisturbances in Respiratory FunctionSeff CausapinAinda não há avaliações
- Physical Diagnosis of The ThoraxDocumento3 páginasPhysical Diagnosis of The ThoraxSeff Causapin100% (1)
- Physical Diagnosis of Cardiovascular SystemDocumento6 páginasPhysical Diagnosis of Cardiovascular SystemSeff Causapin100% (1)
- Pathophysiology of SLEDocumento16 páginasPathophysiology of SLESeff CausapinAinda não há avaliações
- Salmon Ellos IsDocumento3 páginasSalmon Ellos IsSeff CausapinAinda não há avaliações
- Clinicopathologic Narrative ReportDocumento3 páginasClinicopathologic Narrative ReportSeff CausapinAinda não há avaliações
- MNGT of AmoebiasisDocumento6 páginasMNGT of AmoebiasisSeff CausapinAinda não há avaliações
- Tubulointerstitial DsesDocumento3 páginasTubulointerstitial DsesSeff CausapinAinda não há avaliações
- LeptospirosisDocumento2 páginasLeptospirosisSeff CausapinAinda não há avaliações
- Sympathomimetic Agents: CLIN. PHARM (Dr. Salvador) Asthma 05 SEPT 2017Documento3 páginasSympathomimetic Agents: CLIN. PHARM (Dr. Salvador) Asthma 05 SEPT 2017Seff Causapin100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Quick Guide DVTDocumento26 páginasQuick Guide DVTdrkrsticAinda não há avaliações
- Venous Thromboembolism (VTE) Pathophysiology September 2016Documento46 páginasVenous Thromboembolism (VTE) Pathophysiology September 2016Nick GouvatsosAinda não há avaliações
- Antithrombotic Drugs: Pharmacology and Implications For Dental PracticeDocumento9 páginasAntithrombotic Drugs: Pharmacology and Implications For Dental PracticeMariana VLedezmaAinda não há avaliações
- Heparin and WarfarinDocumento2 páginasHeparin and WarfarinBaeyer100% (1)
- CPG Unstable AnginaDocumento58 páginasCPG Unstable AnginaAmir HassenAinda não há avaliações
- Antiplatelet DrugsDocumento40 páginasAntiplatelet DrugsJanielWrightAinda não há avaliações
- Hema Stago DLLDocumento9 páginasHema Stago DLLMaya RustamAinda não há avaliações
- Cva Trombosis 3Documento11 páginasCva Trombosis 3fitriAinda não há avaliações
- Anticoagulants: Presented By: ABHILASH Moderator: DR CH RAHUL MDDocumento103 páginasAnticoagulants: Presented By: ABHILASH Moderator: DR CH RAHUL MDabhilashreddy45100% (1)
- Perioperative Anticoagulation Bridging Guideline PostedDocumento6 páginasPerioperative Anticoagulation Bridging Guideline PostedNuc Alexandru100% (1)
- DVT ProphylaxisDocumento30 páginasDVT ProphylaxissivaAinda não há avaliações
- PICU Drug Handbook 2014 PDFDocumento106 páginasPICU Drug Handbook 2014 PDFMelissa SantosoAinda não há avaliações
- Methodist Healthcare 6-26 PDFDocumento172 páginasMethodist Healthcare 6-26 PDFTom Ling IIAinda não há avaliações
- Deep Venous ThrombosisDocumento56 páginasDeep Venous ThrombosisSrikant Konchada100% (1)
- Venous DiseaseDocumento45 páginasVenous DiseaseNinch Nagac100% (1)
- Concept Map For EndocarditisDocumento3 páginasConcept Map For EndocarditisSavanna ChambersAinda não há avaliações
- Common Medications in Surgery 2017-18Documento35 páginasCommon Medications in Surgery 2017-18Mu AbAinda não há avaliações
- NHMRC VTE Prevention Guideline Summary For CliniciansDocumento2 páginasNHMRC VTE Prevention Guideline Summary For CliniciansRatnaSuryati100% (1)
- Anticoagulant & Thrombolytic DrugsDocumento68 páginasAnticoagulant & Thrombolytic Drugsezrider7Ainda não há avaliações
- Deep Venous Thrombosis: Anne M. Aquila, APRNDocumento20 páginasDeep Venous Thrombosis: Anne M. Aquila, APRNTan RøbìñAinda não há avaliações
- Continuous Renal Replacement TherapyDocumento32 páginasContinuous Renal Replacement TherapyJayarani Ashok100% (1)
- Anticoagulants ParamedDocumento20 páginasAnticoagulants ParamedManikanta GupthaAinda não há avaliações
- Book Reading DVTDocumento15 páginasBook Reading DVTMahendra SeptadiAinda não há avaliações
- Switching Between AnticoagulantsDocumento2 páginasSwitching Between AnticoagulantsSylvinho46Ainda não há avaliações
- 2017 06 16 Stroke in PregnancyDocumento49 páginas2017 06 16 Stroke in PregnancyayubahriAinda não há avaliações
- MBF7823423Documento425 páginasMBF7823423Pete PetersAinda não há avaliações
- Antiphospholipid SyndromeDocumento8 páginasAntiphospholipid SyndromeVijeyachandhar DorairajAinda não há avaliações
- Anticoagulation Options For Intermittent HDDocumento10 páginasAnticoagulation Options For Intermittent HDNarinder SharmaAinda não há avaliações
- Stago BrochureDocumento44 páginasStago BrochureagbnetAinda não há avaliações
- Venous Thromboembolism and Obstetric Anaesthesia TOTW 207 2010Documento9 páginasVenous Thromboembolism and Obstetric Anaesthesia TOTW 207 2010Juan Ramón González MasisAinda não há avaliações