Escolar Documentos
Profissional Documentos
Cultura Documentos
Dua's Layer PDF
Enviado por
tasiambdTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Dua's Layer PDF
Enviado por
tasiambdDireitos autorais:
Formatos disponíveis
UPDATE/REVIEW
Duas Layer: its discovery, characteristics
and applications
Harminder S. Dua, BBS, DO, DO (Lond), MS, MNAMS, FRCS, FRCOphth., FEBO, MD, PhD1;
Lana A. Faraj, MD, MSc1; Dalia G. Said, MD, FRCS1
ABSTRACT: Definitive treatment for loss of corneal transparency or for corneal
distortion is a corneal transplant. When the sight affecting pathology lies in the corneal
stroma, deep anterior lamellar keratoplasty (DALK) allows retention of the healthy
recipient endothelium and Descemets layer. The Big Bubble (BB) technique described
by Mohamed Anwar is the most popular Descemets baring technique worldwide. It
involves the injection of air into the corneal stroma, thus stripping the DM from the deep
stroma and allowing excision of the affected tissue. Over nearly a decade of performing
DALK by the BB technique, a number of clues pointed to a novelty in the surgical
anatomy of the posterior cornea which, after characterisation, was termed the Duas layer.
This report summarizes the events that suggested the existence, provided evidence, and
finally led to the characterisation of the Duas layer, along to its clinical relevance and the
applications of this discovery.
J Emmetropia 2014; 5: 211-223
Loss of corneal transparency or corneal distortion cornea. Full thickness corneal grafts or penetrating
leading to visual impairment and blindness can keratoplasty, to manage both stromal and endothelial
occur for two main reasons stromal disease with disease, then became the norm and remained as the
or without scarring and endothelial disease with standard of care for most of the one hundred years,
consequent corneal hydration. The definitive despite its many well recognised problems. Major
treatment for these conditions is a corneal problems include a prolonged visual recovery time,
transplant. The first human corneal transplant was weaker structural integrity of the eye rendering
performed more than a hundred years ago1. The it susceptible to rupture following trivial trauma,
initial emphasis was on lamellar grafts wherein the high astigmatism and graft rejection and failure.
anterior scarred layer of the cornea was replaced by Inventions and innovations in eye banking,
a similar layer of clear tissue taken from a donor technology and instrumentation, particularly in
the last decade have enabled refinements in corneal
transplantation that address many of the problems
mentioned above. When the endothelium is affected,
1
Academic Ophthalmology, Division of Clinical Neuroscience, specific replacement of the endothelial layer can be
School of Medicine, University of Nottingham, England. undertaken in the procedures termed Descemets
Financial disclosure: The authors have no commercial or financial stripping endothelial keratoplasty (DSEK) and
interests in the medical findings derived from this study. Descemets membrane endothelial keratoplasty
(DMEK)2,3. Endothelial transplantation allows for
Copyright Authorization: All reproductions from the British Journal
of Ophthalmology and from Ophthalmology are in accordance with very rapid visual recovery, is astigmatically neutral,
the journal policies wherein authors are permitted to reproduce parts does not weaken the eye and also appears to have a
of their own publications for other publications such as book chapters reduced incidence of rejection.
with due acknowledgement to the source. When the sight affecting pathology lies in the
Corresponding Author: Harminder S. Dua corneal stroma, it is no longer necessary to replace
Room Division of Ophthalmology and Visual Sciences B floor, Eye the entire cornea. Deep anterior lamellar keratoplasty
ENT Centre, Queens Medical Centre, Derby Road (DALK) allows retention of the healthy recipient
Queens Medical Centre
Nottingham
endothelium and Descemets layer while replacing
NG7 2UH the entire stroma and epithelium2-5. This virtually
E- mail: harminder.dua@nottingham.ac.uk eliminates the risk of rejection related graft failure
2014 SECOIR ISSN: 2171-4703 211
Sociedad Espaola de Ciruga Ocular Implanto-Refractiva
212 DUAS LAYER
and also leaves the eye more secure than after a vacuum trephine (Figure 1A). A 27 or 30 gauge, angled
penetrating keratoplasty. Most of the techniques sharp pointed needed, bevel down (or a blunt ended
deployed to perform DALK attempt to reach the cannula with a hole on the lower surface, near the tip)
Descemets membrane (DM), i.e. remove the entire mounted on a 5 or 10 ml Luer lock syringe filled with
stroma. One approach, known as the Big Bubble air, is passed through the deep stroma starting in the
(BB) technique, involves the injection of air into the groove made by the trephination, towards the central
corneal stroma, which when successful, strips the part of the cornea (Figure 1B). Air is forced into the
DM from the deep stroma allowing excision of the stroma until a large bubble is seen to form and allowed
affected stroma whilst retaining the recipient DM to expand till it extends just beyond the trephine mark
and endothelium2-5. This can also be achieved with (Figure 1C). Approximately half to two thirds thickness
the injection of viscoelastic substances or balanced of the anterior stroma outlined by the trephine mark is
salt solution6. Collectively these techniques are then dissected off (Figure 1D). Some aqueous is released
referred to as Descemets baring techniques where through a paracentesis to reduce the eye pressure
it is claimed that the cleavage occurs as a plane that (Figure1E) and the roof of the bubble, made of deep
enables the DM to be laid bare4, 5. stroma is punctured with a sharp knife (Figure 1F).
A spatula is inserted in the plane between the deep
THE BIG BUBBLE TECHNIQUE FOR DALK stroma and the DM and the stroma incised in a cruciate
manner to divide the deep stroma into four quadrants
Understanding this technique is important for the (Figure1G). Each quadrant is then excised with a pair of
understanding of the clues that led to the discovery of the curved corneal scissors (Figure 1H), laying bare the DM
Duas layer and its clinical relevance. The Big Bubble (Figure 1I). The donor button, approximately 0.25 mm
(BB) technique described by Mohamed Anwar2-5 larger than the host trephine diameter, is stripped off its
(Figure1) is the most popular technique worldwide that DM (Figure 1J), placed on the exposed recipients DM
is used for separating the DM from the corneal stroma. (Figure 1K) and sutured to the recipient rim (Figure 1L).
A central trephination (between 7 mm and 8.5 mm) to There are several variations to the above technique but
deep lamellar depth is carried out with a manual or a the principles remain as described above. For example,
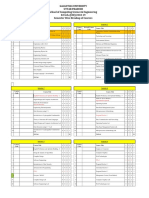
Figure 1. Steps of Deep Anterior Lamellar Keratoplasty (DALK). A. Central trephination of between 7 to 8.25 mm. B. A 30 gauge needle is
inserted bevel down into deep stroma under a drop of hyaluronic acid which acts as a magnifier. C. Injection of air creates a big bubble (BB) the
limits of which are defined by a white line. D. The anterior half to two thirds of corneal stroma are dissected and removed. E. A paracentesis
is performed to reduce eye pressure. F. The stromal wall of the BB is punctured. G. A spatula is inserted in the plane between the stroma and
Descemets membrane (DM) and the stroma incised in a cruciate manner. H. The four quadrants of the deep stroma are excised. I. The anterior
surface of the DM is exposed. J. The DM and endothelium from the donor button is stripped off. K. The donor button is placed on the host
DM and L. sutured in place.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 213
instead of inserting a spatula in the plane between deep c) However, on occasions when the BB did not
stroma and DM, the space is filled with a cohesive reach the edge of the trephine mark, the deep stroma (roof
viscoelastic agent and divided into quadrants with a pair of the bubble) was seen to be attached to the hosts DM
of scissors; some surgeons may dissect off the top half or by fine strands of tissue which had to be mechanically
two thirds of the trephined cornea and then inject air broken or cut to extend the cleavage plane to the
in the deep stroma to obtain the BB. Others insert the trephine mark before excising the respective quadrant
needle or cannula of the air filled syringe tangentially of deep stroma (Figure 2C). This begged the question
along the periphery of the cornea rather than radially that if the plane of cleavage with the BB technique is the
towards the pupil margin. same as when DM is peeled off the donor button; why
do strands appear when separating stroma from the DM
and not when separating DM from stroma?
CLINICAL CLUES THAT SUGGESTED THE d) When there was an inadvertent micro or macro
EXISTENCE OF DUAS LAYER perforation of the deep stroma during the operation, the
torn DM did not scroll like the DM is known to do
Over nearly a decade of performing DALK by the BB (Figure 2D and 2E).
technique, one of us (HSD) noted a number of clues e) During suturing of full thickness corneal donor
that pointed to a novelty in the surgical anatomy of the buttons in PK, a distinct edge of the DM is very often
posterior cornea (Figure 2). Surgeons who perform DALK seen as the needle emerges from deep stroma, anterior
by the BB technique can easily relate to these clues. to DM. This edge is attributed to the DM. However, in
a) Intra-operatively, the exposed DM felt more DALK, when the DM was peeled off the donor button,
resilient than DM, and could withstand pressure the edge was still present suggesting that it is caused by
or force applied by a blunt instrument or swab something else (Figure 2F).
(Figure2A). f ) We and several surgeons4 have noted and co
b) The DM could in the vast majority of cases, mmented on the better structural integrity of the globe
be peeled off the donor corneal button very easily and after a DALK compared to a PK. DALK eyes could
smoothly (Figure 2B). This suggested that the plane withstand a degree of blunt trauma without rupture
of cleavage between DM and corneal stroma was unlike eyes that have undergone PK. It was counter
smooth and uniform offering little resistance during intuitive to attribute this additional strength entirely to
separation. the retained host DM.
Figure 2. Clinical clues suggesting the presence of Duas layer (DL). A. The exposed Descemets membrane (DM) is tougher and more resilient
than true DM. B. DM strips off easily from the donor lenticule without any strands extending between DM and overlying stroma. C. When the
big bubble does not extend to the trephine mark the stroma has to be mechanically separated from the underlying DM. Strands of collagen
are seen to extend between stroma and DM, which have to be mechanically severed or cut. D. A cannula is inserted through a tear in the
DM during DALK following an inadvertent tear intra-operatively. The DM has not scrolled. E. Post operatively, the same eye as in E, shows
a linear fold unlike the double contour line of a torn DM. F. When a suture is passed through the donor lenticule from which the DM has been
stripped, a distinct edge, normally attributed to the DM is still visible. All these clues suggested the presence of another layer besides the DM.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
214 DUAS LAYER
All the above were considered as clinical clues and starts as two or more small bubbles at the periphery
not evidence. Some had substance but others were which enlarge centrally to meet and coalesce. At times
mere clinical impressions and anecdotes. Collectively both Type 1 and Type 2 BB can appear in the same
however, they raised sufficient doubt on the concept of sclero-corneal disc. These are termed Mixed bubbles
Descemets baring in DALK leading to the hypothesis (Figure 3C). The two bubbles in mixed-BB can be in
that there exists in the posterior corneal stroma adjacent various combinations, a complete Type 1 BB and a
to the DM, a distinct layer of tissue, which provides a partial Type 2 BB (most common), a complete Type 1
plane of cleavage between its anterior surface and deep and a complete Type 2 BB and rarely a complete Type
stroma in DALK. This hypothesis was proposed and 2 with a partial Type 1 BB. Type 1 BB was the most
early clinical and histological evidence of its existence common (approximately 80%) and mixed BB the least.
was provided at the annual congress of The Royal The DM could be completely peeled off a Type 1BB
College of Ophthalmologists UK, in May 2007 and without deflating the BB (Figure 4A) suggesting that
further evidence presented at the Societa Italiana Cellule the posterior wall of the Type 1 B, in addition to the
Staminali e Superficie Oculare, VI Congresso S.I.C.S.S.O. DM is made of another distinct layer of tissue. This
Lecce, June 14-16, 2007. layer was termed the pre-Descemets layer (Duas layer)
(DL)7. Equally it was possible to first peel off the DM
from the sclero-corneal disc and then inject air to
THE EVIDENCE create a complete Type 1 BB indicating that the DM
is not essential for the creation of a Type 1BB. When
Ex-vivo experiments were performed on human sclero- an attempt was made to peel the DM off a Type 2 BB
corneal discs not suitable for transplantation; that it deflated immediately indicating that a Type 2 BB is
were maintained in organ culture medium and those a pre-Descemetic collection of air. Similarly, when the
dissected from fresh (within 24 hours of enucleation) DM was peeled off a mixed BB the Type 2 component
donor whole globes. Air was injected in the deep stroma deflated but the Type 1 component remained intact.
to simulate the surgical DALK procedure. Air was With continued injection of air, a Type 1 BB (with DM
noted to spread from the point of injection anteriorly, peeled off) became tense but did not extend beyond a
circumferentially and posteriorly to fill the corneal maximum of 9 mm diameter. At a pressure of around
stroma and eventually result in the formation of a BB. 700 mm Hg (with the tip of the injecting needle
Three types of bubbles could be produced. A Type 1 inserted through the posterior stroma to appear in the
bubble, which starts in the centre of the cornea by the centre of the BB) the Type 1 BB burst with a popping
coalescence of multiple smaller bubbles (Figure 3A) and sound. The bursting pressure of a Type 2 BB was
expands centrifugally and posteriorly to assume a well variable and much less because at times the DM burst
circumscribed dome shaped appearance. It reaches a and on other occasions it disinserted along a segment
maximum diameter of 9 mm and maximum height of its peripheral attachment. This indicates that DL
(measured from epithelium) of 5.5 mm. A Type 2 like the DM is impervious to air. This is an important
bubble, which is a thin walled bubble that starts at characteristic of the DL as compared to the rest of the
the periphery of the sclero-corneal disc and enlarges stroma where air moves in all directions. The tissue
on continuing injection of air to spread across almost of DL presented as a glistening, pliable, resilient and
the entire surface of the sclero-corneal disc (Figure 3B) tough layer (Figure4B). Tugging or pulling on the DL
reaching a diameter of 10-11 mm and a maximum with a forceps after removing the DM resulted in the
thickness of 6.5 mm. Occasionally this Type 2 BB formation of striae that could be seen extending from
Figure 3. Types of Big bubbles (BB). A. A type-1 BB, which is centrally located and does not extend for more than 9mm in diameter. This
is a pre-Duas layer BB (reproduced from the authors own publication in the Journal Ophthalmology 2013 [Reference 9]). B. A type-2 BB
which is thin walled and covers the entire posterior surface of the cornea. This is a pre-Descemetic BB. C. Mixed BB a central type-1 BB is
associated with a peripheral partial type-2 BB.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 215
Figure 4. A. A type-1 BB does not deflate when the Descemets membrane (DM) is peeled off. Peeling DM reveals the underlying Duas layer
(DL). B. The exposed and cut DL is seen as a flexible, pliable, resilient layer of tissue. Tugging on the tissue produces striae which extend to the
periphery of the cornea (reproduced from the authors own publication in the Journal Ophthalmology 20139).
the tip of the forceps radially across the boundary of the non-banded zones (Figure 5C). The collagen fibres are
BB to the limbus. This indicated that the DL extended largely oriented longitudinally and transversely with
to the limbus but the zone between the edge of the BB some running in an oblique direction (Figure 5D).
and the limbus was firmly attached to the underlying Long spacing collagen is prominent in DL towards
stroma. This attachment could not be broken either its posterior aspect closer to the apposition with DM
by injection of air or by attempts to mechanically and (Figures 5D, 5E). Occasionally broken strands of
physically peel of the DL from the edge of the BB collagen can be seen on the anterior surface of DL and
outwards. When DL from a Type 1 BB was excised appear as a recoiled clump of collagen (Figure 5F). In
along its circumference, further injection of air did not comparison, the corresponding width of the corneal
result in creation of another BB indicating that the DL stroma anterior to DL in un-inflated control eyes shows
is not a random separation of some posterior stromal only 3-5 lamellae. The fibril diameter in DL measures
lamellae of the corneal stroma. around 21.70 2.43 nm and in the corneal stroma
immediately overlying the DL it is 24.20 2.68 nm.
Characteristics of Duas layer (Description derived This difference is statistically significant with the DL
from the authors own recent publications references)7-9 fibrils being narrower. The inter-fibrillar distance is the
same in the DL (9.64 7.74 nm) as in the posterior
The clinical characteristics of DL as described above stroma (10.09 7.91 nm). However as the inter-fibrillar
and the histological features are largely derived from distance is measured between centres of adjacent fibrils
examination of the part of DL that makes up the the space between the narrower fibrils is greater in DL
posterior wall of the Type 1 BB with and without the than in the posterior corneal stroma. This can allow for
DM attached to it. Though the vast majority of eye greater filling-in with proteoaminoglycans and give it
donors in which it was demonstrated were in the age a gel like structure which in turn could explain why it
range of 50 to 94 years, it has also been demonstrated is impervious to air. On scanning electron microscopy
in infants and children. the anterior surface of DL shows parallel bundles of
Histological examination by light and electron collagen regularly arranged while the posterior surface
microscopy confirmed that the posterior wall of a Type shows a smooth pleated pattern made of coarse bundles
1 BB is made of a collagenous layer of tissue (DL) and of collagen (Figure 6A) and differs from the appearances
the DM and endothelium. Strands of collagen extend of the deep stroma (Figure 6B) and DM (Figure 6C).
from the adjacent stroma into the DL (Figure 5A). The Strands of collagen bundles bridge the space between
mean SD thickness of DL is 10.15 3.6 microns the DL and the stromal bed as demonstrated by
(range 6.3 to 15.83) compared to DM which showed both scanning and transmission electron microscopy
a mean thickness of 10.97 2.36 microns (range (Figure 5A, 6D). This explains the strands seen
7.8 to 13.98). The DL is made of collagen bundles intra-operatively as described above (see also clinical
organised as tightly packed thin lamellae numbering implications). Unlike the corneal stroma, DL that forms
5-8 (Figure5B). DM peeled from DL and from mixed the posterior wall of a Type 1BB did not demonstrate
BB does not show any split between banded and any keratocytes. Histology of mixed bubbles shows that
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
216 DUAS LAYER
a b
c d
e f
Figure 5. A. Light photomicrograph of a Type-1 BB from which the Descemets membrane (DM) has been peeled off centrally to reveal
the Duas layer (DL). Strands of collagen bundles (S) are seen extending from the stroma to DL. The separation occurs along the last row of
keratocytes (arrow). B-F.Transmission electron micrographs: B. DL is made of multiple thin lamellae closely applied to Descemets membrane
(DM). An endothelial cell (EC) is seen on the posterior surface of DM. Bar = 10 microns. C. The posterior wall of a Type-2 BB showing
histological features of DM; the banded (BZ) and non-banded (NBZ) zones and endothelium. The same features were seen in DM peeled
off a Type-1 BB. There was no split in BZ and NBZ. Bar = 5 microns. D. DL from a Type-1 BB made of multiple compact lamellae with
collagen bundles running in longitudinal, transverse and oblique directions. Bar = 5 microns. E. DL from a Type-1 BB with long spacing
collagen (arrow) adjacent to the DM. Bar = 1 micron. This is also evident as dark material in (D). F. A recoiled broken strand is seen on DL
as a clump of collagen (between the two arrows). Some keratocyte cellular debris is also present. Reproduced from the authors own publication
in the Journal Ophthalmology 20139.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 217
Figure 6. Scanning electron micrographs (SEM). A. The anterior
surface (star) and posterior surface (triangle) of Duas layer
(DL) showing parallel and regularly arranged collagen bundles
and a smooth pleated pattern respectively. The edge of the
Descemets membrane is also seen. B. The stromal bed of a type-
1 big bubble showing a criss-cross pattern with gaps related to
passage of air (arrows). This contrasts with the appearance of the
anterior surface of DL seen in a. C. The anterior surface of the
Descemets membrane (DM) presents as a very smooth surface.
D. Strands of collagen are seen extending from the stromal bed
to the anterior surface of DL. Ends of broken strands are visible
as small round dots (arrow). E. The end of the cleavage created
by the air bubble between DL and posterior stroma is visible.
DL is seen as a distinct and compact layer. Reproduced from the
authors own publication in the Journal Ophthalmology 20139.
the central BB is made of DL and DM with the air stroma. Collagen V was weakly positive in both DL and
separating DL from the posterior stroma as in a Type 1 stroma. There is no difference in the intensity of staining
BB, while the posterior bubble is due to air between DL for proteoglycans lumican, mimecan and decorin in DL
and DM as in a Type 2 BB. No split between banded and corneal stroma. Absence of keratocytes was also
and non-banded zones of the DM occurs in mixed noted by the lack of CD34 positivity in DL.
bubbles (Figure 5C). In summary, evidence from the ex-vivo experiments
Immunohistology demonstrates that DL, like corneal on human donor eyes therefore suggest that following
stroma, is primarily composed of collagen I. Collagens, intra-stromal injection of air DL separates no greater
IV, V and VI were present in DL of which IV and VI than 9 mm forming the type 1 bubble, which commences
were more in DL compared to adjacent deep corneal centrally by the accumulation and coalescence of
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
218 DUAS LAYER
several small bubbles and expands centrifugally; that body and root of the iris (Figure 7). Scanning electron
DL extends to the periphery but is firmly adherent to microscopy shows that the trabecular beams emerge
the peripheral stroma, that it is impervious to air, that radially from the anterior surface of the peripheral edge
the DM can be peeled off the type 1 bubble without of Schwalbes line or zone and are wrapped around by
deflating it, that the presence of DM is not essential for the peripheral part of the DM (Figure 8). However,
the formation of a type 1 bubble, that mixed bubbles when the DM is stripped off the posterior surface of
can occur and are not due to a split between banded and the cornea, DL can be seen as a smooth sheet, which
non-banded zones of the DM, that the DL that forms begins to split into radially oriented broad beams which
the wall of the type 1 bubble is devoid of keratocytes, in turn divide and subdivide to form narrower beams
that it contains a fair amount of type VI collagen and which interconnect and intertwine with similar adjacent
long spacing collagen, that it is not a random separation beams as they extend towards the iris and ciliary body,
of the posterior stroma leaving behind some residual constituting the trabecular meshwork (TM). This
stroma but a distinct layer that cannot be re-created observation is substantiated by transmission electron
by blowing out further residual stroma after excising microscopy (TEM) (Figure 9).
the first one (the DL), that the diameter of the fibrils in TEM of the peripheral part of the cornea confirms
the DL is significantly smaller than that of the posterior that DL continues beyond the termination of DM
cornea, and that the pre-Descemetic (Type 2) bubbles (Figure 9A). The compact lamellar arrangement of
start predominantly at the periphery and spread across DL begins to open approximately 350 microns central
the entire posterior surface of the cornea10. to the termination of the DM. Trabecular cells are
seen in the peripheral cornea in DL extending to a
Duas Layer and Trabecular Meshwork mean of 322 m (range 260 to 390 m) central to
the termination of DM (Figure 9B-G). Here they are
Further interesting information has emerged upon associated with deposition of basement membrane
examination of the termination of DL at the periphery which separate lamellae of DL. Attachments of the
along the circumference of the cornea at it junction with trabecular cells to the basement membrane and to each
the limbus. By light microscopy of cross sections of the other are visible within the periphery of DL. (Figure
cornea it can be seen that DL, which is visible as a band 9E-G). The morphology of trabecualr cells seen in
of tissue anterior to DM extends peripherally beyond the DL is distinct from keratocyte cell bodies that are
termination of DM, initially as a compact band, which seen further anterior to DM in the posterior corneal
then spreads out in a triangular manner with the fibres stroma. (Figure 9E). Whilst nuclei of trabecular cells
diverging further as they approach the sclera, ciliary and keratocytes can be demonstrated by DAPI staining
(nuclear stain) the trabecular cells are negative for CD34
(keratocyte marker) which stains all the keratocytes in
the corneal stroma. The presence of trabecular cells
in DL corresponds to the point at which the collagen
lamellae of DL began to split and separate. The 5
to 8 lamellae of DL separate in the antero-posterior
direction and also split into narrower bands which
intertwine and cross each other as they extend towards
the sclera, ciliary body and iris root. The majority of
the trabecular beams that form the TM posterior to the
canal of Schlemm are made of collagen fibres arising
form the posterior aspect of DL. The anterior collagen
fibres, together with some fibres of the deep limbus/
sclera form the anterior wall of the canal of Schlemm.
Long spacing collagen that has been described in DL is
also abundant in the TM. Elastic fibres are present in
the TM but not in DL.
The separation of DL collagen lamellae into broad
and narrow beams along the circumference of the
Figure 7. Light photomicrograph illustrating Duas layer extending
termination of DL and their continuity with the TM
beyond the termination of the DM (black arrow) and fanning out as
the trabecular meshwork. From the point indicated by the white arrow
beams seen on SEM and with the collagen core of the
the stromal fibres can be seen to diverge and spread out as the beams of TM beams seen on TEM establish that the TM is a
the trabecular meshwork before attaching to the ciliary body and the continuation of DL. SEM of DL after stripping off the
iris. CB, ciliary body; S, canal of Schlemm. Reproduced from the authors DM illustrates that DL continues imperceptibly with
own publication in the British Journal of Ophthalmology, 201410. the broader beams of the apical part of the TM.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 219
Figure 8. Scanning electron micrographs (SEM). A. The peripheral cornea with Descemets membrane (DM) in situ. The endothelial cells stop (thick
arrow) just before the zone with curly lines (star). The trabecular beams are seen to emerge from the peripheral termination of the DM (thin arrow)
and can be seen to be mainly radially oriented. The beams are generally thicker near their origin and become narrower distal to the termination of
the DM. The beams can be seen to divide, subdivide and interconnect. Bar = 100 m. B. SEM of periphery of Duas layer (DL) from which the
DM has been removed. DL is visible as a homogenous sheet. There is a tear in DL (arrow) through which the distinctly different architecture of the
underlying stroma is visible. At the periphery, DL tissue spreads out as the trabecular beams as described in (A). Bar= 100 m. C. The transition of
DL into the trabecular beams is clearly visible. Bar = 10 m. D. The splitting of DL into broad sheets which narrow, subdivide and make connections
with adjacent beams to form the trabecular meshwork is clearly seen. Near the edge of DL they appear as broad(er) sheets which narrow distally to
become more like beams. Bar = 10 m. Reproduced from the authors own publication in the British Journal of Ophthalmology, 201410.
The demonstration of the presence of trabecular cells last row of keratocytes and the DM reduces compared
within the peripheral cornea in DL is another important to the central part of DL.
observation. These cells are surrounded by basement Thus, while the bulk of the corneal stroma merges
membrane with which they establish attachments, at the periphery with the scleral stroma the collagen
within DL. TM beams are known to be enveloped of DL continues as the TM. The significance of the
with a basal lamina to which trabecular/endothelial observations and the importance of the TM in relation
cells attach11. The presence of these cells with basement to glaucoma, a blinding disease, should influence the
membrane in the periphery of DL strongly suggests that direction of some relevant research in determining
the formation of the TM beams commences in DL, interactions between the cornea and the TM.
approximately 500 microns central to the termination
of the DM. Staining for laminin, which is a basement CLINICAL IMPLICATIONS
membrane component12 is strongly positive in the AND APPLICATIONS
TM and the peripheral DL corroborating the above
observation. The central collagen core of the TM beams Identification of the DL and its relationship to the
is acellular15. This is consistent with the finding that no different types of big bubbles formed on injection of
keratocytes are noted in DL either. This suggests that air is clinically very relevant to the DALK procedure.
the formation of the TM commences in the peripheral Surgeons have long recognised the formation of a
cornea, central (anterior) to the termination of the DM central BB with a white ring as the commonest type of
and not at the termination of the DM. As DL becomes BB. This is clearly a Type 1 BB. The interesting clinical
thinner towards the periphery the distance between the understanding here is that most surgeons make a trephine
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
220 DUAS LAYER
b c d
e f g
Figure 9. Transmission electron micrographs (TEM) A. Montage of TEM sections from peripheral part of cornea to trabecular meshwork. Duas
layer (DL) fibres anterior to Descemets membrane (DM) are seen (double arrows) to split and separate central to the termination of DM (single
arrow) and continue to diverge to form the narrow beams of the trabecular meshwork. This illustrates that the starting point of the trabecular
meshwork is anterior to the DM, in DL of the peripheral cornea. The dark black bands correspond to the grid of the TEM. Bar (seen on the black
bands) = 5 m. B. A large trabecular cell (Star) is seen anterior to DM within the collagen of DL. The cell is surrounded with basement membrane
(BM) (black arrows). No keratocytes are visible in the adjacent stroma on either side. Bar = 10 m. C. A large trabecular cell (star) with a prominent
nucleus is seen anterior to DM in the collagen of DL. There is BM material between it and the collagen tissue to which it is closely applied. No
keratocytes are visible in the adjacent stroma on either side. Bar = 2 m. D. A large trabecular cell is seen anterior to DM in the collagen of DL. The
cell body of a keratocyte (arrow) is seen approximately 15 microns from the DM in the posterior corneal stroma but no keratocyte is visible in DL.
Bar = 5 m. E. Distinct layers of BM are seen separating the collagen of DL anterior to DM. The cell body of a transversely sectioned trabecular cell
in DL with attachments to BM (arrows) is also seen. Bar = 2 m. F. Cell-cell adhesions are distinctly visible (arrows) between cells in DL. Bar = 1
m. G. Cell BM attachments are distinctly seen (arrows) in DL. DM = Descemets membrane. Cell-cell and cell basement membrane attachments
of the kind seen in (F) and (G) are not usually associated with keratocytes; Bar = 1 m. Reproduced from the authors own publication in the British
Journal of Ophthalmology, 201410.
incision of between 7.5 to 8.5 mm diameter and stop be physically broken or cut. This also indicates that the
the BB when it reaches the trephine mark. The fact is plane of separation of a Type 1 BB is not between deep
that the BB stops itself. It does not extend beyond 9 mm stroma and DM but rather between deep stroma and
hence it is important that DALK greater than 9 mm DL. The demonstration of DL also explains the reason
should not be attempted as air separation of DL from for the classical white ring seen surrounding most big
the deep stroma will not occur to the trephine incision bubbles. In Type 1 BB the air separating DL from deep
and mechanical separation with a spatula will have to be stroma stretches the attachments between DL and the
attempted. This carries a risk of perforation of DL. An stroma. As these break the BB enlarges and so does the
ideal size for DALK, based on this observation would surrounding white ring. When the separation reaches its
be no greater than 8 mm. Even so, in some instances maximum, the stretching of tissue between the central
the BB may not be centred on the trephine incision DL and the stroma at the edge of the BB produces the
and for varying clock hours along the circumference white ring. As soon as the stretching force is released or
mechanical separation will be required. Strands of eased by withdrawal of the needle or escape of air, the
collagen tissue are seen extending between the anterior white ring markedly fades in whiteness or disappears,
surface of the DL and the deep stroma, which have to supporting the explanation offered.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 221
Figure 10. A. Immunofluorescence histology montage, collagen VI (bar = 500 m). Duas layer (DL) forming the posterior wall of a big bubble
(BB), the adjacent attached part of the DL and the trabecular meshwork (TM) all show strong staining for collagen VI suggesting that the layer
is a continuum from the centre of the cornea across the periphery into the trabecular meshwork. B. Immunofluorescence histology montage,
collagen V (bar = 500 m). DL forming the posterior wall of the BB was weakly positive for collagen V but the attached part of DL and the TM
stained stronger for collagen V. Arrow indicates the end of the BB. C. Immunofluorescence histology montage, laminin (bar = 100 m). The
remnant of Descemets membrane (DM) (arrow), the peripheral part of DL and TM stain positive for laminin. This is most likely related to the
basement membrane seen in the DL anterior to the DM at the periphery of the cornea. D. Immunofluorescence histology montage, laminin
(bar = 500 m). The peripheral part of DL and TM stain strongly for laminin. The DM has been removed. White line indicates part of DL
anterior and central to DM. E. Immunofluorescence histology montage of CD34 (keratocyte marker, bar = 500 m). The stroma is strongly
positive for CD34 cells. DL is negative for CD34. The TM and peripheral DL show nuclei (blue dots = DAPI [4,6-diamidino-2-phenylindole]
stain in all sections) but the corresponding cells are negative (lack of green fluorescence) for CD34 indicating that these cells are not keratocytes.
Reproduced from the authors own publication in the British Journal of Ophthalmology, 201410.
Surgeons performing DALK by the big bubble For almost as long as the big bubble DALK procedure
technique have also reported the occasional sudden has been in vogue, surgeons have commented on the
appearance of a big bubble that extends to the periphery appearance of distinctly visible double bubbles thought
in one or more quadrants without the classical white admittedly rare. The explanation offered and accepted
ring. Terms such as explosive bubble or glassy bubble for this has been a split between banded and non-banded
have been used to explain this type of bubble. This is zones of the DM, usually partial with air accumulating
clearly the Type 2 or pre-Descemetic BB that extends between deep stroma and DM and in a pocket between
to the periphery and as there is an easily separable plane the split banded and nonbanded zones of DM. The
of cleavage between DM and DL, a white ring does not knowledge of DL has not made it absolutely clear that
appear. such a split does not occur but rather the double bubbles
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
222 DUAS LAYER
are the Mixed BB as described above, one between deep It is postulated that in patients with keratoconus,
stroma and DL and the other between DL and DM. DL stretches along with the DM and that acute hydrops
The latter can be partial or complete. is not just due to a tear in the DM but also due to a tear
Clinical experience has also taught us that during or dehiscence in DL. Discontinuity of both DM and
BB DALK, if the DM is punctured, at times it scrolls DL, in the background of abnormal collagen related to
in the classical manner described for tears in DM keratoconus is more likely result in sudden hydration
and at times it does not. This difference can now be of the stroma rather than a tear in DM alone. It is also
attributed to punctures/tears in DM vs punctures/tears postulated that Descemetoceles, which are believed
in DL. In the latter situation, the opening tends not to offer some resistance before perforation, retain
to spontaneously extend and DALK can be completed this strength due to a covering of DL. When DL is
despite the tear. The risk of double chamber too is less damaged or destroyed by proteolytic enzymes, the DM
compared to a DM tear. Furthermore, descriptions rapidly perforates. Anecdotal evidence to demonstrate
of bursting of the DM following intraoperative presence of a DL covering over DM in Descemetcoeles
puncture have been reported. Once again, it is now is available. Macular dystrophy, which presents as
apparent that this is more likely to be a phenomenon opacities across the entire stroma, has been shown to
associated with a Type 1 BB than with a Type 2 BB. affect DL as well. When DALK by BB technique is
Intraoperative signs such as the appearance of a carried out for macular dystrophy, residual opacities are
BB from the periphery spreading centrally, absence present in the retained DL with a Type 1 BB. Some
of a white ring, rapid expansion of the BB which surgeons have left these and complete the operation
extends well beyond the trephine mark, a very smooth as normal and other have painstakingly dissected off
surface of the anterior wall of the BB after removal of DL (converting the Type 1 BB to a Type 2 BB) to
the anterior stroma (as against the rough appearance remove all opacities. Thus for macular dystrophy, a
related to broken strands of stroma of DL) are Type 2 bubble may be more appropriate though the
indicative of the presence of a Type 2 BB. A spatula advantage of removing DL in these patients has yet
may be inserted between the anterior wall of the BB to be demonstrated. In our experience and that of a
and the deep stroma along the circumference of the high volume DALK surgeon (Dr. Tarek Katamish,
trephine mark. If it passes readily in the plane the BB Cairo) in most patients with post infectious corneal
wall is likely to be DM and not DL. Knowledge of the scarring; removal of the affected stroma by the big
presence of a Type 1 or Type 2 BB helps the surgeon to bubble technique reveals a clear (unscarred) DL. This
take additional precautions, such as repeated release of is an interesting observation which could be related to
aqueous through the paracentesis to lower eye pressure the paucity of keratocytes in this layer, which would
and taking care not to touch the larger Type 2 BB with otherwise undergo transformation to myofibroblasts
the tip of the instrument used to make the paracentesis and fibroblasts following infection and inflammation
opening, thus making the operation safer. There are no and lead to scarring. Thus the knowledge of the
definitive tips that can predict the appearance of the existence of DL is informing our understanding of
Type 1 bubble but insertion of the needle or cannula posterior corneal pathology.
as deep as possible helps. For a long time surgeons The knowledge of this layer and understanding of
have known that a DALK eye is less susceptible to its biomechanical properties in terms of its strength,
rupture following trauma compared to a PK eye. This flexibility and resilience has encouraged surgeons
was attributed to the retention of the recipients DM. to perform innovative surgical procedures. After
However, we now know that it is the eyes where DALK removal of the corneal stroma by the big bubble
has been completed with a Type 1 BB, i.e where DL is technique in cases with corneal scarring one surgeon
retained, that are stronger due to the strength afforded (Dr. Ahmad Atef, Cairo) has successfully performed
by the DL. When air was injected in the stroma of a phacoemulsification procedure with lens implant
corneal buttons obtained from eyes that had undergone in two patients). This procedure termed the DALK-
phacoemulsification surgery it was noted that the site Triple procedure13 is a direct clinical application of
of cataract incision and side port(s) remained weak the understanding of the biomechanical properties
and that air leaked from these sites restricting the and strength of the DL. Drs. Agarwal A and Dua HS
size of the bubble formed due to loss of air pressure have developed an innovative procedure for endothelial
in the stroma. This would apply to any full thickness transplant termed pre-Descemets endothelial
penetrating injury to the cornea thus telling us that keratoplasty (PDEK) wherein a donor endothelial graft
DALK should be performed with caution in eyes with is prepared by harvesting a lenticule composed of DL +
previous penetrating injury (surgical or traumatic) as DM + endothelium14. This is relatively easier to handle,
internal leakage of air and failure to obtain a BB or one tends to scroll less and can be harvested from eyes of
of adequate size is a definitive risk. any age (as young as 1 year).
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
DUAS LAYER 223
How this layer affects and contributes to the 5. Anwar M, Teichmann KD. Big-bubble technique to bare
biomechanics of the posterior cornea remains to be Descemets membrane in anterior lamellar keratoplasty. J
determined. Experiments towards ascertaining this Cataract Refract Surg. 2002; 28:398-403.
6. Melles GRJ, Remeijer L, Geerards AJM, Beekhuis WH. A Quick
are underway. Unlike DL, the TM also has a network
Surgical Technique for Deep, Anterior Lamellar Keratoplasty
of elastic (like) fibres15 that are linked to the tendon of Using Visco-dissection. Cornea. 2000; 19:427-32.
the ciliary muscle and find attachment in the corneal 7. Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal
stroma15. It is believed that the ciliary muscle tone can anatomy redefined: a novel pre-Descemets layer (Duas layer).
directly affect the TM beams and influence the flow Ophthalmology. 2013; 120:1778-85.
of aqueous15. Biomechanical properties of the eye are 8. Dua HS, Faraj LA, Branch MJ, Yeung AM, Elalfy MS, Said DG,
known to affect the pathogenesis of glaucoma16. The Gray T, Lowe J. The collagen matrix of the human trabecular
cornea is subject to constant stress related to movements meshwork is an extension of the novel pre-Descemets layer
induced by blinks, eye rubbing and heartbeat17. It is likely (Duas layer). Br J Ophthalmol. 2014; 95
9. Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Whats in a
that some of this is transmitted to the TM through the
Name? The Novel Pre-posterior Limiting Lamina Layer.
extension of DL in to the core of the TM beams. Eyes Ophthalmology. 2014. DOI: 10.1016/j.ophtha.2013.12.001
with glaucoma and thin corneas are known to have greater 10. Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Author reply: To
visual field loss at presentation and greater shallowing of PMID 23714320. Ophthalmology. 2014; 121:e25-6.
the cup after treatment indicating greater displacement 11. Tripathi BJ, Hansen M, Li J, Tripathi RC. Identification of type
(compliance) of the lamina cribrosa18, 19. This is attributed VI collagen in the trabecular meshwork and expression of its
to the biomechanics of a thin cornea. A recent study mRNA by trabecular cells. Exp Eye Res. 1994; 58:181-7.
comparing DALK with penetrating keratoplasty (PK) for 12. Martin GR, Timpl R. Laminin and other basement membrane
keratoconus reported that incidence of high intraocular components. Annu Rev Cell Biol. 1987; 3:57-85.
13. Zaki AA, Elalfy MS, Said DG, Dua HS. Deep anterior lamellar
pressure and secondary glaucoma was significantly higher
keratoplasty-triple procedure: a useful clinical application of the
in patients undergoing PK20. In PK DL is completely pre-Descemets layer (Duas layer). Eye. 2014. DOI: 10.1038/
transected along the graft host junction while in DALK eye.2014.273
DL is preserved. The effect of DL on posterior corneal 14. Agarwal A, Dua HS, Narang P, Kumar DA, Agarwal A, Jacob
biomechanics and on the TM and consequently on S, Agarwal A, Gupta A. Pre-Descemets endothelial keratoplasty
aqueous drainage will be an area of investigation. It is (PDEK). Br J Ophthalmol. 2014; 98:1181-5.
our experience and observation and that of several other 15. Lutjen-Drecoll E, Futa R, Rohen JW. Ultrahistochemical studies
surgeons that during the DALK procedure escape of small on tangential sections of the trabecular meshwork in normal and
air bubbles into the anterior chamber of the eye through glaucomatous eyes. Invest Ophthalmol Vis Sci. 1981; 21:563-
73.
the trabecular meshwork is a common occurrence. As
16. Mangouritsas G, Morphis G, Mourtzoukos S, Feretis E.
DL is impervious to air and the corneo-scleral trabecular Association between corneal hysteresis and central corneal
meshwork has pores, air injected into the stroma can only thickness in glaucomatous and non-glaucomatous eyes. Acta
escape into the anterior chamber through the pores at Ophthalmol. 2009; 87:901-5.
the extreme periphery. This also supports the association 17. Singh K, Dion C, Costantino S, Wajszilber M, Lesk MR, Ozaki
between the DL and the trabecular meshwork beams. T. Development of a novel instrument to measure the pulsatile
Ongoing work on the dynamics of the big bubble movement of ocular tissues. Exp Eye Res. 2010; 91:63-8.
formation, both Type 1 and Type 2 is likely to reveal 18. Shah H, Kniestedt C, Bostrom A, Stamper R, Lin S. Role of
further interesting aspects related to the microanatomy central corneal thickness on baseline parameters and progression
of visual fields in open angle glaucoma. Eur J Ophthalmol.
of the respective parts of the cornea and is also likely to
2007; 17:545-9.
provide information on the structure and arrangement of 19. Lesk MR, Hafez AS, Descovich D. RElationship between central
collagen fibres in the substantia propria (stroma) of the corneal thickness and changes of optic nerve head topography
cornea. and blood flow after intraocular pressure reduction in open-
angle glaucoma and ocular hypertension. Arch Ophthalmol.
REFERENCES 2006; 124:1568-72.
20. Zhang YM, Wu SQ, Yao YF. Long-term comparison of full-bed
1. Armitage WJ, Tullo AB, Larkin DF. The first successful full- deep anterior lamellar keratoplasty and penetrating keratoplasty
thickness corneal transplant: a commentary on Eduard Zirms in treating keratoconus. J Zhejiang Univ Sci B. 2013; 14:438-
landmark paper of 1906. Br J Ophthalmol. 2006; 90:1222-3. 50.
2. Anwar M. Dissection technique in lamellar keratoplasty. Br J
Ophthalmol. 1972; 56:711-3. First author:
3. Melles GR, Lander F, Rietveld FJ, Remeijer L, Beekhuis
WH, Binder PS. A new surgical technique for deep stromal, Harminder S. Dua, MD, PhD
anterior lamellar keratoplasty. Br J Ophthalmol. 1999; Neuroscience, School of Medicine,
83:327-33. University of Nottingham, England.
4. Fontana L TG. Atlas of Lamellar Keratoplasty. San Giovan:
Fabiano, 2007.
JOURNAL OF EMMETROPIA - VOL 5, OCTOBER-DECEMBER
Você também pode gostar
- Mecha World Compendium Playbooks BWDocumento12 páginasMecha World Compendium Playbooks BWRobson Alves MacielAinda não há avaliações
- Analysis of Rates (Nh-15 Barmer - Sanchor)Documento118 páginasAnalysis of Rates (Nh-15 Barmer - Sanchor)rahulchauhan7869Ainda não há avaliações
- Kyestone Flaps PDFDocumento9 páginasKyestone Flaps PDFDra. Bianca Ariza MoralesAinda não há avaliações
- Highlights ASME Guides Preheat PWHT IDocumento4 páginasHighlights ASME Guides Preheat PWHT IArul Edwin Vijay VincentAinda não há avaliações
- PETAL Sentence StartersDocumento1 páginaPETAL Sentence StartersSnip x Hunt manAinda não há avaliações
- Endoscopic Endonasal Dacryocystorhinostomy: Best Surgical Management For DCRDocumento4 páginasEndoscopic Endonasal Dacryocystorhinostomy: Best Surgical Management For DCRwhiezardAinda não há avaliações
- New Technique of Deep Anterior Lamellar KeratoplastyDocumento5 páginasNew Technique of Deep Anterior Lamellar KeratoplastyLeonardo TorquettiAinda não há avaliações
- An Introduction To Corneal TransplantationDocumento2 páginasAn Introduction To Corneal TransplantationNovii NoviiAinda não há avaliações
- Boynton 2015Documento8 páginasBoynton 2015IvonneAinda não há avaliações
- Descemet Membrane Endothelial Keratoplasty in Pseudophakic Bullous Keratopathy: Outcomes and Evidence-Based SuggestionsDocumento6 páginasDescemet Membrane Endothelial Keratoplasty in Pseudophakic Bullous Keratopathy: Outcomes and Evidence-Based SuggestionsRaymond 102014223Ainda não há avaliações
- Capa de Dua en La CórneaDocumento8 páginasCapa de Dua en La CórneakaritoAinda não há avaliações
- 293 2045 1 PBDocumento3 páginas293 2045 1 PBSaurabh JainAinda não há avaliações
- DR Sonali Sahoo - JC - 05-08-2019Documento6 páginasDR Sonali Sahoo - JC - 05-08-2019Raúl Plasencia SaliniAinda não há avaliações
- DWEK DSO ReviewDocumento11 páginasDWEK DSO ReviewnoonilAinda não há avaliações
- Management of Post-Keratoplasty AstigmatismDocumento11 páginasManagement of Post-Keratoplasty Astigmatismdianis0506Ainda não há avaliações
- 10 Descemet's Stripping Automated Endothelial Keratoplasty - Innovations in Surgical TechniqueDocumento5 páginas10 Descemet's Stripping Automated Endothelial Keratoplasty - Innovations in Surgical TechniqueMashhoor AlfayezAinda não há avaliações
- Txin KCEye VisionDocumento15 páginasTxin KCEye VisionmorellmireiaAinda não há avaliações
- CXL Thin CorneaDocumento10 páginasCXL Thin CorneaApps OmAinda não há avaliações
- Corneal Edema Post Cataract SurgeryDocumento13 páginasCorneal Edema Post Cataract SurgeryPrathibha M ChachadiAinda não há avaliações
- Keratoplasty PDFDocumento5 páginasKeratoplasty PDFFachri PadmaridhoAinda não há avaliações
- Atopic Dermatitis Is A Risk Factor For Intracorneal Ring Segment ExtrusionDocumento7 páginasAtopic Dermatitis Is A Risk Factor For Intracorneal Ring Segment ExtrusionJuliana FreitasAinda não há avaliações
- Cornea Duanes Ophthalmology 2337 2337Documento75 páginasCornea Duanes Ophthalmology 2337 2337Endre Shitaye KulkiAinda não há avaliações
- Endothelial KeratoplastyDocumento6 páginasEndothelial KeratoplastyRijal SaputroAinda não há avaliações
- Descemet Membrane Detachment During Cataract Surgery: Etiology and ManagementDocumento7 páginasDescemet Membrane Detachment During Cataract Surgery: Etiology and Managementjorge vegaAinda não há avaliações
- Newer Trends in Lamellar Keratoplasty: Dr. Hijab MehtaDocumento6 páginasNewer Trends in Lamellar Keratoplasty: Dr. Hijab MehtaNur Zulaekha Soraya YayaAinda não há avaliações
- Combination of Periocular Myocutaneous Flaps For One-Stage Reconstruction of Extensive Defects of The EyelidDocumento5 páginasCombination of Periocular Myocutaneous Flaps For One-Stage Reconstruction of Extensive Defects of The EyelidBrînduşa CiobanuAinda não há avaliações
- Corneal Transplantation in Modern EraDocumento16 páginasCorneal Transplantation in Modern Eraसुनन्दन भट्टAinda não há avaliações
- Ormond 2013Documento12 páginasOrmond 2013Hafiz AlfarizieAinda não há avaliações
- Ibm 1Documento7 páginasIbm 1rintanfsAinda não há avaliações
- Anterior Chamber Air Bubble To Achieve Graft Attachment After DMEK: Is Bigger Always Better?Documento4 páginasAnterior Chamber Air Bubble To Achieve Graft Attachment After DMEK: Is Bigger Always Better?David MartínezAinda não há avaliações
- Clínica Evidencie of The Pre-Descemets Layer (Dua's Layer) in Corneal Pathology, H.S Dua, Nature, 2016Documento2 páginasClínica Evidencie of The Pre-Descemets Layer (Dua's Layer) in Corneal Pathology, H.S Dua, Nature, 2016Reila KnbsAinda não há avaliações
- Alcohol Debridement of The Corneal Epithelium in PRK and LASEK: An Electron Microscopic StudyDocumento4 páginasAlcohol Debridement of The Corneal Epithelium in PRK and LASEK: An Electron Microscopic StudymauricehungAinda não há avaliações
- An Incident of Subcutaneous Emphysema Following Laser Tooth ExposureDocumento4 páginasAn Incident of Subcutaneous Emphysema Following Laser Tooth ExposureVeronica ChinAinda não há avaliações
- Epiphora Drainage by DCR - Long-Term Results: Original ResearchDocumento5 páginasEpiphora Drainage by DCR - Long-Term Results: Original ResearchSaatvik AtriAinda não há avaliações
- Current Trends Rhinoplasty Rollin DDocumento7 páginasCurrent Trends Rhinoplasty Rollin Dmaxillo.arrasAinda não há avaliações
- Deep Anterior Lamellar Keratoplasty: A Surgeon 'S Guide: SciencedirectDocumento14 páginasDeep Anterior Lamellar Keratoplasty: A Surgeon 'S Guide: SciencedirectAshis BiswasAinda não há avaliações
- Management of Complex Orbital Fractures: Article in PressDocumento5 páginasManagement of Complex Orbital Fractures: Article in Pressstoia_sebiAinda não há avaliações
- INTRODUCTION NeewDocumento33 páginasINTRODUCTION NeewMuhammad MustafaAinda não há avaliações
- Cataract Surgery, 3rd Edition: PART VII - Management of Complications Chapter 49 - Corneal Edema After Cataract SurgeryDocumento14 páginasCataract Surgery, 3rd Edition: PART VII - Management of Complications Chapter 49 - Corneal Edema After Cataract Surgerymithaa octoviagnesAinda não há avaliações
- NigerJClinPract2181075-1842756 003042Documento3 páginasNigerJClinPract2181075-1842756 003042Alma AlvarezAinda não há avaliações
- The History of Corneal Transplantation: Chad K RostronDocumento14 páginasThe History of Corneal Transplantation: Chad K RostronDebby SiltamiAinda não há avaliações
- CoronectomyDocumento6 páginasCoronectomyToothless bdgAinda não há avaliações
- The Resiliency of The Corneal Endothelium To Refractive and Intraocular SurgeryDocumento11 páginasThe Resiliency of The Corneal Endothelium To Refractive and Intraocular SurgeryKreAch3RAinda não há avaliações
- Foam ImpressionDocumento3 páginasFoam ImpressionbkprosthoAinda não há avaliações
- Cataract Surgery in Corneal Transplantation: ReviewDocumento5 páginasCataract Surgery in Corneal Transplantation: ReviewMariana Luzardo bravoAinda não há avaliações
- Kyung 2013Documento4 páginasKyung 2013thompson sousa thompsonAinda não há avaliações
- Mandal 2016Documento4 páginasMandal 2016maria astridAinda não há avaliações
- Correction of The Soft Tissue Pollybeak Using Triamcinolone InjectionDocumento5 páginasCorrection of The Soft Tissue Pollybeak Using Triamcinolone Injectionmiglena-filipova-5062Ainda não há avaliações
- 217 222CicatricialEctropionDocumento7 páginas217 222CicatricialEctropionRania EAinda não há avaliações
- Matching Surgical Approach To Condylar Fracture TypeDocumento7 páginasMatching Surgical Approach To Condylar Fracture TypeMashood AhmedAinda não há avaliações
- 2019 Article 716Documento5 páginas2019 Article 716Manling JaoAinda não há avaliações
- Review Article: Pathogenesis and Management of Macular Hole: Review of Current AdvancesDocumento8 páginasReview Article: Pathogenesis and Management of Macular Hole: Review of Current AdvancesIvonne AffendyAinda não há avaliações
- 2019 Article 716Documento5 páginas2019 Article 716Manling JaoAinda não há avaliações
- Calli2021, Lamellar Corneal Patch Grafts in The ManagementDocumento5 páginasCalli2021, Lamellar Corneal Patch Grafts in The Managementrino agustian prajaAinda não há avaliações
- Phototherapeutic Keratectomy: Who Are The Best Candidates and How Do You Treat Them?Documento3 páginasPhototherapeutic Keratectomy: Who Are The Best Candidates and How Do You Treat Them?Mashhoor AlfayezAinda não há avaliações
- Medial Thigh FlapDocumento28 páginasMedial Thigh Flapdrgurpal74Ainda não há avaliações
- The Temporoparietal Galea Flap: Luc Cesteleyn, MD, DDSDocumento14 páginasThe Temporoparietal Galea Flap: Luc Cesteleyn, MD, DDSlaljadeff12Ainda não há avaliações
- Suture TipDocumento5 páginasSuture Tipstéphan AlessandroAinda não há avaliações
- Human Corneal Anatomy Rede Fined: A Novel Pre-Descemet's Layer (Dua's Layer)Documento8 páginasHuman Corneal Anatomy Rede Fined: A Novel Pre-Descemet's Layer (Dua's Layer)alejandro matiasAinda não há avaliações
- Meds CapeDocumento13 páginasMeds CapeputrishabrinaAinda não há avaliações
- IJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.HDocumento6 páginasIJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.Hiaset123Ainda não há avaliações
- A New Approach To The Treatment of True-Combined Endodontic-Periodontic Lesions by The Guided Tissue Regeneration TechniqueDocumento4 páginasA New Approach To The Treatment of True-Combined Endodontic-Periodontic Lesions by The Guided Tissue Regeneration TechniqueKarin Noga VerhagenAinda não há avaliações
- Article 3Documento7 páginasArticle 3Lana DbbAinda não há avaliações
- Complications in UveitisNo EverandComplications in UveitisFrancesco PichiAinda não há avaliações
- Jul - Dec 09Documento8 páginasJul - Dec 09dmaizulAinda não há avaliações
- Research FinalDocumento55 páginasResearch Finalkieferdem071908Ainda não há avaliações
- Hare and Hyena: Mutugi KamundiDocumento18 páginasHare and Hyena: Mutugi KamundiAndresileAinda não há avaliações
- Alaba Adeyemi AdediwuraDocumento12 páginasAlaba Adeyemi AdediwuraSchahyda ArleyAinda não há avaliações
- ISA InTech Journal - April 2021Documento50 páginasISA InTech Journal - April 2021Ike EdmondAinda não há avaliações
- Best Mutual Funds For 2023 & BeyondDocumento17 páginasBest Mutual Funds For 2023 & BeyondPrateekAinda não há avaliações
- Maya Deren PaperDocumento9 páginasMaya Deren PaperquietinstrumentalsAinda não há avaliações
- Li JinglinDocumento3 páginasLi JinglincorneliuskooAinda não há avaliações
- Nantai Catalog NewDocumento30 páginasNantai Catalog Newspalomos100% (1)
- Sale Counter List JuneDocumento9 páginasSale Counter List Junep6a4nduAinda não há avaliações
- GGG Sri MDocumento2 páginasGGG Sri MGiovanni LuigiAinda não há avaliações
- Multinational MarketingDocumento11 páginasMultinational MarketingraghavelluruAinda não há avaliações
- Central University of Karnataka: Entrance Examinations Results 2016Documento4 páginasCentral University of Karnataka: Entrance Examinations Results 2016Saurabh ShubhamAinda não há avaliações
- Mueller Hinton Agar (M-H Agar) : CompositionDocumento2 páginasMueller Hinton Agar (M-H Agar) : CompositionRizkaaulyaaAinda não há avaliações
- UNIT 5-8 PrintingDocumento17 páginasUNIT 5-8 PrintingNOODAinda não há avaliações
- Is 2 - 2000 Rules For Rounded Off For Numericals PDFDocumento18 páginasIs 2 - 2000 Rules For Rounded Off For Numericals PDFbala subramanyamAinda não há avaliações
- Instant Download Business in Action 7Th Edition Bovee Solutions Manual PDF ScribdDocumento17 páginasInstant Download Business in Action 7Th Edition Bovee Solutions Manual PDF ScribdLance CorreaAinda não há avaliações
- Shri Naina Devi Aarti English 167Documento5 páginasShri Naina Devi Aarti English 167ratt182Ainda não há avaliações
- WWW Studocu Com in N 29646569 Sid 01682568219Documento1 páginaWWW Studocu Com in N 29646569 Sid 01682568219Nivetha SelvamuruganAinda não há avaliações
- Optimized Maximum Power Point Tracker For Fast Changing Environmental ConditionsDocumento7 páginasOptimized Maximum Power Point Tracker For Fast Changing Environmental ConditionsSheri ShahiAinda não há avaliações
- Safety Bulletin 09 - Emergency Escape Breathing Device - Product RecallDocumento2 páginasSafety Bulletin 09 - Emergency Escape Breathing Device - Product RecallMuhammadAinda não há avaliações
- Educationusa 2022globalguide Final Reduced SizeDocumento84 páginasEducationusa 2022globalguide Final Reduced SizeAnna ModebadzeAinda não há avaliações
- GPP Calendar of Activities 2022 23 SdoDocumento5 páginasGPP Calendar of Activities 2022 23 SdoRomel GarciaAinda não há avaliações
- Caring For Women Experiencing Breast Engorgement A Case ReportDocumento6 páginasCaring For Women Experiencing Breast Engorgement A Case ReportHENIAinda não há avaliações
- Galgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesDocumento2 páginasGalgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesRohit Singh BhatiAinda não há avaliações
- Yetta Company ProfileDocumento6 páginasYetta Company ProfileAfizi GhazaliAinda não há avaliações