Escolar Documentos
Profissional Documentos
Cultura Documentos
Prevalence and Association of Cost of Hospital Malnutrition in Pediatric Intensive Care Unit of Sanglah Hospital During 2015
Enviado por
Inez Ann Marie TumbelakaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Prevalence and Association of Cost of Hospital Malnutrition in Pediatric Intensive Care Unit of Sanglah Hospital During 2015
Enviado por
Inez Ann Marie TumbelakaDireitos autorais:
Formatos disponíveis
Crit Care Shock (2017) 20:10-16
Prevalence and association of cost and hospital malnutrition in Pedi-
atric Intensive Care Unit Sanglah Hospital during 2015
Daisy Suriadji, Dyah Kanya Wati, I Gusti Lanang Sidiartha, Ida Bagus Suparyatha, I Nyoman Budi
Hartawan
Abstract WHO AnthroPlus software.
Background: Early nutritional screening and Results: From January to December 2015, there
adequate enteral nutrition for critically ill pa- were 477 patients admitted to the PICU and 456
tients, started 24 hours after admission in pedi- were enrolled in this study. Malnutrition was
atric intensive care unit (PICU) are accepted to observed in 72 patients (15.8%) during PICU
improve health outcomes. Malnutrition prior to admission, 56 (17.2%) during discharged, and
admission worsens the prognosis of severely ill only 13 (2.9%) suffered from malnutrition dur-
children and it will lead to a higher mortality, a ing hospitalization. Multivariate analysis
longer length of stay, and a higher health cost. showed that malignancy was the only factor as-
Objective: The main outcome was to investigate sociated with in-hospital malnutrition. Malnu-
the prevalence of hospital malnutrition on ad- trition during admission and discharge were not
mission, discharge, and in-hospital in PICU associated with an increase in the length of hos-
Sanglah Hospital, Bali during 2015. The sec- pital stay. But, in-hospital malnutrition was as-
ondary outcome was to investigate the associa- sociated with longer length of stay (3.2 vs 14.0
tion of cost and hospital malnutrition. days, p<0.001), and was associated with addi-
Methods: A retrospective study was conducted tional cost of Rp 5,500,000.
in PICU Sanglah Hospital, Bali, from January Conclusion: Malnutrition was observed in 72
to December 2015. patients during PICU admission, 56 during dis-
Patients and participants: Children aged 1 charged and only 13 during hospitalization.
month to 12 years with complete medical rec- Hospital malnutrition was associated with addi-
ords. We assessed the prevalence of hospital tional cost of Rp 5,500,000.
malnutrition using WHO Anthro software or
.
Key words: Hospital malnutrition, children, intensive care unit.
Introduction child has fewer calorie reservation and higher rest-
Malnutrition is a broad term that can be used to ing energy expenditure. Therefore, children have
describe any imbalance in nutrition, even during poorer tolerance to fasting than adults, more prone
hospitalization. Malnutrition affects approximately to protein depletion and become malnourished.
50% of hospitalized children and 25-70% of criti- This condition is worsened by growth and devel-
cally ill children. Children are very susceptible to opment, which require high energy expenditures.
nutrition problem, especially when they are ill. In (1,2)
comparison with an adult, a child has lower per- Malnutrition in the ill children is associated with
centage of muscle mass and fat. Consequently, a altered metabolism and increased or decreased me-
. tabolism, and catabolism, and reduced nutrient de-
livery. In critically ill children, the first body re-
From Pediatric Department, Faculty of Medicine, Udayana sponse to the disease is to rapidly decrease meta-
University, Sanglah Hospital, Bali, Indonesia (Daisy Suriadji, bolic rate, accompanied by a decrease in oxygen
Dyah Kanya Wati, I Gusti Lanang Sidiartha, Ida Bagus Supar- consumption, thus reduces energy production. The
yatha, I Nyoman Budi Hartawan).
second phase is a disturbance in hormonal regula-
Address for correspondence: tion marked by hypercatabolism, negative nitrogen
Dr. Dyah Kanya Wati, MD balance, lose weight and muscle mass, and altera-
Pediatric Consultant, Critical Care Medicine tion in carbohydrate metabolism. Malnutrition pri-
Udayana University, Sanglah Hospital
Pulau Nias Street, Denpasar 80114, Indonesia or admission worsens the prognosis in severely ill
Tel: +62-361-246211 children and it will lead to a higher mortality, a
Fax: +62-361-244038 longer length of stay, and a higher health cost.
Email: dyahpediatric@yahoo.com (1,3)
10 Crit Care Shock 2017 Vol. 20 No. 1
Improvement in the evaluation and monitoring of measured by lying in children who were unable to
the nutritional status in the critically ill children stand. The length or height was measured once on
will reduce the prevalence of malnutrition in chil- admission with an assumption that it will not
dren admitted to the intensive care unit. The main changed significantly on discharge.
outcome of this study was to investigate the preva- The weight, height, and age were analyzed based
lence of hospital malnutrition on admission, dis- on the World Health Organization (WHO) guide-
charge, and in-hospital in PICU Sanglah Hospital, lines. The results were weight-for-age, weight-for-
Bali during 2015. The secondary outcome was to height or stature, body mass index (BMI)-for-age,
investigate the association of cost and hospital and weight-for-stature for z-score. Nutritional sta-
malnutrition. tus was classified according to WHO criteria: un-
derweight when weight-for-stature z-scores less
Methods than -2 SD, stunted when stature-for-age z-scores
A retrospective study was conducted in PICU, less than -2 SD, and wasted when weight-for-
Sanglah Hospital, Bali during January to Decem- stature z-scores under -2 SD. (3,6)
ber 2015. We used consecutive sampling methods. The diagnosis used in our analysis was the diagno-
The inclusion criteria were children under 12-year- sis made on discharge. A patient was categorized
old, and had a complete medical record in PICU. into an emergency or a planned admission case,
We collected the patients anthropometry data having a surgery or a medical underlying disease.
from their admissions and on their discharges. The Moreover, the diagnosis was classified into single
exclusion criteria were patients with edema, asci- and multiple diagnoses. We examined whether
tes, hydrocephalus, organomegaly, and history of there was dysphagia, congenital abnormality, ma-
low birth weight. We only used the first data for lignancy, or HIV infection. The in-hospital malnu-
patients who were hospitalized more than once. trition was a defined using Walker and Hendricks
The sample size was calculated by using a single criteria: decreased of weight >2% within a week,
proportion formula with 0.05 and 5% precision. >5% within a month, >7% within 3 months, or
A precedent study conducted in our hospital >10% within 6 months during hospitalization. This
showed the proportion of the in-hospital malnutri- cut-off point was adopted in the absence of specific
tion was 17.5%. (4,5) It led to a minimum estimat- criteria from the literature on this topic. The length
ed sample size of 354 subjects. Our study has ob- of stay (LOS) was the number of days counted
tained permission from Ethic Committee of from the day of admission until the day of dis-
Sanglah Hospital Bali, and the study was conduct- charge.
ed according to the principles of the Declaration of The descriptive data are frequency of sex, age, di-
Helsinki and the ICH Harmonized Tripartite agnosis, LOS, malnutrition at the time of admis-
Guideline for Good Clinical Practice (1996). sion and discharge, and prevalence of in-hospital
The age was determined by the time since birth malnutrition. A bivariate analysis was performed
until the time of admission (in months). The sex using chi-square and independent t-test to assess
was determined based on phenotype appearance the patient length of stay when in-hospital malnu-
and divided to male and female. A low birth trition was present or absent.
weight was defined as birth weight less than 2500 A logistic regression test was used to obtain the
grams. odd ratio (OR) and confident interval 95% (CI
The anthropometric data were collected by pediat- 95%). A p value less than 0.05 was considered as
ric residents who were on duty in the Nutrition and statistical significance. The statistical analysis was
Metabolic Diseases Subdivision. Weight was processed using SPSS 19.0 for Windows.
measured using baby weight scale for children un-
der 2-year-old and a standing scale for children Results
older than 2. Children were weighed in kilograms A total of 477 cases were eligible. Twenty-one
with light underclothes or naked and infants were were excluded because 4 had incomplete data, 6
without diapers. The weight was evaluated twice: had organomegaly, 5 had hydrocephalus, 3 had
once on admission and once on discharge. The edema or ascites, and 3 had low birth weight. Thus,
length was measured in centimeters using a hori- the study enrolled the remaining 456 cases. The
zontal wooden stadiometer for children under 2- actual numbers of children were 426. However, 30
year-old, in a recumbent position. The height was of them were admitted to the hospital and PICU
measured in centimeters using a plastic ruler fixed twice. In consequence, we analyze them as new
on a wall for children above 2-year-old by standing cases, resulting in a total of 456. Out of 456, there
up close to the wall bare feet. The length was were 202 (44.3%) males and 254 (55.7%) females,
. .
Crit Care Shock 2017 Vol. 20 No. 1 11
giving a male-female ratio of 1:1.3. The subject was 2.9%. The incidence of in-hospital malnutri-
characteristics are shown in Table 1. tion at Sanglah Hospital in 2007 was 30.1% in
The subjects were followed from the daily medical children under 5-year-old and in 2009 was 17% in
record, from their admission to PICU until their all children admitted to our hospital. (4,5) If the
discharge from PICU. During the treatment in PICU in-hospital malnutrition is compared to the
PICU, 121 died. The prevalence of malnutrition on total in-hospital malnutrition, the PICU in-hospital
admission was 15.8% (72/456) and 17.2% (56/326) malnutrition was very low. It might be because
on discharge. The prevalence of in-hospital malnu- most children in PICU had acute illnesses. It seems
trition in PICU was 2.9% (13/456). that chronic illness more related with in-hospital
We observed that a longer LOS was an important malnutrition. Our study is similar to other studies
risk factor for in-hospital malnutrition. The data of which found malnutrition during admission was
in-hospital malnutrition (Table 2) revealed that not related to in-hospital malnutrition, but pro-
there were associations between in-hospital malnu- longed hospitalization was associated with in-
trition with multiple diagnoses, malnutrition on hospital malnutrition. (12) Nutritional screening,
admission and discharge, dysphagia, congenital proper nutritional care, and underlying disease
anomaly, malignancy, and HIV infection. The LOS treatment become greatly considered to prevent in-
was longer in children with in-hospital malnutri- hospital nutrition in children.
tion (Table 3). A multivariate analysis showed that Acute in-hospital malnutrition has been widely
malignancy was the only factor associated with in- documented in the literature with its prevalence
hospital malnutrition (Table 4). 20-50%. The results vary depend on the patient
population, variable definition, and the criteria
Discussion used to diagnose. (3) Even though every clinician
Nutrition is an essential aspect of the clinical man- agrees with its importance, there are problems in
agement of children admitted to a hospital. But, defining in-hospital malnutrition. In fact, there is
nutritional support in the critically ill children has not a readily available data can be used as a basis
not been well investigated. It remains a controver- of the cut-off point for the weight loss percentage,
sial issue in pediatric critical care. Critical illness which the term ought to be applied. (13,14) Kac
often alters cellular energy metabolism, even the took the parameter for in-hospital malnutrition as
exact mechanisms are poorly understood. The met- decreased of z-score of weight for age 0.5 SD.
abolic rates in children with critical illness are of- (15) Sidiartha used cut off point 0.5 z-score weight
ten under the predicted basal metabolic rate in the for stature. (4) Rocha and Sidiartha applied the
first week. And, anabolism does not occur. Over- criteria for in-hospital malnutrition as a decrease of
feeding is challenging more than underfeeding in body weight 2% in a week, 5% in a month, or
the first week of illness because the excess protein 10% in 6 months during hospitalization. (5,12)
does not prevent a catabolism but increase the ca- Different results were achieved because of the dif-
tabolism of body protein. (7) ferences in the range of patients age, the criteria of
In-hospital malnutrition has been a worldwide real- in-hospital malnutrition, and also the different pat-
ity and challenge. Its prevalence has been reported tern of underlying disease in PICU.
to be in the range of 6.1% to 51.6%. (7,8) Malnu- LOS was a factor associated with weight loss dur-
trition has a negative impact on the patients out- ing hospitalization. (15,16) Our results also
come by increasing morbidity, mortality, length of showed that in-hospital malnutrition in our PICU
hospital stay, and costs. Despite improvements in was associated with a longer hospital stay, and it
intensive care technology, feeding possibilities, led to high-cost hospitalization. In our hospital,
and increased awareness of the significance of ad- longer LOS is associated with additional cost of Rp
equate nutritional support, the prevalence of acute 5,500,000. In-hospital malnutrition is also associ-
malnutrition remains high in a pediatric intensive ated with the underlying disease and clinical condi-
care unit. (9,10) tion. Our study showed that malignancy was asso-
There are several studies about in-hospital malnu- ciated with in-hospital malnutrition.
trition in children. The incidence of in-hospital In-hospital malnutrition was affected by many fac-
malnutrition in Wahidin Sudirohusodo Hospital, tors. Sermet-Gaudelus and colleagues at Necker-
Makasar, Indonesia was about 8.9%. (11) The in- Enfants Malades Hospital in Paris showed that
cidence of in-hospital malnutrition in Sanglah most predictive factors of weight loss in children
Hospital decreased from 30.1% in 2007 to 17% in during a hospital stay were poor food intake, pain,
2009. (4,5) Our study found the incidence of in- and severity of the disease. The combination of
hospital malnutrition in children admitted to PICU these factors was the best predictor whether a pa-
. .
12 Crit Care Shock 2017 Vol. 20 No. 1
tient was at risk of nutritional depletion. (17) In Conclusion
contrast, exposure to hospital infections and emo- Various definitions were used to describe in-
tional disorders caused by separation from the fam- hospital malnutrition. Studies around in-hospital
ily environment may reduce appetite, and were malnutrition are rarely found due to different cate-
reflected in the decreased dietary intake. gories used. The prevalence of in-hospital malnu-
The limitation of this study was that we only per- trition in a pediatric intensive care unit remains
formed a retrospective examination of the daily substantial. Malnutrition was observed in 72 pa-
nutritional and anthropometry from the medical tients on PICU admission, 56 on discharge and
record. The anthropometry examination was per- only 13 during hospitalization. Hospital malnutri-
formed only on the admission to and on the dis- tion was associated with additional cost of Rp
charge from PICU. Prospective studies, with more 5,500,000.
sensitive tools to assess acute severe illness in
children, are needed.
Crit Care Shock 2017 Vol. 20 No. 1 13
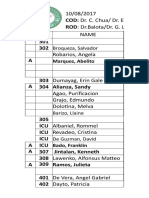
Table 1. Subject characteristics
Characteristics Total=456
n Percentage (%)
Sex
- Male 202 44.3
- Female 254 55.7
Hospital admission type
- Emergency 411 90.0
- Non-emergency 45 10.0
Department
- Medical 347 76.1
- Surgery 109 23.1
Malnutrition on admission 72 15.8
Malnutrition on discharge 56 12.2
Table 2. Bivariate analysis of in-hospital malnutrition and its association with the variables
Variables In-hospital malnutrition
Yes No p
n % n %
Multiple diagnosis Present 13 100 54 12.2 <0.001
Absent 0 0 389 87.8
Malnutrition
- On admission Present 12 92.3 60 13.5 <0.001
Absent 1 7.7 383 86.5
- On discharge Present 12 92.3 13 2.9 <0.001
Absent 1 7.7 430 97.1
Dysphagia Present 10 76.9 40 9.1 <0.001
Absent 3 23.1 403 90.9
Congenital anomaly Present 5 38.5 25 5.6 <0.001
Absent 8 61.5 418 94.4
Malignancy Present 0 0 13 2.9 0.04
Absent 13 100 430 97.1
HIV infection Present 5 38.5 23 5.2 <0.001
Absent 8 61.5 420 94.8
Table 3. Independent sample t-test for in-hospital malnutrition and mean of length of stay
Group n Mean (SD) Mean difference (95% CI) p
In-hospital malnutrition <0.001
- Yes 13 14.000 (1.225) 10.869
- No 443 3.231 (0.663) (10.491-11.247)
14 Crit Care Shock 2017 Vol. 20 No. 1
Table 4. Multivariate analysis of in-hospital malnutrition factors
Factors Coefficient p OR 95% CI
Multiple diagnoses -1.810 0.086 0.164 0.021-1.291
Dysphagia 0.007 0.993 1.007 0.240-4.221
Congenital anomaly 0.009 0.354 1.009 0.990-1.027
Malignancy 0.013 0.011 1.013 1.003-1.023
HIV infection 0.005 0.412 1.005 0.992-1.019
Crit Care Shock 2017 Vol. 20 No. 1 15
References
1. Prieto MB, Cid JL. Malnutrition in the critical- 2008;167:1441-7.
ly ill child: the importance of enteral nutrition. 9. Joosten KF, Hulst JM. Malnutrition in pediat-
Int J Environ Res Public Health 2011;8:4353- ric hospital patients: current issues. Nutrition
66. 2011;27:133-7.
2. Barker LA, Gout BS, Crowe TC. Hospital mal- 10. Correia MI, Campos AC, ELAN Cooperative
nutrition: prevalence, identification, and im- Study. Prevalence of hospital malnutrition in
pact on patients and the healthcare system. Int Latin America: the multicenter ELAN study.
J Environ Res Public Health 2011;8:514-27. Nutrition 2003;19:823-5.
3. Nasar SS, Susanto JC, Lestari ED, Djais J, 11. Juliaty A. Malnutrisi rumah sakit pada bangsal
Prawitasari T. Malnutrisi di Rumah Sakit. In: anak Rumah Sakit Dr. Wahidin Sudirohusodo
Sjarif DR, Lestari ED, Mexitalia M, Nasar SS. Makassar. Sari Pediatri 2013;15:65-8.
Editors. Buku Ajar Nutrisi Pediatrik dan Pe- 12. Rocha GA, Rocha EJ, Martins CV. The effects
nyakit Metabolik. 1st ed. Jakarta: BP IDAI; of hospitalization on the nutritional status of
2011. p. 165-76. children. J Pediatr (Rio J) 2006;82:70-4.
4. Sidiartha IGL. Insidens malnutrisi rawat inap 13. Marginean O, Pitea AM, Voidazan S, Mar-
pada anak balita di Rumah Sakit Umum Pusat ginean C. Prevalence and assessment of mal-
Sanglah Denpasar. Sari Pediatri 2008;9:381-5. nutrition risk among hospitalzed children in
5. Sidiartha IGL. Insidens malnutrisi rumah sakit Romania. J Health Popul Nutr 2014;32:97-102.
pada anak di Rumah Sakit Umum Pusat Sang- 14. Wonoputri N, Djais JT, Rosalina I. Validity of
lah Denpasar. Medicina 2012;43:15-8. nutrtitional screening tools for hospitalized
6. World Health Organization. Training course children. J Nutr Metab 2014;2014:143649.
on child growth assessment, WHO; lecture 15. Kac G, Camacho-Dias P, Silva-Coutinho D,
given 2008. Silveira-Lopes R, Marins VV, Pinheiro AB.
7. Joffe A, Anton N, Lequier L, Vandermeer B, Length of stay is associated with incidence of
Tjosvold L, Larsen B, et al. Nutritional support in-hospital malnutrition in a group of low-
for critically ill children. Cochrane Database income Brazilian children. Salud Publica Mex
Syst Rev 2016;(5):CD005144. 2000;42:407-12.
8. Mokkink LB, van der Lee JH, Grootenhuis 16. UNICEF. The state of the worlds children.
MA, Offringa M, Heymans HS, Dutch Nation- New York, USA: Brodock Press; 2009.
al Consensus Committee Chronic Diseases and 17. Sermet-Gaudelus I, Poisson-Salomon AS, Co-
Health Conditions in Childhood. Defining lomb V, Brusset MC, Mosser F, Berrier F, et
chronic diseases and health conditions in al. Simple pediatric nutritional risk score to
childhood (0-18 years of age): National identify children at risk of malnutrition. Am J
concensus in the Netherlands. Eur J Pediatr Clin Nutr 2000;72:64-70.
.
16 Crit Care Shock 2017 Vol. 20 No. 1
Você também pode gostar
- Telaah Jurnal Diana Nubatonis - 2 LembarDocumento3 páginasTelaah Jurnal Diana Nubatonis - 2 LembarDiana Manu NubatonisAinda não há avaliações
- Nutritional Status of Children in Critical Condition at Admission To Pediatric Intensive Care UnitsDocumento6 páginasNutritional Status of Children in Critical Condition at Admission To Pediatric Intensive Care UnitsAnonymous h0DxuJTAinda não há avaliações
- PYMS TamizajeDocumento6 páginasPYMS TamizajeKevinGallagherAinda não há avaliações
- PYMS Is A Reliable Malnutrition Screening ToolsDocumento8 páginasPYMS Is A Reliable Malnutrition Screening ToolsRika LedyAinda não há avaliações
- Factors Influencing Nutritional Status and Food Consumption Patterns of ChildrenDocumento18 páginasFactors Influencing Nutritional Status and Food Consumption Patterns of ChildrenpopongAinda não há avaliações
- Nutritional Assessment of Children With CHD CompareDocumento9 páginasNutritional Assessment of Children With CHD CompareIntan Robi'ahAinda não há avaliações
- Frequency of Malnutrition Among Children Under 2 Years and Its Relationship With Inadequate Breast Feeding PracticeDocumento3 páginasFrequency of Malnutrition Among Children Under 2 Years and Its Relationship With Inadequate Breast Feeding PracticeAndhika SatriyaAinda não há avaliações
- Maternal Short Stature and Stunting Among Under Two Children in NepalDocumento10 páginasMaternal Short Stature and Stunting Among Under Two Children in NepalvinuthaAinda não há avaliações
- Nej Mo JurnalDocumento11 páginasNej Mo JurnalAnnisa RahmaniAinda não há avaliações
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDocumento5 páginasInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenIvana YunitaAinda não há avaliações
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDocumento5 páginasInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenAnonymous h0DxuJTAinda não há avaliações
- Babies Born To Obese Mothers: What Are The Characteristics and Outcomes?Documento8 páginasBabies Born To Obese Mothers: What Are The Characteristics and Outcomes?IJPHSAinda não há avaliações
- Obstetric Research Journal DayandanteDocumento4 páginasObstetric Research Journal DayandanteKrizelle MesinaAinda não há avaliações
- Ebp Team Assignment Group 10Documento15 páginasEbp Team Assignment Group 10api-621785757Ainda não há avaliações
- Clinical Impact of Prescribed Doses of Nutrients For Patients Exclusively Receiving Parenteral Nutrition in Japanese HospitalsDocumento9 páginasClinical Impact of Prescribed Doses of Nutrients For Patients Exclusively Receiving Parenteral Nutrition in Japanese Hospitalsmarco marcoAinda não há avaliações
- Factors Influencing Malnutrition Among Under Five Children at Kitwe Teaching Hospital, ZambiaDocumento10 páginasFactors Influencing Malnutrition Among Under Five Children at Kitwe Teaching Hospital, ZambiaInternational Journal of Current Innovations in Advanced Research100% (1)
- Optimal Timing For Introducing Enteral Nutrition in The Neonatal Intensive Care UnitDocumento8 páginasOptimal Timing For Introducing Enteral Nutrition in The Neonatal Intensive Care UnitAnonymous 1EQutBAinda não há avaliações
- Shu Hwa Ong, Winnie Siew Swee Chee, L. Mageswary Lapchmanan, Shan Ni Ong, Zhi Chin Lua, and Jowynna Xia-Ni YeoDocumento7 páginasShu Hwa Ong, Winnie Siew Swee Chee, L. Mageswary Lapchmanan, Shan Ni Ong, Zhi Chin Lua, and Jowynna Xia-Ni YeoNurlyanti RustamAinda não há avaliações
- Skrining GiziDocumento7 páginasSkrining GiziifaAinda não há avaliações
- 1246 7206 1 PBDocumento6 páginas1246 7206 1 PBNensy AnggrainyAinda não há avaliações
- Nutrients 09 00221 v2Documento11 páginasNutrients 09 00221 v2Firman FajriAinda não há avaliações
- Improved Nutrition Delivery and Nutrition Status in Critically Ill Children With Heart DiseaseDocumento9 páginasImproved Nutrition Delivery and Nutrition Status in Critically Ill Children With Heart DiseasedaindesAinda não há avaliações
- Assessment of Nutritional Status Based On Strongkids Tool in Iranian Hospitalized ChildrenDocumento7 páginasAssessment of Nutritional Status Based On Strongkids Tool in Iranian Hospitalized Childrenfarah febriyantiAinda não há avaliações
- Cardenas 2021 Nday 2 JPEN Jpen.2085Documento10 páginasCardenas 2021 Nday 2 JPEN Jpen.2085CamilaAinda não há avaliações
- Nutritional Status of Children Admitted To The Pediatric Department at A Tertiary Care Hospital, Sana'a, YemenDocumento6 páginasNutritional Status of Children Admitted To The Pediatric Department at A Tertiary Care Hospital, Sana'a, YemenInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Jurnal StrongKIDSDocumento6 páginasJurnal StrongKIDSUmmi ToibahAinda não há avaliações
- Malnutrition in Hospitalized ChildrenDocumento5 páginasMalnutrition in Hospitalized ChildrenPutri Wulan SukmawatiAinda não há avaliações
- Anthropometry Assessment in Children With Disease Related MalnutritionDocumento10 páginasAnthropometry Assessment in Children With Disease Related Malnutritionberlian29031992Ainda não há avaliações
- Growth in HIV-infected Children On Long-Term Antiretroviral TherapyDocumento11 páginasGrowth in HIV-infected Children On Long-Term Antiretroviral TherapyChristian Alexis Loza CorderoAinda não há avaliações
- Espghan 2015 - Abstracts JPGN FinalDocumento963 páginasEspghan 2015 - Abstracts JPGN FinalAdriana RockerAinda não há avaliações
- Nutrition Status and Risk Factors Associated With Length of Hospital Stay For Surgical PatientsDocumento8 páginasNutrition Status and Risk Factors Associated With Length of Hospital Stay For Surgical PatientsFarida MufidatiAinda não há avaliações
- Effectiveness of Nutritional Supplementation During The - 2022 - The Lancet RegDocumento11 páginasEffectiveness of Nutritional Supplementation During The - 2022 - The Lancet RegCawee CawAinda não há avaliações
- EJCM - Volume 36 - Issue 1 - Pages 45-60-1Documento16 páginasEJCM - Volume 36 - Issue 1 - Pages 45-60-1Yaumil FauziahAinda não há avaliações
- Estreñimiento y TeaDocumento9 páginasEstreñimiento y TeaElena Martin LopezAinda não há avaliações
- Comparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsDocumento5 páginasComparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsGita TrisnawatiAinda não há avaliações
- BLW 2018 DoganDocumento25 páginasBLW 2018 DoganGenesis VelizAinda não há avaliações
- STAMP (Kids)Documento8 páginasSTAMP (Kids)Rika LedyAinda não há avaliações
- Nutritional Intervention ArticleDocumento6 páginasNutritional Intervention Articleanil agarwalAinda não há avaliações
- Infant Feeding and Feeding Transitions During The First Year of LifeDocumento9 páginasInfant Feeding and Feeding Transitions During The First Year of LifeVinitha DsouzaAinda não há avaliações
- Lipid Based Suppl Vs CSB Mod Underwt Malawi 2010Documento14 páginasLipid Based Suppl Vs CSB Mod Underwt Malawi 2010Fiqah KasmiAinda não há avaliações
- Perioperative Nutritional Prehabilitation in Malnourished Children With Congenital Heart Disease A Randomized ControlleDocumento29 páginasPerioperative Nutritional Prehabilitation in Malnourished Children With Congenital Heart Disease A Randomized ControlleRahmania InendaAinda não há avaliações
- Effects of A Feeding Intervention in Patients With Alzheimer's DiseaseDocumento9 páginasEffects of A Feeding Intervention in Patients With Alzheimer's DiseaseDanielly Danino BasilioAinda não há avaliações
- Diarrhea, Dehydration, and The Associated Mortality in Children With Complicated Severe Acute Malnutrition: A Prospective Cohort Study in UgandaDocumento11 páginasDiarrhea, Dehydration, and The Associated Mortality in Children With Complicated Severe Acute Malnutrition: A Prospective Cohort Study in Ugandasalma romnalia ashshofaAinda não há avaliações
- Comparison of Malnutrition and Malnutrition Screening Tools in Pediatric Oncology Patients A Cross-Sectional StudyDocumento5 páginasComparison of Malnutrition and Malnutrition Screening Tools in Pediatric Oncology Patients A Cross-Sectional StudySebastian MarinAinda não há avaliações
- Validitas SNAQDocumento8 páginasValiditas SNAQDanang Adit KuranaAinda não há avaliações
- Under-Five Protein Energy Malnutrition Admitted at The University of Nigeria Teaching Hospital, Enugu: A 10 Year Retrospective ReviewDocumento7 páginasUnder-Five Protein Energy Malnutrition Admitted at The University of Nigeria Teaching Hospital, Enugu: A 10 Year Retrospective ReviewhfathiardiAinda não há avaliações
- The Use of Home-Based Therapy With Ready-toUse Therapeutic Food To Treat Malnutrition in A Rural Area During A Food CrisisDocumento4 páginasThe Use of Home-Based Therapy With Ready-toUse Therapeutic Food To Treat Malnutrition in A Rural Area During A Food Crisismirfanjee89Ainda não há avaliações
- 1 PB PDFDocumento12 páginas1 PB PDFMegayana Yessy MarettaAinda não há avaliações
- Belin2021 NutritionalScreeningDocumento11 páginasBelin2021 NutritionalScreeningcaparrosolorena5Ainda não há avaliações
- Article Assignment 3 - Breanna LaliberteDocumento3 páginasArticle Assignment 3 - Breanna Laliberteapi-240098584Ainda não há avaliações
- Jurnal Hiperemesis GravidarumDocumento6 páginasJurnal Hiperemesis GravidarumArief Tirtana PutraAinda não há avaliações
- Nutrients 09 00520Documento9 páginasNutrients 09 00520husynAinda não há avaliações
- 28 - MatthewDocumento6 páginas28 - MatthewRosa PerezAinda não há avaliações
- Antibiotics As Part of The Management of Severe Acute MalnutritionDocumento13 páginasAntibiotics As Part of The Management of Severe Acute Malnutritionmarisa armyAinda não há avaliações
- CHRONIC DiseaseDocumento6 páginasCHRONIC Diseaseberlian29031992Ainda não há avaliações
- Nutr Clin Pract 2014 Asfaw 192 200Documento10 páginasNutr Clin Pract 2014 Asfaw 192 200Iván OsunaAinda não há avaliações
- Pemulihan Gizi Buruk Rawat Jalan Dapat Memperbaiki Asupan Energi Dan Status Gizi Pada Anak Usia Di Bawah Tiga TahunDocumento7 páginasPemulihan Gizi Buruk Rawat Jalan Dapat Memperbaiki Asupan Energi Dan Status Gizi Pada Anak Usia Di Bawah Tiga TahunMaidah UslahAinda não há avaliações
- Nutrition in Surgical Pediatric Patients - 2Documento11 páginasNutrition in Surgical Pediatric Patients - 2Mireia PerezAinda não há avaliações
- Angka Insiden Dan Faktor Risiko Malnutrisi Rumah Sakit Pada Anak Rawat Inap Di RSUP Sanglah, Bali, IndonesiaDocumento7 páginasAngka Insiden Dan Faktor Risiko Malnutrisi Rumah Sakit Pada Anak Rawat Inap Di RSUP Sanglah, Bali, IndonesiaElsa rosantiAinda não há avaliações
- 1 HISTORY 6 OctDocumento180 páginas1 HISTORY 6 OctInez Ann Marie TumbelakaAinda não há avaliações
- Correlation of Clinical Examination and Ultrasonogram With Histopathology in Predicting The Metastatic Axillary Lymph Nodes in Breast CancerDocumento6 páginasCorrelation of Clinical Examination and Ultrasonogram With Histopathology in Predicting The Metastatic Axillary Lymph Nodes in Breast CancerInez Ann Marie TumbelakaAinda não há avaliações
- 2011 Hospital MalnutritionDocumento14 páginas2011 Hospital MalnutritiontopiqAinda não há avaliações
- Nutritional Screening and Guidelines For Managing The Child With Faltering GrowthDocumento3 páginasNutritional Screening and Guidelines For Managing The Child With Faltering GrowthInez Ann Marie TumbelakaAinda não há avaliações
- Lipid Modification: Cardiovascular Risk Assessment and The Modification of Blood Lipids For The Primary and Secondary Prevention of Cardiovascular DiseaseDocumento55 páginasLipid Modification: Cardiovascular Risk Assessment and The Modification of Blood Lipids For The Primary and Secondary Prevention of Cardiovascular DiseaseInez Ann Marie TumbelakaAinda não há avaliações
- Abnormal Uterine Bleeding 7-17-16 HengstebeckDocumento54 páginasAbnormal Uterine Bleeding 7-17-16 HengstebeckInez Ann Marie TumbelakaAinda não há avaliações
- Hypokalemia - A Clinical UpdateDocumento12 páginasHypokalemia - A Clinical UpdateRushi PatelAinda não há avaliações
- KetamineDocumento27 páginasKetaminesamfarmer3330% (2)
- Deworming: Fit For SchoolDocumento9 páginasDeworming: Fit For SchoolLark SantiagoAinda não há avaliações
- Oxford: ReferenceDocumento846 páginasOxford: ReferenceNMC NEPHROLOGY100% (1)
- Death Anxiety Care PlanDocumento4 páginasDeath Anxiety Care PlanAaLona Robinson86% (7)
- Palicka Simpozion Management RiscDocumento60 páginasPalicka Simpozion Management Risccornelialautarescu6411Ainda não há avaliações
- Drug Education in The PhilippinesDocumento32 páginasDrug Education in The PhilippinesTrixie Ann MenesesAinda não há avaliações
- Bacterial MeningitisDocumento2 páginasBacterial MeningitisSpideyPacerAinda não há avaliações
- PRISMA 2009 ChecklistDocumento7 páginasPRISMA 2009 ChecklistRezky PutriAinda não há avaliações
- Census FormatDocumento35 páginasCensus Formatkolintang1Ainda não há avaliações
- Soal Prof. BalaDocumento3 páginasSoal Prof. BalaronnyAinda não há avaliações
- Lyrica - Prescribing InfoDocumento42 páginasLyrica - Prescribing InfoPoojaAinda não há avaliações
- BodyBallancer Lipo Brochure PDFDocumento2 páginasBodyBallancer Lipo Brochure PDFRoss Gale100% (1)
- Cholecystitis Nursing Care PlanDocumento4 páginasCholecystitis Nursing Care PlanMDCITY83% (6)
- Ciesluk Meagan Cover LetterDocumento1 páginaCiesluk Meagan Cover Letterapi-508459908Ainda não há avaliações
- Gavage Feeding RepDocumento6 páginasGavage Feeding RepEon Provido AlfaroAinda não há avaliações
- ESR Microsed PermaiDocumento20 páginasESR Microsed PermaiHishamudin RaisAinda não há avaliações
- Effect of Iron Containing Supplements On Rats DenDocumento6 páginasEffect of Iron Containing Supplements On Rats Dendhea hutabaratAinda não há avaliações
- Buku Urology 20190902 A5Documento20 páginasBuku Urology 20190902 A5Magdalena Oktavia KristantiAinda não há avaliações
- Hand Burns: Karen J. Kowalske, MD, David G. Greenhalgh, MD, Scott R. Ward, PHD, PTDocumento4 páginasHand Burns: Karen J. Kowalske, MD, David G. Greenhalgh, MD, Scott R. Ward, PHD, PTsantizptAinda não há avaliações
- Goldberg 2012Documento8 páginasGoldberg 2012Carlos Luque GAinda não há avaliações
- 14-Antiameobic Antifungal 2021Documento22 páginas14-Antiameobic Antifungal 2021Amr SalemAinda não há avaliações
- Primary Review: Psoas Abscess: Case of The LiteratureDocumento3 páginasPrimary Review: Psoas Abscess: Case of The LiteratureDung Tran HoangAinda não há avaliações
- DRUGS (Topotecan)Documento2 páginasDRUGS (Topotecan)BARRISTERFLOWERSEAURCHIN6Ainda não há avaliações
- Audit On BFHIDocumento40 páginasAudit On BFHIYoung MilkAinda não há avaliações
- Fluid, Electrolytes, Acid Base BalanceDocumento18 páginasFluid, Electrolytes, Acid Base Balanceashdmb217100% (5)
- Myasis, Tungiasis and LoiasisDocumento34 páginasMyasis, Tungiasis and LoiasisMateo LópezAinda não há avaliações
- Pentacam GuidelineDocumento43 páginasPentacam GuidelineEvelyn SepulvedaAinda não há avaliações
- Anaphylactic Death FinalDocumento73 páginasAnaphylactic Death Finalkhaled eissaAinda não há avaliações
- Government College of Nursing JodhpurDocumento7 páginasGovernment College of Nursing JodhpurNaresh JeengarAinda não há avaliações