Escolar Documentos
Profissional Documentos
Cultura Documentos
14 Iajps14062017 PDF
Enviado por
Baru Chandrasekhar RaoTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
14 Iajps14062017 PDF
Enviado por
Baru Chandrasekhar RaoDireitos autorais:
Formatos disponíveis
IAJPS 2017, 4 (06), 1511-1519 Bassam R.
Almutairi et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN: 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
http://doi.org/10.5281/zenodo.815368
Available online at: http://www.iajps.com Research Article
ASSESSMENT OF THE PREVALENCE OF MULTI-DRUG RESISTANCE
ISOLATES OF KLEBSIELLA PNEUMONIAE AMONG THE PATIENTS
AT NORTHERN AREA ARMED FORCES HOSPITAL (NAAFH) OF THE
EASTERN REGION OF SAUDI ARABIA
Bassam R. Almutairi*1, Mohd. Imran2, Emad Obaid3, Monadil H. M. Ali3, Abdulkhaliq J.
Alsalman3
1
Faculty of Pharmacy, Northern Border University, Rafha - 91911, P.O. BOX 840, Kingdom of Saudi
Arabia.
2
Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Northern Border University, Rafha -
91911, P.O. BOX 840, Kingdom of Saudi Arabia.
3
Department of Clinical Pharmacy, Faculty of Pharmacy, Northern Border University, Rafha - 91911,
P.O. BOX 840, Kingdom of Saudi Arabia.
Abstract:
The objective of this study was to assess the prevalence of multi-drug resistance isolates of Klebsiella pneumoniae among the
patients at Northern Area Armed Forces Hospital (NAAFH) of the Eastern region of Saudi Arabia. This retrospective, chart
review observational study was conducted from February 1, 2016 to February 29, 2016 at Northern Area Armed Forces Hospital
(NAAFH), a 330-bed community general hospital located in the Eastern region of Saudi Arabia. A total of 870 isolates were
identified in 298 patients (3 isolates per patient involving multiple sites). It was observed that the risk of females being infected or
colonized with K. pneumoniae was higher than males; the K. pneumoniae was more frequently encountered in hospitalized
patient compared to outpatients; a greater number of isolates were obtained from medical service; and the K. pneumoniae was
more likely to be isolated from the genitourinary system. Prevalence of multi-drug resistance of K. pneumoniae to antibacterial
agents showed that 41% isolates were resistant to third generation cephalosporin primarily due to production of ESBLs, but this
was considered statistically insignificant (RR 1.18; 95% CI, 0.96 to 1.47; p = 0.131). The K. pneumoniae producing
carbapenemase (KPC) were significantly prominent in this series (RR 0.32; 95%CI, 0.23 to 0.43; p < 0.001). The rapid growth
of the K. pneumoniae species that are resistant to carbapenem, a class of drugs considered the last-line of defense, is a matter of
concern.
Kew Words: Prevalence, multi-drug resistance isolates, Klebsiella pneumoniae, Saudi Arabia.
Corresponding author:
QR code
Bassam R. Almutairi,
Faculty of Pharmacy,
Northern Border University, Rafha - 91911, P.O. BOX 840,
Kingdom of Saudi Arabia.
ph.basam@gmail.com.
Mobile Number: +966554399634
Please cite this article in press as Bassam R. Almutairi et al, Assessment of The Prevalence of Multi-Drug
Resistance Isolates of Klebsiella Pneumoniae Among The Patients at Northern Area Armed Forces Hospital
(NAAFH) of The Eastern Region of Saudi Arabia, Indo Am. J. P. Sci, 2017; 4(06).
www.iajps.com Page 1511
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
INTRODUCTION:
Infections caused by Klebsiella pneumoniae have has a pharmacy which is limited to a primary health
become endemic in health care systems [1]. This care formulary.
organism can be found as normal flora in the mouth,
skin, and intestinal tract, where it initially does not Data Collection
cause disease [2]. Although found in these organ Data were collected on all patients within NAAFH
systems as normal flora, K. pneumoniae can progress (inpatient and outpatient) in whom K. pneumoniae
into severe bacterial infections leading to pneumonia, was isolated by the microbiology laboratory. This
bloodstream infections, wound infections, urinary study was approved by Northern Area Armed Forces
tract infections, and meningitis. Patients who require Hospital Ethics Committee (February 16, 2016).
equipment such as catheters or ventilators are at high Clinical patient information was collected from the
risk for infections. Also, a patient administered a patients antibiogram, missing patient data was
course of broad-spectrum antibiotic treatment is at an accessed through the computerized physician order
even higher risk due to the disruption of the normal entry (CPOE) by the investigator. Data collected
flora of the bacteria in the body, deeming it more included demographic information, patient location,
susceptible to pathogens [2]. The principal type of service or sub-specialty where applicable,
pathogenic reservoirs for transmission of Klebsiella anatomical site of the isolate. Patients treated with at
are the gastrointestinal tract and the hands of hospital least one of the following were analyzed; cefazolin,
personnel. Because of their ability to spread rapidly cefuroxime, ceftriaxone, cefotaxime, ceftazidime,
in the hospital environment, these bacteria tend to imipenem-cilastatin, piperacillin-tazobactam,
cause nosocomial outbreaks [3]. Hospital outbreaks ciprofloxacin, levofloxacin, cefepime, amikacin,
of multidrug-resistant Klebsiella spp., especially gentamicin, tobramycin and
those in neonatal wards, are often caused by new trimethoprim/sulfamethoxazole (TMP/SMX) in
types of strains, the so-called extended-spectrum- whom K. pneumoniae was confirmed using the CDC
beta-lactamase (ESBL) producers [4]. What is of definitions [7] for infection. The initial K.
major concern clinically is the current onslaught of pneumoniae isolate was considered the baseline
multi-drug resistant K. pneumoniae species that have isolate. Baseline resistance was defined as resistance
also become resistant to carbapenems [1, 3-6]. of baseline isolate to any of the study antibacterials
Reports from elsewhere highlight the challenges and multi-drug resistance was defined as resistance to
faced by infectious disease specialists and healthcare any 3 of these antibacterials. Microbiologic outcomes
systems management of treating these isolates owing were categorized as susceptible, baseline
to the limited formulary antibacterial armament [1-6]. resistance, multi-drug resistant, extended-
To the best of our knowledge studies related to the spectrum beta-lactamases (ESBL) producers and
assessment of the prevalence of multi-drug resistance carbapenem-resistance enterobacteriaceae (CRE).
isolates of Klebsiella pneumoniae among the patients These outcomes were compared between services,
in some regions of Saudi Arabia has not been carried between community-acquired versus hospital-
out. Accordingly, the objective of this study was to acquired (nosocomial) infection.
assess the prevalence of multi-drug resistance isolates
of Klebsiella pneumoniae among the visitor at The minimal inhibitory concentrations used to
Northern Area Armed Forces Hospital (NAAFH) of determine susceptibility thresholds for the different
the Eastern region of Saudi Arabia. antibacterials aimed at K. pneumoniae were,
according to the NAAFH guidelines ( 8 for
METHODS: cefazolin, 4 for cefuroxime 8 g/mL for
This retrospective, chart review observational study piperacillin-tazobactam, < 8 g/mL for cefepime, < 1
was conducted from February 1, 2016 to February g/mL for ceftazidime, 4 for ceftriaxone, 2 for
29, 2016 at Northern Area Armed Forces Hospital cefotaxime, < 4g/mL for imipenem-cilastatin, 2
(NAAFH), a 330-bed community general hospital g/mL for levofloxacin, 1g/mL for ciprofloxacin,
located in the Eastern region of Saudi Arabia. The < 1 for gentamicin, TMP/SMX 0.5/9.5 and < 2 for
hospital has 40 intensive care unit beds (12 adult, 21 tobramycin). Isolates with intermediate susceptibility
neonatal and 6 pediatric) with approximately 4,716 were considered resistant. At NAAFH, MICs for
admissions per year. In addition, the hospital operates meropenem and aztreonam are not routinely
about 8 peripheral health care centers (clinics) that performed. All collected data were entered into an
offer primary care (ambulatory) services to the Excel spreadsheet (Microsft Corporation, Redmond.
community. The outpatient and central pharmacy are Wash.).
located in the hospital proper adjacent to the medical
laboratory (central pharmacy). Each peripheral clinic
www.iajps.com Page 1512
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
Data analysis genitourinary system (46%) followed by the
Descriptive statistics were used to summarize data. respiratory (25%), others (25%), and wound (18%)
Demographic data and all other categorical variables and less frequently encountered were K. pneumoniae
were analyzed using the 2 statistic and Fischers isolated from the bloodstream (4%). These findings
exact test between genders. Continuous variables were found to be statistically insignificant (p =
such as age were analyzed using Student t-test or 0.878).
Mann-Whitney U-test for nonparametric data.
Comparisons between the frequency of isolating K. Prevalence of multi-drug resistance of K. pneumoniae
pneumoniae in hospitalized patients (nosocomial) (Table 1) to anti-bacterial showed that 41% isolates
versus isolates from the community as well as the were resistant to third generation cephalosporin
frequency of susceptible isolates compared to primarily due to production of ESBLs, but this was
resistant ones were quantified using the relative risk. considered statistically insignificant (RR 1.18; 95%
Multivariate regression was performed to establish CI, 0.96 to 1.47; p = 0.131). However, resistance of
correlations between variables and the Pearsons K. pneumoniae to cephalosporin as a class (including
product-moment correlation coefficient (r2) was used. 1st and 2nd generation cephaolosporin) was
Alternatively, either Kendalls tau correlation or statistically significant (RR = 1.27; 95% CI, 1.14
Spearman rho correlation was used for ordinal to1.41; p < 0.001). The Klebsiella pneumoniae
variables where applicable. Multiple regression producing carbapenemase (KPC) were significantly
statistics were employed in the case of multiple prominent in this series (RR 0.32; 95% CI, 0.23 to
variances. Data were analyzed using Stata (Version 0.43; p < 0.001). All other resistance patterns of K.
12; StataCorp, College Station, TX, USA) statistical pneumoniae to formulary antibacterial were
software. Statistical significance was defined with a p statistically non-significant.
value of less than 0.05.
DISCUSSION:
RESULTS: The prevalence of multi-drug resistant K.
A total of 870 isolates of K. pneumoniae were pneumoniae due to ESBL production was identified
recovered from 298 patients (average of 2.9 isolates in 121 (41%) patients in this study. ESBL producing
per patient from multiple sites). The overall average K. pneumoniae poses a unique challenge in the
age of our study population was 50.3928.07. treatment and eradication of this organism given
Females, on average, were significantly younger than limited formulary options available. Currently, to
their male counterparts (46.08 28.23 vs 57.76 treat ESBL-producing K. pneumoniae clinicians have
27.47; 95%CI, -18.23 to -5.1; p = 0.0006). Females to use carbapenem. Carbapenem are stable in the
were significantly more likely to be infected or presence of hydrolytic effects of ESBLs, which may
colonized with K. pneumoniae than males (63% vs explain the consistent finding that 98% of ESBL-
37%; 95% CI, 0.576 to 0.686). The distribution of K. producing organisms retain susceptibility to either
pneumoniae by age range indicates that most of the imipenem or meropenem [11-13]. These reports are
isolates were recovered from the 71-80 age range consistent with our findings in that in the current
(22%, 66). The 31-40 age range was next with 45 study, all ESBL-producing isolates were susceptible
isolates (15%) followed by the 21-30 (13%), 0-10 to imipenem or meropenem, but 38% were resistant
(12%) and the 41-50 (10%) age ranges. In the 51-60 to piperacillin-tazobactam, 31% were resistant to
(8%), 61-70 (6%) age ranges, K. pneumoniae was not aminoglycosides, and 37% were resistant to
as common as the foregoing age ranges. K. ciprofloxacin (Figure 2). Other reports have
pneumoniae was isolated with less frequency in the suggested that the inferior outcome associated with
81-90 (6%), 91-100 (3%) and in the age range greater apparently active cephalosporin and -lactam / -
than 100 (4%) (Figure 1). lactamase inhibitors, compared with that for other
antibiotic classes, could be explained by the
K. pneumoniae was more frequently encountered in inoculum effect [14]. This effect (in which MICs of a
hospitalized patients (nosocomial) compared to drug increase up to 100-fold in the presence of
patients visiting outpatient clinics (80% vs 20%; 95% increased inocula) is consistently observed with
CI, 0.156 to 0.247). Of the patients who acquired K. cefotaxime, ceftriaxone, and cefepime against ESBL-
pneumoniae from the hospital (nosocomial), a greater producing organisms [14]. An inoculum effect is
number were isolated from the medical service (44%) least frequently observed with carbapenem;
followed very closely by intensive care units (41%) piperacillin-tazobactam has an inoculum effect
[adult intensive care unit (ICU) 74%, pediatric (ICU) intermediate between those of carbapenem and
19% and neonatal (ICU) 7%] (Figure 2). The K. cephalosporin [14]. Apart from the inoculum effect,
pneumoniae was more likely to be isolated from the an alternative explanation for failure of -lactam
www.iajps.com Page 1513
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
antibiotics is failure to achieve pharmacodynamic as the inoculum increases. The relatively poor
targets. Quinolones are not prone to substantially outcome for patients treated with quinolones in this
increase their MICs against ESBL-producing strains study is possibly the result of under dosing [15].
70 66
60
50 45
40 37 38
30 29
23
20 18 19
8 11
10
4
0
0-10 11-20 21-30 31-40 41-50 51-60 61-70 71-80 81-90 91-100 >100
Fig 1: Prevalence of K. pneumoniae by age range
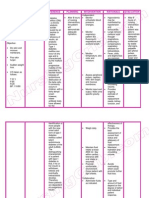
Table 1: Demographic, clinical and microbiological data
Community
Nosocomial -acquired
Parameter (N = 238) (N = 60) RR 95% CI p-Value
Age 55.3 29.1 31.1 13.7 -29 to -19 <0.001
Female, n (%) 141 (75%) 47 (25%) 0.76 0.64 to 0.90 = 0.005
Site of isolation
Blood, n (%) 12(4%) 0
Genitourinary, n (%) 93 (39%) 43 (72%) 0.55 0.44 to 0.68 =
0.000006
Respiratory, n (%) 74(31%) 0
Skin and skin structure infection, n (%) 43(18%) 10 (17%) 1.08 0.58 to 2.03 = 0.82
Other*, n (%) 16(7%) 7 (12%) 0.58 0.25 to 1.34 = 0.22
Intensity of culturing (susceptibility patterns)
Susceptible Resistant N,
Antibiotic Class N, (%) (%) RR 95% CI p-Value
Cephalosporin, n (%) 516 (58) 378 (42) 1.27 1.14 to1.41 0.001
1st generation 168 (56.38) 130 (43.62) 1.34 1.09 to 1.66 0.008
2nd generation 171 (57.38) 127 (42.62) 1.28 1.04 to 1.60 0.023
3rd generation 177 (59.40) 121 (40.60) 1.18 0.96 to 1.47 0.131
(ESBLs)
Aminoglycoside, n (%) 194 (65.10) 104 (34.90) 0.93 0.74 to 1.16 0.507
Quinilone, n (%) 189 (63.42) 109 (36.58) 0.10 0.80 to 1.24 0.984
Carbapenem, n (%) 252 (84.56) 46 (15.44) 0.32 0.23 to 0.43 <0.001
(CRE)
Piperacillin/tazobactam, n (%) 184 (61.74) 114 (38.26) 1.07 0.87 to 1.33 0.536
Sulfamethoxazole/trimethoprim, n (%) 178 (59.73) 120 (40.27) 1.17 0.94 to 1.45 0.167
RR = relative risk or risk ratio. CI =confidence interval; n = number of patients.
www.iajps.com Page 1514
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
Fig 2: Susceptibility of K. pneumoniae to Antibiotic classes
The increase in ESBL-producing Klebsiella were recorded at 41% in our report compared to 91%
pneumoniae can be attributable to the extensive use in the 2006-2011 surveillance report, a 50% increase
of third-generation cephalosporin in this study. (Figure 2). Our results correlate with findings from
Reports from elsewhere state that extended the United States where the proportion of K.
spectrum -lactamase enzymes were first described pneumoniae strains resistant to ceftazidime increased
in K. pneumonia and Serratia marcescens isolates in from 1.5% in 1987 to 3.6% in 1991, and by 1993 as
1983 in Europe [16] and in K. pneumoniae and many as 20% of the strains were resistant to
Escherichia coli isolates in 1989 in the United States ceftazidime in some teaching hospitals [18,19]. Of
[17]. Since then, there has been a marked increase in 824 K. pneumoniae strains isolated from 15 hospitals
the incidence of bacteria that produce ESBL in New York City during 1999, 34% expressed ESBL
enzymes. There is strong agreement between the enzymes [20].
ESBL-producing K. pneumoniae data in our report
compared to other reports elsewhere in that ESBLs
www.iajps.com Page 1515
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
% Extended spectrum -lactamases 120
100
r2 = 0.79
80
60
40 Proportion antibiotic
20 use
Fig 3: Proportion of 3rd generation use versus ESBL-producing
There was a strong correlation (r 2 = 0.79) between increases dramatically among hospitalized patients,
the proportion of third generation cephalosporin used as colonization rates increase in direct proportion to
and the production of ESBLs (Figure 3). the length of stay [23] (Figure 4).
Epidemiological studies suggest that the increasingly
widespread use of third-generation cephalosporin is a Outbreaks of ESBL-producing organisms have been
major risk factor that has contributed to the described. Asymptomatic patients colonized with
emergence of ESBL-producing K. pneumoniae [21- ESBL-producing K. pneumoniae can serve as
23]. Several additional risk factors for colonization reservoirs for this pathogen with subsequent patient-
and infection with ESBL-producing organisms (not to-patient spread via the hands of health care
included in our report) have been reported and workers. In addition, contaminated patient-care items
include: arterial and central venous catheterization, and artificial fingernails worn by health care workers
gastrointestinal tract colonization with ESBL- have been implicated in transmission [24-27]. Most
producing organisms, prolonged length of stay in an studies have demonstrated a poor adherence to
intensive-care unit, low birth weight in preterm infection control policies as an important factor.
infants, prior antibiotic use, and mechanical Outbreaks of ESBL-producing K. pneumoniae in
ventilation [20-22]. Furthermore, there is strong NICUs have been notable for high attack rates and
agreement between our findings and reports from large numbers of colonized infants [28]. The
elsewhere [23] in that patients in the long-term unit neonates at greatest risk for colonization are those
(medical service) were identified as mostly affected with a longer length of stay, a lower estimated
(44%) due to increased length of stay as well as gestational age and/or a lower birth weight [23].
patients in the ICU (41%). Carriage of this organism
maternity
pediatrics
surgery
4% 3% 8%
medicine
44%
Intensive
care
41%
Fig 4: Isolation of nosocomial K. pneumoniae by service
www.iajps.com Page 1516
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
Table 2: Relationship between carbapenem utilization and susceptibility
Year % susceptible Quantity used 95%CI (quantity used)
Lower Upper
2007 98 9271 0.0720 0.0773
2008 99 2634 0.0932 0.0994
2009 99 3402 0.1384 0.1457
2010 100 5021 0.1199 0.1268
2011 100 4358 0.1729 0.1809
2014 95 6251 0.1214 0.1282
2015 85 4410 0.2577 0.2669
Prescribing carbapenem due to multi-drug resistance, CRE is important for several reasons. First, invasive
including ESBL production (Table 2) has resulted in infections (e.g., bloodstream infections) with CRE
selection pressure that favors resistance to are associated with mortality rates exceeding 40%
carbapenem through the production of [31, 33]; this is significantly higher than mortality
carbapenemase [29,30] resulting in carbapenem- rates observed for carbapenem-susceptible
resistant K. pneumoniae (CRKP) [29] through Enterobacteriaceae. Of note, because the majority of
production of what is known as KPC (Klebsiella positive cultures were from urine, overall in-hospital
pneumoniae carbapenemase)-type -lactamase mortality rates associated with positive cultures were
[29,30] which fall under what is currently known as lower in the EIP CRE surveillance (4%) [33].
carbapenem resistant Enterobacteriaceae (CRE) [31]. Second, carbapenem-resistant strains frequently
In this report, there was a weak inverse correlation (r 2 possess additional resistance mechanisms that render
= -0.01123) between carbapenem utilization and the them resistant to most available antimicrobials; pan-
emergence of carbapenem resistance (Table 2). When resistant CRE has been reported [34]. Further, novel
comparing K. pneumoniae resistance to carbapenem antimicrobials for multidrug-resistant gram-negative
between 2015 (15%) and 2007 2011 report (2%), it bacilli are in early stages of development and not
can be seen that there has been an increase in likely to be available soon [35]. Third, CRE can
resistance no carbapenem by isolates of K. spread rapidly in health care settings [36, 3]. Fourth,
pneumoniae [10]. Enterobacteriaceae is a common cause of community
infections, and CRE have the potential to move from
Other reports state that although CRE remain their current niche among health-careexposed
relatively uncommon in most acute-care hospitals in patients into the community [37, 38]. The K.
the United States, they have become an increasingly pneumoniae was significantly isolated from
recognized cause of infection during the past decade, hospitalized patients (80% vs 20%, p < 0.001).
especially among Klebsiella, likely because of the
emergence of carbapenemase-producing strains [32, CONCLUSION:
33]. In 2012, the number of facilities reporting CRE Resistance of K. pneumoniae to available formulary
as a cause of infection was small, and spread of these antibiotics is concerning in view of the fact that no
organisms appears to be uneven both regionally and new antibiotics are in the pipeline. What is of more
among facilities within regions. Fewer than 5% of concern to infectious disease specialists and
short-stay acute-care hospitals reported CRE from healthcare systems is the rapid growth of K.
health-careassociated infections in the first half of pneumoniae species that are resistant to carbapenem,
2012 [32]; CRE more often were reported from a class of drugs considered the last-line of defense.
LTACHs. Data from population-based surveillance Our findings are supported by reports in another
suggest most CRE clinical isolates came from series of patients as demonstrated above. Our
cultures collected outside of hospitals from patients findings that 41% of K pneumoniae isolates produced
with substantial health care exposures [31]. These ESBLs and that 15% produced KPC are disturbing.
findings suggest that although CRE are increasing in Reports have indicated that multi-drug resistant
prevalence, their distribution is limited [31, 32]. organisms are associated with increased hospital
www.iajps.com Page 1517
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
length of stay and an increase in health care resource 10.Dube EM. Antimicrobial Stewardship Program
consumption. Its prudent that health care systems Annual Report. Northern Area Armed Forces
implement strategies that would arrest the spread of Hospital, 2010- 2011, unpublished.
multi-drug resistant K. pneumoniae. 11.Winokur PL, Canton R, Casellas JM, Legakis N.
Variations in the prevalence of strains expressing an
STUDY LIMITATIONS extended-spectrum b-lactamase phenotype and
The study design being retrospective poses certain characterization of isolates from Europe, the
challenges in missing patient data. Microbiology Americas, and the Western Pacific region. Clin Infect
surveillance data were missing for certain 3 years as Dis, 2001; 32(Suppl 2):S94-103.
indicated above. Therefore, the outcomes of our 12.Babini GS, Livermore DM. Antimicrobial
findings should be interpreted with caution. resistance amongst Klebsiella spp. collected from
intensive care units in Southern and Western Europe
REFERENCES: in 19971998. J Antimicrob Chemother, 2000;
1.Centers for Disease Control and Prevention. 2016. 45:183-189.
Klebsiella pneumoniae in Healthcare Settings. 13.Goossens H. MYSTIC program: summary of
[ONLINE] Available at: European data from 1997 to 2000. Diagn Microbiol
www.cdc.gov/HAI/organisms/klebsiella/klebsiella.ht Infect Dis, 2001; 41:183-189.
ml. [Accessed on February 2, 2016]. 14.Thomson KS, Moland ES. Cefepime, piperacillin-
2.Keynan Y, Rubinstein E. The changing face of tazobactam, and the inoculum effect in tests with
Klebsiella pneumoniae infections in the community. extended-spectrum -lactamaseproducing
Int J Antimicrob Agents, 2007; 30:385-389. Enterobacteriaceae. Antimicrob Agents Chemother,
3.Nordmann P, Cuzon G, Naas T. The real threat of 2001; 45:3548-3554.
Klebsiella pneumoniae carbapenemase-producing 15.Schentag JJ. Clinical pharmacology of the
bacteria. Lancet Infect Dis, 2009; 9:228-236. fluoroquinolones: Studies in human dynamic/kinetic
4.Neuner EA, Yeh JY, Hall GS, Sekeres J, Endimiani models. Clin Infec Dis, 2000; 31(Suppl 2):S40-44.
A, Bonomo RA, Shrestha NK, Fraser TG, Duin DV. 16.Itokazu G, Quinn J, Bell-Dixon C, Kahan F,
Treatment and Outcomes in Carbapenem-resistant Weinstein R. Antimicrobial resistance rates among
Klebsiella pneumoniae Bloodstream Infections. aerobic Gram-negative bacilli recovered from
Diagn Microbiol Infect Dis, 2011; 69(4): 357-362. patients in intensive care units: Evaluation of a
5.Yigit H, Queenan AM, Anderson GJ, Domenech- national postmarketing surveillance program. Clin
Sanchez A, Biddle JW, Steward CD, Alberti S, Bush Infect Dis, 1996; 23:779-784.
K, Tenover FC. Novel carbapenem-hydrolyzing beta- 17.Burwen DR, Banerjee SN, Gaynes RP.
lactamase, KPC-1, from a carbapenem-resistant strain Ceftazidime resistance among selected nosocomial
of Klebsiella pneumoniae, Antimicrob Agents Gram-negative bacilli in the United States. National
Chemother, 2001; 45:1151-1161. Nosocomial Infections Surveillance System. J Infect
6.Hirsch EB, Tam VH. Detection and treatment Dis, 1994; 170:1622-1625.
options for Klebsiella pneumoniae carbapenemases 18.Quinn JP, Miyashiro D, Sahm D, Flamm R, Bush
(KPCs): an emerging cause of multidrug-resistant K. Novel plasmid-mediated -lactamase (TEM-10)
infection. J Antimicrob Chemother, 2010; conferring selective resistance to ceftazidime and
65(6):1119-1125. aztreonam in clinical isolates of Klebsiella
7.Garner JS, Jarvis WR, Emori TG, Horan TC, pneumoniae. Antimicrob Agents Chemother, 1989;
Hughes JM. CDC definitions for nosocomial 33:1451-1456.
infections. Am J Infect Control, 1988; 16:128-140. 19.Quale JM, Landman D, Bradford PA, Visalli M,
8.Dhar S, Martin ET, Lephart PR, McRoberts JP, Ravishankar J, Flores C, Mayorga D, Vangala K,
Chopra T, Burger TT, Tal-Jasper R, Hayakawa K, Adedeji A. Molecular epidemiology of a citywide
Ofer-Friedman H, Lazarovitch T, Zaidenstein R, outbreak of extended-spectrum -lactamase-
Perez F, Bonomo RA, Kaye KS, Marchaim D. Risk producing Klebsiella pneumoniae infection. Clin
factors and outcomes for carbapenem-resistant Infect Dis, 2002; 35:834-841.
Klebsiella pneumoniae isolation, stratified by its 20.Sirot D. Extended-spectrum plasmid-mediated -
multilocus sequence typing: ST258 versus non- lactamases. J Antimicrob Chemother, 1995; 36(Suppl
ST258. Open Forum Infect Dis, 2016; 3(1):ofv213. A):19-34.
9.Yinnon AM, Butnaru A, Raveh D, Jerassy Z, 21.Meyer KS, Urban C, Eagan JA, Berger BJ, Rahal
Rudensky B. Klebsiella bacteraemia: community JJ. Nosocomial outbreak of Klebsiella infection
versus nosocomial infection. QJM, 1996; 89(12):933- resistant to late-generation cephalosporins. Ann
941. Intern Med, 1993; 119:353-358.
www.iajps.com Page 1518
IAJPS 2017, 4 (06), 1511-1519 Bassam R. Almutairi et al ISSN 2349-7750
22.Naumovski L, Quinn JP, Miyashiro D, Patel M, versus nosocomial infection. QJM. 1996; 89(12):933-
Bush K, Singer SB, Graves D, Palzkill T, Arvin AM. 941.
Outbreak of ceftazidime resistance due to a novel 30. Centers for Disease Control and Prevention.
extended-spectrum -lactamase in isolates from Guidance for control of infections with carbapenem-
cancer patients. Antimicrob Agents resistant or carbapenemase-producing
Chemother, 1992; 36:1991-1996. Enterobacteriaceae in acute care facilities. MMWR
23.Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Morb Mortal Wkly Rep, 2009; 58:256-260.
Fishman NO. Extended-spectrum -lactamase- 31.Gupta N, Limbago BM, Patel JB, Kallen AJ.
producing Escherichia coli and Klebsiella Carbapenemresistant Enterobacteriaceae:
pneumoniae: risk factors for infection and impact of epidemiology and prevention. Clin Infect Dis, 2011;
resistance on outcomes. Clin Infect Dis, 2001; 53:60-67.
32:1162-1171. 32.Patel G, Huprikar S, Factor SH, Jenkins SG,
24.Jacoby GA. Extended-spectrum -lactamases and Calfee DP. Outcomes of carbapenem-resistant
other enzymes providing resistance to oxyimino-- Klebsiella pneumoniae infection and the impact of
lactams. Infect Dis Clin North Am, 1997; 11:875- antimicrobial and adjunctive therapies. Infect Control
887. Hosp Epidemiol, 2008; 29:1099-1106.
25.Jacoby GA. Editorial response: epidemiology of 33.Elemam A, Rahimiam J, Mandell W. Infection
extended-spectrum -lactamases. Clin Infect Dis, with panresistant Klebsiella pneumoniae: a report of
1998; 27:81-83. 2 cases and a brief review of the literature. Clin Infect
25.Gaillot O, Marujouls C, Abachin E, Lecuru F, Dis, 2009; 49:271-274.
Arlet G, Simonet M, Berche P. Nosocomial outbreak 34.Bassetti M, Ginocchio F, Mikulska M, Taramasso
of Klebsiella pneumoniae producing SHV-5 L, Giacobbe DR. Will new antimicrobials overcome
extended-spectrum -lactamase, originating from a resistance among Gram-negatives? Expert Rev Anti
contaminated ultrasonography coupling gel. J Clin Infect Ther, 2011; 9:909-922.
Microbiol, 1998; 36:1357-1360. 35.Won SY, Munoz-Price LS, Lolans K, Hota B,
26.French GL, Shannon KP, Simmons N. Hospital Weinstein RA, Hayden MK. Emergence and spread
outbreak of Klebsiella pneumoniae resistant to broad- of Klebsiella pneumoniae carbapenemase-producing
spectrum cephalosporins and -lactamase inhibitor Enterobacteriaceae. Clin Infect Dis, 2011; 53:532-
combinations by hyper production of SHV-5 - 540.
lactamase. J Clin Microbiol, 1996; 34:358-363. 36.Leavitt A, Navon-Venezia S, Chmelnitsky I,
27.Casewell MW, Phillips I. Aspects of the plasmid- Schwaber MJ, Carmeli Y. Emergence of KPC-2 and
mediated antibiotic resistance and epidemiology KPC-3 in carbapenem-resistant Klebsiella
of Klebsiella species. Am J Med, 1981; 70:459-462. pneumoniae strains in an Israeli hospital. Antimicrob
28.Gupta A, San Gabriel P, Haas J. Extended Agents Chemother, 2007; 51:3026-3029.
spectrum -lactamase (ESBL) producing Klebsiella 37.Kochar S, Sheard T, Sharma R, Hui A, Tolentino
pneumoniae outbreak in a neonatal intensive care unit E, Allen G, Landman D, Bratu S, Augenbraun M,
(NICU). Abstract number 241. In: 12th Annual Quale J. Success of an infection control program to
Scientific Meeting of Society for Healthcare reduce the spread of carbapenem-resistant Klebsiella
Epidemiology of America (SHEA), Salt Lake City, pneumoniae. Infect Control Hosp Epidemiol, 2009;
UT, April, 2002. SHEA. 30:447-452.
29.Yinnon AM, Butnaru A, Raveh D, Jerassy Z,
Rudensky B. Klebsiella bacteraemia: community
www.iajps.com Page 1519
Você também pode gostar
- 04 Iajps04062017Documento9 páginas04 Iajps04062017Baru Chandrasekhar RaoAinda não há avaliações
- Ofac 034Documento6 páginasOfac 034Imene FlAinda não há avaliações
- COMPARATIVE ASSESSMENT OF ANTIBIOTIC SUSCEPTIBILITY IN ESBL AND NON-ESBL Klebsiella Pneumoniae IN A TERTIARY HOSPITALDocumento8 páginasCOMPARATIVE ASSESSMENT OF ANTIBIOTIC SUSCEPTIBILITY IN ESBL AND NON-ESBL Klebsiella Pneumoniae IN A TERTIARY HOSPITALijmb333Ainda não há avaliações
- Accepted ManuscriptDocumento23 páginasAccepted ManuscriptMrcom HvqyAinda não há avaliações
- Emergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, PakistanDocumento1 páginaEmergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, Pakistanali zohaibAinda não há avaliações
- Antimicrobial Susceptibility Against MetronidazoleDocumento7 páginasAntimicrobial Susceptibility Against MetronidazolekityamuwesiAinda não há avaliações
- Atashi 2017Documento5 páginasAtashi 2017Shaukat MehmoodAinda não há avaliações
- 3 Saritanayak EtalDocumento7 páginas3 Saritanayak EtaleditorijmrhsAinda não há avaliações
- tmpD1AB TMPDocumento9 páginastmpD1AB TMPFrontiersAinda não há avaliações
- Lahiry 2021Documento11 páginasLahiry 2021AsmaAinda não há avaliações
- Pharmacy: Cephalosporins: A Focus On Side Chains and - Lactam Cross-ReactivityDocumento16 páginasPharmacy: Cephalosporins: A Focus On Side Chains and - Lactam Cross-ReactivityKenneth DayritAinda não há avaliações
- Does Nephrotoxicity Develop Less Frequently When Vancomycin Is Combined With Imipenem-Cilastatin Than With Meropenem? A Comparative StudyDocumento8 páginasDoes Nephrotoxicity Develop Less Frequently When Vancomycin Is Combined With Imipenem-Cilastatin Than With Meropenem? A Comparative StudyAsma BahriAinda não há avaliações
- Nejmoa1911998 PDFDocumento11 páginasNejmoa1911998 PDFStella NoviaAinda não há avaliações
- ArticleDocumento16 páginasArticleTunde OdetoyinAinda não há avaliações
- Jac-Antimicrobial ResistanceDocumento7 páginasJac-Antimicrobial ResistanceJuan Manuel Jiménez LeónAinda não há avaliações
- 1 s2.0 S1201971220302617 MainDocumento7 páginas1 s2.0 S1201971220302617 MainFaizah ShabrinaAinda não há avaliações
- HD MicrobaDocumento5 páginasHD MicrobaDian ApriantoAinda não há avaliações
- Antibiotic Myths For The Infectious Diseases ClinicianDocumento13 páginasAntibiotic Myths For The Infectious Diseases CliniciandrthanallaAinda não há avaliações
- JURNAL Cefaclor Vs Amoxicillin in The Treatment of AcuteDocumento8 páginasJURNAL Cefaclor Vs Amoxicillin in The Treatment of Acuterichard gunturAinda não há avaliações
- Oxacillin Resistant Staphylococcus Aureus Among Hiv Infected and Non-Infected Kenyan PatientsDocumento8 páginasOxacillin Resistant Staphylococcus Aureus Among Hiv Infected and Non-Infected Kenyan PatientsRina ErlinaAinda não há avaliações
- Jvim 31 901Documento6 páginasJvim 31 901Muhammad Imam NoorAinda não há avaliações
- New Guidelines For NeumoniaDocumento7 páginasNew Guidelines For NeumoniacarlosAinda não há avaliações
- Journal 3Documento11 páginasJournal 3margareth silaenAinda não há avaliações
- Knowledge, Attitude and Practice of Healthcare Professionals On Dose Adjustment of Acenocoumarol in AlgeriaDocumento9 páginasKnowledge, Attitude and Practice of Healthcare Professionals On Dose Adjustment of Acenocoumarol in AlgeriaMediterr J Pharm Pharm SciAinda não há avaliações
- Neumonia Asosiada A VentiladorDocumento11 páginasNeumonia Asosiada A VentiladorYnomata RusamellAinda não há avaliações
- New Delhi metallo-β-lactamase-1-producing Klebsiella pneumoniae isolates in hospitalized patients in Kashan, IranDocumento5 páginasNew Delhi metallo-β-lactamase-1-producing Klebsiella pneumoniae isolates in hospitalized patients in Kashan, IranSubhecchha BaidyaAinda não há avaliações
- Ciu 219Documento11 páginasCiu 219Fi NoAinda não há avaliações
- Jac-Antimicrobial ResistanceDocumento7 páginasJac-Antimicrobial ResistanceKarla HernandezAinda não há avaliações
- 1 s2.0 S1201971209000435 MainDocumento7 páginas1 s2.0 S1201971209000435 MainGopalaKrishnanAinda não há avaliações
- MRSA Nosocomial Infection BacteryDocumento6 páginasMRSA Nosocomial Infection BacteryZUKHRUFIA ISNA PRAMADEWIAinda não há avaliações
- Predictors of Positive Blood Culture and Deaths Among Neonates With Suspected Neonatal Sepsis in A Tertiary Hospital, Mwanza-TanzaniaDocumento9 páginasPredictors of Positive Blood Culture and Deaths Among Neonates With Suspected Neonatal Sepsis in A Tertiary Hospital, Mwanza-Tanzaniafasya azzahraAinda não há avaliações
- 394 Full PDFDocumento20 páginas394 Full PDFHaltiAinda não há avaliações
- Updated IDSA - ATS Guidelines On Management of Adults With HAP andDocumento11 páginasUpdated IDSA - ATS Guidelines On Management of Adults With HAP andMeet UnsriAinda não há avaliações
- Falagas 2013 (CRE)Documento11 páginasFalagas 2013 (CRE)Nattawat TeerawattanapongAinda não há avaliações
- 891-894 DR SepehriDocumento4 páginas891-894 DR Sepehrimahardikathesa_21490Ainda não há avaliações
- Risk Factors and The Resistance Mechanisms Involved in Pseudomonas Aeruginosa Mutation in Critically Ill PatientsDocumento9 páginasRisk Factors and The Resistance Mechanisms Involved in Pseudomonas Aeruginosa Mutation in Critically Ill PatientsElsiana LaurenciaAinda não há avaliações
- Cross Sectional Study On Antibiotic Resistance Pattern of Almonella Typhi Clinical Isolates From AngladeshDocumento6 páginasCross Sectional Study On Antibiotic Resistance Pattern of Almonella Typhi Clinical Isolates From AngladeshStella AngelicaAinda não há avaliações
- Klebsiella Pneumoniae: Trends in The Hospital and Community SettingsDocumento5 páginasKlebsiella Pneumoniae: Trends in The Hospital and Community SettingskhanfahsAinda não há avaliações
- 29-Infect Drug Resist - 2023 - Pathogen Burden Among ICU Patients in a Tertiary Care Hospital in Hail KSA With Particular Reference to Β-Lactamases ProfileDocumento11 páginas29-Infect Drug Resist - 2023 - Pathogen Burden Among ICU Patients in a Tertiary Care Hospital in Hail KSA With Particular Reference to Β-Lactamases ProfileskazharuddinAinda não há avaliações
- Articulo Klebsiella Pneumoniae PDFDocumento5 páginasArticulo Klebsiella Pneumoniae PDFOscarEduardoAinda não há avaliações
- Abdul Aziz2015 PDFDocumento18 páginasAbdul Aziz2015 PDFSambit DashAinda não há avaliações
- Xin 2016, Pfge&MlstDocumento8 páginasXin 2016, Pfge&MlstSarah KKCAinda não há avaliações
- Clinical Analisis of Sputum Gram StainsDocumento7 páginasClinical Analisis of Sputum Gram Stainspelcastre r.Ainda não há avaliações
- Journal 8Documento7 páginasJournal 8margareth silaenAinda não há avaliações
- Resistance Mechanisms - United States, 2006-2017: Vital Signs: Containment of Novel Multidrug-Resistant Organisms andDocumento6 páginasResistance Mechanisms - United States, 2006-2017: Vital Signs: Containment of Novel Multidrug-Resistant Organisms andKenny HaAinda não há avaliações
- Heat MapDocumento25 páginasHeat MapSilvi Zakiyatul IlmiyahAinda não há avaliações
- Choosing Antibiotic Therapy For Severe Community-Acquired PneumoniaDocumento7 páginasChoosing Antibiotic Therapy For Severe Community-Acquired PneumoniaJuan Sebastian SuarezAinda não há avaliações
- Prevalence of Positive Blood Cultures in The Emergency Department of A Tertiary Hospital A Retrospective Single-Centre StudyDocumento6 páginasPrevalence of Positive Blood Cultures in The Emergency Department of A Tertiary Hospital A Retrospective Single-Centre Studyeditorial.boardAinda não há avaliações
- Aac 00177-22Documento13 páginasAac 00177-22Robert StryjakAinda não há avaliações
- Niños Clin - Infect - Dis - 2014 - May - 15 - 58 (10) - 1439-48Documento10 páginasNiños Clin - Infect - Dis - 2014 - May - 15 - 58 (10) - 1439-48mariangelAinda não há avaliações
- NaraawadeeniamhundkkDocumento6 páginasNaraawadeeniamhundkkDevanti EkaAinda não há avaliações
- National Ambulatory Antibiotic Prescribing Patterns For Pediatric Urinary Tract Infection, 1998 - 2007Documento9 páginasNational Ambulatory Antibiotic Prescribing Patterns For Pediatric Urinary Tract Infection, 1998 - 2007Rodolfo Rodriguez CamposAinda não há avaliações
- 1 s2.0 S1201971220308407 MainDocumento2 páginas1 s2.0 S1201971220308407 MainАня МурзаковаAinda não há avaliações
- Kontou 2017Documento5 páginasKontou 2017María Cristina RomanoAinda não há avaliações
- Serratia Marcescensbacteraemia in Preterm Neonate - A Case ReportDocumento4 páginasSerratia Marcescensbacteraemia in Preterm Neonate - A Case ReportIJAR JOURNALAinda não há avaliações
- Antigen-Stimulated PBMC Transcriptional Protective Signatures For Malaria ImmunizationDocumento18 páginasAntigen-Stimulated PBMC Transcriptional Protective Signatures For Malaria Immunizationyowan wandikboAinda não há avaliações
- 1 PDFDocumento9 páginas1 PDFFlorencia IrenaAinda não há avaliações
- Mycoplasma Pneumoniae: Prevalance in Navi Mumbai, India Biomedical. Indian Journal of Applied ResearchDocumento4 páginasMycoplasma Pneumoniae: Prevalance in Navi Mumbai, India Biomedical. Indian Journal of Applied ResearchSpinalis 2017Ainda não há avaliações
- Background Changing Patterns of Neonatal Fungal Sepsis in A Developing CountryDocumento5 páginasBackground Changing Patterns of Neonatal Fungal Sepsis in A Developing CountryNada AhmedAinda não há avaliações
- Cancer Immunology: Bench to Bedside Immunotherapy of CancersNo EverandCancer Immunology: Bench to Bedside Immunotherapy of CancersAinda não há avaliações
- Analytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationDocumento8 páginasAnalytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationBaru Chandrasekhar RaoAinda não há avaliações
- Knowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyDocumento8 páginasKnowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyBaru Chandrasekhar RaoAinda não há avaliações
- Gastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsDocumento7 páginasGastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsBaru Chandrasekhar RaoAinda não há avaliações
- Development and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormDocumento11 páginasDevelopment and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormBaru Chandrasekhar RaoAinda não há avaliações
- A Brief Review On YawsDocumento7 páginasA Brief Review On YawsBaru Chandrasekhar RaoAinda não há avaliações
- Review On: Inventory ManagementDocumento8 páginasReview On: Inventory ManagementBaru Chandrasekhar RaoAinda não há avaliações
- Relationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityDocumento4 páginasRelationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityBaru Chandrasekhar RaoAinda não há avaliações
- An Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentDocumento6 páginasAn Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentBaru Chandrasekhar RaoAinda não há avaliações
- Descriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreDocumento4 páginasDescriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreBaru Chandrasekhar RaoAinda não há avaliações
- Pharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoDocumento7 páginasPharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoBaru Chandrasekhar RaoAinda não há avaliações
- RP-HPLC Method Development and Validation of Alogliptin Bulk and Tablet Dosage FormDocumento8 páginasRP-HPLC Method Development and Validation of Alogliptin Bulk and Tablet Dosage FormBaru Chandrasekhar RaoAinda não há avaliações
- Assessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaDocumento7 páginasAssessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaBaru Chandrasekhar RaoAinda não há avaliações
- The Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalDocumento11 páginasThe Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalBaru Chandrasekhar RaoAinda não há avaliações
- Pharmacological and Phytochemical Evidence of Scutia Genus Plants - A ReviewDocumento7 páginasPharmacological and Phytochemical Evidence of Scutia Genus Plants - A ReviewBaru Chandrasekhar RaoAinda não há avaliações
- DISTINCTIVE PHARMACOLOGICAL ACTIVITIES OF Eclipta Alba AND IT'S COUMESTAN WEDELOLACTONEDocumento7 páginasDISTINCTIVE PHARMACOLOGICAL ACTIVITIES OF Eclipta Alba AND IT'S COUMESTAN WEDELOLACTONEBaru Chandrasekhar RaoAinda não há avaliações
- STUDIES ON QUALITATIVE PHYTOCHEMICAL ANALYSIS AND ANTIBACTERIAL ACTIVITY OF Piper NigrumDocumento7 páginasSTUDIES ON QUALITATIVE PHYTOCHEMICAL ANALYSIS AND ANTIBACTERIAL ACTIVITY OF Piper NigrumBaru Chandrasekhar RaoAinda não há avaliações
- Determination of Bioactive Compounds From Piper Longum L. by Using HP-LC AnalysisDocumento4 páginasDetermination of Bioactive Compounds From Piper Longum L. by Using HP-LC AnalysisBaru Chandrasekhar RaoAinda não há avaliações
- Determination of Bioactive Compounds From Piper Nigrum L by Using Ft-Ir Spectroscopic AnalysisDocumento3 páginasDetermination of Bioactive Compounds From Piper Nigrum L by Using Ft-Ir Spectroscopic AnalysisBaru Chandrasekhar RaoAinda não há avaliações
- DETERMINATION OF BIOACTIVE COMPOUNDS FROM Piper Nigrum. L BY USING HPLC ANALYSISDocumento3 páginasDETERMINATION OF BIOACTIVE COMPOUNDS FROM Piper Nigrum. L BY USING HPLC ANALYSISBaru Chandrasekhar RaoAinda não há avaliações
- Nursing Care Plan Diabetes Mellitus Type 1Documento2 páginasNursing Care Plan Diabetes Mellitus Type 1deric85% (46)
- Joy BoosterDocumento2 páginasJoy BoosterAlexsandro TorezinAinda não há avaliações
- Technical RequirementsDocumento14 páginasTechnical RequirementsLucas GuadaAinda não há avaliações
- 67 9268Documento34 páginas67 9268Salvador ReyesAinda não há avaliações
- Mechanical Energy Storage: Created by Nick StroudDocumento24 páginasMechanical Energy Storage: Created by Nick StroudAli ShazanAinda não há avaliações
- Chapter 3Documento26 páginasChapter 3Francis Anthony CataniagAinda não há avaliações
- Philippines and Singapore Trade Relations and Agreements: 1. What Leads To Said Agreement?Documento11 páginasPhilippines and Singapore Trade Relations and Agreements: 1. What Leads To Said Agreement?Ayrah Erica JaimeAinda não há avaliações
- Preparatory Newsletter No 3 2013Documento22 páginasPreparatory Newsletter No 3 2013SJC AdminAinda não há avaliações
- Heat and Mass Chapter 2Documento49 páginasHeat and Mass Chapter 2Mvelo PhungulaAinda não há avaliações
- T.Y.B.B.A. (CA) Sem VI Practical Slips 2019 PatternDocumento30 páginasT.Y.B.B.A. (CA) Sem VI Practical Slips 2019 PatternJai Ramteke100% (2)
- Report Palazzetto Croci SpreadsDocumento73 páginasReport Palazzetto Croci SpreadsUntaru EduardAinda não há avaliações
- Difference Between Dada and SurrealismDocumento5 páginasDifference Between Dada and SurrealismPro FukaiAinda não há avaliações
- 热虹吸管相变传热行为CFD模拟 王啸远Documento7 páginas热虹吸管相变传热行为CFD模拟 王啸远小黄包Ainda não há avaliações
- Syntax Ps4Documento6 páginasSyntax Ps4blue_child86% (7)
- An1914 PDFDocumento56 páginasAn1914 PDFUpama Das100% (1)
- Debug and AssemblerDocumento9 páginasDebug and AssemblerManoj GurralaAinda não há avaliações
- Unit 9 TelephoningDocumento14 páginasUnit 9 TelephoningDaniela DanilovAinda não há avaliações
- Tia Portal V16 OrderlistDocumento7 páginasTia Portal V16 OrderlistJahidul IslamAinda não há avaliações
- Canadian Solar-Datasheet-All-Black CS6K-MS v5.57 ENDocumento2 páginasCanadian Solar-Datasheet-All-Black CS6K-MS v5.57 ENParamesh KumarAinda não há avaliações
- Linic - by SlidesgoDocumento84 páginasLinic - by SlidesgoKhansa MutiaraHasnaAinda não há avaliações
- Plasterboard FyrchekDocumento4 páginasPlasterboard FyrchekAlex ZecevicAinda não há avaliações
- Variables in The EquationDocumento3 páginasVariables in The EquationfiharjatinAinda não há avaliações
- Algorithm Design TechniquesDocumento24 páginasAlgorithm Design TechniquespermasaAinda não há avaliações
- BLDG Permit Form (Back To Back)Documento2 páginasBLDG Permit Form (Back To Back)ar desAinda não há avaliações
- Emergency Floatation Helicoptero PDFDocumento14 páginasEmergency Floatation Helicoptero PDFterrywhizardhotmail.com The Best Of The Best.Ainda não há avaliações
- Programmable Logic Controllers: Basic Ladder Logic ProgrammingDocumento9 páginasProgrammable Logic Controllers: Basic Ladder Logic Programminganuradha19Ainda não há avaliações
- D90KSDocumento1 páginaD90KSAmilton filhoAinda não há avaliações
- #5-The Specialities in The Krithis of Muthuswamy DikshitharDocumento5 páginas#5-The Specialities in The Krithis of Muthuswamy DikshitharAnuradha MaheshAinda não há avaliações
- Free DMAIC Checklist Template Excel DownloadDocumento5 páginasFree DMAIC Checklist Template Excel DownloadErik Leonel LucianoAinda não há avaliações
- CE - 441 - Environmental Engineering II Lecture # 11 11-Nov-106, IEER, UET LahoreDocumento8 páginasCE - 441 - Environmental Engineering II Lecture # 11 11-Nov-106, IEER, UET LahoreWasif RiazAinda não há avaliações