Escolar Documentos
Profissional Documentos
Cultura Documentos
Artigo Lancet 2017
Enviado por
Ende IasmimDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Artigo Lancet 2017
Enviado por
Ende IasmimDireitos autorais:
Formatos disponíveis
Series
Syndemics 2
Non-communicable disease syndemics: poverty, depression,
and diabetes among low-income populations
Emily Mendenhall, Brandon A Kohrt, Shane A Norris, David Ndetei, Dorairaj Prabhakaran
The co-occurrence of health burdens in transitioning populations, particularly in specific socioeconomic and cultural Lancet 2017; 389: 95163
contexts, calls for conceptual frameworks to improve understanding of risk factors, so as to better design and This is the second in a Series of
implement prevention and intervention programmes to address comorbidities. The concept of a syndemic, developed three papers about syndemics
by medical anthropologists, provides such a framework for preventing and treating comorbidities. The term See Editorial page 881
syndemic refers to synergistic health problems that affect the health of a population within the context of persistent See Comment pages 888 and 889
social and economic inequalities. Until now, syndemic theory has been applied to comorbid health problems in poor School of Foreign Service,
immigrant communities in high-income countries with limited translation, and in low-income or middle-income Georgetown University,
Washington, DC, USA
countries. In this Series paper, we examine the application of syndemic theory to comorbidities and multimorbidities (E Mendenhall PhD);
in low-income and middle-income countries. We employ diabetes as an exemplar and discuss its comorbidity with Department of Psychiatry,
HIV in Kenya, tuberculosis in India, and depression in South Africa. Using a model of syndemics that addresses Duke Global Health Institute,
transactional pathophysiology, socioeconomic conditions, health system structures, and cultural context, we illustrate Duke University, Durham, NC,
USA (B A Kohrt MD); MRC
the different syndemics across these countries and the potential benefit of syndemic care to patients. We conclude Developmental Pathways for
with recommendations for research and systems of care to address syndemics in low-income and middle-income Health Research Unit, Faculty
country settings. of Health, University of the
Witwatersrand, Johannesburg,
South Africa
Introduction the affluent to the less affluent.9 Although there are (Prof S A Norris PhD);
This Series paper investigates syndemics involving non- recognised global transformations in obesity, food Department of Psychiatry,
communicable diseases (NCDs) to show the complexities practices, and activity patterns,10 this does not ensure that University of Nairobi
through which social, psychological, and biological universal one-size-fits-all interventions will be effective (Prof D Ndetei MD); Africa
Mental Health Foundation,
factors come together to shape emergent and pervasive across populations. We argue that contextual factors Nairobi, Kenya (Prof D Ndetei);
global health problems. Syndemic refers to the clustering matter, because people experience diabetes differently Public Health Foundation of
of two or more diseases within a population that across social contexts, and this affects how diabetes India, Centre for Chronic
Disease Control, New Delhi,
contributes to, and results from, persistent social and becomes syndemic. This framework is exemplified in
India (Prof D Prabhakaran MD);
economic inequalities.1 The concept focuses on instances scholarship on syndemic suffering that has employed and London School of Hygiene
in which multiple health problems interact, often empirical analysis of individual-level experiences of & Tropical Medicine, London,
biologically, with each other and the sociocultural, syndemic interaction to show how social problems that UK (Prof D Prabhakaran)
economic, and physical environment.1,2 For example, in cluster with diabetes and depression differ across Correspondence to:
the mid-1990s, the anthropologist Merrill Singer26 contexts.7,11,12 For instance, immigration-related stress is Dr Emily Mendenhall, School of
Foreign Service, Georgetown
explored how substance abuse, violence, and AIDS central to the mental health of many Mexican immigrant University, Washington,
cluster together and affect one another among an women with diabetes who have undocumented family DC 20057, USA
impoverished inner-city population in the USA; he members or are themselves undocumented.7 This mental em1061@georgetown.edu
coined the term SAVA syndemic to describe this process. stress differs from women residing in the same
By recognising how these mutually interacting factors communities with different ethnic and legal statuses,
promote adverse health outcomes, the syndemic such as Puerto Ricans and African Americans.8 A
framework moves beyond disease-specific or
multimorbidity models to evaluate how social and
economic conditions foster and exacerbate disease Key messages
clusters.7,8 Syndemics provide a tool for empirically Non-communicable diseases share common risk factors
evaluating how health statuses of multi-morbidity arise resulting in escalation of comorbidities, especially among
in a population, and what health interventions might be low-income, marginalised populations worldwide
most effective for mitigating them. The clustering of social and health problems is often
We focus on type 2 diabetes and discuss how mental overlooked in social epidemiology and other models of
illness and infectious disease can cluster with metabolic epidemiological transition
conditions in both high-income countries (HICs) and low- Syndemic care requires that we recognise how social
income and middle-income countries (LMICs). As obesity problems cluster with and affect medical problems, and that
and other NCDs such as diabetes, hypertension, and heart co-occurring diseases can present differently than singular
disease escalate in LMICs, these conditions become more disorders
prevalent among low-income populations, shifting from
www.thelancet.com Vol 389 March 4, 2017 951
Series
syndemic approach can then be applied to design response, alterations in glucose transport, and potentially
integrated chronic care that can be locally relevant and through dysregulation of the hypothalamic-pituitary-
most effective at mitigating the root causes of co-occurring adrenal axis,27,29 as well as behavioural patterns, including
conditions in public health and medicine.13 consumption of high-caloric foods, low engagement in
Our goal is to examine how syndemic approaches physical activity, and use of antidepressants that enhance
previously limited to socially and economically weight gain,20 and social factors that promote stress,
disadvantaged populations in HICs could be expanded to eating, and reduced physical activity.19
apply to conditions in LMICs. We triangulate research Moreover, there is ongoing debate about the role of
from medicine, public health, and anthropology to antidepressants increasing the risk of type 2 diabetes, with
illustrate how poverty, depression, and diabetes cluster in diverse causal pathways that require further research.2931
the low-income populations in HICs, and we illuminate In the short term, use of selective serotonin reuptake
the various facets of their interaction. We bring this inhibitors can improve glycaemic control.31 Long-term
discussion to LMIC contexts and discuss diabetes observational studies have mixed outcomes, with some
comorbidity with HIV in Kenya, tuberculosis in India, meta-analyses suggesting increased lifetime risk of type 2
and depression in South Africa. Considering how social diabetes.30,3235 The increased use of second-generation
and health problems cluster together and mutually antipsychotic augmentation for depression treatment
exacerbate one another differently across contexts is an poses risks for diabetes given the metabolic changes
indispensable way in which we can frame, understand, associated with these medications when used as
and treat NCDs. Through a syndemic orientation, global adjuvants.36 Numbers of prescriptions for second-
health practitioners can recognise in their clinical generation antipsychotics tripled between 2000 and 2010
practice and community-based intervention how social, in the USA, with one in eight adults with depression
cultural, and political factors facilitate disease clusters being prescribed a second-generation antipsychotic. Rates
and escalate morbidity and mortality. of second-generation antipsychotic augmentation were
higher among adults with diabetes.37 Untreated depression
Principles of syndemic theory is a risk factor for diabetes through behavioural pathways
Syndemic theory provides a framework to advance including poor diet, limited exercise, and other
medicine, health systems, and human rights by bringing vulnerability behaviours. Psychological treatments of
multiple fields together to recognise, describe, and depression, such as cognitive behavioural therapy,
appropriately intervene in the complex multiple disease improve glycaemic control in patients with diabetes29,31 and
burdens that afflict susceptible populations. We describe reduces risk factors for type 2 diabetes in people with
how syndemic theory enables us to: recognise biological depression in general.
interactions between co-occurring conditions that can Second, we can describe under what circumstances
belie the true interaction of two or more conditions; diseases interact. For example, socioeconomic factors
describe under what circumstances two or more medical such as poverty, migration, discrimination, exposure to
conditions interact and what can be done to intervene; chronic and acute trauma, including violence, and drivers
and intervene in ways that address social and medical of social and economic marginalisation are associated
conditions that interact, and promise to offset the burden with mental health, diabetes, or both. Trade policies that
of their interaction. promote big food corporations, and economic or social
First, we must recognise biological interactions marginalisation processes that limit primary food staples
between two diseases for a syndemic to occur (figure). to highly processed, high sugar, high carbohydrate diets,
This interaction can occur because of common risk create an obesogenic environment that increases risk of
factors, whether genetic or environmental, and obesity and diabetes when combined with livelihood
iatrogenically through biological effects of treatment on factors that limit opportunities for physical activity.3841
other physiological systems. Depression and diabetes co- Chronic exposure to interpersonal violence affects
occurrence exemplifies this interaction. Epidemiological hypothalamic-pituitary-adrenal axis processes that alter
studies show a two-times increase in depression in metabolism, food preferences, and protection from
people with diabetes compared with the general global disease.42 Results from studies investigating adverse
population, resulting in adverse effects on morbidity and childhood experiences show that these experiences
mortality.1416 Evidence dating back to 199317 and 200118 increase the risk of physical and mental health
shows that the two conditions maintain a bidirectional disorders.43,44 Differential clustering of risk factors, from
relationship,1921 by which diabetes contributes to local food practices to exposure to violence, combined
depression22 and depression in those with diabetes is with variation in access to risk reduction and protective
associated with non-adherence to diabetes treatment,16,23 factors, will contribute to different syndemic emergence
increased diabetes complications,24 and poor glycaemic across settings. Furthermore, the health system in which
control.25 Depression and diabetes also share biological diseases are treated affects how the diseases interact,
origins,21,2628 particularly the activation of innate including detection, types of treatment, such as the
immunity that leads to a cytokine-mediated inflammatory influence of pharmacological therapies on other health
952 www.thelancet.com Vol 389 March 4, 2017
Series
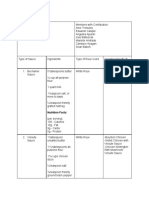
A How do the biological processes and pathophysiology of co-occurring conditions interact?
Pathophysiology of one condition contributes to the other.
Condition Condition Structural and social inequalities shape risk of exposure
Medical treatment of one condition contributes to
A B to environmental and social stressors that contribute to
iatrogenic development of the other condition
inflammatory responses, antiviral activity, and other
Genetic and epigenetic factors predispose to both health conditions disease processes.
Structural,
B How are the conditions experienced by patients and their social networks? social,
Somatic experience Daily activities Meaning and
Perceived pain, functional Perceived ability to perform Effect on social role, personal Culture shapes meaning associated with suffering and cultural
limitations, changes in physical, socio-emotional, value, worldview, and social responses to suffering, illness, and disability.
factors
physical appearance and cognitive tasks moral experience Structural and social factors impede adherence to
clinical recommendations.
C How do medical institutions address co-occurring conditions?
Referral Referral
Primary care services
Specialists coordinate with primary care after referral Culture influences categorisation of medical specialties,
Medical Medical training models for health workers, financing of health
Specialists might or might not coordinate with each other
specialty specialty systems, and stigma among health workers. Structural
Treatment guidelines and collaborative care models for commonly and social inequalities impede access to care, and social
A co-occuring conditions. Financing models to reduce all-cause hospital B
policies promote or impede good health.
readmission incentivise comprehensive care. Social policies address
inequalities
Figure: Model for syndemic approaches to health
(A) Example: depression contributes to pro-inflammatory responses and reduces glucose tolerance. Conversely, inflammatory cytokines associated with diabetes
contribute to depression. Treatment of a depressed patient using an atypical antipsychotic adjuvant could contribute to metabolic syndrome, increasing the risk of
diabetes. (B) Example: a patient might not perceive diabetes and depression as separate conditions. Instead, the patient focuses on functional limitations such as
fatigue and poor concentration. (C) Example: patients diagnosed with diabetes could be provided with health promotion interventions to reduce risk of
depression. Patients with both conditions could be enrolled in a collaborative care treatment programme. Social policies should address common risk factors for
diabetes and depression (eg, diet and exercise constraints, financial insecurity, interpersonal violence, and social cohesion).
conditions, and the economic burden of gaining access to for epidemiological studies to measure how economic
health services (figure). burden of health care worsens health outcomes,
Anthropological research shows that unique social measuring the syndemic suffering of individual lives can
factors cluster with depression and diabetes within be extrapolated to address population-level health
specific populations and social contexts to produce outcomes.7
syndemic suffering. This was documented by the VIDDA Poverty is an established contributor to increased
syndemic that revealed how violence, immigration, and depression and diabetes in HICs,47,48 with growing
abuse clustered with depression and diabetes in Mexican evidence for increased prevalence of diabetes among
immigrant women in Chicago, USA.2 VIDDA reveals how middle-income and low-income populations in LMICs.49
being a woman and an immigrant or migrant leads to Yet the potential for adverse interaction of these two
certain patterns of exposure to structural violence, diseases is even greater in LMICs, where social and
immigration-related stress, and interpersonal abuse economic hardship further increase the risk of
and marginalisation within the health system.45 The concurrent depression in diabetes.50 Measuring
anthropological study not only illustrated how poverty and depression and diabetes in low-income populations is
subjugation influence psychological distress and diabetes, more difficult because of delayed care-seeking, and
but also how internalised emotion, associated with past thereby diagnosis, due to social and financial constraints
abuses and feelings of grief and longing for family in LMIC contexts.51
displaced by migration and documentation, can influence Third, we must intervene in ways that address social
illness. Also, there was evidence that misdiagnosis of grief and medical conditions that interact, and promise to
for psychosis in one Mexican immigrant woman resulted offset the burden of their interaction. This intervention is
in her admission to a psychiatric hospital, rapid weight important because diseases that interact as a result of
gain due to the administration of psychotropic medication, social, environmental, or political factors might require
and the onset of diabetes.46 These conclusions emerged intervention that extends beyond the health system, and
from empirical analysis of life-history narrative, and from could be detected or mitigated by routine engagement
psychiatric and biological data that revealed associations with the health system.52 This can be realised by a health
between specific sources of social suffering and health system that promotes high quality or integrated health
outcomes, and therefore have major implications for both services. For example, there would be lower incidence of
mental health and diabetes care. Although it is common tuberculosis and opportunistic infections in patients
www.thelancet.com Vol 389 March 4, 2017 953
Series
transport, fuelled the escalation of obesity and other
Diabetes (type 2) HIV/AIDS Tuberculosis Depression
related NCDs, including diabetes, in LMICs.39,62 Economic
India transitions have also had an effect on the increase in
Population 86155%50,63,64 031%65 0204%66,67 4515%6870 NCD prevalence among low-income populations (table);41
Low-income urban population 1112% 64,71
035% 65
04611% 66,67
193%69 since they carry a larger portion of the NCD burden,
Kenya understanding the role of local social contexts in disease
Population 36%63,72 60%73 03%74 766%75 incidence and managementderived from ethnographic
Low-income urban population 4810%76,77 10612%78,79 07%*80 30%75 and mixed-methods researchbecomes crucial for
South Africa designing effective prevention and treatment modalities.
Population 7183%63,72 1120%81,82 08%82 510%68,83,84 Epidemiological transition of NCDs to low-income
Low-income urban population 121% 85,86
2230% 87,88
155% 89
90%83 populations in LMICs poses a complex medical context
USA in which NCDs interact with infectious chronic diseases,
Population 911%63,90 0409%91 0003%92 66%93 such as HIV/AIDS and tuberculosis.97 Although such
Low-income urban population 10%94 21%95 097%92 154%96 diseases were considered emergencies two decades ago,
today HIV/AIDS and tuberculosis are effectively
*Cause of death data from urban slum populations. The data reported are from New York City only.
controlled and managed in many contexts with practices
Table: Prevalence of type 2 diabetes, HIV/AIDS, tuberculosis, and depression in India, Kenya, South Africa, resembling clinical and public health efforts for chronic
and the USA conditions.98 Indeed, a small number of health delivery
programmes, such as Academic Model Providing Access
with HIV in settings with early detection and access to to Healthcare (AMPATH) and Partners in Health,99,100
and effective delivery of antiretrovirals.53 Moreover, have shown that infectious chronic diseases programmes
integrating comprehensive screening for co-occurring also can integrate chronic NCD care for those living with
conditions, such as screening for metabolic disorders HIV/AIDS. Despite the growing body of research
among those who routinely take antiretrovirals,54 would showing the effect of NCDs on low-income populations,49
promote detection and control of NCDs that are and the negative effect that NCDinfectious chronic
traditionally marginalised within the health system.55 disease convergence has on people with low income in
The most relevant integration of health services for LMICs,101,102 more traditional global health priorities,
syndemic depression and diabetes is of mental health including HIV/AIDS, tuberculosis, and malaria, continue
services into primary care settings.5658 Mental disorders to receive the majority of development assistance.59 There
are often under-diagnosed in primary care settings is evidence that by overlooking the looming economic
because there is no screening or treatment, and because and biological repercussions of NCDs, global health
mental distress can present in different ways across financing lags behind the epidemiological burden of
contexts. In LMICs, unrecognised depression can be as disease,103 with the consequence of overburdening health
high as 40% among people with diabetes or systems with people seeking care for diabetes when their
hypertension.49,50,59 In health systems that integrate diabetes is in advanced stages. Yet, by incorporating
mental health into primary care, early detection and measures for NCDsincluding tobacco use and
treatment leads to lower comorbidity of common mental prevalence of cardiovascular disease, diabetes, cancer,
disorders with other NCDs,57,60 as well as fewer and chronic respiratory diseases among adults aged
complications. 3070 yearsin the Sustainable Development Goals,
there is potential for more political and financial attention
Diabetes syndemics in rapidly transitioning to be directed to NCDs.
economies Local contexts influence syndemic interaction of
Syndemics provide an important alternative to NCD diabetes with diseases of poverty and must be recognised
epidemiology because the framework addresses how in the design and implementation of interventions. For
social conditions affect the emergence and medical example, structural factors influence the emergence of
outcomes related to NCDs such as diabetes, cancer, NCDs by affecting not only what people eat,39 but also
stroke, and mental illness. Broadly, epidemiologists have how people move securely in the world,104 addressing
shown that rapid economic growth has contributed to issues from unemployment to laws surrounding
demographic, nutrition, and health transitions that have immigration and personal securities; these factors have
extensively shaped the incidence and prevalence of been closely linked to obesity105 and diabetes.42
obesity.9,61 Such transitions come together through Sociocultural factors, such as gender inequality, racism,
technological innovations, labour opportunities, rural-to- and social networks, also influence stress, mental health,
urban migration, access to education, and social mobility, and incidence and experience of NCDs.106,107
which greatly transform how people think, move, and Anthropological research on syndemics reveals that
nourish their bodies. For example, the influx of highly diabetes interacts differently with one or two diseases of
processed and high-caloric food, sugar-sweetened poverty across contexts.8,108 Although depression
beverages, cheap oil, and mechanisation of tools and commonly occurs with diabetes,109 social experiences vary
954 www.thelancet.com Vol 389 March 4, 2017
Series
based on social, cultural, and economic variance within depression are experienced differently among the affluent
and between populations.8,48 For example, the legacy of and the poor, with different social factors contributing to
the HIV/AIDS epidemic has had a profound impact on mental illness in those with diabetes, on the basis of
how people experience living with diabetes; research socioeconomic status;117 for example, social isolation affects
from Kenya and South Africa underscores the social wealthy Indian mothers, and financial insecurity in low-
consequences of caring for AIDS-orphaned income mothers causes extreme stress and psychological
grandchildren in the lives of middle-aged patients with distress, including depression.117
diabetes.11,110 In these contexts, the social cost of the In these cases, social and economic factors contribute to
epidemic (as opposed to the biological effect) mediates psychological distress, and depression continues to have a
their ability to dedicate social and financial resources to negative effect on their diabetes. This negative biofeedback
managing their chronic illness. Recognising what social loop underscores the importance of recognising how social
forces interact with the comorbidity within and between conditions influence medical conditions.57,111 As diabetes
populations is important, because although biological increases among low-income populations in LMICs,
interactions are similar between depression and diabetes, structural and social factors play an important part in what
social interactions could have a differential effect on diseases of poverty become syndemic with diabetes, in
biological outcomes. This point relates both to the social addition to depression. In South Africa, care for diabetes
and financial cost of the AIDS epidemic, as well as how and depression are separated within the health-care
living with both HIV and diabetes changes the way institution so that if someone presents with depressive
in which diabetes is experienced. Heterogeneity of symptoms during routine diabetes care, structural barriers
designing care packages for syndemic clusters then impede their ability to seek mental health care (panel 1).118
occurs at the local level and underscores the idea that
one-size-fits all treatment modalities hinders productive Syndemic poverty, diabetes, and HIV in LMICs
dialogue about local social and medical needs. We next HIV comorbidities, typically with tuberculosis and
discuss diabetes comorbidity with depression, HIV, and opportunistic infections, have undergone extensive
tuberculosis in LMIC settings that are undergoing rapid research and have been the topic of clinical guideline
socioeconomic change. development. However, comorbidities of HIV with NCDs
have received considerably less attention. NCD-HIV
Syndemic poverty, diabetes, and depression in LMICs syndemics emerge in LMICs as a result of global reduction
A syndemic model is crucial to understand how context of infectious diseases,98 broad management of HIV as an
contributes to the experience and epidemiology of infectious chronic disease,101 and escalation of NCDs in
depression and diabetes co-occurrence between HIC and low-income populations.102 Economic growth, international
LMIC settings, and how it varies within countries. investment, and effective antiretroviral therapy have
Globally, diabetes intersects with chronic depression profoundly shaped the incidence and prevalence of
more frequently in low-income populations because of HIV/AIDS in the most affected countries, as well as
the strong relationship between depression and poverty111 longevity of those living with HIV.54 Increasingly, there is
and the stresses linked to poor access to, and extraordinary epidemiological evidence of syndemic clustering of HIV
costs of, diabetes care.49 We have already outlined how and diabetes within the same communities; this is possible
the co-occurrence of diabetes and depression has today because people with HIV are living a decade
received extensive biomedical attention,19 often longer than they did two decades previously.119 For
highlighting an underlying biological interaction,27 bi- instance, 143% of 1251 adult women residing in Soweto,
directionality,109 and economic effects of comorbidity.112 South Africa, a township of Johannesburg, have diabetes,85
Depression also increases risk for morbidity and and in the same community one in four people is HIV-
mortality in those with diabetes113 and this is common positive.120 Similarly, in Nairobi slums, an estimated 12% of
among socially and economically disadvantaged urban adult low-income Kenyans have HIV/AIDS78 and
populations.49,114 Therefore, there is substantial evidence 10% of adults aged between 40 and 54 years have
that the interactions and outcomes of depression and diabetes.76 Cohort studies in Uganda and South Africa
diabetes are mediated by social contexts,8,115 and therefore document HIV-NCD convergence;121124 psychological
are particularly devastating among low-income distress increases among those with multiple conditions
populations in HICs116 and LMICs.49 and NCDs are lower among older adults without HIV,
Clear epidemiological evidence shows that depression which might result from routine antiretroviral therapy.125
presents more commonly among those with diabetes More epidemiological studies are needed that document
compared with the general population in LMICs,50 and the co-occurrence of diabetes and HIV within the same
increasingly in low-income populations in LMICs.49 individuals; however, anthropological research shows that
However, only a few studies have provided in-depth people with HIV are developing diabetes and this poses
analysis of how the cluster of these two diseases complex medical issues, including the prioritisation of
materialises within these populations. Anthropological HIV care over diabetes care because of international donor
research from India addresses how diabetes and stipulations on AIDS funding.11 Since diabetes clusters
www.thelancet.com Vol 389 March 4, 2017 955
Series
Panel 1: Syndemic care in Soweto, South Africathe case of diabetes and depression
Clinical vignette Often, adherence to treatment regimens is compromised
A 45-year-old woman presents with frequent urination and because diabetes, depression, or both, are not well managed.
foot soreness. A finger prick was taken to establish that she has Barriers from going to two separate places will affect one or both
type 2 diabetes. She has not previously received routine medical diseases. This is further complicated if people have more than
care for this condition. two morbidities, including tuberculosis or HIV.118
Of the 4050-year-old female population in Soweto, 143% are Syndemic care system
diabetic and 50% will not know they have diabetes.85 We do not Syndemic care in South Africa would align with current
know what percentage have depression. The likelihood that this restructuring of health systems that involves a four-pronged
woman has depression is high. Individuals with symptoms like approach for comprehensive health-care coverage, including a
those described will often go to a clinic, since health-service primary health-care package, ward-based outreach teams, school
access in South Africa is good. Those with diabetes, depressive health services, and an integrated chronic disease management
symptoms, or both, will be referred to a tertiary hospital. model. Such an approach would view patients as one unit as
Current care system opposed to diseases as one unit. Syndemic care would provide a
Often, patients do not know they have diabetes because limited clinic where, even if you go there for testing for one disorder,
community prevention or screening campaigns exist. Once such as HIV or diabetes, clinicians would employ a holistic
symptoms become severe, patients will seek care initially at a approach. This would include testing for major comorbidities,
clinic and then at a tertiary hospital, where they will be including HIV, tuberculosis, hypertension, and diabetes,
diagnosed and have a treatment regimen identified. They can alongside a general mental health assessment. Ones mental
receive check-ups and medicines (particularly metformin) at the health has a direct effect on how people adhere to long-term
community level. Common mental disorders are rarely treatment regimens. Because physical diseases are most likely to
diagnosed at community clinics or tertiary hospitals. be chronic, mental health states will affect other chronic care
conditions. Once comorbidity profiles are formulated, then the
Most people with depression who seek medical care at a treatment of that patient would be holistic.
community clinic will be undiagnosed with depression. If
symptoms are severe, patients might be referred to a tertiary Syndemic care would ensure task-sharing across the health system.
institution that has a psychiatric clinic to screen, diagnose, and Nurses would prioritise mental health screening and multi-
assign treatment. The tertiary institution will manage mental morbidity screening. After the general health assessment
health medication and management. screening, each patient would meet with a counsellor and clinician
as they set up their care plan. The clinic would serve as a place of
In this system, chronic care for diabetes and depression would be diagnosis, treatment, and receipt of medicine. Community-based
completely isolated to different clinics, doctors, and treatment support over the course of ones illness would involve assignment
plans. Clinics can capture clinical information. But the system will of a community health worker to provide long-term syndemic care
not identify the patient as someone with two chronic conditions that addresses social and medical problems, such as social support,
and will not share information with clinics providing concurrent accessing and taking medications, and identifying any risk for
care. The social cost of this system requires patients to seek complication or further problems.
chronic medical care and medicines from two clinics.
with infectious chronic diseases, social conditionssuch exclusive priorities displace other diseases126 and derail
as living in close quarters, food security, and feeling safe strategic partnerships for building health systems and
and affordable and accessible medical care become strengthening community health.127 Therefore,
syndemic co-factors that create the potential for disease recognising the role of health systems and the delivery of
clustering and adverse interactions. primary health care to low-income populations holds an
Financing of health systems has a fundamental role in important position in syndemics. This is particularly true
modelling syndemics because it determines which in countries that do not have universal health coverage to
diseases are prioritised, tested, and treated in primary assure accessible care for all members of the population.
care settings. An exemplar of this is how global HIV In Kenya, diseases are individuated into specialty
funding shapes health systems and practices. In contexts clinicssuch as a diabetes clinic, HIV clinic, and
where the international donors provide free HIV testing tuberculosis clinicthat are devoid of a coordinated
and treatment, prioritisation of HIV has historically person-centred medical care model that addresses
overshadowed other diseases that afflict low-income individual patients unique needs (panel 2).
populations, including NCDs such as diabetes and
depression. Although it is clear that investment in the Syndemic poverty, diabetes, and tuberculosis
HIV/AIDS platform has a positive effect on other areas of Living in close quarters and high rates of tuberculosis,
global health,55 there is competing evidence that such including drug-resistant tuberculosis, pose complex
956 www.thelancet.com Vol 389 March 4, 2017
Series
Panel 2: Syndemic care in Nairobi, Kenyathe case of diabetes and HIV/AIDS
Clinical vignette symptoms become extreme; these tests require out-of-pocket
A 40-year-old woman with HIV presents with thirst and payments for patients who do or do not have HIV. If a physician
frequent urination. She receives antiretroviral therapy weekly. diagnoses one disease, then rarely are they examined for
She reports that she is feeling tired and cries most of the day comorbidities, including diseases that commonly cluster
and is referred to a counsellor in the HIV clinic. together, such as depression, hypertension, and diabetes.
In Kibera slum in Nairobi, Kenya, 12% of the population has HIV Patients will pay out-of-pocket for any medications associated
and 10% of middle-aged adults have type 2 diabetes.128 More with non-communicable diseases.11
than half of primary care patients suffer from one or more of Syndemic care system
the following: anxiety (31%), depression (26%), and Syndemic care in Kenya requires a reorientation of priority
somatoform disorder (13%),129 but rarely are they evaluated for diseases. Currently, the prioritisation of infections such as HIV/
mental distress unless they are HIV-positive. Blood tests for AIDS and tuberculosis marginalises other diseases that might
diabetes require out-of-pocket payments so they are rarely cause adverse health alone or together with infectious diseases.
conducted in public clinics. Syndemic care requires common conditions, including HIV,
Current care system tuberculosis, malaria, diabetes, hypertension, depression,
The patient goes to the public clinic and receives free voluntary alcoholism, and smoking, to be evaluated when individuals first
counselling and testing for HIV. If the individual is HIV-positive, enter a triage clinic. This would include a standard medical
then they enrol in an HIV care pathway that is completely free for history, standard evaluation of blood pressure, a symptom
the patient (funded primarily by international donor funding). checklist for tuberculosis (and sputum test for those with a
If the patient is diagnosed with HIV at a small facility, then they cough), screening for psychiatric and behavioural conditions,
will be referred to a tertiary hospital to begin medical treatment. and a blood test for HIV and type 2 diabetes.
If they are diagnosed at a tertiary hospital, then the patient will Syndemic care involves comprehensive health evaluation
be scheduled for comprehensive care at that facility. All costs for provided free-of-charge as preventive care. This requires
antiretroviral treatment as well as tuberculosis treatment, a investment in the health system and eventual provision of
common opportunistic infection, are provided free of cost. testing and medication for these common diseases. This care is
There are high compliance rates for HIV and tuberculosis important for people with HIV and other common conditions
medication. A patient with HIV who presents with depressive or that might go undiagnosed; a modified list of priority diseases
anxious symptoms will be referred to a counsellor associated could be used in rural areas.
with the HIV clinic where they could receive treatment. Syndemic care requires community-based follow-up to
However, patients who are not HIV-positive will rarely be evaluate health outcomes and modification of treatment
examined for common mental disorders, and only in the most regimens. This would be carried out by community health
extreme cases will they be referred to a social worker associated workers as opposed to requiring patients to return to the
with the outpatient clinic or to a counsellor in the HIV clinic. primary health centre, which would contribute to decreased
Individuals who present with symptoms of type 2 diabetes, cost and improved medical outcomes.
such as frequent thirst and urination, will only be tested if
medical problems. The re-emergence of tuberculosis in for spreading tuberculosis from or to those with
response to the emergence of HIV/AIDS, and resultant diabetes. Biological vulnerability for tuberculosis
co-infection, has been a priority in global health as infection when someone has diabetes poses a greater
evidenced by funding and treatment guidelines. With environmental risk, especially when living in close
increasing rates of diabetes among low-income quarters with someone with active tuberculosis. Even
communities, there is a need to consider how diabetes more, tuberculosis can exacerbate or even initiate
increases risk of active tuberculosis. Diabetes diabetes by predisposing individuals to impaired
unidirectionally triples the risk of active tuberculosis, glucose tolerance, and tuberculosis drugs (eg,
particularly among the impoverished.130 Although this rifampicin) can make it more difficult to control
comorbidity has only recently received international diabetes.138 Recognising biological and social
attention,131133 the number of studies examining vulnerability for infection among those with diabetes
syndemic interactions of diabetes and tuberculosis has shows how important a syndemic understanding can
increased in recent years, drawing from evidence in beparticularly in syndemic interactions between
Indonesia,134 India,135 and among Hispanic people NCDs and infectious chronic diseases in people living
in the USA.136,137 Diabetes-tuberculosis interactions in high residential-density environments. With
produce biological, social, and economic confluence population health models that are focused on causation,
among populations, not only because of demand for the assumption that you can intervene in disease-
chronic care for both diseases, but also the propensity specific pathways, as opposed to syndemic-based
www.thelancet.com Vol 389 March 4, 2017 957
Series
Panel 3: Syndemic care in Delhi, Indiathe case of diabetes and tuberculosis
Clinical vignette will receive diabetes treatment and follow-up. Some patients
A 51-year-old man presents with a cough that has persisted for seeking care at primary health-care centres or private
2 weeks. After initial treatment with a private practitioner he is practitioner-led clinics will return every 3 months for monitoring
referred to a centre that has facilities to diagnose tuberculosis. of blood glucose. Diabetes care will continue after tuberculosis
Once diagnosed after sputum examination and chest treatment is complete, although there is not any modification of
radiograph, he is assigned treatment for tuberculosis. When the diabetes treatment regimens for people with concurrent
treatment did not work after 1 month, the patient is identified tuberculosis compared with those without tuberculosis.
with multidrug-resistant tuberculosis and assigned a new Low-income populations are most likely to seek medical care
course of treatment. A finger stick blood sample is then drawn from public clinics located in the community. Tuberculosis and
to test for type 2 diabetes. diabetes rates are much higher than previously suspected in
For the 4065-year-old population in Delhi, around 13% have low-income populations; people with diabetes are more likely
tuberculosis (compared with less than 04% in total in India; see to acquire active tuberculosis and have poorer tuberculosis
table). Those who present with tuberculosis are 23-times more treatment outcomes. Tuberculosis also worsens blood sugar
likely to have diabetes.139 In Delhi, 126% of people with control, revealing a bidirectional relationship.133 But there are
tuberculosis have diabetes and 9% are undiagnosed with no guidelines for current glucose testing alongside tuberculosis
diabetes. Depression is also a common comorbidity with treatment regimens, and no management protocols.
diabetes and tuberculosis but is rarely tested. Patients seeking
Syndemic care system
public care will be cared for at the primary care clinic.
Syndemic care views patients as one unit as opposed to having
Current care system discrete diseases. Syndemic care would provide a triage clinic
Most likely the patient will present at the primary care centre where all patients are tested for diabetes, hypertension,
with a cough. The patient will be advised to go home and depression, alcoholism, HIV, and frequency of smoking. Other
return if the cough persists for 2 weeks. If the cough persists diseases would be screened for on the basis of a symptoms
then the patient will begin standard treatment for tuberculosis, checklist (eg, those with a cough would have a sputum test).
which is a 1-month course of direct observed therapy, short- Syndemic care would require community-based follow-up to
term, in which the patient returns to the primary care centre evaluate health outcomes and modification of treatment
every day, where the drugs are administered. If the patient regimens. This would be carried out by community health
does not respond to these drugs, then the patient is diagnosed workers as opposed to requiring patients to return to the
with multidrug-resistant tuberculosis and a revised treatment primary health centre. Syndemic care thus would treat the
plan is administered. It is at this point that the patient will be whole patient as opposed to on a case-by-case or
tested for diabetes. The patient is never evaluated for disease-by-disease basis. Syndemic care would further
depression, anxiety, or alcohol use. contribute to the avoidance of multiple visits to specialists and
The patient might report symptoms of thirst, hunger, and reduce costs. Syndemic care should have a very important role
frequent urination when seeking care for a cough. When a for care of elderly people because of the common role of
patient with tuberculosis also has diabetes, they are commonly multimorbidity and effect of social factors on mental and
referred to a diabetologist in a secondary care centre, where they physical health outcomes in older people.
prevention and treatment, would clearly overlook the syndemic care, panels 13).5 Indeed, there are many
diabetes-tuberculosis syndemic because they are viewed models of effective integrated health care delivery and
as having distinctly different origins and disease critiques of how clinical interventions neglect social or
progression. Panel 3 describes the growing challenge of non-medical problems.140 Many physicians simply believe
diabetes and tuberculosis in India, and the public that structural and social interventions are not our
health and clinical responses. job,141 a belief that points to how clinical training
explicitly focuses on diagnosis and treatment without
Application of syndemic models to improve considering how social problems affect medical
global health problems.142 Moreover, with increasing complexity of
The syndemic framework can have a measurable effect patient care, there is increased risk of negative sequelae
on health care and quality of life when applied to public for both patients and health-care providers.143
health and clinical medicine. Syndemics render There is an obvious need for integrated chronic care
prevention and intervention programmes more that addresses the negative feedback loop between
successful when addressing the multiple disorders and structural and social problems, diabetes, and co-occurring
specific contextual vulnerabilities holistically, rather than conditions such as depression, HIV, and tuberculosis.
viewing the disorders individually or as extractable from While this approach might seem outside the purview of
the context in which they occur (as shown by models for clinical medicine, there is a precedent, such as the work
958 www.thelancet.com Vol 389 March 4, 2017
Series
of Rwandas Ministry of Health with Partners in Health system, from provision of HIV care148 to mental health
and the Clinton Foundation.99 Together, Rwandas care.149 Task-sharing, also called task-shifting, is when tasks
Ministry of Health was able to design NCD care for those that are often conducted by specialists, such as diagnosis
living with HIV and AIDS in a largely rural and and management of disease or distribution of medications,
decentralised health-care delivery system. This model are transferred to less-skilled health workers with specific
moved forward the extensive work of Partners in Health training.150 Task-sharing provides an exemplar system
that has traditionally recognised that addressing structural through which syndemic care is delivered; however, it
and social problems is central to mitigating the effects of requires training for holistic health models as opposed to
social and economic marginalisation and improving singular diseases (as is traditionally delivered). Therefore,
community and individual health.141 The model illustrates instead of one community health worker for malaria, and
how instead of focusing on behavioural or lifestyle factors another for mental health, community health workers
for HIV prevention (which have been the standard for would receive syndemic care training. There are increasing
clinical treatment in the USA), attention should be given numbers of examples of mental health interventions being
to the aspects that make HIV a social disease, such as integrated into maternal and child health services given
poverty, gender inequality, and racism.144 Other integrative the strong link between the two domains.151153
programmes, such as AMPATH,145 and a growing body of A syndemic approach for community health workers
research on global mental health,13,57,58 similarly show a would incorporate a standard checklist of myriad
measureable improvement in morbidity and mortality symptoms, to evaluate priority social and health
outcomes through integrative primary health care that conditionsfrom tuberculosis to nutrition, smoking,
bring together interventions for social, psychological, and overcrowded living conditions, and strong or weak social
physical problems. South Africa provides another networks. Once the general screening identifies or
example of national-level integration of services that negates these priority diseases, then individuals will
result from political priorities within transformation of undergo extensive evaluation and set up an integrated
the health system and primary health-care re- treatment plan in the primary health centre with
engineering.146 Tuberculosis was integrated alongside recognition of the complex social and medical conditions
HIV in 2009 and a joint HIV, tuberculosis, and sexually that coexist. Comprehensive, people-centred healthcare
transmitted infection national strategic plan was delivery will enable community health workers to identify
developed. These integrative services have shown a more complex array of social, psychological, and
improvements in health outcomes and management of physical symptoms that affect overall health. Indeed, this
patients, but little has been done regarding the diagnosis approach builds on existing arguments for the integration
and management of NCDs among people living with or of health services and strengthening of health systems in
without HIV/AIDS.147 It appears that integration at these LMICs that are feasible and cost-effective,154 especially in
levels tends to depend on individuals rather than systems. response to increasing incidence of NCDs and infectious
We argue that the concept of syndemic care11 can chronic diseases.52,155 Nevertheless, a syndemic care
actualise coordinated, patient-centred medical visits that model must be comprehensively implemented to prevent
involve comprehensive testing and treatment and routine overburdening community health workers with extra
diagnosis for infections and NCDs, from HIV to tasks. With increasing distribution of tasks to community
tuberculosis, typhoid, diabetes, hypertension, anxiety, health workers, there is growing concern about the
and depression. Once diagnosed, care for these medical economic burden, lack of compensation, and
concerns should be administered from one medical contribution to personal physical and mental health
centre and caregiver so that individuals do not need to problems.156,157 This is especially problematic given that
seek care from multiple, disease-specific centres. the majority of community health workers are women
Community health workers visiting homes in urban and thus bear the greatest burden of uncompensated or
slums can help ensure that patients attend clinic visits, undercompensated labour.158,159
access essential medicines, and manage their multiple Indeed, a syndemic care model is meant to enhance
morbidities; however, community-based care must capabilities of community health workers by increasing
recognise how social problems impede mental and the number of health problems they see but reducing the
physical health. The Philips Foundation is currently geographical region they survey. Moreover, syndemic care For the Philips Foundation see
piloting such programmes through Community Life is intended to simplify care at the community level by http://www.philips.com/a-w/
foundation/philips-foundation.
Centers in Kenya. If development aid were committed to having integrated treatment protocols rather than separate html
such an approach, it would foster opportunities to algorithms for diabetes, mental health conditions,
confront the dynamic socialmedical interactions that maternal and child health, and aspects of social services.
complicate peoples social and medical lives.
Syndemic care should be available at the primary care Recommendations and steps forward
level as well as the community level through integrated We recommend that a syndemic framework be adopted
health care and the strengthening of health systems. Task- as a tool for recognising, researching, testing, evaluating,
sharing has been used by health workers across the health and implementing integrated health programmes,
www.thelancet.com Vol 389 March 4, 2017 959
Series
especially those dealing with multiple chronic conditions. accompanied these projects, including the Public Health Foundation
First, researchers and care providers must recognise how of India and Centre for Chronic Disease Control in New Delhi, India;
Africa Mental Health Foundation in Nairobi, Kenya; MRC/Wits
social and medical problems cluster and interact within Universitys Developmental Pathways for Health Research Unit in
certain populations. Understanding what social problems Johannesburg, South Africa; and John H. Stroger, Jr. Hospital of Cook
affect certain disease clusters across geopolitical contexts County in Chicago, USA. We thank H Stowe McMurray for assistance
and within specific regions and populations is imperative. with the table.
Second, funding institutions must provide opportunities References
for research and data that use a syndemic framework. 1 Singer M. A dose of drugs, a touch of violence, a case of AIDS:
conceptualizing the SAVA syndemic. Free Inq Creat Sociol 1996;
This requires that the syndemic framework is clearly 24: 99110.
operationalised, based on ethnographically grounded 2 Singer MC. Introduction to syndemics: a systems approach to
research, and measurable so that researchers can public and community health. San Francisco: Jossey-Bass, 2009.
3 Singer MC. Aids and the health crisis of the US urban poor:
explicitly propose what social and health problems are the perspective of critical medical anthropology. Soc Sci Med 1994;
concurrent and interacting. Indeed, showing statistically 39: 93148.
how syndemics can improve health outcomes and the 4 Singer MC, Erickson PI, Badiane L, et al. Syndemics, sex and the
city: Understanding sexually transmitted diseases in social and
cost-effectiveness of the health systems is imperative. cultural context. Soc Sci Med 2006; 63: 201021.
Third, more evidence for the effectiveness of integrative 5 Singer MC, Clair S. Syndemics and public health:
care and task-sharing across health workers is needed to reconceptualizing disease in bio-social context. Med Anthropol Q
2003; 17: 42341.
detect syndemic problems and deliver syndemic care.
6 Singer MC. Deperate measures: a syndemic approach to the
Models for the delivery of integrating mental health care anthropology of health in a violent city. In: Rylko-Bauer B,
into primary care provide a foundation for this approach.62 Whiteford L, Farmer P, eds. Global health in times of violence.
Fourth, randomised controlled trials will need to evaluate New Mexico: School for Advanced Research Press, 2009: 13756.
7 Mendenhall E. Syndemic suffering: social distress, depression, and
the syndemic model as a tool for improving outcomes diabetes among Mexican immigrant women. Walnut Creek, CA:
and to determine if the syndemic (re)orientation is Left Coast Press, 2012.
effective. Fifth, on the basis of the aforementioned steps, 8 Mendenhall E. Beyond comorbidity: a critical perspective of
syndemic depression and diabetes in cross-cultural contexts.
policy change will be necessary to move beyond singular Med Anthropol Q 2015; 30: 46278.
disease models and incorporate more integrative 9 Omran A. The epidemiologic transition: a theory of the
syndemic frameworks of disease emergence, interaction, epidemiology of population change. Milbank Q 1971; 49: 38.
and subsequent adverse outcomes. Finally, 10 Popkin BM. Global nutrition dynamics: the world is shifting rapidly
toward a diet linked with noncommunicable diseases.
implementation of syndemic care will provide people- Am J Clin Nutr 2006; 84: 28998.
centred medical care that does not align health-care 11 Mendenhall E, Omondi GB, Bosire E, et al. Stress, diabetes, and
delivery with international donor politics (thereby infection: syndemic suffering in an urban public hospital clinic in
Kenya. Soc Sci Med 2015; 146: 1120.
prioritising one disease, such as HIV, tuberculosis, or 12 Mendenhall E. Syndemic suffering in Soweto: violence and
malaria, more than diseases marginalised by aid funding, inequality at the nexus of health transition in South Africa.
such as NCDs). Instead, a syndemic orientation will Ann Anthropol Pract 2015; 38: 30218.
ensure that the clusters of diseases that emerge among 13 Patel V, Chisholm D, Parikh R, et al. Addressing the burden of
mental, neurological, and substance use disorders: key messages
impoverished populations are recongised as complex and from Disease Control Priorities, 3rd edition. Lancet 2016;
contextually situated. This approach will advance global 387: 167285.
health policy and outcomes among the most socially and 14 Schmitz N, Gariepy G, Smith KJ, et al. Recurrent subthreshold
depression in type 2 diabetes: an important risk factor for poor
economically disadvantaged populations. health outcomes. Diabetes Care 2014; 37: 9708.
Contributors 15 Anderson R, Grigsby A, Freedland K, et al. Anxiety and poor
EM conceptualised, wrote, and edited the article; BAK conceptualised glycemic control: a meta-analytic review of the literature.
and edited the article; SAN, DN, and DP drafted panels and commented Int J Psychiatry Med 2002; 32: 23547.
on the article. 16 Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes
treatment nonadherence: a meta-analysis. Diabetes Care 2008;
Declaration of interests 31: 2398403.
We declare no competing interests. 17 Gavard J, Lustman P, Clouse R. Prevalence of depression in adults
with diabetes: an epidemiological evaluation. Diabetes Care 1993;
Acknowledgments
16: 116778.
This paper discusses research conducted in India, Kenya, South Africa,
18 Anderson R, Freedland K, Clouse R, Lustman P. The prevalence of
and the USA funded by the following institutions: National Institutes
comorbid depression in adults with diabetes. Diabetes Care 2001;
of Health Fogarty International Center (R24 TW007988), Georgetown 24: 106978.
Universitys School of Foreign Service, the South African Medical
19 Holt RIG, de Groot M, Golden SH. Diabetes and depression.
Research Council, the National Science Foundation, and Northwestern Curr Diabetes Rep 2014; 14: 491.
Universitys Cells to Society. BAK is funded by the US National
20 Golden SH, Lazo M, Carnethon M, Page P. Depressive symptoms
Institute of Mental Health (NIMH) through Reducing Barriers to and diabetesexamining a bidirectional association between
Mental Health Task Sharing (K01MH104310-01). SAN is supported by depression and diabetes. J Am Med Assoc 2008; 299: 275159.
the UK MRC/DfID Africa Research Leader Scheme. This research 21 Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F.
study would have been impossible without the hundreds of people Depression as a risk factor for the onset of type 2 diabetes mellitus.
with diabetes willing to share their life stories and health-care A meta-analysis. Diabetologia 2006; 49: 83745.
experiences with us; we are grateful for their time, patience, and 22 Nouwen A, Winkley K, Twisk J, et al. Type 2 diabetes mellitus as a
openness. This study would also be impossible without the institutions risk factor for the onset of depression: A systematic review and
and especially research assistants who hosted, facilitated, and meta-analysis. Diabetologia 2010; 53: 248086.
960 www.thelancet.com Vol 389 March 4, 2017
Series
23 van der Feltz-Cornelis CM, Nuyen J, Stoop C, et al. Effect of 46 Mendenhall E. The cost of healthcare: poverty, depression, and
interventions for major depressive disorder and significant diabete among mexican immigrants in the united states. In: Kohrt BA,
depressive symptoms in patients with diabetes mellitus: a systematic Mendenhall E, eds. Global mental health: anthropological
review and meta-analysis. Gen Hosp Psychiatry 2010; 32: 38095. perspectives. Walnut Creek, CA: Left Coast Press, 2015.
24 de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. 47 Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A.
Association of depression and diabetes complications: Type 2 diabetes incidence and socio-economic position: a systematic
a meta-analysis. Psychosom Med 2001; 63: 61930. review and meta-analysis. Int J Epidemiol 2011; 40: 80418.
25 Lustman PJ, Anderson RJ, Freeland KE, de Groot M, Carney RM, 48 Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence
Clouse RE. Depression and poor glycemic control. Diabetes Care for the relation between socioeconomic status and depression,
2000; 23: 93442. obesity, and diabetes. J Psychosom Res 2002; 53: 89195.
26 Mezuk B, Chaikiat , Li X, Sundquist J, Kendler KS, Sundquist K. 49 Leone T, Coast E, Narayanan S, De-Graft Aikins A. Diabetes and
Depression, neighborhood deprivation and risk of type 2 diabetes. depression comorbidity and socio-economic status in low and
Health Place 2013; 23: 6369. middle income countries (LMICs): a mapping of the evidence.
27 Musselman DL, Betan E, Larsen H, Phillips LS. Relationship of Global Health 2012; 8: 1.
depression to diabetes types 1 and 2: epidemiology, biology, and 50 Mendenhall E, Norris SA, Shidhaye R, Prabhakaran D.
treatment. Biol Psychiatry 2003; 54: 31729. Depression and type 2 diabetes in low- and middle-income countries:
28 Talbot F, Nouwen A. A review of the relationship between a systematic review. Diabetes Res Clin Pract 2014; 103: 27685.
depression and diabetes in adults: is there a link? Diabetes Care 51 Jaspers L, Colpani V, Chaker L, et al. The global impact of
2000; 23: 155662. non-communicable diseases on households and impoverishment:
29 Moulton CD, Pickup JC, Ismail K. The link between depression and a systematic review. Eur J Epidemiol 2014; 30: 16388.
diabetes: the search for shared mechanisms. 52 Beaglehole R, Epping-Jordan J, Patel V, et al. Improving the
Lancet Diabetes Endocrinol 2015; 3: 46171. prevention and management of chronic disease in low-income and
30 Kivimki M, Batty G, Jokela M, et al. Antidepressant medication use middle-income countries: a priority for primary health care.
and risk of hyperglycemia and diabetes mellitus: a noncausal Lancet 2008; 372: 94049.
association? Biol Psychiatry 2011; 70: 97884. 53 Saito S, Mpofu P, Carter E, et al. Declining tuberculosis incidence
31 Deuschle M. Effects of antidepressants on glucose metabolism and among people receiving hiv care and treatment services in east Africa,
diabetes mellitus type 2 in adults. Curr Opin Psychiatr 2013; 26: 6065. 20072012. J Acquir Immune Defic Syndr 2016; 71: e96106.
32 Kivimaki M, Hamer M, Batty G, et al. Antidepressant medication 54 Bloomfield GS, Hogan JW, Keter A, et al. Hypertension and obesity
use, weight gain, and risk of type 2 diabetes: a population-based as cardiovascular risk factors among HIV seropositive patients in
study. Diabetes Care 2010; 33: 261116. Western Kenya. PLoS One 2011; 6: e22288.
33 Yoon J, Cho E-G, Lee H-K, Park S. Antidepressant use and diabetes 55 Ravishankar N, Gubbins P, Cooley RJ, et al. Financing of global
mellitus risk: a meta-analysis. Korean J Fam Med 2013; 34: 22840. health: tracking development assistance for health from 1990
to 2007. Lancet 2009; 373: 211324.
34 Barnard K, Peveler R, Holt R. Antidepressant medication as a risk
factor for type 2 diabetes and impaired glucose regulation. 56 Patel V, Araya R, Chatterjee S, et al. Treatment and prevention of
Syst Rev 2013; 36: 333745. mental disorders in low-income and middle-income countries.
Lancet 2007; 370: 9911005.
35 Wu CS, Gau SS, Lai M-S. Long-term antidepressant use and the
risk of type 2 diabetes mellitus: a population-based, nested 57 Prince M, Patel V, Saxena S, et al. No health without mental health.
case-control study in Taiwan. J Clin Psychiatry 2014; 75: 3138. Lancet 2007; 370: 85977.
36 Spielmans G, Berman M, Linardatos E, Rosenlicht N, Perry A, 58 Lund C, Tomlinson M, de Silva M, et al. PRIME: a programme to
Tsai A. Adjunctive atypical antipsychotic treatment for major reduce the treatment gap for mental disorders in five low-and
depressive disorder: a meta-analysis of depression, quality of life, middle-income countries. PLoS Med 2012; 9: e1001359.
and safety outcomes. PLoS Med 2013; 10: e1001403. 59 Neupane D, Panthi B, McLachlan CS, et al. Prevalence of
37 Gerhard T, Akincigil A, Correll C, Foglio N, Crystal S, Olfson M. undiagnosed depression among persons with hypertension and
National trends in second-generation antipsychotic augmentation associated risk factors: a cross-sectional study in urban Nepal.
for nonpsychotic depression. J Clin Psychiatry 2014; 75: 49097. PLoS One 2015; 10: e0117329.
38 Popkin BM, Hawkes C. Sweetening of the global diet, particularly 60 Druss BG, von Esenwein SA, Compton MT, Rask KJ, Zhao L,
beverages: patterns, trends, and policy responses. Parker RM. A randomized trial of medical care management for
Lancet Diabetes Endocrinol 2016; 4: 17486. community mental health settings: the Primary Care Access, Referral,
and Evaluation (PCARE) study. Am J Psychiatry 2010; 167: 15159.
39 Basu S, Stuckler D, McKee M, Galea G. Nutritional determinants of
worldwide diabetes: an econometric study of food markets and 61 Popkin BM, Adair LS, Ng SW. Global nutrition transition and the
diabetes prevalence in 173 countriescorrigendum. pandemic of obesity in developing countries. Nutr Rev 2012; 70: 321.
Public Health Nutr 2012; 16: 1. 62 Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B.
40 Vellakkal S, Subramanian SV, Millett C, Basu S, Stuckler D, Ultra-processed products are becoming dominant in the global food
Ebrahim S. Socioeconomic inequalities in non-communicable system. Obes Rev 2013; 14: 2128.
diseases prevalence in India: disparities between self-reported 63 Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U,
diagnoses and standardized measures. PLoS One 2013; 8: e68219. Shaw JE. Global estimates of diabetes prevalence for 2013 and
41 Vellakkal S, Millett C, Basu S, et al. Are estimates of socioeconomic projections for 2035. Diabetes Res Clin Pract 2014; 103: 13749.
inequalities in chronic disease artefactually narrowed by 64 Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of
self-reported measures of prevalence in low-income and type 2 diabetes: Indian scenario. Indian J Med Res 2007; 125: 21730.
middle-income countries? Findings from the WHO-SAGE survey. 65 Ministry of Health and Family Welfare, Government of India.
J Epidemiol Community Health 2014; 69: 21825. Chapter 12: HIV Prevalence. In: National Family Health Survey
42 Lee C, Tsenkova V, Carr D. Childhood trauma and metabolic (NFHS-3), 20052006. Delhi, 2007. http://dhsprogram.com/pubs/
syndrome in men and women. Soc Sci Med 2012; 29: 9971003. pdf/FRIND3/FRIND3-Vol1andVol2.pdf (accessed Jan 24, 2017).
43 Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood 66 Oxlade O, Murray M. Tuberculosis and poverty: why are the poor at
abuse and household dysfunction to many of the leading causes of greater risk in India? PLoS One 2012; 7: 18.
death in adults: the Adverse Childhood Experiences (ACE) study. 67 Urban Health Division, Ministry of Health and Family Welfare.
Am J Prev Med 1998; 14: 24558. Health of the urban poor in India. Key results from the National
44 Danese A, Moffitt T, Harrington H, et al. Adverse childhood Family Health survey, 200506. Delhi, 2007. http://dhsprogram.com/
experiences and adult risk factors for age-related disease: pubs/pdf/FRIND3/FRIND3-Vol1andVol2.pdf (accessed Jan 24, 2017).
depression, inflammation, and clustering of metabolic risk 68 Kessler RC, Bromet EJ. The epidemiology of depression across
markers. Arch Pediatr Adolesc Med 2009; 163: 113543. cultures. Annu Rev Public Health 2013; 34: 11938.
45 Mendenhall E, Jacobs EA. Interpersonal abuse and depression 69 Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of
among mexican immigrant women with type 2 diabetes. depression in a large urban south Indian populationthe Chennai
Cult Med Psychiatry 2012; 36: 13653. urban rural epidemiology study (CURES70). PLoS One 2009; 4: e7185.
www.thelancet.com Vol 389 March 4, 2017 961
Series
70 Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of 93 Center for Behavioral Health Statistics and Quality. Behavioral
mental disorders: an update from the WHO World Mental Health health trends in the United States: results from the 2014 National
(WMH) surveys. Epidemiol Psichiatr Soc 2011; 18: 2333. Survey on Drug Use and Health. https://www.samhsa.gov/data/
71 Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf
High prevalence of diabetes, obesity and dyslipidaemia in urban (accessed Jan 24, 2017).
slum population in northern India. Int J Obes Relat Metab Disord 94 Meyer PA, Yoon PW, Kaufmann RB. Introduction: CDC health
2001; 25: 172229. disparities and inequalities reportUnited States, 2013 surveillance
72 IDF. IDF diabetes atlas. 7th edn. Brussels: International Diabetes summaries. MMWR Suppl 2013; 62: 35.
Federation, 2015. 95 Denning P, DiNenno E. Communities in crisis: is there a
73 National AIDS and STI Control Programme. Kenya HIV estimates generalized HIV epidemic in impoverished urban areas of
2014. http://www.unaids.org/sites/default/files/country/ the United States? https://www.cdc.gov/hiv/pdf/statistics_poverty_
documents/KEN_narrative_report_2014.pdf (accessed Jan 24, poster.pdf (accessed Jan 24, 2017).
2017). 96 Pratt LA, Brody DJ. Depression in the US household population,
74 World Health Organization. Global tuberculosis report 2014. 20092012. Hyattsville, MD: National Center for Health Statistics,
Geneva: World Health Organization, 2014. 2014.
75 Ndetei DM, Khasakhala LI, Kuria MW, Mutiso VN, 97 Oni T, McGrath N, BeLue R, et al. Chronic diseases and
Ongecha-Owuor FA, Kokonya DA. The prevalence of mental multi-morbiditya conceptual modification to the WHO ICCC
disorders in adults in different level general medical facilities in model for countries in health transition. BMC Public Health 2014;
Kenya: a cross-sectional study. Ann Gen Psychiatry 2009; 8: 1. 14: 575.
76 Ayah R, Joshi MD, Wanjiru R, et al. A population-based survey of 98 Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years
prevalence of diabetes and correlates in an urban slum community (DALYs) for 291 diseases and injuries in 21 regions, 19902010:
in Nairobi, Kenya. BMC Public Health 2013; 13: 371. a systematic analysis for the Global Burden of Disease Study 2010.
77 Oti SO, van de Vijver SJ, Agyemang C, Kyobutungi C. Lancet 2012; 380: 2197223.
The magnitude of diabetes and its association with obesity in the 99 Kidder A, Kwan G, Cancedda C, Bukhman G. Chronic care
slums of Nairobi, Kenya: results from a cross-sectional survey. integration for endemic non-communicable diseases: Rwanda
Trop Med Int Health 2013; 18: 152030. Edition. Boston: Partners in Health, 2011.
78 Madise NJ, Ziraba AK, Inungu J, et al. Are slum dwellers at 100 Pastakia SD, Ali SM, Kamano JH, et al. Screening for diabetes and
heightened risk of HIV infection than other urban residents? hypertension in a rural low income setting in western Kenya
Evidence from population-based HIV prevalence surveys in Kenya. utilizing home-based and community-based strategies.
Health Place 2012; 18: 114452. Global Health 2013; 9: 21.
79 Magadi M. The disproportionate high risk of HIV infection among 101 Oni T, Unwin N. Why the communicable/non-communicable
the urban poor in sub-Saharan Africa. AIDS Behav 2013; 17: 164554. disease dichotomy is problematic for public health control
80 Ogaro TD, Githui W, Kikuvi G, et al. Diversity of Mycobacterium strategies: implications of multimorbidity for health systems in an
tuberculosis strains in Nairobi, Kenya. Afr J Health Sci 2012; era of health transition. Int Health 2015; 7: 110.
20: 8290. 102 Oni T, Youngblood E, Boulle A, McGrath N, Wilkinson R, Levitt N.
81 Health and Development Africa. Global AIDS response. Republic Patterns of HIV, TB, and non-communicable disease multi-
of South Africa. Johannesburg: Health and Development Africa, morbidity in peri-urban South Africaa cross sectional study.
2012. BMC Infect Dis 2015; 17: 20.
82 Mayosi BM, Lawn JE, Niekerk A Van, et al. Health in South Africa: 103 Daniels Jr ME, Donilon TE, Bollyky TJ. The emerging global health
changes and challenges since 2009. Lancet 2012; 380: 202943. crisis: noncommunicable diseases in low- and middle-income
countries. New York: Council on Foreign Relations, 2014.
83 Herman A, Stein D, Seedat S, Heeringa S, Moomal H, Williams D.
The South African Stress and Health (SASH) study: 12-month and 104 Corburn J, Hildebrand C. Slum sanitation and the social
lifetime prevalence of common mental disorders. determinants of womens health in Nairobi, Kenya.
South African Med J 2009; 99: 33944. J Environ Public Health 2015; published online April.
DOI:10.1155/2015/209505.
84 Stein DJ, Seedat S, Herman A, et al. Lifetime prevalence of psychiatric
disorders in South Africa. Br J Psychiatry 2008; 192: 11217. 105 Hoffmann R, Eikemo TA, Kulhnov I, et al. Obesity and the
potential reduction of social inequalities in mortality: evidence from
85 Crowther NJ, Norris SA. The current waist circumference cut point
21 European populations. Eur J Public Health 2015; published online
used for the diagnosis of metabolic syndrome in sub-Saharan
May 25. DOI:10.1093/eurpub/ckv090.
African women is not appropriate. PLoS One 2012; 7: e48883.
106 Steel Z, Marnane C, Iranpour C, et al. The global prevalence of
86 Peer N, Steyn K, Lombard C, Lambert EV, Vythilingum B, Levitt NS.
common mental disorders: a systematic review and meta-analysis
Rising diabetes prevalence among urban-dwelling black
1980-2013. Int J Epidemiol 2014; 43: 47693.
South Africans. PLoS One 2012; 7: e43336.
107 Needham B, Hill TD. Do gender differences in mental health
87 Lohrmann GM, Botha B, Violari A, Gray GE. HIV and the urban
contribute to gender differences in physical health? Soc Sci Med
homeless in Johannesburg. South Afr J HIV Med 2012; 13: 201013.
2010; 71: 147279.
88 Lawn SD, Bekker L-G, Middelkoop K, Myer L, Wood R. Impact of
108 Richter M. Comorbidity: reconsidering the unit of analysis. Med
HIV infection on the epidemiology of tuberculosis in a peri-urban
Anthropol Q 2016; 30: 53644.
community in South Africa: the need for age-specific interventions.
Clin Infect Dis 2006; 42: 104047. 109 Renn BN, Feliciano L, Segal DL. The bidirectional relationship of
depression and diabetes: a systematic review. Clin Psychol Rev 2011;
89 Claassens M, Nikuze A, Chivese T, Zunza M, Beyers N. Evidence to
31: 123946.
Inform South African Tuberculosis policies (EVISAT) project:
a systematic review of the epidemiology of and programmatic 110 Mendenhall E, Norris SA. When HIV is ordinary and diabetes new:
response to TB in people living in urban informal settlements in remaking suffering in a South African Township. Glob Public Health
South Africa. Stellenbosch: World Health Organization, 2014. 2015; 10: 44962.
90 American Diabetes Association. National diabetes statistics report, 111 Lund C, Breen A, Flisher AJ, et al. Poverty and common mental
20092012, 2014 estimates of diabetes and its burden in the disorders in low and middle income countries: a systematic review.
epidemiologic estimation methods. 2014. https://www.cdc.gov/ Soc Sci Med 2010; 71: 51728.
diabetes/data/statistics/2014statisticsreport.html (accessed Jan 24, 112 Molosankwe I, Patel A, Jos Gagliardino J, Knapp M, McDaid D.
2017). Economic aspects of the association between diabetes and
91 Hall H, An Q, Tang T, et al. National HIV testing dayprevalence depression: a systematic review. J Affect Disord 2012; 142: S4255.
of diagnosed and undiagnosed HIV infectionUnited States, 113 van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J,
20082012. Morb Mortal Wkly Rep 2015; 64: 66762. Pouwer F. Depression and risk of mortality in people with diabetes
92 CDC. Reported tuberculosis in the United States, 2014. https:// mellitus: a systematic review and meta-analysis. PLoS One 2013;
www.cdc.gov/tb/statistics/reports/2014/ (accessed Jan 24, 2017). 8: e57058.
962 www.thelancet.com Vol 389 March 4, 2017
Series
114 de Groot M, Pinkerman B, Wagner J, Hockman E. 138 Dooley K and Chaisson R. Tuberculosis and diabetes mellitus:
Depression treatment and satisfaction in a multicultural sample of convergence of two epidemics. Lancet Infect Dis 2009; 12: 73746.
type 1 and type 2 diabetic patients. Diabetes Care 2006; 29: 54953. 139 Chachra V, Arora V. Study on prevalance of diabetes mellitus in
115 Weaver LJ, Mendenhall E. Applying syndemics and chronicity: patients with TB under DOTS strategy. Indian J Tuberc 2014; 61: 6571.
interpretations from studies of poverty, depression, and diabetes. 140 Kleinman A. Four social theories for global health. Lancet 2010;
Med Anthropol 2014; 33: 92108. 375: 151819.
116 Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and 141 Farmer PE, Nizeye B, Stulac S, Keshavjee S. Structural violence and
high risk for diabetes using A1C criteria in the US population in clinical medicine. PLoS Med 2006; 3: 168691.
19882006. Diabetes Care 2010; 33: 56268. 142 Luhrman TM. Of two minds: an anthropologist looks at American
117 Mendenhall E, Shivashankar R, Tandon N, Ali MK, Narayan KM, psychiatry. New York: Vintage, 2001.
Prabhakaran D. Stress and diabetes in socioeconomic context: 143 Shippee ND, Shah ND, May CR, Mair FS, Montori VM.
a qualitative study of urban Indians. Soc Sci Med 2012; 75: 252229. Cumulative complexity: a functional, patient-centered model of
118 Mendenhall E, Norris SA. Diabetes care among urban women in patient complexity can improve research and practice.
Soweto, South Africa: a qualitative study. BMC Public Health 2015; J Clin Epidemiol 2012; 65: 104151.
15: 1300. 144 Farmer P, Landre F, Mukherjee JS, et al. Community-based
119 Bor J, Herbst AJ, Newell ML, Brnighausen T. Increases in adult life approaches to HIV treatment in resource-poor settings. Lancet 2001;
expectancy in rural South Africa: valuing the scale-up of HIV 358: 40409.
treatment. Science 2013; 339: 96165. 145 Quigley F. Walking together, walking far: how a US and African
120 Karim SA, Churchyard G, Karim QA, Lawn S. HIV infection and medical school partnership is winning the fight against HIV/AIDS.
tuberculosis in South Africa: an urgent need to escalate the public Indianapolis: University of Indiana Press, 2009.
health response. Lancet 2009; 374: 92133. 146 Pillay Y, Mamatja D, Mbengashe T, et al. Joint review of HIV, TB
121 Nyirenda M, Newell ML, Mugisha J, et al. Health, wellbeing, and and PMTCT programmes in South Africa. Department of Health
disability among older people infected or affected by HIV in (South Africa), 2014. http://www.hst.org.za/publications/joint-
Uganda and South Africa. Glob Health Action 2013; 6: 19201. review-hiv-tb-and-pmtct-programmes-south-africa-april-2014
122 Nyirenda M, Chatterji S, Falkingham J, et al. An investigation of (accessed Jan 24, 2017).
factors associated with the health and well-being of HIV-infected or 147 South Africa Government. Negotiated service delivery agreement-
HIV-affected older people in rural South Africa. BMC Public Health FOR OUTCOME 2: a long and healthy life for all South Africans.
2012; 12: 259. Johannesburg, 2010. http://www.gov.za/sites/www.gov.za/files/
123 Gomez-Oliver FX, Thorogood M, Bocquier P, et al. delivery%20agreement%20Health%20Sector%20NSDA.pdf
Social conditions and disability related to the mortality of older (accessed Jan 24, 2017).
people in rural south africa. Int J Epidemiol 2014; 43: 153141. 148 McGuire M, Ben Farhat J, Pedrono G, et al. Task-sharing of HIV
124 Scholten F, Mugisha J, Seeley J, et al. Health and functional status care and ART initiation: evaluation of a mixed-care non-physician
among older people with HIV/AIDS in Uganda. BMC Public Health provider model for ART delivery in rural Malawi. PLoS One 2013;
2011; 11: 886. 8: 110.
125 Mugisha JO, Schatz EJ, Randell M, et al. Chronic disease, risk 149 Padmanathan P, DeSilva M. The acceptability and feasibility of
factors and disability in adults aged 50 and above living with and tasksharing for mental healthcare in low- and middle-income
without HIV: findings from the Wellbeing of Older People study in countries: a systematic review. Soc Sci Med 2013; 97: 82e86.
Uganda. Global Health Action 2016; 1: 111. 150 WHO. Task shifting: rational redistribution of tasks among health
126 Shiffman J. Has donor prioritization of HIV/AIDS displaced aid for workforce teams: global recommendations and guidelines.
other health issues? Health Policy Plan 2008; 23: 95100. Geneva: World Health Organization, 2008.
127 Panter-Brick C, Eggerman M, Tomlinson M. How might global 151 Rahman A, Malik A, Sikander S, Roberts C, Creed F.
health master deadly sins and strive for greater virtues? Cognitive behaviour therapy-based intervention by community
Glob Health Action 2014; 7: 15. health workers for mothers with depression and their infants in
128 Hulzebosch A, van de Vijver S, Egondi T, Oti SO, Kyobutungi C. rural Pakistan: a cluster-randomised controlled trial. Lancet 2008;
Profile of people with hypertension in Nairobis slums: a descriptive 372: 90209.
study. Global Health 2015; 11: 26. 152 Rahman A, Patel V, Maselko J, Kirkwood B. The neglected m in
129 Aillon J, Ndetei D, Khasakhala L, et al. Prevalence, type and MCH programmeswhy mental health of mothers is important
comorbidity of mental disorders in a Kenyan primary health centre. for child nutrition. Trop Med Int Heal 2008; 13: 57983.
Soc Psychiatry Psychiatr Epidemiol 2014; 49: 125768. 153 Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting
130 Riza AL, Pearson F, Ugarte-Gil C, et al. Clinical management of intervention to address maternal psychological wellbeing and child
concurrent diabetes and tuberculosis and the implications for development and growth in rural Uganda: a community-based,
patient services. Lancet Diabetes Endocrinol 2014; 2: 74053. cluster-randomised trial. Lancet Glob Health 2015; 3: e45869.
131 International Union Against Tuberculosis and Lung Disease. 154 Lewin S, Lavis JN, Oxman AD, et al. Supporting the delivery of
The Union: health solutions for the poor. http://www.theunion.org/ cost-effective interventions in primary health-care systems in
what-we-do/publications/general/english/1 (accessed Jan 24, 2017). low-income and middle-income countries: an overview of
132 Lnnroth K, Roglic G, Harries AD. Improving tuberculosis systematic reviews. Lancet 2008; 372: 92839.
prevention and care through addressing the global diabetes 155 Samb B, Desai N, Nishtar S, et al. Prevention and management of
epidemic: from evidence to policy and practice. chronic disease: a litmus test for health-systems strengthening in
Lancet Diabetes Endocrinol 2014; 2: 73039. low-income and middle-income countries. Lancet 2010; 376: 178597.
133 The Lancet Diabetes & Endocrinology. Diabetes and 156 Maes K. Community health workers and social change.
tuberculosisa wake-up call. Lancet Diabetes Endocrinol 2014; Ann Anthropol Pract 2015; 39: 115.
2: 677. 157 Maes K, Closser S, Vorel E, Tesfaye Y. Using community health
134 Alisjahbana B, van Crevel R, Sahiratmadja E, den Heijer M, Maya A. workers. Ann Anthropol Pract 2015; 39: 4257.
Diabetes mellitus is strongly associated with tuberculosis in 158 Closser S. Pakistans lady health worker labor movement and the
Indonesia. Int J Tuberc Lung Dis 2006; 10: 696700. moral economy of heroism. Ann Anthropol Pract 2015; 39: 1628.
135 Kant L. Diabetes mellitustuberculosis: the brewing double trouble. 159 Maes K, Closser S, Vorel E, Tesfaye Y. A womens development
Indian J Tuberc 2003; 50: 834. army: narratives of community health worker investment and
136 Pablos-Mendez A, Blustein J, Knirsch C. The role of diabetes empowerment in rural Ethiopia. Stud Comp Int Dev 2015;
mellitus in the higher prevalence of tuberculosis among Hispanics. 50: 45578.
Am J Public Health 1997; 87: 57479.
137 Ponce-De-Leon A, Garcia-Garcia L, Garcia-Sancho M,
Gomez-Perez F, Valdespino-Gomez J. Tuberculosis and diabetes in
southern Mexico. Diabetes Care 2004; 27: 158490.
www.thelancet.com Vol 389 March 4, 2017 963
Você também pode gostar
- Patients Rights: Presented By: Ederlyn Papa-Destura, RN, ManDocumento57 páginasPatients Rights: Presented By: Ederlyn Papa-Destura, RN, ManteuuuuAinda não há avaliações
- Breathe OlogyDocumento59 páginasBreathe OlogyPere Ureña Bartrina73% (22)
- Sexual QigongDocumento3 páginasSexual Qigongfahim100% (1)
- Attachment Theory Lesson and HandoutDocumento29 páginasAttachment Theory Lesson and Handoutguptaamrit100% (1)
- Integrated DM Care - Multidisciplinary ApproachDocumento257 páginasIntegrated DM Care - Multidisciplinary ApproachJacob Dougherty100% (1)
- Review Mcqs For 2016 Systemic PathologyDocumento8 páginasReview Mcqs For 2016 Systemic PathologySameer100% (1)
- AETCOM 1.1 What Does It Mean To Be A DoctorDocumento7 páginasAETCOM 1.1 What Does It Mean To Be A DoctorDev Malav100% (1)
- Uses of EpidemiologyDocumento28 páginasUses of EpidemiologyBinita Shakya0% (1)
- Ecmo and Life Support Systems Quadrox Pls and Rotaflow Hardware and AccessoriesDocumento10 páginasEcmo and Life Support Systems Quadrox Pls and Rotaflow Hardware and AccessoriesManigandan DhamodhiranAinda não há avaliações
- SWOT ANALYSIS ApolloDocumento3 páginasSWOT ANALYSIS ApolloSudhir PawarAinda não há avaliações
- The Worldwide Economic Impact of Dementia 2010Documento14 páginasThe Worldwide Economic Impact of Dementia 2010Andreia Polido de AlmeidaAinda não há avaliações
- Socioeconomic Status and NCDDocumento13 páginasSocioeconomic Status and NCDARVIN ZUBIAGAAinda não há avaliações
- Beyond Tuberculosis A Person-Centred and Rights-BasedDocumento7 páginasBeyond Tuberculosis A Person-Centred and Rights-BasedFilebar MohammedAinda não há avaliações
- NIDDK International Conference Report On Diabetes and Depression: Current Understanding and Future DirectionsDocumento11 páginasNIDDK International Conference Report On Diabetes and Depression: Current Understanding and Future Directionsyeremias setyawanAinda não há avaliações
- Health Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesDocumento9 páginasHealth Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesgamzeAinda não há avaliações
- Health in ContextDocumento1 páginaHealth in ContextvvvAinda não há avaliações
- Perspectives of Nursing in The Care of The Patient With Diabetes MellitusDocumento7 páginasPerspectives of Nursing in The Care of The Patient With Diabetes MellitusSammy OhAinda não há avaliações
- Primer: MultimorbidityDocumento22 páginasPrimer: MultimorbidityGUSTAVO VERA REALAinda não há avaliações
- NCD View Point 3Documento3 páginasNCD View Point 3upashana medhiAinda não há avaliações
- Depresión 6Documento8 páginasDepresión 6MarianneAinda não há avaliações
- Evaluation of Depression and Coping Skill Among HIV-Positive People in Kolkata, IndiaDocumento6 páginasEvaluation of Depression and Coping Skill Among HIV-Positive People in Kolkata, IndiaAFINA AZIZAHAinda não há avaliações
- Rethinking Diabetes: Entanglements with Trauma, Poverty, and HIVNo EverandRethinking Diabetes: Entanglements with Trauma, Poverty, and HIVAinda não há avaliações
- Multimorbidity Primer NatureDocumento22 páginasMultimorbidity Primer Natureangie saenzAinda não há avaliações
- 2019-Emociones Pensamientos Experiencias en DM PDFDocumento9 páginas2019-Emociones Pensamientos Experiencias en DM PDFPsico AstralAinda não há avaliações
- Priorities, 3rd Edition: ReviewDocumento14 páginasPriorities, 3rd Edition: ReviewNatasha AlbaShakiraAinda não há avaliações
- NCD and NutritionDocumento14 páginasNCD and NutritionPradip kumar yadavAinda não há avaliações
- JoWC - 2022 - 31 - 11 - 000 - Da Fonseca Cerqueira 221020 BC 2Documento14 páginasJoWC - 2022 - 31 - 11 - 000 - Da Fonseca Cerqueira 221020 BC 2HelenaAinda não há avaliações
- Pmed 1001443Documento5 páginasPmed 1001443misterchemitaAinda não há avaliações
- Preventing The Onset of Depressive Disorders in Low and Middle Income Countries An OverviewDocumento6 páginasPreventing The Onset of Depressive Disorders in Low and Middle Income Countries An OverviewDarien Alfa CiptaAinda não há avaliações
- A Cross-Sectional Analysis ofDocumento17 páginasA Cross-Sectional Analysis ofYayat VieriAinda não há avaliações
- Management and Education in Patients With Diabetes Mellitus PDFDocumento7 páginasManagement and Education in Patients With Diabetes Mellitus PDFhartatiAinda não há avaliações
- JPM 12 00643Documento12 páginasJPM 12 00643dw21541Ainda não há avaliações
- Format PengkajianDocumento8 páginasFormat PengkajianHandiniAinda não há avaliações
- The "A To Z" of Managing Type 2 Diabetes in Culturally Diverse PopulationsDocumento15 páginasThe "A To Z" of Managing Type 2 Diabetes in Culturally Diverse PopulationsWilber CarrascoAinda não há avaliações
- No 5Documento2 páginasNo 5georgechris12eAinda não há avaliações
- Ajol File Journals - 414 - Articles - 232278 - Submission - Proof - 232278 4933 563181 1 10 20220921Documento14 páginasAjol File Journals - 414 - Articles - 232278 - Submission - Proof - 232278 4933 563181 1 10 20220921alkinhamisiAinda não há avaliações
- 1 s2.0 S0165032717320232 MainDocumento7 páginas1 s2.0 S0165032717320232 MainMiguel DebonoAinda não há avaliações
- Concept of Non Communicable Diseases - NCDEDocumento7 páginasConcept of Non Communicable Diseases - NCDEFirly Azra GhassanieAinda não há avaliações
- Prevalence of Metabolic Syndrome Among An Urban Population in KenyaDocumento7 páginasPrevalence of Metabolic Syndrome Among An Urban Population in KenyaMutia UlfaAinda não há avaliações
- Ijhpm 5 619 PDFDocumento4 páginasIjhpm 5 619 PDFBaoz PingAinda não há avaliações
- Akhter - Influences of Social Issues On Type 1 Diabetes Self Management Are We Doing EnoughDocumento7 páginasAkhter - Influences of Social Issues On Type 1 Diabetes Self Management Are We Doing EnoughAlexandraAinda não há avaliações
- The INtegrating DEPrEssioN and Diabetes treatmENTDocumento27 páginasThe INtegrating DEPrEssioN and Diabetes treatmENTAnita Chandra KusumaAinda não há avaliações
- Good Paper KAP Cut Off Two LevelsDocumento18 páginasGood Paper KAP Cut Off Two LevelsSiti Hadijah Aspan, M.PHAinda não há avaliações
- 2014 - Public Health and Clinical Health DifferencesDocumento3 páginas2014 - Public Health and Clinical Health DifferencesEric AryeepahAinda não há avaliações
- 2018 - Caderno de Textos Oficina (04-10)Documento7 páginas2018 - Caderno de Textos Oficina (04-10)Carla SantosAinda não há avaliações
- Global Dimensions of Diabetes Information and Syn 2015 Annals of Global HeaDocumento2 páginasGlobal Dimensions of Diabetes Information and Syn 2015 Annals of Global HeaarmanAinda não há avaliações
- States With Genetic Disorders Models of Comprehensive Multidisciplinary Care For Individuals in The UnitedDocumento8 páginasStates With Genetic Disorders Models of Comprehensive Multidisciplinary Care For Individuals in The UnitedRita SofiaAinda não há avaliações
- Poverty Increases Type 2 Diabetes Incidence and Inequality of Care Despite Universal Health CoverageDocumento7 páginasPoverty Increases Type 2 Diabetes Incidence and Inequality of Care Despite Universal Health CoverageHitmanAinda não há avaliações
- SantosSalas2019 SocialDisparitiesDocumento12 páginasSantosSalas2019 SocialDisparitiesAdriana VargasAinda não há avaliações
- Global, National, and Local Approaches To Mental Health: Examples From IndiaDocumento20 páginasGlobal, National, and Local Approaches To Mental Health: Examples From Indiaujangketul62Ainda não há avaliações
- Geriatrics: Memory and Learning Complaints in Relation To Depression Among Elderly People With MultimorbidityDocumento9 páginasGeriatrics: Memory and Learning Complaints in Relation To Depression Among Elderly People With MultimorbidityPutri AyuningtyasAinda não há avaliações
- NCD in Poor CountriesDocumento6 páginasNCD in Poor CountriesjmbobitAinda não há avaliações
- Lep266 282Documento17 páginasLep266 282Hasana NurAinda não há avaliações
- Strengthening The Quality Agenda in Health Care in Low-And Middle-Income Countries: Questions To ConsiderDocumento5 páginasStrengthening The Quality Agenda in Health Care in Low-And Middle-Income Countries: Questions To ConsiderJose RamirezAinda não há avaliações
- Journal #1Documento30 páginasJournal #1p.nicaalexandriaAinda não há avaliações
- Healthframework PaperDocumento9 páginasHealthframework Paperapi-449184986Ainda não há avaliações
- Medical SociologyDocumento25 páginasMedical SociologyHajra MirzaAinda não há avaliações
- Diabetes and Mental HealthDocumento3 páginasDiabetes and Mental HealthVENNA FADILLAHAinda não há avaliações
- Understanding Psychological Symptoms of Endometriosis From A Research Domain Criteria PerspectiveDocumento14 páginasUnderstanding Psychological Symptoms of Endometriosis From A Research Domain Criteria PerspectiveSamar HamadyAinda não há avaliações
- 2015 - in - Is Dengue A Disease of PovertyDocumento9 páginas2015 - in - Is Dengue A Disease of PovertyAwal IkhwaniAinda não há avaliações
- Dengue in CambodiaDocumento10 páginasDengue in CambodiaRobert BennettAinda não há avaliações
- IMPO - Sequeira - Adolescent Health Series The Status of Adolescent Mental Health ResearchDocumento9 páginasIMPO - Sequeira - Adolescent Health Series The Status of Adolescent Mental Health ResearchEffortAinda não há avaliações
- Journal Homepage: - : IntroductionDocumento8 páginasJournal Homepage: - : IntroductionIJAR JOURNALAinda não há avaliações
- Evidence-Based Psycho-Oncology: A Priority in Mental Health: EditorialDocumento2 páginasEvidence-Based Psycho-Oncology: A Priority in Mental Health: EditorialGrace LAinda não há avaliações
- NCM 112 Week 2 Journal ReadingDocumento4 páginasNCM 112 Week 2 Journal ReadingBrandy JaffarAinda não há avaliações
- Etnografi Jurnal - Riset KualitatifDocumento16 páginasEtnografi Jurnal - Riset KualitatifRasymiAinda não há avaliações
- The Role of Diet and Nutrition On Mental Health and WellbeingDocumento3 páginasThe Role of Diet and Nutrition On Mental Health and WellbeingMeha RajAinda não há avaliações
- Survival KitDocumento2 páginasSurvival KitDump KsksAinda não há avaliações
- GNM Practical Book 12.12.13 PDFDocumento54 páginasGNM Practical Book 12.12.13 PDFHimachal BagdiAinda não há avaliações
- WorldAlzheimerReport2019 Spanish SummaryDocumento13 páginasWorldAlzheimerReport2019 Spanish SummaryFonoaudiólogos En cuidado crítico ColombiaAinda não há avaliações
- The EFQM Excellence Model European and Dutch ExperDocumento12 páginasThe EFQM Excellence Model European and Dutch Experifa pannyaAinda não há avaliações
- MCM Youth E-Nnovation Summit (MCM YES)Documento6 páginasMCM Youth E-Nnovation Summit (MCM YES)z permruruAinda não há avaliações
- Care Delivery Models and Staffing: Fidela B. Ansale, R.N., Doctor of Science in NursingDocumento25 páginasCare Delivery Models and Staffing: Fidela B. Ansale, R.N., Doctor of Science in NursingAliah BataloAinda não há avaliações
- Assistant Housekeeper/ Housekeeping ManagerDocumento5 páginasAssistant Housekeeper/ Housekeeping ManagerRuizo ElisabethAinda não há avaliações
- STI Guidelines 2021Documento192 páginasSTI Guidelines 2021Carlos QuirozAinda não há avaliações
- A Quantitative Study About Time Management and Its Relation To Procrastination Among Senior High School Students of Our Lady of Fatima UniversityDocumento20 páginasA Quantitative Study About Time Management and Its Relation To Procrastination Among Senior High School Students of Our Lady of Fatima UniversityClaire GonoAinda não há avaliações
- The Importance of Sports For Students: Need Help With The Assignment?Documento1 páginaThe Importance of Sports For Students: Need Help With The Assignment?Mayank MotwaniAinda não há avaliações
- DIS Project Proforma 2015 PDFDocumento7 páginasDIS Project Proforma 2015 PDFVidyesh Nair100% (2)
- History of Psychological AssessmentDocumento3 páginasHistory of Psychological AssessmentAbrar AhmadAinda não há avaliações
- Krok 1 Stomatology 2006Documento21 páginasKrok 1 Stomatology 2006helloAinda não há avaliações
- Nutrition FactsDocumento3 páginasNutrition FactsMARIELLE LOUISE JAMON ANDRADEAinda não há avaliações
- Paper 1 Practice - News ReportDocumento4 páginasPaper 1 Practice - News Reportbreanna erylleAinda não há avaliações
- Drew Leder, AnorexiaDocumento5 páginasDrew Leder, AnorexiasaffaroAinda não há avaliações
- Australian Dental Journal: Sugary Drink Consumption and Dental Caries in New South Wales TeenagersDocumento7 páginasAustralian Dental Journal: Sugary Drink Consumption and Dental Caries in New South Wales TeenagersRega RegiawanAinda não há avaliações
- Superiority Inferiority ComplexDocumento9 páginasSuperiority Inferiority ComplexAyesha AkbarAinda não há avaliações
- Appendix: The Scales Scale of Positive and Negative Experience (SPANE)Documento2 páginasAppendix: The Scales Scale of Positive and Negative Experience (SPANE)shekhy123Ainda não há avaliações
- Biological Activities of Crude Extracts and Chemical Constituents of Aegle MarmelosDocumento13 páginasBiological Activities of Crude Extracts and Chemical Constituents of Aegle MarmeloskavalapparaAinda não há avaliações
- SSC Home Learning Plan Week 4Documento9 páginasSSC Home Learning Plan Week 4Dangay National High SchoolAinda não há avaliações
- PVA Risk Guide: A Guide To Improving The SafetyDocumento34 páginasPVA Risk Guide: A Guide To Improving The SafetyHashem GamAinda não há avaliações