Escolar Documentos
Profissional Documentos
Cultura Documentos
2013-11-25 S Nechvatal CSM - 2014 - Handouts
Enviado por
J Roberto Meza OntiverosDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
2013-11-25 S Nechvatal CSM - 2014 - Handouts
Enviado por
J Roberto Meza OntiverosDireitos autorais:
Formatos disponíveis
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
PHYSICAL THERAPY IN THE
St. Marys Hospital
EMERGENCY DEPARTMENT: HOW TO
START AND SUSTAIN A SUCCESSFUL
EMERGENCY CARE PT SERVICE Part of SSM Healthcare based in St. Louis
320 beds
COMBINED SECTIONS MEETING 2014
Medicare Accountable Care Organization (ACO)
F E B R U A R Y 3 RD- 6 TH, 2 0 1 4 L A S V E G A S , N E V A D A partnered with Dean Clinics
EHR Epic
T U E S D A Y , F E B R U A R Y 4 TH, 2 0 1 4
Physicians contracted through Dean Clinics (except
8:00 AM 10:00 AM
for ED physicians)
SARAH NECHVATAL, PT, DPT
ST. MARYS HOSPITAL MADISON, WISCONSIN
Course Description St. Marys Hospital Emergency Services
1. Describe the development of the PT consultation Average door to doc time is 14 minutes
service in the St. Marys Hospital ED. Bedside registration
2. Review the process and outcome measures of the pilot
Hospital Campus Emergency Department
year of the St. Marys Hospital PT ED project.
Level III trauma center
3. Provide evidence of value of PT in the ED. 29 beds
4. Review which diagnoses and populations are Unit based medical imaging
commonly seen in the ED. St. Marys Sun Prairie Emergency Center
5. Suggest what tools and skills are needed to be an ED Level IV trauma center
PT. 10 beds
6. Offer suggestions on how to start your own PT Laboratory, radiology and helicopter transport
consultation service in your ED. Staffed by Madison Emergency Physicians
Course Objectives St. Marys Hospital Physical Therapy
Upon completion of this course, participants will be 12-13 PT/PTAs on each day (6 Saturday/5 Sunday)
able to: Hours of PT availability 8:30-4:00
1. Explain how PT can add value to an ED. Patients are scheduled in EPIC by Administrative Assistant
2. Collect data before and after implementation of PT Monthly caseload rotations
Pulmonary
in the ED to justify the value of the service.
Neuro
3. Establish a successful ED PT consultation service. Cardiac
4. Sustain a successful ED PT consultation service. Medsurg
Oncology
Ortho
Float
Property of Sarah Nechvatal, not to be
copied without permission. 1
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
ED PT Care Pathway PT Diagnoses
1. ED PT on Float caseload evals only Back pain (acute or chronic)
2. ED staff identifies appropriate patient Limb pain
3. Enters PT referral in EPIC and calls Float cell Non-surgical fractures
phone to give info
Non-cardiac chest pain
4. PT calls administrative assistant to reschedule
next patient on float load Falls
5. PT arrives within 20 minutes Gait instability
6. PT eval and treat <60 minutes Failure to thrive
7. Coordinate with RN, Physician/PA, Care Vertigo/vestibular dysfunction
Management for D/C planning
Care Management A typical ED visit
Relationship between Care Management and PT is
Triage
vital MD assessment
Medications
Cyndi Benson-Lein, RN Case Manager Imaging (if necessary)
Need for increased Care Management presence in
the ED
Responsible for utilization management
Hospital Admission
Decreasing unnecessary admissions Discharge from ED
Unable to mobilize
Referral back to PCP
Unable to manage symptoms
Finding medical necessity before inpatient admission Referral to outpatient PT with the
OPO stay or potential conversion
symptom as the diagnosis
to inpatient status
Who comes to the ED? What if we could
True emergencies Decrease unnecessary admissions
Losing life
Losing limb(Wilsey et al, 2008) Decrease re-admissions or re-visits to the ED for
Perceived emergencies same diagnosis
~85% of ED patients have non-life threatening injuries(Padgett & Better manage symptoms in the ED
Brodsky,1992)
~11% of ED patients have chronic pain as their C/C (Cordell et al, 2002) Improve patient satisfaction in the ED
Patients with pain feel the need to have objective results to justify
their symptoms (Wilsey et al, 2008) Decreased unnecessary outpatient PCP visits
Frequent visitors Decrease the length of time between ED visit and
Re-admissions or re-visits outpatient PT visit
Use of ED as primary care Decrease time between ED visit and home health
Convenience users services introduction
Property of Sarah Nechvatal, not to be
copied without permission. 2
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
Project Background Implementation Steps
Opportunity: To practice exceptional stewardship 1. Update the rehab director
by providing the appropriate level of care for our
2. Discuss with PT colleagues
patients in the ED
3. Identify lead PT and a few substitutes
1. Return visits to the Emergency Department (ED) for unresolved 4. Create steering team of stakeholders
symptoms 1. Sarah Nechvatal, PT
2. Extended observation stays 2. Cyndi Benson-Lein, Lead RN Case Manager
3. Inappropriate admissions to hospital 3. Nancy Rung, Rehab Director
4. Theresa Ojala, ED Director
Identifies opportunities for Physical Therapy (PT) and Case 5. Anthony Callisto, MD Medical Director of ED
Management (CM) in the ED 6. Sheryl Krause, RN, Emergency Medicine CNS
7. Deb Dees, ED RN
Implementation Steps
5. Developed care pathway
6. Presentation to the ED physician group
- Pathway
- Narcotics education
7. Presentation to the ED Nursing staff
- Pathway
- Narcotics education
8. Presentations to Rehab and Care Management
Prepared by: 9. Meeting with community resources
- Area outpatient PT clinics and clinic directors
Cyndi Benson-Lein, RN Case Manager - Home health agency schedulers
Sarah Nechvatal, DPT, Physical Therapist 10. Go Live! on November 1, 2010
Goals ED PT Care Pathway
1. Decrease number of observation patients within 1. ED PT on Float caseload evals only
our selected population by 10% over 6 months. 2. ED staff identifies appropriate patient
3. Enters PT referral in EPIC and calls Float cell
2. Decrease observation length of stay within our
phone to give info
selected population by an average of 12 hours over 4. PT calls administrative assistant to reschedule
6 months. next patient on float load
5. PT arrives within 20 minutes
6. PT eval and treat <60 minutes
3. Decrease return visits to the ED within 5 days for
7. Coordinate with RN, Physician/PA, Care
same complaint by 10% over 6 months. Management for D/C planning
Property of Sarah Nechvatal, not to be
copied without permission. 3
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
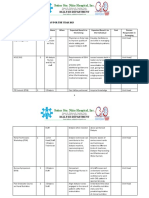
Implementation Steps Process Measures
5. Developed care pathway Number of Emergency Department Referrals
During the First Year
6. Presentation to the ED physician group 25
- Pathway 21
20 20
- Narcotics education 20 19
18
17
7. Presentation to the ED Nursing staff 15
16 16 16
- Pathway 15
- Narcotics education ED Referrals
10
8. Presentations to Rehab and Care Management 7 7
9. Meeting with community resources 5
- Area outpatient PT clinics and clinic directors
- Home health agency schedulers 0
Nov Dec Jan Feb March April May June July Aug Sept Oct
10. Go Live! on November 1, 2010
Process Measures Outcome Measures
Number of Emergency Department Referrals Number of Observation Patients within our Selected
During the First Year Patient Population that were admitted through the ED
8 70
7 63
7 60
58 57
6 50 51 52 51 51
49 49 49
47
5 45
43 42 41
43 44
42 41
40
37
4 ED Referrals 35 36
30 31 Previous Year
3 26 Pilot Year
20
2
1 10
0 0
Nov Dec Jan Feb March April May June July Aug Sept Oct
Changes After 1st Month Outcome Measures
Dr. Bell new consultation service Average Observation Length of Stay within our Selected
Be present. Patient Population in Days
Be seen.
Trimmed mean= 1.22
Get in with the nurses.
Dizziness 1.78
Documented in the ED during down time 1.23
Introduced myself to everyone I didnt recognize
Talked with the nursing staff Limb Pain 1.34
Trimmed mean for Pilot
Pilot Year
Made reminder signs for the walls @ each ED phone 1.53 Previous Year
Invited nursing staff into my sessions
Empowering the hospitalists Back Pain 1.42
1.51
Making believersone at a time (Hold the Bucket)
0.00 0.20 0.40 0.60 0.80 1.00 1.20 1.40 1.60 1.80 2.00
Property of Sarah Nechvatal, not to be
copied without permission. 4
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
A Review Lesson on Averages Outcome Measures
3 + 4 + 4 + 26 + 24 + 30 = 91
PT Qualifying Patients Who Return to the ED within 5 days and ED
Patients who are Admitted within 5 days of ED Visit with Same Complaint
12
916 = 15.17 hours 10 10
7 7 7 7
Axis Title
6 6
Previous Year
5
Pilot Year
4 4 4
3 3 3 3
2 2 2
1 1 1 1 1 1
0 0
A Review Lesson on Averages Process Measures
3 + 4 + 4 + 26 + 24 + 30 = 91 35
Number of PT Referrals Throughout the Day
32
916 = 15.17 hours 30 28 29
25 23 23
20 18
3 + 4 + 4 + 26 + 24 + 30 = 80 15 14
17
PT Referrals
803 = 26.67 hours 10
0
8:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00
Outcome Measures ED Volume per Hour of Day
Average Observation Length of Stay within our Selected
Patient Population in Days
Trimmed mean= 1.22
Dizziness 1.78
1.23
Trimmed mean for Pilot
Limb Pain 1.34
Pilot Year
1.53 Previous Year
Back Pain 1.42
1.51
0.00 0.20 0.40 0.60 0.80 1.00 1.20 1.40 1.60 1.80 2.00
Property of Sarah Nechvatal, not to be
copied without permission. 5
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
ED Volume per Day of Week Process Measures
Discharge Disposition from ED after PT
6.50% 3% 0.50%
11% Home
Inpatient
Observation
SNF
ALF
79%
Process Measures Process Measures
Call to Contact Time Home Services after Discharge Home from ED
Expectation: 20 minutes 50%
45% 43%
Expectation achieved: 80% 40%
35%
Average: 16 minutes and 36 seconds 30% 28%
24%
25%
Treatment Time 20% 18%
Expectation: 60 minutes
15%
10% Percentage of Services
Expectation achieved: 89% 5%
0%
Average: 45 minutes and 12 seconds
Process Measures Process Measures
Chief Complaint Payor
3% 3%
4%
9
13 Medicare
Back Pain 11% Dean
74 Limb Pain Self Pay
40 Falls/Gait Instability
49%
Medicaid/BadgerCare
14% WPS
Vertigo/Dizziness
Misc Worker's Comp
Other insurance
52 16%
Property of Sarah Nechvatal, not to be
copied without permission. 6
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
Lessons Learned Tracking Return Visits
1. Make SMART goals after collecting data. Same ICD-9 codes
Specific, Measurable, Attainable, Realistic and Timely Runs a Re-Admission report (within 5 days)
2. Data collection always takes longer than expected. Return visits: ED visit, D/C from ED, return to ED
Admitted within 5 days: ED visit, D/C from ED, then is admitted
3. Educate the hospitalist group before to hospital (through ED or direct admit from outpatient)
implementation. Chart Audits to see who could have benefitted from
4. Do a full year for the pilot. PT during the first visit to prevent second visit
Include ICD-9 codes in both primary and secondary
5. Conduct a study group for PTs to review vestibular diagnoses
and musculoskeletal exam and treatment so that more Back pain primary diagnosis both visits
PTs feel comfortable in that role Fall with leg pain, return with gait instability primary, secondary
Fracture then readmitted for surgery 3 days later
Collecting Outcome Measures
Connect with your ED data analyst (a.k.a. CQI,
information systems)
Data analysts track re-admits or re-visits
Trendstar (billing tool) and HDM are commonly
used programs
We now use Epic instead of HDM
Trendstar has a 1-2 month lag
Connect with medical record ICD-9 coders to
identify ICD-9 codes
Observation Patients: Number & LOS Why Didnt We
Observation charge code (instead of inpatient) Track for the post-pilot year?
Too time consuming to do chart audits
Actual vs Billed time Other variables were introduced that could affect these outcomes
Actual time is the whole time they are Audit charts of patient who returned within 30 days?
observation Too time consuming to do chart audits for that many patients
Would PT intervention one day prevent a return visit to the ED 3
Billed time deducts procedures and weeks later? Probably not.
consultations Track patient satisfaction?
Only included patients who were observation the We didnt think we could do a before and after since the current
practice is randomly survey patients with random diagnoses
whole time St. Josephs Carondelet tracked 80% of patients were satisfied
with the PT service. (Woods, 2000)
Property of Sarah Nechvatal, not to be
copied without permission. 7
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
Skills and Character Traits Needed Value of PT in the ED
Musculoskeletal exam Enthusiastic PTs are less likely to miss significant knee injury and can
Manual therapy Confident deliver the diagnostic service more cost effectively than
Joint mobs senior house officers(Jibuike et al, 2003)
Active learner
Soft tissue work Patients with acute LBP, with or without referred leg
Flexible pain, had statistically significant reduction in pain and
Modalities increased satisfaction with PT intervention when
Time management
Vestibular assessment compared to control group who received walking training
Lead PT and walking aids only(Lau et al, 2008)
G Code expertise Persistent
Extended scope physiotherapists (ESP) achieve higher
Ability to communicate Good salesperson patient satisfaction with assessment/treatment of
the proper series of events Diplomatic peripheral soft tissue injuries and associated fractures
for a musculoskeletal compared to physicians and emergency nurse
condition practitioners (McClellan et al, 2006)
Resources Needed Value of PT in the ED
High-low table (ED beds) ED physicians perceive PT has value due to increasing the
US/E-stim machine scope of their management options for musculoskeletal
Access to ice and heat modalities pain (an alternative for narcotic use), vestibular
Massage cream
impairments and evaluating mobility of potentially unsafe
patients. Physicians perceive that PTs have reduced their
Exercise library and patient education handouts (ie.
Exercise Pro) workload (Lebec et al, 2010)
Gait belts
Access to stairs/curb step Barnes-Jewish Hospital in St. Louis surveyed ED personnel
DME: crutches, 2ww, youth 2ww, 4ww with seat, who report satisfaction with the PTs management of
standard walker, platform attachments for walker and musculoskeletal pain, contribution to differential diagnosis,
crutches, straight cane, quad cane, manual w/c and discharge recommendations (Fleming-McDonnell et al, 2010)
What does the future hold? Less Money Lost in the ED?
Keep the conversation going with stakeholders Traditional ED care with physician assessment, tests,
Direct Access medications, nursing staff is billed as thousands of
EMTALA (Emergency Medical Treatment and Labor Act) dollars
The right care, the right place (sort of), at the right time The reimbursement does not cover the actual cost
Potential to prevent chronic progression and its high associated
and therefore the ED is a money loser
costs (Lebec & Jogodka, 2009)
PT practices relatively independently cost is mostly
Proving value of PT in the ED
Cost effective care
just PT wages and supplies used during
Increased patient satisfaction treatment(Lebec & Jogodka, 2009)
Improved clinical outcomes
Property of Sarah Nechvatal, not to be
copied without permission. 8
Physical Therapy in the Emergency 11/25/2013
Department: How to Start and Sustain a
Successful Emergency Care PT Service
Where to Start? References
1. Identify lead PT, lead Case Manager and a few substitutes Lebec MT, et al. Emergency department physical therapist
2. Identify stakeholders and start the conversation service: A pilot study examining physician perceptions. The
3. Identify what is important to that individual role (ie. Internet Journal of Allied Health Sciences and Practice.
Administrator) 2010;8(1):1-12.
How will this help the system? Lebec MT, Jogodka CE. The physical therapist as a
How will this affect FTEs? musculoskeletal specialist in the emergency department.
Will this prevent readmissions? Journal of Orthopaedic & Sports Physical Therapy.
Will this increase our outpatient PT referrals? (Is there 2009;39(3):221-9.
opportunity for downstream revenue?)
McClellan CM, Greenwood R, Benger JR. Effect of an extended
How will this affect staff satisfaction?
scope physiotherapy service on patient satisfaction and the
How will this affect patient satisfaction?
outcome of soft tissue injuries in an adult emergency
4. Meet with data analyst and collect data on whats important
department. Emergency Medicine Journal. 2006;23:384-7.
5. Create goals
Where to Start? References
6. Create your steering team Padgett DK, Brodsky B. Psychosocial factors influencing non-
Lead PT, Case Manager (Social Worker or RN Case Manager), ED
RN, ED physician, ED nursing director, & Rehab Director urgent use of the emergency room: a review of the literature and
7. Create care pathway recommendations for research and improved service delivery.
8. Educate stakeholder groups (pathway & what is important to them) Social Science Medicine. 1992;35(9):1189-97.
ED physicians
Wilsey BL, Fishman SM, Ogden C, et al. Chronic pain
ED nursing
Hospitalists/Internal Medicine
management in the emergency department: a survey of attitudes
Rehab department
and beliefs. Pain Medicine. 2008;9:1073-80.
Care Management department Woods EN. The emergency department: a new opportunity for
Community Resources (home health, outpatient clinics, etc) physical therapy. PT: Magazine of Physical Therapy.
Administration
2000;8(9):42-8.
9. Gather equipment and resources
10. 1 year for pilot period
11. Keep the conversation going with regular meetings/updates with
stakeholders and ask for their feedback
References Questions?
Cordell WH, Keene KK, Giles BK, et al. The high prevalence of pain in sarahnechvatal@gmail.com
emergency medical care. American Journal of Emergency Medicine.
2002;20(3):165-9.
Fleming-McDonnell D, et al. Physical therapy in the emergency
department: development of a novel practice venue. Physical Therapy.
2010;90(3):420-6.
Jibuike OO, Paul-Taylor G, Maulvi S, et al. Management of soft tissue
knee injuries in an accident and emergency department: the effect of
the introduction of a physiotherapy practitioner. Emergency Medicine
Journal. 2003;20:37-9.
Lau PM, Chow DH, Pope MH. Early physiotherapy intervention in an
Accident and Emergency department reduces pain and improves
satisfaction for patients with acute low back pain: a randomised trial.
Australian Journal of Physiotherapy. 2008;54:243-9.
Property of Sarah Nechvatal, not to be
copied without permission. 9
Você também pode gostar
- Emergency Orthopedics HandbookNo EverandEmergency Orthopedics HandbookDaniel PurcellAinda não há avaliações
- General Surgery Resident HandbookDocumento32 páginasGeneral Surgery Resident Handbookprekos 65Ainda não há avaliações
- WS Pengelolaan Asuhan Pasien Di IGDDocumento56 páginasWS Pengelolaan Asuhan Pasien Di IGDisni maftuhahAinda não há avaliações
- Clinical JudgementDocumento6 páginasClinical Judgementapi-664535132Ainda não há avaliações
- LampiranDocumento9 páginasLampiranNYONGKERAinda não há avaliações
- Efficacy-Of-Early-Passive-Tilting-In-Minimizing-Icuacquired-Weak-2018 MarceDocumento29 páginasEfficacy-Of-Early-Passive-Tilting-In-Minimizing-Icuacquired-Weak-2018 MarcebastianAinda não há avaliações
- Asuhan Keperawatan Pasien Di Instalasi Gawat Darurat: Sri Purwaningsih, SKP, MkesDocumento56 páginasAsuhan Keperawatan Pasien Di Instalasi Gawat Darurat: Sri Purwaningsih, SKP, MkesAnonymous 2TVrNDPgSAinda não há avaliações
- Emergency TriageDocumento3 páginasEmergency Triagepinutttttt100% (1)
- English 105 "Dietary Program To Diabetus Melitus": Academic: I'IN NOVIANA M.PDDocumento14 páginasEnglish 105 "Dietary Program To Diabetus Melitus": Academic: I'IN NOVIANA M.PDayuAinda não há avaliações
- Issue 30 - The Nurse Advocate - Hamad Medical Corporation - December 2017Documento20 páginasIssue 30 - The Nurse Advocate - Hamad Medical Corporation - December 2017Brent ForemanAinda não há avaliações
- PICU NICU OrientationDocumento8 páginasPICU NICU OrientationSony PrabowoAinda não há avaliações
- Emergency DepartmentDocumento9 páginasEmergency DepartmentSarah Mae SanchezAinda não há avaliações
- Triage PDFDocumento7 páginasTriage PDFAnonymous nEQNlgbYQCAinda não há avaliações
- International Emergency Nursing: SciencedirectDocumento24 páginasInternational Emergency Nursing: SciencedirectRazak AbdullahAinda não há avaliações
- A Room With A View On Call Specialist Panels andDocumento4 páginasA Room With A View On Call Specialist Panels andAGGREY DUDUAinda não há avaliações
- Comparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GDocumento14 páginasComparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GIJAR JOURNALAinda não há avaliações
- Can Physiotherapists Contribute To Care in The Emergency Department?Documento3 páginasCan Physiotherapists Contribute To Care in The Emergency Department?J Roberto Meza OntiverosAinda não há avaliações
- 3 15 2021 Clinical Nuring JudgementDocumento6 páginas3 15 2021 Clinical Nuring Judgementapi-543808198Ainda não há avaliações
- 21 Contemporary Pediatric Cardiovascular NursingDocumento7 páginas21 Contemporary Pediatric Cardiovascular NursingVictor PazAinda não há avaliações
- Capstone PaperDocumento5 páginasCapstone Paperapi-453431426Ainda não há avaliações
- Preceptorship 2019 NursalamDocumento147 páginasPreceptorship 2019 NursalamSTIKES Katolik St. Vincentius a Paulo100% (2)
- Research Report: The Physical Function Intensive Care Test: Implementation in Survivors of Critical IllnessDocumento9 páginasResearch Report: The Physical Function Intensive Care Test: Implementation in Survivors of Critical IllnessPamela DíazAinda não há avaliações
- The Digital Rectal ExaminationDocumento2 páginasThe Digital Rectal ExaminationGabriela GalvezAinda não há avaliações
- Bringing TO Healthcare: Private LimitedDocumento21 páginasBringing TO Healthcare: Private LimitedAmit ShrivastavaAinda não há avaliações
- Annie Elizabeth ResumeeDocumento1 páginaAnnie Elizabeth ResumeeLizAinda não há avaliações
- Portofolio 2 Maulidiyah SafitriDocumento2 páginasPortofolio 2 Maulidiyah Safitrimaulidiyah safitriAinda não há avaliações
- StaffingDocumento39 páginasStaffingCharlotte T. BorjaAinda não há avaliações
- Joseph POCDocumento16 páginasJoseph POCAdeboye josephAinda não há avaliações
- Thomas 2015Documento7 páginasThomas 2015Gisele Elise MeninAinda não há avaliações
- Staff Development Plan 2023Documento5 páginasStaff Development Plan 2023SSNHI Dialysis Training CenterAinda não há avaliações
- 2012 FSJT 30 Questions Practice PaperDocumento34 páginas2012 FSJT 30 Questions Practice Papermimoadel.maAinda não há avaliações
- Clinical Nursing JudgementDocumento5 páginasClinical Nursing Judgementapi-403115643Ainda não há avaliações
- Intensive CareDocumento28 páginasIntensive CareEldo Kancil100% (1)
- Bristol Pain DocumentDocumento79 páginasBristol Pain DocumentRohit BharadwajAinda não há avaliações
- Roberto Padlan (Resume)Documento5 páginasRoberto Padlan (Resume)Merian PadlanAinda não há avaliações
- 422 PaperDocumento8 páginas422 Paperapi-384505435Ainda não há avaliações
- Scholarly Paper - Senior CapstoneDocumento6 páginasScholarly Paper - Senior Capstoneapi-545895101Ainda não há avaliações
- My ResearchsDocumento2 páginasMy ResearchsNigel KorokaAinda não há avaliações
- R0111 - Experiências de Enfermeiros de Emergência Pré-Hospitalar em Incidentes Críticos - 2020Documento6 páginasR0111 - Experiências de Enfermeiros de Emergência Pré-Hospitalar em Incidentes Críticos - 2020Sky WingsAinda não há avaliações
- Scholarly PaperDocumento5 páginasScholarly Paperapi-661467979Ainda não há avaliações
- Tintu Jones Karedan - 121534968Documento5 páginasTintu Jones Karedan - 121534968Mumtaj AnsariAinda não há avaliações
- Resume-Preetha JoseDocumento7 páginasResume-Preetha Joseapi-551188095Ainda não há avaliações
- Frontline Nurses' Clinical Judgment in Recognizing, Understanding, andDocumento11 páginasFrontline Nurses' Clinical Judgment in Recognizing, Understanding, andPaulaAinda não há avaliações
- Nejmp 1215594Documento4 páginasNejmp 1215594Cj AlmazanAinda não há avaliações
- Itls 9th Edition Prep Packet Advanced Provider VersionDocumento19 páginasItls 9th Edition Prep Packet Advanced Provider VersionUmidagha BaghirzadaAinda não há avaliações
- Issue 28 - The Nurse Advocate - Hamad Medical Corporation - February 2017Documento20 páginasIssue 28 - The Nurse Advocate - Hamad Medical Corporation - February 2017Brent ForemanAinda não há avaliações
- Medical ProcedureDocumento3 páginasMedical ProcedureRuby HartAinda não há avaliações
- Med Student Guide FinalDocumento28 páginasMed Student Guide Finalhabtsh habshaAinda não há avaliações
- Siddharth Gandhi 2019A8PS0448GDocumento30 páginasSiddharth Gandhi 2019A8PS0448GSiddharth GandhiAinda não há avaliações
- Paediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenDocumento7 páginasPaediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenT RonaskyAinda não há avaliações
- Clinical Nursing JudgementDocumento8 páginasClinical Nursing Judgementapi-546517574Ainda não há avaliações
- Contin Educ Anaesth Crit Care Pain-2008-Gauntlett-121-4Documento4 páginasContin Educ Anaesth Crit Care Pain-2008-Gauntlett-121-4Wahyu HidayatiAinda não há avaliações
- FLYER A3 Origin Point Therapy v2Documento1 páginaFLYER A3 Origin Point Therapy v2Victor Guerrero100% (1)
- A Clinical Guide To URINE DRUG TESTING PDFDocumento26 páginasA Clinical Guide To URINE DRUG TESTING PDFTavo AAinda não há avaliações
- Analysis of Clinical Nursing Judgement - Steven LukacDocumento7 páginasAnalysis of Clinical Nursing Judgement - Steven Lukacapi-508092399Ainda não há avaliações
- Clinical Nursing Judgment Paper 1Documento5 páginasClinical Nursing Judgment Paper 1api-740431489Ainda não há avaliações
- Admission To NICU CA4068v3Documento12 páginasAdmission To NICU CA4068v3Hana ChristyantiAinda não há avaliações
- Sciences Basic To PsychiatryDocumento2 páginasSciences Basic To Psychiatrynisha chauhanAinda não há avaliações
- Kns 182 Midterm BrochureDocumento2 páginasKns 182 Midterm Brochureapi-743194100Ainda não há avaliações
- ScriptDocumento13 páginasScript張水蛙Ainda não há avaliações
- 2009 CutaneousScarringAClinicalReview PDFDocumento7 páginas2009 CutaneousScarringAClinicalReview PDFJ Roberto Meza OntiverosAinda não há avaliações
- Sistema de Información Científica: Red de Revistas Científicas de América Latina, El Caribe, España y PortugalDocumento7 páginasSistema de Información Científica: Red de Revistas Científicas de América Latina, El Caribe, España y PortugalJ Roberto Meza OntiverosAinda não há avaliações
- 2005-Burd-Hypertrophic - Scar - Vs - Keloid - CME - Copiar PDFDocumento8 páginas2005-Burd-Hypertrophic - Scar - Vs - Keloid - CME - Copiar PDFJ Roberto Meza OntiverosAinda não há avaliações
- 1953 A Modified Harvard Step Test For The Evaluation of Physical Fitness PDFDocumento16 páginas1953 A Modified Harvard Step Test For The Evaluation of Physical Fitness PDFJ Roberto Meza OntiverosAinda não há avaliações
- Biomechanical Considerations in Patellofemoral Joint RehabilitationDocumento7 páginasBiomechanical Considerations in Patellofemoral Joint RehabilitationJ Roberto Meza OntiverosAinda não há avaliações
- NIH Public Access: Author ManuscriptDocumento15 páginasNIH Public Access: Author ManuscriptJ Roberto Meza OntiverosAinda não há avaliações
- Can Physiotherapists Contribute To Care in The Emergency Department?Documento3 páginasCan Physiotherapists Contribute To Care in The Emergency Department?J Roberto Meza OntiverosAinda não há avaliações
- A Simple Method For Measurement of Mechanical Power in JumpingDocumento10 páginasA Simple Method For Measurement of Mechanical Power in JumpingJ Roberto Meza OntiverosAinda não há avaliações
- A Simple Method For Measurement of Mechanical Power in Jumping PDFDocumento10 páginasA Simple Method For Measurement of Mechanical Power in Jumping PDFJ Roberto Meza OntiverosAinda não há avaliações
- c12 Resus Sop r05 Dec15Documento6 páginasc12 Resus Sop r05 Dec15AnggriawanCaesarNurfattah100% (1)
- Lru DeftacDocumento7 páginasLru DeftacVince VI Dacer Generalao100% (1)
- JADWAL ATLS Palembang FK Unsri 22-23 Nov 2019 (1840) Utk PesertaDocumento3 páginasJADWAL ATLS Palembang FK Unsri 22-23 Nov 2019 (1840) Utk PesertaNamira Firdha KesumaAinda não há avaliações
- Shock: Robert H. Sirait, DR.,SP An Dept. of Anesthesia FK UKI JakartaDocumento22 páginasShock: Robert H. Sirait, DR.,SP An Dept. of Anesthesia FK UKI JakartaMuhammad Faisal AminAinda não há avaliações
- 20-3550 Blscomplete Ecard English enDocumento2 páginas20-3550 Blscomplete Ecard English enapi-649513506Ainda não há avaliações
- 1 Introduction To EmsDocumento32 páginas1 Introduction To EmsMichael RebatoAinda não há avaliações
- Key Skills For Hospital DoctorsDocumento3 páginasKey Skills For Hospital DoctorsMustafaAinda não há avaliações
- CPG Hypovolaemic ShockDocumento3 páginasCPG Hypovolaemic ShockZuldi ErdiansyahAinda não há avaliações
- Airway Needs: En-S/s Pport HTMLDocumento8 páginasAirway Needs: En-S/s Pport HTMLFahri FurqanAinda não há avaliações
- 4 - Prehospital Management Particularities of The Patient With Cardiorespiratory ArrestDocumento18 páginas4 - Prehospital Management Particularities of The Patient With Cardiorespiratory ArrestGhimpu DanielaAinda não há avaliações
- Slide 16 TriageDocumento10 páginasSlide 16 TriageSiti Dona IsnaeniAinda não há avaliações
- CPR Infants and ChildrenDocumento26 páginasCPR Infants and ChildrenMaria Alena Rose Salmero100% (1)
- PoCUS Program 1016Documento3 páginasPoCUS Program 1016Josh BurkeAinda não há avaliações
- Topic 5 DUW1012 - Occupational First AidDocumento21 páginasTopic 5 DUW1012 - Occupational First AidNazrina RinaAinda não há avaliações
- HypovolaemicShock SummaryDocumento11 páginasHypovolaemicShock SummarywidyaputraAinda não há avaliações
- Abem HistoryDocumento6 páginasAbem HistoryOsman PazAinda não há avaliações
- Ra 8344Documento6 páginasRa 8344April Isidro100% (1)
- Autopulse Ems Brochure UkDocumento5 páginasAutopulse Ems Brochure UkForum PompieriiAinda não há avaliações
- Performance Checklist CPRDocumento2 páginasPerformance Checklist CPRMhel MGAinda não há avaliações
- Polytrauma, ABC of Trauma & Its ManagementDocumento33 páginasPolytrauma, ABC of Trauma & Its ManagementMongolian MutuAinda não há avaliações
- A237738 PDFDocumento89 páginasA237738 PDFD.M.Ravindra DhanapalaAinda não há avaliações
- PTC MCQDocumento7 páginasPTC MCQYevan HarryBrata0% (1)
- Shaken Baby Syndrome A Review of 20 CasesDocumento4 páginasShaken Baby Syndrome A Review of 20 Casestamis1982Ainda não há avaliações
- Limmer Ch01 LectureDocumento22 páginasLimmer Ch01 LectureShumeng YangAinda não há avaliações
- Flujogramas Europa 2010 Poster RCPDocumento9 páginasFlujogramas Europa 2010 Poster RCPMinina Delka MedinaAinda não há avaliações
- EMS Advisory Council PresentationDocumento21 páginasEMS Advisory Council Presentationsavannahnow.comAinda não há avaliações
- TBR AclsDocumento9 páginasTBR Aclsric_vir_014Ainda não há avaliações
- JADWAL BLENDED LEARNING BTCLS 5 HariDocumento3 páginasJADWAL BLENDED LEARNING BTCLS 5 HariwidyaaladinAinda não há avaliações
- Emergency Assistance PlanDocumento4 páginasEmergency Assistance PlanTerence100% (1)
- Acls - Megacode - UpdatedDocumento4 páginasAcls - Megacode - UpdatedDivine Dela Pena100% (1)