Escolar Documentos
Profissional Documentos
Cultura Documentos
Acute Coronary Syndrome
Enviado por
Muhammad Naquib AliTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Acute Coronary Syndrome
Enviado por
Muhammad Naquib AliDireitos autorais:
Formatos disponíveis
Acute Coronary Syndrome (ACS)
ACS include:
1. STEMI
2. NSTEMI
3. Unstable angina (UA)
* The difference between UA & NSTEMI is that in the latter, there is occluding thrombus, which leads to myocardial
necrosis and a rise in serum troponins or creatine kinase-MB (CK-MB).
Pathophysiology
Mechanism which is common to ACS is rupture or erosion of the fibrous cap of a coronary artery plaque. This
leads to platelet aggregation and adhesion, localized thrombosis, vasoconstriction and distal thrombus
embolization. The presence of rich lipid pool within the plaque and a thin, fibrous cap is associated with an
increased risk of rupture. Platelet release of serotonin and thromboxane A2 result in myocardial ischaemia due to
reduction of coronary blood flow.
Symptoms Signs
1. Acute central chest pain >20 mins, may radiate to 1. Pallor, Sweatiness, anxiety, distress
arm or jaw 2. Pulse > or <
2. Ass. with nausea, dyspnea, sweatiness & 3. Hyper or hypotension
palpitation. 4. 4th heart sound (atrial gallop)
3. May present without chest pain in elderly & 5. May present with signs of heart failure (JVP,
diabetics (such Pt may present with syncope, 3rd heart sound, basal crepitation)
pulm. oedema, epigastric pain & vomiting)
Investigation
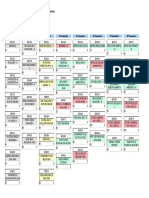
1. Electrocardiogram (ECG) 2. Biochemical Markers
NSTEMI
ST depression and T-wave inversion
ECG should be repeated when patient is in pain
STEMI
New & persistent ST elevation or left bundle
branch block pattern
ECG changes confined to the leads that face the
infarction
Transient ST elevation is seen with coronary
spasm or Prinzmetals angina
3. Transthoracic Echocardiogram (TTE)
Helpful to confirm MI, as wall motion
abnormalities are detected early in STEMI
May detect alt diagnoses; aortic dissection,
pericarditis or pulmonary embolism.
Diagnosis of Acute Myocardial Infarction
When there is evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischaemia.
Any one of the following criteria meets the diagnosis of MI:
1. Detection of rise and fall of cardiac biomarker values (preferably cardiac troponin) with at least one of the
following:
a. Symptoms of ischaemia.
b. New ST-segment-T wave changes or new left bundle branch block.
c. Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
(identification of intracoronary thrombus by angiography or autopsy).
Você também pode gostar
- Acute Coronary SyndromeDocumento41 páginasAcute Coronary SyndromeShrests SinhaAinda não há avaliações
- Acute Coronary Syndrome: Imelva Yulviani GirsangDocumento34 páginasAcute Coronary Syndrome: Imelva Yulviani GirsangAmeel BubbleeAinda não há avaliações
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisNo EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisNota: 5 de 5 estrelas5/5 (1)
- Acute Coronary Syndrome (G4)Documento6 páginasAcute Coronary Syndrome (G4)Francis Josh DagohoyAinda não há avaliações
- Cardiovascular DiseaseDocumento27 páginasCardiovascular DiseaseKyrajane EsguerraAinda não há avaliações
- Unstable Angina (UAP) and non-STEMIDocumento66 páginasUnstable Angina (UAP) and non-STEMIIddrisu Abdul-AzizAinda não há avaliações
- ACS LectureDocumento76 páginasACS Lecture21701101047 Laksmita AnggaraniAinda não há avaliações
- Cardio InternetDocumento46 páginasCardio InternetnaimAinda não há avaliações
- Manual of Cardiovascular Medicine 5th Edition Ebook PDFDocumento61 páginasManual of Cardiovascular Medicine 5th Edition Ebook PDFcaren.shipman316100% (48)
- DR Rahul VarshneyDocumento64 páginasDR Rahul VarshneyIMAinda não há avaliações
- Neacsu Aurelia EssayDocumento3 páginasNeacsu Aurelia EssaySimona NeacsuAinda não há avaliações
- Acute Coronary SyndromeDocumento48 páginasAcute Coronary SyndromeAchmad ulil Albab100% (1)
- STEMi Reading MaterialDocumento14 páginasSTEMi Reading MaterialJerry GohAinda não há avaliações
- Acute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - LecturioDocumento36 páginasAcute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - Lecturiokujtimepira2Ainda não há avaliações
- Diagnosis and Management of Myocardial InfarctionDocumento69 páginasDiagnosis and Management of Myocardial InfarctionSanjana GkAinda não há avaliações
- Myocard InfarctionDocumento2 páginasMyocard InfarctionupaAinda não há avaliações
- Cardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaDocumento3 páginasCardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaMariana NannettiAinda não há avaliações
- Coronay Artery Disease: Dr. Bibek Poudel Department of Medicine City Medical College HospitalDocumento22 páginasCoronay Artery Disease: Dr. Bibek Poudel Department of Medicine City Medical College HospitalitsmailbbkAinda não há avaliações
- Media 115008 en PDFDocumento12 páginasMedia 115008 en PDFsukandeAinda não há avaliações
- Acute Coronary SyndromeDocumento5 páginasAcute Coronary SyndromeLuis OportoAinda não há avaliações
- Treatment of Acute Coronary Syndrome: Part 1: Non-ST-segment Acute Coronary SyndromeDocumento8 páginasTreatment of Acute Coronary Syndrome: Part 1: Non-ST-segment Acute Coronary SyndromeTiago SouzaAinda não há avaliações
- Diagnosis & Management of NstemiDocumento26 páginasDiagnosis & Management of NstemiwlshakespeareAinda não há avaliações
- Overview of Acute Coronary Syndromes (ACS) : MSD Manual Professional VersionDocumento11 páginasOverview of Acute Coronary Syndromes (ACS) : MSD Manual Professional VersionSuhadak DrsAinda não há avaliações
- Topic:: Unstable AnginaDocumento44 páginasTopic:: Unstable AnginaApurba100% (1)
- Acute Coronary Syndrome Myocardial Infarction and Unstable Angina Clinical St. Paul University Philippines Lecturio AcademyDocumento44 páginasAcute Coronary Syndrome Myocardial Infarction and Unstable Angina Clinical St. Paul University Philippines Lecturio AcademyGen XAinda não há avaliações
- Coronary Artery Disease (Cad)Documento4 páginasCoronary Artery Disease (Cad)Freddy PanjaitanAinda não há avaliações
- Acute Coronary SyndromeDocumento12 páginasAcute Coronary SyndromeAnamaria SAinda não há avaliações
- How To Diagnose STEMI?Documento6 páginasHow To Diagnose STEMI?Adhie BadriAinda não há avaliações
- Acute Coronary Syndrome Sindroma Koroner AkutDocumento57 páginasAcute Coronary Syndrome Sindroma Koroner Akutendah100% (1)
- PATH - Ischaemic Heart Disease (13p)Documento13 páginasPATH - Ischaemic Heart Disease (13p)vikashchahal1987Ainda não há avaliações
- Acute Coronary SyndromeDocumento84 páginasAcute Coronary SyndromeRinkita MallickAinda não há avaliações
- Acute Choronary SyndromeDocumento7 páginasAcute Choronary SyndromeSafana NazeerAinda não há avaliações
- Chest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsDocumento16 páginasChest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsJose AnaconaAinda não há avaliações
- ACS LectureDocumento74 páginasACS Lecturekarin amalia sabrinaAinda não há avaliações
- Acute Coronary Syndrome Sindroma Koroner Akut: Toni Mustahsani Aprami, DR., SPPD, SPJPDocumento57 páginasAcute Coronary Syndrome Sindroma Koroner Akut: Toni Mustahsani Aprami, DR., SPPD, SPJPrian susantoAinda não há avaliações
- Ardhendu Sinha Ray - Essentials of Internal Medicine-Jp Medical LTD (2017) - 92-105Documento14 páginasArdhendu Sinha Ray - Essentials of Internal Medicine-Jp Medical LTD (2017) - 92-105Noveno CAinda não há avaliações
- Acute Coronary Syndrome: by Ho NisaDocumento58 páginasAcute Coronary Syndrome: by Ho NisaShre RanjithamAinda não há avaliações
- Acute Coronary Syndrome: Carrie Hurst FY1Documento28 páginasAcute Coronary Syndrome: Carrie Hurst FY1Envhy AmaliaAinda não há avaliações
- Acute Coronary, Angina Pectoris and Myocardial InfractionDocumento26 páginasAcute Coronary, Angina Pectoris and Myocardial Infractionabeer alzhoorAinda não há avaliações
- Acute Coronary Syndrome - Management, Diagnostics and TreatmentDocumento27 páginasAcute Coronary Syndrome - Management, Diagnostics and TreatmentOlga GoryachevaAinda não há avaliações
- 2 - Ischemic Heart DiseaseDocumento42 páginas2 - Ischemic Heart Diseasesamar yousif mohamedAinda não há avaliações
- Sindrom Koroner Akut (Acute Coronary Syndrome)Documento44 páginasSindrom Koroner Akut (Acute Coronary Syndrome)Hendri Saputra0% (1)
- "Fifth Problem. The Painful Heartbeat": Emergency Medicine BlockDocumento78 páginas"Fifth Problem. The Painful Heartbeat": Emergency Medicine BlockFirdaus AldyAinda não há avaliações
- Acute Coronary Syndrome ACSDocumento9 páginasAcute Coronary Syndrome ACSChen BrionesAinda não há avaliações
- Acute Coronary Sindromes 21046 61975Documento28 páginasAcute Coronary Sindromes 21046 61975Simina ÎntunericAinda não há avaliações
- Acute Coronary Syndrome: Kingdom of Saudi Arabia Ministry of Health King Fahad Hofuf Hospital Nursing EducationDocumento33 páginasAcute Coronary Syndrome: Kingdom of Saudi Arabia Ministry of Health King Fahad Hofuf Hospital Nursing EducationAqeelAinda não há avaliações
- Myocardial InfarctionDocumento16 páginasMyocardial Infarctioniyah_18Ainda não há avaliações
- Cardiology Plabable PDFDocumento22 páginasCardiology Plabable PDFTirtha Taposh100% (1)
- Acute MiDocumento61 páginasAcute MiMalueth AnguiAinda não há avaliações
- Ischemic Heart DiseaseDocumento6 páginasIschemic Heart DiseaseApril Joy Villacorta PonceAinda não há avaliações
- TM 9 TM 9 Only Clinical Exam of Heart and Circulatory System AGWEnglishDocumento73 páginasTM 9 TM 9 Only Clinical Exam of Heart and Circulatory System AGWEnglishcellin rubianti azzharaAinda não há avaliações
- Myocardial Infarction (MI)Documento29 páginasMyocardial Infarction (MI)ناصر دويكاتAinda não há avaliações
- Medicine 2Documento47 páginasMedicine 2Ahmed AlrawiAinda não há avaliações
- Coronary Heart Disease 3Documento47 páginasCoronary Heart Disease 3Silvia RAinda não há avaliações
- Second Problem Emergency Medicine Block: "Give Your Heart A Break"Documento59 páginasSecond Problem Emergency Medicine Block: "Give Your Heart A Break"waraney palitAinda não há avaliações
- Satjit Bhusri, MD Cardiologist Lenox Hill Hospital: Jeff Chianfagna Rpa-CDocumento76 páginasSatjit Bhusri, MD Cardiologist Lenox Hill Hospital: Jeff Chianfagna Rpa-CAjaz JunachAinda não há avaliações
- Ischemic Heart DiseaseDocumento5 páginasIschemic Heart DiseaseBert DivinagraciaAinda não há avaliações
- Activity 1 GenPathoDocumento7 páginasActivity 1 GenPathoJolly S. SendinAinda não há avaliações
- MEDI7112 GIT Lecture Checklist 2015Documento2 páginasMEDI7112 GIT Lecture Checklist 2015zjaffri89Ainda não há avaliações
- AP1 Lab4 Intro To Skeleton FA2021Documento15 páginasAP1 Lab4 Intro To Skeleton FA2021Kim VenturaAinda não há avaliações
- Occupational Therapy - Play, SIs and BMTsDocumento3 páginasOccupational Therapy - Play, SIs and BMTsAnnbe Barte100% (1)
- An Are Rob I C DegradationDocumento18 páginasAn Are Rob I C DegradationMartuchis EstradaAinda não há avaliações
- Global Atlas of AsthmaDocumento196 páginasGlobal Atlas of AsthmaMinerva Stanciu50% (2)
- Science 10 3rd Quarter Exam - PDF - Messenger Rna - RibosomeDocumento1 páginaScience 10 3rd Quarter Exam - PDF - Messenger Rna - RibosomeKedir MohammedAinda não há avaliações
- Brain Chip ReportDocumento30 páginasBrain Chip Reportsrikanthkalemla100% (3)
- FLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeDocumento3 páginasFLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeAizaz ul HaqAinda não há avaliações
- Jaw RelationDocumento48 páginasJaw RelationBharanija100% (1)
- Analiza Haplo Grupa Bosnjaka I Dr.Documento12 páginasAnaliza Haplo Grupa Bosnjaka I Dr.damirzeAinda não há avaliações
- Biomechanical Comparison of Axial and Tilted Implants For Mandibular Full-Arch Fixed ProsthesesDocumento9 páginasBiomechanical Comparison of Axial and Tilted Implants For Mandibular Full-Arch Fixed ProsthesesTeresa BeltranAinda não há avaliações
- Yuvdz3wu 13jDocumento2 páginasYuvdz3wu 13jNael LacerdaAinda não há avaliações
- Big Book of Kaiju #0Documento17 páginasBig Book of Kaiju #0Boracchio Pasquale100% (1)
- Unit 5.2 RespirationsDocumento5 páginasUnit 5.2 RespirationsAssasination ClassroomAinda não há avaliações
- Sturge-Weber Syndrome. Study of 55 PatientsDocumento7 páginasSturge-Weber Syndrome. Study of 55 PatientsdzhzrnAinda não há avaliações
- Trousseau Sign of MalignancyDocumento2 páginasTrousseau Sign of MalignancyAmr MuhammedAinda não há avaliações
- Sbk3023 Food Science and NutritionDocumento20 páginasSbk3023 Food Science and NutritionKuMohdSyafiqAinda não há avaliações
- Perfusionist Job DescriptionDocumento3 páginasPerfusionist Job DescriptionNouman IshaqAinda não há avaliações
- Medind - Nic.in Icb t05 I5 Icbt05i5p445Documento4 páginasMedind - Nic.in Icb t05 I5 Icbt05i5p445Ester SibaraniAinda não há avaliações
- A Rare Variation of The Digastric Muscle: Original ResearchDocumento3 páginasA Rare Variation of The Digastric Muscle: Original ResearchYeraldin EspañaAinda não há avaliações
- SaucerizationDocumento12 páginasSaucerizationSaran NuiAinda não há avaliações
- Regulation of Heart RateDocumento27 páginasRegulation of Heart RateGaurav SinghAinda não há avaliações
- DMLT I IiDocumento11 páginasDMLT I IisyedzahidshabirAinda não há avaliações
- Physiologic Transition From Intrauterine To Extrauterine LifeDocumento12 páginasPhysiologic Transition From Intrauterine To Extrauterine Lifeyhojar PisfilAinda não há avaliações
- Digestion Test BiologyDocumento3 páginasDigestion Test BiologyKatrīna SimanovskaAinda não há avaliações
- Case Report Myoma Uterine: Supervised By: Dr. Hesty Duhita Permata, SP - OGDocumento12 páginasCase Report Myoma Uterine: Supervised By: Dr. Hesty Duhita Permata, SP - OGNiki Rizqi rachmawatiAinda não há avaliações
- Thomas K. Rayhawk: Graduate Coursework in Medicinal Pharmacology & Physiology University of Missouri-ColumbiaDocumento3 páginasThomas K. Rayhawk: Graduate Coursework in Medicinal Pharmacology & Physiology University of Missouri-ColumbiaThomas RayhawkAinda não há avaliações
- Postharvest Treatments To Control Physiological and Pathological DisordersDocumento6 páginasPostharvest Treatments To Control Physiological and Pathological DisordersJhonJairoGuerreroCentenoAinda não há avaliações
- Medical CertificateDocumento5 páginasMedical CertificatePrasanna VenkatAinda não há avaliações
- CDNA ExtractionDocumento4 páginasCDNA Extractionvikashisar009Ainda não há avaliações