Escolar Documentos
Profissional Documentos
Cultura Documentos
Pat Revised Msii
Enviado por
api-339160012Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Pat Revised Msii
Enviado por
api-339160012Direitos autorais:
Formatos disponíveis
UNIVERSITY OF SOUTH FLORIDA
COLLEGE OF NURSING
Student: Aimee Achat
Assignment Date:09/16/16
MSI & MSII PATIENT ASSESSMENT TOOL .
Agency: SBN - STJ
1 PATIENT INFORMATION
Patient Initials: J.L. Age: 57 Admission Date: 09/13/16
Gender: Female Marital Status: Married Primary Medical Diagnosis:
Primary Language: English Pulmonary nodule
Level of Education: 11th grade Other Medical Diagnoses: (new on this admission)
Occupation (if retired, what from?): Supervisor at Bealls N/A
Number/ages children/siblings: none
Served/Veteran: N/A Code Status: Full code
If yes: Ever deployed? Yes or No
Living Arrangements: Lives with husband, dog and cat Advanced Directives: Yes
If no, do they want to fill them out?
Surgery Date: 09/13/16
Culture/ Ethnicity /Nationality: Caucasian; American Procedure: Left upper lobectomy
Religion: Christian Type of Insurance: Blue Cross Blue Shield
1 CHIEF COMPLAINT:
Left upper lobe nodule
3 HISTORY OF PRESENT ILLNESS: (Be sure to OLDCART the symptoms in addition to the hospital course of
stay)
Patient is a 59 year old married Caucasian female with a past medical history of hypertension and breast cancer. She has a
past surgical history of a bilateral mastectomy, stage 1 reconstruction, right breast lumpectomy, collar bone surgery,
hysterectomy, laparotomy, and tonsillectomy. Patient was undergoing a routine screening mammogram in February, when
there were concerned findings which prompted an MRI and subsequently resulted in bilateral mastectomy. About four
months later, the patient returned to her primary care physician for a follow up and to obtain a baseline CT scan, however
the CT scan revealed a left upper lobe nodule.
University of South Florida College of Nursing Revision September 2014 1
2 PAST MEDICAL HISTORY/PAST SURGICAL HISTORY Include hospitalizations for any medical
illness or operation; include treatment/management of disease
Date Operation or Illness
1961 Strabismus
1965 Tonsillectomy
1973 Clavicle fracture surgery
1976 Femur arterioplasty
1982 Right salpingo-oophorectomy
1983 Total hysterectomy
1992 Lumpectomy
05/2016 Double mastectomy
09/2016 Left upper lobectomy
(angina, MI, DVT etc.)
Stomach Ulcers
Environmental
Mental Health
Age (in years)
FAMILY
Heart Trouble
Bleeds Easily
Hypertension
Cause
Alcoholism
MEDICAL
Glaucoma
Problems
Problems
Allergies
of
Diabetes
Arthritis
Seizures
Anemia
Asthma
Kidney
HISTORY
Cancer
Tumor
Stroke
Death
Gout
(if
applicable)
Father 54 M.I.
Mother 45 I.C.H
Sister 57
Brother 56
Brother 55
Brother
52
relationship
Comments: Include age of onset
1 IMMUNIZATION HISTORY
(May state U for unknown, except for Tetanus, Flu, and Pna) YES NO
Routine childhood vaccinations
Routine adult vaccinations for military or federal service
Adult Diphtheria (Date)
Adult Tetanus (Date) Is within 10 years?
Influenza (flu) (Date) Is within 1 years?
Pneumococcal (pneumonia) (Date) Is within 5 years?
Have you had any other vaccines given for international travel or
occupational purposes? Please List
If yes: give date, can state U for the patient not knowing date received
University of South Florida College of Nursing Revision September 2014 2
1 ALLERGIES
NAME of
OR ADVERSE Type of Reaction (describe explicitly)
Causative Agent
REACTIONS
Sulfa drugs Hives
Medications
Hay fever Watery and itchy eyes
Other (food, tape,
latex, dye, etc.)
5 PATHOPHYSIOLOGY: (include APA reference and in text citations) (Mechanics of disease, risk factors, how to
diagnose, how to treat, prognosis, and include any genetic factors impacting the diagnosis, prognosis or
treatment)
A pulmonary nodule is a small rounded growth in the lung usually less than three centimeters and is usually caused by
infections such as mycobacterium tuberculosis, non-infection causes such as rheumatoid arthritis, or neoplasms such as a
sarcoma (Cleveland Clinic, 2016). According to the Cleveland Clinic (2016), the nodules are diagnosed by different
diagnostic tests: Chest X-rays usually indicated that there is an abnormality on the lung, Computerized Tomography (CT)
scan may be used for a more detailed image of the spot, a Positron Emission Tomography (PET) scan will be ordered to
see if it is benign or malignant and a Biopsy will be done as a final indicator of whether or not the nodule is malignant.
Truong et al. (2013) stated that the factors associated with increased risk were the patients age, the presence of
symptoms, history of smoking, and a history of exposure to asbestos, uranium or radon. A benign nodule will not need to
be taken out, however, if it is malignant without metastasis then it can be removed surgically by thoracotomy or video-
assisted thoracoscopy (Cleveland Clinic, 2016).
5 MEDICATIONS: [Include both prescription and OTC; hospital (include IVF) , home (reconciliation), routine, and PRN
medication . Give trade and generic name.]
Name Norvasc/amlodipine Concentration Dosage Amount 5mg
Route orally Frequency Take 1 tablet by mouth daily
Pharmaceutical class Calcium channel blocker Home Hospital or Both
Indication It dilates blood vessels and improves blood flow for patients with high blood pressure and angina
Adverse/ Side effects: Swelling of legs, stomach pain, nausea, face flushing, arrhythmia, palpitations
Nursing considerations/ Patient Teaching: Change positions slowly to avoid dizziness and falls.
Name Microzide/hydrochlorothiazide Concentration Dosage Amount 25mg
Route orally Frequency Take 1 tablet by mouth daily
Pharmaceutical class: Diuretic Home Hospital or Both
Indication: Used to treat high blood pressure and to treat fluid retention
Adverse/ Side effects: vision problems, nausea, vomiting, tachycardia, muscle pain, dark urine
Nursing considerations/ Patient Teaching: Get vision checks annually with ophthalmologist
University of South Florida College of Nursing Revision September 2014 3
Name Klor-con/Potassium Chloride ER Concentration Dosage Amount 10 mEq
Route orally Frequency Take 1 tablet by mouth daily
Pharmaceutical class: Potassium supplement Home Hospital or Both
Indication: To prevent or to treat low blood levels of potassium.
Adverse/ Side effects: GI effects, nausea, vomiting, abdominal pain, flatulence, diarrhea
Nursing considerations/ Patient Teaching: Have the patient report any type of GI symptoms such as tarry stools or other evidence of GI bleeding.
Name Arimidex/anastrozole Concentration Dosage Amount 1mg
Route orally Frequency Take 1 tablet by mouth daily
Pharmaceutical class: Antineoplastic agent Home Hospital or Both
Indication: adjuvant treatment of hormone receptor-positive early breast cancer
Adverse/ Side effects: constipation, nausea, vomiting, breast swelling or tenderness, vaginal bleeding, hair thinning, weight changes, osteoporosis
Nursing considerations/ Patient Teaching: Adding Calcium and vitamin D supplements in diet and include weight-bearing exercises.
Name Caltrate + 600/calcium 600 +D Concentration Dosage Amount 600 + D
Route orally Frequency Take 1 tablet by mouth twice a day
Pharmaceutical class: Vitamins Home Hospital or Both
Indication: Treating or preventing Calcium deficiency
Adverse/ Side effects: severe allergic reaction, nausea, vomiting, constipation.
Nursing considerations/ Patient Teaching: Do not take more than directed and include weight-bearing exercise to regimen for strengthening of bones.
Name Concentration Dosage Amount
Route Frequency
Pharmaceutical class Home Hospital or Both
Indication
Adverse/ Side effects
Nursing considerations/ Patient Teaching
Name Concentration Dosage Amount
Route Frequency
Pharmaceutical class Home Hospital or Both
Indication
Adverse/ Side effects
Nursing considerations/ Patient Teaching
University of South Florida College of Nursing Revision September 2014 4
5 NUTRITION: Include type of diet, 24 HR average home diet, and your nutritional analysis with recommendations.
Diet ordered in hospital? Normal Analysis of home diet (Compare to My Plate and
Diet patient follows at home? Normal Consider co-morbidities and cultural considerations):
24 HR average home diet:
Breakfast: granola bar, smoothies (yogurt, kale), Include a cup of fruit to diet to increase nutrients. Berries
Coffee with sugar and milk are a good form of antioxidants for free radicals.
Lunch: steamed chicken with vegetables and a cup of rice Replace potatoes with mashed, steamed cauliflower to
reduce calories.
Dinner: pork, beef or chicken, potatoes and vegetables Use the palm of your hand as a measurement of how much
lean meat to eat at lunch.
Snacks: Fiber one bars, Hersheys dark chocolate, yogurt Replace pork with fish for omega fats.
Liquids (include alcohol): water
Use this link for the nutritional analysis by comparing the patients
24 HR average home diet to the recommended portions, and use
My Plate as a reference.
1 COPING ASSESSMENT/SUPPORT SYSTEM: (these are prompts designed to help guide your discussion)
Who helps you when you are ill?
Herself, friends, or husband
How do you generally cope with stress? or What do you do when you are upset?
Patients states that she walks 3 miles a day or talks to friends about problems
Recent difficulties (Feelings of depression, anxiety, being overwhelmed, relationships, friends, social life)
Depressed about how husband views her body with her double mastectomy
+2 DOMESTIC VIOLENCE ASSESSMENT
Consider beginning with: Unfortunately many, children, as well as adult women and men have been or currently are
unsafe in their relationships in their homes. I am going to ask some questions that help me to make sure that you are
safe.
Have you ever felt unsafe in a close relationship? ______Yes____________________________________________
Have you ever been talked down to? Yes___________ Have you ever been hit punched or slapped? _Yes__________
Have you been emotionally or physically harmed in other ways by a person in a close relationship with you?
_______Yes__________________ If yes, have you sought help for this? _Therapy for 3 years_______
Are you currently in a safe relationship? Yes
University of South Florida College of Nursing Revision September 2014 5
4 DEVELOPMENTAL CONSIDERATIONS:
Eriksons stage of psychosocial development: Trust vs. Mistrust Autonomy vs. Doubt & Shame Initiative vs. Guilt Industry vs.
Inferiority Identity vs. Role Confusion/Diffusion Intimacy vs. Isolation Generativity vs. Self absorption/Stagnation Ego Integrity vs. Despair
Check one box and give the textbook definition (with citation and reference) of both parts of Ericksons developmental stage for your
patients age group: According to Treas (2014), generativity refers to being an active member of society and the individual will feel as
though they are making a difference in the world. Whereas, stagnation refers to the inability to find a way to contribute to society.
Describe the stage your patient is in and give the characteristics that the patient exhibits that led you to your determination:
The patient is in the self-absorption stage/stagnation stage because she feels regretful about not being able to raise/have
children and not finishing her high school diploma in her previous years.
Describe what impact of disease/condition or hospitalization has had on your patients developmental stage of life:
Due to the patients illness throughout her life, she feels like she has had no control over her fate and has not been able to
accomplish all her goals.
+3 CULTURAL ASSESSMENT:
What do you think is the cause of your illness?
Patient states her illness is due to her smoking for 30 years, her parents both smoked throughout her life, drinking alcohol,
and eating too much junk food.
What does your illness mean to you?
A means to an end
+3 SEXUALITY ASSESSMENT: (the following prompts may help to guide your discussion)
Consider beginning with: I am asking about your sexual history in order to obtain information that will screen for
possible sexual health problems, these are usually related to either infection, changes with aging and/or quality of
life. All of these questions are confidential and protected in your medical record
Have you ever been sexually active?__Yes_______________________________________________________________
Do you prefer women, men or both genders? ___Men______________________________________________________
Are you aware of ever having a sexually transmitted infection? _No__________________________________________
Have you or a partner ever had an abnormal pap smear?_No_________________________________________________
Have you or your partner received the Gardasil (HPV) vaccination? ___________________________________________
Are you currently sexually active? ___Yes________________________ If yes, are you in a monogamous relationship?
___Yes_________________ When sexually active, what measures do you take to prevent acquiring a sexually transmitted
disease or an unintended pregnancy? ___No_______________________________
How long have you been with your current partner?___24 years_____________________________________________
Have any medical or surgical conditions changed your ability to have sexual activity? ___Yes, breast cancer__________
Do you have any concerns about sexual health or how to prevent sexually transmitted disease or unintended pregnancy?
No
University of South Florida College of Nursing Revision September 2014 6
1 SPIRITUALITY ASSESSMENT: (including but not limited to the following questions)
What importance does religion or spirituality have in your life?
Despite going to church on and off throughout her life because her parents did not go, the patient has used religion as her life-line
when she is scared or worried about her health.
______________________________________________________________________________________________________
Do your religious beliefs influence your current condition?
_The patient states that her religion gives her peace and strength for operations and the many health conditions she has.
___________________________________________________________________________________________________
______________________________________________________________________________________________________
+3 SMOKING, CHEMICAL USE, OCCUPATIONAL/ENVIRONMENTAL EXPOSURES:
1. Does the patient currently, or has he/she ever smoked or used chewing tobacco? Yes No
If so, what? How much?(specify daily amount) For how many years? 33 years
Smoke cigarettes 1-2 packs per day (age 17 thru 50 )
If applicable, when did the
Pack Years: 1-2 ppd x 33 years
patient quit? 50
Does anyone in the patients household smoke tobacco? If Has the patient ever tried to quit? Yes
so, what, and how much? Yes smoke cigarettes If yes, what did they use to try to quit? Chantix
2. Does the patient drink alcohol or has he/she ever drank alcohol? Yes No
What? How much? 4/5 quart to gallon For how many years? 19 years
Liquor Volume: ~ 1250 ml (age 16 thru 35 )
Frequency:
If applicable, when did the patient quit?
35 years old after diagnosis of breast cancer
3. Has the patient ever used street drugs such as marijuana, cocaine, heroin, or other? Yes No
If so, what?
Marijuana How much? For how many years? 41 years
1 to 2 puffs a day (age 16 thru now )
Is the patient currently using these drugs?
If not, when did he/she quit?
Yes No
4. Have you ever, or are you currently exposed to any occupational or environmental Hazards/Risks
Worked in home construction with insulation and dry wall. Also worked in a paint factory and exposed to the fumes.
5. For Veterans: Have you had any kind of service related exposure?
University of South Florida College of Nursing Revision September 2014 7
10 REVIEW OF SYSTEMS NARRATIVE
Gastrointestinal Immunologic
Nausea, vomiting, or diarrhea Chills with severe shaking
Integumentary Constipation Irritable Bowel Night sweats
Changes in appearance of skin GERD Cholecystitis Fever
Problems with nails Indigestion Gastritis / Ulcers HIV or AIDS
Dandruff Hemorrhoids Blood in the stool Lupus
Psoriasis Yellow jaundice Hepatitis Rheumatoid Arthritis
Hives or rashes Pancreatitis Sarcoidosis
Skin infections Colitis Tumor
Use of sunscreen SPF: 15 Diverticulitis Life threatening allergic reaction
Bathing routine: once a day Appendicitis Enlarged lymph nodes
Other: Abdominal Abscess Other:
Be sure to answer the highlighted area Last colonoscopy? 2013
HEENT Other: Hematologic/Oncologic
Difficulty seeing Genitourinary Anemia
Cataracts or Glaucoma nocturia Bleeds easily
Difficulty hearing dysuria Bruises easily
Ear infections hematuria Cancer
Sinus pain or infections polyuria Blood Transfusions
Nose bleeds kidney stones Blood type if known:
Post-nasal drip Normal frequency of urination: 4 x/day Other:
Oral/pharyngeal infection Bladder or kidney infections
Dental problems Metabolic/Endocrine
Routine brushing of teeth 1 x/day Diabetes Type:
Routine dentist visits x/year Hypothyroid /Hyperthyroid
Vision screening: every 4 years Intolerance to hot or cold
Other: Osteoporosis
Other:
Pulmonary
Difficulty Breathing Central Nervous System
Cough - dry or productive WOMEN ONLY CVA
Asthma Infection of the female genitalia Dizziness
Bronchitis Monthly self breast exam Severe Headaches
Emphysema Frequency of pap/pelvic exam Migraines
Pneumonia Date of last gyn exam? 11/2015 Seizures
Tuberculosis menstrual cycle regular irregular Ticks or Tremors
Environmental allergies menarche age? 16 Encephalitis
last CXR?: 9/10/16 menopause age? Meningitis
Date of last Mammogram &Result:
Other: Other:
01/2016; breast cancer
Date of DEXA Bone Density & Result:
Cardiovascular 2012 - OSTEOPENIA Mental Illness
Hypertension Depression
Hyperlipidemia Schizophrenia
Chest pain / Angina 222 Anxiety
Myocardial Infarction 2012 Bipolar
CAD/PVD Other:
CHF Musculoskeletal
Murmur Injuries or Fractures Childhood Diseases
Thrombus Weakness Measles
Rheumatic Fever Pain Mumps
Myocarditis Gout Polio
Arrhythmias Osteomyelitis Scarlet Fever
University of South Florida College of Nursing Revision September 2014 8
Last EKG screening, when? 9/9/16 Arthritis Chicken Pox
Other: Other: Other:
General Constitution
Recent weight loss or gain: weight gain
How many lbs? 30 lbs
Time frame? 5 months
Intentional? No
How do you view your overall health?
Is there any problem that is not mentioned that your patient sought medical attention for with anyone?
Any other questions or comments that your patient would like you to know?
University of South Florida College of Nursing Revision September 2014 9
10 PHYSICAL EXAMINATION:
General Survey: well- Height: 170 cm Weight: 87.6 kg BMI: 30 Pain: (include rating and
groomed and dressed Pulse: 73 Blood Pressure: (include location) location)
appropriately Respirations: 20 134/84 (brachial) 2/10 (incision site)
Temperature: (route SpO2 97% Is the patient on Room Air or O2
taken?) 97 (oral) Room air
Overall Appearance: [Dress/grooming/physical handicaps/eye contact]
clean, hair combed, dress appropriate for setting and temperature, maintains eye contact, no obvious handicaps
Overall Behavior: [e.g.: appropriate/restless/odd mannerisms/agitated/lethargic/other]
awake, calm, relaxed, interacts well with others, judgment intact
Speech: [e.g.: clear/mumbles /rapid /slurred/silent/other]
clear, crisp diction
Mood and Affect: pleasant cooperative cheerful talkative quiet boisterous flat
apathetic bizarre agitated anxious tearful withdrawn aggressive hostile loud
Other:
Integumentary
Skin is warm, dry, and intact Skin turgor elastic No rashes, lesions, or deformities
Nails without clubbing Capillary refill < 3 seconds Hair evenly distributed, clean, without vermin
Patient has an incision site dressing that is clean and dry.
Central access device Type: Location: Date inserted:
Fluids infusing? no yes - what?
HEENT: Facial features symmetric No pain in sinus region No pain, clicking of TMJ Trachea midline
Thyroid not enlarged No palpable lymph nodes sclera white and conjunctiva clear; without discharge
Eyebrows, eyelids, orbital area, eyelashes, and lacrimal glands symmetric without edema or tenderness
PERRLA pupil size / mm Peripheral vision intact EOM intact through 6 cardinal fields without nystagmus
Ears symmetric without lesions or discharge Whisper test heard: right ear- 13 inches & left ear- 13 inches
Nose without lesions or discharge Lips, buccal mucosa, floor of mouth, & tongue pink & moist without lesions
Dentition: No missing teeth or known dental problems
Comments:
Pulmonary/Thorax: Respirations regular and unlabored Transverse to AP ratio 2:1 Chest expansion
symmetric
Percussion resonant throughout all lung fields, dull towards posterior bases
Sputum production: thick thin Amount: scant small moderate large
Color: white pale yellow yellow dark yellow green gray light tan brown red
Lung sounds: clear without adventitious sounds
RUL: CL LUL: CL
RML: CL LLL: CL
RLL: CL
CL Clear; WH Wheezes; CR Crackles; RH Rhonchi; D Diminished; S Stridor; Ab - Absent
Cardiovascular: No lifts, heaves, or thrills
Heart sounds: S1 S2 audible Regular Irregular No murmurs, clicks, or adventitious heart sounds No JVD
University of South Florida College of Nursing Revision September 2014 10
Rhythm (for patients with ECG tracing tape 6 second strip below and analyze)
Calf pain bilaterally negative Pulses bilaterally equal [rating scale: 0-absent, 1-barely palpable, 2-weak, 3-normal, 4-bounding]
Apical pulse: 3 Carotid: 3 Brachial: 3 Radial: 3 Femoral: 3 Popliteal: 3 DP: 3 PT: 3
No temporal or carotid bruits Edema: 0 [rating scale: 0-none, +1 (1-2mm), +2 (3-4mm), +3 (5-6mm), +4(7-8mm) ]
Location of edema: N/a pitting non-pitting
Extremities warm with capillary refill less than 3 seconds
GI Bowel sounds active x 4 quadrants; no bruits auscultated No organomegaly
Percussion dull over liver and spleen and tympanic over stomach and intestine Abdomen non-tender to palpation
Last BM: (date 09 / 15 / 2016 ) Formed Semi-formed Unformed Soft Hard Liquid Watery
Color: Light brown Medium Brown Dark Brown Yellow Green White Coffee Ground Maroon Bright Red
Nausea emesis Describe if present:
Genitalia: Clean, moist, without discharge, lesions or odor Not assessed, patient alert, oriented, denies problems
Other Describe:
GU Urine output: Clear Cloudy Color: yellow Previous 24 hour output: 800 mLs
Foley Catheter Urinal or Bedpan Bathroom Privileges without assistance or with assistance
CVA punch without rebound tenderness
Musculoskeletal: Full ROM intact in all extremities without crepitus
Strength bilaterally equal at ___5____ RUE ___5____ LUE __5_____ RLE & ___5____ in LLE
[rating scale: 0-absent, 1-trace, 2-not against gravity, 3-against gravity but not against resistance, 4-against some resistance, 5-against full resistance]
vertebral column without kyphosis or scoliosis
Neurovascular status intact: peripheral pulses palpable, no pain, pallor, paralysis or paresthesia
Neurological: Patient awake, alert, oriented to person, place, time, and date Confused; if confused attach mini mental exam
CN 2-12 grossly intact Sensation intact to touch, pain, and vibration Rombergs Negative
Stereognosis, graphesthesia, and proprioception intact Gait smooth, regular with symmetric length of the stride
DTR: [rating scale: 0-absent, +1 sluggish/diminished, +2 active/expected, +3 slightly hyperactive, +4 Hyperactive, with intermittent or transient clonus]
Triceps: +2 Biceps: +2 Brachioradial: +2 Patellar: +2 Achilles: +2 Ankle clonus: positive negative Babinski: positive negative
University of South Florida College of Nursing Revision September 2014 11
10 PERTINENT LAB VALUES AND DIAGNOSTIC TEST RESULTS (include pertinent normals as well
as abnormals, include rationale and analysis. List dates with all labs and diagnostic tests):
Chest CT scan positive for left upper lobe nodule
PET scan revealed 1.4 cm left upper lobe nodule with SUV of 3.5
Pertinent includes labs that are checked when on certain medications, monitored for the disease process, need
prior to and after surgery, and pertinent to hospitalization. Do not forget to include diagnostic tests, such as
Ultrasounds, X-rays, CT, MRI, HIDA, etc. If a lab or test is not in the chart (such as one that is done preop) then
include why you expect it to be done and what results you expect to see.
Lab Dates Trend Analysis
HGB Hemoglobin was normal Bleeding from the
12.7 09/13/16 pre-op but dropped surgery caused the
11.6 09/14/16 slightly after the surgery. hemoglobin to drop.
+2 CURRENT HEALTHCARE TREATMENTS AND PROCEDURES: (Include all medical, nursing,
multidisciplinary treatments and procedures, such as diet, vitals, activity, scheduled diagnostic tests, consults,
accu checks, etc. Also provide rationale and frequency if applicable.)
After tolerating clear and soft diets, patient is now on a regular diet, vitals will be taken every 4 hours, and
patient can ambulate with assistance. Consults were placed with the surgeon on patients progress and
With the pulmonary doctor on recovery. Patient will continue to use incentive spirometer five times an hour.
8 NURSING DIAGNOSES (actual and potential - listed in order of priority)
1. Ineffective breathing pattern r/t pain
2. At risk for infection r/t invasive procedure
3. Acute pain r/t surgical procedure, coughing, deep breathing
4. Risk for bleeding
5. Deficient knowledge r/t self-care, effective breathing exercises, pain relief
6. Risk for injury
7. Risk for vascular trauma
University of South Florida College of Nursing Revision September 2014 12
CARE PLAN
Nursing Diagnosis: Ineffective breathing pattern r/t pain
Patient Goals/Outcomes Nursing Interventions to Rationale for Interventions Evaluation of Goal on Day Care
Achieve Goal Provide References is Provided
Patient will have improved chest Patient will use incentive Using an incentive spirometer can Patient will have reached an
expansion by the end of the shift. spirometer 5 times an hour. reduce the risk of atelectasis appropriate level on the marker
(Ackley, 2011) without difficulty.
The patient will have an absence Patient will walk with assistance Ambulation can help break up Patient will be walking without
of dyspnea at the time of discharge around the unit as tolerated. secretions that block airways. dyspnea.
(Ackley, 2011)
Include a minimum of one
Long term goal per care plan
University of South Florida College of Nursing Revision September 2014 13
15 CARE PLAN
Nursing Diagnosis: At risk for infection r/t invasive procedure
Patient Goals/Outcomes Nursing Interventions to Rationale for Interventions Evaluation of Goal on Day Care
Achieve Goal Provide References is Provided
Patient will demonstrate proper The nurse will educate the patient By introducing the use of hand Patient will remain free from
hand washing at the end of the on how to properly wash hands. rubbing with an alcoholic solution, symptoms of infection by the end
day. there was significant improved of the day.
hand-cleansing compliance
(Ackley, 2011)
Patient will incorporate healthy Educate patient on the importance Tissue repair requires increased Patient incision site will be healing
eating habits by her follow-up of lean protein to help with the protein and carbohydrates properly at office visit.
appointment. healing of her wound. (Ackley, 2011)
Include a minimum of one
Long term goal per care plan
2 DISCHARGE PLANNING: (put a * in front of any pt education in above care plan that you would include for discharge teaching)
Consider the following needs:
SS Consult
* Dietary Consult
PT/ OT
Pastoral Care
* Durable Medical Needs
* F/U appointments
* Med Instruction/Prescription
University of South Florida College of Nursing Revision September 2014 14
* are any of the patients medications available at a discount pharmacy? *Yes No
* Rehab/ HH
Palliative Care
University of South Florida College of Nursing Revision September 2014 15
References
Ackley, B.J., & Ladwig, G.B. (2011). Nursing Diagnosis Handbook: An evidence-based guide to
planning care. St Louis, MO: Elsevier.
Cleveland Clinic. (2016). Pulmonary nodules. Retrieved from
http://my.clevelandclinic.org/health/diseases_conditions/hic_Pulmonary_Nodules
Treas, L. S., & Wilkinson, J. M. (2014). Basic Nursing. Philadelphia, PA: F.A. Davis Company.
Truong, M. T., Ko, J. P., Rossi, S. E., Rossi, I., Viswanathan, C., Bruzzi, J. F., . . . Erasmus, J. F.
(2013, October 19). Update in the Evaluation of the Solitary Pulmonary Nodule.
Radio Graphics, 34(6), 1658-1679. http://dx.doi.org/10.1148/rg.346130092
University of South Florida College of Nursing Revision September 2014 16
University of South Florida College of Nursing Revision September 2014 17
Você também pode gostar
- ms1 Pat 2-2Documento21 páginasms1 Pat 2-2api-404285262Ainda não há avaliações
- Pat Med Surg IDocumento21 páginasPat Med Surg Iapi-399464028Ainda não há avaliações
- Msii Pat 1-1Documento22 páginasMsii Pat 1-1api-404285262Ainda não há avaliações
- Pat Fall 1-1Documento17 páginasPat Fall 1-1api-339160012Ainda não há avaliações
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocumento16 páginasUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-402496681Ainda não há avaliações
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocumento19 páginasUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-418237167Ainda não há avaliações
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocumento21 páginasUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-385494784Ainda não há avaliações
- Pat ms1 3 08Documento14 páginasPat ms1 3 08api-371817203Ainda não há avaliações
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocumento17 páginasUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-355083078Ainda não há avaliações
- Pat Semester 1Documento16 páginasPat Semester 1api-404285262Ainda não há avaliações
- Pat ms1 1Documento18 páginasPat ms1 1api-314810052Ainda não há avaliações
- Pat Fundies 2016Documento18 páginasPat Fundies 2016api-371817203Ainda não há avaliações
- Pat Revised 9-2014 Msi Msii 2 1 1Documento28 páginasPat Revised 9-2014 Msi Msii 2 1 1api-353928268Ainda não há avaliações
- Pat 1Documento21 páginasPat 1api-315208605Ainda não há avaliações
- Ms Pat 2Documento19 páginasMs Pat 2api-379546477Ainda não há avaliações
- Pat ms2Documento20 páginasPat ms2api-355298006Ainda não há avaliações
- Pat Med Surg IIDocumento19 páginasPat Med Surg IIapi-399464028Ainda não há avaliações
- ms1 PatDocumento14 páginasms1 Patapi-364212510Ainda não há avaliações
- Portfolio Pat 1Documento18 páginasPortfolio Pat 1api-365835586Ainda não há avaliações
- Harriman Ms II Pat GradedDocumento20 páginasHarriman Ms II Pat Gradedapi-380537580Ainda não há avaliações
- Pat 1 Medsurg 1Documento17 páginasPat 1 Medsurg 1api-354599629Ainda não há avaliações
- Kristina Nealy ms1 Pat 1 2Documento19 páginasKristina Nealy ms1 Pat 1 2api-314372295Ainda não há avaliações
- Ms 1 Pat Marline FaustinDocumento18 páginasMs 1 Pat Marline Faustinapi-365764138Ainda não há avaliações
- Pat 2Documento19 páginasPat 2api-404415990Ainda não há avaliações
- Pat FundiesDocumento18 páginasPat Fundiesapi-355298006Ainda não há avaliações
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocumento24 páginasUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-315444338Ainda não há avaliações
- Pat 1Documento20 páginasPat 1api-315208605Ainda não há avaliações
- Jamie Pat Number 1 Fall 2015Documento23 páginasJamie Pat Number 1 Fall 2015api-314246440Ainda não há avaliações
- Pat FundiesDocumento16 páginasPat Fundiesapi-338998736Ainda não há avaliações
- Pat Revised 9-2014 FundamentalsDocumento14 páginasPat Revised 9-2014 Fundamentalsapi-355083078Ainda não há avaliações
- University of South Florida College of Nursing: Fundamental Patient Assessment ToolDocumento17 páginasUniversity of South Florida College of Nursing: Fundamental Patient Assessment Toolapi-317257077Ainda não há avaliações
- Pat 2 Medical Surgical IDocumento23 páginasPat 2 Medical Surgical Iapi-417993254Ainda não há avaliações
- Pat1 2Documento16 páginasPat1 2api-385494784Ainda não há avaliações
- Pat F 1Documento18 páginasPat F 1api-379546477Ainda não há avaliações
- University of South Florida College of Nursing: Fundamental Patient Assessment ToolDocumento19 páginasUniversity of South Florida College of Nursing: Fundamental Patient Assessment Toolapi-418237167Ainda não há avaliações
- Pat 1 FundamentalsDocumento17 páginasPat 1 Fundamentalsapi-417993254Ainda não há avaliações
- Medical History FormatDocumento5 páginasMedical History Formatkrzia TehAinda não há avaliações
- Health History Questionnaire: Yes Self Family What Treatment Received and Date(s)Documento3 páginasHealth History Questionnaire: Yes Self Family What Treatment Received and Date(s)Vignesh VijayAinda não há avaliações
- Fundamentals PatDocumento27 páginasFundamentals Patapi-417446716Ainda não há avaliações
- CVDPROG - Flowchart-RiskAssessment-OtherDocumento1 páginaCVDPROG - Flowchart-RiskAssessment-OtherHanif FebrianAinda não há avaliações
- NSG 120 Patient Care Plan ProjectDocumento25 páginasNSG 120 Patient Care Plan Projectgodfreykaruku21Ainda não há avaliações
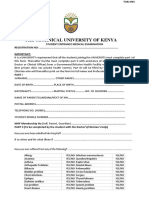
- The Technical University of KenyaDocumento3 páginasThe Technical University of Kenyalixus mwangi100% (1)
- Adult Medical History Form: Please Complete All Pages NameDocumento5 páginasAdult Medical History Form: Please Complete All Pages NameCaroline IberfuentesAinda não há avaliações
- Ramsay Sime Darby World Health Day E-Brochure FINALDocumento22 páginasRamsay Sime Darby World Health Day E-Brochure FINALJasmine LeeAinda não há avaliações
- Patient Assessment Form For AdultsDocumento2 páginasPatient Assessment Form For AdultsAriane CauanAinda não há avaliações
- NSG 120 Patient Care Plan Project RevisedDocumento26 páginasNSG 120 Patient Care Plan Project Revisedgodfreykaruku21Ainda não há avaliações
- NZSSD 2016Documento7 páginasNZSSD 2016elproedrosAinda não há avaliações
- Nicanor Reyes Medical Foundation: Far Eastern UniversityDocumento2 páginasNicanor Reyes Medical Foundation: Far Eastern UniversityAudreyAinda não há avaliações
- Uncpn Form New Patient Medical HistoryDocumento5 páginasUncpn Form New Patient Medical HistorySonuraj rana RanaAinda não há avaliações
- OB-GYN Intake Form New Patient InformationDocumento6 páginasOB-GYN Intake Form New Patient InformationaltenereAinda não há avaliações
- Karni - MCU EXP 040322Documento9 páginasKarni - MCU EXP 040322denstar silalahiAinda não há avaliações
- 02.borang Diabetes Outcome UpdateDocumento1 página02.borang Diabetes Outcome Updatesuhairizwan ab wahabAinda não há avaliações
- As Per Merchant Shipping (Medical Examination) Rules, 2010 & Ism/Stcwcode /9 and MLC Convention 2006 (A Rhha 2Documento4 páginasAs Per Merchant Shipping (Medical Examination) Rules, 2010 & Ism/Stcwcode /9 and MLC Convention 2006 (A Rhha 2avishkar guptaAinda não há avaliações
- Maternity Admission Forms: Congratulations and Thank You For Choosing To Give Birth To Your Baby at The BaysDocumento9 páginasMaternity Admission Forms: Congratulations and Thank You For Choosing To Give Birth To Your Baby at The BaysraraAinda não há avaliações
- Hope Week 4Documento11 páginasHope Week 4Joseph Patrick OcapanAinda não há avaliações
- Nicanor Reyes Medical Foundation: Far Eastern UniversityDocumento2 páginasNicanor Reyes Medical Foundation: Far Eastern UniversityGeorgeMarcusAinda não há avaliações
- New Patient Health History Form: (Please Explain Below)Documento2 páginasNew Patient Health History Form: (Please Explain Below)KevinAinda não há avaliações
- Activity 2 (Big Leaps)Documento4 páginasActivity 2 (Big Leaps)Cameron De GuzmanAinda não há avaliações
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsNo EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsAinda não há avaliações
- Nurse Resume 2017Documento2 páginasNurse Resume 2017api-339160012Ainda não há avaliações
- Professional GoalsDocumento2 páginasProfessional Goalsapi-339160012Ainda não há avaliações
- Cover LetterDocumento1 páginaCover Letterapi-339160012Ainda não há avaliações
- Pat Draft Reviewed by JsDocumento14 páginasPat Draft Reviewed by Jsapi-339160012Ainda não há avaliações
- Med Error PaperDocumento4 páginasMed Error Paperapi-339160012Ainda não há avaliações
- Picot SynthesisDocumento8 páginasPicot Synthesisapi-339160012Ainda não há avaliações
- Pharmacotherapy SC CertificateDocumento1 páginaPharmacotherapy SC Certificateapi-338998736Ainda não há avaliações
- Achat Graded Health Policy Paper FinalDocumento12 páginasAchat Graded Health Policy Paper Finalapi-339160012Ainda não há avaliações
- Fundamentals FinalDocumento6 páginasFundamentals Finalapi-339160012Ainda não há avaliações
- Is 200 HcaDocumento1 páginaIs 200 Hcaapi-354841289Ainda não há avaliações
- Patient Safety VopptDocumento11 páginasPatient Safety Vopptapi-339160012Ainda não há avaliações
- Certificate 1Documento1 páginaCertificate 1api-339160012Ainda não há avaliações
- Pythiosis Insidiosum7-12cDocumento1 páginaPythiosis Insidiosum7-12cdmestrinerAinda não há avaliações
- Guide Questions For NCM 107Documento4 páginasGuide Questions For NCM 107Miguel LigasAinda não há avaliações
- SarcomaDocumento2 páginasSarcomaedrichaAinda não há avaliações
- Cross Sectional Studies Hemed 2015Documento12 páginasCross Sectional Studies Hemed 2015delovinaAinda não há avaliações
- Pros and Cons of Continuing Nursing EducationDocumento14 páginasPros and Cons of Continuing Nursing EducationstanleyAinda não há avaliações
- 2018 Jordanian Conference BookletDocumento51 páginas2018 Jordanian Conference BookletAurelian Corneliu MoraruAinda não há avaliações
- Acupuncture (Presentation) by Zheng JiayinDocumento15 páginasAcupuncture (Presentation) by Zheng Jiayinpaperbin100% (1)
- Paramyxovir Idae: Disease/Viral FactorsDocumento22 páginasParamyxovir Idae: Disease/Viral FactorsMary ChristelleAinda não há avaliações
- PNM Shaiha KKBB 2023Documento15 páginasPNM Shaiha KKBB 2023haslinda84Ainda não há avaliações
- Health Services Available To The Students/Trainees: Tel. No. (088) 564-5172Documento1 páginaHealth Services Available To The Students/Trainees: Tel. No. (088) 564-5172Edsoney M. DiagosoAinda não há avaliações
- Nursing Board Review Medical SurgicalDocumento9 páginasNursing Board Review Medical SurgicalPhilip Simangan0% (1)
- Making Every School A Health-Promoting School: Implementation GuidanceDocumento89 páginasMaking Every School A Health-Promoting School: Implementation GuidancePablo MateusAinda não há avaliações
- Modified Hemorrhoidal Artery Ligation Malang Procedure As An Alternative Therapy in Management of Haemorrhoid Grade IIIDocumento4 páginasModified Hemorrhoidal Artery Ligation Malang Procedure As An Alternative Therapy in Management of Haemorrhoid Grade IIIInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- HR Report For Handing OverDocumento19 páginasHR Report For Handing OverSimon DzokotoAinda não há avaliações
- GEMS Presentation: Health Market InquiryDocumento47 páginasGEMS Presentation: Health Market InquiryYash RohiraAinda não há avaliações
- Naeyc Standard 1Documento1 páginaNaeyc Standard 1api-265296849Ainda não há avaliações
- Learners Individual Reading Assessment ToolDocumento7 páginasLearners Individual Reading Assessment ToolMhen AcenasAinda não há avaliações
- Faktor-Faktor Yang Berhubungan Dengan Kualitas Handover Pasien Di Ruang Rawat Inap Rumah SakitDocumento6 páginasFaktor-Faktor Yang Berhubungan Dengan Kualitas Handover Pasien Di Ruang Rawat Inap Rumah SakitAyu PurbaAinda não há avaliações
- 10 Physical and Mental Benefits of BasketballDocumento4 páginas10 Physical and Mental Benefits of BasketballJohn Kenzo NavatoAinda não há avaliações
- Team Work in Palliative Care: Ns. Endah Panca Lydia F, MkepDocumento15 páginasTeam Work in Palliative Care: Ns. Endah Panca Lydia F, Mkepyana suryanaAinda não há avaliações
- It's Perfectly NormalDocumento4 páginasIt's Perfectly NormalEric Fuseboxx50% (4)
- Contracted Pelvis by KABERA ReneDocumento14 páginasContracted Pelvis by KABERA ReneKABERA RENEAinda não há avaliações
- Nur 111 Session 17 Sas 1Documento8 páginasNur 111 Session 17 Sas 1Zzimply Tri Sha UmaliAinda não há avaliações
- BioF5-4.4 Contribution of Science and Technology To Human ReproductionDocumento24 páginasBioF5-4.4 Contribution of Science and Technology To Human ReproductionteahockAinda não há avaliações
- Alcohol Treatment CodesDocumento3 páginasAlcohol Treatment CodesMia JacksonAinda não há avaliações
- Burning Mouth SyndromeDocumento28 páginasBurning Mouth SyndromeMelissa KanggrianiAinda não há avaliações
- Drexel University: Commencement Ceremonies College of MedicineDocumento25 páginasDrexel University: Commencement Ceremonies College of MedicineChimpAinda não há avaliações
- Cure For Cancer or Placebo Effect!Documento3 páginasCure For Cancer or Placebo Effect!samantha willisAinda não há avaliações
- Reikalingi ISO StandartaiDocumento2 páginasReikalingi ISO StandartaiIndreAinda não há avaliações
- The China Study Diiet Plan - MP TiwariDocumento3 páginasThe China Study Diiet Plan - MP Tiwarirajanlko100% (1)