Escolar Documentos
Profissional Documentos
Cultura Documentos
PIRO Score For Community-Acquired Pneumonia - Articulo Cohorte
Enviado por
ChangTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
PIRO Score For Community-Acquired Pneumonia - Articulo Cohorte
Enviado por
ChangDireitos autorais:
Formatos disponíveis
See
discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/23712126
PIRO score for community-acquired
pneumonia: A new prediction rule for
assessment of severity in intensive care unit
patients with community-acquired
pneumonia
ARTICLE in CRITICAL CARE MEDICINE JANUARY 2010
Impact Factor: 6.15 DOI: 10.1097/CCM.0b013e318194b021 Source: PubMed
CITATIONS DOWNLOADS VIEWS
62 980 202
6 AUTHORS, INCLUDING:
Jordi Rello Thiago Lisboa
VHIR Vall dHebron Research Institute Universidade Federal do Rio Grande do Sul
275 PUBLICATIONS 8,061 CITATIONS 96 PUBLICATIONS 1,478 CITATIONS
SEE PROFILE SEE PROFILE
Manel Lujn Richard G Wunderink
Corporaci Sanitria Parc Taul Northwestern University
46 PUBLICATIONS 640 CITATIONS 245 PUBLICATIONS 9,299 CITATIONS
SEE PROFILE SEE PROFILE
Available from: Manel Lujn
Retrieved on: 17 June 2015
PIRO score for community-acquired pneumonia: A new prediction
rule for assessment of severity in intensive care unit patients with
community-acquired pneumonia*
Jordi Rello, MD, PhD; Alejandro Rodriguez, MD, PhD; Thiago Lisboa, MD; Miguel Gallego, MD;
Manel Lujan, MD; Richard Wunderink, MD, PhD
Objective: To develop a severity assessment tool to predict vivors than in survivors (4.6 1.2 vs. 2.3 1.4). Considering the
mortality in community-acquired pneumonia (CAP) patients in observed mortality for each PIRO score, the patients were strat-
intensive care unit (ICU), comparing its performance with Acute ified in four levels of risk: a) Low, 0 2 points; b) Mild, 3 points; c)
Physiology and Chronic Health Evaluation (APACHE) II score and high, 4 points; and d) Very high, 5 8 points. Mild-risk (hazard
American Thoracic Society/Infectious Disease Society of America ratio HR 1.8; 95% confidence interval CI 1.12.9; p < 0.05),
(ATS/IDSA) criteria as a prognostic index in CAP patients requiring high-risk (HR 3.1; 95% CI 2.0 4.7; p < 0.001), and very high
ICU admission. risk levels (HR 6.3; 95% CI 4.29.4; p < 0.001) were signifi-
Design: Secondary analysis of prospective observational co- cantly associated with higher risk of death in Cox proportional
hort study. hazards regression analysis. Furthermore, analysis of variance
Setting: Thirty-three ICUs. showed that higher levels of PIRO score were significantly asso-
Patients: Five hundred and twenty-nine adult patients with ciated with higher mortality (p < 0.001), prolonged length of stay
CAP requiring ICU admission. in the ICU (p < 0.001), and days of mechanical ventilation (p <
Measurements and Main Results: A severity assessment score 0.001). Receiver operating characteristic curves showed that PIRO
was developed based on the PIRO (predisposition, insult, re- score (area under the curve [AUC] 0.88) performed better than
sponse, and organ dysfunction) concept including the presence of APACHE II (AUC 0.75, p < 0.001) and ATS/IDSA criteria (AUC
the following variables: Comorbidities (chronic obstructive pul- 0.80, p < 0.001) to predict 28-day mortality.
monary disease, immunocompromise); age >70 years; multilobar Conclusions: The PIRO score performed well as 28-day mor-
opacities in chest radiograph; shock, severe hypoxemia; acute tality prediction tool in CAP patients requiring ICU admission with
renal failure; bacteremia and acute respiratory distress syndrome. a better performance than APACHE II and ATS/IDSA criteria in this
PIRO score was obtained at ICU within 24 hours from admission, subset of patients. Furthermore, PIRO score also is associated
and one point was given for each present feature (range, 0 8 with increased healthcare resource utilization in CAP patients
points). The mean PIRO score was significantly higher in nonsur- admitted in the ICU. (Crit Care Med 2009; 37:456 462)
T he pneumonia severity index department. Patients in class V (130 ence sponsored by Society of Critical Care
(PSI) was designed to classify points) have the highest severity, with an Medicine, European Society of Intensive
patients with community-ac- estimated mortality of 27%. This is a het- Care Medicine, American College of
quired pneumonia (CAP) to erogeneous group of patients with a wide Chest Physicians, ATS, and Surgical In-
guide home discharge at the emergency range of severity, and 2 of 3 remain out of fection Society and provided the basis for
the intensive care unit (ICU) (1). The Amer- introducing PIRO as a hypothesis-gener-
ican Thoracic Society (ATS)-revised criteria ating model for future research (6). It was
*See also p. 744. (2) and the CURB-65 (confusion, urea, re- inspired in the TNM system (7), which
From the Critical Care Department (JR, AR, TL), spiratory rate, blood pressure, and age 65 classifies malignant tumor grade, and
Joan XXIII University Hospital, University Rovira and
Virgili, Institut Pere Virgili, CIBER Enfermedades Res- years) score (3) are better to assist decisions was developed to denote the extent of
piratorias, Tarragona, Spain; Pneumology Department regarding site of care. Unfortunately none pathologic involvement, stratify thera-
(MG, ML), Corporacio Sanitaria Parc Taul, Sabadell, of the scores stratify patients with high peutic approaches, and predict outcome.
Spain; and Pulmonary and Critical Care Division (RW), severity. A score identifying different levels The elements of the PIRO concept (6) are
Northwestern University Hospital, Chicago, IL.
Supported, in part, by 06/06/36 from Fondo de
of risk would be useful to improve decision predisposition (chronic illness, age, and
Investigaciones Sanitarias (CIBERes Enfermedades making in terms of the most appropriate comorbidities); insult (injury, bactere-
Respiratorias) and by 2005/SGR/920 from AGAUR. treatment site, comparison in clinical tri- mia, endotoxin); response (neutropenia,
The authors has not disclosed any potential con- als, and better define criteria to indicate hypoxemia, hypotension); and organ dys-
flicts of interest.
For information regarding this article, E-mail:
adjuvant therapies. The use of biologi- function.
jordi.rello@urv.cat or jrello.hj23.ics@gencat.net cal (4) or physiologic (5) markers re- In this article, we hypothesize that
Copyright 2009 by the Society of Critical Care mains premature. improvements in the management of
Medicine and Lippincott Williams & Wilkins In 2003, an international panel of ex- ICU patients with severe CAP (SCAP)
DOI: 10.1097/CCM.0b013e318194b021 perts participated in a consensus confer- may follow the development of a stag-
456 Crit Care Med 2009 Vol. 37, No. 2
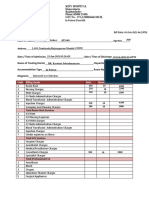
Table 1. Variables included in PIRO score for community-acquired pneumonia evidence of pneumonia as primary diagnosis,
confirmed by chest radiograph and clinical
Score Variables Point findings. The study focused on patients in the
ICU and excluded patients with respiratory
Predisposition Comorbidities (chronic obstructive pulmonary disease or 1
infection other than pneumonia (e.g., exacer-
immunocompromise)
70 yrs 1 bation of chronic obstructive pulmonary dis-
Insult Bacteremia 1 ease). A wide range of demographic, clinical,
Multilobar opacities in chest radiograph 1 and laboratory measures were recorded in
Response Shock 1.1 each patient, as described elsewhere (10).
Severe hypoxemia Patients were observed until death or ICU
Organ dysfunction Acute renal failure acute respiratory distress syndrome 1.1
Score range 08 discharges. Following Food and Drug Admin-
istration recommendations for clinical trials,
PIRO, predisposition, insult, response, and organ dysfunction. 28-day survival was chosen as primary end-
point. Patients discharged from the ICU before
90 28 days were considered as survivors.
The CAPUCI database was used to develop
80 76.6
the severity assessment model based on the
PIRO concept (6). The variables used in the
70
new score (chronic obstructive pulmonary dis-
60 56.1 ease, immunocompromise, multilobar opaci-
Mortality rate (%)
ties in chest radiograph, shock, severe hypox-
50 emia, and acute renal failure) were selected
from the current literature as the more signif-
40 34.4 icant in CAP prognosis (10 12) or because
30 25 they were considered with clinical importance
(bacteremia and acute respiratory distress syn-
20 17.1
12.6
drome). A clinical predictor rule (PIRO score
7.8 for CAP) was subsequently calculated at ICU
10
within 24 hours from admission, and one
0 point was given for each feature that was
0 to 5 6 to 10 11 to 15 16 to 20 21 to 25 26 to 30 more 31 present (range, 0 8 points) (Table 1). In ad-
dition, the severity of illness was assessed by
APACHE II Score (points) APACHE II (8) and by 2007 ATS/IDSA criteria
Figure 1. Twenty-eight-day mortality rate according Acute Physiology and Chronic Health Evaluation (9) for each patient at ICU admission.
(APACHE) II score in 529 patients with community-acquired pneumonia. Definitions. CAP was defined as an acute
lower respiratory tract infection characterized
by a) an acute pulmonary infiltrate evident on
Table 2. Incidence and associated mortality with Our objectives were to develop an as- chest radiographs and consistent with pneu-
PIRO score variables sessment tool to enable the stratification monia; b) confirmatory findings on clinical
of critically ill patients with CAP into examination; and c) acquisition of the infec-
Incidence Mortality
Variables n (%) OR Univariate mortality risk groups to compare the per- tion outside a hospital, long-term care facility,
formance of the PIRO score with the or nursing home (10).
Comorbidities 258 (48.8) 1.9 (1.32.8) Acute Physiology and Chronic Health Immunocompromise was defined as pri-
70 yrs 163 (30.8) 1.9 (1.32.9) mary immunodeficiency or immunodeficiency
Bacteremia 89 (16.8) 1.8 (1.12.8) Evaluation (APACHE) II score (8) and
secondary to radiation treatment, use of cyto-
Multilobar 250 (47.3) 4.2 (2.76.3) 2007 ATS/IDSA criteria (9) as a prognos-
opacities in toxic drugs or steroids (daily doses 20 mg of
tic index in ICU patients admitted with prednisolone or the equivalent for 2 weeks,
chest radiograph
Shock 270 (51.0) 12.4 (7.321.2) CAP and to evaluate prediction of PIRO or acquired immunodeficiency syndrome or
Severe hypoxemia 349 (66.0) 19.9 (8.646.1) score for healthcare resources utilization. malignancy (10). Multilobar compromise in
Acute renal failure 178 (33.6) 12.6 (8.119.8)
Acute respiratory 23 (4.3) 70.1 (9.91408.9)
chest radiograph was considered when more
distress METHODS than single lobe opacities were observed in
syndrome chest radiograph. Shock was defined as the
This is a historical cohort study including need for vasopressors for 4 hours after ade-
PIRO, predisposition, insult, response, and or- all patients with CAP requiring ICU admission quate fluid replacement (10, 12); Severe hy-
gan dysfunction. prospectively recorded in the CAPUCI Data- poxemia was defined as the PaO2/FIO2 ratio
base (10). Details of this study have been pre- 300 requiring mechanical ventilation (either
sented elsewhere (10 12). Briefly, 529 consec- invasive or noninvasive). Acute renal failure
ing system inspired in the PIRO con- utive patients with SCAP admitted in the ICU was defined as an urine output of 20 mL/hr
cept, which can better characterize the in 33 hospitals in Spain were enrolled. Insti- or a total urine output of 80 mL in 4 hours.
syndrome on the basis of predisposing tutional review board approval was obtained in Details of other definitions have been reported
factors and premorbid conditions, the accordance with local requirements, and in- elsewhere (5, 10 12).
nature of the underlying affection, the formed consent was waived because of the The 2007 ATS/IDSA criteria (9) were de-
characteristics of the host response, observational nature of the study. fined based on the presence of major criteria.
and the extend of the resultant organ The patients enrolled were consecutive pa- Major criteria are defined as requirement of
dysfunction. tients with age 18 years, with conclusive mechanical ventilation and presence of septic
Crit Care Med 2009 Vol. 37, No. 2 457
Table 3. Distribution of PIRO, Acute Physiology, and Chronic Health Evaluation II score and calculated in all patients. By convention, ac-
ATS/IDSA criteria in different subset of patients cording to the mortality rate observed, pa-
tients were classified into four levels of sever-
Acute Physiology ity: low, mild, high, and very high risk.
and Chronic Health The patients were stratified by PIRO score,
PIRO Score Evaluation II Score ATS/IDSA Major Criteria and ATS/IDSA major criteria presence and
survival curves were compared using Cox Pro-
Variable (n) Mean SD Mean SD 0 1 2 portional Hazards regression.
The operative indices (sensitivity, specific-
Survivors ity, positive, and negative predictive values) of
Yes 381 2.3 1.4 17.6 6.5 144 (97.3) 129 (87.8) 108 (46.2)
PIRO score were determined for different cut-
No 148 4.6 1.2a 23.6 6.6a 4 (2.7) 18 (12.2) 126 (53.8)a
Bacteremia off point, and the positive Likelihood ratio was
Yes 90 4.3 1.5 21.8 6.5 20 (13.5) 17 (11.6) 52 (22.2) calculated.
No 439 2.7 1.6a 18.7 7.0a 128 (86.5) 130 (88.4) 182 (78.8)a The discriminative power of APACHE II
Chronic obstructive score, ATS/IDSA criteria, and PIRO score for
pulmonary Disease CAP were assessed through measuring and
Yes 196 3.6 1.6 21.0 7.0 48 (32.4) 53 (36.1) 95 (40.6) pairwise comparing the area under the re-
No 333 2.6 1.6a 18.3 6.8a 100 (67.6) 94 (63.9) 139 (59.4) ceiver operating characteristic (ROC). The
Immunocompromise ROC curve was plotted for each score using
Yes 70 3.7 1.5 20.4 6.3 14 (9.5) 20 (13.6) 36 (15.4) sensitivity and specificity values for true pre-
No 459 2.8 1.7a 19.8 7.1 134 (90.5) 127 (86.4) 198 (84.6)
diction of ICU mortality across the whole
Age mt 70 yrs
Yes 163 3.9 1.6 22.2 6.1 39 (26.3) 45 (30.6) 79 (33.8) range of possible cut-off of predictive mortal-
No 366 2.5 1.6a 17.9 7.0a 109 (73.7) 102 (69.4) 155 (66.2) ity. The area under ROC (AUROC) curve was
Multilobar compromise considered a composite index of discrimina-
Yes 250 3.8 1.5 20.2 7.1 39 (26.3) 52 (35.3) 159 (67.9) tion (13). As AUROC approaches 1.0, the
No 279 2.1 1.4a 18.4 6.9a 109 (73.7) 95 (64.7) 75 (32.1)a model becomes more perfect; as the perfor-
Shock mance of the model become more random, the
Yes 270 4.1 1.3 21.6 7.1 0 (0) 38 (25.8) 234 (100) AUROC trends toward 0.5. All results were
No 259 1.7 1.1a 16.7 6.0a 148 (100) 109 (74.2) 0 (0)a tested against APACHE II score and ATS/IDSA
Severe hypoxemia
criteria. The results are expressed as odds ra-
Yes 349 3.7 1.4 20.7 7.1 5 (3.4) 111 (75.5) 234 (100)
No 180 1.4 1.1a 16.3 5.9a 143 (96.6) 36 (24.5) 0 (0)a tios and p values with 95% confidence inter-
Acute renal failure vals (CIs) and using ROC to plot sensitivity
Yes 178 4.5 1.2 23.0 6.5 12 (8.1) 29 (19.7) 137 (58.5) against specificity. The area under the curve,
No 351 2.1 1.3a 17.3 6.5a 136 (91.9) 118 (80.3) 97 (41.5)a standard error, and 95% CI are given and
Acute respiratory values were compared using the Students t
distress syndrome test. The chi-square test was used to compare
Yes 23 4.5 1.5 22.6 6.1 3 (2.0) 5 (3.4) 15 (6.4) proportions. The significance level of all anal-
No 506 2.9 1.7 19.1 7.0a 145 (98.0) 142 (96.6) 219 (93.6) ysis was defined as p 0.05.
ATS/IDSA, American Thoracic Society/Infectious Disease Society of America; PIRO, predisposition,
insult, response, and organ dysfunction. RESULTS
a
p 0.01.
The baseline characteristics of pa-
100 tients who did and did not survive to ICU
5 13 Alive have been reported elsewhere (10 12).
90 3 Dead The mean of APACHE II score at ICU
80
40
admission for all patients was 18.8 7.4,
Number of patients
70 being higher (p 0.01) in nonsurvivors
60 than survivors (22.9 7.6 vs. 17.4 6.8,
50 53 respectively). When the patients were dis-
91 87
86
40 0
tributed according to the APACHE II
30 scoring, the mortality rate increased sig-
53
20 37
nificantly (p 0.001) (Fig. 1).
26
10 22 Distribution and association with
5 8 mortality for each variable considered in
0 0
PIRO score are detailed in Table 2. Details
0 1 2 3 4 5 6 7 on distribution of the variables consid-
PIRO Score (points) ered for the PIRO score according to
Figure 2. Distribution of 529 patients according predisposition, insult, response, and organ dysfunc- APACHE II and ATS/IDSA major criteria
tion (PIRO) score and intensive care unit outcome. are shown in Table 3. When using ATS/
IDSA criteria, mortality decreased from
shock. Patients were classified as having 0, 1, The association between the PIRO score for 53% for patients with two major criteria,
or 2 major ATS/IDSA criteria. CAP and mortality was first assessed by strat- 12% with only one major criteria, and
Statistical Analysis. Data were analyzed ifying patients according to different levels of only 2.7% for patients admitted to the
using SPSS version 11.0 for windows (Chi- PIRO score and later into distinct risk groups. ICU with absence of major criteria. Dis-
cago, IL). Risk classes according to the PIRO score was tribution of 529 patients (survivors and
458 Crit Care Med 2009 Vol. 37, No. 2
100
100.0 shown). Presence of ATS/IDSA criteria
was also tested with Cox proportional re-
90 83.9
gression analysis, and the presence of 1
80
70.7 or 2 criteria was associated with higher
70 mortality (p 0.05) (Fig. 5). Finally,
Mortality rate (%)
60 discrimination of PIRO score for CAP was
p<0.001
50 43.0 assessed using ROC curves. The area un-
40 der ROC curve (Fig. 6) showed consistent
30 mortality discrimination by PIRO score
20
(0.88, 95% CI 0.83 0.9), with a better
13.0
performance than APACHE II score (0.75,
10 3.4 5.2
0.0 95% CI 0.70 0.80) and with a significant
0
difference between areas (p 0.001).
0 1 2 3 4 5 6 7 ATS/IDSA major criteria presence (area
under the curve 0.80, 95% CI 0.77
PIRO Score (points)
0.84) also shows significant difference be-
Figure 3. Twenty-eight-day mortality rate according predisposition, insult, response, and organ tween the areas (p 0.001).
dysfunction (PIRO) score for community-acquired pneumonia.
In survivors, medical resources utili-
zation (Table 7), evaluated using length
of stay in the ICU and mechanical venti-
nonsurvivors) according with PIRO score jor criteria are shown in Table 4. Table 5 lation days, increased significantly ac-
for CAP are shown in Figure 2. The mean shows predictive values for different cut- cording to level of risk defined by the
PIRO score for all patients was 2.9 1.7, off points of PIRO score. A PIRO score PIRO score (Fig. 7).
being significantly higher (p 0.001) in cut-off 4 points was associated with the
nonsurvivors than survivors (4.6 1.2 best performance to predict death with a DISCUSSION
vs. 2.3 1.4, respectively). When the sensitivity of 86% and specificity of 76%.
patients were distributed according PIRO Considering the observed mortality for This is the first study designed to assess
scoring, the mortality rate increased sig- each PIRO score (Fig. 3), the patients were the usefulness of a score inspired in the
nificantly (p 0.001) (Fig. 3). There was stratified in four levels of risk: a) Low, 0 2 PIRO concept to stratify critically ill pa-
no difference in PIRO score between early points; b) Mild, 3 points; c) high, 4 points; tients with CAP. Our findings support that
or late ICU mortality in SCAP patients. and d) Very high, 5 8 points. In the uni- this score, based on the PIRO concept (6,
Distribution and mortality of patients ac- variate analysis (Table 6) the mild, high, 14 17), is feasible for stratification of se-
cording to the presence of ATS/IDSA ma- and very high risk levels were associated verity and improved prediction of 28-days
with significantly higher risk of death. mortality when compared with the
The effect of each PIRO risk levels was APACHE II score (8) and the 2007 ATS/
Table 4. Mortality according to presence of ATS/ tested with the Cox proportional hazards IDSA criteria (9) for CAP severity. Further-
IDSA major criteria more, it was useful to predict healthcare
regression analysis, and it showed that
mild (hazard ratio 1.8; 95% CI 1.12.9; utilization (length of stay in the ICU and
Risk According
ATS/IDSA Criteria n (%) Death (%) p 0.05), high (hazard ratio 3.1; 95% CI requirement of mechanical ventilation).
2.0 4.7; p 0.001), and very high risk The PIRO concept (6, 14 17) has
Absence of major 148 (28.0) 4 (2.7) level (hazard ratio 6.3; 95% CI 4.29.4; arisen as a classification scheme for sep-
criteria p 0.001) were significantly associated sis that considers the predisposing con-
One major criteria 147 (27.8) 18 (12.2)
with higher risk of death (Fig. 4). This ditions, the nature and extent of insult,
Two major criteria 234 (44.2) 126 (53.8) the nature and magnitude of the host
association remained significant when
the model was adjusted by the severity of response, and the degree of concomitant
ATS/IDSA, American Thoracic Society/Infec-
organ dysfunction. Our score was build
tious Disease Society of America. illness (APACHE II score) (data no
based in this concept and has included
variables significantly associated with
Table 5. Test characteristics of PIRO score for mortality in 529 patients hospitalized with severe mortality in univariate analysis in our
community-acquired pneumonia database of SCAP patients admitted to
ICU. These parameters selected were
Positive Negative Positive based on prior evidence supporting its
PIRO Score Sensitivity Specificity Predictive Predictive Likelihood association with poor prognosis and fit
(n 529) (%) (%) Value (%) Value (%) Ratio
with the PIRO definitions.
mt 1 100 10 30 100 1.1 A potential strength of our study is the
2 98 32 36 98 1.4 simplicity of the PIRO score. It is based
3 95 56 46 96 2.1 on easily available variables, all with
4 86 79 61 93 4.0 known impact in the CAP mortality. It
5 59 93 76 85 8.3
allows an easy risk stratification of pa-
6 23 99 87 77 17.5
7 5 100 100 73 NA tients in different levels of severity with
progressive rates of mortality. Further-
PIRO, predisposition, insult, response, and organ dysfunction. more, it is also associated with progres-
Crit Care Med 2009 Vol. 37, No. 2 459
Table 6. Univariate analysis for mortality of different PIRO score level of risk sive increment in medical resources uti-
lization in ICU. Optimize therapy based
Univariate Analysis
on this classification is a strategy that
Risk According PIRO Score n (%) Death (%) OR (95%CI) should be evaluated, as patients at higher
risk might benefit from more aggressive
Low risk (02 points) 222 (42.0) 8 (3.6) 1 strategies or adjuvant therapy (e.g., cor-
Mild risk (3 points) 100 (18.9) 13 (13.0) 4.0 (1.610.0) ticosteroids).
High risk (4 points) 93 (17.6) 40 (43.0) 20.2 (8.945.7) The use of scores to evaluate CAP se-
Very high risk (58 points) 114 (21.5) 87 (76.3) 86.2 (37.7197.0)
verity is a useful strategy to identify sub-
sets of patients likely to need more com-
plex local healthcare setting. The
majority of studies assessing severity in
1,0 CAP patients are done in emergency set-
LOW ting. The PSI was described by Fine et al
(18) and aimed to identify patients who
MILD could be discharged home with safety. It
0,8
overestimates age and can underestimate
severity, particularly in patients without
Cumulative survival
HIGH
comorbidities. There is no validation
0,6 study evaluating the impact of the need of
ICU based on PSI index. Recently, Valen-
cia et al (1) showed that only 20% of PSI
VERY HIGH
class V patients are admitted to the ICU,
0,4 which shows that many patients classified
as severe based in this score may be not
so severe. The CURB-65 score based on
0,2
confusion, urea, respiratory rate, blood
pressure, and age and its variations are
easier to use and predict mortality well
(3, 20 22). However, this score per-
0,0 formed poorly when needed for ICU ad-
mission was the endpoint (23).
0 4 8 12 16 20 24 28 Our results also show that presence of
Days major ATS/IDSA criteria (9) was associ-
ated with higher mortality. Several stud-
Figure 4. Survival graph (Cox analysis) for 529 patients stratified by predisposition, insult, response,
and organ dysfunction score (censored at 28 days).
ies have already evaluated these criteria
but never in a subset of ICU patients.
However, a more detailed evaluation tool
such as PIRO-based score may add useful
1,0 0 major criteria
information and allow a more accurate
1 major criteria
prediction in this group of patients. The
APACHE II (8) is not a specific score to
0,8 evaluate severity in CAP patients. How-
ever, Kollef et al (24) evaluated APACHE
II accuracy to predict mortality in pa-
Cumulative Survival
0,6 tients with methicilin-resistant Staphylo-
2 major criteria
coccus aureus pneumonia and found that
APACHE II score has better accuracy
0,4
when compared with CURB-65 and CRB-
65. This difference was present in com-
munity-acquired methicilin-resistant
Staphylococcus aureus pneumonia and
0,2
health care-associated methicilin-resis-
tant Staphylococcus aureus pneumonia,
demonstrating the utility of this tool to
0,0 predict mortality in this subset of pa-
tients. Furthermore, APACHE II is the
0 4 8 12 16 20 24 28
most widely employed score to evaluate
Days risk of death in intensive care and has
Figure 5. Survival graph (Cox analysis) for 529 patients stratified by presence of American Thoracic been validated in different subsets of pa-
Society/Infectious Disease Society of America major criteria (censored at 28 days). tients (2527).
460 Crit Care Med 2009 Vol. 37, No. 2
1,0 patients. Identifying the subset of critically
ill patients with SCAP likely to have adverse
PIRO Score APACHE II Score
outcomes seems to be a key step in reduc-
0,8 ing morbidity and mortality.
Our study has several limitations. Al-
though all selected variables were signif-
icantly associated with mortality, they
Sensitivity
0,6
were selected arbitrarily. Furthermore,
the same weight (presence/absence) was
adjudicated for each variable, although
0,4
ATS/IDSA odds ratios in univariate analysis were
Criteria
different, to enhance simplicity. Under
these conditions, PIRO score performed
0,2 very well and predicted 28-day mortality
in ICU patients, which is better than
other available tools, such as APACHE II
0,0 (8) and ATS/IDSA criteria (9). Indeed, a
0,0 0,2 0,4 0,6 0,8 1,0 clinically useful set of criteria for evalu-
1- Specificity ating infected patients will necessarily be
Figure 6. Receiver operating characteristic curves comparing predisposition, insult, response, and organ somewhat arbitrary. It must be judged
dysfunction (PIRO) score, American Thoracic Society/Infections Disease Society of America (ATS/IDSA) successful if clinicians regard them as an
criteria, and Acute Physiology and Chronic Health Evaluation (APACHE) II to predict 28-day mortality. aid for decision making at the bedside (6).
Further studies should validate PIRO
Table 7. Healthcare resource utilization in survivors, according to risk levels, defined by PIRO score score in populations with different de-
grees of severity and for hospital mortal-
Intensive Care Unit Length of Stay Mechanical Ventilation Days ity and 90-day mortality rates. Whether
our findings may be extrapolated to pa-
Level of Risk Median Median
PIRO Score Mean (SD) (Interquartile Range) Mean (SD) (Interquartile Range)
tients out of the ICU (e.g., emergency
department) is unknown. Unfortunately,
Low 10.3 (9.0) 7 (413) 4.0 (7.0) 1.0 (05) we were not able to establish compari-
Mild 19.4 (15.4)a 15 (827) 12.4 (13.5)a 8 (217) sons with PSI (18) or CURB (19) or
High 22.1 (21.0)a 14 (629) 16.5 (20.4)a 10 (423) APACHE IV scores (28) as we do not have
Very high 26.0 (23.8)a 22 (929) 17.8 (19.0)a 10 (522)
these data collected. However, an original
PIRO, predisposition, insult, response, and organ dysfunction. aspect of our study was to evaluate SCAP
a
p 0.05 (analysis of variance). patients admitted to ICU, although PSI
Interquartile range 2575. (18) and CURB score (19) have not been
adequately validated in this population.
Days MV LOS ICU Another potential limitation is the ab-
28 26 sence of protocolized criteria for ICU ad-
mission between different institutions.
22.1
This is because of the absence of gold
21 19.4
17.8 standard or definitive criteria to define
p<0.001 16.5
ICU admission (1). These decisions are
Days
14 12.8 12.4 mainly based on clinical judgment, and
8.9 its variability may limit the potential gen-
7.3
7 5.9 eralization of our findings. Further stud-
3.3 ies should clarify this issue.
1.3
In conclusion, we developed a severity
0
assessment score for CAP patients based on
0 1 2 3 4 >5 the PIRO concept (6, 14 17), which ade-
PIRO score quately predicted 28-day mortality in CAP
Figure 7. Length of stay (LOS) in intensive care unit (ICU) and mechanical ventilation (MV) days on patients admitted to ICU. Furthermore, be-
survivors according to predisposition, insult, response, and organ dysfunction (PIRO) score. ing associated with increment in medical
resources utilization in ICU, it performed
better than the APACHE II score (8) and
A very conflicting issue in CAP is def- vere community-acquired pneumonia pa- ATS/IDSA criteria (9) to identify patients
inition of SCAP. None of the scores till tients in the emergency department. How- with higher risk of death. Its simplicity may
date has focused on SCAP patients admitted ever, in this study, only 4% of patients were help to stratify patients with PSI above 130
to ICU. The available CAP severity assess- admitted to ICU, and in-hospital mortality (class V) in different categories of severity,
ment scores do not include ICU patients was less than 10%. All our patients were being useful for pharmacoeconomic or out-
significantly. Espana et al (20) describe a admitted in the ICU, and overall mortality come comparisons, and to select candidates
clinical prediction rule for identifying se- was 28%, a much more severe subset of for adjunctive therapy in clinical trials.
Crit Care Med 2009 Vol. 37, No. 2 461
REFERENCES 10. Bodi M, Rodrguez A, Sole-Violan J, et al: Development and validation of a clinical pre-
Antibiotic prescription for community- diction rule for severe community-acquired
1. Valencia M, Badia JR, Cavalcanti M, et al: acquired pneumonia in the intensive care pneumonia. Am J Respir Crit Care Med 2006;
Pneumonia severity index class V patients unit: Impact of adherence to Infectious Dis- 174:1249 1256
with community-acquired pneumonia: Char- ease Society of America guidelines on sur- 21. Angus DC, Marrie TJ, Obrosky DS, et al:
acteristics, outcomes and value of severity vival. Clin Infect Dis 2005; 41:1709 1716 Severe community-acquired pneumonia: Use
scores. Chest 2007; 132:515522 11. Rello J, Rodrguez A, Torres A, et al: Impli- of intensive care services and evaluation of
2. Ewig S, Ruiz M, Mensa J, et al: Severe com- cations of COPD in patients admitted to the American and British Thoracic Society diag-
munity-acquired pneumonia: Assessment of intensive care unit by community-acquired nostic criteria. Am J Respir Crit Care Med
severity criteria. Am J Respir Crit Care Med pneumonia. Eur Respir J 2006; 27: 2002; 166:717723
1998; 158:11021108 1210 1216 22. Bauer TT, Ewig S, Marrie R, et al; the CAP-
3. Lim WS, van del Eerden MM, Laing R, et al: 12. Rodrguez A, Mendia A, Sirvent J-M, et al: NETZ Study Group: CRB-65 predicts death
Defining community acquired pneumonia Combination antibiotic therapy improves from community-acquired pneumonia. J Int
severity on presentation to hospital: An in- survival in patients with community-ac- Med 2006; 260:93101
ternational derivation and validation study. quired pneumonia and shock. Crit Care Med 23. Feldman C: Prognostic scoring system:
Thorax 2003; 58:377378 2007; 35:14931498 Which one is best? Curr Opin Infect Dis
4. Rello J, Rodrguez A: Severity of illness as- 13. Hanley J, McNeil B: The meaning and the use 2007; 20:165169
sessment for managing community-acquired of the area under a receiver operating char- 24. Kollef KE, Reichley RM, Micek ST, et al: The
pneumonia. Intensive Care Med 2007; 33: acteristic (ROC) curve. Radiology 1982; 143: modified APACHE II score outperforms
20432044 29 36 CURB65 pneumonia severity score as a pre-
5. Blot S, Rodrguez A, Sole-Violan J, et al: 14. Angus DC, Burgner D, Wunderink R, et al: dictor of thirty-day mortality on methicillin-
Effects of delayed oxygenation assessment on The PIRO concept: P is for predisposition. resistant Staphylococcus aureus pneumonia.
time to antibiotic delivery and mortality in Crit Care 2003; 7:248 251 Chest 2007; In Press
patients with severe community-acquired 15. Vincent JL, Opal S, Torres A, et al: The PIRO 25. Kaya E, Dervisoglu A, Polat C: Evaluation of
pneumonia. Crit Care Med 2007; 35: concept: I is for infection. Crit Care 2003; diagnostic findings and scoring systems in
2509 2514 7:252255 outcome prediction in acute pancreatitis.
6. Levy MM, Fink MP, Marshall JC, et al: 2001 16. Gerlach H, Dhainaut JF, Harbarth S, et al: World J Gastroenterol 2007; 13:3090 3094
SCCM/ESICM/ACCP/ATS/SIS International The PIRO concept: R is for response. Crit 26. Niskanen M, Kari A, Nikki P, et al: Acute
sepsis definitions conference. Crit Care Med Care 2003; 7:256 259 physiology and chronic health evaluation
2003; 31:1250 1256 17. Vincent JL, Wendon J, Groeneveld J, et al: APACHE II Score and Glasgow coma score as
7. Denoix PX: Enquete permanent dans les cen- The PIRO concept: O is for organ dysfunc- predictors outcome from intensive care after
tres anticancereaux. Bull Inst Natl Hyg 1946; tion. Crit Care 2003; 7:260 264 cardiac arrest. Crit Care Med 1991; 19:
1:70 75 18. Fine MJ, Auble TE, Yealy DM, et al: A predic- 14651473
8. Knaus WA, Draper EA, Wagner DP, et al: tion rule to identify low-risk patients with 27. Grmec S, Gasparovic V: Comparison of
APACHE II: A severity of disease classifica- community-acquired pneumonia. N Engl APACHE II, MEES and Glasgow Coma
tion system. Crit Care med 1985; 13: J Med 1997; 336:243250 Scale in patients with nontraumatic coma
818 829 19. British Thoracic Society and the Public for prediction of mortality Crit Care 2001;
9. Mandell LA, Wunderink RG, Anzuetto A, et Health Laboratory Service: Community- 5:19 23
al: Infectious Disease Society of America/ acquired pneumonia in adults in British hos- 28. Zimmerman JE, Kramer AA, McNair DS, et
American Thoracic Society consensus guide- pitals in 19821983: A survey of aetiology, al: Acute Physiology and Chronic Health
lines on the management of community- mortality, prognostic factors and outcome. Q Evaluation (APACHE) IV: Hospital mortality
acquired pneumonia in adults. Clin Infect J Med 19876; 239:195220 assessment for todays critically ill patients.
Dis 2007; 44(Suppl 2):S27S72 20. Espana PP, Capelastegui A, Gorordo I, et al: Crit Care Med 2006; 34:12971310
462 Crit Care Med 2009 Vol. 37, No. 2
Você também pode gostar
- Hydatidiform Mole - Epidemiology, Clinical Features, and Diagnosis - UpToDateDocumento22 páginasHydatidiform Mole - Epidemiology, Clinical Features, and Diagnosis - UpToDateChangAinda não há avaliações
- Practice Bulletin: Medical Management of Ectopic PregnancyDocumento7 páginasPractice Bulletin: Medical Management of Ectopic PregnancyChangAinda não há avaliações
- JCPDocumento11 páginasJCPChangAinda não há avaliações
- RCOG Guidelines - Gestational Trophoblastic DiseaseDocumento12 páginasRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- Gestational Trophoblastic Disease - Pathology - UpToDateDocumento18 páginasGestational Trophoblastic Disease - Pathology - UpToDateChangAinda não há avaliações
- RHEUMATOLOGY GUIDE FOR DISEASES AND TREATMENTSDocumento15 páginasRHEUMATOLOGY GUIDE FOR DISEASES AND TREATMENTSkeyurbAinda não há avaliações
- Evaluation of Couples With Recurrent Pregnancy Loss - UpToDateDocumento8 páginasEvaluation of Couples With Recurrent Pregnancy Loss - UpToDateChangAinda não há avaliações
- Hydatidiform Mole - Management - UpToDateDocumento15 páginasHydatidiform Mole - Management - UpToDateChangAinda não há avaliações
- Spontaneous Abortion - Risk Factors, Eti..., and Diagnostic Evaluation - UpToDateDocumento24 páginasSpontaneous Abortion - Risk Factors, Eti..., and Diagnostic Evaluation - UpToDateChangAinda não há avaliações
- Ectopic Pregnancy - Incidence, Risk Factors, and Pathology - UpToDateDocumento15 páginasEctopic Pregnancy - Incidence, Risk Factors, and Pathology - UpToDateChangAinda não há avaliações
- Practice Bulletin: Medical Management of Ectopic PregnancyDocumento7 páginasPractice Bulletin: Medical Management of Ectopic PregnancyChangAinda não há avaliações
- Preterm Birth - Risk Factors and Interventions For Risk Reduction - UpToDateDocumento35 páginasPreterm Birth - Risk Factors and Interventions For Risk Reduction - UpToDateChangAinda não há avaliações
- Tiki Taka CK EndocrinologyDocumento17 páginasTiki Taka CK EndocrinologykeyurbAinda não há avaliações
- TiKi TaKa CK Preventive MedicineDocumento3 páginasTiKi TaKa CK Preventive MedicinenonsAinda não há avaliações
- Hepatology Tiki TakaDocumento19 páginasHepatology Tiki TakaChangAinda não há avaliações
- TikiTaka StatisticsDocumento37 páginasTikiTaka StatisticsChangAinda não há avaliações
- Practice Bulletin No 171 Management of Preterm.61 PDFDocumento10 páginasPractice Bulletin No 171 Management of Preterm.61 PDFLoreGGuerreroAinda não há avaliações
- Tiki Taka Notes Final PDFDocumento104 páginasTiki Taka Notes Final PDFAditiSahak62Ainda não há avaliações
- Rafa Gastrica 1 PDFDocumento37 páginasRafa Gastrica 1 PDFChangAinda não há avaliações
- Assessing The Learning Environment of A Faculty - Articulo ValidacionDocumento14 páginasAssessing The Learning Environment of A Faculty - Articulo ValidacionChangAinda não há avaliações
- Corticosteroids For Managing Tuberculous Meningitis (Review)Documento4 páginasCorticosteroids For Managing Tuberculous Meningitis (Review)ChangAinda não há avaliações
- Sensitivity and Specificity of The Semiquantitative Latex Agglutination - Articulo Prueba DXDocumento5 páginasSensitivity and Specificity of The Semiquantitative Latex Agglutination - Articulo Prueba DXChangAinda não há avaliações
- Article PDFDocumento25 páginasArticle PDFChangAinda não há avaliações
- Efficacy and Safety of Paracetamol For Spinal Pain and Osteoarthritis Meta-Analysis - Articulo Revisión Sistemática PDFDocumento13 páginasEfficacy and Safety of Paracetamol For Spinal Pain and Osteoarthritis Meta-Analysis - Articulo Revisión Sistemática PDFChangAinda não há avaliações
- Criterios Diagnosticos y Grado de Severidad ColecistitisDocumento12 páginasCriterios Diagnosticos y Grado de Severidad ColecistitisYoub Luis Caro RojasAinda não há avaliações
- Production in Progress PDFDocumento1 páginaProduction in Progress PDFChangAinda não há avaliações
- Laboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottDocumento29 páginasLaboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottChangAinda não há avaliações
- Guarino 2014Documento21 páginasGuarino 2014ChangAinda não há avaliações
- TG13 Updated Tokyo Guidelines For The Management of AcuteDocumento7 páginasTG13 Updated Tokyo Guidelines For The Management of AcutechizonaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Infection Control in ICU'sDocumento58 páginasInfection Control in ICU'stummalapalli venkateswara rao100% (1)
- Hospital Bill FormatDocumento2 páginasHospital Bill Formatsandee1910100% (1)
- Part One: Expressions (Items 1-15) Choose The Best Answer. Make-Up Class (1-3)Documento18 páginasPart One: Expressions (Items 1-15) Choose The Best Answer. Make-Up Class (1-3)หมิงฮวาAinda não há avaliações
- Hospital Case Study Max S.SDocumento8 páginasHospital Case Study Max S.SIqRa JaVedAinda não há avaliações
- ICU/CCU Only Competencies and Johns Hopkins MHA ICU ProjectDocumento107 páginasICU/CCU Only Competencies and Johns Hopkins MHA ICU Projecthery100% (2)
- Aplanando La CurvaDocumento6 páginasAplanando La CurvaJorge Alonso Pachas ParedesAinda não há avaliações
- Ballad Health Wise County Update Info SheetDocumento4 páginasBallad Health Wise County Update Info SheetAnonymous iBvi6lqXeUAinda não há avaliações
- Gordana Pavliša, Marina Labor, Hrvoje Puretić, Ana Hećimović, Marko Jakopović, Miroslav SamaržijaDocumento12 páginasGordana Pavliša, Marina Labor, Hrvoje Puretić, Ana Hećimović, Marko Jakopović, Miroslav SamaržijaAngelo GarinoAinda não há avaliações
- J Ijnurstu 2017 12 012Documento8 páginasJ Ijnurstu 2017 12 012Osborn KhasabuliAinda não há avaliações
- Use of Communication Tools For Mechanically Ventilated Patients in The Intensive Care UnitDocumento8 páginasUse of Communication Tools For Mechanically Ventilated Patients in The Intensive Care UnitCatalina CarreñoAinda não há avaliações
- Nurses' Knowledge and Practice Regarding Oral Care in Intubated Patients at Selected Teaching Hospitals, ChitwanDocumento8 páginasNurses' Knowledge and Practice Regarding Oral Care in Intubated Patients at Selected Teaching Hospitals, ChitwanAnonymous izrFWiQAinda não há avaliações
- McKenzie Aasfe 1st Place Division2Documento23 páginasMcKenzie Aasfe 1st Place Division2Margaret McKenzieAinda não há avaliações
- Peran Perawat Keperawatan KritisDocumento21 páginasPeran Perawat Keperawatan KritisRudi HariyonoAinda não há avaliações
- Anesthesia Analgesia September 2009Documento291 páginasAnesthesia Analgesia September 2009Alexandra PavloviciAinda não há avaliações
- Early Enteral NütritionDocumento9 páginasEarly Enteral NütritionSema NurAinda não há avaliações
- A P I C P C: A V U: Ospital Cquired Ressure Njuries in Ritical and Rogressive ARE Voidable Ersus NavoidableDocumento21 páginasA P I C P C: A V U: Ospital Cquired Ressure Njuries in Ritical and Rogressive ARE Voidable Ersus NavoidableDwi CahyoAinda não há avaliações
- 2020 Article 712Documento8 páginas2020 Article 712Agrinto TaloimAinda não há avaliações
- The Debate On The EThics of AI in Health Care Pre Print PDFDocumento35 páginasThe Debate On The EThics of AI in Health Care Pre Print PDFutkarsh kandpalAinda não há avaliações
- Nasal Cannula Vs Venturi MaskDocumento8 páginasNasal Cannula Vs Venturi MaskRoslitha HaryaniAinda não há avaliações
- SLEDDDocumento38 páginasSLEDDrini purwantiAinda não há avaliações
- Acute Care PDFDocumento509 páginasAcute Care PDFamatory1702Ainda não há avaliações
- Namachivayam 2012Documento9 páginasNamachivayam 2012dian rosmala lestariAinda não há avaliações
- NYCM Quill + Scope - Vol 3Documento102 páginasNYCM Quill + Scope - Vol 3burxardAinda não há avaliações
- Manpower Planning at Different LevelsDocumento13 páginasManpower Planning at Different Levelsdr_shilpa11Ainda não há avaliações
- Sedation and Analgesia in Critically Ill Neurologic PatientsDocumento24 páginasSedation and Analgesia in Critically Ill Neurologic PatientsrazaksoedAinda não há avaliações
- Ccs InfoDocumento13 páginasCcs Info786ss100% (1)
- Immediate Post Anesthetic RecoveryDocumento12 páginasImmediate Post Anesthetic Recoverysubvig100% (2)
- SMT ProfileDocumento12 páginasSMT ProfileTOHEEDAinda não há avaliações
- Guía Manejo Del Shock 2023Documento67 páginasGuía Manejo Del Shock 2023Alvaro ArriagadaAinda não há avaliações
- Presentation On Assessment of Patient in CCU: Presented byDocumento75 páginasPresentation On Assessment of Patient in CCU: Presented bySandhya HarbolaAinda não há avaliações