Escolar Documentos
Profissional Documentos
Cultura Documentos
Peptic Ulcer Bleeding Risk. The Role of Helicobacter: Pylori Infection in NSAID/Low-Dose Aspirin Users
Enviado por
Tiara Grhanesia DenashuryaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Peptic Ulcer Bleeding Risk. The Role of Helicobacter: Pylori Infection in NSAID/Low-Dose Aspirin Users
Enviado por
Tiara Grhanesia DenashuryaDireitos autorais:
Formatos disponíveis
684 ORIGINAL CONTRIBUTIONS nature publishing group
see related editorial on page x
Peptic Ulcer Bleeding Risk. The Role of Helicobacter
STOMACH
Pylori Infection in NSAID/Low-Dose Aspirin Users
C. Sostres, MD1, P. Carrera-Lasfuentes, PhD2, R. Benito, MD3, P. Roncales4, M. Arruebo, MD4, M.T. Arroyo, MD1, L. Bujanda, MD5,
L.A. Garca-Rodrguez, MD6 and A. Lanas, MD1, 2, 4
OBJECTIVES: Helicobacter pylori (H. pylori) infection and NSAID/low-dose aspirin (ASA) use are associated with
peptic ulcer disease. The risk of peptic ulcer bleeding (PUB) associated with the interaction of these
factors remains unclear. The objective of this study was to determine the risk of PUB associated
with the interaction between H. pylori infection and current nonsteroidal anti-inammatory drugs
(NSAIDs) or low-dose ASA use.
METHODS: This was a case-control study of consecutive patients hospitalized because of PUB. Controls were
matched by age, sex, and month of admission. H. pylori infection status was determined in all cases
and controls by serology. Drug use was determined by structured questionnaire. Adjusted relative
risk (RR) associated with different factors, and the interaction between NSAID/ASA and H. pylori
infection was estimated by logistic regression analysis.
RESULTS: The study included 666 cases of PUB and 666 controls; 74.3% cases and 54.8% controls (RR:
2.6; 95% condence interval (CI): 2.03.3) tested positive for H. pylori infection; 34.5% of cases
had current NSAID use compared with 13.4% of controls (RR: 4.0; 95% CI: 3.05.4). Respective
proportions for low-dose ASA use were 15.8 and 12%, respectively (RR: 1.9; 95% CI: 1.32.7). The
RR of PUB for concomitant NSAID use and H. pylori infection suggested an additive effect (RR: 8.0;
95% CI: 5.012.8), whereas no interaction was observed with ASA use (RR: 3.5; 95% CI: 2.06.1).
CONCLUSIONS: NSAID, low-dose ASA use, and H. pylori infection are three independent risk factors for the
development of PUB, but there were differences in the interaction effect between low-dose ASA
(no interaction) or NSAID (addition) use and H. pylori infection, which may have implications for
clinical practice in prevention strategies.
Am J Gastroenterol 2015; 110:684689; doi:10.1038/ajg.2015.98; published online 21 April 2015
INTRODUCTION NSAID sharing a number of pathogenic mechanisms, studies on
Helicobacter pylori (H. pylori) infection, nonsteroidal anti- the interaction between these two risk factors has yielded con-
inflammatory drugs (NSAIDs), and low-dose aspirin (ASA) use flicting data leaving this relationship uncertain (2). In addition,
are three independent and the most important modifiable risk in the last years, the use of low-dose ASA has increased as a result
factors in the pathogenesis of gastroduodenal peptic ulcers (1). In of accumulating evidence for its benefits in primary and sec-
clinical practice, the coincidence of H. pylori infection with the ondary prevention of cardiovascular and cerebrovascular events
intake of one of those drugs in the same patient is frequent and (35). Low-dose ASA damages the upper gastrointestinal (GI)
may have important clinical consequences. In this way, whether tract through both local and systemic effects (4,5). Although it
NSAID intake in the presence of H. pylori infection may fur- is commonly asserted that H. pylori infection will increase the
ther increase the risk of peptic ulcer is still under intense debate. risk of ASA-associated GI side effects, the impact and influence of
Clinicians might expect at least an additive if not a synergistic H. pylori infection on the incidence of upper GI bleeding (UGIB)
effect on the risk of peptic ulcer. However, despite H. pylori and in patients taking ASA is also still unclear (6). These conflicting
1
Universitary Hospital Lozano Blesa, Gastroenterology Unit, Zaragoza, Spain; 2CIBERehd, Madrid, Spain; 3Universitary Hospital Lozano Blesa, Microbiology
Unit, Zaragoza, Spain; 4Health Science Institute of Aragon, Zaragoza, Spain; 5Universitary Hospital of Donostia, San Sebastian, Spain; 6CEIFE, Madrid, Spain.
Correspondence: C. Sostres, MD, Universitary Hospital Lozano Blesa, Gastroenterology Unit, Calle San Juan Bosco 15, Zaragoza 50009, Spain.
E-mail: carlossostres@gmail.com
Received 13 October 2014; accepted 14 February 2015
The American Journal of GASTROENTEROLOGY VOLUME 110 | MAY 2015 www.amjgastro.com
Você também pode gostar
- Peptic Ulcer and Non-Steroidal Anti-Inflammatory: AgentsDocumento6 páginasPeptic Ulcer and Non-Steroidal Anti-Inflammatory: AgentsJon Wafa AzwarAinda não há avaliações
- 375 PDFDocumento7 páginas375 PDFHasnan HabibAinda não há avaliações
- Helicobacter Pylori Infection A Recent Approach ToDocumento13 páginasHelicobacter Pylori Infection A Recent Approach ToTha Vila Le ColloAinda não há avaliações
- Prevalence and Predictors of Gastritis Among Patients Attending Health Care Facilities in Jazan, KSADocumento8 páginasPrevalence and Predictors of Gastritis Among Patients Attending Health Care Facilities in Jazan, KSAShirleyAinda não há avaliações
- CDC Update On Gonorrhea: Expand Treatment To Limit ResistanceDocumento4 páginasCDC Update On Gonorrhea: Expand Treatment To Limit ResistanceFebyan AbotAinda não há avaliações
- Hazzard's Peptic UlcerDocumento10 páginasHazzard's Peptic UlcerAhmedAinda não há avaliações
- Fimmu 14 1091780Documento11 páginasFimmu 14 1091780e.claragg00Ainda não há avaliações
- Antiphospholipid Syndrome and Recurrent Miscarriage - A Systematic ReviewDocumento10 páginasAntiphospholipid Syndrome and Recurrent Miscarriage - A Systematic ReviewDelanaura PuspitasariAinda não há avaliações
- Saccharomyces Boulardii in Helicobacter Pylori Eradication in Children, A Randomized Trial From IranDocumento5 páginasSaccharomyces Boulardii in Helicobacter Pylori Eradication in Children, A Randomized Trial From IranJUAN SEBASTIAN AVELLANEDA MARTINEZAinda não há avaliações
- Complications of Proton Pump Inhibitor Therapy 2017Documento14 páginasComplications of Proton Pump Inhibitor Therapy 2017Ingrid Miroslava Reyes DiazAinda não há avaliações
- NIH Public Access: Pesticide Use and Incident Diabetes Among Wives of Farmers in The Agricultural Health StudyDocumento19 páginasNIH Public Access: Pesticide Use and Incident Diabetes Among Wives of Farmers in The Agricultural Health StudyNiken RahmatiaAinda não há avaliações
- A Prospective Observational Study of Prescribing Patterns in Peptic Ulcer DiseaseDocumento40 páginasA Prospective Observational Study of Prescribing Patterns in Peptic Ulcer DiseaseGeet MaanAinda não há avaliações
- Probiotic Allergic RhinitsDocumento7 páginasProbiotic Allergic Rhinitscharoline gracetiani nataliaAinda não há avaliações
- Overview of The Complications of Peptic Ulcer DiseaseDocumento27 páginasOverview of The Complications of Peptic Ulcer DiseaseIulia OpreaAinda não há avaliações
- Kavitt Robert T Diagnosis and Treatment of Peptic 2019Documento10 páginasKavitt Robert T Diagnosis and Treatment of Peptic 2019Nix Santos100% (1)
- Pylori 7Documento12 páginasPylori 7fprasasyaaAinda não há avaliações
- Out 28Documento18 páginasOut 28EndraAinda não há avaliações
- NSAID GastropathyDocumento16 páginasNSAID GastropathyNaswa ArviedaAinda não há avaliações
- Guidelines For Prevention of NSAID-Related Ulcer ComplicationsDocumento11 páginasGuidelines For Prevention of NSAID-Related Ulcer ComplicationsPeet UpAinda não há avaliações
- 5 Recent Trials in Stress Ulcer ProphylaxisDocumento6 páginas5 Recent Trials in Stress Ulcer ProphylaxisCharan Teja Reddy AvulaAinda não há avaliações
- Jurnal ManggisDocumento22 páginasJurnal ManggisAyundaAinda não há avaliações
- Hepatology - 2016 - Bagante - Cholangiocarcinoma Risk Factors and The Potential Role of AspirinDocumento3 páginasHepatology - 2016 - Bagante - Cholangiocarcinoma Risk Factors and The Potential Role of Aspirinsuraj rajpurohitAinda não há avaliações
- Antibiotic Prophylaxis in Cirrhosis: Good and Bad: ReviewsDocumento13 páginasAntibiotic Prophylaxis in Cirrhosis: Good and Bad: ReviewsGiani Herrera HurtadoAinda não há avaliações
- Righi (2016)Documento6 páginasRighi (2016)PelagyalAinda não há avaliações
- TerjemahanDocumento4 páginasTerjemahanEduard YoshinoAinda não há avaliações
- Helicobacter Pylori, Homologous-: Recombination Genes, and Gastric CancerDocumento10 páginasHelicobacter Pylori, Homologous-: Recombination Genes, and Gastric CancerCarla ZuritaAinda não há avaliações
- Practice Guidelines for Candidiasis TreatmentDocumento17 páginasPractice Guidelines for Candidiasis TreatmentCristian HaesbaertAinda não há avaliações
- Chapter 2 (Abeleda)Documento2 páginasChapter 2 (Abeleda)John Patrick AbeledaAinda não há avaliações
- The Rise and Decline of Nonsteroidal Antiinflammatory Drug-Associated Gastropathy in Rheumatoid ArthritisDocumento8 páginasThe Rise and Decline of Nonsteroidal Antiinflammatory Drug-Associated Gastropathy in Rheumatoid ArthritiscthjgfytvfnoAinda não há avaliações
- PatoDocumento10 páginasPatoYiro YazawaAinda não há avaliações
- Global Prevalence of Norovirus in Cases of Gastroenteritis: A Systematic Review and Meta-AnalysisDocumento6 páginasGlobal Prevalence of Norovirus in Cases of Gastroenteritis: A Systematic Review and Meta-AnalysisSeruni Allisa AslimAinda não há avaliações
- Brauchli2008 2Documento9 páginasBrauchli2008 2jungHAENAAinda não há avaliações
- Helicobacter PyloriDocumento14 páginasHelicobacter PyloriRaisa AriesthaAinda não há avaliações
- Peptic Ulcer Case Study 1Documento9 páginasPeptic Ulcer Case Study 1Alejandro Daniel Landa MoralesAinda não há avaliações
- 04 Chapter 1Documento5 páginas04 Chapter 1fafafsf hshsAinda não há avaliações
- NIH Public Access: Author ManuscriptDocumento21 páginasNIH Public Access: Author ManuscriptgiannidietAinda não há avaliações
- Content ServerDocumento14 páginasContent ServerNourma Kusuma WinawanAinda não há avaliações
- Asthma Under Control Is Inversely Related With Erosive Esophagitis Among Healthy AdultsDocumento12 páginasAsthma Under Control Is Inversely Related With Erosive Esophagitis Among Healthy AdultsSagena Nurul CarismaAinda não há avaliações
- Concise Definitive Review: Stress Ulcer ProphylaxisDocumento11 páginasConcise Definitive Review: Stress Ulcer ProphylaxisMuhammad Umar RazaAinda não há avaliações
- Longitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionDocumento11 páginasLongitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionMITA RESTINIA UINJKTAinda não há avaliações
- Ni Hms 925820Documento18 páginasNi Hms 925820Anna Puteri GozaliAinda não há avaliações
- Cancer Medicine: Pioglitazone and Bladder Cancer Risk: A Systematic Review and Meta-AnalysisDocumento11 páginasCancer Medicine: Pioglitazone and Bladder Cancer Risk: A Systematic Review and Meta-AnalysisMaria MontoyaAinda não há avaliações
- Mediterranean Diet and Risk of Sjögren's SyndromeDocumento6 páginasMediterranean Diet and Risk of Sjögren's SyndromeMaria Paula Cuellar MarquezAinda não há avaliações
- MainDocumento10 páginasMainrafika triasaAinda não há avaliações
- Helicobacter Pylori and Gastric MalignancyDocumento6 páginasHelicobacter Pylori and Gastric Malignancyabangku4164Ainda não há avaliações
- Fungalinfections in The Icu: Marya D. Zilberberg,, Andrew F. ShorrDocumento18 páginasFungalinfections in The Icu: Marya D. Zilberberg,, Andrew F. ShorrGiselle BaiãoAinda não há avaliações
- River A 2016Documento6 páginasRiver A 2016andismAinda não há avaliações
- Practice Guidelines For The Diagnosis and Management of Aspergillosis: 2016 Update by The Infectious Diseases Society of AmericaDocumento10 páginasPractice Guidelines For The Diagnosis and Management of Aspergillosis: 2016 Update by The Infectious Diseases Society of Americakarol castellonAinda não há avaliações
- Nutrigenomics Dang - Et - Al-2014-Periodontology - 2000Documento7 páginasNutrigenomics Dang - Et - Al-2014-Periodontology - 2000Dr. DeeptiAinda não há avaliações
- UlcerDocumento5 páginasUlcerabriyahAinda não há avaliações
- Neumonia Asosiada A VentiladorDocumento11 páginasNeumonia Asosiada A VentiladorYnomata RusamellAinda não há avaliações
- E Borkowska ResearchproposalDocumento8 páginasE Borkowska Researchproposalapi-308689495Ainda não há avaliações
- Acid-Suppressive Therapy and Risk of Infections: Pros and ConsDocumento38 páginasAcid-Suppressive Therapy and Risk of Infections: Pros and ConsSaya AkuAinda não há avaliações
- Probiotics For The Prevention of Pediatric Antibiotic-Associated DiarrheaDocumento7 páginasProbiotics For The Prevention of Pediatric Antibiotic-Associated DiarrheaJUAN SEBASTIAN AVELLANEDA MARTINEZAinda não há avaliações
- BR J Haematol - 2013 - Samarasinghe - Incidence and Outcome of Pancreatitis in Children and Young Adults With AcuteDocumento4 páginasBR J Haematol - 2013 - Samarasinghe - Incidence and Outcome of Pancreatitis in Children and Young Adults With AcuteEvelin SennaAinda não há avaliações
- 1750 1164 8 3 PDFDocumento7 páginas1750 1164 8 3 PDFRiley RilanAinda não há avaliações
- International Journal of Hepatology & GastroenterologyDocumento7 páginasInternational Journal of Hepatology & GastroenterologySciresAinda não há avaliações
- Histoplasma Capsulatum PDFDocumento12 páginasHistoplasma Capsulatum PDFRobert MacedoAinda não há avaliações
- Histoplasma Capsulatum PDFDocumento12 páginasHistoplasma Capsulatum PDFRobert MacedoAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalAinda não há avaliações
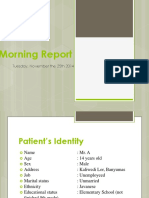
- Morning Report 24 November 2014Documento53 páginasMorning Report 24 November 2014Tiara Grhanesia DenashuryaAinda não há avaliações
- Template Morning Report FK UGMDocumento55 páginasTemplate Morning Report FK UGMTiara Grhanesia DenashuryaAinda não há avaliações
- 14-Year-Old Patient Morning ReportDocumento57 páginas14-Year-Old Patient Morning ReportTiara Grhanesia DenashuryaAinda não há avaliações
- Acls PDFDocumento53 páginasAcls PDFKeez HaruAinda não há avaliações
- Daftar PustakaDocumento3 páginasDaftar PustakaTiara Grhanesia DenashuryaAinda não há avaliações
- Exercise Is A Type of Physical Activity Consisting of Planned, Structured, and Repetitive BodilyDocumento3 páginasExercise Is A Type of Physical Activity Consisting of Planned, Structured, and Repetitive BodilyTiara Grhanesia DenashuryaAinda não há avaliações
- Morning Report 21 November 2014Documento54 páginasMorning Report 21 November 2014Tiara Grhanesia DenashuryaAinda não há avaliações
- Answer Key For Reading PracticeDocumento1 páginaAnswer Key For Reading PracticeTiara Grhanesia DenashuryaAinda não há avaliações
- Accepted Manuscript: YprrvDocumento27 páginasAccepted Manuscript: YprrvTiara Grhanesia DenashuryaAinda não há avaliações
- Harris SDocumento2 páginasHarris STiara Grhanesia DenashuryaAinda não há avaliações
- Head CT Scan Interpretation: A 5-Step ApproachDocumento180 páginasHead CT Scan Interpretation: A 5-Step ApproachTiara Grhanesia DenashuryaAinda não há avaliações
- ADocumento2 páginasATiara Grhanesia DenashuryaAinda não há avaliações
- Hyponatremia in Children With Acute Respiratory Infections: A ReappraisalDocumento6 páginasHyponatremia in Children With Acute Respiratory Infections: A ReappraisalTiara Grhanesia DenashuryaAinda não há avaliações
- Referat Sarkopenia Pada GeriatriDocumento2 páginasReferat Sarkopenia Pada GeriatriTiara Grhanesia DenashuryaAinda não há avaliações
- Head CT Scan Interpretation: A 5-Step ApproachDocumento180 páginasHead CT Scan Interpretation: A 5-Step ApproachTiara Grhanesia DenashuryaAinda não há avaliações
- Oral Ondansetron For Gastroenteritis in A Pediatric Emergency DepartmentDocumento8 páginasOral Ondansetron For Gastroenteritis in A Pediatric Emergency DepartmentTiara Grhanesia DenashuryaAinda não há avaliações
- Guideline For Hypertensive Emergency Treatment PDFDocumento4 páginasGuideline For Hypertensive Emergency Treatment PDFTiara Grhanesia DenashuryaAinda não há avaliações
- Cah 01 10 Ts DiarrDocumento14 páginasCah 01 10 Ts DiarrTiara Grhanesia DenashuryaAinda não há avaliações
- JGJDocumento55 páginasJGJTiara Grhanesia DenashuryaAinda não há avaliações
- Protocols For Hyperlactatemia Induction in The Lactate Minimum Test Adapted To Swimming RatsDocumento5 páginasProtocols For Hyperlactatemia Induction in The Lactate Minimum Test Adapted To Swimming RatsTiara Grhanesia DenashuryaAinda não há avaliações
- 2016 Acute Diarrhea PDFDocumento21 páginas2016 Acute Diarrhea PDFTiara Grhanesia DenashuryaAinda não há avaliações
- 18 Arias 018Documento24 páginas18 Arias 018Tiara Grhanesia DenashuryaAinda não há avaliações
- Fave Rio 2014Documento8 páginasFave Rio 2014Tiara Grhanesia DenashuryaAinda não há avaliações
- The God Helmet PDFDocumento5 páginasThe God Helmet PDFTiara Grhanesia DenashuryaAinda não há avaliações
- Food Chemistry: Lijun You, Mouming Zhao, Joe M. Regenstein, Jiaoyan RenDocumento7 páginasFood Chemistry: Lijun You, Mouming Zhao, Joe M. Regenstein, Jiaoyan RenTiara Grhanesia DenashuryaAinda não há avaliações
- Chat Kin 2016Documento8 páginasChat Kin 2016Tiara Grhanesia DenashuryaAinda não há avaliações
- Bohu 2014Documento7 páginasBohu 2014Tiara Grhanesia DenashuryaAinda não há avaliações
- Acute Diare WHO 2005Documento50 páginasAcute Diare WHO 2005Boby Abdul RahmanAinda não há avaliações
- Patient psychiatric history and physical examDocumento20 páginasPatient psychiatric history and physical examTiara Grhanesia DenashuryaAinda não há avaliações
- SAT EssayDocumento1 páginaSAT EssayBhavye GuptaAinda não há avaliações
- Control PlanDocumento6 páginasControl PlanEshioAinda não há avaliações
- Cement Evaluation GuidelinesDocumento164 páginasCement Evaluation GuidelinesSaid Nahum Montes CarballoAinda não há avaliações
- Impacts of Foreign Direct Investment On Local Communities in Oromia RegionDocumento12 páginasImpacts of Foreign Direct Investment On Local Communities in Oromia RegionInternational Journal of Business Marketing and ManagementAinda não há avaliações
- Sensor Failure Detection Identification and Accommodation Using Fully Connected Cascade Neural NetworkDocumento10 páginasSensor Failure Detection Identification and Accommodation Using Fully Connected Cascade Neural NetworkBayram TasdelenAinda não há avaliações
- Enhancing Sexuality Through The Feldenkrais MethodDocumento1 páginaEnhancing Sexuality Through The Feldenkrais MethodAlexander Fuxbauer100% (1)
- Debra D. Heaney v. Oklahoma Goodwill Industries, Inc., 106 F.3d 413, 10th Cir. (1997)Documento2 páginasDebra D. Heaney v. Oklahoma Goodwill Industries, Inc., 106 F.3d 413, 10th Cir. (1997)Scribd Government DocsAinda não há avaliações
- Transistor (PNP)Documento2 páginasTransistor (PNP)gorgor1Ainda não há avaliações
- Paleoclimate Labels of Late Quaternary, Southern Tamil NaduDocumento1 páginaPaleoclimate Labels of Late Quaternary, Southern Tamil NaduDr.Thrivikramji.K.P.Ainda não há avaliações
- 20742A ENU TrainerHandbook PDFDocumento688 páginas20742A ENU TrainerHandbook PDFFernando CorderoAinda não há avaliações
- Onto-Cartography - An Ontology of Machines and Media (Levy Bryant)Documento18 páginasOnto-Cartography - An Ontology of Machines and Media (Levy Bryant)fandoaxelAinda não há avaliações
- Marketing Management - Unit 1Documento69 páginasMarketing Management - Unit 1Shivanjali FXECAinda não há avaliações
- Earthquake Dynamics of Base-Isolated Buildings: Chopra: Prentice-Hall PAGES JUL. 19, 2000 14:40 ICC Oregon (503) 221-9911Documento24 páginasEarthquake Dynamics of Base-Isolated Buildings: Chopra: Prentice-Hall PAGES JUL. 19, 2000 14:40 ICC Oregon (503) 221-9911MakaraSoyAinda não há avaliações
- Juniornews 22Documento2 páginasJuniornews 22api-325693877Ainda não há avaliações
- Mastering Traditional Philippine Arts and CraftsDocumento2 páginasMastering Traditional Philippine Arts and Craftsnikko candaAinda não há avaliações
- Heavy Metal - Hard Rock PlaylistDocumento6 páginasHeavy Metal - Hard Rock PlaylisttikfarAinda não há avaliações
- Emailing 11. Dr. Manoj Gupta - Pelvic RT PlanningDocumento69 páginasEmailing 11. Dr. Manoj Gupta - Pelvic RT PlanningafshanAinda não há avaliações
- Owasp Top Ten 2004Documento31 páginasOwasp Top Ten 2004Nilesh ManitAinda não há avaliações
- Neet Brahmastra Part-01Documento8 páginasNeet Brahmastra Part-01Aniket Priyadarshi 01Ainda não há avaliações
- Current Trends in The Employment ProcessDocumento1 páginaCurrent Trends in The Employment ProcessDariya MinAinda não há avaliações
- Adumadan CatalogDocumento13 páginasAdumadan CatalogmudiareAinda não há avaliações
- Past Perfect Continuous WorksheetDocumento4 páginasPast Perfect Continuous WorksheetAntonio GonzálezAinda não há avaliações
- Seminar Report On Electro Active Polymers Done by Manojkumar Mahadevan, IndiaDocumento26 páginasSeminar Report On Electro Active Polymers Done by Manojkumar Mahadevan, Indianikhil_prasanthAinda não há avaliações
- Contributions of The Negro To Human Civilization, ChamberlainDocumento22 páginasContributions of The Negro To Human Civilization, ChamberlainLuis GrailletAinda não há avaliações
- Books On Islam Jarir Bookstore KSADocumento1 páginaBooks On Islam Jarir Bookstore KSAygd4qy468cAinda não há avaliações
- Emerging Developments in Organizational Thought, 1975Documento14 páginasEmerging Developments in Organizational Thought, 1975Nam Repus33% (9)
- 99 Names of Allah With Meaning and Benefits - WonderfulinfoDocumento19 páginas99 Names of Allah With Meaning and Benefits - WonderfulinfosiesmannAinda não há avaliações
- What Is A Process Scheduler? State The Characteristics of A Good Process Scheduler? Which Criteria Affect The Schedulers Performance?Documento6 páginasWhat Is A Process Scheduler? State The Characteristics of A Good Process Scheduler? Which Criteria Affect The Schedulers Performance?partha deyAinda não há avaliações
- Daniel Mathew Divorce PetitionDocumento4 páginasDaniel Mathew Divorce PetitionDinesh Patra100% (1)
- SWOT Analysis Helps Bakery Improve PerformanceDocumento44 páginasSWOT Analysis Helps Bakery Improve Performancehyebibie76% (49)