Escolar Documentos
Profissional Documentos
Cultura Documentos
Dengue During Pregnancy and Adverse Fetal Outcomes
Enviado por
Rinche AnnurDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Dengue During Pregnancy and Adverse Fetal Outcomes
Enviado por
Rinche AnnurDireitos autorais:
Formatos disponíveis
Introduction Style Definition: Normal: Font:serotype provides
(Default) Timeslong-la
New
Dengue selama kehamilan dan efek luaran yang Roman, is9 endemic
Dengue, a mosquito-borne viral disease, pt, Font in
color:
particular serotype, wherea
moreBlack, Justified, Indent: Left:
serotypes is temporary.4 The
merugikan: sebuah tinjauan systematik dan meta- -0.01",
than 100 countries (mainly in South
Asia) and is spreading to newspacing:
First line:
America
areas, with
0.09", Space
and southeast
outbreaks
Multiple 1.04 liof
After:
with 0.7 pt, Line
subsequent infections.
increasing magnitude and severity.1 It is estimated that each dengue disease is not comp
analysis year, 390 million people are infected with dengue and 96 prediction of which patient
million develop clinical symptoms.2 A study of dengue not possible, although some
Enny S Paixo, Maria Gloria Teixeira, Maria da Conceio N Costa, Laura C Rodrigues seroprevalence in pregnant women in Brazil showed that severe disease have been id
recent infection (IgM positive) had occurred in 28% of children), 4 presence of c
68
Ringkasan participants.3 Most people with dengue infection either have infections, and ethnic origin
no symptoms or have mild self-limited disease (including against the severe form i
Latar belakang: sedikit yang mengetahui efek yang merugikan dari infeksi dengue selama kehamilan terhadap luaran
fever, headache, retroocular pain, muscle and joint pain, licensed vaccine exists for d
janin. Pada penelitian sistematik dan meta analisis kita estimasikan peningkatan risiko dari 4 wanita yang mendapat nausea, vomiting, and rash); a small proportion of infections eff ective. Treatment is sym
infeksi dengue selama kehamilan. progress to severe illness, with rapid onset of capillary manifestations, mostly con
therapy and management of
leakage accompanied by bleeding, thrombocytopenia, and
Metode penelitian: untuk sistematik review dan meta analisis, digunakan Medline, Embase, Global Health Library liver injury.4 Since women of reproduc
dan Scopus sebelum 1 agustus 2015. Kita masukkan penelitian yang melaporkan luaran dari wanita hamil yang There are four serotypes of dengue virus: DENV 1, DENV 2,risk of dengue infection, wh
mendapat infeksi dengue. Penelitian Case-control, cohort, dan cross-sectional di inklusikan. Kita ekslusikan laporan DENV 3, and DENV 4. Infection with one
kasus, studi ekologi, review dan penelitian invitro dan penelitian tanpa data luaran persalinan. Judul dan abstrak
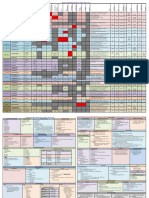
yang masuk dalam inklusi dan kualitas masukkan dalam meta analisis. Untuk ssetiap penelitian, dicatat d For each
study, we recorded study design, year of publication, study location, period of study, and authors and we extracted
Articles
data for population characteristics such as the number of pregnancies, dengue diagnostic information, and the
frequency of outcomes. We investigated four adverse fetal outcomes: stillbirth, miscarriage, preterm birth, and low
birthweight. We estimated the increase in risk of these adverse fetal outcomes by use of Mantel-Haenszel methods.
We assessed heterogeneity of odds ratios (OR) with the I statistic.
Findings We identifi ed 278 non-duplicate records, of which 107 full-text articles were screened for eligibility. 16
studies were eligible for inclusion in the systematic review and eight were eligible for the meta-analyses, which
included 6071 pregnant women, 292 of whom were exposed to dengue during pregnancy. For miscarriage, the OR
was 351 (95% CI 1151077, I=00%, p=0765) for women with dengue infection during pregnancy compared with
those without. We did not do a meta-analysis for stillbirth because this outcome was investigated in only one study
with a comparison group; we calculated the crude relative risk to be 67 (95% CI 21213) in women with
symptomatic dengue compared with women without dengue. Preterm birth and low birthweight were the most
common adverse pregnancy outcomes. The OR for the association with dengue was 171 (95% CI 106276,
I=561%, p=0058) for preterm birth and 141 (95% CI 090221, I=00%, p=0543) for low birthweight.
Lancet Infect Dis 2016
Interpretation Evidence suggests that symptomatic dengue during pregnancy might be associated with fetal adverse Published Online March
3, 2016
outcomes. If confi rmed, it would be important to monitor pregnancies during which dengue is diagnosed and to http://dx.doi.org/10.101
consider pregnant women in dengue control policies. 6/ S1473-
3099(16)00088-8
See Online/Comment
Funding National Council for Scientifi c and Technological Development (CNPq).
http://dx.doi.org/10.1016/
S1473-3099(16)00130-4
Department of Infectious
Disease Epidemiology, Faculty
of Epidemiology and
Population Health, London
School of Hygiene & Tropical
Medicine, London, UK
(E S Paixo MSc,
L C Rodrigues PhD); and
Instituto de Sade Coletiva,
Salvador, Brazil
(M G Teixeira PhD,
M da C N Costa PhD)
Correspondence to:
Mrs Enny S Paixo, London
School of Hygiene & Tropical
Medicine, London WC1E 7HT,
UK enny.cruz@lshtm.ac.uk
www.thelancet.com/infection Published online March 3, 2016 http://dx.doi.org/10.1016/S1473-3099(16)00088-8 1
Articles
Research in context
Evidence before this study dengue infection alone, in the absence of clinical symptoms,
Prematurity and low birthweight are among the main does not aff ect the outcome of pregnancy, but also that
causes of neonatal and infant death and although clinical dengue during pregnancy seems to increase the
awareness of the importance of stillbirth is increasing, the frequency of stillbirth, prematurity, and low birthweight.
causes remain unknown. Evidence suggests a role in
Added value of this study
preterm birth, low birthweight, and stillbirth for some
To our knowledge, our study is the fi rst to show an
infections such as syphilis, toxoplasmosis, rubella,
association between dengue infection during pregnancy and
cytomegalovirus, and herpes. Dengue is epidemic in many
adverse fetal outcomes. Better understanding of the eff ects
regions of the world, including the Americas, Asia, and of dengue during pregnancy is needed to improve
Oceania, but the eff ect of dengue infection during knowledge about the burden of this disease, including cost
pregnancy on fetal outcomes is not well understood or effi cacy estimates, and to inform initiatives to reduce fetal
documented. We searched Medline, Embase, Global Health and neonatal mortality.
Library, and Scopus for articles published before Aug 1,
2015, using the terms: dengue, or dengue haemorrhagic Implications of all the available evidence
fever AND pregnancy outcomes, pregnancy If an association between dengue infection during
complication, low birth weight, small for gestational pregnancy and adverse fetal outcomes can be confi rmed,
age, intrauterine growth restriction, stillbirth, fetal recommendations should be made for the close monitoring
death, preterm birth, preterm delivery, preterm of pregnancies during which dengue is diagnosed and for
labour, abortion, or miscarriage. We independently strategies for dengue control to include pregnant women as
screened titles and abstracts to select the papers for an at-risk population. In view of how common dengue
inclusion and scored the quality of those included in infection is, original research needs to be done with
metaanalyses. We identifi ed 16 published studies that met appropriately sized studies and rigorous methodology to
our inclusion criteria. The research base is sparse and has investigate the eff ects of dengue in pregnancy and the
many limitations, with only seven studies investigating the relevance of clinical symptoms and the gestational age at
evidence in a comparative way. Some preliminary evidence which the infection occurs.
suggests that
during pregnancy is associated with adverse fetal outcomes needs to be established. In 2010, a study with the largest
systematic review15 of dengue infection during pregnancy and fetal outcomes was published. The sample size was
investigators reviewed 19 case reports, nine cases series, and two cohorts, and concluded that vertical included. Eligible
transmission is possible; however, the evidence was not suffi cient to confi rm whether dengue study designs were
infection during pregnancy increases the risk of adverse outcomes. The eff ects of infection during casecontrol, cohort,
pregnancy on fetal outcomes remain unclear. and cross-sectional
With this systematic review and meta-analysis, we aimed to investigate whether the published studies and
scientifi c literature shows increased risk of stillbirth, miscarriage, preterm birth, and low birthweight unselected case
for women who had dengue infection during pregnancy. series (ie, those in
which participants
Methods were selected
independently of
Search strategy and eligibility criteria outcome). Case
We report this systematic review and meta-analysis in accordance with the Preferred Reporting Items reports, ecological
for Systematic Reviews and Meta-Analysis (PRISMA) statement.16 We searched Medline, Embase, studies, reviews, in-
Scopus, and Global Library to identify studies reporting fetal outcomes in women who had dengue vitro studies, and
infection during the pregnancy. We searched databases up to Aug 1, 2015, with the terms dengue studies without
or dengue haemorrhagic fever AND pregnancy outcomes, pregnancy complication, low birth information about
weight, small for gestational age, intrauterine growth restriction, stillbirth, fetal death, pregnancy outcomes
preterm birth, preterm delivery, preterm labour, abortion, or miscarriage. We were excluded. We
supplemented our database searchers by screening the bibliographies of the previous systematic sought to extract
review article.15 We used the explode function for dengue, pregnancy outcomes, and pregnancy patient-level data.
complications. This function automatically includes all narrower terms in the hierarchical list during Article titles and
the search to retrieve citations that carry the specifi ed MeSH heading (or subheading). We used no abstracts were
language restrictions. We reviewed all titles and abstracts of publications identifi ed in the primary screened indepen
search for relevance and eligibility, after duplicates had been removed. dently by two
Eligible publications were original studies that reported any fetal outcome for pregnant women who had dengue infection reviewers (ESP and
during the gestational period. To avoid overlapping populations, if participants were included in more than one report, the MdCNC) to select
2 www.thelancet.com/infection Published online March 3, 2016 http://dx.doi.org/10.1016/S1473-3099(16)00088-8
Articles
Formatted: Right, Line spacing: Multiple 1.15 li
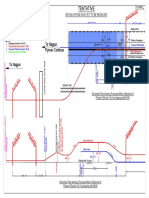
papers for full text screening. Full texts were independently assessed by these reviewers. In case of disagreements, a third 664 records identified through database searching
reviewer (MGT) was consulted and a decision was agreed by consensus. 117 MEDLINE
111 Global Health Library
Data analysis 199 Scopus
We used a spreadsheet to record information from eligible articles about study design, year of publication, study location, 237 Embase
study period, and authors. We also recorded population characteristics such as the number of pregnancies, dengue diagnostic 1 record identified from a systematic review
information, and frequency of each outcome.
We studied four adverse fetal outcomes for which data were available from more than one study: miscarriage, defi ned as 387 duplicates removed
a non-viable product of conception after less than 22 weeks; stillbirth, defi ned as fetal death in utero at or after 22 weeks
of gestation or at a weight of more than 500 g (we also included two studies without gestational age and birthweight
278 screened
information, but classifi ed by the author as stillbirth); preterm birth, defi ned as live delivery before 37 weeks of gestation;
and a composite outcome of low birthweight, defi ned as birthweight less than 2500 g, or intrauterine growth restriction,
defi ned as birthweight less than the tenth percentile for gestational age. We defi ned dengue infection during pregnancy by 171 did not answer the research question
use of clinical criteria (symptoms of dengue), laboratory criteria (positive test from one of IgM detection by ELISA, viral
RNA detection via PCR, NS1 viral antigen detection, or positive viral culture), or both.
107 assessed for eligibility
Two authors (ESP, LCR) independently scored the quality of the studies included in meta-analyses in accordance with the
Newcastle-Ottawa scale (NOS).17 This scale was used for cohort and case-control studies and a modifi ed version was used
for case series studies and cross-sectional studies. In the NOS, cohort and casecontrols studies are scored between zero and 91 excluded
nine stars for nine questions that cover three items (selection, comparability, and outcome); cross-sectional studies are scored 32 had no data for fetal outcomes
34 case reports
between zero and eight, and case series are scored between zero and six. We deemed nine stars to be 100%, so a perfect 20 reviews or ecological studies
case series (six stars) would be assessed as scoring 67 %. The fi nal score was agreed between the two reviewers. 5 overlapping datasets
When eff ect estimates were not presented in the papers, we calculated the proportion of participants with outcome events
on the basis of the data within each study. For stillbirths, preterm births, and low birthweight the denominator was the total 16 included in systematic review
number of pregnant women beyond week 22 of gestation, and for miscarriages the denominator was the total number of all
pregnancies. We then estimated the 95% CIs for each outcome and study with the Poisson distribution, because of the small
numbers of cases.18 8 studies included in meta-analyses
In cohort, case-control, and cross-sectional studies, we estimated odds ratios (OR) afresh by comparing odds of fetal Figure 1: Study selection
outcomes in pregnancies with and without dengue infection during pregnancy. We did meta-analysis for miscarriages,
preterm birth, and low birthweight or intrauterine growth restriction; we did not do a metaanalysis for stillbirths because
this outcome was investigated in only one study with a comparison group. It was possible to estimate the OR for preterm
birth in one of the case series studies19 because it provided the required comparative data for the same year. This allowed us
to include this study in the meta-analysis with the other studies that had a comparison group. To estimate the increase in
risk of adverse fetal outcomes, we used the Mantel-Haenszel test, because the data are sparse in terms of events and study
size.20 This test makes an adjustment to the study weights according to the variation or heterogeneity, among the varying eff
ects. We assessed heterogeneity of OR with the I statistic. We analysed the data with Stata version 14.0.
Role of the funding source
The funder of this study had no role in study design, data collection, data analysis, data
interpretation, or writing of the report. All authors had full access to all the data in the study and
had fi nal responsibility for the decision to submit for publication.
Results
Our initial search identifi ed 665 papers, 387 of which were duplicates (fi gure 1). After screening,
107 articles were assessed for eligibility and 91 were excluded because they did not meet the
inclusion criteria. We included 16 articles19,2135 in the systematic review (fi ve cohorts, one case-
control, one cross-sectional study, and nine cases series), and eight19,2124,28,29,35 in the meta-analysis
(table). The studies were published from 1994 to 2014, and were done in ten countries (Brazil,19,21
Colombia,22 Cuba,23 France [French Guiana],24 India,2527 Malaysia,2830 Mexico,31 Sri Lanka,32,33
Sudan,34 and Venezuela35).
Formatted: Normal
www.thelancet.com/infection Published online March 3, 2016 http://dx.doi.org/10.1016/S1473-3099(16)00088-8 3
Articles
Miscarriage as a potential adverse outcome associated with dengue six case series,19,25,27,30,31,33 one case-control study,29 and one cohort study.22
infection during pregnancy was described in Prevalence of miscarriage associated with dengue infection during
4 www.thelancet.com/infection Published online March 3, 2016 http://dx.doi.org/10.1016/S1473-3099(16)00088-8
Articles
Formatted: Right, Line spacing: Multiple 1.15 li
pregnancy ranged from 38% (95% CI 00210) in Sri Lanka to 16% 33
infection. We did not do a meta-analysis for stillbirth because this
3032
(43410) in India.25 In the single study that controlled for outcome was investigated in only one study with a comparison group.
confounding,29 which was done in Malaysia, the OR for recent dengue In the cohort study done in French Guiana,24 the crude relative risk
infection was 42 (95% CI 1214) for cases of miscarriage versus (calculated by us from data presented in the
controls after adjustment for maternal age, gestational age, parity, and
ethnic origin.29 We used two studies (a case-control and a cohort OR=odds ratio.
study)22,29 to do the meta-analysis for miscarriage as a pregnancy study) for stillbirth was 67 (95% CI 21213)
outcome potentially associated with dengue pregnancy; the crude for women with symptomatic dengue compared
overall OR was 351 (95% CI 1151077, I=0%, p=0765; fi gure 2). with Preterm birth and low birthweight (or
Stillbirths were investigated in four case series 25,3032 and one cohort intrauterine growth restriction) were the most
study.24 Prevalence of stillbirth in pregnant women who had dengue common adverse pregnancy outcomes for
women with dengue infection
OR (95% CI) Weight
Country Study design Number of pregnant women Prevalence (%) of fetal outcomes Other fi ndings and comments NOS Included
Tan et al (2012)28 320 (0961071) 8498 %
admitted with dengue in pregnant women with dengue score in meta
22
infectionRestrepo et al (2004) 527 (02411335)
analyses 1502%
Total (I=00%, p=0765) 351 (1151077) 10000%
Ismail and Malaysia Case series 16 dengue cases confi rmed in clinic, Preterm birth: 266% Retrospective study of medical records of all No
colleagues, laboratory, or both (95% CI7268) pregnant women with dengue admitted to a
200630 000882
Miscarriage: 62% (95% CI 0134)maternity wards 1 between 2000 and 2004 113
Stillbirth: 66% (95% CI 0137) DengueOR was defi
(95% ned
CI) as an acute febrile illness with
two or more clinical manifestation and only 50% of
patients were serologically
Dengue infection decreases positiveincreases
Dengue infection
4 participants lost to follow-up
risk of miscarriage risk of miscarriage
Waduge and Sri Lanka Case series 26 dengue cases Preterm birth: 4% (95% CI 0122)All pregnant women admitted to hospital with No
colleagues, Laboratory confi
rmed Figure 2:Association
Low birthweight: 16% between dengue
confi infectioninfections
rmed dengue during pregnancy and miscarriage
were included
200633 (95% CI4341)
Miscarriage: 38% (95% CI 021)
Malhotra and India Case series 8 dengue cases No adverse fetal outcomes None of the neonates born were infected No
colleagues, Laboratory confi
rmed observed One neonatal death attributed to arthrogyposis
200526 congenital
Chitra and India Case series 14 dengue cases Preterm birth: 15% (95% CI 255) Retrospective analysis of medical records of all No
Panicker, Laboratory confi
rmed Miscarriage: 7% (95% CI 0239) pregnant women with dengue infection admitted to
201127 a maternity ward during 200910
One co-infection with malaria was reported; this case
had congenital anomaly and was medically
terminated
Average birthweight was 244 kg, but study did not
report how many babies weighted <25 kg
Two participants lost to follow-up
Agrawal and India Case series 25 dengue cases Preterm birth: 80% Retrospective analysis of medical records of all No
colleagues, Laboratory confi
rmed (95% CI 196129) pregnant women with confi rmed dengue infection
201425 Low birthweight: 52% admitted to the maternity ward during the study
(95% CI2693) period
Stillbirth: 47% (95% CI 0126)
Miscarriage: 16% (4340)
Sastr and Mexico Case series 21 dengue cases Miscarriage: 47% (95% CI 0126)Retrospective analysis of medical records of all No
Gonzalez, Laboratory confi
rmed Stillbirth: 5% (95% CI 0126) pregnant women with confi rmed dengue infection
200931 admitted to a maternity ward during the study
period 200507
For stillbirths, preterm births, and low birthweight, the denominator was the total number of pregnant women beyond week 22 of gestation, and for miscarriages the denominator was the total number of
pregnancies, unless otherwise noted. OR=odds ratio. NOS=Newcastle-Ottawa Scale. PAHO=Pan American Health Organization. rth*Stillbi
defined as fetal death in utero weighing 500 g or at 22 weeks of
gestation or after. Intrauterine growth restriction defi ned as birthweight less than the tenth percentile for gestational age. Stillbirth with out defi nition occurred after 22 weeks. Stillbirth
nition
without defi
with no information about gestational age.
Formatted: Indent: Hanging: 0.2", Right: 0.01", Spac
: Study characteristics
Table After: 1.1 pt, Line spacing: Multiple 1.01 li, Numbere
infection during pregnancy varied between 47% (95% CI 01260) in + Level: 1 + Numbering Style: 1, 2, 3, + Start at: 1 +
India25 and 130% (16480) in Sri Lanka.32 In three of the four case Alignment: Left + Aligned at: 0.2" + Indent at: 0.2"
series, stillbirths occurred only in women who had severe dengue
women without dengue. Formatted: Left: 0.39", Right: 0.51", Top: 1.79",
A
OR (95% CI) Bottom:
Weight 0.64", Section start: Continuous, Width: 8.2
A 24
Friedman et al (2014) OR (95%
195 CI)
(101375)
Height:
Weight
3955%
11.1", Number of columns: 2, Col #1 width:
Tan et al (2008)28 089 (038208) 4.01",
4002% Not Force equal column width
24
Friedman
Restrepo etet al
al (2004)
(2014)
22 220
106 (104466)
(025459) 3489 %
Formatted:
1181%
Tan et alet
(2008) 28
042
Normal
Barroso al (2009)23 300 (010173)
(0471904) 3776
427%
%
www.thelancet.com/infection Published online March 3, 2016 http://dx.doi.org/10.1016/S1473-3099(16)00088-8 5
21 22
Restrepo
Leite et alet(2004)
al (2004) 106 (020561) 1177
066 (0031243) 435% %
Alvarenga
Total (I=00%, (2009)19
et al p=0543) 141 (098870)
291 (090221) 10000%
1496 %
Angarita et al (2013)35 3656 (16083626) 062%
Total (I=561%, p=0058)
00348 1 287 171 (106276) 10000%
Você também pode gostar
- Antibiotic Chart-Infectious Disease Bug Drug Table-2019Documento2 páginasAntibiotic Chart-Infectious Disease Bug Drug Table-2019Duy LuuAinda não há avaliações
- PRTG Report 10361 - Report Voltage Gps - Created 2019-08-16 08-34-38 (2019-08-05 00-00 - 2019-08-12 00-00) UTC - Part 01Documento10 páginasPRTG Report 10361 - Report Voltage Gps - Created 2019-08-16 08-34-38 (2019-08-05 00-00 - 2019-08-12 00-00) UTC - Part 01muhammad saoqiAinda não há avaliações
- Radiology 101Documento2 páginasRadiology 101Nadhirah AnandaAinda não há avaliações
- PRTG Report 4886 - Disponibilidad de Servicios - Created 2023-06-12 09-02-01 (2023-05-01 00-00 - 2023-05-31 00-00) UTC - Part 05Documento16 páginasPRTG Report 4886 - Disponibilidad de Servicios - Created 2023-06-12 09-02-01 (2023-05-01 00-00 - 2023-05-31 00-00) UTC - Part 05geometro00Ainda não há avaliações
- Departments of Neurology, James J. Peters Veterans Affairs Medical Center, Bronx, NY, and Mount Sinai School of Medicine, New York, NYDocumento1 páginaDepartments of Neurology, James J. Peters Veterans Affairs Medical Center, Bronx, NY, and Mount Sinai School of Medicine, New York, NYyuliAinda não há avaliações
- Ppt. CLL and XMRV Houston 2010Documento1 páginaPpt. CLL and XMRV Houston 2010mindykitei_cfscentralAinda não há avaliações
- Computation: Theory ofDocumento10 páginasComputation: Theory ofSuraj DasguptaAinda não há avaliações
- Parasite - Table - 2015 - 2 - .PDF Filename UTF-8''Parasite Table 2015Documento2 páginasParasite - Table - 2015 - 2 - .PDF Filename UTF-8''Parasite Table 2015Shayma K MaaliAinda não há avaliações
- Ujian Patoflow Yola MTDocumento1 páginaUjian Patoflow Yola MTAdam SipahutarAinda não há avaliações
- Algoritmo Trauma RenalDocumento1 páginaAlgoritmo Trauma RenalRobert MacedoAinda não há avaliações
- Dorota Jarecka, Sylwester Arabas, Maciej Fijalkowski, Anna Jaruga, Davide Del VentoDocumento1 páginaDorota Jarecka, Sylwester Arabas, Maciej Fijalkowski, Anna Jaruga, Davide Del VentoNotes btechAinda não há avaliações
- StoryboardDocumento2 páginasStoryboardapi-604338261Ainda não há avaliações
- Latina 2008 09 LatinosInActionDocumento1 páginaLatina 2008 09 LatinosInActionDorkys RamosAinda não há avaliações
- Review: Diffusion-Weighted MR Imaging in Acute Stroke: Theoretic Considerations and Clinical ApplicationsDocumento9 páginasReview: Diffusion-Weighted MR Imaging in Acute Stroke: Theoretic Considerations and Clinical ApplicationsDiego Letelier GfellAinda não há avaliações
- PRTG Report 4886 - Disponibilidad de Servicios - Created 2023-06-12 09-02-01 (2023-05-01 00-00 - 2023-05-31 00-00) UTC - Part 06Documento15 páginasPRTG Report 4886 - Disponibilidad de Servicios - Created 2023-06-12 09-02-01 (2023-05-01 00-00 - 2023-05-31 00-00) UTC - Part 06geometro00Ainda não há avaliações
- Tradiderunt Me: Tenebrae ResponsoriesDocumento3 páginasTradiderunt Me: Tenebrae ResponsoriessounditoutAinda não há avaliações
- Type of deviation conformity assessmentDocumento14 páginasType of deviation conformity assessmentNurul Fatia JannahAinda não há avaliações
- SM Slides 2upDocumento63 páginasSM Slides 2upSiva PrasadAinda não há avaliações
- Phased Array Probes Application MatrixDocumento1 páginaPhased Array Probes Application MatrixFethi BELOUISAinda não há avaliações
- Lecture 7: Generate powerful pulses with pulsed lasersDocumento25 páginasLecture 7: Generate powerful pulses with pulsed lasersLethargic AzadhirachtaAinda não há avaliações
- Facial A N PDFDocumento5 páginasFacial A N PDFSagar SinhaAinda não há avaliações
- Domain and Range Set and Interval NotationsDocumento1 páginaDomain and Range Set and Interval NotationsHafsa KhanAinda não há avaliações
- ICRADocumento9 páginasICRAMaiova N. Annisa100% (1)
- Suicide Mortality Rate (Per 100 000 Population), by WHO Region, 2016Documento1 páginaSuicide Mortality Rate (Per 100 000 Population), by WHO Region, 2016John KirubakaranAinda não há avaliações
- O Meu Neno Canta: Ejercicio para 3º GE 15/11Documento2 páginasO Meu Neno Canta: Ejercicio para 3º GE 15/11Amanda Pinos FernándezAinda não há avaliações
- Pandas Cheat Sheet FinalDocumento1 páginaPandas Cheat Sheet FinalASWINKUMAR RAinda não há avaliações
- EIA WarehouseDocumento3 páginasEIA WarehouseAnnabella1234Ainda não há avaliações
- Diámetro, Longitud Equivalente, Presión Hf y Presión TotalDocumento15 páginasDiámetro, Longitud Equivalente, Presión Hf y Presión TotalBrayan StibenAinda não há avaliações
- Stream A Of: HOW Much? Where?Documento2 páginasStream A Of: HOW Much? Where?Anonymous scfS5sbpMAinda não há avaliações
- Invoicing SystemDocumento1 páginaInvoicing SystemMahmoud HadiyaAinda não há avaliações
- Pontaj 5 - 2021.xls MIKEDocumento1 páginaPontaj 5 - 2021.xls MIKEDiana DutuAinda não há avaliações
- Usaid An Icn Hemocue Population 2022Documento1 páginaUsaid An Icn Hemocue Population 2022Samson DesieAinda não há avaliações
- Excel Single & Two PopulationDocumento20 páginasExcel Single & Two PopulationAzmienz HierzanzAinda não há avaliações
- Dreadlock holiday music sheetDocumento1 páginaDreadlock holiday music sheetwrojasAinda não há avaliações
- Agnus Missa Tertia (Haller)Documento4 páginasAgnus Missa Tertia (Haller)Coral Jesus DespojadoAinda não há avaliações
- SRS of ProjectDocumento5 páginasSRS of ProjectnileshAinda não há avaliações
- Mronj Staging and TaxDocumento1 páginaMronj Staging and Taxnapat kidsanakaraketAinda não há avaliações
- 111COVID REPORT Latest - PagesDocumento2 páginas111COVID REPORT Latest - PagesNikunjAinda não há avaliações
- HL7 Version 3Documento29 páginasHL7 Version 3DaSheng SunAinda não há avaliações
- Yumi Ono, Yoshifumi Onishi, Takafumi Koshinaka, Soichiro Takata, and Osamu HoshuyamaDocumento5 páginasYumi Ono, Yoshifumi Onishi, Takafumi Koshinaka, Soichiro Takata, and Osamu HoshuyamaJuan Camilo Gomez SotoAinda não há avaliações
- Reach 1A Tentative DrawingDocumento3 páginasReach 1A Tentative DrawingTUSHAR RATHODAinda não há avaliações
- Chapter 1, Unit 1, Human Anatomy and Physiology 1, B Pharmacy 1st Sem, Carewell PharmaDocumento8 páginasChapter 1, Unit 1, Human Anatomy and Physiology 1, B Pharmacy 1st Sem, Carewell Pharmasidharthnagar3456Ainda não há avaliações
- AspirationsDocumento10 páginasAspirationsdr satnam kaurAinda não há avaliações
- Loïc Caloren - NBS 2021 PosterDocumento1 páginaLoïc Caloren - NBS 2021 PosterCBR UBCAinda não há avaliações
- 1941-08-17 (Tribune) - 77 Towns in First Regional BlackoutDocumento2 páginas1941-08-17 (Tribune) - 77 Towns in First Regional Blackoutpaio.michaeltabuyanAinda não há avaliações
- R.F. Laine1-2, K.L. Tosheva1, R.D.M. Gray1, P. Almada1, D. Albrecht1, J. Mercer1, C. Leterrier3, P.M. Pereira1-2, S. Culley1-2 and R. Henriques1-2 Equal ContributionDocumento3 páginasR.F. Laine1-2, K.L. Tosheva1, R.D.M. Gray1, P. Almada1, D. Albrecht1, J. Mercer1, C. Leterrier3, P.M. Pereira1-2, S. Culley1-2 and R. Henriques1-2 Equal ContributionAlejandro VillamarinAinda não há avaliações
- Flow Chart Block Diagram: COMSATS Institute of Information Technology, Attock PakistanDocumento1 páginaFlow Chart Block Diagram: COMSATS Institute of Information Technology, Attock Pakistaniram shezadiAinda não há avaliações
- Statistics and Data AnalysisDocumento20 páginasStatistics and Data Analysisjake_calderónAinda não há avaliações
- WEG CFW500 Installation Guide Parameter Reference 10007479673 en Es PT ZHDocumento12 páginasWEG CFW500 Installation Guide Parameter Reference 10007479673 en Es PT ZHRicardo LeiteAinda não há avaliações
- Strip Map for Proposed Pavement MaintenanceDocumento2 páginasStrip Map for Proposed Pavement MaintenanceNekroz UsAinda não há avaliações
- IONIX ModelDocumento6 páginasIONIX ModelTrường Bửu TrầnAinda não há avaliações
- European Commission project aims for 100% renewable energy on Spanish islandDocumento2 páginasEuropean Commission project aims for 100% renewable energy on Spanish islandV TsekAinda não há avaliações
- Rad DocumentationDocumento45 páginasRad DocumentationMissoft waresAinda não há avaliações
- Empirical Support For Resilience As More Than The Counterpart and Absence of Vulnerability and Symptoms of Mental DisorderDocumento14 páginasEmpirical Support For Resilience As More Than The Counterpart and Absence of Vulnerability and Symptoms of Mental DisorderFaten NajarAinda não há avaliações
- Rates of Prosecution and Sentencing For Black People Were 3 Times Higher Than White PeopleDocumento1 páginaRates of Prosecution and Sentencing For Black People Were 3 Times Higher Than White PeopleAnvil YuenAinda não há avaliações
- Contractor Safety AuditDocumento1 páginaContractor Safety Auditmohamad ifthekharAinda não há avaliações
- Posters Composite EN 201608 Web PDFDocumento1 páginaPosters Composite EN 201608 Web PDFMd. Razibul IslamAinda não há avaliações
- Ballad of BoothDocumento2 páginasBallad of BoothKarter DolanAinda não há avaliações
- The Great Divide-CompletoDocumento13 páginasThe Great Divide-CompletoDaniel FaliosaAinda não há avaliações
- Guideline On Good Pharmacovigilance (GVP) - Module VIII - Post-Authorisation Safety Studies (Rev. 2)Documento27 páginasGuideline On Good Pharmacovigilance (GVP) - Module VIII - Post-Authorisation Safety Studies (Rev. 2)Salló TivadarAinda não há avaliações
- Purposeful Sampling in Qualitative Research SynthesisDocumento14 páginasPurposeful Sampling in Qualitative Research SynthesisRahulAinda não há avaliações
- Metastatic Breast CancerDocumento49 páginasMetastatic Breast CancerMeryl Angeline UcabAinda não há avaliações
- "Incivility, Social Undermining, Bullying Oh My!": A Call To Reconcile Constructs Within Workplace Aggression ResearchDocumento23 páginas"Incivility, Social Undermining, Bullying Oh My!": A Call To Reconcile Constructs Within Workplace Aggression ResearchanshulAinda não há avaliações
- Peri-Operative Chest Physiotherapy For Paediatric Cardiac Patients: A Systematic Review and Meta-AnalysisDocumento13 páginasPeri-Operative Chest Physiotherapy For Paediatric Cardiac Patients: A Systematic Review and Meta-AnalysisMarceloCorralesAinda não há avaliações
- Literature Review On Tuberculosis PDFDocumento8 páginasLiterature Review On Tuberculosis PDFafmzfvlopbchbe100% (1)
- Review Bias in Clinical Intervention ResearchDocumento9 páginasReview Bias in Clinical Intervention ResearchHesed VirtoAinda não há avaliações
- Phisiotherapy PDFDocumento8 páginasPhisiotherapy PDFSandra LandaetaAinda não há avaliações
- Epidemiology LectureDocumento3 páginasEpidemiology Lecturekep1313Ainda não há avaliações
- JDI Meta-Analysis 2Documento19 páginasJDI Meta-Analysis 2Agustinus KurniawanAinda não há avaliações
- Cultural Variations in Attachment Patterns Meta-AnalysisDocumento1 páginaCultural Variations in Attachment Patterns Meta-AnalysisGladei Carmelita100% (1)
- Nutrition-sensitive factors that contribute to childhood stuntingDocumento12 páginasNutrition-sensitive factors that contribute to childhood stuntingAndi Fahira NurAinda não há avaliações
- Selection Methods - Scmidt - The - Validity - and - Utility PDFDocumento13 páginasSelection Methods - Scmidt - The - Validity - and - Utility PDFYoussef AlyAinda não há avaliações
- Antenatal Corticosteroid Therapy Before 24 Weeks.13-1Documento11 páginasAntenatal Corticosteroid Therapy Before 24 Weeks.13-1mutya yulindaAinda não há avaliações
- Salk 2017Documento41 páginasSalk 2017Marius CosmaAinda não há avaliações
- Industrial and Organizational PsychologyDocumento20 páginasIndustrial and Organizational PsychologyCătălina BodnariucAinda não há avaliações
- Mastery in Coaching A Complete Psychological Toolkit For Advanced Coaching (Jonathan Passmore) (Z-Lib.-6Documento345 páginasMastery in Coaching A Complete Psychological Toolkit For Advanced Coaching (Jonathan Passmore) (Z-Lib.-6hoidoeimanAinda não há avaliações
- Community Medicine Module Book PDFDocumento37 páginasCommunity Medicine Module Book PDFLiya SuwarniAinda não há avaliações
- Effects of Tapering On Performance A Meta-AnalysisDocumento8 páginasEffects of Tapering On Performance A Meta-Analysisxcite4everAinda não há avaliações
- Palmatier, Houston Hulland (2017) Review ArticlesDocumento5 páginasPalmatier, Houston Hulland (2017) Review ArticlesSoh Mei LingAinda não há avaliações
- Yoga and AxietyDocumento14 páginasYoga and AxietyLie LhianzaAinda não há avaliações
- 07 Positive Accounting TheoryDocumento4 páginas07 Positive Accounting TheoryBhupendra RaiAinda não há avaliações
- Implementing TQM to Enhance Customer SatisfactionDocumento16 páginasImplementing TQM to Enhance Customer SatisfactionAida ZaraAinda não há avaliações
- Acupoint Stimulation For Fibromyalgia 2013Documento15 páginasAcupoint Stimulation For Fibromyalgia 2013silkofosAinda não há avaliações
- BSNR guidelines for neuroimaging in headacheDocumento39 páginasBSNR guidelines for neuroimaging in headacheBEREKETAinda não há avaliações
- A Single Preoperative Dose of Tranexamic Acid Reduces Perioperative Blood LossDocumento7 páginasA Single Preoperative Dose of Tranexamic Acid Reduces Perioperative Blood LossCarlosA.DíazAinda não há avaliações
- The McKenzie Method For Low Back PainDocumento9 páginasThe McKenzie Method For Low Back PainRupesh Mamidi100% (1)
- 1 s2.0 S2772368222000130 MainDocumento23 páginas1 s2.0 S2772368222000130 MainHandayaniAinda não há avaliações
- 2003 Tranfield Et AlDocumento17 páginas2003 Tranfield Et Allatellagiulia192Ainda não há avaliações
- Effects of Yoga in Adults With Type 2 Diabetes Mellitus: A Meta-AnalysisDocumento9 páginasEffects of Yoga in Adults With Type 2 Diabetes Mellitus: A Meta-AnalysisPerez Wahyu PurnasariAinda não há avaliações