Escolar Documentos
Profissional Documentos
Cultura Documentos
Journal Nejmcpc1208145 PDF
Enviado por
Irmagian PaleonTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Journal Nejmcpc1208145 PDF
Enviado por
Irmagian PaleonDireitos autorais:
Formatos disponíveis
The n e w e ng l a n d j o u r na l of m e dic i n e
case records of the massachusetts general hospital
Founded by Richard C. Cabot
Nancy Lee Harris, m.d., Editor Eric S. Rosenberg, m.d., Editor
Jo-Anne O. Shepard, m.d., Associate Editor Alice M. Cort, m.d., Associate Editor
Sally H. Ebeling, Assistant Editor Emily K. McDonald, Assistant Editor
Case 16-2013: A 12-Year-Old Girl
with Irritability, Hypersomnia,
and Somatic Symptoms
Suzanne L. Bender, M.D., Nicole A. Sherry, M.D., and Ricard Masia, M.D., Ph.D.
Pr e sen tat ion of C a se
Dr. Elizabeth G. Pinsky (Psychiatry): A 12-year-old girl was seen in the outpatient psy- From the Departments of Psychiatry
chiatry clinic of this hospital because of severe irritability, hypersomnia, and mul- (S.L.B.), Pediatrics (N.A.S.), and Pathol-
ogy (R.M.), Massachusetts General Hos-
tiple somatic symptoms. pital; and the Departments of Psychiatry
The patient had celiac disease but had been otherwise well until approximately (S.L.B.), Pediatrics (N.A.S.), and Pathol-
8 months earlier, when she became increasingly irritable and reported daily stom- ogy (R.M.), Harvard Medical School
both in Boston.
achaches, tingling and pain in her arms and legs, dizziness, anorexia, and severe
fatigue; she also became increasingly somnolent, sleeping up to 13 hours per N Engl J Med 2013;368:2015-24.
DOI: 10.1056/NEJMcpc1208145
night. She had frequent angry outbursts directed at her mother and sister, and acted Copyright 2013 Massachusetts Medical Society.
out physically on occasion. She became increasingly isolated from her friends and
lost interest in activities. Her performance in school deteriorated, and she failed
mathematics. Approximately 4.5 months before this presentation, red-cell indexes
and results of thyroid-function tests were normal, and testing for heterophile an-
tibody was negative; other test results are shown in Table 1. She was referred to
the outpatient gastroenterology, neurology, and psychiatry clinics of this hospital.
The patient was born to a 39-year-old mother by cesarean section because of
maternal preeclampsia, and her childhood development was normal. A diagnosis
of celiac disease had been made at the age of 8 years, when she presented with
abdominal pain and constipation; elevated levels of tissue transglutaminase anti-
body (70 U per milliliter) and endomysial antibody (80 U per milliliter) were de-
tected, and examination of a biopsy specimen of the duodenum showed changes
consistent with celiac disease. She adhered to a gluten-free diet and had been
otherwise well. She had a history of anxiety and depression; she had no response
to a trial of sertraline but did have a response to both escitalopram, begun 2 years
before this evaluation, and 7 months of cognitive behavioral therapy. Sixteen
months before this evaluation, the first of three episodes of severe vomiting re-
quiring intravenous hydration occurred; subsequent episodes occurred 6 months
and 4 months before this evaluation, each preceded by fever and viral symptoms.
There was no associated headache, and neurologic evaluation including an electro-
encephalogram was reportedly normal.
n engl j med 368;21 nejm.org may 23, 2013 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
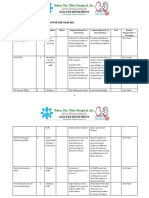
Table 1. Laboratory Data.*
Reference Range, 4.5 Mo before Evaluation, 6 Wk after Evaluation, On Admission,
Variable Other Hospital Pediatricians Office Pediatricians Office Other Hospital
Blood
Hematocrit (%) 32.138.7 35.3 (ref 35.045.0) 40.9 (ref 3440) 40.3
Hemoglobin (g/dl) 11.313.4 11.9 (ref 11.515.5) 13.7 (ref 11.016.0) 13.8
3)
White-cell count (per mm 55209290 3600 (ref 450013,500) 5260 (ref 400010,800) 5070
Differential count (%)
Neutrophils 4676 39.1 45.0 (ref 30.085.0) 39
Lymphocytes 839 45.9 44.7 (ref 15.055.0) 45
Monocytes 47 9.9 6.7 (ref 010.0) 7
Eosinophils 13 4.5 3.4 (ref 05.0) 6
Basophils 01 0.6 0.2 (ref 02.0) 1
Atypical lymphocytes 04 2
Erythrocyte sedimentation rate (mm/hr) 020 3 7 8
Heterophile Negative Negative Negative
Free thyroxine (ng/dl) 0.801.90 0.9 (ref 0.91.4) 1.25
Thyrotropin (U/ml) 0.7005.700 3.43 9.64 6.820
Sodium (mmol/liter) 135148 133 (ref 137145) 126
Potassium (mmol/liter) 3.204.50 5.2 (ref 3.55.1) 5.55
Chloride (mmol/liter) 99111 93 (ref 98107) 94
Carbon dioxide (mmol/liter) 2230 26.0 (ref 22.030.0) 23
Urea nitrogen (mg/dl) 518 22 (ref 717) 18
Creatinine (mg/dl) 0.31.0 0.6 (ref 0.51.0) 0.5
Calcium (mg/dl) 10.6 (ref 8.310.3)
Alkaline phosphatase (U/liter) 60335 235 (ref 38126) 209
Aspartate aminotransferase (U/liter) 240 63 (ref 1546) 58 (hemolyzed
specimen)
Creatine kinase (U/liter) 4150 476
Urine
Sodium (mmol/liter) 119
Creatinine (mg/dl) 67.4
* Ref denotes reference range at the pediatricians office. To convert the values for free thyroxine to picomoles per liter, multiply by 12.87. To
convert the values for urea nitrogen to millimoles per liter, multiply by 0.357. To convert the values for creatinine to micromoles per liter,
multiply by 88.4. To convert the values for calcium to millimoles per liter, multiply by 0.250.
Reference values are affected by many variables, including the patient population and the laboratory methods used. The ranges shown are
obtained from the laboratories at the other hospital.
The patients mother noted that the patient and her paternal grandmother had celiac dis-
had a long history of daydreaming. She had not ease; a paternal uncle had bipolar disorder; and
begun to menstruate. She had no history of head other relatives had anxiety, depression, or atten-
injury, loss of consciousness, urinary symptoms, tion deficithyperactivity disorder (ADHD). There
hospitalizations, or surgery. Her only medication was no family history of cystic fibrosis, inflam-
was 10 mg daily of escitalopram. She had no matory bowel disease, liver disease, pancreatitis,
known allergies. She lived with her parents and or diabetes mellitus.
younger sister. Her mother had thyroid disease; On examination, the patient was slim and ap-
maternal and paternal aunts, a paternal uncle, peared exhausted, without apparent physical dis-
2016 n engl j med 368;21 nejm.org may 23, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
tress. The blood pressure was 83/52 mm Hg, the ferase, and C-reactive protein were normal; other
pulse 102 beats per minute, the head circumfer- test results are shown in Table 1. Bupropion was
ence 53.2 cm, the weight 35.4 kg, and the height stopped, and she was referred to the emergency
149.9 cm, with a body-mass index (the weight in department of another hospital.
kilograms divided by the square of the height in On examination, the blood pressure was
meters) of 15.8 (12th percentile for age). The skin 87/45 mm Hg, the pulse 92 beats per minute with
was freckled, with multiple dark nevi and slight the patient in a supine position and 124 beats per
hyperpigmentation in the axillae. Results of minute while she was standing, the tympanic
cranial-nerve testing and funduscopic examina- temperature 36.4C, and the weight 33.5 kg. The
tion were normal. Strength was full throughout. remainder of the examination was normal. An
Reflexes were brisk, and plantar responses were electrocardiogram reportedly showed sinus rhythm
flexor. Clonus (2 to 3 beats, unsustained) on the at 100 beats per minute, with a normal axis, a
right foot occurred, but the finding was not eas- prolonged QT interval corrected for heart rate of
ily repeated. The patient initially rocked on her 505 msec, a T-wave inversion in lead III, and bi-
feet during tandem gait but later skipped and phasic T waves in lead V3. Test results are shown
jumped without difficulty. Results of sensory ex- in Table 1. The patient was admitted to the other
amination and Romberg testing were normal. hospital.
When talking with the psychiatrist, the patient Additional diagnostic tests were performed.
focused primarily on her pain and fatigue. She
appeared withdrawn and disengaged, with a sad Differ en t i a l Di agnosis
and apathetic affect. Her speech was sparse,
slow, and soft at times, and eye contact and Dr. Suzanne L. Bender: I am aware of the diagnosis
spontaneous movements were limited. Her three in this case. This 12-year-old girl with celiac dis-
wishes were to have a cell phone so she could call ease adhered to her gluten-free diet. She reported
her mother when she became nervous while many somatic symptoms and had hypersomnia
waiting for her mother to pick her up at school, but appeared in no physical distress. No medical
to have different friends, and to have school be illness had been found by her pediatrician, gas-
different. There was no delusional content, sui- troenterologist, or neurologist. She was irritable,
cidal ideation, or hallucinations. In the waiting with frequent angry outbursts at home, and had
area, she fell asleep, awakening to gentle shak- academic difficulty at school. She was referred to
ing but not to voice. Magnetic resonance imag- child psychiatry for evaluation. Because some med-
ing (MRI) of the head was normal. Diagnoses of ical conditions take time to become apparent, a
major depressive disorder and generalized anxi- multidisciplinary team was established to coor-
ety disorder were made. dinate ongoing diagnosis and treatment in this
Weekly therapy sessions were begun. During child with somatic symptoms that had no clear
the next 3 weeks, the administration of escitalo- cause but that impaired daily functioning.
pram was changed to bedtime; the administra-
tion of bupropion was begun and gradually in- Somatic symptoms
creased to 75 mg daily. The patient continued to Emotional distress may be affecting this patients
have worsening dizziness, lightheadedness, head- bodily function. This is well-described in irrita-
aches, stomachaches, and musculoskeletal pain. ble bowel syndrome as the braingut axis. Psy-
She had two episodes of vomiting at school, with chosocial influences affect gut motility and may
nonbloody, nonbilious emesis and dry heaves, increase visceral sensitivity. A change in gut mo-
and her oral intake decreased. tility and visceral sensitivity may in turn increase
On repeat examination in the psychiatry clinic anxiety and depression in some patients.1-3 There
6 weeks after the initial evaluation, the patient ap- is an ongoing conversation between the brain and
peared listless and pallid. Her weight was 34.0 kg. the body. When I talk to families in my clinic
She was referred to her pediatrician for further about this mindbody interaction, I explain that
evaluation. On examination at the pediatricians this is why we have a neck. In addition, some chil-
office 5 days later, the weight was 32.9 kg. Blood dren may have difficulty distinguishing emotional
levels of platelets, glucose, total protein, albumin, pain from physical pain. All they know is that
total and direct bilirubin, alanine aminotrans- they dont feel well, and then this is translated, in
n engl j med 368;21 nejm.org may 23, 2013 2017
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
their minds, into feeling sick. Emotional distress mononucleosis, and disorders involving calcium
expressed as somatic symptoms is a new type of metabolism are associated with depressive symp-
referred pain pain that is referred from brain toms; these disorders have already been consid-
to body. ered in this case and do not seem to explain her
Pediatric patients with somatization are likely symptoms. She has celiac disease, and adoles-
to have psychopathological symptoms, family cents with celiac disease have a higher lifetime
dysfunction, and poor performance and atten- prevalence of major depressive disorders before
dance at school.4 Children with abdominal pain diagnosis and before adoption of a gluten-free
who have a negative medical workup may have diet than do matched controls.9 Celiac disease
been exposed to a traumatic event and may have with malabsorption may cause vitamin B12 and
underlying anxiety.5 In addition, the mothers of folate deficiencies, both of which are associated
such children often have higher rates of anxiety, with mood disorders.10,11 An additional screen-
depression, and various physical ailments, as ing blood chemical profile would be useful for
compared with a control population.5,6 identifying abnormal liver and renal function
It is notable that one of this patients three and abnormal levels of electrolytes, vitamins, and
wishes was not a wish to feel physically better. glucose, which may be associated with mood
Her wishes to have different friends and to symptoms (Tables 2 and 3).11 Irritability may be
have school be different signal that these areas due to the effects of a substance (e.g., a drug of
in her life are causing distress and perhaps her abuse, a medication, or a toxin).8 Although sur-
experience of pain. reptitious substance abuse could account for all
this patients symptoms, it would be highly un-
Irritable Mood likely in a well-supervised child whose only
Evaluation of pediatric irritable mood includes medication is escitalopram.
an assessment of a childs functioning at home
and at school. This patients frequent fights with Depression
her mother and sister and concerns about her On a review of this patients symptoms, she meets
peer group could both cause and result in her all the criteria for a major depressive episode
current irritability. Although this patient had (i.e., for more than 2 weeks, she has had persis-
anxiety, her symptoms could not be explained by tent irritable mood and five or more of the fol-
anxiety alone. Persons with anxiety usually pre lowing neurovegetative symptoms: low energy,
sent with sleeplessness or restlessness, and not decreased appetite, hypersomnia, diminished in-
with hypersomnia and psychomotor retardation. terest in daily activities, psychomotor retardation,
Academic struggles may also decrease self- and decreased concentration). She reported no sad-
esteem and emotional resiliency. This patients ness, feelings of worthlessness, or suicidal ide-
grades dropped, she failed mathematics, and she ation, but children often have trouble recognizing
expressed concern about school. A consideration and reporting their emotional state. Alexithymia
in this case is attention-deficit disorder, inatten- (the inability to express ones feelings) does not
tive type. Young girls with this disorder who do rule out depression. Child psychiatrists base
not have behavioral issues are often first diag- their diagnoses on observation and on reports
nosed during middle school, when organiza- from parents, as well as on the childs self-report.
tional challenges increase. The results of neuro- Prepubertal patients with depression commonly
psychological testing could show whether this present with somatic symptoms, irritability, or
child has a nonverbal learning disorder, defined social withdrawal, whereas adolescents are more
on a test such as the Wechsler Intelligence Scale likely to have hypersomnia or psychomotor retarda-
for Children, fourth edition, as a verbal compre- tion. This patient, straddling the worlds of child-
hension score that is much greater than the per- hood and adolescence, had all these symptoms.8
ceptual reasoning score. Difficulties with organi- This patient did not have a recent loss or
zation, social skills, and academics, specifically trauma to account for her symptoms. It was pos-
mathematics, are often seen in children with this sible that she was in the depressive phase of an
disorder.7 emerging pediatric bipolar disorder, since she had
This patients irritability could be due to a some risk factors, including an early onset of de-
medical condition.8 Anemia, thyroid dysfunction, pression, atypical depression with hypersomnia,
2018 n engl j med 368;21 nejm.org may 23, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
Table 2. Differential Diagnosis of Irritable Mood in Children.*
General medical condition Neurologic Metrizamide
Autoimmune Brain tumor Metronidazole
Celiac disease Multiple sclerosis Nalidixic acid
Polyarteritis nodosa Stroke Narcotics
Rheumatoid arthritis Temporal lobe epilepsy Nifedipine
Systemic lupus erythematosus Nutritional Nonsteroidal antiinflammatory drug
Cardiovascular Vitamin B12 deficiency Norfloxacin
Cardiac tumors Folate deficiency Oral contraceptive pill
Congestive heart failure Medication use Oseltamivir phosphate
Hypertensive encephalopathy Acyclovir Phenylephrine
Anemia Anabolic steroids Prazosin
Endocrine Anticonvulsants Procaine derivatives: penicillin G procaine,
Diabetes mellitus Carbamazepine lidocaine, procainamide
Hyperadrenalism Phenytoin Thyroid hormones
Hypoadrenalism Primidone Trimethoprimsulfamethoxazole
Hyperparathyroidism Asparaginase Exposure to substances
Hypoparathyroidism Baclofen Alcohol-use disorders
Hypopituitarism Barbiturates Amphetamine-use disorders
Hypothyroidism Benzodiazepines Carbon monoxide
Hyperthyroidism Beta-blockers Cocaine-use disorders including withdrawal
Infectious Bromides Heavy metals
Hepatitis Bromocriptine Methylsulfonylmethane
Human immunodeficiency virus Clonidine Opioid use
Influenza Glucocorticoid Bereavement
Lyme disease Cycloserine Trauma
Mononucleosis Dapsone Acute stress disorder
Metabolic Digitalis Posttraumatic stress disorder
Acidbase problems Diltiazem Other mood disorders
Hypokalemia Disopyramide Major depressive disorder
Hypernatremia Ethionamide Bipolar I disorder
Hyponatremia Halothane (postoperatively) Bipolar II disorder
Renal failure Histamine H2receptor antagonists Bipolar disorder, not otherwise specified
Neoplastic Interferon alfa Cyclothymic disorder
Occult cancer Isoniazid Dysthymic disorder
Isotretinoin Adjustment disorder with depressed mood
Mefloquine Depressive disorder, not otherwise
specified
Metoclopramid
* The table is modified from Geringer et al.11
and an extensive family history of mood disor- The more risk factors a patient has, the more
ders. However, the absence of adverse effects likely it is that depression will develop.17,18
(e.g., agitation) associated with her use of esci- While I continued to collect laboratory data, I
talopram argues against a current diagnosis of made a preliminary diagnosis in this patient of
bipolar illness.12-15 treatment-resistant major depressive disorder.
The patient had several risk factors for major More information would clarify the potential
depressive disorder, including a family history of diagnosis of attention-deficit disorder, inatten-
depression,16 the presence of another nonaffective tive type.
psychiatric disorder predating the depression (anx-
iety), female sex (after puberty), and multiple Management of Childhood Depression
major life stressors (including a physical illness, Both medications and psychotherapy are used to
family conflict, and poor performance in school). treat childhood depression. Many different psy-
n engl j med 368;21 nejm.org may 23, 2013 2019
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
adults provide guidance for medications for this
Table 3. Screening Laboratory Evaluation of Irritability
in a Child with Somatic Symptoms.* child with treatment-resistant depression. Aug-
menting an antidepressant with either buspirone
Complete blood count with differential count or sustained-release bupropion results in a 30%
Complete blood chemical panel including calcium increase in the remission rate; therefore, it is a
Blood and urine toxicologic analysis reasonable next step for this child, who had
Vitamin B12 treatment-resistant major depressive disorder and
Folate no response to two trials of an SSRI.20,32,33 Bu-
Heterophile antibody test propion works through noradrenergic and dopa-
Thyrotropin minergic mechanisms and affects different neu-
Other tests to consider rotransmitters from those affected by SSRIs. If
Cerebrospinal fluid analysis the administration of bupropion were added, this
Electroencephalogram
patient could continue on escitalopram to treat
her anxiety. Bupropion is also used to treat at-
Neuroimaging
tentional disorders and may help reduce the pa-
* The table is modified from Geringer et al.11 tients reported daydreaming.34 I have found bu-
propion to be very effective in the treatment of
disengaged adolescents with somatic symptoms
chotherapies (e.g., psychodynamic psychothera- who have not responded to an SSRI.
py, family therapy, interpersonal psychotherapy, The clinical approach to major depressive
and cognitive behavioral therapy) are thought to disorder and multiple somatic symptoms in this
be effective in the treatment of pediatric depres- treatment-resistant child needs to be inclusive
sion.19-22 Cognitive behavioral therapy and relax- and comprehensive. Further laboratory studies
ation techniques have been useful in the treat- are warranted to screen for a medical condition
ment of chronic pain.23 that is fueling the mood disorder (Table 3). I rec-
Only two selective serotonin-reuptake inhibitors ommended weekly cognitive behavioral therapy
(SSRIs) are approved by the Food and Drug Ad- (for problem-solving and cognitive restructuring),
ministration (FDA) fluoxetine for the treatment the practice of relaxation techniques (to help
of children 8 years of age or older, and escitalo- with chronic pain),23 and the use of a psychody-
pram for the treatment of children 12 years of namic approach for identifying and discussing
age or older. The FDA issued a black-box warn- the patients feelings about her friends, family,
ing in 2004 that some children, adolescents, and and school. Escitalopram and bupropion were
young adults may have an increased risk of sui- administered. I recommended evaluation for pos-
cidal thoughts or behavior while taking antide- sible attention-deficit disorder, as well as neuro-
pressants.24 One meta-analysis showed that the psychological testing to identify any learning
increased risk in suicidal thoughts was between disorders.
1% and 3%.25 Another meta-analysis concluded Despite these approaches, the patients so-
that the clinical benefits associated with the use matic symptoms worsened, and she began to
of antidepressants in children with depression lose weight and appear ill. She was urgently re-
outweighed the risks.26 ferred back to her pediatrician.
In patients who have not previously received
treatment, evidence supports the use of fluoxetine DR . SUZ A NNE L . BENDERS
combined with cognitive behavioral therapy for DI AGNOSIS
the safest and fastest clinical response.27,28 This
patients depression continued despite psycho- Major depressive disorder and high suspicion for
therapy and two trials of an SSRI. Although a concurrent medical illness.
venlafaxine has been studied as an alternative
antidepressant agent for adolescents with treat- Pathol o gic a l Discussion
ment-resistant depression, it has a higher inci-
dence of side effects, including suicidality, over Dr. Ricard Masia: The patient had undergone upper
the long term than do SSRIs.29-31 gastrointestinal endoscopy at 8 years of age. Dif-
Studies of treatment-resistant depression in fuse mildly scalloped mucosa was found in the
2020 n engl j med 368;21 nejm.org may 23, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
second part of the duodenum. Biopsy specimens
A
showed duodenal mucosa with subtotal villous
atrophy and crypt hyperplasia (Fig. 1A). The
number of intraepithelial lymphocytes was mark-
edly increased, with more than 40 intraepithelial
lymphocytes per 100 enterocytes, and there was
associated enterocyte injury (Fig. 1B). In the con-
text of the patients symptoms and positive anti
tissue transglutaminase antibody test, these
findings were consistent with duodenal involve-
ment by celiac disease. According to the Marsh
Oberhuber classification, the histologic findings
correspond to a type 3b lesion (subtotal villous
B
atrophy, crypt hyperplasia, and >40 intraepithe-
lial lymphocytes per 100 enterocytes).35
The diagnostic tests performed at the other
hospital included a plasma cortisol test, which
involved three specimens drawn at baseline and
during a cosyntropin stimulation test, all measur-
ing less than 0.3 g per deciliter (8.3 nmol per
liter; reference range, 5.0 to 25.0 g per deciliter
[138.0 to 689.8 nmol per liter]). The plasma corti-
cotropin level was 2069 pg per milliliter (456 pmol
per liter; reference range, 46 pg per milliliter Figure 1. Duodenal-Biopsy Specimen (Hematoxylin
and Eosin).
[10 pmol per liter]), the anti21-hydroxylase anti-
The duodenal mucosa shows subtotal villous atrophy
body level 684.2 U per milliliter (reference range, and crypt hyperplasia (Panel A). The number of intra-
1.0), and the plasma renin activity 5633 ng per epithelial lymphocytes is markedly increased (Panel B,
deciliter per hour (reference range, 50 to 330). arrows).
These results indicate adrenal insufficiency.
Data are limited regarding the pathological
findings in patients with both celiac disease and
Addisons disease; therefore, it is difficult to as- 21-hydroxylase antibody level are diagnostic of
sess whether findings on examination of small- autoimmune primary adrenal failure. This re-
bowel-biopsy specimens can help identify patients sults in a loss of adrenal glucocorticoid, miner-
with celiac disease who are at increased risk for alocorticoid, and androgen production because
the development of Addisons disease. However, of destruction of the adrenal cortex by autoreac-
case series involving patients with Addisons dis- tive T cells. As a result of the loss of negative
ease have identified some patients with previously feedback of cortisol on the hypothalamus and
known or undiagnosed celiac disease. Although pituitary, corticotropin levels rise dramatically and
most patients with celiac disease and Addisons levels of thyrotropin can rise mildly. Because of
disease had destructive lesions (MarshOberhuber the loss of the effects of mineralocorticoids on
type 3) on duodenal biopsy, some patients had a salt and water balance, there is decreased renal
histologically normal mucosa.36-39 These data perfusion pressure, which drives the production
suggest that there is no reliable correlation be- of plasma renin activity.
tween biopsy findings and the risk of the devel- Through the lens of an endocrinologist, this
opment of Addisons disease. patients signs and symptoms match the text-
book description of adrenal insufficiency, just as
Discussion of M a nagemen t they matched the textbook picture of major de-
pressive disorder when interpreted by her psy-
Dr. Nicole A. Sherry: The undetectable plasma corti- chiatrist. Specifically, the patient had chronic
sol levels, elevated plasma corticotropin level, weakness, fatigue, anorexia, nausea, vomiting,
elevated plasma renin activity, and elevated abdominal pain, dizziness, and muscle and joint
n engl j med 368;21 nejm.org may 23, 2013 2021
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
pains. She had weight loss, hyperpigmentation, Dr. Pinsky: The patient was discharged from
hypotension, hyponatremia, hyperkalemia, hy- the other hospital taking only escitalopram and
percalcemia, anemia, and eosinophilia. Even glucocorticoid-replacement and mineralocorticoid-
more striking, she had had episodes of acute replacement therapy. The nausea, vomiting, pain,
adrenal crises with profound deterioration dur- and weakness diminished rapidly, and her appe-
ing intercurrent viral illnesses over the preced- tite quickly improved; her mother reported that
ing year and a half that had required three hos- the patient ate two candy bars on the way home
pitalizations. from the hospital. Fatigue persisted but was
The diagnosis of Addisons disease is often improved. The hope was that her symptoms had
missed for some time, as it was in this case. In all been related to underlying adrenal insuffi-
one study, only 47% of the cases were diagnosed ciency and that she might eventually be able to
within 1 year after initial symptoms and more discontinue escitalopram.
than 20% were diagnosed more than 5 years After approximately 3 months of glucocorticoid-
after initial symptoms.40 Thirty percent of the replacement therapy, the patient continued to be
patients had seen five physicians before the di- socially withdrawn and anxious, was still sleep-
agnosis of Addisons disease was made. More ing 12 to 14 hours a day, and struggled with
than 80% had had a previous incorrect diagno- inattention and academic faltering. Neuropsy-
sis, 50% of which were psychiatric disorders and chiatric testing was performed and was sugges-
31% of which were gastrointestinal diseases. tive of ADHD, although assessment of attention
In this case, there is an important clue to the was confounded by depressed mood and anxiety,
diagnosis. This patient had a personal history of as well as her recent medical illness. The admin-
celiac disease and a family history of both celiac istration of bupropion was resumed. After several
disease and autoimmune thyroid disease. This weeks, symptoms of withdrawal, anxiety, ener-
constellation of diseases is highly suggestive of gy, and attention improved. At the end of the
the autoimmune polyglandular syndrome type 2 academic year, the patient was the champion of
and should alert the clinician that the patient is the science fair.
at high risk for other autoimmune disorders, in- Dr. Sherry: Although the focus of current treat-
cluding autoimmune adrenal insufficiency, thy- ment studies has been finding a better physio-
roid disease, and celiac disease.41 logical match of hormonal replacement to help
After the diagnosis of Addisons disease was with psychiatric symptoms, this patients symp-
made, the patient was treated with hydrocorti- toms were successfully treated with a combina-
sone (9 mg per square meter of body-surface tion of traditional hormonal replacement and
area divided into three doses daily) and fludro- psychopharmacologic approaches.
cortisone (0.1 mg daily). Although the somatic Dr. Nancy Lee Harris (Pathology): Are there any
symptoms resolved, she continued to have psy- comments or questions?
chiatric symptoms. It has been recognized that Dr. Joshua Roffman (Psychiatry): In retrospect,
for patients with adrenal insufficiency who ad- were there any red flags in the patients presen-
here to current treatment regimens, the quality tation that suggested a medical component to
of life can be impaired,42 with a perception of her symptoms that we should look for when
reduced general health and vitality and increased evaluating depression in children?
fatigue as compared with population norms. Pa- Dr. Bender: At first, this patient looked tired
tients with autoimmune polyendocrine syndromes but otherwise physically well and she had a
have lower scores in these measures on subjec- negative medical workup. Many patients with a
tive health-assessment questionnaires than do similar presentation get better with psychiatric
those with adrenal insufficiency in isolation.43,44 treatment. Some medical diagnoses become clear
The administration of adrenal androgens that as symptoms evolve over time, which is why on-
have not been traditionally replaced may improve going coordinated care between psychiatry and
the quality of life. Several short-term studies have pediatrics is so critical for patients with somatic
shown that the administration of dehydroepi- symptoms. A key moment was when the patient,
androsterone improves psychological health,45,46 who had appeared well, started to look sick. Dr.
but the results are mixed, and longer-term stud- Pinsky recognized that her condition had changed
ies have not shown as pronounced an effect.43,47 and referred her for additional evaluation.
2022 n engl j med 368;21 nejm.org may 23, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
A Physician: Were her parents angry that it reportedly normal. Because of the axillary freck-
took 16 months for a diagnosis to be made? ling, I entertained the diagnosis of neurofibro-
The Patients Father: For a very long time, our matosis 1. I referred her for an ophthalmologic
daughter has had continuing mental and physi- examination to look for Lisch nodules and or-
cal problems. It was difficult and traumatic, but dered a brain MRI to rule out an intracranial
were very thankful for all the doctors who even- process that might account for the nausea and
tually made the diagnosis and brought her to vomiting.
where she is today. Dr. Sherry: Addisons disease can be associated
Dr. Harris: I think its instructive to learn of with other skin findings, such as more gener-
the usual delay in the diagnosis of Addisons alized hyperpigmentation, especially in sun-
disease. There are so many possible causes of all exposed areas, whereas neurofibromatosis can
these symptoms that Addisons disease is not on be associated with caf au lait lesions. In this
the top of anyones differential diagnosis. patient with no other skin findings, a distinction
Dr. Harland Winter (Pediatric Gastroenterology): between Addisons disease and neurofibromato-
Was the axillary hyperpigmentation a potential sis could not be made on the basis of axillary
clue to adrenal insufficiency? freckling alone.
Dr. Sherry: Yes, hyperpigmentation in Addisons
disease is due to an increase in melanocyte- A nat omic a l Di agnosis
stimulating hormone. The axillae are a typical
location for hyperpigmentation, which is most Celiac disease, Addisons disease, and major de-
often diffuse. pressive disorder.
Dr. Robin M. Jones (Neurology): The patient was Presented at Psychiatry Grand Rounds.
referred to me from gastroenterology because of Dr. Sherry reports receiving consulting fees and grant support
recurrent nausea and vomiting, which had been through her institution from MacroGenics. No other potential
conflict of interest relevant to this article was reported.
attributed to the cyclic vomiting syndrome at an Disclosure forms provided by the authors are available with
outside institution. An electroencephalogram was the full text of this article at NEJM.org.
References
1. Elsenbruch S. Abdominal pain in irri- Straight talk about psychological testing pressed children. J Am Acad Child Ado-
table bowel syndrome: a review of putative for kids. New York: Guilford Press, 2004: lesc Psychiatry 1994;33:461-8.
psychological, neural and neuro-immune 151-77. 14. Forty L, Smith D, Jones L, et al. Clini-
mechanisms. Brain Behav Immun 2011; 8. Diagnostic and statistical manual of cal differences between bipolar and uni-
25:386-94. mental disorders, 4th ed. rev.: DSM-IV-R. polar depression. Br J Psychiatry 2008;
2. Drossman DA. The functional gastro- Washington, DC: American Psychiatric 192:388-9.
intestinal disorders and the Rome II pro- Association, 2000. 15. Benazzi F. Classifying mood disor-
cess. Gut 1999;45:Suppl 2:II1-II5. 9. Pynnnen PA, Isomets ET, Aronen ders by age-at-onset instead of polarity.
3. Koloski NA, Jones M, Kalantar J, Welt- ET, Verkasalo MA, Savilahti E, Aalberg Prog Neuropsychopharmacol Biol Psychi-
man M, Zaguirre J, Talley NJ. The brain VA. Mental disorders in adolescents with atry 2009;33:86-93.
gut pathway in functional gastrointesti- celiac disease. Psychosomatics 2004;45: 16. Weissman MM, Wickramaratne P,
nal disorders is bidirectional: a 12-year 325-35. Nomura Y, et al. Families at high and low
prospective population-based study. Gut 10. Garca-Manzanares A, Lucendo AJ. risk for depression: a 3-generation study.
2012;61:1284-90. Nutritional and dietary aspects of celiac Arch Gen Psychiatry 2005;62:29-36.
4. Campo JV, Jansen-McWilliams L, disease. Nutr Clin Pract 2011;26:163-73. 17. Lewinsohn PM, Rohde P, Seeley JR.
Comer DM, Kelleher KJ. Somatization in 11. Geringer ES, Querques J, Kolodziej Major depressive disorder in older adoles-
pediatric primary care: association with MS, Burns TE, Stern TA. Diagnosis and cents: prevalence, risk factors, and clini-
psychopathology, functional impairment, treatment of depression in the intensive cal implications. Clin Psychol Rev 1998;
and use of services. J Am Acad Child Ado- care unit patient. In: Irwin RS, Rippe JM, 18:765-94.
lesc Psychiatry 1999;38:1093-101. eds. Irwin and Rippes intensive care 18. Rohde P, Lewinsohn PM, Seeley JR.
5. Wasserman AL, Whitington PF, Rivara medicine. 7th ed. Philadelphia: Lippincott Comorbidity of unipolar depression: II.
FP. Psychogenic basis for abdominal pain Williams & Wilkins, 2012:2087-98. Comorbidity with other mental disorders
in children and adolescents. J Am Acad 12. Akiskal HS, Maser JD, Zeller PJ, et al. in adolescents and adults. J Abnorm Psy-
Child Adolesc Psychiatry 1988;27:179-84. Switching from unipolar to bipolar II: chol 1991;100:214-22.
6. Campo JV, Bridge J, Lucas A, et al. an 11-year prospective study of clinical 19. Weisz JR, McCarty CA, Valeri SM. Ef-
Physical and emotional health of mothers and temperamental predictors in 559 pa- fects of psychotherapy for depression in
of youth with functional abdominal pain. tients. Arch Gen Psychiatry 1995;52: children and adolescents: a meta-analy-
Arch Pediatr Adolesc Med 2007;161:131-7. 114-23. sis. Psychol Bull 2006:132:132-49.
7. Braaten E, Felopulos G. Nonverbal 13. Geller B, Fox LW, Clark KA. Rate and 20. Choe CJ, Emslie GJ, Mayes TL. De-
learning disorders and Asperger syn- predictors of prepubertal bipolarity dur- pression. Child Adolesc Psychiatric Clin
drome. In: Braaten E, Felopolus G, eds. ing follow-up of 6- to 12-year-old de- N Am 2012;21:807-29.
n engl j med 368;21 nejm.org may 23, 2013 2023
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
21. Birmaher B, Brent D, Bernet W, et al. the Treatment of SSRI-Resistant Depres- liac disease in Italian patients affected by
Practice parameter for the assessment and sion in Adolescents (TORDIA) study. Am J Addisons disease. Scand J Gastroenterol
treatment of children and adolescents with Psychiatry 2009;166:418-26. 2006;41:302-5.
depressive disorders. J Am Acad Child 30. Vitiello B, Emslie G, Clarke G, et al. 39. Betterle C, Lazzarotto F, Spadaccino
Adolesc Psychiatry 2007;46:1503-26. Long-term outcome of adolescent depres- AC, et al. Celiac disease in North Italian
22. Hofmann SG, Asnaani A, Vonk IJJ, sion initially resistant to selective sero- patients with autoimmune Addisons dis-
Sawyer AT, Fang A. The efficacy of cogni- tonin reuptake inhibitor treatment: a fol- ease. Eur J Endocrinol 2006;154:275-9.
tive behavioral therapy: a review of meta- low-up study of the TORDIA sample. 40. Bleicken B, Hahner S, Ventz M, Quink
analyses. Cognit Ther Res 2012;36:427-40. J Clin Psychiatry 2011;72:388-96. ler M. Delayed diagnosis of adrenal insuf-
23. Palermo TM, Eccleston C, Lewan- 31. Brent D, Emslie G, Clarke G, et al. ficiency is common: a cross-sectional
dowski AS, Williams AC, Morley S. Ran- Switching to another SSRI or to venlafax- study in 216 patients. Am J Med Sci 2010;
domized controlled trials of psychologi- ine with or without cognitive behavioral 339:525-31.
cal therapies for management of chronic therapy for adolescents with SSRI-resis- 41. Eisenbarth GS, Gottlieb PA. Autoim-
pain in children and adolescents: an up- tant depression: the TORDIA randomized mune polyendocrine syndromes. N Engl J
dated meta-analytic review. Pain 2010; controlled trial. JAMA 2008;299:901-13. Med 2004;350:2068-79.
148:387-97. 32. Trivedi MH, Fava M, Wisniewski SR, 42. Lvs K, Loge JH, Husebye ES. Subjec-
24. Antidepressant medications for chil- et al. Medication augmentation after the tive health status in Norwegian patients
dren and adolescents: information for failure of SSRIs for depression. N Engl J with Addisons disease. Clin Endocrinol
parents and caregivers. Bethesda, MD: Med 2006;354:1243-52. (Oxf) 2002;56:581-8.
National Institute of Mental Health, 2011 33. Hughes CW, Emslie GJ, Crismon ML, 43. Gurnell EM, Hunt PJ, Curran SE, et al.
(http://www.nimh.nih.gov/health/topics/ et al. Texas Childrens Medication Algo- Long-term DHEA replacement in primary
child-and-adolescent-mental-health). rithm Project: update from Texas Consen- adrenal insufficiency: a randomized, con-
25. Hammad TA, Laughren T, Racoosin J. sus Conference Panel on Medication trolled trial. J Clin Endocrinol Metab
Suicidality in pediatric patients treated Treatment of Childhood Major Depressive 2008;93:400-9.
with antidepressant drugs. Arch Gen Psy- Disorder. J Am Acad Child Adolesc Psy- 44. Hahner S, Loeffler M, Fassnacht M, et
chiatry 2006;63:332-9. chiatry 2007;46:667-86. al. Impaired subjective health status in
26. Bridge JA, Iyengar S, Salary CB, et al. 34. Barrickman LL, Perry PJ, Allen AJ, et 256 patients with adrenal insufficiency
Clinical response and risk for reported al. Bupropion versus methylphenidate in on standard therapy based on cross-sec-
suicidal ideation and suicide attempts in the treatment of attention-deficit hyper- tional analysis. J Clin Endocrinol Metab
pediatric antidepressant treatment: a meta- activity disorder. J Am Acad Child Adolesc 2007;92:3912-22.
analysis of randomized controlled trials. Psychiatry 1995;34:649-57. 45. Arlt W, Callies F, van Vlijmen JC, et al.
JAMA 2007;297:1683-96. 35. Oberhuber G, Granditsch G, Vogel- Dehydroepiandrosterone replacement in
27. March J, Silva S, Petrycki S, et al. sang H. The histopathology of coeliac women with adrenal insufficiency. N Engl
Fluoxetine, cognitive-behavioral therapy, disease: time for a standardized report J Med 1999;341:1013-20.
and their combination for adolescents with scheme for pathologists. Eur J Gastroen- 46. Hunt PJ, Gurnell EM, Huppert FA, et
depression: Treatment for Adolescents terol Hepatol 1999;11:1185-94. al. Improvement in mood and fatigue af-
With Depression Study (TADS) random- 36. OLeary C, Walsh CH, Wieneke P, et ter dehydroepiandrosterone replacement
ized controlled trial. JAMA 2004;292: al. Coeliac disease and autoimmune Ad- in Addisons disease in a randomized,
807-20. disons disease: a clinical pitfall. QJM double blind trial. J Clin Endocrinol
28. March JS, Silva S, Petrycki S, et al. The 2002;95:79-82. Metab 2000;85:4650-6.
Treatment for Adolescents With Depres- 37. Myhre AG, Aarsety H, Undlien DE, 47. Alkatib AA, Cosma M, Elamin MB, et
sion Study (TADS): long-term effective- Hovdenak N, Aksnes L, Husebye ES. High al. A systematic review and meta-analysis
ness and safety outcomes. Arch Gen Psy- frequency of coeliac disease among pa- of randomized placebo-controlled trials
chiatry 2007;64:1132-43. [Erratum, Arch tients with autoimmune adrenocortical of DHEA treatment effects on quality of
Gen Psychiatry 2008;65:101.] failure. Scand J Gastroenterol 2003;38: life in women with adrenal insufficiency.
29. Brent DA, Emslie GJ, Clarke GN, et al. 511-5. J Clin Endocrinol Metab 2009;94:3676-
Predictors of spontaneous and systemati- 38. Biagi F, Campanella J, Soriani A, 81.
cally assessed suicidal adverse events in Vailati A, Corazza GR. Prevalence of coe- Copyright 2013 Massachusetts Medical Society.
Lantern Slides Updated: Complete PowerPoint Slide Sets from the Clinicopathological Conferences
Any reader of the Journal who uses the Case Records of the Massachusetts General Hospital as a teaching exercise or reference
material is now eligible to receive a complete set of PowerPoint slides, including digital images, with identifying legends,
shown at the live Clinicopathological Conference (CPC) that is the basis of the Case Record. This slide set contains all of the
images from the CPC, not only those published in the Journal. Radiographic, neurologic, and cardiac studies, gross specimens,
and photomicrographs, as well as unpublished text slides, tables, and diagrams, are included. Every year 40 sets are produced,
averaging 50-60 slides per set. Each set is supplied on a compact disc and is mailed to coincide with the publication of the
Case Record.
The cost of an annual subscription is $600, or individual sets may be purchased for $50 each. Application forms for the current
subscription year, which began in January, may be obtained from the Lantern Slides Service, Department of Pathology,
Massachusetts General Hospital, Boston, MA 02114 (telephone 617-726-2974) or e-mail Pathphotoslides@partners.org.
2024 n engl j med 368;21 nejm.org may 23, 2013
The New England Journal of Medicine
Downloaded from nejm.org on November 10, 2013. For personal use only. No other uses without permission.
Copyright 2013 Massachusetts Medical Society. All rights reserved.
Você também pode gostar
- Data Interpretation For Medical Students, 2e (Pastest)Documento642 páginasData Interpretation For Medical Students, 2e (Pastest)Test MRCP100% (1)
- Case 3-2020: A 44-Year-Old Man With Weight Loss, Diarrhea, and Abdominal PainDocumento10 páginasCase 3-2020: A 44-Year-Old Man With Weight Loss, Diarrhea, and Abdominal PainAlvaro Andres Flores JimenezAinda não há avaliações
- NEJM Case Report 40-2017Documento10 páginasNEJM Case Report 40-2017A. Rauf100% (1)
- S64 - FPSC Loha Mandi Jaipur House MKT, Opp. Dr. B.K.Agarwal, Loha Mandi, Ph.0562-4301106, 9897155250 Agra 282002Documento4 páginasS64 - FPSC Loha Mandi Jaipur House MKT, Opp. Dr. B.K.Agarwal, Loha Mandi, Ph.0562-4301106, 9897155250 Agra 282002Jagtendra IndoliaAinda não há avaliações
- KumkumDocumento9 páginasKumkumdeepika kushwah71% (14)
- Lifeguarding ManualDocumento405 páginasLifeguarding Manualmegan100% (3)
- Caso 24 2016NEJMcpc1503829Documento14 páginasCaso 24 2016NEJMcpc1503829claudia montesAinda não há avaliações
- Case 31 - 2019Documento12 páginasCase 31 - 2019Gustavo AngelesAinda não há avaliações
- Caso Clínico para A P1 - Vale 1 Ponto ExtraDocumento11 páginasCaso Clínico para A P1 - Vale 1 Ponto ExtraNubia Ferrari GuedesAinda não há avaliações
- Nejmcpc 2027096Documento10 páginasNejmcpc 2027096Camille MalilayAinda não há avaliações
- Nej M CPC 2100282Documento10 páginasNej M CPC 2100282Paulo Ricardo D. PereiraAinda não há avaliações
- Nej M CPC 2103461Documento10 páginasNej M CPC 2103461monaAinda não há avaliações
- Uso CorticoidesDocumento9 páginasUso CorticoidesRolando Lopez ZegarraAinda não há avaliações
- Acute Kidney FailureDocumento8 páginasAcute Kidney FailureJuan Diego Ferreyros ArroyoAinda não há avaliações
- Caso Especial Grupo 1Documento18 páginasCaso Especial Grupo 1Josè BermúdezAinda não há avaliações
- Case 2-2019 - A 36-Year-Old Man With Rash, Abdominal Pain, and Lymphadenopathy - Chen Et Al - 2019Documento9 páginasCase 2-2019 - A 36-Year-Old Man With Rash, Abdominal Pain, and Lymphadenopathy - Chen Et Al - 2019nejdAinda não há avaliações
- Cabot 2015Documento9 páginasCabot 2015Analia CortezAinda não há avaliações
- Case 1-2010Documento11 páginasCase 1-2010isravg94Ainda não há avaliações
- Valores de Referencia NEJMDocumento16 páginasValores de Referencia NEJMMarlinAinda não há avaliações
- A 43-Year-Old Man With Diabetes, Hypogonadism, Cirrhosis, Arthralgias, and FatigueDocumento8 páginasA 43-Year-Old Man With Diabetes, Hypogonadism, Cirrhosis, Arthralgias, and FatigueLara SousaAinda não há avaliações
- Blood Report PDFDocumento6 páginasBlood Report PDFPratyush ParagAinda não há avaliações
- Porfiria y GBDocumento13 páginasPorfiria y GBnkjkbjhknAinda não há avaliações
- Infectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersNo EverandInfectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersAinda não há avaliações
- WM68Documento4 páginasWM68CloudCom TechnologyAinda não há avaliações
- Faring It IsDocumento10 páginasFaring It Isnanda tsalasaniAinda não há avaliações
- Nej M CPC 1209935Documento9 páginasNej M CPC 1209935drfmentAinda não há avaliações
- Manish 1Documento1 páginaManish 1Manish kumarAinda não há avaliações
- Nejmcpc 2300910Documento9 páginasNejmcpc 2300910carb0ne14rAinda não há avaliações
- LoiuDocumento32 páginasLoiuDevi Grania AmeliaAinda não há avaliações
- NEJMcpc 2312731Documento11 páginasNEJMcpc 2312731cehborrotoAinda não há avaliações
- Caso Clinico - SepsisDocumento9 páginasCaso Clinico - SepsisJavier EspezuaAinda não há avaliações
- Texas A and M ResultsDocumento6 páginasTexas A and M ResultsraisingaddieAinda não há avaliações
- Incase Susp Leukemia EditingDocumento28 páginasIncase Susp Leukemia EditingDea PuspitaAinda não há avaliações
- Aeftih00xz45wh31kru1fekbDocumento6 páginasAeftih00xz45wh31kru1fekbAvantika BirwalAinda não há avaliações
- Rosh Review 11Documento6 páginasRosh Review 11Sarwar BaigAinda não há avaliações
- Blood Screening ReportDocumento2 páginasBlood Screening ReportSarathAinda não há avaliações
- Lab ResultDocumento1 páginaLab Resultrakibul islamAinda não há avaliações
- Case Scenario Osteoarthritis Week 16 GerontologDocumento5 páginasCase Scenario Osteoarthritis Week 16 GerontologMary Josette NavarraAinda não há avaliações
- Sikund Diagnostic CentreDocumento3 páginasSikund Diagnostic CentreAnuja GairolaAinda não há avaliações
- Case StudyDocumento43 páginasCase StudyElena Cariño De Guzman100% (1)
- 10 1016@j Thromres 2019 10 005Documento7 páginas10 1016@j Thromres 2019 10 005Ibrahim Al ShantiAinda não há avaliações
- Nrz540jtrj1gwhdtvsdgmmtaDocumento2 páginasNrz540jtrj1gwhdtvsdgmmtaAsthaAinda não há avaliações
- Kusum Lata - 2401327Documento2 páginasKusum Lata - 2401327gauravsaxena0307Ainda não há avaliações
- Patient Profile: Personal InformationDocumento13 páginasPatient Profile: Personal Informationdr yasminAinda não há avaliações
- Nej M CPC 2309382Documento8 páginasNej M CPC 2309382mnf6bb2tckAinda não há avaliações
- Supplementary Online Content: © 2020 American Medical Association. All Rights ReservedDocumento19 páginasSupplementary Online Content: © 2020 American Medical Association. All Rights ReservedMai GonzalezAinda não há avaliações
- QuizDocumento4 páginasQuizyousefjarrar606Ainda não há avaliações
- Health HistoryDocumento28 páginasHealth HistoryAnastasya Gishella RorongAinda não há avaliações
- Case 21-2012: A 27-Year-Old Man With Fatigue, Weakness, Weight Loss, and Decreased LibidoDocumento13 páginasCase 21-2012: A 27-Year-Old Man With Fatigue, Weakness, Weight Loss, and Decreased Libidodamian velmonteAinda não há avaliações
- 473 845 1 SM PDFDocumento7 páginas473 845 1 SM PDFDodi JajaAinda não há avaliações
- Mycobacteria Cocos PDFDocumento6 páginasMycobacteria Cocos PDFMila Fer D. PridonttAinda não há avaliações
- CBC LalpathDocumento2 páginasCBC Lalpathmoyic39272Ainda não há avaliações
- Blood ReportDocumento3 páginasBlood ReportPratyush ParagAinda não há avaliações
- NEJM 5 Colitis UlcerosaDocumento11 páginasNEJM 5 Colitis Ulcerosa0228154Ainda não há avaliações
- Ancylostoma Duodenale Presented As Severe Anaemia: A Case Report in A Tertiary Care Centre, North-East IndiaDocumento5 páginasAncylostoma Duodenale Presented As Severe Anaemia: A Case Report in A Tertiary Care Centre, North-East IndiaIJAR JOURNALAinda não há avaliações
- ReportViewer 1Documento1 páginaReportViewer 1khantula73Ainda não há avaliações
- Cazuri CliniceDocumento32 páginasCazuri CliniceHeba VerebceanAinda não há avaliações
- Case ICM I Week 1 SeninDocumento4 páginasCase ICM I Week 1 Seninjose feterAinda não há avaliações
- Case 15-2017: A 27-Year-Old Woman With Anemia, Thrombocytosis, and Skin Lesions After Travel AbroadDocumento10 páginasCase 15-2017: A 27-Year-Old Woman With Anemia, Thrombocytosis, and Skin Lesions After Travel AbroadGénesis LeónAinda não há avaliações
- Hematologi Efek LinezolideDocumento4 páginasHematologi Efek Linezolideendah rahmadaniAinda não há avaliações
- Diagnosis of Blood and Bone Marrow DisordersNo EverandDiagnosis of Blood and Bone Marrow DisordersSa A. WangAinda não há avaliações
- Brain Resuscitation: Nabil El Sanadi, MD, MBA, Marc Plotkin, MDDocumento33 páginasBrain Resuscitation: Nabil El Sanadi, MD, MBA, Marc Plotkin, MDIrmagian PaleonAinda não há avaliações
- 5 Local Anaesthetic PharmacologyDocumento7 páginas5 Local Anaesthetic PharmacologyMahavir GemavatAinda não há avaliações
- Mickal1968 PDFDocumento5 páginasMickal1968 PDFIrmagian PaleonAinda não há avaliações
- H1localane PDFDocumento20 páginasH1localane PDFMohammed FeroAinda não há avaliações
- 2000PPDS447Documento278 páginas2000PPDS447Irmagian PaleonAinda não há avaliações
- TrichuriasisDocumento13 páginasTrichuriasisIrmagian PaleonAinda não há avaliações
- 1.4.10 DePlatchett PIDDocumento24 páginas1.4.10 DePlatchett PIDIrmagian PaleonAinda não há avaliações
- HTN Late PregnancyDocumento2 páginasHTN Late PregnancyDellAinda não há avaliações
- Odontogenic SinusitisDocumento65 páginasOdontogenic SinusitisIrmagian PaleonAinda não há avaliações
- Journal Nejmcpc1208145Documento10 páginasJournal Nejmcpc1208145Irmagian PaleonAinda não há avaliações
- Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineDocumento12 páginasOutcomes After Angiography With Sodium Bicarbonate and AcetylcysteineIrmagian PaleonAinda não há avaliações
- Journal Nejmcpc1215971Documento11 páginasJournal Nejmcpc1215971Irmagian PaleonAinda não há avaliações
- AHA Hypertension Guidelines 2017Documento22 páginasAHA Hypertension Guidelines 2017Anonymous elSqPhzKAinda não há avaliações
- Addar Professor Gyneoncologist Ob/Gyn Dept - Kkuh and College of Medicine Mking Saud UniversityDocumento83 páginasAddar Professor Gyneoncologist Ob/Gyn Dept - Kkuh and College of Medicine Mking Saud UniversityDawn MarcoAinda não há avaliações
- Nejmcp033496 PDFDocumento11 páginasNejmcp033496 PDFIrmagian PaleonAinda não há avaliações
- Journal Nejmcibr1302851Documento2 páginasJournal Nejmcibr1302851Irmagian PaleonAinda não há avaliações
- Australia Awards Brochure PDFDocumento2 páginasAustralia Awards Brochure PDFIrmagian PaleonAinda não há avaliações
- Huang2016 PDFDocumento11 páginasHuang2016 PDFIrmagian PaleonAinda não há avaliações
- Doipdf10 1056NEJMcp0912024 PDFDocumento7 páginasDoipdf10 1056NEJMcp0912024 PDFIrmagian PaleonAinda não há avaliações
- Fluids, Electrolytes, and Dehydration: Mark Davenport and S. H. S. SyedDocumento12 páginasFluids, Electrolytes, and Dehydration: Mark Davenport and S. H. S. SyedHario Tri HendrokoAinda não há avaliações
- Research ArticleDocumento8 páginasResearch ArticleIrmagian PaleonAinda não há avaliações
- Nejmoa067407 PDFDocumento9 páginasNejmoa067407 PDFIrmagian PaleonAinda não há avaliações
- Baru 414.2.full PDFDocumento6 páginasBaru 414.2.full PDFIrmagian PaleonAinda não há avaliações
- Doipdf10 1056NEJMcp012067 PDFDocumento6 páginasDoipdf10 1056NEJMcp012067 PDFIrmagian PaleonAinda não há avaliações
- Nejmoa 040388Documento11 páginasNejmoa 040388Irmagian PaleonAinda não há avaliações
- Doipdf10 1056NEJMcp0912024 PDFDocumento7 páginasDoipdf10 1056NEJMcp0912024 PDFIrmagian PaleonAinda não há avaliações
- New England Journal Medicine: The ofDocumento9 páginasNew England Journal Medicine: The ofIrmagian PaleonAinda não há avaliações
- Nejmcp033496 PDFDocumento11 páginasNejmcp033496 PDFIrmagian PaleonAinda não há avaliações
- Functional Hypothalamic Amenorrhea: Clinical PracticeDocumento7 páginasFunctional Hypothalamic Amenorrhea: Clinical PracticeIrmagian PaleonAinda não há avaliações
- Evidence Based SearchDocumento5 páginasEvidence Based SearchGluteus MAXAinda não há avaliações
- PulpektomiDocumento4 páginasPulpektomiRysmah Zainal ArifinAinda não há avaliações
- Mammogram Waiver - Peace Corps Mammogram Form TG-355-2 (Initial Approval 08/2012)Documento3 páginasMammogram Waiver - Peace Corps Mammogram Form TG-355-2 (Initial Approval 08/2012)Accessible Journal Media: Peace Corps DocumentsAinda não há avaliações
- Hospital Business PlanDocumento49 páginasHospital Business PlanJoseph QuillAinda não há avaliações
- OB Dystocia Part II and IIIDocumento6 páginasOB Dystocia Part II and IIICyner CruzAinda não há avaliações
- Articulators, Uses and Importance in Prosthodontics Presented by DR Aghimien Osaronse A 5 MAY, 2009Documento25 páginasArticulators, Uses and Importance in Prosthodontics Presented by DR Aghimien Osaronse A 5 MAY, 20092oclockAinda não há avaliações
- Empanelled Hospitals On SRDocumento17 páginasEmpanelled Hospitals On SRpradeeperd10011988Ainda não há avaliações
- 194 Surgical Cases PDFDocumento160 páginas194 Surgical Cases PDFkint100% (4)
- Demirjian 1976Documento11 páginasDemirjian 1976careAinda não há avaliações
- Light CriteriaDocumento4 páginasLight CriteriaKei Adam KurataAinda não há avaliações
- VT Vs SVT AberrantDocumento41 páginasVT Vs SVT AberrantAl Hijjah FadhilahAinda não há avaliações
- Anastesi TopikalDocumento10 páginasAnastesi TopikallamhotfarmaAinda não há avaliações
- T D B G &: H E Iffe Rence E Tween OodDocumento54 páginasT D B G &: H E Iffe Rence E Tween Oodrajesh bathulaAinda não há avaliações
- Hospital Thesis Chapter 3aDocumento49 páginasHospital Thesis Chapter 3aParisGeronimoAinda não há avaliações
- Immunization Form International Visiting StudentsDocumento2 páginasImmunization Form International Visiting Studentsmellb99Ainda não há avaliações
- Contrast Media in Diagnostic RadiologyDocumento56 páginasContrast Media in Diagnostic RadiologyFaiq Syukri Bin SaparudinAinda não há avaliações
- Chapter 1 Overview of Critical Care StudentDocumento40 páginasChapter 1 Overview of Critical Care StudentEmilyAinda não há avaliações
- Pediatric BLSDocumento32 páginasPediatric BLSYuni AjahAinda não há avaliações
- 002 - CPR CommitteeDocumento2 páginas002 - CPR Committeeshehab elsayedAinda não há avaliações
- DisorientedDocumento13 páginasDisorientedThurston3Ainda não há avaliações
- Staff Development Plan 2023Documento5 páginasStaff Development Plan 2023SSNHI Dialysis Training CenterAinda não há avaliações
- OpllDocumento10 páginasOpllTeofilus KristiantoAinda não há avaliações
- 13th & 14th WK - Oxygen Therapy With VideoDocumento89 páginas13th & 14th WK - Oxygen Therapy With VideoJesus Mario Lopez100% (1)
- Health CareerDocumento66 páginasHealth CareerDianne Joy MinaAinda não há avaliações
- Glycerol Suppositories Bp0001Documento2 páginasGlycerol Suppositories Bp0001FREDAinda não há avaliações
- Pre - & Suffix For HematologyDocumento2 páginasPre - & Suffix For HematologyFrieda Cayabyab0% (1)
- OxytocinDocumento1 páginaOxytocinSubbie OutlierAinda não há avaliações
- Assessment of ShoulderDocumento31 páginasAssessment of ShoulderNithin NairAinda não há avaliações