Escolar Documentos
Profissional Documentos
Cultura Documentos
N N N N N: ©2014 Uptodate
Enviado por
Dayron TorresTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
N N N N N: ©2014 Uptodate
Enviado por
Dayron TorresDireitos autorais:
Formatos disponíveis
Page 1 of 7
Below is a topic taken from UpToDate that I thought you might find interesting.
UpToDate is an online clinical decision support resource featuring over 10,000 clinical topics designed to give
immediate answers to clinical questions at the point of care. Visit us on the web at www.uptodate.com.
2014 UpToDate
Official Topic from UpToDate, the clinical decision support resource accessed by 700,000+ clinicians
worldwide. Available via the web and mobile devices, subscribe to UpToDate at www.uptodate.com/store.
Patient information: Ankylosing spondylitis and other spondyloarthritis (Beyond the Basics)
Author Section Editor Deputy Editor
David T Yu, MD Joachim Sieper, MD Jerry M Greene, MD
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Feb 2014. | This topic last updated: Jun 10, 2013.
ANKYLOSING SPONDYLITIS OVERVIEW Ankylosing spondylitis (AS) is a chronic inflammatory disease
that causes pain in the back, the neck, and, sometimes, the hips. The back is composed of multiple separate
bones known as vertebrae. Ankylosing means joining together and refers to an inflexibility between the
vertebrae. Spondylitis means inflammation of the vertebrae. Spondyloarthritis refers to a group of diseases
that share a tendency to cause spondylitis, some of which also cause inflammation of other joints besides
those of the spine.
This topic discusses the symptoms, diagnostic tests, possible complications, and treatment of one of the
family of spondyloarthritis diseases, ankylosing spondylitis. It also discusses some of the diseases that are
classified as subtypes of spondyloarthritis. Separate topic reviews are available that discuss some of the
medications used to treat ankylosing spondylitis and exercises that can help people with ankylosing spondylitis
with stretching and strengthening. (See "Patient information: Disease-modifying antirheumatic drugs
(DMARDs) (Beyond the Basics)" and "Patient information: Arthritis and exercise (Beyond the Basics)".)
SPONDYLOARTHRITIS FAMILY OF ARTHRITIS Spondyloarthritis is a family of arthritis, of which
ankylosing spondylitis is the most common member. The other members are:
n Undifferentiated spondyloarthritis
n Non-radiographic axial spondyloarthritis
n Reactive arthritis
n Arthritis associated with psoriasis (psoriatic arthritis)
n Arthritis associated with inflammatory bowel diseases (ulcerative colitis or Crohns disease)
Spondyloarthritis has also been classified into axial and peripheral spondyloarthritis according to whether
the involvement is mainly in the spine or in the extremities. Ankylosing spondylitis belongs to the axial class
of spondyloarthritis. Many patients diagnosed as having an axial form of undifferentiated spondyloarthritis
may subsequently develop ankylosing spondylitis. Separate topic reviews discuss reactive arthritis, psoriatic
arthritis, and inflammatory bowel diseases. (See "Patient information: Reactive arthritis (formerly Reiter
syndrome) (Beyond the Basics)" and "Patient information: Psoriatic arthritis (Beyond the Basics)" and "Patient
information: Ulcerative colitis (Beyond the Basics)" and "Patient information: Crohn disease (Beyond the
Basics)".)
ANKYLOSING SPONDYLITIS SYMPTOMS The most common symptom of ankylosing spondylitis is pain
in the lower back. Pain, stiffness, and limited mobility in other joints also occur in some patients. More
detailed information is available separately. (See "Clinical manifestations of ankylosing spondylitis in adults".)
Spinal pain Spinal pain, almost always in the lower back, is usually the first and most common symptom
of ankylosing spondylitis. Back pain that occurs with ankylosing spondylitis generally has some of the following
characteristics:
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 2 of 7
n Begins in early adulthood (before 45 years of age)
n Has gradual onset (rather than sudden onset after an acute injury)
n Lasts longer than three months
n Is worse after rest (for example, in the morning)
n Improves with activity
n Wakes you up in the second half of the night
n Can cause morning stiffness lasting more than 30 minutes
n Can cause buttock pain that alternates between the left and right side
Limited spinal mobility The flexibility of the back may be reduced. Putting on shoes and stockings may
become difficult due to a limited ability to bend forward.
Other symptoms
n Hip pain Arthritis of the hips is relatively common in ankylosing spondylitis, causing pain in the groin
or buttocks or difficulty walking.
n Shoulder pain Inflammation of the tendon and bone may cause shoulder pain and limited mobility of
the affected shoulder(s).
n Arthritis in other joints Pain, stiffness, and swelling of other joints may occur. A single joint
(monoarthritis) or a few joints (oligoarthritis) may be affected.
n Enthesitis An enthesis is a region in which a tendon or a ligament attaches to bone. Enthesitis
(inflammation of an enthesis) is a symptom of spondyloarthritis. In addition to the spine, a major area
of symptomatic enthesitis is at the heel.
n Constitutional features As with any chronic inflammatory disease, people with ankylosing spondylitis
may be tired and may feel unwell. Difficulty sleeping, caused by back or joint pain at night, may
contribute to fatigue. Low-grade fevers and weight loss occur in some patients.
n Other affected systems Body systems other than the joints can be affected. (See 'Ankylosing
spondylitis complications' below.)
ANKYLOSING SPONDYLITIS RISK FACTORS Ankylosing spondylitis is three times more common in
males than in females. It is usually diagnosed in young adults between the ages of 20 and 30 years.
The disease can be more common in certain families. For example, a person's risk of developing ankylosing
spondylitis increases if a first-degree relative (parent, sibling, or child) has ankylosing spondylitis. The
presence of a gene called HLA-B27 may also increase the risk of developing ankylosing spondylitis.
ANKYLOSING SPONDYLITIS DIAGNOSIS The diagnosis of ankylosing spondylitis is based upon a
combination of a patient's symptoms, physical examination, and imaging tests. (See "Diagnosis and
differential diagnosis of ankylosing spondylitis in adults".)
Imaging tests People with ankylosing spondylitis develop characteristic changes in the sacroiliac joints
(the joint that connects the base of the spine [sacrum] and large pelvic bone [ilium]). These changes can be
seen on x-ray images, although x-ray changes take time to develop and may not be apparent until years after
the onset of ankylosing spondylitis.
Imaging tests such as magnetic resonance imaging (MRI) are more sensitive than plain x-rays and may be
used if ankylosing spondylitis is suspected but is not clearly seen on x-ray.
Other tests There is no blood test that, by itself, is capable of definitively diagnosing or excluding
ankylosing spondylitis. However, testing for a particular type of gene, HLA-B27, can be helpful in selected
groups of patients. Ankylosing spondylitis is unlikely in a patient with a negative test for HLA-B27 who is white
and of European descent. Ankylosing spondylitis is even less likely if x-rays and MRI are normal or show no
changes to suggest ankylosis of the sacroiliac joint or inflammation in that area.
ANKYLOSING SPONDYLITIS COMPLICATIONS Complications of ankylosing spondylitis are uncommon,
with the exception of anterior uveitis.
Anterior uveitis Uveitis, or inflammation of part of the eye, is the most common ankylosing spondylitis-
related problem that does not involve joints. Uveitis causes pain in the eye, blurring of vision, and light
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 3 of 7
sensitivity. Uveitis requires immediate medical attention and treatment with eye medications but often
resolves within several months.
Spinal fractures and spinal cord injuries Spinal fractures and spinal cord injuries are 4 and 11 times
more common in patients with ankylosing spondylitis than in the general population. Most of the acute
fractures occur in the neck. The preceding injuries might be trivial and of low impact. Patients with spinal cord
injuries may have only minor initial neurological symptoms. Any neck or spine injury requires immobilization,
consultation with a doctor, and evaluation in an emergency facility. More than half of neck fractures in
patients with ankylosing spondylitis are undetectable by plain x-ray. Computed tomography and MRI are more
sensitive imaging techniques.
Neurologic problems Cauda equina syndrome is a rare complication that occurs in people with
longstanding disease who have severe stiffening of the spine. The symptoms result from damage to many
nerves in the lower back and include abnormal sensation, weakness, and difficulty with bladder and bowel
control. Men may experience erectile dysfunction or impotence.
Cardiovascular disease The most serious problem is a leaking aortic valve (aortic regurgitation) which
can cause symptoms of heart failure, including leg or ankle swelling (edema) and shortness of breath during
exercise or exertion. (See "Patient information: Heart failure (Beyond the Basics)".)
Pulmonary disease Many people with ankylosing spondylitis are unable to expand the chest normally
during breathing because of stiffness between the ribs and the spine. In some cases, changes in the lungs can
result. This may or may not cause breathing problems.
Ulcerations in the bowel Some people with ankylosing spondylitis will develop ulcerations in the lining of
the bowels, although these ulcerations do not usually cause any symptoms.
EFFECTS OF ANKYLOSING SPONDYLITIS ON DAILY LIFE Ankylosing spondylitis can affect daily life in
various ways. Dressing, reaching, rising from a chair, getting up from the floor, standing, climbing steps,
looking to the side or over the shoulder, exercising, and doing household or work-related tasks can become
more difficult as a result of the limited joint and spinal motion in ankylosing spondylitis. These limitations can
affect you and your family, and many people with ankylosing spondylitis will require assistance from family
and friends.
ANKYLOSING SPONDYLITIS TREATMENT Ankylosing spondylitis treatment is tailored for each
individual, based on the characteristics and severity of the disease. Treatment may include any of the
following (see "Assessment and treatment of ankylosing spondylitis in adults"):
Exercise Exercise should be part of the treatment program for everyone with ankylosing spondylitis. It can
include home exercises, individual or group exercise with a physical therapist, or physical therapy (PT)
treatments. Optimally, each patient should be evaluated and given instructions by a physical therapist. The
exercise should consist of posture training, deep breathing, back extension, and other stretching movements.
(See "Patient information: Arthritis and exercise (Beyond the Basics)".)
Information about exercises designed for people with ankylosing spondylitis is available on the following
website: www.nass.co.uk/exercise/.
Safety issues Because of the increased risk of serious spinal injury from slips and falls, people with
ankylosing spondylitis should take care to avoid such mishaps. Some simple measures include limiting the use
of alcohol. Pain relieving drugs (such as codeine and other narcotics) and sedatives (sleeping pills) should also
be used cautiously, if at all, since these also increase the risk of falling. Contact sports and other high-impact
activities should be avoided.
Shower or tub grab-bars and night-lights decrease the chance of a fall. Loose rugs increase the risk of tripping
and should be removed or carefully attached to the floor with removable adhesive strips or pads. Seat belts
reduce the risk of injury in a car crash and should be worn while driving or riding in a vehicle. A wrap-around
rear view mirror can improve visibility for drivers who cannot turn their head and neck.
To avoid developing deformities of the neck, a thin, rather than a thick, pillow is recommended for sleeping.
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 4 of 7
Medications
Nonsteroidal antiinflammatory drugs (NSAID) An NSAID is commonly used to control pain and
stiffness. NSAIDs need to be taken on a regular basis for several weeks before their maximum effect can be
judged. (See "Patient information: Nonsteroidal antiinflammatory drugs (NSAIDs) (Beyond the Basics)".)
Sulfasalazine Sulfasalazine is a disease modifying antirheumatic drug, or DMARD, that may be given to
slow or stop the progression of ankylosing spondylitis. It may be given along with NSAIDs. This drug provides
some relief of arthritis symptoms but is not helpful if ankylosing spondylitis only affects the spine. (See
"Patient information: Disease-modifying antirheumatic drugs (DMARDs) (Beyond the Basics)" and "Patient
information: Sulfasalazine and the 5-aminosalicylates (Beyond the Basics)".)
Anti-tumor necrosis factor therapy A group of medicines known as anti-tumor necrosis factor agents
(anti-TNF) or TNF inhibitors is often effective in the treatment of ankylosing spondylitis. Examples of anti-TNF
medications include infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab. People who do
not respond to one anti-TNF treatment may respond to another. Improvement in symptoms is common and
may occur within a few weeks of starting the drugs. However, these drugs may not be very effective in
stopping the progression of the disease.
n Who should use anti-TNF therapy? Not every patient with ankylosing spondylitis needs anti-TNF
therapy. In general, people with active disease in the spine who have not responded fully to NSAIDs
may be candidates. The decision to use anti-TNF therapy depends upon several factors that should be
discussed with your clinician.
Some clinicians may also recommend a glucocorticoid injection into particularly painful or swollen joints,
especially if there is only one or a two that are causing the most pain. (See 'Glucocorticoids (steroids)' below.)
Glucocorticoids (steroids) In some cases, a glucocorticoid injection into the sacroiliac joint may help
provide relief in patients who have sacroiliac pain that has not responded to other therapies.
In contrast, taking glucocorticoids by mouth is rarely necessary in ankylosing spondylitis treatment.
Surgery Hip or spine surgery may be beneficial in selected patients with ankylosing spondylitis. Surgical
procedures may include one or more of the following:
Total hip replacement Insertion of an artificial hip may be recommended in patients with ankylosing
spondylitis who have severe, persistent hip pain or severely limited mobility due to hip joint arthritis. (See
"Patient information: Total hip replacement (arthroplasty) (Beyond the Basics)".)
Spinal surgery Fusion of the bones in the cervical spine may be recommended for a small number of
patients who develop dislocation of these bones. Such surgery may help prevent spinal cord damage.
Wedge osteotomy Wedge osteotomy involves the removal of a wedge-shaped piece of bone from a
vertebra, followed by realignment of the spine. The spine is then braced and is allowed to heal in a better
position. This type of procedure may be recommended for people who develop severe deformities of the neck.
PREVENTING ANKYLOSING SPONDYLITIS COMPLICATIONS Because the severity and outcome of
ankylosing spondylitis vary considerably among patients, treatment must be tailored to each particular
patient. However, all patients can benefit from the following:
n Stop smoking cigarettes. People who smoke and have ankylosing spondylitis can have problems with
their breathing. Ankylosing spondylitis can limit the movement of the chest and can reduce the amount
of air the lungs can hold. (See "Patient information: Quitting smoking (Beyond the Basics)".)
n Maintain correct posture, and participate in an exercise program. (See "Patient information: Arthritis
and exercise (Beyond the Basics)".)
n Consume an adequate amount of calcium and vitamin D in order to reduce the risk of bone loss
(osteoporosis). Products that contain calcium and vitamin D include dairy products like milk, cheese,
and yogurt or non-prescription calcium and vitamin D supplements. (See "Patient information: Calcium
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 5 of 7
and vitamin D for bone health (Beyond the Basics)".)
Medications that treat bone loss may be recommended if you have already lost bone strength. (See "Patient
information: Bone density testing (Beyond the Basics)" and "Patient information: Osteoporosis prevention and
treatment (Beyond the Basics)".)
UNDIFFERENTIATED SPONDYLOARTHRITIS Someone who has spondyloarthritis but who does not have
sufficient features to be diagnosed as having ankylosing spondylitis, reactive arthritis, arthritis associated with
psoriasis, ulcerative colitis, or Crohns disease may be diagnosed as having undifferentiated spondyloarthritis.
The major involvement might be the spine, the extremities, or both. The approach by the doctors toward
diagnosis and treatment are similar to those of ankylosing spondylitis listed above. (See 'Ankylosing
spondylitis treatment' above.) If the symptoms are mostly in the spine, the clinician may diagnose it as non-
radiographic spondyloarthritis instead of undifferentiated spondyloarthritis.
If a diagnosis of undifferentiated spondyloarthritis or non-radiographic spondyloarthritis is made, additional
medical visits are necessary, because, with time, one of the more specific types of spondyloarthritis may be
diagnosed. However, some patients continue to have undifferentiated spondyloarthritis or non-radiographic
spondyloarthritis, and some go into remission and can stop taking medications for pain and stiffness.
AXIAL AND PERIPHERAL SPONDYLOARTHRITIS Spondyloarthritis is also classified into axial and
peripheral types. In patients with axial spondyloarthritis, the symptoms are mainly, but not exclusively,
related to the spine. In patients with peripheral spondyloarthritis, the symptoms are mainly, but not
exclusively, experienced in the extremities.
NON-RADIOGRAPHIC AXIAL SPONDYLOARTHRITIS Patients with non-radiographic axial
spondyloarthritis are very similar to those with ankylosing spondylitis except that the sacroiliac joints of the
pelvis are normal by x-ray. Some patients with non-radiographic axial spondyloarthritis do have MRI changes
of the sacroiliac joints.
WHERE TO GET MORE INFORMATION Your healthcare provider is the best source of information for
questions and concerns related to your medical problem.
This article will be updated as needed on our web site (www.uptodate.com/patients). Related topics for
patients, as well as selected articles written for healthcare professionals, are also available. Some of the most
relevant are listed below.
Patient level information UpToDate offers two types of patient education materials.
The Basics The Basics patient education pieces answer the four or five key questions a patient might have
about a given condition. These articles are best for patients who want a general overview and who prefer
short, easy-to-read materials.
Patient information: Ankylosing spondylitis (The Basics)
Patient information: Arthritis and exercise (The Basics)
Patient information: Reactive arthritis (Reiter syndrome) (The Basics)
Beyond the Basics Beyond the Basics patient education pieces are longer, more sophisticated, and more
detailed. These articles are best for patients who want in-depth information and are comfortable with some
medical jargon.
Patient information: Disease-modifying antirheumatic drugs (DMARDs) (Beyond the Basics)
Patient information: Arthritis and exercise (Beyond the Basics)
Patient information: Nonsteroidal antiinflammatory drugs (NSAIDs) (Beyond the Basics)
Patient information: Sulfasalazine and the 5-aminosalicylates (Beyond the Basics)
Patient information: Total hip replacement (arthroplasty) (Beyond the Basics)
Patient information: Quitting smoking (Beyond the Basics)
Patient information: Calcium and vitamin D for bone health (Beyond the Basics)
Patient information: Bone density testing (Beyond the Basics)
Patient information: Osteoporosis prevention and treatment (Beyond the Basics)
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 6 of 7
Professional level information Professional level articles are designed to keep doctors and other health
professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and
they contain multiple references to the research on which they are based. Professional level articles are best
for people who are comfortable with a lot of medical terminology and who want to read the same materials
their doctors are reading.
Clinical manifestations of ankylosing spondylitis in adults
Diagnosis and differential diagnosis of ankylosing spondylitis in adults
Diseases of the chest wall
General guidelines for use of anti-tumor necrosis factor alpha agents in ankylosing spondylitis and in
peripheral and non-radiographic axial spondyloarthritis
Pathogenesis of spondyloarthritis
Assessment and treatment of ankylosing spondylitis in adults
Non-radiographic axial spondyloarthritis, undifferentiated spondyloarthritis, and peripheral spondyloarthritis
The following organizations also provide reliable health information.
n National Library of Medicine
(www.nlm.nih.gov/medlineplus/healthtopics.html)
n Spondylitis Association of America
(www.spondylitis.org)
n Spondyloarthritis Research and Treatment Network
(www.spartangroup.org)
n National Institute of Arthritis and Musculoskeletal and Skin Diseases
(301) 496-8188
(http://www.niams.nih.gov/)
n American College of Rheumatology/Association of Rheumatology
(404) 633-3777
(www.rheumatology.org)
n The Arthritis Foundation
(800) 283-7800
(www.arthritis.org)
[1-8]
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
Dagfinrud H, Kvien TK, Hagen KB. The Cochrane review of physiotherapy interventions for ankylosing
1
spondylitis. J Rheumatol 2005; 32:1899.
Brophy S, Mackay K, Al-Saidi A, et al. The natural history of ankylosing spondylitis as defined by
2
radiological progression. J Rheumatol 2002; 29:1236.
Maugars Y, Mathis C, Berthelot JM, et al. Assessment of the efficacy of sacroiliac corticosteroid injections in
3
spondylarthropathies: a double-blind study. Br J Rheumatol 1996; 35:767.
Braun J, Pham T, Sieper J, et al. International ASAS consensus statement for the use of anti-tumour
4
necrosis factor agents in patients with ankylosing spondylitis. Ann Rheum Dis 2003; 62:817.
Mau W, Zeidler H, Mau R, et al. Clinical features and prognosis of patients with possible ankylosing
5
spondylitis. Results of a 10-year followup. J Rheumatol 1988; 15:1109.
Rudwaleit M, van der Heijde D, Landew R, et al. The development of Assessment of SpondyloArthritis
6 international Society classification criteria for axial spondyloarthritis (part II): validation and final selection.
Ann Rheum Dis 2009; 68:777.
Rudwaleit M, van der Heijde D, Landew R, et al. The Assessment of SpondyloArthritis International Society
7 classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis
2011; 70:25.
Sampaio-Barros PD, Bortoluzzo AB, Conde RA, et al. Undifferentiated spondyloarthritis: a longterm
8
followup. J Rheumatol 2010; 37:1195.
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Page 7 of 7
Topic 577 Version 13.0 All rights reserved. 2014 UpToDate, Inc.
UpToDate Customer Service
Wolters Kluwer Health
95 Sawyer Rd
Waltham, MA 02453-3471
1.800.998.6374 (US & Canada) tel.
+1.781.392.2000 (all other countries) tel.
customerservice@uptodate.com
www.uptodate.com
mhtml:file://C:\Users\Dayron\AppData\Local\Microsoft\Windows\Temporary Internet File... 20/3/2014
Você também pode gostar
- Ankylosing Spondylitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandAnkylosing Spondylitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Ankylosing Spondylitis Information BookletDocumento43 páginasAnkylosing Spondylitis Information BookletUmmu aiman50% (2)
- All About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsNo EverandAll About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsAinda não há avaliações
- What Is Ankylosing Spondylitis?: Sacroiliac JointsDocumento7 páginasWhat Is Ankylosing Spondylitis?: Sacroiliac JointsBharat VishwamitraAinda não há avaliações
- Osteoarthritis: Natural Drugless Treatments That Really Work!No EverandOsteoarthritis: Natural Drugless Treatments That Really Work!Ainda não há avaliações
- LBP 2Documento12 páginasLBP 2Attika DiniAinda não há avaliações
- A Guide to Back Pain: Symptoms; Causes; Treatment; PreventionNo EverandA Guide to Back Pain: Symptoms; Causes; Treatment; PreventionAinda não há avaliações
- Ankylosing Spondylarthritis PDFDocumento3 páginasAnkylosing Spondylarthritis PDFMa OlayaAinda não há avaliações
- Ankylosing LeafletfaDocumento2 páginasAnkylosing LeafletfaAaron NelsonAinda não há avaliações
- Ankylosing SpondilytisDocumento4 páginasAnkylosing Spondilytisandreas kevinAinda não há avaliações
- Ankylosing SpondylitisDocumento15 páginasAnkylosing Spondylitisevan872Ainda não há avaliações
- Untitled PresentationDocumento16 páginasUntitled PresentationtasneemsofiAinda não há avaliações
- Lec4 Ankylosing SpondylitisDocumento25 páginasLec4 Ankylosing Spondylitissana mumtazAinda não há avaliações
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocumento131 páginasApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathAinda não há avaliações
- Low BackacheDocumento23 páginasLow Backachemanoj ramlal kandoiAinda não há avaliações
- The Danger of AnkylosingDocumento4 páginasThe Danger of AnkylosingZeeshan IslamAinda não há avaliações
- Report SciDocumento25 páginasReport SciHershey Cordero BrionesAinda não há avaliações
- Hip Disorders: Symptoms of Hip ProblemsDocumento5 páginasHip Disorders: Symptoms of Hip ProblemsChethan K NarayanAinda não há avaliações
- Guidebook Guidebook: Answers and Practical Advice Answers and Practical AdviceDocumento34 páginasGuidebook Guidebook: Answers and Practical Advice Answers and Practical AdviceluckymaanAinda não há avaliações
- Ankylosing SpondylitisDocumento6 páginasAnkylosing SpondylitisAnonymous VzFhQ3iAinda não há avaliações
- SpondylolisthesisDocumento7 páginasSpondylolisthesisPutri WulandariAinda não há avaliações
- A Positive Response To Ankylosing Spondylitis: Guidebook For PatientsDocumento18 páginasA Positive Response To Ankylosing Spondylitis: Guidebook For PatientsdipanshuroyAinda não há avaliações
- LimpDocumento7 páginasLimpRakesh DudiAinda não há avaliações
- Pott Disease: Signs and SymptomsDocumento8 páginasPott Disease: Signs and SymptomsJason KurniawanAinda não há avaliações
- Low Back Pain OverviewDocumento3 páginasLow Back Pain OverviewEvans Oktora RolindriAinda não há avaliações
- Ankylosing Spondylitis: Submitted by Safeer Mohammed S 302 General Medicine Submitted To Dr. Marietta DavidianDocumento20 páginasAnkylosing Spondylitis: Submitted by Safeer Mohammed S 302 General Medicine Submitted To Dr. Marietta DavidianSafeer VarkalaAinda não há avaliações
- ArthritiscomplicationsDocumento2 páginasArthritiscomplicationsSai Krishna SeethamrajuAinda não há avaliações
- LBP EmedicineDocumento15 páginasLBP EmedicinenararyasriAinda não há avaliações
- Spinal Cord InjuryDocumento3 páginasSpinal Cord InjuryAdriane TomakinAinda não há avaliações
- Patient Education - Systemic Lupus Erythematosus (Beyond The Basics) - UpToDateDocumento14 páginasPatient Education - Systemic Lupus Erythematosus (Beyond The Basics) - UpToDatepakiza noorAinda não há avaliações
- Four Myths About Spondylitis: Clinician's GuideDocumento2 páginasFour Myths About Spondylitis: Clinician's GuideAmy YoungAinda não há avaliações
- S Pondy Lols Ys ThesisDocumento35 páginasS Pondy Lols Ys ThesisSal LieAinda não há avaliações
- Surgery - Orthopedic Surgery and NeurosurgeryDocumento88 páginasSurgery - Orthopedic Surgery and Neurosurgeryteena6506763Ainda não há avaliações
- Ortho 26 Exam QuestionsDocumento9 páginasOrtho 26 Exam Questionsmehmi123100% (6)
- DefinitionDocumento12 páginasDefinitionwirdha100% (1)
- Low Back Pain: Respectfully Submitted By: Princess Edelweiss M. Corpuz Wendy Pearn F. Castañeda Andre Kaien S. CorpuzDocumento14 páginasLow Back Pain: Respectfully Submitted By: Princess Edelweiss M. Corpuz Wendy Pearn F. Castañeda Andre Kaien S. CorpuzJusthine Mhay BalanceAinda não há avaliações
- Low BackDocumento7 páginasLow BackMuhammad FahmyAinda não há avaliações
- Low Back Pain 20-ns-5161 March 2020 508cDocumento24 páginasLow Back Pain 20-ns-5161 March 2020 508cRajib ChowdhuryAinda não há avaliações
- Ankylosing SpondylitisDocumento34 páginasAnkylosing SpondylitisLau100% (2)
- Unit5 Handicap ModuleDocumento14 páginasUnit5 Handicap Moduleted deangAinda não há avaliações
- Ankilosig SpondilithisDocumento5 páginasAnkilosig SpondilithisFrancois Donatien De SadeAinda não há avaliações
- c2Documento37 páginasc2LuisAngelPonceTorresAinda não há avaliações
- Ankylosing Spondylitis: Submitted By: Jamae Baldueza Sunshine Bisda Fritzie Mae CoruñaDocumento20 páginasAnkylosing Spondylitis: Submitted By: Jamae Baldueza Sunshine Bisda Fritzie Mae CoruñaJayvee Novenario CasaljayAinda não há avaliações
- Bamboo SpineDocumento1 páginaBamboo Spinecitihomes2009Ainda não há avaliações
- Locomotor ImpairmentDocumento11 páginasLocomotor ImpairmentAbhishek BiswalAinda não há avaliações
- Soul Free - Spinal Cord Injury Knowledge Packet 29. 09. 2013Documento6 páginasSoul Free - Spinal Cord Injury Knowledge Packet 29. 09. 2013Maddala NagendrakumarAinda não há avaliações
- Jawahar Navodaya Vidyalaya Kagal KolhapurDocumento27 páginasJawahar Navodaya Vidyalaya Kagal KolhapurSujay NirmaleAinda não há avaliações
- Nursing Care For Patients Undergoing Total Hip Arthroplasty: December 2018Documento13 páginasNursing Care For Patients Undergoing Total Hip Arthroplasty: December 2018Stella GašparušAinda não há avaliações
- 4yo Refusing To WalkDocumento7 páginas4yo Refusing To WalkdakewtwontonAinda não há avaliações
- Patient - Info/doctor/ankylosing Spondylitis ProDocumento8 páginasPatient - Info/doctor/ankylosing Spondylitis ProJasleen KaurAinda não há avaliações
- 11 FinalDocumento3 páginas11 Finalrehan.rpoAinda não há avaliações
- Final - Spinal Stenosis L4, L5 Secondary To Spondylolisthesis L4, L5 Grade II With Hypertrophized Ligament Um and Radiculopathy With Myelopathy Right SidedDocumento66 páginasFinal - Spinal Stenosis L4, L5 Secondary To Spondylolisthesis L4, L5 Grade II With Hypertrophized Ligament Um and Radiculopathy With Myelopathy Right SidedJai - Ho100% (1)
- Rachialgia - Written ReportDocumento4 páginasRachialgia - Written ReportNathaly MoraAinda não há avaliações
- Musculoskeletal Disorders YvonneDocumento7 páginasMusculoskeletal Disorders Yvonnerommel lunaAinda não há avaliações
- Cervical Spondylosis 2Documento32 páginasCervical Spondylosis 2Zuha HundalAinda não há avaliações
- Ankylosing SpondylitisDocumento29 páginasAnkylosing SpondylitisKrisna ajiAinda não há avaliações
- Case Study On Spondylosis: DefinitionDocumento6 páginasCase Study On Spondylosis: Definitionsai vasavi bandaruAinda não há avaliações
- Types of Spine Curvature DisordersDocumento7 páginasTypes of Spine Curvature DisordersNicu MacariAinda não há avaliações
- I. Definition of Disease: Start in The Teens and 20sDocumento4 páginasI. Definition of Disease: Start in The Teens and 20sAriaAinda não há avaliações
- NR 509 Midterm PPDocumento76 páginasNR 509 Midterm PPLou EscobarAinda não há avaliações
- Catalyst 4948E Netflow-Lite: © 2010 Cisco And/Or Its Affiliates. All Rights Reserved. 1Documento23 páginasCatalyst 4948E Netflow-Lite: © 2010 Cisco And/Or Its Affiliates. All Rights Reserved. 1Dayron TorresAinda não há avaliações
- ReferencesDocumento4 páginasReferencesDayron TorresAinda não há avaliações
- Current Service Catalogue TemplateDocumento9 páginasCurrent Service Catalogue TemplateDayron TorresAinda não há avaliações
- NeedsDocumento1 páginaNeedsDayron TorresAinda não há avaliações
- PwrData - 2017 12 13 18 53 33Documento605 páginasPwrData - 2017 12 13 18 53 33Dayron TorresAinda não há avaliações
- Weekly World of Music, Rock and Roll: Sample Music Cue SheetDocumento23 páginasWeekly World of Music, Rock and Roll: Sample Music Cue SheetDayron TorresAinda não há avaliações
- 2015 PDFDocumento1 página2015 PDFDayron TorresAinda não há avaliações
- ExamPricingChange PDFDocumento2 páginasExamPricingChange PDFDayron TorresAinda não há avaliações
- Magia Pensar GrandeDocumento16 páginasMagia Pensar GrandeDayron TorresAinda não há avaliações
- Macs Not in InventoryDocumento1 páginaMacs Not in InventoryDayron TorresAinda não há avaliações
- Ogunda MeyiDocumento5 páginasOgunda MeyiDayron TorresAinda não há avaliações
- Letter of Financial SupportDocumento1 páginaLetter of Financial SupportDayron TorresAinda não há avaliações
- ICND1 100-101: Al - HTMLDocumento3 páginasICND1 100-101: Al - HTMLDayron TorresAinda não há avaliações
- HumansDocumento1 páginaHumansDayron TorresAinda não há avaliações
- LXBR Circuit Breaker/Relays and Circuit Breakers For LXBC PanelsDocumento2 páginasLXBR Circuit Breaker/Relays and Circuit Breakers For LXBC PanelsDayron TorresAinda não há avaliações
- Pulmonary EdemaDocumento10 páginasPulmonary EdemaNader Smadi100% (6)
- Session #2 SAS - Funda (Lec)Documento8 páginasSession #2 SAS - Funda (Lec)Mary Maxiluch TabudlongAinda não há avaliações
- Med ClaimDocumento4 páginasMed ClaimDevesh Pratap SinghAinda não há avaliações
- RIZAL SummaryDocumento5 páginasRIZAL Summarydianara trinidadAinda não há avaliações
- Pedia Notes PrintDocumento6 páginasPedia Notes PrintDre Valdez100% (5)
- Bioethics Unit IiiDocumento4 páginasBioethics Unit IiiShannel J. DabalosAinda não há avaliações
- Cardiac Tamponade 2Documento23 páginasCardiac Tamponade 2Jethro Floyd QuintoAinda não há avaliações
- Kavita Priya Labetalol in Pih - IDocumento58 páginasKavita Priya Labetalol in Pih - IKavita PriyaAinda não há avaliações
- Cardiovascular Physiology Case 9Documento50 páginasCardiovascular Physiology Case 9Kim AcostaAinda não há avaliações
- GIT5Documento78 páginasGIT5justiceboakyeAinda não há avaliações
- Comorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFDocumento24 páginasComorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreaming0% (1)
- NRC - Skill Competency Checklist - PainAsessmentOlderAdults - SkillChecklistDocumento2 páginasNRC - Skill Competency Checklist - PainAsessmentOlderAdults - SkillChecklist紅玉練Ainda não há avaliações
- Euros Core OrgDocumento6 páginasEuros Core OrgClaudio Walter VidelaAinda não há avaliações
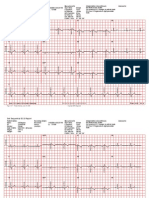
- Universal ECG Sample ReportsDocumento6 páginasUniversal ECG Sample ReportsHemant Soni100% (1)
- Quality of Life in Pediatric Patients After ProvidingDocumento5 páginasQuality of Life in Pediatric Patients After ProvidingrindaAinda não há avaliações
- Seinfeld Syncope'': To The EditorDocumento1 páginaSeinfeld Syncope'': To The EditorJason ChambersAinda não há avaliações
- Meningitis-Malaria E PDFDocumento44 páginasMeningitis-Malaria E PDFSana ShafeeqAinda não há avaliações
- Urinary CathetersDocumento5 páginasUrinary CathetersJyoti Pariyar100% (1)
- Mental Health LawDocumento8 páginasMental Health LawAnnAinda não há avaliações
- Article PDF Neeraj Madan Nidhi Kathuria 49Documento3 páginasArticle PDF Neeraj Madan Nidhi Kathuria 49evieramawati_4536812Ainda não há avaliações
- Neuroanatomy Textbook ComparisonDocumento2 páginasNeuroanatomy Textbook ComparisonSuiweng Wong100% (1)
- Mid Trimester InductionDocumento6 páginasMid Trimester InductionYwagar YwagarAinda não há avaliações
- Apollo Hospitals - Presentation (ETOP)Documento24 páginasApollo Hospitals - Presentation (ETOP)p_sonera0% (1)
- Journal NCM 118 (Lec) Nicolas, Sherena Q. BSN IV-1Documento15 páginasJournal NCM 118 (Lec) Nicolas, Sherena Q. BSN IV-1Sherena NicolasAinda não há avaliações
- Neurological Physiotherapy AssessmentDocumento7 páginasNeurological Physiotherapy Assessmentramesh babuAinda não há avaliações
- BloodbasicsnoteguideDocumento2 páginasBloodbasicsnoteguideapi-292042538Ainda não há avaliações
- Charcot JointDocumento8 páginasCharcot JointAtika SugiartoAinda não há avaliações
- Applications of Tomotherapy PDFDocumento4 páginasApplications of Tomotherapy PDFMalu Paras LacsonAinda não há avaliações
- Myocardial BridgingDocumento13 páginasMyocardial BridgingAsik AliAinda não há avaliações
- Thymatron 4Documento8 páginasThymatron 4srinivasanaAinda não há avaliações
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 4.5 de 5 estrelas4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4.5 de 5 estrelas4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceNo EverandTo Explain the World: The Discovery of Modern ScienceNota: 3.5 de 5 estrelas3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsNo EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsNota: 4.5 de 5 estrelas4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingNo EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingNota: 4 de 5 estrelas4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)