Escolar Documentos
Profissional Documentos
Cultura Documentos
15 CR Autoimmune Hemolysis in Malaria
Enviado por
Ria Septi HarmiaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
15 CR Autoimmune Hemolysis in Malaria
Enviado por
Ria Septi HarmiaDireitos autorais:
Formatos disponíveis
© JAPI • february 2012 • VOL.
60 51
Case Report
Autoimmune Hemolysis in Malaria: A Report of Three
Cases
Vishnu Sharma1, Rohini Samant2, Ashit Hegde3, Khushrav Bhaja3
Abstract
We have recently treated three patients with malaria who developed post malaria immune mediated hemolysis.
These cases, seen with in a span of three month period (September 09 to November 09) form the basis of this
report. Out of three patients, two were treated with steroids and both responded favorably.
Introduction Case 2
M alaria continues to be an important disease in humans.
Its clinical manifestations are due to (a) invasion and
destruction of RBCs by the parasite and (b) host reaction to
A 7 year old girl developed high grade, intermittent fever
with chills in the first week of September 09. Peripheral smear
showed both P. vivax and P. falciparum malarial parasite (MP).
the malarial parasite infection. Anemia, the most common She was admitted to another facility. On admission her Hb was
complication, is due to accelerated RBC removal by the spleen, 11.1g/dl, platelet count was 50,000/mm3 and bilirubin was 5.2
obligatory RBC destruction at parasite schizogony, and mg/dl (direct 4.0mg/dl, indirect 1.2 mg/dl). She was treated with
ineffective erythropoiesis. However the extent of hemolysis intravenous artesunate 2.4mg/kg/day for 5 days followed by
in malaria is much greater than encountered in other parasite mefloquine 15mg/kg. She also received injectable ceftriaxone
induced hemolytic states. An associated or added immune 1g IV OD and quinine 10mg/kg tid PO for 4 days. The fever
mediated hemolysis has been postulated. We describe here three improved on the 3rd day of treatment. A repeat peripheral smear
cases that developed post malaria immune mediated hemolysis. was negative. Fever recurred on 7th day of admission and the
Hb dropped to 5.1gm/dl. She received 2 units of PRBCs and
Case 1 transferred to our hospital. On admission at our Hospital she
A 15 year old girl was admitted at our hospital with the history was febrile (temp 102F), pale; Hb was 9.0g/dl, bilirubin was
of high grade intermittent fevers for 4 days. Her peripheral 1.7mg/dl and peripheral smear was negative for MP. Rapid
smear was positive for both P. vivax and P. falciparum malarial malaria antigen test was negative. Urine examination showed
parasites. On admission her Hb was 9.1g/dl; the platelet count reddish colour with urobilinogen +++, 12 wbcs and 15 rbc/
was 24,000/mm3. She was treated with intravenous artesunate hpf. Fever continued, and Hb dropped to 4.9g/dl on the 13th day
120 mg/day for 5days .The fever responded but recurred on the of her illness. She received 1 unit of PRBC under steroid cover.
4th day. A repeat peripheral smear for malarial parasites and the Other investigations showed reticulocyte count 7.18%, plasma
rapid malaria antigen test were negative. Ceftriaxone 1gm IV Hb 270mg/dl(N=1-40), LDH 670U/L, ANA 1:100 +++ speckled
bd and doxycycline 100mg/bd PO were added to the treatment pattern, P-ANCA 1+, cold agglutinins 1:16 positive, APLA IgG
but the fever persisted. On the 9th day, the Hb dropped to 4.8g/ and IgM 16 and 14 U/ml (N< 10 U/ml), G-6PD was normal. She
dl; the reticulocyte count was 1.88%, LDH was 481U/L (N = became afebrile on 20th day of her illness and started passing clear
4-240), plasma Hb was 273 mg/L (N=1-40) and Coombs’ test was colored urine. She was discharged on the12th day of admission.
negative. She was given 2 units of packed RBC’s; Hb improved On follow up after 4 weeks she was better, off treatment and the
to 6.3 g/dl. The fever continued. Hb again dropped to 3.5g/dl Hb was 10.1gm/dl.
on the 13th day. In view of continued fever and two episodes
suggestive of hemolysis, she was treated with prednisolone Case 3
1mg/kg/day and further investigated. APLA IgG and IgM tests A 15 year old female suffered from fever with chills in the
were strongly positive, ANA was negative, G-6PD value was second week of November’ 09 and was admitted in another
normal and cold agglutinins were elevated at 1:1280. Her fever facility. Her peripheral smear was positive for P. falciparum,
improved and Hb rose to 6gm/dl. On follow up after 4 weeks Hb was 11.1g/dl and the platelet count was 1.60lacs/mm3. Her
she was better; Hb was 8.2g/dl. Prednisolone was tapered over platelets dropped to 25000/mm3 in 4 days and she developed
6 weeks and stopped. icterus and was transferred to Hinduja Hospital on the 4th day.
On admission, her Hb was 8.7g/dl, platelet count was 3000/mm3,
S. bilirubin 21.8mg/dl (direct 15.2 mg/dl, indirect 6.6 mg/dl),
albumin 1.6 gm/dl. She was started on IV artesunate 120mg/day,
ceftriaxone 2g/day and was treated with platelet transfusions
1
Registrar, 2Consultant Rheumatologist, Department of
(6 RDPs). The platelet count improved gradually, S. bilirubin
Rheumatology, 3Consultant Physician, Department of
decreased to 6 mg/dl within a week, but the fever continued and
Internal Medicine, PD Hinduja National Hospital and
Hb dropped gradually to 4.5 mg/dl by the 11th day. Repeated
Medical Research Centre, Veer Savarkar Marg, Mahim,
peripheral smears were negative for MP, rapid malaria test was
Mumbai – 400016
negative, G6 PD was normal, reticulocyte count was 0.28%, LDH
Received: 15.07.2010; Accepted: 17.09.2011 458 (N=135-214), Haptoglobin 5.83 g/dl (13-163), plasma Hb 442
© JAPI • february 2012 • VOL. 60 129
52 © JAPI • february 2012 • VOL. 60
mg/l (N=1-40), Coombs’ test and ANA were negative, APLA IgG, Besides anti-erythrocyte Ab, other autoantibodies have
IgM were mild positive. The cold agglutinins titres were 1:16. also been observed during the course of malaria. Important
She was started on prednisolone 0.5 mg/kg body weight. The among these are ANA, APLA and occasionally ANCA. Anti
fever improved and Hb stablilised. She was discharged on 15th phospholipid antibodies were strongly positive in two and
day of admission with no fever and Hb 7.3 g/dl. On follow up weakly positive in one patient. Benign antiphosphopholipid
after 2 months her Hb was 12.1 g/dl and prednisolone had been antibodies are known to develop in malaria, but whether these
tapered down to 5 mg/day, it was discontinued. contribute to hemolysis is not known. Cryoglobulin titers were
high in all the three patients, with very high titers in one patient.
Discussion High cryoglobulin titres have been reported in patients with
Anemia is frequently associated with malaria; its rate of malaria, especially with falciparum malaria, however their role
occurrence depends on age of the patient and endemicity. in hemolysis in malaria is not known.
Anemia is caused by a variety of pathophysiologic mechanisms There have been two single case reports of association of
which include hemolysis, reduced red cell deformation of malaria and autoimmune hemolysis, one was from Korea
parasitized and non-parasitized erythrocytes, increased splenic and other from Canada.6,2 In India, prevalence of malaria is
clearance, variable degree of bone marrow dyserythropoiesis very high, but there have been no similar cases reported from
and cytokine dysregulation (significant increase in IFN gamma, India. It could be due to rarity of this phenomenon or due to
IL-6, TNF-alpha, IL-1, MIF, HIF-1 and decrease in IL-10 and underreporting. The autoimmune hemolysis seems to be short
IL-12 levels).5 In areas where malarial infection is endemic, lived or self limiting as two of our patients responded very well
co-morbidities like other parasitic infections, iron, folate and to steroids which were stopped gradually in 6 weeks. After
Vitamin B12 deficiency, deficiency of other nutrients and effects discontinuing steroids patients did not have drop in Hb and
of anti- malarial drugs both through immune and non-immune remained asymptomatic. The purpose of this communication
mechanisms are important considerations.5 However extent of is to emphasize that autoimmune hemolysis should be thought
hemolysis in malaria is much greater than that seen in other of if a patient with malaria develops post treatment hemolysis
parasite induced hemolysis and combined mechanism with or persistent anemia.
immune mediated hemolysis has been suggested.1
All the three patients being reported had sudden and Acknowledgments
significant drop in Hb levels between 7th to 14th day of illness We are grateful to Prof. V.R. Joshi, MD, Consultant
necessitating PRBC transfusion. Peripheral smears were negative Rheumatologist and Director, Research, for his critical review
for MP and rapid malaria test was negative at the time of drop in of manuscript and Dr. Nagaraj S, DNB(Paed), PG Registrar,
Hb. All had high plasma Hb levels with raised LDH levels. But the Department of Rheumatology, PD Hinduja National Hospital
reticulocyte count was increased in only one patient, and direct and MRC, for help in the preparation of manuscript.
Coombs’ test was positive in only one patient. The hemolytic
episodes cannot be explained by malarial parasitemia alone and Refrences
would fit in with autoimmune hemolysis. Moreover two patients
1. Dhaliwal G, Cornett PA, Tierney LM jr.: Hemolytic anemia. Am
had persistent high fever after clearance of parasitemia and both Fam Physician 1979;69:2599-606.
fever and anemia responded to corticosteroid treatment.
2. Drouin J, Rock G, Jolly E. Plasmodium falciparum malaria
A proportion of patients suffering from malaria develop mimicking autoimmune hemolytic anemia during pregnancy. Can
immune hemolysis.2 The reasons for immune hemolysis are Med Assoc J 1985;132
multifactorial e.g. antibodies directed to parasite antigens 3. Turrini F, Gribaldi G, Carta F, Mannu F, Arse P. Mechanism of
sticking to red cells, immune complex deposition leading to band-3 oxidation and clustering in the phagocytosis of Plasmodium
bystander hemolysis due to parasite antigen or drug antibody falciparum-infected erythrocytes. Rodex Report 2003;8:300-303.
complex, or due to oxidative damage and aggregation of 4. Stouti JA, Odindo AO, Owuor BO, Mibei EK, Opollo Mo, Waitumbi
red cell anion channel protein, subsequent coating of this Jn. Loss of red blood cell complement regulatory proteins and
denatured protein by naturally occurring autoantibody susceptibility to severe malarial anemia. J Infect Dis 2003;187:522-
followed by their removal by reticuloendothelial system3. In 525.
addition, increased levels of cytokines including TNF-alpha 5. Ghosh K, Ghosh K. Pathogenesis of anemia in malaria: a concise
can activate macrophages which, in a hyperactive stage, may review. Parasit Res 2007;101:1463-1469.
reduce their threshold for amount of antibody coating needed 6. Lee S W, Lee S E Chung B H, Hwang T J, Shin H S. A case of
for phagocytosis. Also, anticomplementary defense of red cell Plasmodium vivax malaria associated with autoimmune hemolytic
membrane, which protects rbcs’ from inadvertent complement anemia. Infect Chemother 2008;40:63-66.
mediated lysis, is reduced in malarial infection due to loss of
complement regulatory proteins CD-55 and CD-59. This coupled
with increased levels of immune complexes in malarial infection
makes rbcs susceptible to complement mediated lysis.4
130 © JAPI • february 2012 • VOL. 60
Você também pode gostar
- 2761 8144 1 SMDocumento6 páginas2761 8144 1 SMAnnisa apriliaAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderAinda não há avaliações
- 1768 PDFDocumento2 páginas1768 PDFAndhiky Raymonanda MadangsaiAinda não há avaliações
- Case Report 2 - 2015Documento3 páginasCase Report 2 - 2015Nguyen Trong PhuocAinda não há avaliações
- Hyper-Reactive Malarial Splenomegaly: Rare Cause of Pyrexia of Unknown OriginDocumento3 páginasHyper-Reactive Malarial Splenomegaly: Rare Cause of Pyrexia of Unknown OriginAshvanee sharmaAinda não há avaliações
- Case Report MalariaDocumento3 páginasCase Report MalarialilisAinda não há avaliações
- Prolonged Cholestasis Due To Hepatitis A Virus Infection in A Young Adolescent Male With A Known Case of Hemoglobin E Disease: Early Response To Steroid TherapyDocumento4 páginasProlonged Cholestasis Due To Hepatitis A Virus Infection in A Young Adolescent Male With A Known Case of Hemoglobin E Disease: Early Response To Steroid TherapyBOHR International Journal on GastroenterologyAinda não há avaliações
- Jak 2 Negative Polycythemia Vera in A Tertiary Care Center in West Up Population in India :a Rare Presentation of 5 CasesDocumento5 páginasJak 2 Negative Polycythemia Vera in A Tertiary Care Center in West Up Population in India :a Rare Presentation of 5 CasesIJAR JOURNALAinda não há avaliações
- Paediatrica Indonesiana: Case ReportDocumento5 páginasPaediatrica Indonesiana: Case Reportsarliance letteAinda não há avaliações
- JIC Abstract - SLE and EvansDocumento1 páginaJIC Abstract - SLE and EvansTirth ViraniAinda não há avaliações
- Case Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDocumento4 páginasCase Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDhruva PatelAinda não há avaliações
- Typhoid Fever and Viral Hepatitis in A g6pd DeficientDocumento2 páginasTyphoid Fever and Viral Hepatitis in A g6pd DeficientLoy GarikAinda não há avaliações
- Dengue CKDDocumento5 páginasDengue CKDbamhoi07Ainda não há avaliações
- Case Report: Hyperhemolysis Syndrome Without Underlying Hematologic DiseaseDocumento4 páginasCase Report: Hyperhemolysis Syndrome Without Underlying Hematologic DiseaseEliana LopezAinda não há avaliações
- Northrop 2015Documento4 páginasNorthrop 2015Annisa Badriyyah HakimahAinda não há avaliações
- Fulltext - Hematology v3 Id1118Documento3 páginasFulltext - Hematology v3 Id1118Thành Nguyễn VănAinda não há avaliações
- Tuberculosis: in Patients With ErythematosusDocumento4 páginasTuberculosis: in Patients With ErythematosusHarsha CAinda não há avaliações
- Malaria Case Studies Only - EnglishDocumento11 páginasMalaria Case Studies Only - EnglishFeik Emelje100% (1)
- Dengue Hemorrhagic Fever With Disseminated Intravascular CoagulationDocumento2 páginasDengue Hemorrhagic Fever With Disseminated Intravascular CoagulationPutriPasaribuAinda não há avaliações
- Dengue Pedia CaseDocumento10 páginasDengue Pedia CaseSam Raven AndresAinda não há avaliações
- Successful Management of Severe Chronic Autoimmune Hemolytic Anemia With Low Dose Cyclosporine and Prednisone in An InfantDocumento4 páginasSuccessful Management of Severe Chronic Autoimmune Hemolytic Anemia With Low Dose Cyclosporine and Prednisone in An InfantFatimatuzzahra ShahabAinda não há avaliações
- Fatal Hemolytic Anemia Associated With Metformin: A Case ReportDocumento13 páginasFatal Hemolytic Anemia Associated With Metformin: A Case ReportChairunisa AmiriaAinda não há avaliações
- Secondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportDocumento5 páginasSecondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportivanAinda não há avaliações
- 2016 Visceral Leishmaniasis Turning Into CLDDocumento4 páginas2016 Visceral Leishmaniasis Turning Into CLDPratyay HasanAinda não há avaliações
- Autoimmune Hemolytic Anemia Warm-Antibody Type (Warm AIHA) in An 8-Year-Old Balinese GirlDocumento5 páginasAutoimmune Hemolytic Anemia Warm-Antibody Type (Warm AIHA) in An 8-Year-Old Balinese GirlFatimatuzzahra ShahabAinda não há avaliações
- Clinical Nephrology and Renal Care: ClinmedDocumento3 páginasClinical Nephrology and Renal Care: ClinmedChandan VishwakarmaAinda não há avaliações
- MalariaDocumento9 páginasMalariaDANIELLE GRACE SABERONAinda não há avaliações
- Wasp StingDocumento3 páginasWasp StingShruthi KyAinda não há avaliações
- Ejm 04900 Case - Report CetinDocumento3 páginasEjm 04900 Case - Report CetinShwan OmarAinda não há avaliações
- Dengue Fever With Hepatitis E and Hepatitis A Infection PDFDocumento2 páginasDengue Fever With Hepatitis E and Hepatitis A Infection PDFAMENDBEAinda não há avaliações
- PDF TJP 1945Documento5 páginasPDF TJP 1945Karelau KarniaAinda não há avaliações
- Hemolysis Following Platelet Transfusions From ABO-incompatible DonorsDocumento3 páginasHemolysis Following Platelet Transfusions From ABO-incompatible Donorsmy accountAinda não há avaliações
- Disseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractDocumento3 páginasDisseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractAmelia Fitria DewiAinda não há avaliações
- Case 2Documento3 páginasCase 2Vivi DeviyanaAinda não há avaliações
- Amoxicillin and Ceftriaxone As Treatment Alternatives To Penicillin For Maternal Syphilis 2017Documento3 páginasAmoxicillin and Ceftriaxone As Treatment Alternatives To Penicillin For Maternal Syphilis 2017Jose Luis Morales BautistaAinda não há avaliações
- Crigler Najjar Syndrome Type 2 (CNS Type 2) : An Unwonted Cause of Jaundice in AdultsDocumento2 páginasCrigler Najjar Syndrome Type 2 (CNS Type 2) : An Unwonted Cause of Jaundice in AdultsIsaacAinda não há avaliações
- Case Study For Colon CancerDocumento2 páginasCase Study For Colon Cancerrhimineecat7150% (2)
- Clinical Management COVID 19 Mild Mod Severe - RecordOfAchievement 1Documento4 páginasClinical Management COVID 19 Mild Mod Severe - RecordOfAchievement 1chandanAinda não há avaliações
- Falciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesDocumento3 páginasFalciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesMuhammad Taufik AdhyatmaAinda não há avaliações
- Clinical Case StudyDocumento4 páginasClinical Case StudyNoor MahmoudAinda não há avaliações
- Typhoid Hepatitis: KhoslaDocumento3 páginasTyphoid Hepatitis: Khoslakevin ivandiAinda não há avaliações
- Antiphospholipid Syndrome in Pediatrics. Rheum Dis Clin N Am 33. 2007Documento25 páginasAntiphospholipid Syndrome in Pediatrics. Rheum Dis Clin N Am 33. 2007sprnv2Ainda não há avaliações
- Case Study CyanosisDocumento3 páginasCase Study CyanosishatomiAinda não há avaliações
- Chong 2018Documento2 páginasChong 2018keisy MarquezAinda não há avaliações
- Prof - Samuel Aazir CaseDocumento2 páginasProf - Samuel Aazir Caseأحمد فياضAinda não há avaliações
- Case Report - TOCILIZUMAB IN CKDDocumento5 páginasCase Report - TOCILIZUMAB IN CKDDenisa Carmen ColiofAinda não há avaliações
- 46 Singh EtalDocumento3 páginas46 Singh EtaleditorijmrhsAinda não há avaliações
- Edisi 2 Artcl 6Documento4 páginasEdisi 2 Artcl 6jackbayAinda não há avaliações
- A Case of Typhoid Fever Presenting With Multiple ComplicationsDocumento4 páginasA Case of Typhoid Fever Presenting With Multiple ComplicationsCleo CaminadeAinda não há avaliações
- Guillain Barr Syndrome Occurring Synchronously With Systemic Lupus Erythematosus As Initial Manifestation Treated Successfully With Low DoseDocumento5 páginasGuillain Barr Syndrome Occurring Synchronously With Systemic Lupus Erythematosus As Initial Manifestation Treated Successfully With Low DoseTessa CruzAinda não há avaliações
- Case Report: 17-Year-Old Boy With Renal Failure and The Highest Reported Creatinine in Pediatric LiteratureDocumento5 páginasCase Report: 17-Year-Old Boy With Renal Failure and The Highest Reported Creatinine in Pediatric LiteratureYunika ArumAinda não há avaliações
- In Deep: Cerebral Toxoplasmosis: Diagnostic DilemmaDocumento3 páginasIn Deep: Cerebral Toxoplasmosis: Diagnostic DilemmaYukii Triby-a AnniimesztAinda não há avaliações
- IgA NephropathyDocumento6 páginasIgA NephropathySyed AlmaazAinda não há avaliações
- Acute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseDocumento4 páginasAcute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseMuhFarizaAudiAinda não há avaliações
- 2019 - Article - 2130 - Fulminant Type 1 Diabetes Mellitus Associated With Coxsackievirus Type B1 Infection During PregnancyDocumento4 páginas2019 - Article - 2130 - Fulminant Type 1 Diabetes Mellitus Associated With Coxsackievirus Type B1 Infection During PregnancyRahmaAinda não há avaliações
- tmp61DD TMPDocumento7 páginastmp61DD TMPFrontiersAinda não há avaliações
- Aripiprazole HypoglycemiaDocumento4 páginasAripiprazole HypoglycemiarinkuAinda não há avaliações
- Fatal Metformin Overdose Presenting With Progressive HyperglycemiaDocumento5 páginasFatal Metformin Overdose Presenting With Progressive HyperglycemiaW Antonio Rivera MartínezAinda não há avaliações
- DHF Central Artery OclusionDocumento2 páginasDHF Central Artery OclusionRia Septi HarmiaAinda não há avaliações
- Pencegahan TBC Aids Di AsiaDocumento4 páginasPencegahan TBC Aids Di AsiaRia Septi HarmiaAinda não há avaliações
- Aki and MalariaDocumento4 páginasAki and MalariaRia Septi HarmiaAinda não há avaliações
- Malaria and StrokeDocumento3 páginasMalaria and StrokeRia Septi HarmiaAinda não há avaliações
- Case Report: Fatal Staphylococcal Infection Following Classic Dengue FeverDocumento4 páginasCase Report: Fatal Staphylococcal Infection Following Classic Dengue FeverRia Septi HarmiaAinda não há avaliações
- Animales en Peligro de Extinción en InglesDocumento7 páginasAnimales en Peligro de Extinción en InglesDarl GarcíaAinda não há avaliações
- Grade 6 Science Document 1Documento8 páginasGrade 6 Science Document 1api-269382376Ainda não há avaliações
- Horizontal Jaw Relation, Method of Recording andDocumento93 páginasHorizontal Jaw Relation, Method of Recording andHaroon Mohamed100% (1)
- Clinical Manual of Otolaryngology Clear ScanDocumento283 páginasClinical Manual of Otolaryngology Clear ScanAyman Yakout100% (4)
- Role and Responsibilities of Livestock Sector in Poverty2Documento18 páginasRole and Responsibilities of Livestock Sector in Poverty2Sunil GamageAinda não há avaliações
- Tetracycline Antibiotics: Medical UsesDocumento2 páginasTetracycline Antibiotics: Medical UsesHanumant SuryawanshiAinda não há avaliações
- Nephrotic and NephriticDocumento3 páginasNephrotic and Nephritickguzman92Ainda não há avaliações
- Pashto DictionaryDocumento436 páginasPashto DictionaryRs0% (1)
- IndomethacinDocumento17 páginasIndomethacinRajpal Singh KochharAinda não há avaliações
- The Soul According To The Ethnolinguistic Groups of The PhilippinesDocumento4 páginasThe Soul According To The Ethnolinguistic Groups of The PhilippinesEarl SantosAinda não há avaliações
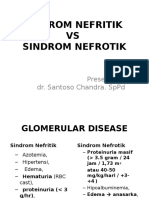
- Sindroma Nefrotik Vs NefritikDocumento23 páginasSindroma Nefrotik Vs NefritikihsanAinda não há avaliações
- Veterinary Anatomy of Domestic Mammals - Textbook and Colour Atlas (2004)Documento703 páginasVeterinary Anatomy of Domestic Mammals - Textbook and Colour Atlas (2004)Adina Constantin100% (1)
- Digestive SystemDocumento41 páginasDigestive SystemRotsen B. VelascoAinda não há avaliações
- Diagnostic Test in Science 4: San Carlos Elementary SchoolDocumento4 páginasDiagnostic Test in Science 4: San Carlos Elementary SchoolJohn Nomel B. Dominguez100% (1)
- Pediatrics MCQs - DR Ranjan Singh - Part 1Documento10 páginasPediatrics MCQs - DR Ranjan Singh - Part 1k sagarAinda não há avaliações
- Leadfinger GoblinDocumento1 páginaLeadfinger GoblinBrianAinda não há avaliações
- 2804 Central Concepts January 2006 Mark SchemeDocumento0 página2804 Central Concepts January 2006 Mark SchemeWK SoohgAinda não há avaliações
- Spoof TextDocumento9 páginasSpoof TextHeather LeeAinda não há avaliações
- Basics On Test Selection For Parasites in The CatDocumento4 páginasBasics On Test Selection For Parasites in The CatChantelle NeufeldAinda não há avaliações
- Syndrome of Inappropriate Vasopressin Sexretion (Siadh)Documento22 páginasSyndrome of Inappropriate Vasopressin Sexretion (Siadh)Moni RethAinda não há avaliações
- Pocket Gait CycleDocumento2 páginasPocket Gait CycleherpthederpAinda não há avaliações
- Neck TrianglesDocumento6 páginasNeck TrianglesJay-arh SebusaAinda não há avaliações
- Bio 205 Lab Final Study GuideDocumento8 páginasBio 205 Lab Final Study GuideJames DuongAinda não há avaliações
- Farm Case StudyDocumento10 páginasFarm Case StudyAnthony WhelanAinda não há avaliações
- 7chakra QualitiesDocumento8 páginas7chakra Qualitiesserby108Ainda não há avaliações
- Pretest 4TH Quarter Pe11Documento5 páginasPretest 4TH Quarter Pe11Analyn Taguran Bermudez100% (1)
- MannitolDocumento2 páginasMannitolJen Recto Palad86% (7)
- Overview Congenital Musculoskeletal DisorderDocumento84 páginasOverview Congenital Musculoskeletal DisorderRyan Trian100% (3)
- Biomentors (MCDB 1B) - Immunology Quiz (ANSWERS)Documento2 páginasBiomentors (MCDB 1B) - Immunology Quiz (ANSWERS)Tiff VoAinda não há avaliações
- Biology PPT 11Documento11 páginasBiology PPT 11agarwalabhinav050Ainda não há avaliações
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNota: 4 de 5 estrelas4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingNo EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingNota: 1 de 5 estrelas1/5 (1)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (59)