Escolar Documentos
Profissional Documentos
Cultura Documentos
Dysglycemia and A History of Reproductive Risk Factors: S D. M D, S Y, P S, S S. A, H C. G, Dream T I
Enviado por
Kevin WewengkangTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Dysglycemia and A History of Reproductive Risk Factors: S D. M D, S Y, P S, S S. A, H C. G, Dream T I
Enviado por
Kevin WewengkangDireitos autorais:
Formatos disponíveis
Cardiovascular and Metabolic Risk
O R I G I N A L A R T I C L E
Dysglycemia and a History of Reproductive
Risk Factors
SARAH D. MCDONALD, MD, MSC1 SONIA S. ANAND, MD, PHD2,4 and the use of the older fasting plasma
SALIM YUSUF, MD, DPHIL2,3,4 HERTZEL C. GERSTEIN, MD, MSC2,4,5 glucose cutoff for diabetes of ⬎7.8
PATRICK SHERIDAN, MSC4 FOR THE DREAM TRIAL INVESTIGATORS mmol/l (⬎140 mg/dl) rather than the cur-
rent, more sensitive value of 7.0 mmol/l
(126 mg/dl) (6).
OBJECTIVE — The purpose of this study was to identify reproductive risk factors associated The prevalence of dysglycemia (type
with dysglycemia (diabetes, impaired glucose tolerance, and impaired fasting glucose) in a 2 diabetes, impaired glucose tolerance
contemporary multiethnic population. [IGT], and impaired fasting glucose
[IFG]) is increasing; however, reproduc-
RESEARCH DESIGN AND METHODS — We studied 14,661 women screened with an tive risk factors are often underrecognized.
oral glucose tolerance test for the Diabetes Reduction Assessment with Ramipril and Rosiglita-
In particular, their association with the
zone Medication (DREAM) trial. Reproductive risk factors were compared in normoglycemic
and dysglycemic women. more recently recognized forms of glucose
dysregulation, IGT and IFG, have not yet
RESULTS — Dysglycemia was significantly associated with the number of children born been well studied. The detection of dys-
(odds ratio 1.03 per child [95% CI 1.01–1.05]), age (1.05 per year [1.04 –1.05]), non-European glycemia could be improved if risk factors
ancestry (1.09 [1.01–1.17]), preeclampsia/eclampsia (1.14 [1.02–1.27]), irregular periods (1.21 were better known. Moreover, if repro-
[1.07–1.36]), and gestational diabetes mellitus (GDM) (1.53 [1.35–1.74]). The relationship ductive factors such as parity and pre-
between GDM and dysglycemia did not differ across BMI tertiles (P ⫽ 0.84) nor did the rela- eclampsia are risk factors for dysglycemia,
tionships of other risk factors. they could be used to refine screening ap-
proaches. The goal of this research was to
CONCLUSIONS — Reproductive factors, particularly GDM, are associated with dysglyce-
identify reproductive risk factors for dys-
mia in middle-aged women from many ethnicities. Reproductive factors can be used to counsel
young women about their future risk of dysglycemia, whereas in middle age they may help screen glycemia in a contemporary, multiethnic
for dysglycemia. group of women.
Diabetes Care 31:1635–1638, 2008 RESEARCH DESIGN AND
METHODS — This is a study of
14,661 women screened as possible par-
G
estational diabetes mellitus (GDM) ated with an increased risk of type 2
is a well-known reproductive risk diabetes, with an odds ratio (OR) of 1.16 ticipants in the Diabetes Reduction As-
factor for subsequent type 2 diabe- per pregnancy (95% CI 1.04 –1.20) (3). sessment with Ramipril and Rosiglitazone
tes (1). Other reproductive factors such as An even larger study comprising 2,310 Medication (DREAM) trial (7,8), a large,
preeclampsia are associated with insulin women with type 2 diabetes reported that international, multicenter, randomized,
resistance during pregnancy and may also parity greater than six was associated with double-blind, controlled diabetes preven-
increase the subsequent risk for diabetes. a relative risk (RR) of diabetes of 1.56 tion trial. Participants were volunteers
Furthermore, some (2– 4) but not all (5) (95% CI 1.27–1.91); however, the esti- recruited from 21 countries on five conti-
studies suggest that pregnancy itself is a mate of the RR decreased to 1.19 (0.97– nents from a wide variety of sources in-
risk factor for future type 2 diabetes. For 1.48) after adjustment for current age (2). cluding first-degree relatives of diabetic
example, a population-based study of The applicability of these results is limited individuals in diabetes clinics, ads in
1,186 elderly women showed that, even by the homogeneity of the population newspapers, pharmacies, national diabe-
after accounting for age, obesity, and fam- (registered nurses with relatively high so- tes associations, newsletters, clinics, com-
ily history of diabetes, parity was associ- cioeconomic status and 98% Caucasian) munity announcements, screening
programs, and targeted mailings. Institu-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● tional research ethics boards at each site
From the 1Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, McMaster Uni- approved the DREAM trial.
versity and Hamilton Health Sciences, Hamilton, Ontario, Canada; the 2Department of Medicine, Mc-
Master University and Hamilton Health Sciences, Hamilton, Ontario, Canada; the 3Division of
Cardiology, McMaster University and Hamilton Health Sciences, Hamilton, Ontario, Canada; the 4Pop-
Assessment
ulation Health Research Institute, McMaster University and Hamilton Health Sciences, Hamilton, On- After an overnight (8 –18 h) fast, partici-
tario, Canada; and the 5Division of Endocrinology and Metabolism, McMaster University and Hamilton pants consumed 75 g anhydrous glucose
Health Sciences, Hamilton, Ontario, Canada. and provided fasting and 2-h blood sam-
Corresponding author: Sarah D. McDonald, mcdonals@mcmaster.ca. ples for local measurement of plasma glu-
Received 27 March 2008 and accepted 27 April 2008.
Published ahead of print at http://care.diabetesjournals.org on 5 May 2008. DOI: 10.2337/dc08-0621. cose. At the same time they completed a
The funding organizations had no part in the design of the study; the collection, analysis, or interpretation 12-page questionnaire regarding baseline
of the data; or the decision to approve publication of the finished manuscript. characteristics, medications, and personal
© 2008 by the American Diabetes Association. Readers may use this article as long as the work is properly and family history, and women com-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons.
org/licenses/by-nc-nd/3.0/ for details.
pleted a 1-page reproductive question-
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby naire regarding regularity of menstrual
marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. cycles, fertility, how many children they
DIABETES CARE, VOLUME 31, NUMBER 8, AUGUST 2008 1635
Dysglycemia and reproductive risk factors
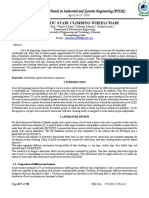
Table 1—Baseline characteristics of participants and age-adjusted univariate analyses of reproductive risk factors and the risk of dysglycemia
Age-adjusted
No P value OR (95% CI)
Dysglycemia dysglycemia (unadjusted) of dysglycemia
n 6,298 8,363
Age (years) 55.1 ⫾ 11.1 50.0 ⫾ 10.0 ⬍0.0001 NA
Number of children 2.74 ⫾ 1.6 2.53 ⫾ 1.3 ⬍0.0001 1.05 (1.04–1.06)
Low socioeconomic states 2,243 (37.7) 2,636 (33.2) ⬍0.0001 1.09 (1.01–1.17)
Non-European ancestry 3,339 (53.0) 4,649 (55.6) 0.002 1.10 (1.02–1.17)
Preeclampsia/eclampsia 700 (11.0) 853 (10.1) 0.10 1.19 (1.07–1.32)
Irregular periods 608 (9.6) 734 (8.8) 0.08 1.22 (1.09–1.38)
GDM 588 (9.4) 673 (8.1) 0.01 1.58 (1.40–1.78)
Early menopause 124 (2.0) 217 (2.6) 0.01 1.24 (0.99–1.56)
BMI (kg/m2) 31.6 ⫾ 6.0 29.4 ⫾ 6.0 ⬍0.0001 1.06 (1.06–1.07)
Data are means ⫾ SD and n (%) unless otherwise indicated. Dysglycemia indicates IFG, IGT, or type 2 diabetes, irregular periods indicates ⱕ6 menstrual cycles per
year between the ages of 18 and 45 years not including pregnancy, and early menopause indicates permanent cessation of menses ⬍45 years of age. NA, not
applicable.
had given birth to, and complications of for reproductive risk factors for dysglyce- 1.01–1.05]), age (1.05 per year [1.04 –
pregnancy including GDM, preeclamp- mia. Factors that were statistically signif- 1.05]), non-European ancestry (1.09
sia, or eclampsia. icant at P ⬍ 0.10 in the age-adjusted [1.01–1.17]), a history of preeclampsia/
analysis were included in the multivariate eclampsia (1.14 [1.02–1.27]), irregular
Definitions logistic regression to determine their in- menses (1.21 [1.07–1.36]), and GDM
Type 2 diabetes was defined as fasting dependent relationship with prevalent (1.53 [1.35–1.74]) (Fig. 1). Early meno-
plasma glucose ⱖ7.0 mmol/l (ⱖ126 mg/ dysglycemia. This model was rerun for pause (1.24 [0.98 –1.53]) and low socio-
dl) or plasma glucose ⱖ11.1 mmol/l each tertile of BMI (and P values for het- economic status (0.95 [0.88 –1.02]) were
(ⱖ200 mg/dl) 2 h after a 75-g oral glucose erogeneity were calculated) to determine no longer significantly associated with
load. IGT was defined as plasma glucose whether the risk of dysglycemia for each dysglycemia.
7.8 –11.0 mmol/l (140 –199 mg/dl) 2 h risk factor varied with BMI. All P values To determine whether there was an
after a 75-g oral glucose load. IFG was are reported as two-tailed. All analyses interaction between BMI and the repro-
defined as fasting glucose of 6.1– 6.9 were performed using SAS software (ver- ductive risk factors, particularly GDM, we
mmol/l (110 –124 mg/dl). Dysglycemia sion 9.1; SAS Institute, Cary, NC). reran the multiple regression model for
was defined as IFG, IGT, or type 2 diabe- each tertile of BMI, with 27.1 and 32.2
tes. Parity was defined as the number of RESULTS — Table 1 presents the base- defining lower, middle, and upper levels.
infants a woman had borne. Irregular line characteristics of the women with (n ⫽ The relationships between GDM and cur-
menses was defined as six or fewer men- 6, 298) and without (n ⫽ 8, 363) dysglyce- rent dysglycemia did not differ signifi-
strual cycles per year between the ages of mia, whose 2-h plasma glucose concentra- cantly across tertiles of BMI (Pheterogeneity
18 and 45 years not including pregnancy tions were 10.0 ⫾ 3.1 versus 5.7 ⫾ 1.1 ⫽ 0.84), nor for any of the other risk fac-
and was used as a surrogate for polycystic mmol/l, respectively (P ⬍ 0.0001), with tors (Pheterogeneity ⱖ0.10 for all). The ORs
ovary syndrome. Early menopause was fasting values of 6.3 ⫾ 1.4 versus 5.0 ⫾ 1.1 for GDM and current dysglycemia for
defined as the permanent cessation of mmol/l (P ⬍ 0.0001, respectively). Women each tertile of BMI (⬍27.1, 27.1–32.2,
menstrual periods before age 45. Income with dysglycemia were significantly older and ⬎32.2) were 1.81 [95% CI 1.42–
range tables with five strata were devel- than those without dysglycemia (55.1 vs. 2.30], 1.44 [1.14 –1.81], and 1.47 [1.20 –
oped specific to each country in which 50.0 years, respectively, P ⬍ 0.0001). After 1.81], respectively.
recruitment occurred; low socioeconomic adjustment for age, most of the reproduc-
status was defined as the lowest strata for tive factors remained significantly associ- CONCLUSIONS — This large, mul-
that country. In Canada, for example, that ated with dysglycemia, including the tiethnic study of middle-aged women
included a household income ⱕ$29,999 number of children a woman gave birth to showed that a history of GDM is indepen-
and for the U.S. it was ⱕ$15,400. Non- (OR 1.05 per child [95% CI 1.04 –1.06]), a dently associated with prevalent dysgly-
European ancestry was defined as anyone history of preeclampsia/eclampsia (1.19 cemia, confirming that pregnancy is a
indicating any ancestry other than Euro- [1.07–1.32]), irregular menses (1.2 [1.09 – “stress test for life” (9,10). This observa-
pean at the time of their clinic visit. 1.38]), GDM (1.58 [1.40 –1.78]), low so- tion may be understood in light of the fact
cioeconomic status (1.09 [1.01–1.17]), and that the occurrence of GDM is clear evi-
Statistical analysis non-European ancestry (1.10 [1.02–1.17]) dence of an impaired ability to maintain
Women were classified as those with and (Table 1). normoglycemia under the metabolic
without dysglycemia. Continuous vari- In a multivariate model that included stress of pregnancy and is consistent with
ables were compared using a t test, and age, ancestry, and fertility-related factors, previous reports (11–14) from smaller
categorical variables were compared with dysglycemia was significantly associated studies. Hence, in young women of child-
a 2 test. Logistic regression was used to with the number of children a woman bearing age, reproductive factors, partic-
calculate age-adjusted ORs and 95% CI gave birth to (OR 1.03 per child [95% CI ularly GDM, can be used to counsel
1636 DIABETES CARE, VOLUME 31, NUMBER 8, AUGUST 2008
McDonald and Associates
dysglycemia was independently associ-
ated with a history of several reproductive
risk factors, particularly GDM. Moreover,
the relationship between prior GDM and
current dysglycemia persisted across BMI
strata.
Acknowledgments — The DREAM Trial was
funded by the Canadian Institutes of Health
Research, sanofi-aventis, GlaxoSmithKline,
and King Pharmaceuticals through the Univer-
sity Industry Grant Program. S.Y. holds a
Heart and Stroke Foundation Chair in Cardio-
vascular Research. S.S.A. holds the Eli Lilly
Canada–May Cohen Chair in Women’s
Health. H.C.G. holds the Population Health
Institute Chair in Diabetes Research spon-
sored by aventis.
References
1. O’Sullivan JB: Diabetes mellitus after
GDM. Diabetes 40 (Suppl. 2):131–135,
1991
2. Manson JE, Rimm EB, Colditz GA,
Figure 1—Dysglycemia indicates IFG, IGT, or type 2 diabetes, CI represents the Wald CI, low Stampfer MJ, Willett WC, Arky RA, Ros-
SES indicates low socioeconomic status, and irregular menses indicates ⱕ6 menstrual cycles per ner B, Hennekens CH, Speizer FE: Parity
year between the ages of 18 and 45 years not including pregnancy. and incidence of non-insulin-dependent
diabetes mellitus. Am J Med 93:13–18,
1992
patients about their future risk of dysgly- factors that identified women at increased 3. Kritz-Silverstein D, Barrett-Connor E,
cemia regardless of future BMI, whereas risk of dysglycemia were elicited with Wingard DL: The effect of parity on the
in middle-aged women a history of repro- simple screening questions, which are later development of non-insulin-depen-
ductive risk factors may be useful as a part of a routine history, and do not re- dent diabetes mellitus or impaired glu-
screening tool for dysglycemia. quire serology or imaging investigations cose tolerance. N Engl J Med 321:1214 –
This study also showed that a history such as pelvic ultrasound. Participants 1219, 1989
4. Peters RK, Kjos SL, Xiang A, Buchanan
of a variety of reproductive risk factors, were asked, for instance, about irregular
TA: Long-term diabetogenic effect of sin-
including irregular menses, parity, and menses as a surrogate for PCOS, as PCOS gle pregnancy in women with previous
preeclampsia, was independently associ- remains undiagnosed in many patients or gestational diabetes mellitus. Lancet 347:
ated with dysglycemia and was not they are unfamiliar with the medical term. 227–230, 1996
explained by age, ethnicity, or socioeco- Although this approach has the potential 5. Collins VR, Dowse GK, Zimmet PZ: Evi-
nomic status. One potential explanation for misclassifying some patients who had dence against association between parity
is the association of many of these factors had fertility-related risk factors as being and NIDDM from five population groups.
with insulin resistance, including pre- unaffected, it suggests that the associa- Diabetes Care 14:975–981, 1991
eclampsia (15,16), pregnancy (17), and, tions between fertility-related risk factors 6. Harris MI, Eastman RC, Cowie CC, Flegal
even in nonobese women, polycystic and dysglycemia are probably even stron- KM, Eberhardt MS: Comparison of diabe-
tes diagnostic categories in the U.S. pop-
ovary syndrome (PCOS) (of which irreg- ger than those observed.
ulation according to the 1997 American
ular menses is a key component) (18 – Limitations of the study include the Diabetes Association and 1980 –1985
21). fact that the participants were asked to World Health Organization diagnostic
This is the only study, to our knowl- recall events, such as pregnancies, which criteria. Diabetes Care 20:1859 –1862,
edge, examining reproductive risk factors in many instances occurred several de- 1997
for dysglycemia involving a broad popu- cades earlier. However, by gathering this 7. Gerstein HC, Yusuf S, Bosch J, Pogue J,
lation, allowing for wide applicability of baseline information before the adminis- Sheridan P, Dinccag N, Hanefeld M,
results. Participation spanned all socio- tration of the oral glucose tolerance test, Hoogwerf B, Laakso M, Mohan V, Shaw J,
economic strata and involved 21 coun- recall bias was limited. We did not have Zinman B, Holman RR: Effect of rosiglita-
tries on five continents. Another strength access to the participants’ medical charts zone on the frequency of diabetes in pa-
tients with impaired glucose tolerance or
is the large sample size (14, 661 women), and relied on patient history, which may
impaired fasting glucose: a randomised
by far the largest study in the literature on not always be reliable and may underesti- controlled trial. Lancet 368:1096 –1105,
reproductive risk factors and dysglyce- mate some of the above associations. 2006
mia, which allowed for control of multi- In summary, in this large, multiethnic 8. Bosch J, Yusuf S, Gerstein HC, Pogue J,
ple confounding factors. Another study of middle-aged women without a Sheridan P, Dagenais G, Diaz R, Avezum
strength is the fact that reproductive risk previous diagnosis of diabetes, prevalent A, Lanas F, Probstfield J, Fodor G, Hol-
DIABETES CARE, VOLUME 31, NUMBER 8, AUGUST 2008 1637
Dysglycemia and reproductive risk factors
man RR: Effect of ramipril on the inci- 13. Dalfra MG, Lapolla A, Masin M, Giglia G, man pregnancy. Am J Obstet Gynecol 170:
dence of diabetes. N Engl J Med 355:1551– Dalla BB, Toniato R, Fedele D: Antepar- 635– 641, 1994
1562, 2006 tum and early postpartum predictors of 18. Amanti-Kandarakis E, Papavassiliou A:
9. Williams D: Pregnancy: a stress test for type 2 diabetes development in women Molecular mechanisms of insulin resis-
life. Curr Opin Obstet Gynecol. 15:465– with gestational diabetes mellitus. Diabe- tance in polycystic ovary syndrome.
471, 2003 tes Metab 27:675– 680, 2001 Trends Mol Med 12:324 –332, 2006
10. Sibai BM, el-Nazer A, Gonzalez-Ruiz A: 14. Buchanan TA, Xiang A, Kjos SL, Lee WP, 19. Sawathiparnich P, Weerakulwattana L,
Severe preeclampsia-eclampsia in young Trigo E, Nader I, Bergner EA, Palmer JP, Santiprabhob J, Likitmaskul S: Obese ad-
primigravid women: subsequent preg- Peters RK: Gestational diabetes: antepar- olescent girls with polycystic ovary syn-
nancy outcome and remote prognosis. tum characteristics that predict postpar- drome (PCOS) have more severe insulin
Am J Obstet Gynecol 155:1011–1016, tum glucose intolerance and type 2 resistance measured by HOMA-IR score
1986 diabetes in Latino women. Diabetes 47:
than obese girls without PCOS. J Med As-
11. Pallardo LF, Herranz L, Martin-Vaquero 1302–1310, 1998
soc Thai 88 (Suppl. 8):S33–S37, 2005
P, Garcia-Ingelmo T, Grande C, Janez M: 15. Kaaja R, Laivuori H, Laakso M, Tikkanen
20. Yilmaz M, Biri A, Karakoc A, Toruner F,
Impaired fasting glucose and impaired MJ, Ylikorkala O: Evidence of a state of
glucose tolerance in women with prior increased insulin resistance in preeclamp- Bingol B, Cakir N, Tiras B, Ayvaz G, Ar-
gestational diabetes are associated with a sia. Metabolism 48:892– 896, 1999 slan M: The effects of rosiglitazone and
different cardiovascular profile. Diabetes 16. Fuh MM, Yin CS, Pei D, Sheu WH, Jeng metformin on insulin resistance and se-
Care 26:2318 –2322, 2003 CY, Chen YI, Reaven GM: Resistance to rum androgen levels in obese and lean pa-
12. Lauenborg J, Hansen T, Jensen DM, Ves- insulin-mediated glucose uptake and tients with polycystic ovary syndrome. J
tergaard H, Molsted-Pedersen L, Hornnes hyperinsulinemia in women who had Endocrinol Invest 28:1003–1008, 2005
P, Locht H, Pedersen O, Damm P: In- preeclampsia during pregnancy. Am J 21. DeUgarte CM, Bartolucci AA, Azziz R:
creasing incidence of diabetes after gesta- Hypertens 8:768 –771, 1995 Prevalence of insulin resistance in the
tional diabetes: a long-term follow-up in a 17. Ciaraldi TP, Kettel M, el-Roeiy A, Madar polycystic ovary syndrome using the ho-
Danish population. Diabetes Care 27: Z, Reichart D, Yen SS, Olefsky JM: Mech- meostasis model assessment. Fertil Steril
1194 –1199, 2004 anisms of cellular insulin resistance in hu- 83:1454 –1460, 2005
1638 DIABETES CARE, VOLUME 31, NUMBER 8, AUGUST 2008
Você também pode gostar
- Early Postpartum Metabolic Syndrome in Women With or Without 2017Documento7 páginasEarly Postpartum Metabolic Syndrome in Women With or Without 2017Lucas LorranAinda não há avaliações
- A Prospective Study of Gestational DMDocumento6 páginasA Prospective Study of Gestational DMOdilia Rondang Mauli SimarmataAinda não há avaliações
- Use of The Estimated Glucose Disposal Rate As A Measure of Insulin Resistance in An Urban Multiethnic Population With Type 1 DiabetesDocumento6 páginasUse of The Estimated Glucose Disposal Rate As A Measure of Insulin Resistance in An Urban Multiethnic Population With Type 1 Diabetesjulio perezAinda não há avaliações
- Jamapediatrics Andes 2019 Oi 190082Documento9 páginasJamapediatrics Andes 2019 Oi 190082TRISNAANHAAinda não há avaliações
- Animal Model For Gestational DiabetesDocumento14 páginasAnimal Model For Gestational DiabetesAnushka DhandeAinda não há avaliações
- Ref 3Documento10 páginasRef 3asshagab04Ainda não há avaliações
- Comparison of Glyburide and Insulin in The Man PDFDocumento18 páginasComparison of Glyburide and Insulin in The Man PDFwinda istikhomahAinda não há avaliações
- The Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyDocumento10 páginasThe Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyaocuAinda não há avaliações
- Overweight and The Metabolic Syndrome in Adult Offspring of Women With Diet-Treated Gestational Diabetes Mellitus or Type 1 DiabetesDocumento7 páginasOverweight and The Metabolic Syndrome in Adult Offspring of Women With Diet-Treated Gestational Diabetes Mellitus or Type 1 DiabetesMyoman FernandaAinda não há avaliações
- Gestational Diabetes Mellitus Acog CopDocumento8 páginasGestational Diabetes Mellitus Acog CopAndrea Sandoval OteroAinda não há avaliações
- Gestational Diabetes Mellitus: Science in MedicineDocumento7 páginasGestational Diabetes Mellitus: Science in MedicinerizqarrAinda não há avaliações
- Garber 2007Documento6 páginasGarber 2007Diana SamuezaAinda não há avaliações
- ACOG Practice Bulletin No137 PDFDocumento11 páginasACOG Practice Bulletin No137 PDFRodrigo Pérez CuelloAinda não há avaliações
- Disbetes Obs PDFDocumento18 páginasDisbetes Obs PDFdhruvAinda não há avaliações
- Effects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceDocumento8 páginasEffects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceAzielAinda não há avaliações
- Personalized Genetic Risk Counseling To Motivate Diabetes PreventionDocumento7 páginasPersonalized Genetic Risk Counseling To Motivate Diabetes PreventionJoban PhulkaAinda não há avaliações
- Metabolic Syndrome in Childhood: Association With Birth Weight, Maternal Obesity, and Gestational Diabetes MellitusDocumento9 páginasMetabolic Syndrome in Childhood: Association With Birth Weight, Maternal Obesity, and Gestational Diabetes MellitusAnnisa FujiantiAinda não há avaliações
- Screening Diabetes ADA 2002Documento4 páginasScreening Diabetes ADA 2002Tri YuliasihAinda não há avaliações
- Dibetes Risk Score - Findrisc - Jaana Lindstrom - ArticleDocumento7 páginasDibetes Risk Score - Findrisc - Jaana Lindstrom - ArticleShayekh M ArifAinda não há avaliações
- Article IJDCD 118Documento3 páginasArticle IJDCD 118Heppy Roosarina Rahayudewi HardjitoAinda não há avaliações
- POSITION STATEMENTPreDMsop TRTRDocumento12 páginasPOSITION STATEMENTPreDMsop TRTRTony CoaAinda não há avaliações
- HISTOMOROFOMEDocumento6 páginasHISTOMOROFOMEMayra PereiraAinda não há avaliações
- Ober 1989Documento11 páginasOber 1989Sarly FebrianaAinda não há avaliações
- Articulo de InvestigacionDocumento8 páginasArticulo de Investigacionjai_santiago_rojasAinda não há avaliações
- Egyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. AltayebDocumento5 páginasEgyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. Altayebida ayu agung WijayantiAinda não há avaliações
- Gestational Diabetes Mellitus Update and Review of Literature 2161 038X.S2 008 PDFDocumento6 páginasGestational Diabetes Mellitus Update and Review of Literature 2161 038X.S2 008 PDFBuluan Mps McadAinda não há avaliações
- Febriyanti M. AdamDocumento23 páginasFebriyanti M. AdamRinda UnoAinda não há avaliações
- Alicia Paper1Documento7 páginasAlicia Paper1Andrés Thiele HortaAinda não há avaliações
- Comparison of Cystic Fibrosis - Related Diabetes With Type 1 Diabetes Based On A German/Austrian Pediatric Diabetes RegistryDocumento8 páginasComparison of Cystic Fibrosis - Related Diabetes With Type 1 Diabetes Based On A German/Austrian Pediatric Diabetes RegistryAgus SetiawanAinda não há avaliações
- AAFP DRC and DiabetesDocumento9 páginasAAFP DRC and DiabetesThaysa LimaAinda não há avaliações
- Effects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceDocumento8 páginasEffects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceOzan OcakAinda não há avaliações
- Gestational Diabetes Mellitus: Thomas A. Buchanan, Anny H. XiangDocumento8 páginasGestational Diabetes Mellitus: Thomas A. Buchanan, Anny H. Xiangalen walkerAinda não há avaliações
- Metformin or Oral Contraceptives For Adolescents With Polycystic Ovarian Syndrome A Meta-AnalysisDocumento14 páginasMetformin or Oral Contraceptives For Adolescents With Polycystic Ovarian Syndrome A Meta-Analysiscristobal ramosAinda não há avaliações
- YogurtDocumento10 páginasYogurtAbd Halim Gazali HAinda não há avaliações
- Final IntroDocumento3 páginasFinal IntroAngelique Claire DavidAinda não há avaliações
- Diabetes Mellitus and Pregnancy: Chapter OutlineDocumento21 páginasDiabetes Mellitus and Pregnancy: Chapter OutlineqalbiAinda não há avaliações
- Artigo Celã - AcaDocumento8 páginasArtigo Celã - AcaSofia Hilda CorreiaAinda não há avaliações
- Article 233554Documento11 páginasArticle 233554رقية ياسينAinda não há avaliações
- Full CommunicationsDocumento6 páginasFull CommunicationsSamir Castolo SanchezAinda não há avaliações
- Annotated BibliographyDocumento20 páginasAnnotated Bibliographyapi-347153077Ainda não há avaliações
- Prevalence of Diabetes Mellitus Amongst Antenatal Clinic Attendees at Booking in A Teaching Hospital in Rivers State, NigeriaDocumento3 páginasPrevalence of Diabetes Mellitus Amongst Antenatal Clinic Attendees at Booking in A Teaching Hospital in Rivers State, NigeriaInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- JurnalDocumento3 páginasJurnalARINAAinda não há avaliações
- 23 Iajps23072017Documento5 páginas23 Iajps23072017Baru Chandrasekhar RaoAinda não há avaliações
- Chapter 1 To 4Documento65 páginasChapter 1 To 4Shakila100% (1)
- Pregnancy Body Mass Index Procedure Metabolic Syndrome X Diabetes Mellitus HyperglycemiaDocumento14 páginasPregnancy Body Mass Index Procedure Metabolic Syndrome X Diabetes Mellitus HyperglycemiaMohamad RifkiAinda não há avaliações
- DM Gestacional 2014Documento6 páginasDM Gestacional 2014mariajuliabechepecheAinda não há avaliações
- S105 FullDocumento7 páginasS105 FullNurul HidayatiAinda não há avaliações
- I J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticDocumento5 páginasI J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticAbed AlhaleemAinda não há avaliações
- Beyond Pregnancy Understanding The Long-Term Implications of Gestational Diabetes MellitusDocumento9 páginasBeyond Pregnancy Understanding The Long-Term Implications of Gestational Diabetes MellitusKIU PUBLICATION AND EXTENSIONAinda não há avaliações
- Jurnal Tentang Gambaran Kondisi Ibu Hamil Dengan Diabetes Mellitus Di RSD Dr. Soebandi Jember Tahun 2013-2017Documento11 páginasJurnal Tentang Gambaran Kondisi Ibu Hamil Dengan Diabetes Mellitus Di RSD Dr. Soebandi Jember Tahun 2013-2017EtiAinda não há avaliações
- By Guest On 26 April 2018Documento8 páginasBy Guest On 26 April 2018silvanaAinda não há avaliações
- Neoreviews 042022cmerev00036Documento12 páginasNeoreviews 042022cmerev00036Agnimitra ChoudhuryAinda não há avaliações
- Prevalence of Gestational Diabetes Mellitus Evaluated by Universal Screening With A 75-g, 2 - Hour Oral Glucose Tolerance Test and IADPSG CriteriaDocumento4 páginasPrevalence of Gestational Diabetes Mellitus Evaluated by Universal Screening With A 75-g, 2 - Hour Oral Glucose Tolerance Test and IADPSG CriteriaCamila Alicia López AndradeAinda não há avaliações
- The Triglyceride-to-HDL Cholesterol RatioDocumento6 páginasThe Triglyceride-to-HDL Cholesterol RatioArthurAinda não há avaliações
- Jurnal PH 13Documento9 páginasJurnal PH 13ruthameliapAinda não há avaliações
- JAMA Intern Med 2021 Apr 1 181 (4) 520-521Documento2 páginasJAMA Intern Med 2021 Apr 1 181 (4) 520-521Samuel SalazarAinda não há avaliações
- DZ 11Documento5 páginasDZ 11licenteAinda não há avaliações
- The Metabolic Syndrome, Diabetes, and Alzheimer's DiseaseDocumento7 páginasThe Metabolic Syndrome, Diabetes, and Alzheimer's DiseaseMICHAELATTOAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsNo EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsAinda não há avaliações
- Prediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalNo EverandPrediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalAinda não há avaliações
- LkpaskebfixxxDocumento835 páginasLkpaskebfixxxKevin WewengkangAinda não há avaliações
- Dysglycemia and Cardiovascular Risk in The General PopulationDocumento4 páginasDysglycemia and Cardiovascular Risk in The General PopulationKevin WewengkangAinda não há avaliações
- Warren SM CH 02 Final PDFDocumento66 páginasWarren SM CH 02 Final PDFSandra0% (1)
- UndangancgDocumento1 páginaUndangancgKevin WewengkangAinda não há avaliações
- PPB 3193 Operation Management - Group 10Documento11 páginasPPB 3193 Operation Management - Group 10树荫世界Ainda não há avaliações
- GATE General Aptitude GA Syllabus Common To AllDocumento2 páginasGATE General Aptitude GA Syllabus Common To AllAbiramiAbiAinda não há avaliações
- 133 The Science and Understanding of TheDocumento14 páginas133 The Science and Understanding of TheCarlos RieraAinda não há avaliações
- ReviewerDocumento2 páginasReviewerAra Mae Pandez HugoAinda não há avaliações
- Numerical Transformer Differential RelayDocumento2 páginasNumerical Transformer Differential RelayTariq Mohammed OmarAinda não há avaliações
- Caso Kola RealDocumento17 páginasCaso Kola RealEvelyn Dayhanna Escobar PalomequeAinda não há avaliações
- Dmta 20043 01en Omniscan SX UserDocumento90 páginasDmta 20043 01en Omniscan SX UserwenhuaAinda não há avaliações
- PE Range Moulded Case Current Transformers: Energy DivisionDocumento7 páginasPE Range Moulded Case Current Transformers: Energy DivisionUlfran MedinaAinda não há avaliações
- Crawler Base DX500/DX600/DX680/ DX700/DX780/DX800: Original InstructionsDocumento46 páginasCrawler Base DX500/DX600/DX680/ DX700/DX780/DX800: Original InstructionsdefiunikasungtiAinda não há avaliações
- Econ 1006 Summary Notes 1Documento24 páginasEcon 1006 Summary Notes 1KulehAinda não há avaliações
- Quantum Hopfield NetworksDocumento83 páginasQuantum Hopfield NetworksSiddharth SharmaAinda não há avaliações
- Overcurrent CoordinationDocumento93 páginasOvercurrent CoordinationKumar100% (1)
- The Finley ReportDocumento46 páginasThe Finley ReportToronto StarAinda não há avaliações
- Napoleon RXT425SIBPK Owner's ManualDocumento48 páginasNapoleon RXT425SIBPK Owner's ManualFaraaz DamjiAinda não há avaliações
- Assessment 21GES1475Documento4 páginasAssessment 21GES1475kavindupunsara02Ainda não há avaliações
- Application of ARIMAX ModelDocumento5 páginasApplication of ARIMAX ModelAgus Setiansyah Idris ShalehAinda não há avaliações
- Aluminium Extrusion Industry in IndiaDocumento3 páginasAluminium Extrusion Industry in Indiakalan45Ainda não há avaliações
- Computer System Architecture: Pamantasan NG CabuyaoDocumento12 páginasComputer System Architecture: Pamantasan NG CabuyaoBien MedinaAinda não há avaliações
- Copeland PresentationDocumento26 páginasCopeland Presentationjai soniAinda não há avaliações
- Lexington School District Two Return To School GuideDocumento20 páginasLexington School District Two Return To School GuideWLTXAinda não há avaliações
- Liga NG Mga Barangay: Resolution No. 30Documento2 páginasLiga NG Mga Barangay: Resolution No. 30Rey PerezAinda não há avaliações
- Emergency and Safety ProceduresDocumento22 páginasEmergency and Safety Procedurespaupastrana94% (17)
- MCS Valve: Minimizes Body Washout Problems and Provides Reliable Low-Pressure SealingDocumento4 páginasMCS Valve: Minimizes Body Washout Problems and Provides Reliable Low-Pressure SealingTerry SmithAinda não há avaliações
- Intelligent Smoke & Heat Detectors: Open, Digital Protocol Addressed by The Patented XPERT Card Electronics Free BaseDocumento4 páginasIntelligent Smoke & Heat Detectors: Open, Digital Protocol Addressed by The Patented XPERT Card Electronics Free BaseBabali MedAinda não há avaliações
- Automatic Stair Climbing Wheelchair: Professional Trends in Industrial and Systems Engineering (PTISE)Documento7 páginasAutomatic Stair Climbing Wheelchair: Professional Trends in Industrial and Systems Engineering (PTISE)Abdelrahman MahmoudAinda não há avaliações
- Digital Documentation Class 10 NotesDocumento8 páginasDigital Documentation Class 10 NotesRuby Khatoon86% (7)
- Dr. Najeebuddin Ahmed: 969 Canterbury Road, Lakemba, Sydney, NSW, Australia, 2195Documento2 páginasDr. Najeebuddin Ahmed: 969 Canterbury Road, Lakemba, Sydney, NSW, Australia, 2195Najeebuddin AhmedAinda não há avaliações
- Gis Tabels 2014 15Documento24 páginasGis Tabels 2014 15seprwglAinda não há avaliações
- IOSA Information BrochureDocumento14 páginasIOSA Information BrochureHavva SahınAinda não há avaliações
- Writing Task The Strategy of Regional Economic DevelopementDocumento4 páginasWriting Task The Strategy of Regional Economic DevelopementyosiAinda não há avaliações