Escolar Documentos
Profissional Documentos
Cultura Documentos
2018 Notice of Hearing Onfor DR Porter CNOH (First Amendment And)
Enviado por
KOLD News 130 notas0% acharam este documento útil (0 voto)
48 visualizações9 páginasNotice of hearing 2018
Título original
2. 21. 2018 Notice of Hearing Onfor Dr Porter CNOH (First Amendment and )
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoNotice of hearing 2018
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
48 visualizações9 páginas2018 Notice of Hearing Onfor DR Porter CNOH (First Amendment And)
Enviado por
KOLD News 13Notice of hearing 2018
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF ou leia online no Scribd
Você está na página 1de 9
SocmrxridvdH er wDd
ll
12
13
15
16
17
18
19
20
21
a2
2B
4
25
26
27
28
Mark Brnovich
Attorney General
(Firm State Bar No. 14000)
‘Anne Froedge
Assistant Attorney General
State Bar No. 011354
Licensing and Enforcement Section
2005 N. Central Avenue
Phoenix, Arizona 85004
Telephone: (602) 542-7984
Fax: (602) 364-3202
Attorneys for the Arizona Medical Board
BEFORE THE ARIZONA MEDICAL BOARD
IN THE OFFICE OF ADMINISTRATIVE HEARINGS
In the Matter of Case No. 17A-14879-MDX
GREGORY J. PORTER, M.D. FIRST AMENDED COMPLAINT AND
NOTICE OF HEARING
Holder of License No. 14879 ; a. .
For the Practice of Allopathic Medicine | (Assigned to Administrative Law Judge
In the State of Arizona. Diane Mihalsky)
JURISDICTION
This Complaint and Notice of Hearing are prepared, and these proceedings are
instituted, under A.R.S. § 32-1451 and 41-1092, et seq.
PARTIES
1. The Board is the duly constituted authority for the regulation and control of
the practice of allopathic medicine in the State of Arizona.
2. Respondent is the holder of license number 14879 for the practice of
allopathic medicine in the State of Arizona.
FACTUAL ALLEGATIONS
1. The Board initiated case number MD-16-0992A after receiving a
complaint regarding Respondent's care and treatment of a 60 year-old female patient
(‘VC") alleging failure to properly prescribe medications, resulting in the patient's
death.
2. VC established care with Respondent on March 2, 2016. VC had a prior
history of chronic pain managed on a stable opiate regimen of Morphine Sulfate
Extended Release 30 mg. at bedtime and oxycodone 15mg as needed for
breakthrough pain (2-3 daily with #75 dispensed for a one-month supply).
3. On VC's first visit with Respondent, he identified her chief complaint as;
“Chronic Pain,” secondary to fibromyalgia and lumbar stenosis with “all over" pain and
occasional sciatica in absence of a history of prior surgery. In addition, Respondent
documented “severe stress” as a subjective complaint. VC's medication list at that
time included Morphine 30mg at bedtime, oxycodone 15mg twice daily, tizanidine 4mg
twice daily and Ibuprofen 800mg three times daily for her pain, in addition to
prescriptions for Xanax (for anxiety) and amlodipine. VC was noted to have a history of
hypothyroidism, and was non-compliant with her medication for that condition.
4. Respondent performed a physical examination of VC and documented
tenderness over the lumbar spine (at L3/4) with normal reflexes and no focal
neurologic deficits. Respondent's plan was to add amitriptyline, recommend water
exercise, and to “consider methadone.” For her non-pain complaints, Respondent
ordered lab studies and adjusted VC's blood pressure medications. VC's last
prescription for morphine and oxycodone would have been due for refill on or about
March 4, 2016: two days after this visit.
5. Respondent saw VC again on March 7, 2016. At that visit, VC reported
improved pain, sleep, and that she was more relaxed with amitriptyline. The
documented history of present illness noted that VC stated “I need morphine.” Her|
2
medication list was recorded as unchanged from the prior visit. Respondent performed
another physical examination and noted tenderness at 13/4. Respondent's)
assessment included fibromyalgia and lumbar radiculopathy. Respondent documented
a plan for VC's pain including the addition of methadone 10mg three times daily as}
needed and “— MS or oxy.”
6. On March 12, 2016, VC was found non-responsive by her daughter.
According to the autopsy report, the bottle of methadone had 73 tablets remaining of|
the 90 dispensed for VC. The pathologist who performed the autopsy opined that the
cause of death was a “mixed drug toxicity: methadone and amitriptyline” with a
contributory cause of death including arteriosclerotic cardiovascular disease.
7. The standard of care required Respondent to utilize diagnostic studies,
outside records and the pharmacy board report information when determining whether
to initiate treatment with opiate therapy. Respondent deviated from this standard of|
care by failing to utilize diagnostic studies, outside records or pharmacy board report
information at the time the decision was made to treat VC with opiate therapy.
8. The standard of care requires an accurate calculation of starting dosage|
when converting the patient's regimen from morphine/oxycodone to methadone, to
start the patient at a recommended dose, and to obtain a baseline EKG to assess for|
QT prolongation prior to starting the patient on methadone. Respondent deviated from
this standard of care by converting VC's regimen from morphine/oxycodone to
methadone without an accurate calculation of starting dose, by starting VC at a dose!
that was well above what would have been recommended, and by failing to obtain a
baseline EKG to assess for QT prolongation prior to starting methadone.
9. The potential for increased CNS depression, QT prolongation, and cardiac}
arrhythmias existed with the combination of amitriptyline and methadone, particularly
since these medications were new for VC.
10. Actual harm occurred to the patient in that VC died with a cause of death
related to her use of methadone and amitriptyline.
141. A physician is required to maintain adequate legible medical records
containing, at a minimum, sufficient information to identify the patient, support the
diagnosis, justify the treatment, accurately document the results, indicate advice and
cautionary warnings provided to the patient and provide sufficient information for|
another practitioner to assume continuity of the patient's care at any point in the
course of treatment. A.R.S. § 32-1401(2). Respondent's records were inadequate in
that portions were illegible and the records were unclear as to the reason for such a
drastic change from VC's previously stable medication regimen. The record is unclear]
as to why Respondent prescribed methadone for VC.
12. During the Board’s consideration of the above captioned matter on May 4,
2017, Respondent stated that he did not believe that methadone was a factor in the
patient's death. Board members commented that after hearing from Respondent, they
were concerned that the Respondent did not appear to understand the ramifications of|
his prescribing and the drug-to-drug interactions of the medications at issue in the
case. One Board member was particularly concerned that Respondent did not
address the findings on the autopsy for VC.
13. Based on the evidence presented, the Board voted unanimously to)
summarily restrict Respondent's license, prohibiting him from prescribing controlled
substances.
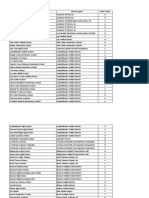
14. The Board initiated case number MD-17-1152 on November 21, 2017,
after a Controlled Substances Prescription Monitoring Program (“CSPMP”)
report indicated that Respondent wrote seven prescriptions to five patients (JC,
EZ, SU, GG, and MM) in violation of his practice restriction.
15. Board staff obtained hard-copy prescriptions for controlled
substances for patients JC, EZ, SU, and GG, that Respondent wrote after the
date of his practice restriction. Of not, the prescriptions for JC were phoned in.
16. In telephone calls with Board staff on November 29, 2017, and
January 3, 2018, Respondent admitted to writing five of the prescriptions in
violation of his practice restriction. Respondent stated that he could not
remember if he gave permission to his office staff to phone in the other two
prescriptions.
ALLEGATIONS OF UNPROFESSIONAL CONDUCT
1. The Board possesses jurisdiction over the subject matter hereof and over
Respondent.
2. The conduct and circumstances described above _ constitute]
unprofessional conduct pursuant to A.R.S. § 32-1401(27)(e) (‘Failing or refusing to
maintain adequate records on a patient.”).
3. The conduct and circumstances described above _ constitute!
unprofessional conduct pursuant to A.R.S. § 32-1401(27)(q) (‘Any conduct or practice
that is or might be harmful or dangerous to the health of the patient or the public.”).
4. The conduct and circumstances described above constitute
unprofessional conduct pursuant to A.R.S. § 32-1401(27)(r) (“Violating a formal
order, probation, consent agreement or stipulation issued or entered into by the
board or its executive director under this chapter.”).
5. The conduct and circumstances described above show that the public|
health, safety or welfare imperatively required emergency action. A.R.S. § 32-1451(D).
NOTICE OF HEARING
YOU ARE HEREBY NOTIFIED that a Formal Hearing on the Complaint
concerning License No. 14879 will be held before Administrative Law Judge Diane
Mihalsky on February 21, 2018, commencing at 9:00 a.m. at the Office of
Administrative Hearings located at 1740 W. Adams Street, Phoenix, Arizona and
continuing on successive days until concluded concerning the matters set forth in this
Complaint and Notice of Hearing, at which time and place, evidence, testimony and
argument in support of the charge set forth in the Complaint will be presented. A
‘transcript of the hearing, together with a written report of the findings, conclusions and
recommended decision of the Administrative Law Judge, will be submitted to the
Board for its consideration and determination of this matter. If the Board finds that
your conduct constitutes unprofessional conduct or that you are mentally or physically]
unable to safely practice medicine, you shall be subject to censure, probation,
‘suspension or revocation of your license, or any combination thereof, for such time,
including permanently, and under such conditions as the Board deems appropriate
and just, as provided in A.R.S. § 32-1451.
Within twenty (20) days of service of this Complaint and Notice of Hearing upon’
you, you are requested to file with the Board and the State’s attorney a written Answer|
to the Complaint. Your Answer should contain specific admission or denials of the
allegations of the Complaint, and may contain concise factual allegations, which you
contend constitute a ground or grounds for defense.
You are hereby notified that the Board may recover the costs of the formal hearin
pursuant to A.R.S. § 32-1451(M) if you are found to have committed the violations allege
herein.
You are further notified that, in the event you are found to have engaged in
unprofessional conduct as charged in this Complaint and Notice of Hearing, the Administrative’
Law Judge and the Board may consider any prior non-disciplinary and disciplinary action
against your license in determining an appropriate sanction in this matter pursuant to A.R.S. §
32-1451(U)
Pursuant to A.R.S. § 32-3206, you have the right to request a copy of the
following information from the Board:
1. Any review conducted by an expert or consultant providing an
evaluation of or opinion on the allegations.
2. Any records on the patient obtained by the board from other health
care providers.
3. The results of any evaluations or tests of the health professional
conducted at the board’s direction.
4. Any other factual information that the board will use in making its
determination.
Please be advised that if you obtain the above-referenced information from the’
board, you may not release it to any other person or entity or use it in any proceeding
or action except the administrative proceeding or appeals related to the administrative
proceeding. Violation of this restriction constitutes an act of unprofessional conduct
under A.R.S. § 32-3206(B).
Pursuant to A.R.S. § 41-1092.06, you have the right to request an informal
settlement conference by filing a written request with the Board no later than twenty’
(20) days before the scheduled hearing. The conference will be held within fifteen (15)
days after receipt of your request. Please note that you waive any right to object to the
participation of the Board's representative in the final administrative decision of the
matter if it is not settled at the conference.
The Office of Administrative Hearings requires that the following notice be
included in the Notice of Hearing:
hearing wil be Conducted through the Office of Adrinistrative
Hearings, an independent agency. Information regarding
procedures, practice pointers, or the online filing of motions is
available through the Office of Administrative Hearings
website at www.azoah.com.
DATED this _/ bo” say of January, 2018.
ARIZONA MEDICAL BOARD
oO
By: WAS be
Patricia E. McSorley
Executive Director
ORIGINAL of the foregoing filed
this \(.** day of January, 2018 with:
Arizona Medical Board
1740 W. Adams Street
Phoenix, AZ 85007
EXECUTED COPY of the foregoing mailed by U.S. mail, e-mail
and U.S. Certified Mail this |(s"*"day of January, 2018 to’
Gregory J Porter, M.D.
(Address of Record)
Respondent
EXECUTED COPY of the foregoing
Emailed this _) lo“ day of January, 2018 to
Greg Hanchett, Director
Office of Administrative Hearings
oahnoticesofhearing@azoah.com
COPIES of the foregoing Mailed/Emailed
this_\(:"* day of January, 2018 to:
Anne Froedge
Assistant Attorney General
SGDILES
15 S. 15" Avenue, 3° Floor South
Phoenix, AZ 85007-2997
Ht
wt
Courtesy copy to:
OTTMAR & ASSOC.
Court Reporters
Mose, \26te/
Arizona Medical Board Staff
#6745171
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Family's notice of claim in girl's death at Tucson schoolDocumento43 páginasFamily's notice of claim in girl's death at Tucson schoolKOLD News 13100% (1)
- Brent Brennan ContractDocumento5 páginasBrent Brennan ContractKOLD News 13Ainda não há avaliações
- Pima County Comments To Arizona DEQ About Copper WorldDocumento20 páginasPima County Comments To Arizona DEQ About Copper WorldKOLD News 13Ainda não há avaliações
- HLC Final ReportDocumento3 páginasHLC Final ReportKOLD News 13Ainda não há avaliações
- PCCEA Complaint To HLC - Oct 8 2022Documento2 páginasPCCEA Complaint To HLC - Oct 8 2022KOLD News 13100% (1)
- Notice of Claim Over Jail DeathsDocumento7 páginasNotice of Claim Over Jail DeathsKOLD News 13Ainda não há avaliações
- 1.18.24 Letter To DOJ Re Facial Recognition and Title VIDocumento6 páginas1.18.24 Letter To DOJ Re Facial Recognition and Title VILindsey BasyeAinda não há avaliações
- Gov. Hobbs Letter To Lawmakers About CRT BillDocumento2 páginasGov. Hobbs Letter To Lawmakers About CRT BillKOLD News 13Ainda não há avaliações
- Active Shooter Incidents in The Us 2022 042623Documento33 páginasActive Shooter Incidents in The Us 2022 042623KOLD News 13Ainda não há avaliações
- Autopsy Report For Wade WelchDocumento8 páginasAutopsy Report For Wade WelchKOLD News 13Ainda não há avaliações
- 2022-12-2 Cochise BOS ReferralDocumento3 páginas2022-12-2 Cochise BOS ReferralKOLD News 13Ainda não há avaliações
- Grijalva Letter To WH&DHS 5.12.2023Documento1 páginaGrijalva Letter To WH&DHS 5.12.2023KOLD News 13Ainda não há avaliações
- 2022-12-2 Cochise BOS ReferralDocumento3 páginas2022-12-2 Cochise BOS ReferralKOLD News 13Ainda não há avaliações
- 2022-11-28 Complaint For Special ActionDocumento53 páginas2022-11-28 Complaint For Special ActionKOLD News 13Ainda não há avaliações
- IARP News ReleaseDocumento13 páginasIARP News ReleaseKOLD News 13Ainda não há avaliações
- Letter To Pima County Board of SupervisorsDocumento3 páginasLetter To Pima County Board of SupervisorsKOLD News 13Ainda não há avaliações
- University of Arizona Public Case DecisionDocumento122 páginasUniversity of Arizona Public Case DecisionKOLD News 13Ainda não há avaliações
- Dervish Interim Complaint (Redacted)Documento2 páginasDervish Interim Complaint (Redacted)KOLD News 13Ainda não há avaliações
- Report Cards For Southern Arizona SchoolsDocumento12 páginasReport Cards For Southern Arizona SchoolsKOLD News 13Ainda não há avaliações
- 2022 08 30 State V City of Tucson ComplaintDocumento15 páginas2022 08 30 State V City of Tucson ComplaintKOLD News 13Ainda não há avaliações
- Search Warrant For Murad Can DervishDocumento14 páginasSearch Warrant For Murad Can DervishKOLD News 13Ainda não há avaliações
- PIO - San - Rafael 5 - 9Documento1 páginaPIO - San - Rafael 5 - 9KOLD News 13Ainda não há avaliações
- Response To BOR Oct-18-2022-122 Shipping Containers in YumaDocumento2 páginasResponse To BOR Oct-18-2022-122 Shipping Containers in YumaKOLD News 13Ainda não há avaliações
- 2022-07-22 Source of Income Ordinance (Redline)Documento3 páginas2022-07-22 Source of Income Ordinance (Redline)KOLD News 13Ainda não há avaliações
- TVUSD Statement - Gary Lewis, TVHS Athletic Director - April 1, 2022Documento1 páginaTVUSD Statement - Gary Lewis, TVHS Athletic Director - April 1, 2022KOLD News 13Ainda não há avaliações
- U.S. Department of Treasury Letter To ArizonaDocumento2 páginasU.S. Department of Treasury Letter To ArizonaKOLD News 13Ainda não há avaliações
- Pima County Vote Centers For Aug. 2, 2022 ElectionDocumento2 páginasPima County Vote Centers For Aug. 2, 2022 ElectionKOLD News 13Ainda não há avaliações
- 2022 Maui Invitational BracketDocumento1 página2022 Maui Invitational BracketKOLD News 13Ainda não há avaliações
- TVUSD Statement - Graffiti Incident, April 1, 2022Documento2 páginasTVUSD Statement - Graffiti Incident, April 1, 2022KOLD News 13Ainda não há avaliações
- Lawsuit Against Pima County Over Insurance Premiums For Unvaccinated EmployeesDocumento16 páginasLawsuit Against Pima County Over Insurance Premiums For Unvaccinated EmployeesKOLD News 13Ainda não há avaliações