Escolar Documentos
Profissional Documentos
Cultura Documentos
Forner Lancet 2012 Hccreview
Enviado por
api-283759086Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Forner Lancet 2012 Hccreview
Enviado por
api-283759086Direitos autorais:
Formatos disponíveis
Seminar
Hepatocellular carcinoma
Alejandro Forner, Josep M Llovet, Jordi Bruix
Hepatocellular carcinoma is the sixth most prevalent cancer and the third most frequent cause of cancer-related Lancet 2012; 379: 1245–55
death. Patients with cirrhosis are at highest risk of developing this malignant disease, and ultrasonography every Published Online
6 months is recommended. Surveillance with ultrasonography allows diagnosis at early stages when the tumour February 20, 2012
DOI:10.1016/S0140-
might be curable by resection, liver transplantation, or ablation, and 5-year survival higher than 50% can be achieved.
6736(11)61347-0
Patients with small solitary tumours and very well preserved liver function are the best candidates for surgical
Barcelona Clinic Liver Cancer
resection. Liver transplantation is most beneficial for individuals who are not good candidates for resection, especially group, Liver Unit, Hospital
those within Milano criteria (solitary tumour ≤5 cm and up to three nodules ≤3 cm). Donor shortage greatly limits its Clínic Barcelona, August Pi
applicability. Percutaneous ablation is the most frequently used treatment but its effectiveness is limited by tumour i Sunyer Biomedical Research
Institute, University of
size and localisation. In asymptomatic patients with multifocal disease without vascular invasion or extrahepatic
Barcelona, Barcelona, Spain
spread not amenable to curative treatments, chemoembolisation can provide survival benefit. Findings of randomised (A Forner MD, J M Llovet MD,
trials of sorafenib have shown survival benefits for individuals with advanced hepatocellular carcinoma, suggesting J Bruix MD); Centro de
that molecular-targeted therapies could be effective in this chemoresistant cancer. Research is active in the area of Investigación Biomédica en
Red de Enfermedades
pathogenesis and treatment of hepatocellular carcinoma.
Hepáticas y Digestivas,
Barcelona, Spain (A Forner,
Introduction than 50% of all cases.4 The relative risk of tumour J M Llovet, J Bruix); Mount Sinai
Hepatocellular carcinoma is the sixth most common development is about 100 in carriers of HBV versus non- Liver Cancer Program, Division
of Liver Diseases, Mount Sinai
neoplasm and the third most frequent cause of cancer carriers, and in HBV carriers with cirrhosis it is even
School of Medicine, New York,
death.1 More than 700 000 cases of this malignant disease higher.4,14 Incidence of hepatocellular carcinoma increases NY, USA (J M Llovet); and
were diagnosed in 2008, with an age-adjusted worldwide with viral load and duration of infection,15 suggesting an Institució Catalana de Recerca
incidence of 16 cases per 100 000 inhabitants.1 Hepato- accumulated risk of long-lasting oncogenic damage. Occult i Estudis Avançats, Barcelona,
Spain (J M Llovet)
cellular carcinoma is the leading cause of death among HBV infection is also associated with increased risk of
Correspondence to:
patients with cirrhosis.2 Here, we update our 2003 Lancet hepatocellular carcinoma because of DNA damage induced
Dr Jordi Bruix, Barcelona Clinic
Seminar3 to include major advances in prevention, by HBV integration.16,17 Hepatocellular carcinoma related Liver Cancer group, Liver Unit,
detection, diagnosis, and treatment that have happened to HBV can be prevented by vaccination. Nationwide IDIBAPS, Hospital Clínic,
since then. vaccination of infants in Taiwan reduced the incidence of Villarrel 170, 08036 Barcelona,
Spain
hepatocellular carcinoma in children aged 6–9 years from
jbruix@clinic.ub.es
Risk factors and prevention 0·52 per 100 000 for those born between 1974 and 1984 to
In most cases, hepatocellular carcinoma develops within 0·13 for those born between 1984 and 1986.18 If infection is
an established background of chronic liver disease chronic, viral replication can be abrogated by antiviral
(70–90% of all patients).4 The worldwide heterogeneous agents, which would prevent progression of liver disease
incidence reflects variations in the main risk factors and, possibly, hepatocellular carcinoma in the long term.19
(table 1).1,5 Most cases of hepatocellular carcinoma (80%) The incidence of hepatocellular carcinoma in individuals
arise in eastern Asia and sub-Saharan Africa, where the with HCV cirrhosis is 3–5% per year.20 Prevention of HCV
dominant risk factor is chronic infection with hepatitis B infection relies on avoidance of viral transmission through
virus (HBV), together with exposure to aflatoxin B1. By contaminated blood. Interruption of evolution from acute
contrast, in North America, Europe, and Japan, infection infection into chronic hepatitis and, ultimately, cirrhosis
with hepatitis C virus (HCV) is the main risk factor, by use of antiviral agents should prevent development of
together with alcohol use.6 Time trends in incidence of hepatocellular carcinoma.21,22 However, if cirrhosis is
hepatocellular carcinoma in developed countries parallel established, risk of hepatocellular carcinoma persists
the timing of HCV spread. In Japan and Europe, where despite antiviral treatment.21 Findings of initial studies
HCV infection spread earlier than in the USA, the suggested that interferon might prevent development of
incidence of hepatocellular carcinoma has almost reached hepatocellular carcinoma in patients with cirrhosis.23,24
a plateau and in some areas it is declining;5,7 however, in However, in randomised controlled trials, long-term
the USA, incidence is still increasing8,9 and the infection
could have a synergistic effect with other risk factors, such
as non-alcoholic fatty liver disease. Diabetes is an Search strategy and selection criteria
independent risk factor for hepatocellular carcinoma,6,10 We searched Medline, Embase, and the Cochrane Library (from January, 2000, to
and mortality rates for liver cancer are five times higher November, 2011) with the terms “hepatocellular carcinoma”, “liver cancer”, and “primary
among men with baseline body-mass index greater than liver carcinoma”. We also searched and reviewed the reference lists of retrieved
40, versus those with a lower body-mass index.11 Tobacco publications for other relevant papers. We only considered papers published in English
raises risk whereas coffee reduces it.12,13 and Spanish. We selected publications largely from the past 5 years, but we did not
The most frequent risk factor for hepatocellular carci- exclude commonly referenced and highly regarded older publications.
noma is chronic HBV infection, which accounts for more
www.thelancet.com Vol 379 March 31, 2012 1245
Seminar
(mammalian target of rapamycin) pathway is disrupted in
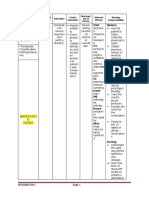
Age-adjusted Risk factors
incidence (x100 000; 40–50% of liver cancers owing to upstream signalling,
[men/women]) inactivation of the tumour suppressor PTEN, or mutations
Hepatitis C virus Hepatitis B virus Alcohol Others of phosphoinositide-3-kinase.32,33 Similarly, insulin-like
growth factor receptor 1 (IGF1R) signalling was active in
Europe ·· 60–70% 10–15% 20% 10%
20% of early hepatocellular carcinomas, and deregulation
Western 7·2/2·1 ·· ·· ·· ··
of the hepatocyte growth factor (HGF) and c-MET pathway
Southern 9·8/3·2 ·· ·· ·· ··
is a common event.29 Wingless (Wnt) signalling is
Northern 3·8/1·6 ·· ·· ·· ··
activated in a third of hepatocellular carcinomas, as a
North America 6·8/2·2 50–60% 20% 20% >10%
result of activating mutations in the transcription factor
Asia and Africa ·· 20% 70% 10% <10%
β catenin, overexpression of Wnt receptors, or inactivation
Eastern Asia 35·5/12·6 ·· ·· ·· ··
of E-cadherin. However, hepatocellular carcinoma is a
Southern Asia 13·9/5·1 ·· ·· ·· ·· highly vascularised cancer and angiogenic activity through
Central Africa 18·9/9·6 ·· ·· ·· ·· signalling of VEGFA, ANGPT2, and fibroblast growth
Data taken from references 1 and 5. factor (FGF) is a key event.28,29,34 Angiogenesis is complex
and has been reviewed elsewhere.28,29,34
Table 1: Age-adjusted incidence and risk factors for hepatocellular carcinoma worldwide, by
geographical area
Molecular classification of hepatocellular
carcinoma
treatment with interferon did not affect the rate of disease Molecular profiling is relevant in cancers such as those
progression and development of hepatocellular carcinoma of breast, lung, colon, and melanoma, and in some
in patients with chronic hepatitis C and advanced instances molecular subclasses and response to treatment
fibrosis.25,26 Alcohol is an important risk factor for are linked—eg, amplification of ERBB2 and response
development of hepatocellular carcinoma and exerts a to trastuzumab. Outcome prediction depends on both
synergistic effect in individuals with chronic infection tumour profiling (defining Wnt subclass, tumour growth
with HBV, HCV, or both.20 Patients who are co-infected factor β [TGF β], and epithelial cell adhesion molecule
with HIV and either HBV or HCV seem to have more [EPCAM] and inflammation class)29,35 and gene expression
rapidly progressive liver disease than patients without of adjacent non-tumoral tissue.36,37 Transfer of this infor-
HIV infection, and when they develop cirrhosis they are mation into treatment decision-making would need
also at increased risk of hepatocellular carcinoma.27 additional validation.
Molecular pathogenesis Surveillance and diagnosis
Hepatocarcinogenesis is a complex multistep process in Surveillance for hepatocellular carcinoma aims to reduce
which many signalling cascades are altered, leading to a disease-related mortality. In uncontrolled studies, survival
heterogeneous molecular profile.28,29 The main mutations seemed to be improved with surveillance but these studies
include the tumour suppressor gene TP53 (present in are affected by biases of lead time (the apparent
about 25–40% of cancers, depending on tumour stage), improvement in survival that comes from the diagnosis
and the gene for β catenin, CTNNB1 (about 25%, pre- being made early in the course of a disease) and length
dominantly in HCV-related hepatocellular carcinoma). time (the apparent improvement in survival that arises
Other mutations are less frequent. Chromosomal amplifi- because surveillance preferentially detects slow-growing
cations (1q, 6p, 8q, 17q, and 20q) and deletions (4q, 8p, 11q, cancers).38 One randomised controlled trial of surveillance
13q, 16q, and 17p) are common and affect important has been done in China (18 816 patients with hepatitis B) to
oncogenes and tumour suppressors. High-level amplifi- compare twice-yearly ultrasonography and measurement
cations have been described in 6p21 (VEGFA) and 11q13 of serum α-fetoprotein (AFP) concentration with no sur-
(cyclin D1 [CCND1]) in 5–10% of patients.28,29 Epigenetic veillance.39 Despite suboptimum adherence to surveillance
alterations are ill-defined in hepatocellular carcinoma, but (<60%), survival of screened participants was 66% at 1 year,
silencing of tumour suppressors (ie, RASSF1, SOCS1, 53% at 3 years, and 46% at 5 years versus 31%, 7%, and 0%,
E-cadherin [CDH1]) and reactivation of oncogenes (MYC) respectively, in unscreened patients. A validation trial in
have been shown.28,29 Finally, microRNA (miRNA) seems developed regions is not feasible: ultrasonography is part
to be able to modulate transcription of key oncogenes.30,31 of routine assessment for patients with liver disease and
As a result of these alterations, several signalling the perceived benefit from surveillance would impair
cascades related to cell survival and proliferation are recruitment of patients.40 Indeed, early detection and
activated and respond to targeted treatments in preclinical treatment of hepatocellular carcinoma is the sole option to
and early clinical studies. With respect to proliferation achieve long-term disease-free survival.
cascades, epithelial growth factor receptor (EGFR) and The decision to begin surveillance depends on the
Ras signalling is activated in more than 50% of degree of risk of hepatocellular carcinoma for the
hepatocellular carcinomas,29 whereas the MTOR individual and the extent to which he or she would be
1246 www.thelancet.com Vol 379 March 31, 2012
Seminar
treated if diagnosed with the malignant disease. Since no
experimental data to indicate the degree of risk that Mass on surveillance
ultrasonography in a
should trigger surveillance are available, the decision is <1 cm
patient with cirrhosis
>1 cm
based on cost-effectiveness models with heterogeneous or chronic hepatitis B
design. They all suggest that surveillance is cost effective
and that efficacy is dictated by incidence of hepatocellular
4-phase MDCT/dynamic MR
carcinoma.41,42 Accordingly, surveillance is recommended
both for patients with cirrhosis who would be treated
effectively if diagnosed with hepatocellular carcinoma Arterial hypervascularisation and
and for those with HBV infection but without cirrhosis, venous or delayed-phase washout
with an annual incidence of more than 0·2%.43 Individuals
with highly impaired liver function (Child-Pugh class C)
Repeat ultrasonography
should be assessed for liver transplantation. If this every 3 months Positive Negative
procedure cannot be offered surveillance is of no benefit
because diagnosis will not be followed by effective
treatment. Similarly, if liver function deteriorates and
prompts major decompensation not leading to assessment Stable over Enlarging Other imaging modality Biopsy
18–24 months (CT or MRI)
for transplantation, surveillance should be cancelled.
The preferred imaging method for surveillance is
ultrasonography; it is well tolerated and widely avail- Arterial hypervascularisation and
able, and it has sensitivity of 60–80% and specificity venous or delayed-phase washout
beyond 90%.44 The most used serological test is AFP.
Unfortunately, even with the most efficient cutoff
(10–20 μg/L), diagnostic sensitivity is around 60%.45–47
Positive Negative
Figures for surveillance are even worse and do not
Return to Proceed
support AFP as a surveillance test. Combined use of AFP
standard according to
and ultrasonography not only does not increase detection surveillance lesion size Treat as hepatocellular carcinoma
rates but also raises false-positive suspicions and cost.44,48
Other tumour markers, such as des-γ carboxiprothrombin Figure 1: Diagnostic algorithm for hepatocellular carcinoma
or AFP fractions, do not have better accuracy.46,47 Modified from reference 43, with permission of John Wiley and Sons. MDCT=multidetector CT.
On the basis of tumour-doubling times and data from MR=magnetic resonance.
the one available trial, screening of patients every
6 months is recommended. A 3-month interval increases ultrasonography is not recommended as the sole diagnostic
detection of small nodules but has no effect on survival,49 imaging technique because it cannot distinguish
and twice-yearly screening has better results than intrahepatic cholangiocarcinoma from hepatocellular
annual.50 Since tumour growth rate is not dictated by risk, carcinoma57,58 and MRI or CT is still needed for staging.
increased risk should not prompt a shorter interval. Non-invasive diagnostic criteria are valid only for
Figure 1 shows the diagnostic algorithm used once a investigation of screen-detected lesions in the liver in
nodule has been detected.43 Nodules 1 cm or smaller are patients with either cirrhosis or long-lasting chronic HBV
diagnosed infrequently as hepatocellular carcinoma and infection who might not have fully developed cirrhosis. In
are almost impossible to diagnose confidently by available other clinical scenarios, a diagnostic biopsy should be
techniques (biopsy could miss the target and the diagnostic requested. However, a negative finding after biopsy does
hypervascular profile is not in place at this stage). not rule out hepatocellular carcinoma since the false-
Furthermore, for these small lesions, pursuing a diagnosis negative rate can reach 30%54 because of sampling error or
of hepatocellular carcinoma would probably lead to more absence of specific histological hallmarks for diagnosis of
harm than benefit.51 When the nodule exceeds 1 cm, this cancer. A three-gene signature including glypican 3
diagnosis can be established by biopsy or by imaging in (GPC3), LYVE1, and survivin (BIRC5) has been proposed,59
the setting of liver cirrhosis. The specific imaging pattern but more tissue is needed with this method than for
is defined by intense contrast uptake during the arterial conventional immunohistochemical staining for GPC3,
phase followed by contrast washout during venous or glutamine synthetase, clathrin heavy chain, and heat-shock
delayed phases in a contrast-enhanced study such as CT or protein 70. This immunohistochemical panel provides
MRI (magnetic resonance is being validated extensively).52,53 100% specificity but still with suboptimum sensitivity.60
The value of these non-invasive criteria for hepatocellular
carcinoma in cirrhosis has been confirmed prospectively.54–56 Staging and prognosis assessment
In nodules of 1–2 cm, typical imaging features have Assessment of prognosis is a crucial step in management
specificities and predictive positive values of near 100% of patients with hepatocellular carcinoma. Years ago,
and sensitivity that can reach 71%. Contrast-enhanced most affected individuals were diagnosed at an advanced
www.thelancet.com Vol 379 March 31, 2012 1247
Seminar
symptomatic stage, when treatment was not feasible and and it is classified as such at explant. End-stage patients are
short-term prognosis was dismal. Diagnosis has now identified easily by any clinical method. They have a very
advanced, and effective early treatment of patients is poor prognosis and no intervention will be of benefit.
associated with median survival beyond 5 years. Any attempt Patients with end-stage liver disease (Child-Pugh C or
to assess prognosis should account for tumour stage, degree advanced Child-Pugh B) should be considered for trans-
of liver function impairment, and presence of cancer-related plantation, but recognition of hepatocellular carcinoma
symptoms.61 Several proposals have been raised to stratify could become a contraindication because of excessive
patients according to expected outcome.61 Some approaches tumour burden. Between these two extreme situations, the
do not take into account the presence of cancer-related clinical profile is very heterogeneous; liver function
symptoms that are major prognostic predictors.62–65 Others includes Child-Pugh classes A and B, and tumour burden
assess tumour burden roughly62 or investigate liver function encompasses liver-only disease without vascular invasion
according to the presence or absence of cirrhosis.66 This or extensive disease with metastatic spread. Patients can be
approach limits clinical usefulness. asymptomatic (performance status 0) or already have
The classification that stratifies patients according to cancer-related symptoms such as pain or malaise (per-
outcome and simultaneously links it with treatment formance status 1–2). As a result, the term non-surgical
indication is the Barcelona Clinic Liver Cancer (BCLC) hepatocellular carcinoma does not indicate any specific
strategy (figure 2). The BCLC classification has been clinical profile or prognosis. The BCLC classification68
validated in different settings and establishes treatment divides this heterogeneous group into two categories: the
recommendations for all stages of hepatocellular carci- intermediate stage (BCLC B), defined by absence of any
noma.67 Patients with early-stage cancer are treated by adverse predictor, and the advanced stage (BCLC C), which
resection, liver transplantation, or ablation, and prognosis includes patients with symptoms, vascular invasion,
can be refined for all these procedures according to extrahepatic spread, or a combination. The BCLC strategy
different variables. The very early stage (BCLC 0) corres- has been validated externally in prospective studies69 and
ponds to patients with well-preserved liver function (Child- has been endorsed by several scientific associations, but
Pugh A) diagnosed with one asymptomatic nodule of less further refinement is still needed. Liver function is
than 2 cm without vascular invasion or satellites. This assessed by the Child-Pugh classification, but class B
stage corresponds to the carcinoma-in-situ entity that, if includes a wide range of patients. Similarly, presence of
resected or ablated, would have excellent outcome with ascites within Child-Pugh class A indicates impaired
almost zero risk of recurrence. Currently, confident prognosis, which should be factored into individual
diagnosis is not feasible by imaging techniques or biopsy assessment of patients and treatment proposals.
Hepatocellular carcinoma
Very early stage (0) Early stage (A) Intermediate stage (B) Advanced stage (C) Terminal stage (D)
Single <2 cm Single or 3 nodules <3 cm Large multinodular Portal invasion Child-Pugh C
Child-Pugh A, PS 0 Child-Pugh A–B, PS 0 Child-Pugh A–B, PS 0 Extrahepatic spread PS 3–4
Child-Pugh A–B, PS 1–2
Potential candidate for Single Three nodules ≤3 cm
liver transplantation
No Yes Portal pressure, bilirubin
Normal Increased Associated diseases
No Yes
Ablation Resection Liver transplantation Ablation Chemoembolisation Sorafenib Best supportive care
Curative treatments Palliative treatments
Figure 2: BCLC staging and treatment strategy
The BCLC system establishes a prognosis in accordance with the five stages that are linked to first-line treatment recommendation. If the recommended option is not feasible because of an
individual patient’s condition, the treatment approach for the next evolutionary disease stage should be considered. Accordingly, patients in BCLC stage A may benefit from transarterial
chemoembolisation, BCLC B patients from sorafenib, and some patients in BCLC stage C with contraindications for sorafenib could enter research trials to assess new agents. BCLC=Barcelona Clinic
Liver Cancer. PS=performance status.
1248 www.thelancet.com Vol 379 March 31, 2012
Seminar
Biomarkers should enable better stratification. High
Benefit Level of evidence
AFP concentration is associated with a poor prognosis,
but no cutoff that would imply a modification in treatment Surgical treatments
decision has been defined. Other tumour markers do not Surgical resection Increases survival 3ii A
refine prognosis or justify their use for staging or Adjuvant treatments Controversial 1 A–D
treatment selection. The same applies for biomarkers Liver transplantation Increases survival 3ii A
such as VEGF, angiopoietin 2, or the proto-oncogene Adjuvant treatments Treatment response 3 Diii
c-Kit. They can refine prognostic prediction within Locoregional treatments
statistical modelling but cannot yet be incorporated into Percutaneous treatment Increases survival 3ii A
assessment of an individual patient. Radiofrequency Increases survival 1ii A
Other modalities Treatment response 2D
Treatment Combined modalities Treatment response 3ii D
For treatment to be most effective, patients should be Chemoembolisation Increases survival 1ii A
selected carefully and the treatment applied skilfully. In Internal radiotherapy (iodine-131, yttrium-90) Treatment response 3ii Diii
view of the complexity of hepatocellular carcinoma and Systemic treatments
the many potentially useful treatments, patients diag- Sorafenib Increases survival 1i A
nosed with this malignant disease should be referred Hormonal compounds No survival benefit 1i A
to multidisciplinary teams that include hepatologists, Tamoxifen ..
radiologists, surgeons, pathologists, and oncologists. By Antiandrogen ..
contrast with other highly prevalent cancers, the level of Seocalcitiol ..
evidence for most therapeutic options for hepatocellular Systemic chemotherapy No survival benefit 1i A
carcinoma is restricted to cohort investigations with a few Immunotherapy No survival benefit 1ii A
randomised controlled trials, most of which addressed
Modified from reference 70, with permission of Oxford University Press. Evidence-based classification adapted from
treatment of advanced disease (table 2).70 Furthermore, as
the National Cancer Institute. 1=randomised controlled trial or meta-analysis (1i=double-blinded, 1ii=non-blinded).
far as we know, no large robust studies have been done to 2=non-randomised controlled trial. 3=case series (3i=population-based, 3ii=non-population-based, consecutive,
compare treatments regarded as potentially curative for 3iii=non-population-based, non-consecutive). A=survival endpoint. B=cause-specific mortality. C=quality of life.
early-stage disease (surgical resection, transplantation, D=indirect surrogates (Di=disease-free survival, Dii=progression-free survival, Diii=tumour response).
percutaneous ablation), and no studies have compared Table 2: Evidence-based benefits of treatments
these methods with no treatment. Surgical resection,
transplantation, and ablation are treatments that offer a
high rate of complete responses and, thus, potential for retention rate is used to identify the best candidates for For the National Cancer
cure.43 The only non-curative treatments that improve resection,81 whereas portal pressure and bilirubin are the Institute see http://www.
cancer.gov
survival are transarterial chemoembolisation and sora- variables used in Europe and the USA.43 Clinically relevant
fenib.71–73 Arterial embolisation without chemotherapy,71 portal hypertension is defined as a hepatic vein pressure
external radiotherapy,74,75 and radioembolisation have gradient greater than 10 mm Hg, but it can also be
shown antitumour activity,76–78 but survival benefit has not confirmed by oesophageal varices or splenomegaly
been proven. Systemic chemotherapy has marginal associated with a platelet count lower than 100×10⁹/L. In
activity with frequent toxic effects, without survival patients without relevant portal hypertension and normal
benefit, and agents such as tamoxifen, octreotide, or concentrations of bilirubin, survival at 5 years is 70%,
antiandrogens are completely ineffective.43,71 whereas it is 50% for individuals with portal hypertension
and is even lower when both adverse factors are present.82,83
Resection With respect to the best candidates for resection, blood
Hepatic resection is the treatment of choice for transfusion will be needed in fewer than 10% of cases, and
hepatocellular carcinoma in individuals without cirrhosis treatment-related mortality should be less than 1%.
(5% of patients in the USA and Europe, 40% in Asia). Therefore, assessment of portal pressure is crucial for
These patients tolerate major resections with low rates of prediction of long-term survival.43
life-threatening complications. In individuals with Most groups restrict the indication for resection to
cirrhosis, careful selection of candidates is vital to avoid patients with one tumour, because multifocality is
treatment-related complications—eg, liver failure with associated with high recurrence and impaired survival.
increased risk of death. Although multifocality need not be viewed as a contra-
For years, selection of candidates for resection has been indication to resection, careful assessment to estimate
based on the Child-Pugh classification,79 but this strategy survival (and associated risks) that might be offered by
has inconsistent predictive value. Some Child-Pugh A other options, such as transplantation, ablation,84 or
patients already have liver functional impairment with chemoembolisation,85–87 is mandatory. Tumour size is not
raised bilirubin concentrations, clinically significant portal a clear-cut limiting factor, but risk of vascular invasion
hypertension, or even minor fluid retention necessitating and dissemination increases with diameter. Malignant
diuretic treatment.80 In Japan, the indocyanine green vascular invasion should be viewed as a contraindication
www.thelancet.com Vol 379 March 31, 2012 1249
Seminar
for resection. By application of these restrictive criteria, transarterial chemoembolisation) are done, even though
the proportion of patients in whom resection can be effectiveness is unproven.99 Policies for transplantation
offered is 5–10%. are implemented that aim to prioritise the sickest
Tumour recurrence complicates 70% of cases at 5 years, patients,52,100 but the only effective method to avoid waiting
combining true recurrence, which usually arises within is to increase the number of donations. Live donation is a
the first 2 years after resection, and de novo tumours.81 valid strategy, with outcomes similar to those of cadaveric
Microvascular invasion, poor histological differentiation, donation, but applicability is reduced because of societal
satellites, and multifocal disease predict early recurrence.81,88 constraints and, scarcity of appropriate donors.
Late recurrence depends mainly on the carcinogenic effect Despite the shortage of liver donors, several researchers
of underlying chronic liver disease.36 This risk can be have proposed expansion of current limits.101–105 Most
estimated by liver function variables related to inflammatory suggestions are based on analysis of tumour stage in the
activity, evolutionary stage, or both. No effective neoadjuvant explanted liver and not on imaging findings at the time of
or adjuvant treatment options to reduce risk of recurrence the patient’s assessment. Furthermore, transplantation to
are available. Systemic chemotherapy and chemoembol- patients who do not meet the Milano criteria is associated
isation have no effect, whereas immunotherapy, retinoids, with increased prevalence of variables associated with risk
and interferon have shown some potential efficacy, but of recurrence (microscopic vascular invasion or satellites).
evidence is not strong enough for them to be used in If the number of livers available exceeded the number of
clinical practice.81 Findings of meta-analyses have candidates for transplantation, a slight expansion would
reinforced the benefits of interferon but heterogeneity of be feasible because it would not negatively affect patients
the interferon used, the duration of the regimen, the with the best transplant profiles.106 The MTOR inhibitor
patients recruited, and trial endpoints prevent valid assess- sirolimus seemed to improve tumour-free survival in
ment.89–91 The most effective option to prevent intrahepatic recipients of liver transplants with a pre-transplantation
recurrence is liver transplantation. Although post-resection diagnosis of hepatocellular carcinoma in preliminary
recurrence affects more than 70% of patients at 5 years in studies, but this hypothesis should be confirmed in a trial
those with a risky profile, it affects fewer than 25% of due to finish in 2014.107
individuals treated by transplantation. Transplantation can,
therefore, be offered to patients initially treated by resection Image-guided tumour ablation
but with a high risk of recurrence according to pathological Image-guided tumour ablation is now a conventional
analysis. This policy not only allows some individuals to be treatment option for patients with early-stage hepato-
treated effectively by resection with avoidance of trans- cellular carcinoma. Ablation induces tumour necrosis by
plantation but also permits best use of the few organs that injection of chemicals (eg, ethanol, acetic acid) or
are available by offering transplantation to patients whose temperature modification (ablation by radiofrequency,
cancer would recur after resection.92 microwave, or laser, or cryoablation). Although tumour
ablation can be undertaken at laparoscopy or surgery, most
Liver transplantation procedures are done percutaneously. The first-line
Hepatocellular carcinoma is the only solid cancer that can technique is now radiofrequency ablation.108 Both ethanol
be treated by liver transplantation, which has completely injection and radiofrequency ablation achieve complete
changed the treatment strategy for this malignant disease. necrosis of almost 100% in hepatocellular carcinomas
In theory, transplantation could simultaneously cure the smaller than 2 cm, but the effectiveness of ethanol injection
tumour and underlying cirrhosis, and effectiveness of the falls in larger tumours, in which radiofrequency ablation
procedure is not affected by the degree of liver function can still be highly effective. Effectiveness diminishes in
impairment. Mazzaferro and colleagues93 showed that larger lesions, and ablation is not recommended for
selection of patients with one hepatocellular carcinoma of tumours larger than 5 cm. Better disease control with
5 cm or smaller, or up to three nodules of 3 cm or smaller, radiofrequency ablation than with ethanol injection could
without vascular invasion or extrahepatic spread (known translate into better outcomes.109–111 Side-effects are more
as the Milano criteria) offered 4-year survival of 75%, with frequent after radiofrequency ablation than after other
recurrence rates below 15%. These results have been approaches and some tumour locations (subcapsular,
validated82,94,95 and are accepted as the benchmark for vicinity of major blood vessels or biliary tree, near to bowel
selection of patients in the USA and Europe.43,96,97 or heart) should be avoided.112 Novel techniques such as
These excellent results were achieved in an era with microwave or electroporation are being evaluated.108
prompt availability of organs. The shortage of donors has Survival after ablation in Child-Pugh A patients is
imposed a delay before transplantation, and during this 50–75% at 5 years, thus paralleling the outcome after
period the tumour can progress and impede trans- surgical resection.108–111 This finding has challenged resec-
plantation.98 This delay impairs the effectiveness of liver tion as the first-line treatment in patients with small
transplantation when considered according to intention solitary hepatocellular carcinomas. Ablation has been
to treat.82 When waiting time exceeds 6 months, treatments compared with resection in early hepatocellular carcinoma
aimed at delaying tumour progression (eg, ablation, in several randomised controlled trials, but the results
1250 www.thelancet.com Vol 379 March 31, 2012
Seminar
have varied.113–115 However, these trials had some limitations trials that found improved survival because of risk of bias
in terms of sample size, and concerns have been raised in (according to Cochrane criteria).117,121 Finally, the Cochrane
some instances about randomisation, treatment allo- analysis had very stringent expectations for survival
cation, and trial implementation; further studies under- improvement (10%).
taken in the USA and Europe are needed urgently. After initial success with transarterial chemoembol-
A specific scenario for ablation is the very early stage of isation, treated tumours are revascularised and can be
hepatocellular carcinoma. Ablation is nearly 100% effective re-treated. However, in the long term, the capacity to keep
in hepatocellular carcinomas smaller than 2 cm and the cancer under control is lost. Development of poly-
survival is almost identical after resection or ablation. vinylalcohol spheres that provide a calibrated vessel
Thus, if transplantation is not an option, ablation would obstruction with slow release of chemotherapeutic agents
become the first-line option and surgery would be justified has allowed the procedure to be standardised while
only in patients with failure of or contraindication to maintaining effectiveness and reducing drug-related
ablation. However, if the strategy of transplantation owing adverse events.122 In current trials, researchers are
to risk of recurrence as per tumour pathology is in place, investigating whether the combination of transarterial
patients who could benefit from transplantation should chemoembolisation with molecular-targeted agents might
still have resection as the first-line approach. Analysis of delay tumour progression after treatment and, ultimately,
resected tumour would distinguish between very early improve survival. Median survival in old series was almost
hepatocellular carcinoma (BCLC 0) with marginal risk of 2 years but, with better selection criteria and optimum
recurrence (thus, no need to consider transplantation) and treatment delivery, median survival exceeds 3 years.85–87
more advanced malignant disease with presence of Therefore, the best candidates for transarterial chemo-
microscopic vascular invasion or satellites that indicate embolisation are patients with compensated Child-Pugh A
transplantation because of high risk of recurrence. This with asymptomatic multifocal or large hepatocellular
change represents a major alteration in BCLC decision- carcinomas not amenable to resection (ie, BCLC stage B).
making, as described in figure 2, because patients Portal vein thrombosis, even if segmental, is a predictor
diagnosed at a very early stage would be considered for of poor tolerability and impaired outcome.123
resection only if a transplant were available. In the future, Radioembolisation with yttrium-90 (Yt⁹⁰)-labelled
imaging techniques or molecular profiling might spheres has much potential, and findings show anti-
distinguish between these two evolutionary tumour stages tumour activity,76–78 but without randomised controlled
and decide between ablation and transplantation without trials to compare this option with any other established
need for resection with pathological assessment. treatment, definition of its role in clinical practice is not
feasible. Validation of safety and effectiveness in different
Image-guided transcatheter tumour treatment cohort studies could indicate its target population.
Image-guided transcatheter treatments are based on
selective intravascular delivery of drugs into arterial Sorafenib
vessels nourishing the tumour, and are considered in Until lately, no effective treatment was available for patients
patients with large cancers or multifocal disease that is diagnosed at advanced stage or who progressed into an
not amenable to curative treatments. Chemotherapeutic advanced stage after other treatments failed. Knowledge of
drugs, embolic particles, or radioactive materials can be molecular events that govern tumour progression and
injected and induce tumour necrosis.108 The only option
that has shown survival benefit116,117 is transarterial chemo- 100 Sorafenib
embolisation. It combines injection of chemotherapeutic Placebo
agents with obstruction of arterial blood supply. More
than 50% of patients have an objective response, as shown 75
Proportion surviving (%)
by extensive tumour necrosis, which translates into
improved survival.71 In a recent meta-analysis, evidence
50 p=0·0001
supporting the benefits of transarterial chemoembolisation
was defined as still limited.118 However, this Cochrane
analysis had several controversial features. It included a 25
randomised controlled trial undertaken in patients with
early hepatocellular carcinoma, in whom transarterial
embolisation (not chemoembolisation) was assessed in 0
0 8 16 24 32 40 48 56 64 72 80
combination with standard treatment for those patients
Weeks
(ablation by ethanol injection or radiofrequency ablation). Number at risk
It also included a trial using absorbable gelatin powder Sorafenib 299 274 241 205 161 108 67 38 12 0 0
Placebo 303 276 224 179 126 78 47 25 7 2 0
with short follow-up that showed poor 1-year survival119 (a
characteristic shared by the most recent investigation)120 Figure 3: Overall survival of patients with advanced hepatocellular carcinoma assigned sorafenib or placebo
without extended follow-up. Furthermore, it excluded two Adapted from reference 72 with permission of the Massachusetts Medical Society.
www.thelancet.com Vol 379 March 31, 2012 1251
Seminar
602 patients, median overall survival in the sorafenib group
Llovet (2008)72 Cheng (2009)73
was 10·7 months (95% CI 9·4–13·3) versus 7·9 months
Sorafenib 800 mg Placebo Sorafenib 800 mg Placebo (6·8–9·1) in the placebo group (hazard ratio 0·69, 95% CI
per day (n=303) (n=299) per day (n=150) (n=76)
0·55–0·87; p=0·0001; figure 3). Survival benefit was
Response rate .. .. .. .. preceded by a delay in time to progression: 5·5 months for
Complete response 0 0 0 0 sorafenib versus 2·8 months for placebo (0·58, 0·45–0·74;
Partial response 7 2 5 1 p<0·001).72 The two groups did not differ in median time
Stable disease 211 204 81 21 to symptomatic progression (4·1 months vs 4·9 months;
Progressive disease .. .. 46 41 p=0·77). The overall incidence of treatment-related adverse
Time to progression (months) 5·5 2·8 2·8 1·4 events (predominantly grade 1 or 2 in severity) was 80% in
Hazard ratio (95% CI) 0·58 (0·45–0·74) .. 0·57 (0·42–0·79) .. the sorafenib group and 52% in the placebo group.
Median survival (months) 10·7 7·9 6·5 4·2 Most frequent adverse events were gastrointestinal,
Hazard ratio (95% CI) 0·69 (0·55–0·87) .. 0·68 (0·50–0·93) .. constitutional, and dermatological in nature. Treatment
interruption owing to side-effects was recorded in 38% of
Data are number of patients, unless otherwise stated.
treated patients versus 37% in controls. These findings
Table 3: Phase 3 clinical trials of sorafenib in patients with advanced hepatocellular carcinoma have been replicated by a randomised controlled trial in
Asia (table 3),73 and safety data were reproduced in a large
phase 4 study of sorafenib in more than 1500 patients.124
Control Phase Identifier*
These results have established sorafenib as the standard of
Adjuvant treatment after resection or ablation care for advanced hepatocellular carcinoma43,125 and have
Sorafenib Placebo 3 NCT00692770 paved the way for development of combination or
Adjuvant treatment after transarterial chemoembolisation sequential strategies to improve the effectiveness of
Sorafenib Placebo 2 NCT00855218 sorafenib as one agent. Several trials are underway (table 4).
Brivanib Placebo 3 NCT00908752 The key issue in early development phases was how to
First-line treatment in advanced hepatocellular carcinoma assess potential effectiveness and to proceed to phase 3
Sorafenib and erlotinib Sorafenib 3 NCT00901901 trials. In all studies with sorafenib so far, survival is
Sorafenib and doxorubicin Sorafenib 3 NCT01015833 improved in the absence of treatment response, according
Sorafenib and C1008 Sorafenib 2 NCT01033240 to conventional definitions.126 New criteria based on
Sorafenib and mapatumumab Sorafenib 2 NCT01258608 biomarkers or functional imaging will have to be developed
Sorafenib and BIBF-1120 Sorafenib 2 NCT01004003 for assessment of efficacy. Until then, the potential
Sorafenib and oxaliplatin and capecitabine Sorafenib 3 NCT01245582 effectiveness of novel agents will have to rely on time to
Sorafenib and bevacizumab Sorafenib 2 NCT00867321 progression, which also marks the time for recruitment of
Bevacizumab and erlotinib Sorafenib 2 NCT00881751 patients into trials to assess the efficacy of novel agents
Brivanib Sorafenib 3 NCT00858871 beyond sorafenib.70 Some attempts will fail, as has
Dovitinib Sorafenib 2 NCT01232296 happened for sunitinib. This drug had a similar molecular
Linifanib (ABT-869) Sorafenib 3 NCT01009593 profile to sorafenib but the trial was interrupted because of
Second-line treatment in advanced hepatocellular carcinoma
futility and safety concerns.127 Others could be positive and,
Brivanib Placebo 3 NCT00825955
hence, changes in management of advanced hepatocellular
ARQ197 Placebo 2 NCT00988741
carcinoma might be introduced in coming years.
Axitinib Placebo 2 NCT01210495
Ramucirumab Placebo 3 NCT01140347
Future perspectives
Treatment of hepatocellular carcinoma has changed greatly
Everolimus Placebo 3 NCT01035229
within the past decade and has become a major area for
OSI-906 Placebo 2 NCT01101906
research. Patients diagnosed with this malignant disease
*From http://www.clinicaltrials.gov. can benefit from effective options that will improve their
survival, whatever the evolutionary stage at which they
Table 4: Randomised phase 2 and 3 multicentre trials in progress
have been diagnosed. Obviously, improvement in several
areas is still needed. Recurrence after ablation or resection
dissemination has allowed development of targeted is a major drawback, and effective preventive agents are
treatments that aim to abrogate these disrupted pathways. needed. Also, progression after effective chemoembolisation
Several drugs are under development, but the only one is an area in which any positive strategy should result in
with proven survival benefit is sorafenib.72,73 This agent, relevant benefit. Finally, identification of novel targets and
which can be administered orally, is a multikinase inhibitor predictors through molecular cell biology will identify new
that blocks Raf signalling and VEGF, PDGF, and c-Kit. therapeutic strategies for advanced stage hepatocellular
It has antiproliferative and antiangiogenic activity and carcinoma and provide better methods for outcome
delays tumour progression. In our phase 3, multicentre, prediction. For that reason, collection of tissue samples
randomised, double-blind, placebo-controlled trial of should be considered in research studies. Molecular
1252 www.thelancet.com Vol 379 March 31, 2012
Seminar
biology data might offer the insight to abrogate malignant 16 Brechot C, Thiers V, Kremsdorf D, Nalpas B, Pol S,
transformation within cirrhotic livers. For these advances Paterlini-Brechot P. Persistent hepatitis B virus infection in subjects
without hepatitis B surface antigen: clinically significant or purely
to take place, continuing active clinical and experimental “occult”? Hepatology 2001; 34: 194–203.
research is essential. Only by combination of all areas of 17 Chen JD, Yang HI, Iloeje UH, et al. Carriers of inactive hepatitis B
expertise will these hopes be realised. virus are still at risk for hepatocellular carcinoma and liver-related
death. Gastroenterology 2010; 138: 1747–54.
Contributors 18 Chang MH, Chen CJ, Lai MS, et al, for the Taiwan Childhood
AF did the literature research. All authors wrote the Seminar and have Hepatoma Study Group. Universal hepatitis B vaccination in
reviewed and approved the final version. Taiwan and the incidence of hepatocellular carcinoma in children.
N Engl J Med 1997; 336: 1855–59.
Conflicts of interest
19 Papatheodoridis GV, Lampertico P, Manolakopoulos S, Lok A.
AF has received consultancy and lecture fees from Bayer Schering
Incidence of hepatocellular carcinoma in chronic hepatitis B
Pharma. JML has received grant support, consultancy fees, or both from patients receiving nucleos(t)ide therapy: a systematic review.
Bayer Schering Pharma, Bristol-Myers Squibb, Biocompatibles, J Hepatol 2010; 53: 348–56.
Biosphere, Novartis, Imclone, Jennerex, Abbott, and OSI. JB has received 20 Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular
grant support, consultancy fees, or both from Bayer Schering Pharma, carcinoma in cirrhosis: incidence and risk factors. Gastroenterology
Bristol-Myers Squibb, Biocompatibles, Terumo, Novartis, Schering 2004; 127: S35–50.
Plough, Eisai, Arqule, Angiodynamics, Kowa, GlaxoSmithKline, 21 Bruno S, Stroffolini T, Colombo M, et al. Sustained virological
Sumitomo, Lilly, and OSI. response to interferon-alpha is associated with improved outcome
Acknowledgments in HCV-related cirrhosis: a retrospective study. Hepatology 2007;
45: 579–87.
The Barcelona Clinic Liver Cancer (BCLC) is funded through the Spanish
Biomedical Research Network (CIBER) for the area of Hepatic and 22 Singal AK, Singh A, Jaganmohan S, et al. Antiviral therapy reduces
risk of hepatocellular carcinoma in patients with hepatitis C
Digestive disorders. This work was supported partly by grants from the
virus-related cirrhosis. Clin Gastroenterol Hepatol 2010; 8: 192–99.
Instituto de Salud Carlos III (PI 08/0146). JML has received grants from
23 Yoshida H, Shiratori Y, Moriyama M, et al, for the IHIT Study
the US National Institutes of Health-NIDDK 1R01DK076986-01, National
Group. Interferon therapy reduces the risk for hepatocellular
Institute of Health (Spain) grant I+D Program (SAF-2007-61898), and the carcinoma: national surveillance program of cirrhotic and
Samuel Waxman Cancer Research Foundation. noncirrhotic patients with chronic hepatitis C in Japan.
References Ann Intern Med 1999; 131: 174–81.
1 Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. 24 Imai Y, Kawata S, Tamura S, et al. Relation of interferon therapy
Estimates of worldwide burden of cancer in 2008: GLOBOCAN and hepatocellular carcinoma in patients with chronic hepatitis C.
2008. Int J Cancer 2010; 127: 2893–917. Ann Intern Med 1998; 129: 94–99.
2 Alazawi W, Cunningham M, Dearden J, Foster GR. Systematic 25 Di Bisceglie AM, Shiffman ML, Everson GT, et al. Prolonged
review: outcome of compensated cirrhosis due to chronic hepatitis therapy of advanced chronic hepatitis C with low-dose
C infection. Aliment Pharmacol Ther 2010; 32: 344–55. peginterferon. N Engl J Med 2008; 359: 2429–41.
3 Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet 26 Bruix J, Poynard T, Colombo M, et al. Maintenance therapy with
2003; 362: 1907–17. peginterferon alfa-2b does not prevent hepatocellular carcinoma in
4 Sherman M. Hepatocellular carcinoma: epidemiology, surveillance, cirrhotic patients with chronic hepatitis C. Gastroenterology 2011;
and diagnosis. Semin Liver Dis 2010; 30: 3–16. 140: 1990–99.
5 Bosetti C, Levi F, Boffetta P, Lucchini F, Negri E, La Vecchia C. 27 MacDonald DC, Nelson M, Bower M, Powles T. Hepatocellular
Trends in mortality from hepatocellular carcinoma in Europe, carcinoma, human immunodeficiency virus and viral hepatitis in
1980–2004. Hepatology 2008; 48: 137–45. the HAART era. World J Gastroenterol 2008; 14: 1657–63.
6 El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011; 28 Farazi PA, DePinho RA. Hepatocellular carcinoma pathogenesis:
365: 1118–27. from genes to environment. Nat Rev Cancer 2006; 6: 674–87.
7 Qiu D, Katanoda K, Marugame T, Sobue T. A Joinpoint regression 29 Villanueva A, Newell P, Chiang DY, Friedman SL, Llovet JM.
analysis of long-term trends in cancer mortality in Japan Genomics and signaling pathways in hepatocellular carcinoma.
(1958–2004). Int J Cancer 2009; 124: 443–48. Semin Liver Dis 2007; 27: 55–76.
8 Tanaka Y, Kurbanov F, Mano S, et al. Molecular tracing of the global 30 Ji J, Shi J, Budhu A, et al. MicroRNA expression, survival, and
hepatitis C virus epidemic predicts regional patterns of hepatocellular response to interferon in liver cancer. N Engl J Med 2009; 361: 1437–47.
carcinoma mortality. Gastroenterology 2006; 130: 703–14. 31 Toffanin S, Hoshida Y, Lachenmayer A, et al. MicroRNA-based
9 Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging classification of hepatocellular carcinoma and oncogenic role of
of hepatitis C virus (HCV)-infected persons in the United States: miR-517a. Gastroenterology 2011; 140: 1618–28.
a multiple cohort model of HCV prevalence and disease 32 Villanueva A, Chiang DY, Newell P, et al. Pivotal role of mTOR
progression. Gastroenterology 2010; 138: 513–21. signaling in hepatocellular carcinoma. Gastroenterology 2008;
10 El-Serag HB, Tran T, Everhart JE. Diabetes increases the risk 135: 1972–83.
of chronic liver disease and hepatocellular carcinoma. 33 Sahin F, Kannangai R, Adegbola O, Wang J, Su G, Torbenson M.
Gastroenterology 2004; 126: 460–68. mTOR and P70 S6 kinase expression in primary liver neoplasms.
11 Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, Clin Cancer Res 2004; 10: 8421–25.
obesity, and mortality from cancer in a prospectively studied cohort 34 Fernandez M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J.
of US adults. N Engl J Med 2003; 348: 1625–38. Angiogenesis in liver disease. J Hepatol 2009; 50: 604–20.
12 Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. 35 Hoshida Y, Nijman SM, Kobayashi M, et al. Integrative
Alcohol, tobacco and obesity are synergistic risk factors for transcriptome analysis reveals common molecular subclasses of
hepatocellular carcinoma. J Hepatol 2005; 42: 218–24. human hepatocellular carcinoma. Cancer Res 2009; 69: 7385–92.
13 Bravi F, Bosetti C, Tavani A, La Vecchia C. Coffee drinking and 36 Hoshida Y, Villanueva A, Kobayashi M, et al. Gene expression in
hepatocellular carcinoma: an update. Hepatology 2009; fixed tissues and outcome in hepatocellular carcinoma.
50: 1317–18. N Engl J Med 2008; 359: 1995–2004.
14 Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular 37 Villanueva A, Hoshida Y, Battiston C, et al. Combining clinical,
carcinoma and hepatitis B virus: a prospective study of 22 707 men pathology, and gene expression data to predict recurrence of
in Taiwan. Lancet 1981; 318: 1129–33. hepatocellular carcinoma. Gastroenterology 2011; 140: 1501–12.
15 Chen CJ, Yang HI, Su J, et al. Risk of hepatocellular carcinoma 38 Croswell JM, Ransohoff DF, Kramer BS. Principles of cancer
across a biological gradient of serum hepatitis B virus DNA level. screening: lessons from history and study design issues.
JAMA 2006; 295: 65–73. Semin Oncol 2010; 37: 202–15.
www.thelancet.com Vol 379 March 31, 2012 1253
Seminar
39 Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of 62 A new prognostic system for hepatocellular carcinoma:
screening for hepatocellular carcinoma. J Cancer Res Clin Oncol a retrospective study of 435 patients: the Cancer of the Liver Italian
2004; 130: 417–22. Program (CLIP) investigators. Hepatology 1998; 28: 751–55.
40 Poustchi H, Farrell G, Strasser S, Lee A, McCaughan G, George J. 63 Tateishi R, Yoshida H, Shiina S, et al. Proposal of a new prognostic
Feasibility of conducting a randomised control trial for liver cancer model for hepatocellular carcinoma: an analysis of 403 patients.
screening: is a randomized controlled trial for liver cancer Gut 2005; 54: 419–25.
screening feasible or still needed? Hepatology 2011; 54: 1998–2004. 64 Kudo M, Chung H, Osaki Y. Prognostic staging system for
41 Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening hepatocellular carcinoma (CLIP score): its value and limitations,
for detection of small hepatocellular carcinoma in western patients and a proposal for a new staging system, the Japan Integrated
with Child-Pugh class A cirrhosis. Am J Med 1996; 101: 422–34. Staging Score (JIS score). J Gastroenterol 2003; 38: 207–15.
42 Arguedas MR, Chen VK, Eloubeidi MA, Fallon MB. Screening for 65 Hsu CY, Huang YH, Hsia CY, et al. A new prognostic model for
hepatocellular carcinoma in patients with hepatitis C cirrhosis: hepatocellular carcinoma based on total tumor volume: the Taipei
a cost-utility analysis. Am J Gastroenterol 2003; 98: 679–90. Integrated Scoring System. J Hepatol 2010; 53: 108–17.
43 Bruix J, Sherman M. Management of hepatocellular carcinoma: 66 Vauthey JN, Lauwers GY, Esnaola NF, et al. Simplified staging
an update. Hepatology 2011; 53: 1020–22. for hepatocellular carcinoma. J Clin Oncol 2002; 20: 1527–36.
44 Singal A, Volk ML, Waljee A, et al. Meta-analysis: surveillance with 67 Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma:
ultrasound for early-stage hepatocellular carcinoma in patients with the BCLC staging classification. Semin Liver Dis 1999; 19: 329–38.
cirrhosis. Aliment Pharmacol Ther 2009; 30: 37–47. 68 Llovet JM, Bustamante J, Castells A, et al. Natural history of untreated
45 Trevisani F, D’Intino PE, Morselli-Labate AM, et al. Serum nonsurgical hepatocellular carcinoma: rationale for the design and
alpha-fetoprotein for diagnosis of hepatocellular carcinoma in evaluation of therapeutic trials. Hepatology 1999; 29: 62–67.
patients with chronic liver disease: influence of HBsAg and 69 Cabibbo G, Enea M, Attanasio M, Bruix J, Craxi A, Camma C.
anti-HCV status. J Hepatol 2001; 34: 570–75. A meta-analysis of survival rates of untreated patients in randomized
46 Marrero JA, Feng Z, Wang Y, et al. Alpha-fetoprotein, des-gamma clinical trials of hepatocellular carcinoma. Hepatology 2010; 51: 1274–83.
carboxyprothrombin, and lectin-bound alpha-fetoprotein in early 70 Llovet JM, Di Bisceglie AM, Bruix J, et al. Design and endpoints of
hepatocellular carcinoma. Gastroenterology 2009; 137: 110–18. clinical trials in hepatocellular carcinoma. J Natl Cancer Inst 2008;
47 Lok AS, Sterling RK, Everhart JE, et al. Des-gamma-carboxy 100: 698–711.
prothrombin and alpha-fetoprotein as biomarkers for the early detection 71 Llovet JM, Bruix J. Systematic review of randomized trials for
of hepatocellular carcinoma. Gastroenterology 2010; 138: 493–502. unresectable hepatocellular carcinoma: chemoembolization
48 Zhang B, Yang B. Combined alpha fetoprotein testing and improves survival. Hepatology 2003; 37: 429–42.
ultrasonography as a screening test for primary liver cancer. 72 Llovet J, Ricci S, Mazzaferro V, et al. Sorafenib in advanced
J Med Screen 1999; 6: 108–10. hepatocellular carcinoma. N Engl J Med 2008; 359: 378–90.
49 Trinchet J-C, Chaffaut C, Bourcier V, et al, for the Groupe d’Etude 73 Cheng A-L, Kang Y-K, Chen Z, et al. Efficacy and safety of sorafenib
et de Traitement du Carcinome Hépatocellulaire (GRETCH). in patients in the Asia-Pacific region with advanced hepatocellular
Ultrasonographic surveillance of hepatocellular carcinoma in carcinoma: a phase III randomised, double-blind,
cirrhosis: a randomized trial comparing 3- and 6-month placebo-controlled trial. Lancet Oncol 2009; 10: 25–34.
periodicities. Hepatology 2011; 54: 1987–97. 74 Dawson LA. The evolving role of radiation therapy in hepatocellular
50 Santi V, Trevisani F, Gramenzi A, et al. Semiannual surveillance is carcinoma. Cancer Radiother 2008; 12: 96–101.
superior to annual surveillance for the detection of early hepatocellular 75 Han KH, Seong J, Kim JK, Ahn SH, Lee do Y, Chon CY. Pilot
carcinoma and patient survival. J Hepatol 2010; 53: 291–97. clinical trial of localized concurrent chemoradiation therapy for
51 Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst locally advanced hepatocellular carcinoma with portal vein
2010; 102: 605–13. thrombosis. Cancer 2008; 113: 995–1003.
52 Pomfret EA, Washburn K, Wald C, et al. Report of a national 76 Hilgard P, Hamami M, Fouly AE, et al. Radioembolization with
conference on liver allocation in patients with hepatocellular yttrium-90 glass microspheres in hepatocellular carcinoma:
carcinoma in the United States. Liver Transpl 2010; 16: 262–78. European experience on safety and long-term survival. Hepatology
53 Colli A, Fraquelli M, Casazza G, et al. Accuracy of ultrasonography, 2010; 52: 1741–49.
spiral CT, magnetic resonance, and alpha-fetoprotein in diagnosing 77 Salem R, Lewandowski RJ, Mulcahy MF, et al. Radioembolization
hepatocellular carcinoma: a systematic review. Am J Gastroenterol for hepatocellular carcinoma using yttrium-90 microspheres: a
2006; 101: 513–23. comprehensive report of long-term outcomes. Gastroenterology 2010;
54 Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 138: 52–64.
20 mm or smaller in cirrhosis: prospective validation of the 78 Sangro B, Carpanese L, Cianni R, et al, on behalf of the European
noninvasive diagnostic criteria for hepatocellular carcinoma. Network on Radioembolization with Yttrium-90 Resin
Hepatology 2008; 47: 97–104. Microspheres (ENRY). Survival after yttrium-90 resin microsphere
55 Sangiovanni A, Manini MA, Iavarone M, et al. The diagnostic and radioembolization of hepatocellular carcinoma across Barcelona
economic impact of contrast imaging technique in the diagnosis of clinic liver cancer stages: a European evaluation. Hepatology 2011;
small hepatocellular carcinoma in cirrhosis. Gut 2010; 59: 638–44. 54: 868–78.
56 Khalili KT, Kim TK, Jang HJ, et al. Optimization of imaging diagnosis 79 Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R.
of 1-2 cm hepatocellular carcinoma: an analysis of diagnostic Transection of the oesophagus for bleeding oesophageal varices.
performance and resource utilization. J Hepatol 2011; 54: 723–28. Br J Surg 1973; 60: 646–49.
57 Chen LD, Xu HX, Xie XY, et al. Intrahepatic cholangiocarcinoma 80 D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and
and hepatocellular carcinoma: differential diagnosis with prognostic indicators of survival in cirrhosis: a systematic review
contrast-enhanced ultrasound. Eur Radiol 2010; 20: 743–53. of 118 studies. J Hepatol 2006; 44: 217–31.
58 Vilana R, Forner A, Bianchi L, et al. Intrahepatic peripheral 81 Llovet JM, Schwartz M, Mazzaferro V. Resection and liver
cholangiocarcinoma in cirrhosis patients may display a vascular transplantation for hepatocellular carcinoma. Semin Liver Dis 2005;
pattern similar to hepatocellular carcinoma on contrast-enhanced 25: 181–200.
ultrasound. Hepatology 2010; 51: 2020–29. 82 Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical
59 Llovet JM, Chen Y, Wurmbach E, et al. A molecular signature to treatment for early hepatocellular carcinoma: resection versus
discriminate dysplastic nodules from early hepatocellular transplantation. Hepatology 1999; 30: 1434–40.
carcinoma in HCV cirrhosis. Gastroenterology 2006; 131: 1758–67. 83 Ishizawa T, Hasegawa K, Aoki T, et al. Neither multiple tumors nor
60 Di Tommaso L, Destro A, Fabbris V, et al. Diagnostic accuracy of portal hypertension are surgical contraindications for hepatocellular
clathrin heavy chain staining in a marker panel for the diagnosis of carcinoma. Gastroenterology 2008; 134: 1908–16.
small hepatocellular carcinoma. Hepatology 2011; 53: 1549–57. 84 Shiina S, Teratani T, Obi S, et al. A randomized controlled trial
61 Forner A, Reig ME, Rodriguez de Lope C, Bruix J. Current strategy of radiofrequency ablation with ethanol injection for small
for staging and treatment: the BCLC update and future prospects. hepatocellular carcinoma. Gastroenterology 2005; 129: 122–30.
Semin Liver Dis 2010; 30: 61–74.
1254 www.thelancet.com Vol 379 March 31, 2012
Seminar
85 Takayasu K, Arii S, Ikai I, et al. Prospective cohort study of 107 Schnitzbauer AA, Zuelke C, Graeb C, et al. A prospective
transarterial chemoembolization for unresectable hepatocellular randomised, open-labeled, trial comparing sirolimus-containing
carcinoma in 8510 patients. Gastroenterology 2006; 131: 461–69. versus mTOR-inhibitor-free immunosuppression in patients
86 Bargellini I, Sacco R, Bozzi E, et al. Transarterial undergoing liver transplantation for hepatocellular carcinoma.
chemoembolization in very early and early-stage hepatocellular BMC Cancer 2010; 10: 190.
carcinoma patients excluded from curative treatment: a prospective 108 Lencioni R. Loco-regional treatment of hepatocellular carcinoma.
cohort study. Eur J Radiol (published online April 3, 2011). Hepatology 2010; 52: 762–73.
DOI:10.1016/j.ejrad.2011.03.046. 109 Germani G, Pleguezuelo M, Gurusamy K, Meyer T, Isgro G,
87 Varela M, Real MI, Burrel M, et al. Chemoembolization of Burroughs AK. Clinical outcomes of radiofrequency ablation,
hepatocellular carcinoma with drug eluting beads: efficacy and percutaneous alcohol and acetic acid injection for hepatocelullar
doxorubicin pharmacokinetics. J Hepatol 2007; 46: 474–81. carcinoma: a meta-analysis. J Hepatol 2010; 52: 380–88.
88 Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing 110 Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review
to early and late phase intrahepatic recurrence of hepatocellular of randomized trials for hepatocellular carcinoma treated with
carcinoma after hepatectomy. J Hepatol 2003; 38: 200–07. percutaneous ablation therapies. Hepatology 2009; 49: 453–59.
89 Breitenstein S, Dimitroulis D, Petrowsky H, Puhan MA, 111 Orlando A, Leandro G, Olivo M, Andriulli A, Cottone M.
Müllhaupt B, Clavien P-A. Systematic review and meta-analysis of Radiofrequency thermal ablation vs. percutaneous ethanol injection
interferon after curative treatment of hepatocellular carcinoma in for small hepatocellular carcinoma in cirrhosis: meta-analysis of
patients with viral hepatitis. Br J Surg 2009; 96: 975–81. randomized controlled trials. Am J Gastroenterol 2009; 104: 514–24.
90 Shen Y-C, Hsu C, Chen L-T, Cheng C-C, Hu F-C, Cheng A-L. Adjuvant 112 Tateishi R, Shiina S, Teratani T, et al. Percutaneous radiofrequency
interferon therapy after curative therapy for hepatocellular carcinoma ablation for hepatocellular carcinoma: an analysis of 1000 cases.
(HCC): a meta-regression approach. J Hepatol 2010; 52: 889–94. Cancer 2005; 103: 1201–09.
91 Miyake Y, Takaki A, Iwasaki Y, Yamamoto K. Meta-analysis: 113 Chen MS, Li JQ, Zheng Y, et al. A prospective randomized trial
interferon-alpha prevents the recurrence after curative treatment of comparing percutaneous local ablative therapy and partial hepatectomy
hepatitis C virus-related hepatocellular carcinoma. J Viral Hepat for small hepatocellular carcinoma. Ann Surg 2006; 243: 321–28.
2010; 17: 287–92. 114 Huang GT, Lee PH, Tsang YM, et al. Percutaneous ethanol injection
92 Sala M, Fuster J, Llovet JM, et al. High pathological risk of recurrence versus surgical resection for the treatment of small hepatocellular
after surgical resection for hepatocellular carcinoma: an indication carcinoma: a prospective study. Ann Surg 2005; 242: 36–42.
for salvage liver transplantation. Liver Transpl 2004; 10: 1294–300. 115 Huang J, Yan L, Cheng Z, et al. A randomized trial comparing
93 Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the radiofrequency ablation and surgical resection for HCC conforming
treatment of small hepatocellular carcinomas in patients with to the Milan criteria. Ann Surg 2010; 252: 903–12.
cirrhosis. N Engl J Med 1996; 334: 693–99. 116 Llovet JM, Real MI, Montaña X, et al, for the Barcelona Clínic Liver
94 Bismuth H, Chiche L, Adam R, Castaing D, Diamond T, Cancer Group. Arterial embolisation or chemoembolisation versus
Dennison A. Liver resection versus transplantation for symptomatic treatment in patients with unresectable hepatocellular
hepatocellular carcinoma in cirrhosis. Ann Surg 1993; 218: 145–51. carcinoma: a randomised controlled trial. Lancet 2002; 359: 1734–39.
95 Jonas S, Bechstein WO, Steinmuller T, et al. Vascular invasion and 117 Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of
histopathologic grading determine outcome after liver transarterial lipiodol chemoembolization for unresectable
transplantation for hepatocellular carcinoma in cirrhosis. Hepatology hepatocellular carcinoma. Hepatology 2002; 35: 1164–71.
2001; 33: 1080–86. 118 Oliveri RS, Wetterslev J, Gluud C. Transarterial (chemo)
96 Bruix J, Sherman M, Llovet JM, et al, for the EASL panel of experts on embolisation for unresectable hepatocellular carcinoma.
HCC. Clinical management of hepatocellular carcinoma: conclusions Cochrane Database Syst Rev 2011; 3: CD004787.
of the Barcelona-2000 EASL conference. J Hepatol 2001; 35: 421–30. 119 Pelletier G, Roche A, Ink O, et al. A randomized trial of hepatic
97 Clavien P-A, Lesurtel M, Bossuyt PMM, Gores GJ, Langer B, Perrier A, arterial chemoembolization in patients with unresectable
on behalf of the OLT for HCC Consensus Group. Recommendations hepatocellular carcinoma. J Hepatol 1990; 11: 181–84.
for liver transplantation for hepatocellular carcinoma: an international 120 Doffoel M, Bonnetain F, Bouche O, et al. Multicentre randomised
consensus conference report. Lancet Oncol (published online Nov 1, phase III trial comparing tamoxifen alone or with transarterial
2011). DOI:10.1016/S1470-2045(11)70175-9. lipiodol chemoembolisation for unresectable hepatocellular
98 Freeman RB, Edwards EB, Harper AM. Waiting list removal rates carcinoma in cirrhotic patients (Fédération Francophone de
among patients with chronic and malignant liver diseases. Cancérologie Digestive 9402). Eur J Cancer 2008; 44: 528–38.
Am J Transplant 2006; 6: 1416–21. 121 Lin DY, Liaw YF, Lee TY, Lai CM. Hepatic arterial embolization in
99 Llovet JM, Mas X, Aponte JJ, et al. Cost effectiveness of adjuvant patients with unresectable hepatocellular carcinoma: a randomized
therapy for hepatocellular carcinoma during the waiting list for liver controlled trial. Gastroenterology 1988; 94: 453–56.
transplantation. Gut 2002; 50: 123–28. 122 Lammer J, Malagari K, Vogl T, et al. Prospective randomized study
100 Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict of doxorubicin-eluting-bead embolization in the treatment of
survival in patients with end-stage liver disease. Hepatology 2001; hepatocellular carcinoma: results of the PRECISION V study.
33: 464–70. Cardiovasc Intervent Radiol 2010; 33: 41–52.
101 Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for 123 Raoul J, Sangro B, Forner A, et al. Evolving strategies for the
hepatocellular carcinoma: expansion of the tumor size limits does management of intermediate-stage hepatocellular carcinoma:
not adversely impact survival. Hepatology 2001; 33: 1394–403. available evidence and expert opinion on the use of transarterial
102 Lee SG, Hwang S, Moon DB, et al. Expanded indication criteria of chemoembolization. Cancer Treat Rev 2011; 37: 212–20.
living donor liver transplantation for hepatocellular carcinoma at 124 Marrero JA, Lencioni R, Kudo M, Nakajima F, Cihon AP, Venook A.
one large-volume center. Liver Transpl 2008; 14: 935–45. Global Investigation of therapeutic Decisions in Hepatocellular
103 Herrero JI, Sangro B, Pardo F, et al. Liver transplantation in Carcinoma and of its Treatment with Sorafenib (GIDEON) second
patients with hepatocellular carcinoma across Milan criteria. interim analysis in more than 1,500 patients: clinical findings in
Liver Transpl 2008; 14: 272–78. patients with liver dysfunction. J Clin Oncol 2011;
104 Mazzaferro V, Llovet JM, Miceli R, et al, on behalf of the Metroticket 29 (suppl): 4001 (abstr).
Investigator Study Group. Predicting survival after liver 125 Benson AB, Abrams TA, Ben-Josef E, et al. NCCN clinical practice
transplantation in patients with hepatocellular carcinoma beyond guidelines in oncology: hepatobiliary cancers.
the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol J Natl Compr Canc Netw 2009; 7: 350–91.
2009; 10: 35–43. 126 Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to
105 Mazzaferro V, Chun YS, Poon RT, et al. Liver transplantation for evaluate the response to treatment in solid tumors.
hepatocellular carcinoma. Ann Surg Oncol 2008; 15: 1001–07. J Natl Cancer Inst 2000; 92: 205–16.
106 Volk ML, Vijan S, Marrero JA. A novel model measuring the harm 127 Cheng A, Kang Y, Lin D, et al. Phase III trial of sunitinib (Su)
of transplanting hepatocellular carcinoma exceeding Milan criteria. versus sorafenib (So) in advanced hepatocellular carcinoma (HCC).
Am J Transplant 2008; 8: 839–46. J Clin Oncol 2011; 29 (suppl): 4000 (abstr).
www.thelancet.com Vol 379 March 31, 2012 1255
Você também pode gostar
- Seminar: Arndt Vogel, Tim Meyer, Gonzalo Sapisochin, Riad Salem, Anna SaborowskiDocumento18 páginasSeminar: Arndt Vogel, Tim Meyer, Gonzalo Sapisochin, Riad Salem, Anna SaborowskiKarolinakuprescenkaiteAinda não há avaliações
- Guideline Karsinoma HepatoselulerDocumento11 páginasGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoAinda não há avaliações
- Chip BetterDocumento10 páginasChip BetterpopAinda não há avaliações
- Molecular Genetics of Colorectal CancerDocumento6 páginasMolecular Genetics of Colorectal Cancermuhammad rizqi romadlonAinda não há avaliações
- Hepatocellular CarcinomaDocumento18 páginasHepatocellular CarcinomaIngrid González EfronAinda não há avaliações
- hepatoCA 2Documento9 páginashepatoCA 2Al VlaovicAinda não há avaliações
- Capitanio 2016Documento13 páginasCapitanio 2016Posgrado CirugiaAinda não há avaliações
- MEHU130 U2 T74 Colorectal CancerDocumento14 páginasMEHU130 U2 T74 Colorectal CancerStefani AtlleAinda não há avaliações
- Pi Is 0923753419472797Documento12 páginasPi Is 0923753419472797Cláudia SilvaAinda não há avaliações
- Adapted, CttoDocumento9 páginasAdapted, CttoNoli JaranillaAinda não há avaliações
- CA Colon OncologyDocumento8 páginasCA Colon OncologyAgstri Dwi MarselaAinda não há avaliações
- Testicular CancerDocumento12 páginasTesticular Cancerghost_724Ainda não há avaliações
- Histopathology of Hepatocellular CarcinomaDocumento11 páginasHistopathology of Hepatocellular CarcinomaCindy Sabina FaleandraAinda não há avaliações
- Case Report 1676563639Documento6 páginasCase Report 1676563639noah jemedafeAinda não há avaliações
- Seminar: Eric Van Cutsem, Xavier Sagaert, Baki Topal, Karin Haustermans, Hans PrenenDocumento11 páginasSeminar: Eric Van Cutsem, Xavier Sagaert, Baki Topal, Karin Haustermans, Hans PrenenLeyla Barnard LagunaAinda não há avaliações
- Cancer and Liver Cirrhosis: Implications On Prognosis and ManagementDocumento16 páginasCancer and Liver Cirrhosis: Implications On Prognosis and ManagementAlifia Ramadhanty PrameswariAinda não há avaliações
- Squamous Cell Tumors Bile Duct Cancers: PathophysiologyDocumento6 páginasSquamous Cell Tumors Bile Duct Cancers: PathophysiologySiti RahmahAinda não há avaliações
- Colon CancerDocumento7 páginasColon CancerKen Ancheta LagayadaAinda não há avaliações
- Hepatocellular Carcinoma: Clinical Frontiers and PerspectivesDocumento13 páginasHepatocellular Carcinoma: Clinical Frontiers and PerspectivesMisnariahIdrusAinda não há avaliações
- Primer: Hepatocellular CarcinomaDocumento28 páginasPrimer: Hepatocellular CarcinomaAinun Aii NoorAinda não há avaliações
- Porcel (2012) Clinical Implications of Pleural Effusions in Ovarian CancerDocumento8 páginasPorcel (2012) Clinical Implications of Pleural Effusions in Ovarian CancerLyka MahrAinda não há avaliações
- Hepatic Metastasis From Colorectal CancerDocumento11 páginasHepatic Metastasis From Colorectal CancerApriani KudiAinda não há avaliações
- Malignant Liver Tumours: Table 1Documento8 páginasMalignant Liver Tumours: Table 1abbasAinda não há avaliações
- Pancreatic Cancer Oxford SurgeryDocumento10 páginasPancreatic Cancer Oxford SurgeryJose Tomás MooreAinda não há avaliações
- Guia Cáncer MtiosDocumento12 páginasGuia Cáncer Mtiosouf81Ainda não há avaliações
- Jurnal Ricky 2Documento24 páginasJurnal Ricky 2Dyki AnwarAinda não há avaliações
- Initial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsDocumento33 páginasInitial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsClaudia YalanAinda não há avaliações
- Seminar: Eric Van Cutsem, Xavier Sagaert, Baki Topal, Karin Haustermans, Hans PrenenDocumento11 páginasSeminar: Eric Van Cutsem, Xavier Sagaert, Baki Topal, Karin Haustermans, Hans PrenenKati RondonAinda não há avaliações
- HCC GudelinesDocumento18 páginasHCC GudelinesVlad CroitoruAinda não há avaliações
- Ca EndometriumDocumento51 páginasCa Endometriumoktaviany810Ainda não há avaliações
- Anal Cancer Guidelines 2014Documento12 páginasAnal Cancer Guidelines 2014Alfredo Alfaro CarvajalAinda não há avaliações
- Published PaperDocumento10 páginasPublished Papermohd aftab siddiquiAinda não há avaliações
- Localised Colon Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocumento15 páginasLocalised Colon Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDrogoman MarianAinda não há avaliações
- Ultrasound Screening For Hepatocellular Carcinoma in Patients With Advanced Liver Fibrosis. An OverviewDocumento7 páginasUltrasound Screening For Hepatocellular Carcinoma in Patients With Advanced Liver Fibrosis. An OverviewarialAinda não há avaliações
- Kuipersetal CRC NRDP2015Documento26 páginasKuipersetal CRC NRDP2015Robert ChristevenAinda não há avaliações
- Staging Systems in Hepatocellular Carcinoma: Fernando Pons, Maria Varela & Josep M. LlovetDocumento7 páginasStaging Systems in Hepatocellular Carcinoma: Fernando Pons, Maria Varela & Josep M. LlovetEphie NoerAinda não há avaliações
- R Azumi Lava 2014Documento12 páginasR Azumi Lava 2014limbert manuelAinda não há avaliações
- Kuipers 2015Documento25 páginasKuipers 2015Fahmi RizalAinda não há avaliações
- Beger Et Al. - 2008 - Bauchspeicheldrüsenkrebs - Heilungschancen MinimalDocumento10 páginasBeger Et Al. - 2008 - Bauchspeicheldrüsenkrebs - Heilungschancen MinimalMaría Reynel TarazonaAinda não há avaliações
- Pancreatic CancerDocumento14 páginasPancreatic Cancerpaulo saAinda não há avaliações
- Fibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleDocumento3 páginasFibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleIKIKIKIKIKI999999Ainda não há avaliações
- Hepato CA 8Documento15 páginasHepato CA 8Al VlaovicAinda não há avaliações
- 19#prognostic HCC 2021Documento7 páginas19#prognostic HCC 2021hitashiAinda não há avaliações
- Cancer Gastrico Lancet 2020Documento14 páginasCancer Gastrico Lancet 2020andreaAinda não há avaliações
- Metastasis Site Liver CancerDocumento7 páginasMetastasis Site Liver CancerChristofel JomanAinda não há avaliações
- Anal Cancer - ESMO-ESSO-ESTRO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocumento11 páginasAnal Cancer - ESMO-ESSO-ESTRO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpNasrudin EfendiAinda não há avaliações
- Liver Tumors - Epidemiology, Diagnosis, Prevention and Treatment (Helen Reeves)Documento184 páginasLiver Tumors - Epidemiology, Diagnosis, Prevention and Treatment (Helen Reeves)JohnQAinda não há avaliações
- Gastric Adenocarcinoma Review and Considerations For Future DirectionsDocumento51 páginasGastric Adenocarcinoma Review and Considerations For Future DirectionsDoctor's BettaAinda não há avaliações
- Hepatocellular Carcinoma CancerDocumento18 páginasHepatocellular Carcinoma Cancerdheva akilAinda não há avaliações
- Colorectal Neoplasia andDocumento9 páginasColorectal Neoplasia andJEFFERSON MUÑOZAinda não há avaliações
- Hepatic Nodules CEUSDocumento8 páginasHepatic Nodules CEUScalustre2016Ainda não há avaliações
- Pertanyaan Referat CA SigmoidDocumento9 páginasPertanyaan Referat CA SigmoidBelladinaMMAinda não há avaliações
- ,Qflghqfhri&Roruhfwdo&Dqfhulq6Dlixo$Qzdu +Rvslwdo0Dodqj-Dqxdu/$SuloDocumento4 páginas,Qflghqfhri&Roruhfwdo&Dqfhulq6Dlixo$Qzdu +Rvslwdo0Dodqj-Dqxdu/$SuloAgus PraktyasaAinda não há avaliações
- PG Art 34580-10Documento15 páginasPG Art 34580-10Horia MineaAinda não há avaliações
- There Are Approximately 4800 New Cases of Small Bowel Cancer Each Year in The UDocumento2 páginasThere Are Approximately 4800 New Cases of Small Bowel Cancer Each Year in The UArassikaAinda não há avaliações
- Cancer de EsofagoDocumento14 páginasCancer de EsofagoLibros MedicinaAinda não há avaliações
- 260-Article Text-875-1-10-20220728Documento4 páginas260-Article Text-875-1-10-20220728hasan andrianAinda não há avaliações
- Colorectal Cancer: Etiology, Pathogenesis and Current TreatmentDocumento6 páginasColorectal Cancer: Etiology, Pathogenesis and Current TreatmentSandra RAinda não há avaliações
- 2021 Recomendations For Srveillance and Manangemnt of Recurrent Esophageal Cancer Following Endoscopic TherapiesDocumento12 páginas2021 Recomendations For Srveillance and Manangemnt of Recurrent Esophageal Cancer Following Endoscopic TherapiesykommAinda não há avaliações
- Human Papillomavirus: Proving and Using a Viral Cause for CancerNo EverandHuman Papillomavirus: Proving and Using a Viral Cause for CancerAinda não há avaliações
- NIH Public Access: Author ManuscriptDocumento14 páginasNIH Public Access: Author Manuscriptapi-283759086Ainda não há avaliações
- Annikasresume 1Documento1 páginaAnnikasresume 1api-283759086Ainda não há avaliações
- Annikas Resume 1Documento1 páginaAnnikas Resume 1api-283759086Ainda não há avaliações
- Robotics Newsletter 11 11 2016Documento2 páginasRobotics Newsletter 11 11 2016api-283759086Ainda não há avaliações
- DBQ - Mexam WarDocumento4 páginasDBQ - Mexam Warapi-283759086Ainda não há avaliações
- BibliographyDocumento2 páginasBibliographyapi-283759086Ainda não há avaliações
- JpessaycorrectedDocumento6 páginasJpessaycorrectedapi-283759086Ainda não há avaliações
- ICD-10 Guidelines For The Physician CoderDocumento17 páginasICD-10 Guidelines For The Physician Coderlina_villegas_13Ainda não há avaliações
- ANNEX 2p GUIDELINES ON PRE ADMISSION SCREENING OF COVID 19 01082022Documento3 páginasANNEX 2p GUIDELINES ON PRE ADMISSION SCREENING OF COVID 19 01082022EllieAinda não há avaliações
- First CaseDocumento11 páginasFirst CaseRisha A.MAinda não há avaliações
- Chronic Kidney DiseaseDocumento29 páginasChronic Kidney DiseaseEsayas KebedeAinda não há avaliações
- Reference PDFDocumento5 páginasReference PDFWina BudiartiAinda não há avaliações
- BIRTH CompressedDocumento2 páginasBIRTH CompressedDip PatraAinda não há avaliações
- Just Another Sebaceous Cyst?: I. Clinical QuestionDocumento3 páginasJust Another Sebaceous Cyst?: I. Clinical QuestionJaessa FelicianoAinda não há avaliações
- Merrell Dow Pharmaceutical Meeting 1982Documento1 páginaMerrell Dow Pharmaceutical Meeting 1982Julia PurperaAinda não há avaliações
- Rhinitis Allergic: Elma Wiliandini G4A020043Documento10 páginasRhinitis Allergic: Elma Wiliandini G4A020043elma wiliandiniAinda não há avaliações
- Passages Final 1Documento17 páginasPassages Final 1api-354601300Ainda não há avaliações
- CIA4001 - FE Answer Scheme - Sem2 - 20192020Documento9 páginasCIA4001 - FE Answer Scheme - Sem2 - 20192020Divya TharshiniAinda não há avaliações
- Gpics V2 - 2019 PDFDocumento252 páginasGpics V2 - 2019 PDFelphabarAinda não há avaliações
- Dysphagia Team in The Public SchoolsDocumento15 páginasDysphagia Team in The Public SchoolsSeresol100% (1)
- Susi Erawati-Fkik PDFDocumento116 páginasSusi Erawati-Fkik PDFCholifaturrizkiyahAinda não há avaliações
- Einstein Syndrome - Circle of MomsDocumento12 páginasEinstein Syndrome - Circle of MomsYasser E KasanAinda não há avaliações
- NCPDocumento5 páginasNCPMcmc Ryan Ferdinand GutierrezAinda não há avaliações
- Ra-075903 Architect Manila 6-2022Documento137 páginasRa-075903 Architect Manila 6-2022MelAinda não há avaliações
- Health Project Proposal SampleDocumento14 páginasHealth Project Proposal SampleEskadmas BelayAinda não há avaliações
- Playbook On Promoting Actions Toward Drowning-Free CommunitiesDocumento52 páginasPlaybook On Promoting Actions Toward Drowning-Free CommunitiesAristotel C. Cabais, RNAinda não há avaliações
- Brain Tumors - Classifications, Symptoms, Diagnosis and TreatmentsDocumento10 páginasBrain Tumors - Classifications, Symptoms, Diagnosis and TreatmentsshamimAinda não há avaliações
- ORC ICF Audit Checklist Jan 2017Documento6 páginasORC ICF Audit Checklist Jan 2017Ita afrika sariAinda não há avaliações
- Psychological ReportDocumento14 páginasPsychological ReportPhcorner Itachi100% (2)
- Guidelines For Schools WHODocumento97 páginasGuidelines For Schools WHONok NookAinda não há avaliações
- Incident Report Acetaldehyde Oximes 24.08.2023Documento3 páginasIncident Report Acetaldehyde Oximes 24.08.2023Alasto JakandeAinda não há avaliações
- Drug Study 2Documento2 páginasDrug Study 2Kim Glaidyl BontuyanAinda não há avaliações
- Addison's DiseaseDocumento9 páginasAddison's Diseaseash ashAinda não há avaliações
- Script 2 Ep1Documento16 páginasScript 2 Ep1Frankie CollinsAinda não há avaliações
- Puerperal SepsisDocumento45 páginasPuerperal SepsisKalo kajiAinda não há avaliações
- Please Edit Your Title PageDocumento12 páginasPlease Edit Your Title PageayeshaAinda não há avaliações