Escolar Documentos
Profissional Documentos
Cultura Documentos
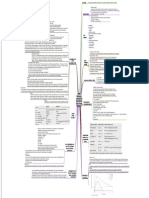
Heart Dysrhythmias Cheat Sheet Explained
Enviado por
pcmundot0 notas0% acharam este documento útil (0 voto)
457 visualizações5 páginasTítulo original
Heart-Dysrhythmias-Cheat-Sheet.pdf
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
457 visualizações5 páginasHeart Dysrhythmias Cheat Sheet Explained
Enviado por
pcmundotDireitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 5
Heart Dysrhythmias Cheat Sheet
Arrhythmias Description Causes Treatment
Irregular atrial and Normal variation of Atropine if rate decreases
ventricular rhythms. normal sinus rhythm in below 40bpm.
Normal P wave preceding athletes, children, and the
each QRS complex. elderly.
Sinus Arrhythmia
Can be seen in digoxin
toxicity and inferior wall
MI.
Atrial and ventricular Normal physiologic Correction of underlying
rhythms are regular. response to fever, cause.
Rate > 100 bpm. exercise, anxiety, Beta-adrenergic blockers
Normal P wave preceding dehydration, or pain. or calcium channel
each QRS complex. May accompany shock, blockers for symptomatic
left-sided heart failure, patients.
Sinus Tachycardia cardiac tamponade,
hyperthyroidism, and
anemia.
Atropine, epinephrine,
quinidine, caffeine,
nicotine, and alcohol use.
Regular atrial and Normal in a well- Follow ACLS protocol for
ventricular rhythms. conditioned heart (e.g., administration of atropine
Rate < 60 bpm. athletes). for symptoms of low
Normal P wave preceding Increased intracranial cardiac output, dizziness,
Sinus Bradycardia each QRS complex. pressure; increased vagal weakness, altered LOC, or
tone due to straining low blood pressure.
during defecation, Pacemaker
vomiting, intubation,
mechanical ventilation.
Atrial and ventricular Infection Treat symptoms with
rhythms normal except for Coronary artery disease, atropine I.V.
missing complex. degenerative heart Temporary pacemaker or
Sinoatrial (SA) Normal P wave preceding disease, acute inferior wall permanent pacemaker if
arrest or block each QRS complex. MI. considered for repeated
Pause not equal to Vagal stimulation, episodes.
multiple of the previous Valsalva’s a euver,
rhythm. carotid sinus massage.
Atrial and ventricular Rheumatic carditis due to No treatment if patient is
Wandering atrial rhythms vary slightly. inflammation involving asymptomatic
pacemaker Irregular PR interval. the SA node.
Digoxin toxicity
P waves irregular with Sick sinus syndrome Treatment of underlying
changing configurations cause if patient is
i dicati g that they are ’t symptomatic.
all from SA node or single
atrial focus; may appear
after the QRS complex.
QRS complexes uniform in
shape but irregular in
rhythm.
Premature, abnormal- May prelude Usually no treatment is
looking P waves that differ supraventricular needed.
in configuration from tachycardia. Treatment of underlying
normal P waves. Stimulants, cause if patient is
QRS complexes after P hyperthyroidism, COPD, symptomatic.
Premature atrial
waves except in very early infection and other heart Carotid sinus massage.
contraction (PAC)
or blocked PACs. diseases.
P wave often buried in the
preceding T wave or
identified in the preceding
T wave.
Atrial and ventricular Physical exertion, If patient is unstable
rhythms are regular. emotion, stimulants, prepare for immediate
Heart rate > 160 bpm; rheumatic heart diseases. cardioversion.
rarely exceeds 250 bpm. Intrinsic abnormality of AV If patient is stable, vagal
P waves regular but conduction system. stimulation, or Valsalva’s
aberrant; difficult to Digoxin toxicity. maneuver, carotid sinus
differentiate from Use of caffeine, massage.
preceding T wave. marijuana, or central Adenosine by rapid I.V.
P wave preceding each nervous system bolus injection to rapidly
Paroxysmal
QRS complex. stimulants. convert arrhythmia.
Supraventricular
Sudden onset and If patient has normal
Tachycardia
termination of arrhythmia ejection fraction, consider
When a normal P wave is calcium channel blockers,
prese t, it’s called beta-adrenergic blocks or
paroxysmal atrial amiodarone.
tachycardia; when a If patient has an ejection
normal P wave is ’t fraction less than 40%,
prese t, it’s called consider amiodarone.
paroxysmal junctional
tachycardia.
Atrial rhythm regular, Heart failure, tricuspid or If patient is unstable with
rate, 250 to 400 bpm mitral valve disease, ventricular rate > 150bpm,
Ventricular rate variable, pulmonary embolism, cor prepare for immediate
depending on degree of pulmonale, inferior wall cardioversion.
AV block MI, carditis. If patient is stable, drug
Atrial flutter
Saw-tooth shape P wave Digoxin toxicity. therapy may include
configuration. calcium channel blockers,
QRS complexes uniform in beta-adrenergic blocks, or
shape but often irregular antiarrhythmics.
in rate.
Anticoagulation therapy
may be necessary.
Atrial rhythm grossly Heart failure, COPD, If patient is unstable with
irregular rate > 300 to 600 thyrotoxicosis, constrictive ventricular rate > 150bpm,
bpm. pericarditis, ischemic prepare for immediate
Ventricular rhythm grossly heart disease, sepsis, cardioversion.
irregular, rate 160 to 180 pulmonary embolus, If stable, drug therapy
bpm. rheumatic heart disease, may include calcium
PR interval indiscernible. hypertension, mitral channel blockers, beta-
No P waves, or P waves stenosis, atrial irritation, adrenergic blockers,
that appear as erratic, complication of coronary digoxin, procainamide,
Atrial Fibrillation
irregular base-line bypass or valve quinidine, ibutilide, or
fibrillatory waves replacement surgery amiodarone.
Anticoagulation therapy
to prevent emboli.
Dual chamber atrial
pacing, implantable atrial
pacemaker, or surgical
maze procedure may also
be used.
Atrial and ventricular Inferior wall MI, or Correction of underlying
rhythms are regular. ischemia, hypoxia, vagal cause.
Atrial rate 40 to 60 bpm. stimulation, sick sinus Atropine for symptomatic
Ventricular rate usually 40 syndrome. slow rate
to 60 bpm. Acute rheumatic fever. Pacemaker insertion if
P waves preceding, hidden Valve surgery patient is refractory to
within (absent), or after Digoxin toxicity drugs
Junctional Rhythm QRS complex; usually Discontinuation of digoxin
inverted if visible. if appropriate.
PR interval (when present)
< 0.12 second
QRS complex
configuration and
duration normal, except in
aberrant conduction.
Atrial and ventricular MI or ischemia Correction of underlying
rhythms are irregular. Digoxin toxicity and cause.
P waves inverted; may excessive caffeine or Discontinuation of digoxin
Premature
precede be hidden within, amphetamine use if appropriate.
Junctional
or follow QRS complex.
Conjunctions
QRS complex
configuration and
duration normal.
Atrial and ventricular Inferior wall MI or Correction of the
rhythms regular ischemia or infarction, underlying cause.
First-degree AV PR interval > 0.20 second. hypothyroidism, Possibly atropine if PR
block P wave preceding each hypokalemia, interval exceeds 0.26
QRS complex. hyperkalemia. second or symptomatic
QRS complex normal. Digoxin toxicity. bradycardia develops.
Use of quinidine, Cautious use of digoxin,
procamide, beta- calcium channel blockers,
adrenergic blocks, calcium and beta-adrenergic
blockers.
Atrial rhythm regular. Severe coronary artery Atropine, epinephrine,
Ventricular rhythm disease, anterior wall MI, and dopamine for
irregular. acute myocarditis. symptomatic bradycardia.
Atrial rate exceeds Digoxin toxicity Temporary or permanent
Second-degree AV ventricular rate. pacemaker for
block Mobitz I PR interval progressively, symptomatic bradycardia.
(Wenckebach) but only slightly, longer Discontinuation of digoxin
with each cycle until QRS if appropriate.
complex disappears.
PR interval shorter after
dropped beat.
Atrial rhythm regular. Inferior or anterior wall Atropine, epinephrine,
Ventricular rhythm regular MI, congenital and dopamine for
and rate slower than atrial abnormality, rheumatic symptomatic bradycardia.
rate. fever. Temporary or permanent
No relation between P pacemaker for
Third-degree AV
waves and QRS symptomatic bradycardia.
block (complex
complexes.
heart block)
No constant PR interval.
QRS interval normal
(nodal pacemaker) or
wide and bizarre
(ventricular pacemaker).
Atrial rhythm regular Heart failure; old or acute If warranted,
Ventricular rhythm myocardial ischemia, procainamide, lidocaine,
irregular infarction, or contusion. or amiodarone I.V.
QRS complex premature, Myocardial irritation by Treatment of underlying
usually followed by a ventricular catheters such cause.
complete compensatory as a pacemaker. Discontinuation of drug
pause Hypercapnia, causing toxicity.
QRS complex wide and hypokalemia, Potassium chloride IV if
Premature
distorted, usually >0.14 hypocalcemia. PVC induced by
ventricular
second. Drug toxicity by cardiac hypokalemia.
contraction (PVC)
Premature QRS complexes glycosides, aminophylline, Magnesium sulfate IV if
occurring singly, in pairs, tricyclic antidepressants, PVC induced by
or in threes; alternating beta-adrenergic. hypomagnesaemia.
with normal beats; focus Caffeine, tobacco, or
from one or more sites. alcohol use.
Ominous when clustered, Psychological stress,
multifocal, with R wave on anxiety, pain
T pattern.
Ventricular rate 140 to Myocardial ischemia, If pulseless: initiate CPR;
Ventricular
220 bpm, regular or infarction, or aneurysm follow ACLS protocol for
Tachycardia
irregular. Coronary artery disease defibrillation.
QRS complexes wide, Rheumatic heart disease If with pulse: If
bizarre, and independent Mitral valve prolapse, hemodynamically stable,
of P waves heart failure, follow ACLS protocol for
P waves no discernible cardiomyopathy administration of
May start and stop Ventricular catheters. amiodarone; if ineffective
suddenly Hypokalemia, initiate synchronized
Hypercalcemia. cardioversion.
Pulmonary embolism.
Digoxin, procainamide,
epinephrine, quinidine
toxicity, anxiety.
Ventricular rhythm and Myocardial ischemia or If pulseless: start CPR,
rate are rapid and chaotic. infarction, R-on-T follow ACLS protocol for
QRS complexes wide and phenomenon, untreated defibrillation, ET
irregular, no visible P ventricular tachycardia, intubation, and
waves Hypokalemia, administration f
Ventricular
hyperkalemia, epinephrine or
Fibrillation
Hypercalcemia, alkalosis, vasopressin, lidocaine, or
electric shock, amiodarone; ineffective
hypothermia. consider magnesium
Digoxin, epinephrine, or sulfate.
quinidine toxicity.
No atrial or ventricular Myocardial ischemia or Start CPR.
rate or rhythm. infarction, aortic valve
No discernible P waves, disease, heart failure,
QRS complexes, or T hypoxemia, hypokalemia,
waves severe acidosis, electric
shock, ventricular
arrhythmias, AV block,
Asystole
pulmonary embolism,
heart rupture, cardiac
tamponade,
hyperkalemia,
electromechanical
dissociation.
Cocaine overdose.
Você também pode gostar
- EKG Rhythms: SVT, Atrial Fibrillation, AV Blocks (39Documento10 páginasEKG Rhythms: SVT, Atrial Fibrillation, AV Blocks (39Saidel ElizondoAinda não há avaliações
- Cardiac Rhythms and Dysrhythmias GuideDocumento14 páginasCardiac Rhythms and Dysrhythmias GuideShawn Gaurav Jha100% (1)
- This Study Resource Was Shared Via: Sinus BradycardiaDocumento3 páginasThis Study Resource Was Shared Via: Sinus BradycardiaPascal St Peter NwaorguAinda não há avaliações
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsAinda não há avaliações
- ECG Rythum Study Guide PDFDocumento9 páginasECG Rythum Study Guide PDFArtika MayandaAinda não há avaliações
- Ccu Survival GuideDocumento10 páginasCcu Survival Guideomegasauron0gmailcom100% (1)
- Acute Lymphocytic LeukemiaDocumento7 páginasAcute Lymphocytic Leukemiamildred alidon100% (1)
- ACLS Provider Manual Supplementary MaterialDocumento86 páginasACLS Provider Manual Supplementary MaterialEma0% (2)
- Patient Education for Ileal Conduit CareDocumento11 páginasPatient Education for Ileal Conduit CareICa MarlinaAinda não há avaliações
- ABCDE Approach PDFDocumento3 páginasABCDE Approach PDFJohn SmithAinda não há avaliações
- Anti-Arrhythmic Agents For Pharmacy PDFDocumento41 páginasAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaAinda não há avaliações
- Myocardium - The heart muscle that surrounds the ventricles and atriaDocumento19 páginasMyocardium - The heart muscle that surrounds the ventricles and atriaFilane AntonetteAinda não há avaliações
- Shock Comparison ChartDocumento2 páginasShock Comparison Chartlinnaete88% (8)
- 100 Beats Per Minute. Many DifferentDocumento4 páginas100 Beats Per Minute. Many Differentjovan teopizAinda não há avaliações
- Plante PacemakersDocumento57 páginasPlante Pacemakersdragon66Ainda não há avaliações
- Acute Coronary SyndromeDocumento1 páginaAcute Coronary SyndromeMike GAinda não há avaliações
- Operating Room Preparation: Philipp Acaso Ralph ArcoDocumento158 páginasOperating Room Preparation: Philipp Acaso Ralph ArcoTiffany Luv Adrias100% (1)
- ACLS Class Packet PDFDocumento9 páginasACLS Class Packet PDFImam GultomAinda não há avaliações
- 17 Cardiac DrugsDocumento6 páginas17 Cardiac DrugshiwaralelataAinda não há avaliações
- ECG Rhythm Strip Interpretation Lesson 4Documento5 páginasECG Rhythm Strip Interpretation Lesson 4phoebjaetanAinda não há avaliações
- Diagnostic Test Purpose Normal Result Nursing ResponsibilityDocumento4 páginasDiagnostic Test Purpose Normal Result Nursing Responsibilitykennethfe agron100% (1)
- CG B Ook: Rapid FindDocumento25 páginasCG B Ook: Rapid FinddellaAinda não há avaliações
- EKG Quick Reference ChartDocumento4 páginasEKG Quick Reference ChartMildaAinda não há avaliações
- ECG StripsDocumento5 páginasECG StripsNursingSchoolNotes100% (1)
- Guide to Improving Interfacility Patient TransfersDocumento56 páginasGuide to Improving Interfacility Patient TransfersBuyungAinda não há avaliações
- Acute Coronary SyndromesDocumento1 páginaAcute Coronary SyndromesCamilo VidalAinda não há avaliações
- Common Cardiac MedicationsDocumento1 páginaCommon Cardiac MedicationsPaige HardekopfAinda não há avaliações
- HeartMurmursExplained SystolicDiastolicManeuversDocumento41 páginasHeartMurmursExplained SystolicDiastolicManeuversurtikikeAinda não há avaliações
- Department of Propaedeutics of Internal Diseases: Kursk State Medical UniversityDocumento88 páginasDepartment of Propaedeutics of Internal Diseases: Kursk State Medical UniversityHendraDarmawanAinda não há avaliações
- Interpret Blood Gas Analysis & Acid-Base ImbalancesDocumento3 páginasInterpret Blood Gas Analysis & Acid-Base ImbalancesChameera Bandara100% (2)
- ECG AbnormalitiesDocumento9 páginasECG Abnormalitiesbigabm062Ainda não há avaliações
- ECG Interpretation GuideDocumento69 páginasECG Interpretation GuideRohini RaiAinda não há avaliações
- Algorithms For IV Fluids Replacement in Midgets and Poodles PDFDocumento5 páginasAlgorithms For IV Fluids Replacement in Midgets and Poodles PDFAnonymous XbmV9JU5Ainda não há avaliações
- Alkalosis Acidosis ChartDocumento1 páginaAlkalosis Acidosis ChartrobingailAinda não há avaliações
- Cardiac Rhythms - ECG ReadingsDocumento15 páginasCardiac Rhythms - ECG Readingsal-obinay shereenAinda não há avaliações
- Interpret ECG Rhythms & Manage ArrhythmiasDocumento6 páginasInterpret ECG Rhythms & Manage Arrhythmiasjh_ajjAinda não há avaliações
- ECG InterpretationDocumento48 páginasECG InterpretationKervayse St.ClairAinda não há avaliações
- ECG - ACLS 2020 ModuleDocumento68 páginasECG - ACLS 2020 ModuleRasheedAladdinNGuiomala100% (1)
- ACLS Study GuideDocumento28 páginasACLS Study GuideNicole Berry100% (1)
- Adult Tachycardia With A Pulse Algorithm: Doses/DetailsDocumento1 páginaAdult Tachycardia With A Pulse Algorithm: Doses/DetailsAlexis HospitalAinda não há avaliações
- CKD Symptoms and TreatmentsDocumento3 páginasCKD Symptoms and TreatmentsrhizzyAinda não há avaliações
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDocumento42 páginasHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezAinda não há avaliações
- Chad Pressors HandoutDocumento12 páginasChad Pressors HandoutquelspectacleAinda não há avaliações
- Blood Gas InterpretationDocumento36 páginasBlood Gas InterpretationMary Charmaine DivinagraciaAinda não há avaliações
- Valvular Heart DiseaseDocumento10 páginasValvular Heart DiseaseEzyan SyaminAinda não há avaliações
- Nursing ResumeDocumento2 páginasNursing Resumeapi-259457383Ainda não há avaliações
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Documento47 páginasPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageAinda não há avaliações
- Normal Impulse Conduction: Sinoatrial NodeDocumento80 páginasNormal Impulse Conduction: Sinoatrial Nodesiusiuwidyanto100% (2)
- CardiomyopathyDocumento1 páginaCardiomyopathyTrisha VergaraAinda não há avaliações
- Left Sided & Right Sided Heart FailureDocumento29 páginasLeft Sided & Right Sided Heart FailureRachelle Ayn100% (3)
- Clinical Lab Guide: by MedgeeksDocumento17 páginasClinical Lab Guide: by MedgeeksHuy HoangAinda não há avaliações
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Cardiac Care and COVID-19: Perspectives in Medical PracticeNo EverandCardiac Care and COVID-19: Perspectives in Medical PracticeAinda não há avaliações
- Exam Prep for:: Bundle: Contemporary Medical-Surgical NursingNo EverandExam Prep for:: Bundle: Contemporary Medical-Surgical NursingAinda não há avaliações
- Respiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandRespiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Microcirculation as Related to ShockNo EverandMicrocirculation as Related to ShockDavid SheproAinda não há avaliações
- Disasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesNo EverandDisasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesMauricio LynnAinda não há avaliações
- ICU Scoring Systems A Complete Guide - 2020 EditionNo EverandICU Scoring Systems A Complete Guide - 2020 EditionAinda não há avaliações
- José Rene Castillo Cisneros You Are the Help Until Help Arrives _ Certificate SurveyDocumento1 páginaJosé Rene Castillo Cisneros You Are the Help Until Help Arrives _ Certificate SurveypcmundotAinda não há avaliações
- 250-tijuanaDocumento1 página250-tijuanapcmundotAinda não há avaliações
- Bureau of Security and Investigative Services: Department of Consumer AffairsDocumento17 páginasBureau of Security and Investigative Services: Department of Consumer AffairspcmundotAinda não há avaliações
- IV Cheatsheet Bgnocolor PDFDocumento2 páginasIV Cheatsheet Bgnocolor PDFHermiie Joii Galang MaglaquiiAinda não há avaliações
- 01ICS100b Visuals Aug2010Documento9 páginas01ICS100b Visuals Aug2010juliheroAinda não há avaliações
- CA Baton Training Manual Outlines Legal Use of ForceDocumento20 páginasCA Baton Training Manual Outlines Legal Use of Forcephilpedro100% (1)
- 20130SB66992CHPDocumento6 páginas20130SB66992CHPpcmundotAinda não há avaliações
- Acute Stroke CEDocumento2 páginasAcute Stroke CEpcmundotAinda não há avaliações
- In-Depth BBP A 09-14-11Documento48 páginasIn-Depth BBP A 09-14-11pcmundotAinda não há avaliações
- Power LOAD SpecSheet MktLit1243RevA2Documento1 páginaPower LOAD SpecSheet MktLit1243RevA2pcmundotAinda não há avaliações
- Acute Stroke One Page-2Documento1 páginaAcute Stroke One Page-2pcmundotAinda não há avaliações
- Acute Stroke One Page-2Documento1 páginaAcute Stroke One Page-2pcmundotAinda não há avaliações
- Citizen Corps Council Registration TutorialDocumento16 páginasCitizen Corps Council Registration TutorialpcmundotAinda não há avaliações
- Hazard1 Earthquakes Slides - Jan2011 PDFDocumento10 páginasHazard1 Earthquakes Slides - Jan2011 PDFpcmundotAinda não há avaliações
- Enrollment Agreement: National UniversityDocumento2 páginasEnrollment Agreement: National UniversitypcmundotAinda não há avaliações
- CERT Radio Communications Plan ManualDocumento15 páginasCERT Radio Communications Plan Manualbuckley1212085Ainda não há avaliações
- Hazard2 Fire Slides Jan2011Documento13 páginasHazard2 Fire Slides Jan2011pcmundotAinda não há avaliações
- Hazard1 Earthquakes Slides Jan2011Documento10 páginasHazard1 Earthquakes Slides Jan2011pcmundotAinda não há avaliações
- California CERT FOG 2014Documento84 páginasCalifornia CERT FOG 2014pcmundotAinda não há avaliações
- Citizen Corps Council Registration TutorialDocumento16 páginasCitizen Corps Council Registration TutorialpcmundotAinda não há avaliações
- Council Registion QuestionsDocumento18 páginasCouncil Registion QuestionspcmundotAinda não há avaliações
- Citizen Corps Council Admin GuideDocumento15 páginasCitizen Corps Council Admin GuidepcmundotAinda não há avaliações
- TTT Participant Manual 101316 CH 508Documento183 páginasTTT Participant Manual 101316 CH 508pcmundotAinda não há avaliações
- Cert Drill 1Documento32 páginasCert Drill 1pcmundotAinda não há avaliações
- CribbingDocumento1 páginaCribbingpcmundotAinda não há avaliações
- California CERT Field Operations Guide 2014Documento84 páginasCalifornia CERT Field Operations Guide 2014pcmundotAinda não há avaliações
- Cert Drill 3-2Documento28 páginasCert Drill 3-2pcmundotAinda não há avaliações
- FEMA Emergency Response Plan 0Documento10 páginasFEMA Emergency Response Plan 0Adam WardAinda não há avaliações
- Emergency Response ResourcesDocumento2 páginasEmergency Response ResourcesGerald LimAinda não há avaliações
- Pharma QuestionerDocumento38 páginasPharma Questionerjohn100% (2)
- Abm-11-D Viernesfritzie M4 Fil-AkadDocumento3 páginasAbm-11-D Viernesfritzie M4 Fil-AkadIsha Manzano Lacuesta100% (1)
- Modified Trauma ScoringDocumento63 páginasModified Trauma ScoringparuAinda não há avaliações
- Isolation Guidelines HealthDocumento204 páginasIsolation Guidelines HealthGrace Datu100% (1)
- Thornwaldt Cyst - A Disease or AnomalyDocumento4 páginasThornwaldt Cyst - A Disease or AnomalyresearchparksAinda não há avaliações
- Dennis N. Muñoz CVDocumento7 páginasDennis N. Muñoz CVDENNIS N. MUÑOZAinda não há avaliações
- Apixaban in Patients With Atrial FibrillationDocumento12 páginasApixaban in Patients With Atrial FibrillationthedancingseaAinda não há avaliações
- ISSVD Recommendations For The Diagnosis and Treatment of Vaginitis PDFDocumento198 páginasISSVD Recommendations For The Diagnosis and Treatment of Vaginitis PDF32daniel1Ainda não há avaliações
- A Systematic Review of Autopsy Findings in Deaths After Covid-19 VaccinationDocumento48 páginasA Systematic Review of Autopsy Findings in Deaths After Covid-19 VaccinationTim BrownAinda não há avaliações
- Rapid Disability Rating ScaleDocumento3 páginasRapid Disability Rating ScaleFatmawatiAinda não há avaliações
- Robotics in Medical ScienceDocumento45 páginasRobotics in Medical SciencePushkar Singh100% (2)
- Identification and Treatment of Retinopathy of Prematurity Update 2017Documento9 páginasIdentification and Treatment of Retinopathy of Prematurity Update 2017G VenkateshAinda não há avaliações
- 3ixso2idq334tonwmfhk0rrcDocumento2 páginas3ixso2idq334tonwmfhk0rrcrishikeshraj2021Ainda não há avaliações
- Rectum: Malueth AbrahamDocumento19 páginasRectum: Malueth AbrahamMalueth AnguiAinda não há avaliações
- Samavritti GiubarelliDocumento1 páginaSamavritti Giubarellirickcalligaro5582Ainda não há avaliações
- Activity 6 Online Resources RetrievalDocumento4 páginasActivity 6 Online Resources RetrievalHazel Jane AquinoAinda não há avaliações
- Activated Charcoal OverviewDocumento3 páginasActivated Charcoal OverviewCarlos Laureano Martinez FloresAinda não há avaliações
- Medical - Surgical Nursing 3 & 4: Final ExaminationsDocumento6 páginasMedical - Surgical Nursing 3 & 4: Final ExaminationsBRYAN JOSEPH TIONGSON100% (1)
- Post-Surgery Nursing Care and Medication EffectsDocumento5 páginasPost-Surgery Nursing Care and Medication EffectsJhevilin RMAinda não há avaliações
- FU-M3-CU11 Respiratory Function and Nursing CareDocumento17 páginasFU-M3-CU11 Respiratory Function and Nursing CareHERLIN HOBAYANAinda não há avaliações
- Type 1 Diabetes OutlineDocumento2 páginasType 1 Diabetes OutlineDominique PorterAinda não há avaliações
- Bab X - Dapus MBCT HipokondriasisDocumento3 páginasBab X - Dapus MBCT HipokondriasisRaisaDesytaAdlizaAinda não há avaliações
- PowerpointDocumento16 páginasPowerpointapi-324998847Ainda não há avaliações
- Brief Mental Status Exam MSE FormDocumento3 páginasBrief Mental Status Exam MSE FormClaire LimosAinda não há avaliações
- Cheung 1988Documento3 páginasCheung 1988Vanessa S DanielAinda não há avaliações
- Penile CancerDocumento58 páginasPenile CancerPatrascu CristiAinda não há avaliações
- Final Announcement ROICAM 4Documento19 páginasFinal Announcement ROICAM 4Piet AshadiAinda não há avaliações
- Perioperative Medicines Management V8Documento7 páginasPerioperative Medicines Management V8Waleed Ahmad.Ainda não há avaliações
- As Level Biology AQA Immune ResponseDocumento11 páginasAs Level Biology AQA Immune ResponseSahib Matharu100% (1)
- Hypertension Pamphlet.Documento5 páginasHypertension Pamphlet.Adelerin David OluwatosinAinda não há avaliações