Escolar Documentos
Profissional Documentos
Cultura Documentos
Helicobacter Pylori Infection
Enviado por
NovitaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Helicobacter Pylori Infection
Enviado por
NovitaDireitos autorais:
Formatos disponíveis
T he new engl and jour nal of me dicine
clinical practice
Helicobacter pylori Infection
Kenneth E.L. McColl, M.D.
This Journal feature begins with a case vignette highlighting a common clinical problem.
Evidence supporting various strategies is then presented, followed by a review of formal guidelines,
when they exist. The article ends with the author’s clinical recommendations.
A 29-year-old man presents with intermittent epigastric discomfort, without weight
loss or evidence of gastrointestinal bleeding. He reports no use of aspirin or non-
steroidal antiinflammatory drugs (NSAIDs). Abdominal examination reveals epi-
gastric tenderness. A serologic test for Helicobacter pylori is positive, and he receives a
10-day course of triple therapy (omeprazole, amoxicillin, and clarithromycin). Six
weeks later, he returns with the same symptoms. How should his case be further
evaluated and managed?
The Cl inic a l Probl e m
Helicobacter pylori, a gram-negative bacterium found on the luminal surface of the From the Division of Cardiovascular and
gastric epithelium, was first isolated by Warren and Marshall in 19831 (Fig. 1). It Medical Sciences, University of Glasgow,
Gardiner Institute, Glasgow, United King-
induces chronic inflammation of the underlying mucosa (Fig. 2). The infection is dom. Address reprint requests to Dr. Mc-
usually contracted in the first few years of life and tends to persist indefinitely un- Coll at the Division of Cardiovascular and
less treated.2 Its prevalence increases with older age and with lower socioeconomic Medical Sciences, University of Glasgow,
Gardiner Institute, 44 Church St., Glas-
status during childhood and thus varies markedly around the world.3 The higher gow G11 6NT, United Kingdom, or at
prevalence in older age groups is thought to reflect a cohort effect related to poorer k.e.l.mccoll@clinmed.gla.ac.uk.
living conditions of children in previous decades. At least 50% of the world’s human This article (10.1056/NEJMcp1001110) was
population has H. pylori infection.2 The organism can survive in the acidic environ- updated on August 4, 2010, at NEJM.org.
ment of the stomach partly owing to its remarkably high urease activity; urease
converts the urea present in gastric juice to alkaline ammonia and carbon dioxide.4 N Engl J Med 2010;362:1597-604.
Copyright © 2010 Massachusetts Medical Society.
Infection with H. pylori is a cofactor in the development of three important upper
gastrointestinal diseases: duodenal or gastric ulcers (reported to develop in 1 to 10%
of infected patients), gastric cancer (in 0.1 to 3%), and gastric mucosa-associated
lymphoid-tissue (MALT) lymphoma (in <0.01%). The risk of these disease outcomes
in infected patients varies widely among populations. The great majority of patients An audio version
with H. pylori infection will not have any clinically significant complications. of this article
is available at
Gastric and Duodenal Ulcers NEJM.org
In patients with duodenal ulcers, the inflammation of the gastric mucosa induced by
the infection is most pronounced in the non–acid-secreting antral region of the
stomach and stimulates the increased release of gastrin.5 The increased gastrin
levels in turn stimulate excess acid secretion from the more proximal acid-secreting
fundic mucosa, which is relatively free of inflammation.5,6 The increased duodenal
acid load damages the duodenal mucosa, causing ulceration and gastric metaplasia.
The metaplastic mucosa can then become colonized by H. pylori, which may contrib-
ute to the ulcerative process. Eradication of the infection provides a long-term cure
of duodenal ulcers in more than 80% of patients whose ulcers are not associated
with the use of NSAIDs.7 NSAIDs are the main cause of H. pylori–negative ulcers.
n engl j med 362;17 nejm.org april 29, 2010 1597
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
T he new engl and jour nal of medicine
Figure 1. Helicobacter pylori.
H. pylori is a gram-negative bacterium with a helical Figure 2. Gastric-Biopsy Specimen Showing Helico-
rod shape. It has prominent flagellae, facilitating its bacter pylori Adhering to Gastric Epithelium and
penetration of the thick mucous layer in the stomach. Underlying Inflammation.
H. pylori is visible as small black rods (arrows) on the
epithelial surface and within the glands. The underly-
Ulceration of the gastric mucosa is believed to ing mucosa shows inflammatory-cell infiltrates.
be due to the damage to the mucosa caused by
H. pylori. As with duodenal ulcers, eradicating the
infection usually cures the disease, provided that specimens of the gastric mucosa often reveal the
the gastric ulcer is not due to NSAIDs.8 presence of H. pylori and associated inflammation,
although this finding is also common in persons
Gastric Cancer without upper gastrointestinal symptoms. Most
Extensive epidemiologic data suggest strong asso- randomized trials of therapy for H. pylori eradica-
ciations between H. pylori infection and noncar- tion in patients with nonulcer dyspepsia have
dia gastric cancers (i.e., those distal to the gastro- shown no significant benefit regarding symp-
esophageal junction).9 The infection is classified toms; a few have shown a marginal benefit,16,17
as a human carcinogen by the World Health Or- but this can be explained by the presence of un-
ganization.10 The risk of cancer is highest among recognized ulceration.18 There is thus little evi-
patients in whom the infection induces inflam- dence that chronic H. pylori infection in the ab-
mation of both the antral and fundic mucosa and sence of gastric or duodenal ulceration causes
causes mucosal atrophy and intestinal metapla- upper gastrointestinal symptoms.
sia.11 Eradication of H. pylori infection reduces the The prevalence of H. pylori infection is lower
progression of atrophic gastritis, but there is little among patients with gastroesophageal reflux dis-
evidence of reversal of atrophy or intestinal meta- ease (GERD) 19 and those with esophageal adeno-
plasia, and it remains unclear whether eradica-
12 carcinoma (which may arise as a complication of
tion reduces the risk of gastric cancer. 13 GERD) than among healthy controls. 20 H. pylori–
associated atrophic gastritis, which reduces acid
Gastric MALT Lymphoma secretion, may provide protection against these
Epidemiologic studies have also shown strong as- diseases. A recent meta-analysis showed no sig-
sociations between H. pylori infection and the pres- nificant association between H. pylori eradication
ence of gastric MALT lymphomas.14 Furthermore, and an increased risk of GERD.21
eradication of the infection causes regression of
most localized gastric MALT lymphomas.15 S tr ate gie s a nd Ev idence
Other Gastrointestinal Conditions Candidates for Testing for H. pylori
At least 50% of persons who undergo endoscopy Infection
for upper gastrointestinal symptoms have no evi- Since the vast majority of patients with H. pylori
dence of esophagitis or gastric or duodenal ulcer- infection do not have any related clinical disease,
ation and are considered to have nonulcer or routine testing is not considered appropriate.22,23
functional dyspepsia. In such patients, biopsy Definite indications for identifying and treating
1598 n engl j med 362;17 nejm.org april 29, 2010
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical practice
the infection are confirmed gastric or duodenal particularly useful in clinical practice for identi-
ulcers and gastric MALT lymphoma.22,23 Testing fying patients with ulcer dyspepsia and those
for infection, and subsequent eradication, also with nonulcer dyspepsia.29
seems prudent after resection of early gastric can- In randomized trials comparing a noninvasive
cers.24 In addition, European guidelines recom- test-and-treat strategy with early endoscopy26,27
mend eradicating H. pylori infection in first-degree or with proton-pump–inhibitor therapy,30,31 the
relatives of patients with gastric cancer and in three strategies resulted in a similar degree of
patients with atrophic gastritis, unexplained iron- symptom improvement, but early endoscopy was
deficiency anemia, or chronic idiopathic thrombo- more expensive than the other two strategies. 32
cytopenic purpura, although the data in support However, the test-and-treat strategy is unlikely
of these recommendations are scant.23 to be cost-effective in populations with a preva-
Patients with uninvestigated, uncomplicated lence of H. pylori infection below 20%.33 Infor-
dyspepsia may also undergo testing for H. pylori mation is lacking on the longer-term outcomes
infection by means of a nonendoscopic (noninva- of these strategies.
sive) method22,23,25; eradication therapy is pre-
scribed for patients with positive test results. Tests for H. pylori Infection
The rationale for this strategy is that in some pa- Table 1 summarizes the various tests for H. pylori
tients with dyspepsia, underlying H. pylori–induced infection.
ulcer disease is causing their symptoms. This
nonendoscopic strategy is not appropriate for Nonendoscopic Tests
patients with accompanying alarm symptoms Serologic testing for IgG antibodies to H. pylori is
(e.g., weight loss, persistent vomiting, or gastro- often used to detect infection. However, a meta-
intestinal bleeding) or for older patients (≥45 or analysis of studies of several commercially avail-
≥55 years of age, depending on the specific set able quantitative serologic assays showed an
of guidelines) with new-onset dyspepsia, in whom overall sensitivity and specificity of only 85% and
endoscopy is warranted.22,23,25 The nonendoscopic 79%, respectively.34 The appropriate cutoff values
strategy is also not generally recommended for vary among populations, and the test results are
patients with NSAID-associated dyspepsia, since often reported as positive, negative, or equivocal.
NSAIDs can cause ulcers in the absence of H. py- Also, this test has little value in confirming erad-
lori infection. ication of the infection, because the antibodies
An attraction of the test-and-treat strategy is persist for many months, if not longer, after
that it avoids the discomfort and costs of endos- eradication.
copy. However, because only a minority of pa- The urea breath test involves drinking 13C-
tients with dyspepsia who have a positive H. pylori labeled or 14C-labeled urea, which is converted
test have underlying ulcer disease, 26,27 most pa- to labeled carbon dioxide by the urease in H. py-
tients treated by means of the test-and-treat strat- lori. The labeled gas is measured in a breath
egy incur the inconvenience, costs, and potential sample. The test has a sensitivity and a specific-
side effects of therapy without a benefit. In a ity of 95%.35 The infection can also be detected
placebo-controlled trial of empirical treatment by identifying H. pylori–specific antigens in a
involving 294 patients with uninvestigated dys- stool sample with the use of polyclonal or mono-
pepsia and a positive H. pylori breath test, the clonal antibodies (the fecal antigen test).36 The
1-year rate of symptom resolution was 50% in monoclonal-antibody test (which also has a
those receiving H. pylori–eradication therapy, as specificity and a sensitivity of 95%36) is more
compared with 36% of those receiving placebo accurate than the polyclonal-antibody test. For
(P = 0.02)28; 7 patients would need to receive both the breath test and the fecal antigen test,
eradication therapy for 1 patient to have a benefit. the patient should stop taking proton-pump in-
A greater benefit would be expected if treatment hibitors 2 weeks before testing, should stop tak-
were limited to patients with an increased prob- ing H2 receptor antagonists for 24 hours before
ability of having an ulcer. However, neither the testing, and should avoid taking antimicrobial
characteristics of the symptoms nor the presence agents for 4 weeks before testing, since these
of other risk factors for ulcer (e.g., male sex, medications may suppress the infection and re-
smoking, and family history of ulcer disease) are duce the sensitivity of testing.
n engl j med 362;17 nejm.org april 29, 2010 1599
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
T he new engl and jour nal of medicine
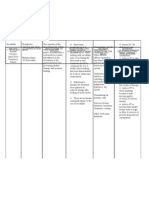
Table 1. Tests for Helicobacter pylori Infection.
Test Advantages Disadvantages
Nonendoscopic
Serologic test Widely available; the least expensive of available Positive result may reflect previous rather than current in-
tests fection; not recommended for confirming eradication
Urea breath test High negative and positive predictive values; False negative results possible in the presence of PPIs or with
useful before and after treatment recent use of antibiotics or bismuth preparations; consid-
erable resources and personnel required to perform test
Fecal antigen test High negative and positive predictive values with Process of stool collection may be distasteful to patient;
monoclonal-antibody test; useful before and false negative results possible in the presence of PPIs or
after treatment with recent use of antibiotics or bismuth preparations
Endoscopic
Urease-based tests Rapid, inexpensive, and accurate in selected False negative results possible in the presence of PPIs or
patients with recent use of antibiotics or bismuth preparations
Histologic assessment Good sensitivity and specificity Requires trained personnel
Culture Excellent specificity; provides opportunity to test Variable sensitivity; requires trained staff and properly
for antibiotic sensitivity equipped facilities
PPI denotes proton-pump inhibitor.
Endoscopic Tests Treatment of H. pylori Infection
H. pylori infection can be detected on endoscopic Various drug regimens are used to treat H. pylori
biopsy of the gastric mucosa, by means of several infection (Table 2). Most include two antibiotics
techniques. The biopsy specimens are usually plus a proton-pump inhibitor or a bismuth prep-
taken from the prepyloric region, but an addi- aration (or both). The most commonly used ini-
tional biopsy specimen obtained from the fundic tial treatment is triple therapy consisting of a
mucosa may increase the test’s sensitivity, espe- proton-pump inhibitor plus clarithromycin and
cially if the patient has recently been treated with amoxicillin, each given twice per day for 7 to 14
a proton-pump inhibitor. days. Metronidazole is used in place of amoxicil-
The urease-based method involves placement lin in patients with a penicillin allergy.
of the endoscopic biopsy specimen in a solution The recommended duration of triple therapy
of urea and pH-sensitive dye. If H. pylori is pres- is typically 10 to 14 days in the United States and
ent, its urease converts the urea to ammonia, in- 7 days in Europe.22,23 A recent meta-analysis of
creasing the pH and changing the color of the 21 randomized trials showed that the rate of
dye. Recommendations for avoiding proton-pump eradication was increased by 4 percentage points
inhibitors, H2 receptor antagonists, and anti- with the use of triple therapy for 10 days as com-
microbial therapy before testing apply to this test pared with 7 days and by 5 percentage points
as well, to minimize the chance of false negative with the use of triple therapy for 14 days as com-
results.37 The test has a sensitivity of more than pared with 7 days38 — absolute differences that
90% and a specificity of more than 95%.35 are statistically significant but of marginal clin-
Another means of diagnosis involves routine ical significance.
histologic testing of a biopsy specimen; if there Another possible initial therapy in areas with
is H. pylori infection, the organism and associ- a high prevalence of clarithromycin-resistant
ated gastritis are apparent on sections stained H. pylori infection (i.e., >20%) is quadruple ther-
with hematoxylin and eosin or Giemsa. Although apy comprising the use of a proton-pump inhibi-
culturing of the organism is also possible and tor, tetracycline, metronidazole, and a bismuth salt
permits testing for sensitivity to antimicrobial for 10 to 14 days23; however, bismuth salts are
agents, facilities for the culture of H. pylori are not available in some countries. A recent meta-
not widely available and the method is relatively analysis of 93 studies showed a higher rate of
insensitive. eradication with quadruple therapy that included
1600 n engl j med 362;17 nejm.org april 29, 2010
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical practice
both clarithromycin and metronidazole than
Table 2. Regimens Used to Treat Helicobacter pylori Infection.
with triple therapy that included both these
agents in populations with either clarithromy- Standard initial treatment (use one of the following three options)
cin or metronidazole resistance.39 Triple therapy for 7–14 days
An alternative initial regimen is 10-day se- PPI, healing dose twice/day
quential therapy, involving a proton-pump inhibi- Amoxicillin, 1 g twice/day†
tor plus amoxicillin for 5 days followed by a Clarithromycin, 500 mg twice/day
proton-pump inhibitor plus clarithromycin and Quadruple therapy for 10–14 days‡
tinidazole for 5 more days. This regimen was
PPI, healing dose twice/day
reported to achieve an eradication rate of 93%,
Tripotassium dicitratobismuthate, 120 mg four times/day
as compared with a rate of 77% with standard
Tetracycline, 500 mg four times/day
triple therapy, in a meta-analysis of 10 random-
ized trials in Italy.40 However, in a trial in Spain, Metronidazole, 250 mg four times/day§
the eradication rate among patients randomly Sequential therapy
assigned to receive sequential therapy was only Days 1–5
84%, indicating a need to confirm its efficacy PPI, healing dose twice/day
before it is used widely.41 Amoxicillin, 1 g twice/day
Days 6–10
Confirmation of Eradication PPI, healing dose twice/day
It is important to confirm the eradication of Clarithromycin, 500 mg twice/day
H. pylori infection in patients who have had an Tinidazole, 500 mg twice/day§
H. pylori–associated ulcer or gastric MALT lym- Second-line therapy, if triple therapy involving clarithromycin was used initially
phoma or who have undergone resection for early (use one or the other)
gastric cancer.22,23 In addition, to avoid repeated Triple therapy for 7–14 days
treatment of patients whose symptoms are not PPI, healing dose once/day
attributable to H. pylori, follow-up testing is indi- Amoxicillin, 1 g twice/day
cated in patients whose symptoms persist after Metronidazole, 500 mg (or 400 mg) twice/day§
H. pylori eradication treatment for dyspepsia. Eradi-
Quadruple therapy, as recommended for initial therapy
cation may be confirmed by means of a urea
breath test or fecal antigen test; these are per- Examples of healing doses of proton-pump inhibitors (PPIs) include the follow-
formed 4 weeks or longer after completion of ther- ing regimens, all twice per day: omeprazole at a dose of 20 mg, esomeprazole
at a dose of 20 mg, rabeprazole at a dose of 20 mg, pantoprazole at a dose of
apy, to avoid false negative results due to suppres- 40 mg, and lansoprazole at a dose of 30 mg. In some studies, esomeprazole
sionof H.pylori. Eradicationcanalsobeconfirmed
22
has been given at a dose of 40 mg once per day.
by testing during repeat endoscopy (Table 1) for † If the patient has an allergy to amoxicillin, substitute metronidazole (at a dose
of 500 mg or 400 mg) twice per day and (in initial triple therapy only) use
patients in whom endoscopy is required. clarithromycin at reduced dose of 250 mg twice per day.
‡ Quadruple therapy is appropriate as first-line treatment in areas in which the
Management of Persistent Infection prevalence of resistance to clarithromycin or metronidazole is high (>20%) or
after Treatment in patients with recent or repeated exposure to clarithromycin or metronidazole.
§ Alcohol should be avoided during treatment with metronidazole or tinidazole,
Before prescribing a second course of therapy, it is owing to the potential for a reaction resembling the reaction to disulfiram with
important to confirm that the infection is still pres- alcohol use.
ent and consider whether additional antimicrobial
treatment is appropriate. Further attempts at erad-
ication are indicated in patients with confirmed pirical acid-inhibitory therapy, endoscopy to check
ulcer or gastric MALT lymphoma or after resec- for underlying ulcer or another cause of symp-
tion for early gastric cancer. However, if the ini- toms, and repeat use of the noninvasive test-and-
tial therapy was for uninvestigated dyspepsia, treat strategy. The possibility that symptoms may
which is associated with a low likelihood of un- be due to a different cause (e.g., biliary tract,
derlying ulcer and symptomatic benefit from erad- pancreatic, musculoskeletal, or cardiac disease or
ication, the appropriateness of further eradication psychosocial stress) should routinely be consid-
therapy is unclear; data from studies designed to ered. If another course of therapy is administered
determine the optimal management of such cases to eradicate H. pylori infection, the importance of
are lacking. Options for treatment include em- adherence to the treatment regimen should be
n engl j med 362;17 nejm.org april 29, 2010 1601
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
T he new engl and jour nal of medicine
for culturing H. pylori and performing sensitivity
Table 3. Guidelines for Evaluation and Management of Helicobacter pylori
Infection. testing and experience with alternative treatments
for the infection. Several regimens have been re-
American College Maastricht III ported to be effective as salvage therapy in case
of Gastroenterology Consensus Report
series. For example, retreatment after treatment
Criteria for testing
failure with a triple regimen consisting of levo-
Active gastric or duodenal ulcer, his- Same as American College of Gastro- floxacin or rifabutin, along with a proton-pump
tory of active gastric or duodenal enterology criteria, with the follow-
ulcer not previously treated for ing additional criteria: gastric can- inhibitor and amoxicillin, has been associated
H. pylori infection, gastric MALT cer in first-degree relative, atrophic with high rates of eradication.45-47 However, cau-
lymphoma, history of endoscop- gastritis, unexplained iron-deficien- tion is warranted in the use of rifabutin, which
ic resection of early gastric can- cy anemia, or chronic idiopathic
cer, or uninvestigated dyspepsia thrombocytopenic purpura† may lead to resistance of mycobacteria in pa-
Criteria for test-and-treat strategy tients with preexisting mycobacterial infection.
Age <55 yr and no alarm symptoms§ Age <45 yr and no alarm symptoms‡§
Duration of therapy A r e a s of Uncer ta in t y
10–14 Days 7 Days
Data from randomized trials are lacking to guide
The American College of Gastroenterology guidelines are reported by Chey, the care of patients whose symptoms persist after
Wong, and the Practice Parameters Committee of the American College of completion of H. pylori eradication therapy for
Gastroenterology22; the Maastricht III consensus report guidelines are reported
uninvestigated dyspepsia. The effect of eradica-
by Malfertheiner and colleagues.23 MALT denotes mucosa-associated lymphoid
tissue. tion of H. pylori infection on the risk of gastric
† Eradication of H. pylori in patients with chronic idiopathic thrombocytopenic cancer is unclear but is currently under study.
purpura has been reported to increase the platelet count, although the data
are limited.
‡ The age cutoff varies among countries, depending on the prevalence of upper Guidel ine s
gastrointestinal cancer.
§ Alarm symptoms include dysphagia, weight loss, evidence of gastrointestinal
The American College of Gastroenterology guide-
bleeding, and persistent vomiting.
lines22 and the Maastricht guidelines23 differ
slightly in their recommendations for testing and
emphasized, since poor adherence may underlie treatment of H. pylori infection (Table 3).
the failure of initial therapy.
The choice of second-line treatment is influ- Concl usions a nd
enced by the initial treatment (Table 2). Treatment R ec omme nda t ions
failure is often related to H. pylori resistance to
clarithromycin or metronidazole (or both agents). The noninvasive test-and-treat strategy for H. py-
If initial therapy did not include a bismuth salt, lori infection is reasonable for younger patients
bismuth-based quadruple therapy is commonly who have upper gastrointestinal symptoms but
used as second-line therapy, with eradication not alarm symptoms, like the patient in the vi-
rates in case series ranging from 57 to 95%.42 gnette. Noninvasive testing can be performed
Triple therapies have also been tested as second- with the use of the urea breath test, fecal antigen
line therapies in patients in whom initial therapy test, or serologic test; the serologic test is the
failed. A proton-pump inhibitor used in combina- least accurate. Triple therapy with a proton-pump
tion with metronidazole and either amoxicillin inhibitor, clarithromycin, and amoxicillin or
or tetracycline is recommended in patients previ- metronidazole remains an appropriate first-line
ously treated with a proton-pump inhibitor, therapy, provided that there is not a high local
amoxicillin, and clarithromycin. 23,43 Clarithro- rate of clarithromycin resistance. Recurrence or
mycin should be avoided as part of second-line persistence of symptoms after eradication therapy
therapy unless resistance testing confirms that for uninvestigated dyspepsia is much less likely
the H. pylori strain is susceptible to the drug.44 to indicate that treatment has failed than to indi-
Patients in whom H. pylori infection persists cate that the symptoms are unrelated to H. pylori
after a second course of treatment and for whom infection. Further eradication therapy should not
eradication is considered appropriate should be be considered unless persistent H. pylori infection
referred to a specialist with access to facilities is confirmed. Data are lacking to inform the op-
1602 n engl j med 362;17 nejm.org april 29, 2010
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical practice
timal management of recurrent or persistent dys- other potential reasons for the symptoms should
pepsia after noninvasive testing and treatment of also be reconsidered.
H. pylori infection. Options include symptomatic Dr. McColl reports receiving lecture fees from AstraZeneca
acid-inhibitory therapy, endoscopy to check for and Nycomed and consulting fees from Sacoor. No other poten-
tial conflict of interest relevant to this article was reported.
underlying ulcer or another cause of symptoms, Disclosure forms provided by the author are available with the
and repeat of the H. pylori test-and-treat strategy; full text of this article at NEJM.org.
References
1. Warren JR, Marshall BJ. Unidentified 12. Leung WK, Lin SR, Ching JY, et al. C, et al. Current concepts in the manage-
curved bacilli on gastric epithelium in ac- Factors predicting progression of gastric ment of Helicobacter pylori infection: the
tive chronic gastritis. Lancet 1983;1:1273-5. intestinal metaplasia: results of a ran- Maastricht III consensus report. Gut 2007;
2. Everhart JE. Recent developments in domised trial on Helicobacter pylori eradi- 56:772-81.
the epidemiology of Helicobacter pylori. cation. Gut 2004;53:1244-9. 24. Fukase K, Kato M, Kikuchi S, et al.
Gastroenterol Clin North Am 2000;29: 13. Malfertheiner P, Sipponen P, Naumann Effect of eradication of Helicobacter py-
559-79. M, et al. Helicobacter pylori eradication lori on incidence of metachronous gastric
3. Woodward M, Morrison C, McColl K. has the potential to prevent gastric can- carcinoma after endoscopic resection of
An investigation into factors associated cer: a state-of-the-art critique. Am J Gas- early gastric cancer: an open-label, ran-
with Helicobacter pylori infection. J Clin troenterol 2005;100:2100-15. domised controlled trial. Lancet 2008;372:
Epidemiol 2000;53:175-81. 14. Parsonnet J, Hansen S, Rodriguez L, 392-7.
4. Marshall BJ, Barrett LJ, Prakash C, et al. Helicobacter pylori and gastric lym- 25. Talley NJ, Vakil N, Practice Parame-
McCallum RW, Guerrant RL. Urea pro- phoma. N Engl J Med 1994;330:1267-71. ters Committee of the American College
tects Helicobacter (Campylobacter) pylori 15. Fischbach W, Goebeler-Kolve ME, of Gastroenterology. Guidelines for the
from the bactericidal effect of acid. Gas- Dragosics B, Greiner A, Stolte M. Long management of dyspepsia. Am J Gastro-
troenterology 1990;99:697-702. term outcome of patients with gastric enterol 2005;100:2324-37.
5. el-Omar EM, Penman ID, Ardill JES, marginal zone B cell lymphoma of mu- 26. McColl KEL, Murray LS, Gillen D, et
Chittajallu RS, Howie C, McColl KEL. cosa associated lymphoid tissue (MALT) al. Randomised trial of endoscopy with
Helicobacter pylori infection and abnor- following exclusive Helicobacter pylori testing for Helicobacter pylori compared
malities of acid secretion in patients with eradication therapy: experience from a with non-invasive H pylori testing alone
duodenal ulcer disease. Gastroenterology large prospective series. Gut 2004;53: in the management of dyspepsia. BMJ
1995;109:681-91. 34-7. 2002;324:999-1002. [Errata, BMJ 2002;325:
6. Gillen D, el-Omar EM, Wirz AA, Ar- 16. Moayyedi P, Soo S, Deeks J, et al. Sys- 479, 580.]
dill JES, McColl KEL. The acid response to tematic review and economic evaluation 27. Lassen AT, Pedersen FM, Bytzer P,
gastrin distinguishes duodenal ulcer pa- of Helicobacter pylori eradication treat- Schaffalitzky de Muckadell OB. Helico-
tients from Helicobacter pylori-infected ment for non-ulcer dyspepsia. BMJ 2000; bacter pylori test-and-eradicate versus
healthy subjects. Gastroenterology 1998; 321:659-64. prompt endoscopy for management of
114:50-7. 17. Laine L, Schoenfeld P, Fennerty MB. dyspeptic patients: a randomised trial.
7. Hentschel E, Brandstätter G, Drag- Therapy for Helicobacter pylori in patients Lancet 2000;356:455-60.
osics B, et al. Effect of ranitidine and with nonulcer dyspepsia: a meta-analysis 28. Chiba N, Van Zanten SJO, Sinclair P,
amoxicillin plus metronidazole on the of randomized, controlled trials. Ann In- Ferguson RA, Escobedo S, Grace E. Treat-
eradication of Helicobacter pylori and the re- tern Med 2001;134:361-9. ing Helicobacter pylori infection in pri-
currence of duodenal ulcer. N Engl J Med 18. McColl KEL. Absence of benefit of mary care patients with uninvestigated
1993;328:308-12. eradicating Helicobacter pylori in patients dyspepsia: the Canadian adult dyspepsia
8. Axon ATR, O’Moráin CA, Bardhan with nonulcer dyspepsia. N Engl J Med empiric treatment–Helicobacter pylori pos-
KD, et al. Randomised double blind con- 2000;342:589. itive (CADET-Hp) randomised controlled
trolled study of recurrence of gastric ulcer 19. Raghunath A, Hungin AP, Wooff D, trial. BMJ 2002;324:1012-6.
after treatment for eradication of Helico- Childs S. Prevalence of Helicobacter py- 29. The Danish Dyspepsia Study Group.
bacter pylori infection. BMJ 1997;314: lori in patients with gastro-oesophageal Value of the unaided clinical diagnosis in
565-8. reflux disease: systematic review. BMJ dyspepsia patients in primary care. Am J
9. Hansen S, Melby KK, Aase S, Jellum E, 2003;326:737-9. Gastroenterol 2001;96:1417-21.
Vollset SE. Helicobacter pylori infection 20. de Martel C, Llosa AE, Farr SM, et al. 30. Jarbol DE, Kragstrup J, Stovring H,
and risk of cardia cancer and non-cardia Helicobacter pylori infection and the risk Havelund T, Schaffalitzky de Muckadell
gastric cancer: a nested case-control study. of development of esophageal adenocarci- OB. Proton pump inhibitor or testing for
Scand J Gastroenterol 1999;34:353-60. noma. J Infect Dis 2005;191:761-7. Helicobacter pylori as the first step for pa-
10. Infection with Helicobacter pylori. In: 21. Yaghoobi M, Farrokhyar F, Yuan Y, tients presenting with dyspepsia? A cluster-
IARC Working Group on the Evaluation Hunt RH. Is there an increased risk of randomized trial. Am J Gastroenterol
of Carcinogenic Risks to Humans. IARC GERD after Helicobacter pylori eradica- 2006;101:1200-8.
monographs on the evaluation of carcino- tion? A meta-analysis. Am J Gastroenterol 31. Manes G, Menchise A, de Nucci C,
genic risks to humans. Vol. 61. Schisto- 2010 January 19 (Epub ahead of print). Balzano A. Empirical prescribing for dys-
somes, liver flukes and Helicobacter pylori. 22. Chey WD, Wong BCY, Practice Param- pepsia: randomised controlled trial of test
Lyon, France: International Agency for eters Committee of the American College and treat versus omeprazole treatment.
Research on Cancer, 1994:177-240. of Gastroenterology. American College of BMJ 2003;326:1118.
11. Uemura N, Okamoto S, Yamamoto S, Gastroenterology guideline on the man- 32. Delaney BC, Innes MA, Deeks J, et al.
et al. Helicobacter pylori infection and the agement of Helicobacter pylori infection. Initial management strategies for dyspep-
development of gastric cancer. N Engl J Am J Gastroenterol 2007;102:1808-25. sia. Cochrane Database Syst Rev 2001;3:
Med 2001;345:784-9. 23. Malfertheiner P, Megraud F, O’Morain CD001961.
n engl j med 362;17 nejm.org april 29, 2010 1603
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical practice
33. Delaney BC, Moayyedi P, Forman D. 39. Fischbach L, Evans EL. Meta-analysis: 44. Lamouliatte H, Mégraud F, Delchier
Initial management strategies for dyspep- the effect of antibiotic resistance status JC, et al. Second-line treatment for failure
sia. Cochrane Database Syst Rev 2003;2: on the efficacy of triple and quadruple to eradicate Helicobacter pylori: a random-
CD001961. first-line therapies for Helicobacter pylori. ized trial comparing four treatment strat-
34. Loy CT, Irwig LM, Katelaris PH, Talley Aliment Pharmacol Ther 2007;26:343-57. egies. Aliment Pharmacol Ther 2003;18:
NJ. Do commercial serological kits for 40. Jafri NS, Hornung CA, Howden CW. 791-7.
Helicobacter pylori infection differ in ac- Meta-analysis: sequential therapy appears 45. Gisbert JP, Morena F. Systematic review
curacy? A meta-analysis. Am J Gastroen- superior to standard therapy for Helico- and meta-analysis: levofloxacin-based res-
terol 1996;91:1138-44. bacter pylori infection in patients naive to cue regimens after Helicobacter pylori
35. Vaira D, Vakil N. Blood, urine, stool, treatment. Ann Intern Med 2008;148:923- treatment failure. Aliment Pharmacol Ther
breath, money, and Helicobacter pylori. 31. [Erratum, Ann Intern Med 2008;149: 2006;23:35-44.
Gut 2001;48:287-9. 439.] 46. Saad RJ, Schoenfeld P, Kim HM, Chey
36. Gisbert JP, Pajares JM. Stool antigen 41. Sánchez-Delgade J, Calvet X, Bujanda L, WD. Levofloxacin-based triple therapy
test for the diagnosis of Helicobacter py- Gisbert JP, Titó L, Castro M. Ten-day se- versus bismuth-based quadruple therapy
lori infection: a systematic review. Helico- quential treatment for Helicobacter pylori for persistent Helicobacter pylori infec-
bacter 2004;9:347-68. eradication in clinical practice. Am J Gas- tion: a meta-analysis. Am J Gastroenterol
37. Midolo P, Marshall BJ. Accurate diag- troenterol 2008;103:2220-3. 2006;101:488-96.
nosis of Helicobacter pylori: urease tests. 42. Gisbert JP, Pajares JM. Helicobacter 47. Qasim A, Sebastian S, Thornton O,
Gastroenterol Clin North Am 2000;29: pylori “rescue” regimen when proton pump et al. Rifabutin- and furazolidone-based
871-8. inhibitor-based triple therapies fail. Ali- Helicobacter pylori eradication therapies
38. Fuccio L, Minardi ME, Zagari RM, ment Pharmacol Ther 2002;16:1047-57. after failure on standard first- and second-
Grilli D, Magrini N, Bazzoli F. Meta-analy- 43. Realdi G, Dore MP, Piana A, et al. Pre- line eradication attempts in dyspepsia pa-
sis: duration of first-line proton-pump treatment antibiotic resistance in Helico- tients. Aliment Pharmacol Ther 2005;21:
inhibitor based triple therapy for Helico- bacter pylori infection: results of three 91-6.
bacter pylori eradication. Ann Intern Med randomized controlled studies. Helico- Copyright © 2010 Massachusetts Medical Society.
2007;147:553-62. bacter 1999;4:106-12.
full text of all journal articles on the world wide web
Access to the complete contents of the Journal on the Internet is free to all subscribers. To use this Web site, subscribers should
go to the Journal’s home page (NEJM.org) and register by entering their names and subscriber numbers as they appear on their
mailing labels. After this one-time registration, subscribers can use their passwords to log on for electronic access to the entire
Journal from any computer that is connected to the Internet. Features include a library of all issues since January 1993 and
abstracts since January 1975, a full-text search capacity, and a personal archive for saving articles and search results of interest.
All articles can be printed in a format that is virtually identical to that of the typeset pages. Beginning 6 months after
publication, the full text of all Original Articles and Special Articles is available free to nonsubscribers.
1604 n engl j med 362;17 nejm.org april 29, 2010
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Você também pode gostar
- Pediatric Gastritis, Gastropathy, and Peptic Ulcer Disease: Education GapDocumento10 páginasPediatric Gastritis, Gastropathy, and Peptic Ulcer Disease: Education GapvgmanjunathAinda não há avaliações
- Platelet Disorders: Practice GapsDocumento14 páginasPlatelet Disorders: Practice GapsMichelleHanAinda não há avaliações
- Bronquiolite Guidelines AAPDocumento32 páginasBronquiolite Guidelines AAPDiego Guedes da SilvaAinda não há avaliações
- Pediatrics in Review 2013 SalmonelosisDocumento11 páginasPediatrics in Review 2013 SalmonelosisCarlos Elio Polo VargasAinda não há avaliações
- Guillian Barre SyndromeDocumento11 páginasGuillian Barre SyndromemohamedAinda não há avaliações
- Guia Aspergilosis Ats Idsa 2016 PDFDocumento60 páginasGuia Aspergilosis Ats Idsa 2016 PDFdayanamikiAinda não há avaliações
- DR Bragg - Endocarditis - Pediatric in Review April 2014Documento9 páginasDR Bragg - Endocarditis - Pediatric in Review April 2014angelicaAinda não há avaliações
- Update On Diarrhea - Peds in Rev 2016Documento12 páginasUpdate On Diarrhea - Peds in Rev 2016TriLightAinda não há avaliações
- Candida LipolyticaDocumento3 páginasCandida LipolyticaVarun Singh ChandelAinda não há avaliações
- Albumin InfusionDocumento21 páginasAlbumin InfusiondinniAinda não há avaliações
- Nutritional Healing For Multiple SclerosisDocumento6 páginasNutritional Healing For Multiple SclerosisBrian Hunter Levins Jr.Ainda não há avaliações
- "Towards Eradicating Tuberculosis" - Aetiopathogenesis of TuberculosisDocumento29 páginas"Towards Eradicating Tuberculosis" - Aetiopathogenesis of Tuberculosisibnbasheer100% (7)
- Pediatrics in Review 2000 Schwartz 257 64Documento10 páginasPediatrics in Review 2000 Schwartz 257 64Aina NurlailaAinda não há avaliações
- Nac 2017Documento18 páginasNac 2017Nataly CortesAinda não há avaliações
- 2013 34 216 Shashi Sahai: Pediatrics in ReviewDocumento14 páginas2013 34 216 Shashi Sahai: Pediatrics in ReviewcarlospinopedAinda não há avaliações
- Common Dysmorphic Syndromes in The NICUDocumento12 páginasCommon Dysmorphic Syndromes in The NICUDaniel PuertasAinda não há avaliações
- Very Update Information About MedicineDocumento13 páginasVery Update Information About MedicinetriAinda não há avaliações
- High Fever, Maculopapular Rash, Perianal Desquamation, and Conjunctivitis in A 3-Year-Old BoyDocumento8 páginasHigh Fever, Maculopapular Rash, Perianal Desquamation, and Conjunctivitis in A 3-Year-Old BoyTri ApriastiniAinda não há avaliações
- Pediatrics in Review-2013-Sahai-216-27Documento14 páginasPediatrics in Review-2013-Sahai-216-27Facu GuerreroAinda não há avaliações
- Introduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPDocumento66 páginasIntroduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPphoenix18075% (4)
- MenstrualDisorders - PIR .2013 PDFDocumento15 páginasMenstrualDisorders - PIR .2013 PDFlina robayoAinda não há avaliações
- Pulmonary Diseases - Dental ManagementDocumento45 páginasPulmonary Diseases - Dental Managementfilyouth4life100% (3)
- Bronchiolitis: Practice GapsDocumento11 páginasBronchiolitis: Practice GapsMichelleHanAinda não há avaliações
- Aap-Bordetella Pertussis (Pertussis)Documento13 páginasAap-Bordetella Pertussis (Pertussis)Ana BlueAinda não há avaliações
- Nosocomial Infection.2Documento19 páginasNosocomial Infection.2Antonius SbbrAinda não há avaliações
- Inflamatory Bowel Disease: Dr. Samir IsmailDocumento82 páginasInflamatory Bowel Disease: Dr. Samir IsmailGhadeer EbraheemAinda não há avaliações
- FLUID MANAGEMENT IN MALNUTRITIONDocumento30 páginasFLUID MANAGEMENT IN MALNUTRITIONCHALIE MEQUAinda não há avaliações
- Pediatric Cervical LymphadenopathyDocumento13 páginasPediatric Cervical LymphadenopathyShaira Aquino VerzosaAinda não há avaliações
- Acrodermatitis EnteropathicaDocumento4 páginasAcrodermatitis EnteropathicaIntan FajrinAinda não há avaliações
- Dka, Cerebral Edema, HhsDocumento90 páginasDka, Cerebral Edema, HhsNazafAinda não há avaliações
- Recent Developments in The Management of Neonatal HyperbilirubinemiaDocumento8 páginasRecent Developments in The Management of Neonatal HyperbilirubinemiaMyrtle SetiawanAinda não há avaliações
- PA 514 Intro To Infectious Disease SyllabusDocumento11 páginasPA 514 Intro To Infectious Disease Syllabuslu100% (1)
- Management of Diabetic Ketoacidosis in Children and AdolescentsDocumento8 páginasManagement of Diabetic Ketoacidosis in Children and AdolescentsnurlatifahAinda não há avaliações
- BacteriaDocumento168 páginasBacteriadenekeAinda não há avaliações
- Foreign Body AspirationDocumento3 páginasForeign Body AspirationAsiya ZaidiAinda não há avaliações
- Clinical Review of Hereditary HaemochromatosisDocumento6 páginasClinical Review of Hereditary HaemochromatosisVijeyachandhar DorairajAinda não há avaliações
- Medical Case 1: Language Centre of Malahayati University at 2010Documento16 páginasMedical Case 1: Language Centre of Malahayati University at 2010putri1114Ainda não há avaliações
- Kawasaki Disease: Education GapDocumento15 páginasKawasaki Disease: Education GapEddy TubónAinda não há avaliações
- Diabetes InsipidusDocumento10 páginasDiabetes InsipidussoniaAinda não há avaliações
- Stafilococo AureusDocumento15 páginasStafilococo AureusJose MosqueraAinda não há avaliações
- Streptococcal Pharyngitis Diagnosis and TreatmentDocumento33 páginasStreptococcal Pharyngitis Diagnosis and TreatmentIkrimaikAinda não há avaliações
- Chapter6 TB MeningitisDocumento50 páginasChapter6 TB MeningitisAldwin BagtasAinda não há avaliações
- Approach To The Child With Anemia - UpToDateDocumento41 páginasApproach To The Child With Anemia - UpToDateDaniel Enrique CardenasAinda não há avaliações
- Adolescents With Tuberculosis-A Review of 145 Cases, 2016Documento5 páginasAdolescents With Tuberculosis-A Review of 145 Cases, 2016Yoseph Arif Putra100% (1)
- COVID 19AndHematology IndiaDocumento6 páginasCOVID 19AndHematology IndiaVandana SharmaAinda não há avaliações
- Peritonsillar AbscessDocumento15 páginasPeritonsillar AbscessFitria MaryolinAinda não há avaliações
- Infectious Diseases (1&2) : TuberculosisDocumento67 páginasInfectious Diseases (1&2) : TuberculosisYesi SaputriAinda não há avaliações
- Infectious Diseases in Pregnancy - 2005 Vol.32 Issues 3Documento290 páginasInfectious Diseases in Pregnancy - 2005 Vol.32 Issues 3Rickky Kurniawan,MDAinda não há avaliações
- Guide to Hemolytic Anemia Causes and SymptomsDocumento18 páginasGuide to Hemolytic Anemia Causes and SymptomsAdisurya NugrahaAinda não há avaliações
- A Summary of The Chemical Mediators Involve in The Acute Inflammatory Response Is Shown in The Table BelowDocumento30 páginasA Summary of The Chemical Mediators Involve in The Acute Inflammatory Response Is Shown in The Table Belowinny100% (1)
- Adjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Documento9 páginasAdjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Edrei Lopez CAinda não há avaliações
- Krisis HipertensiDocumento12 páginasKrisis HipertensiDani NurseAinda não há avaliações
- EMS Infectious Disease PlaybookDocumento86 páginasEMS Infectious Disease PlaybookAryttAinda não há avaliações
- Hemolytic Uremic Syndrome A Case ReportDocumento3 páginasHemolytic Uremic Syndrome A Case ReportAna-Mihaela BalanuțaAinda não há avaliações
- 10 - Infectious Diseases (9700 AS Biology)Documento33 páginas10 - Infectious Diseases (9700 AS Biology)ho100% (1)
- Pediatrics Review 姞: ArticlesDocumento43 páginasPediatrics Review 姞: ArticlesKevinJuliusTanadyAinda não há avaliações
- Anaerobic Infections in HumansNo EverandAnaerobic Infections in HumansSydney FinegoldNota: 5 de 5 estrelas5/5 (1)
- Severe Asthma With Fungal Sensitization: A Case Report and Review of LiteratureDocumento7 páginasSevere Asthma With Fungal Sensitization: A Case Report and Review of LiteratureNovitaAinda não há avaliações
- Tuberculous Pyopneumothorax As A Complication of IDocumento6 páginasTuberculous Pyopneumothorax As A Complication of INovitaAinda não há avaliações
- RigelDocumento52 páginasRigeldewiulfaAinda não há avaliações
- Station UjianDocumento3 páginasStation UjianNovitaAinda não há avaliações
- Station UjianDocumento3 páginasStation UjianNovitaAinda não há avaliações
- Hearing LossDocumento10 páginasHearing LossNovitaAinda não há avaliações
- Acute Pancreatitis and Alcohol Abuse: A Case: NutritionDocumento2 páginasAcute Pancreatitis and Alcohol Abuse: A Case: NutritionNovitaAinda não há avaliações
- UntitledDocumento1 páginaUntitledNovitaAinda não há avaliações
- The Role Endoscopy For IbdDocumento34 páginasThe Role Endoscopy For IbdNovitaAinda não há avaliações
- Hearing LossDocumento10 páginasHearing LossNovitaAinda não há avaliações
- Daftar PustakaDocumento3 páginasDaftar PustakarestyNZAinda não há avaliações
- Daftar PustakaDocumento3 páginasDaftar PustakarestyNZAinda não há avaliações
- Jurnal NIHL NovitaDocumento10 páginasJurnal NIHL NovitaNovitaAinda não há avaliações
- Daftar PustakaDocumento3 páginasDaftar PustakarestyNZAinda não há avaliações
- Station UjianDocumento3 páginasStation UjianNovitaAinda não há avaliações
- SDF GHSDFHDocumento2 páginasSDF GHSDFHNovitaAinda não há avaliações
- Echocardiography ExaminationDocumento73 páginasEchocardiography ExaminationNovita100% (2)
- OxytocicsDocumento36 páginasOxytocicsNovitaAinda não há avaliações
- Vascular ExaminationDocumento22 páginasVascular ExaminationNovitaAinda não há avaliações
- Medical Ethics: See Also: Legal Medicine, Humanism, Medical Interview, Professionalism, Critical CareDocumento3 páginasMedical Ethics: See Also: Legal Medicine, Humanism, Medical Interview, Professionalism, Critical CarecyelzAinda não há avaliações
- Antiinflamasi Steroid GlucocorticoidDocumento18 páginasAntiinflamasi Steroid GlucocorticoidNovitaAinda não há avaliações
- UrolithiasisDocumento1 páginaUrolithiasisNovitaAinda não há avaliações
- Journal of The Neurological Sciences: Naghmeh Jafari, Rogier Q. HintzenDocumento8 páginasJournal of The Neurological Sciences: Naghmeh Jafari, Rogier Q. HintzenNovitaAinda não há avaliações
- Probiotics Review and Future AspectsDocumento5 páginasProbiotics Review and Future AspectsInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Vomiting: Compendium (Yardley, PA) February 2009Documento10 páginasVomiting: Compendium (Yardley, PA) February 2009Vini SasmitaAinda não há avaliações
- EsophagogastroduodenosDocumento6 páginasEsophagogastroduodenosdrnareshkumar3281Ainda não há avaliações
- Peptic Ulcer - Causes, Treatment, and PreventionDocumento24 páginasPeptic Ulcer - Causes, Treatment, and PreventionAmfo Baffoe FrederickAinda não há avaliações
- Gastric Outlet Obstruction (Soltan Aiman NeazyDocumento49 páginasGastric Outlet Obstruction (Soltan Aiman NeazyMohammed ElhashimiAinda não há avaliações
- Genus Calvatia ReviewDocumento9 páginasGenus Calvatia ReviewalAinda não há avaliações
- OLGA Staging For GastritisDocumento9 páginasOLGA Staging For GastritisAndrea AlesandraAinda não há avaliações
- GI Drugs Classification GuideDocumento29 páginasGI Drugs Classification GuideJeneyse Ajap BalcenaAinda não há avaliações
- Stomach and Duodenal Ulcer Classification and TreatmentDocumento79 páginasStomach and Duodenal Ulcer Classification and Treatmentadversal8avrikAinda não há avaliações
- De La Cruz, A - BSN 3b - Case Study For RM 219 - 1st Week of DutyDocumento13 páginasDe La Cruz, A - BSN 3b - Case Study For RM 219 - 1st Week of DutyAlia De La CruzAinda não há avaliações
- HagarDocumento28 páginasHagarSandeep KannegantiAinda não há avaliações
- Pharmacology MCQDocumento30 páginasPharmacology MCQLokesh Mahata71% (7)
- Gastrointestinal and Gastrointestinal and Antiemetic Drugs Antiemetic DrugsDocumento34 páginasGastrointestinal and Gastrointestinal and Antiemetic Drugs Antiemetic DrugsZakir UllahAinda não há avaliações
- A Patient With Caustic Ingestion Injury: Brinna Anindita Budi WidodoDocumento27 páginasA Patient With Caustic Ingestion Injury: Brinna Anindita Budi WidodoBrinna Anindita SatriaAinda não há avaliações
- Peptic Ulcer DiseaseDocumento18 páginasPeptic Ulcer DiseasechetankumarbhumireddyAinda não há avaliações
- Drug Study CHDCDocumento1 páginaDrug Study CHDCIannBlancoAinda não há avaliações
- Jurnal Colic AbdomenDocumento5 páginasJurnal Colic AbdomenMadania PattyAinda não há avaliações
- GERD2Documento28 páginasGERD2Anonymous 2qUGvwI9Ainda não há avaliações
- Acute Abdominal Pain MS LectureDocumento63 páginasAcute Abdominal Pain MS Lectureheka_amrongAinda não há avaliações
- Anti Ulcerant StatDocumento3 páginasAnti Ulcerant StatHumayera KabirAinda não há avaliações
- Siddhamruta Rasa in AmlapittaDocumento8 páginasSiddhamruta Rasa in AmlapittamilindAinda não há avaliações
- V.I. Vernadsky Crimean Federal University Medical Academy named after S.I. Georgievsky Chair of Surgery No1 Objectives for Intermediate Certification 6 yearDocumento49 páginasV.I. Vernadsky Crimean Federal University Medical Academy named after S.I. Georgievsky Chair of Surgery No1 Objectives for Intermediate Certification 6 yearjhuiAinda não há avaliações
- Helicobacter Pylori Infection and TreatmentDocumento3 páginasHelicobacter Pylori Infection and Treatmentto van quyenAinda não há avaliações
- An Unusual Case of Nonsurgical Pneumoperitoneum in A Pediatric P 2023 BurnsDocumento5 páginasAn Unusual Case of Nonsurgical Pneumoperitoneum in A Pediatric P 2023 BurnsAdrian MoralesAinda não há avaliações
- Acute Gastritis Case StudyDocumento19 páginasAcute Gastritis Case StudyJay Villasoto100% (1)
- Proton Pump InhibitorsDocumento1 páginaProton Pump InhibitorsFadhilaKPAinda não há avaliações
- GASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXDocumento11 páginasGASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXRhealyn LegaspiAinda não há avaliações
- Medications Mechanism of Action Indication Contraindication Nursing ResponsibilitiesDocumento4 páginasMedications Mechanism of Action Indication Contraindication Nursing ResponsibilitiesMikhaela Andree MarianoAinda não há avaliações
- UGIBDocumento3 páginasUGIBعلي عليAinda não há avaliações
- High Definition of Homeopathic PracticeDocumento62 páginasHigh Definition of Homeopathic PracticeAmjad Khan100% (1)