Escolar Documentos
Profissional Documentos
Cultura Documentos
Physical Assessment: HR: 100: Cervical Spine Subluxation
Enviado por
Britanny NelsonTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Physical Assessment: HR: 100: Cervical Spine Subluxation
Enviado por
Britanny NelsonDireitos autorais:
Formatos disponíveis
Chief complaint: refusing to walk, seems to be in pain
History: GH is a 9 year old with trisomy 21 who presents with 1 day refusal to walk or bear weight. Mom
Developmental Assessment :
Ht: 115 cm < 3rd Wt: 85.5 kg >95th BMI: 64.8% reports last week G was found by teachers at recess sitting and refusing to stand up. Unsure if there was
>95th Broselow any fall or trauma prior. Later that night however, she was back to her baseline normal self, running around,
Pediatric Code Cart : Green active as usual.
Erikson Stage:
Physical Assessment: HR: 100 Expected:industry vs inferiority She remained well until yesterday morning when she again fell on the tile floor at grandma?s house. She
BP: 101/60 RR:20 O2: 96% immediately got back up and was acting herself, however 30 minutes later she was refusing to stand up
Actual: Autonomy versus shame and doubt (1?3 again and has remained this way since. When mom does make her walk, she is hunched over, taking small
Temperature: 36.7 years)? The development of autonomy during the
steps, favoring her right leg. Grandma noted her legs have been trembling when she tries to walk.
toddler period is centered on children?s increasing ability
-Pt is nonverbal due to to control their bodies, themselves, and their She seems to be in pain whenever having to stand up, from a sitting position, or when mom tries to
environment. They want to do things for themselves
developmental delay using their newly acquired motor skills of walking,
examine her right hip area. When sitting, she will happily play as normal. She has been eating and drinking
-Signs of acute distress when trying climbing, and manipulating and their mental powers of as normal, no change in urine output or stools. Mom sitting and not moving her hips.
selecting and decision making. This prompted ED visit last night, where x-ray of her pelvis, right femur and right tibia fibula were negative
to ambulate Sometimes the patient would try to do things without the for fracture or SCFE. She was discharged with Miralax due to stool burden seen on imaging. She returned
Affects on body: - Cannot turn head assistance of mother. She held onto her stuffed animal.
and favoring of her right leg. CRP was elevated. She was given morphine 4 mg and admitted to general
She accepted a sticker on her hand but was unable to
NERVES C1 ? blood supply to the head, pituitary gland,
scalp, face bones, brain, inner and middle ear, sympathetic
-Pt wears a cervical collar choose one she took the whole page and held it. The pediatrics for further care.
student pointed to various stickers and the patient was Chronic problems:
nervous system - IV site: No redness, no edema, indifferent.
Piaget Stage: -primary enuresis (never bladder trained)
· C2 ? eyes, optic nerves, auditory nerves, sinuses, mastoid IV patent Expected: Concrete operational 7-11 years -URIs
bones, tongue, forehead -Nystamus present -obstructive apnea
Actual:Preoperational (2?7 years)? The predominant
- Nares: white mucus present characteristic of the preoperational stage of intellectual
-Tonsils out development is egocentrism, which in this sense does Family history: HTN, grandmother ? rheumatoid arthritis
not mean selfishness or self-centeredness, but the
-Pt breathes through her mouth inability to put oneself in the place of another.
PHM: morbid obesity, trisomy 21
The patient sorts colors and shapes at school. She
- Neck: ROM: Limited. Pt turns her enjoys coloring and playing. She can recognize her own
name. She is unable to verbalize her thoughts, but she
body. can communicate using sign language. The patient said
PSH: tonsillectomy and adenoidectomy,
- Abdomen: Lesion present RLQ hello to the student and asked to eat and drink. bilateral tympanostomy tubes, catact removal- right eye, umbilical hernia repair
IV fluids D5 0.9 NS with 20 mEq KCL/liter rate 100 ml/hr to infuse over 10 with redness, no edema, circular
hrs SAFE ( pt allowed 117 ml/hr) Immunizations up to date.
Indication:
and quarter sized
Potassium chloride:Treatment/prevention of potassium depletion. - Primary enuresis.
Dextrose - Redness, rash, no edema at
Provides hydration and calories. perineum.
SIde effects:
Potassium chloride :CNS: confusion, restlessness, weakness. CV:
ARRHYTHMIAS, ECG changes. GI: ab- dominal pain, diarrhea, flatulence,
nausea, vomitingtablets, capsules only, GI ulcer- ation, stenotic lesions. Neuro:
paralysis, paresthesia.
Dextrose Endo: inappropriate insulin secretion (long-term use). F and E: fluid
overload, hypokalemia, hypomagnesemia, hypophosphatemia. Local: local
pain/irritation at IV site (hypertonic solution). Metab: glycosuria, hyperglycemia. Diagnostics: Prep and post care for labs and
Contraindications: -Lab values : diagnostic: Child was given anesthesia
Potassium chloride Hyperkalemia; Severe renal impairment; Untreated RDW 16.6 H, Neutrophil 76.6- Infection, Lymphocyte 16 L, to prevent the child from moving during
Addison?s disease ***alkaline phosphate 163 H- High ALP usually means that MRI. Patient is unable to understand
Implications: either the liver has been damaged or a condition causing keeping still for prolonged period of time
Potassium chloride increased bone cell activity is present, lipase 16 L-A low due to developmental and cognitive
1. Assess for signs and symptoms of hypokalemia (weakness, fatigue, U wave level of lipase in the blood may indicate permanent damage delay.
on ECG, arrhythmias, polyuria, polydipsia) and hyperkalemia (see Toxicity and to the lipase-producing cells in the pancreas,
Over- dose). ***C reactive protein 6.4 H - A high or increasing amount
Risk Factors:
2. Lab Test Considerations: Monitor serum potassium before and periodically
-Trauma Cervical spine subluxation of CRP in the blood suggests the presence of inflammation
during therapy. Monitor renal function, serum bicarbonate, and pH. Determine but will not identify its location or the cause.
-age
serum magnesium level if patient has refractory hypokalemia; -Imaging
-Down syndrome: Children participating in sports that may
hypomagnesemia should be corrected to facilitate effectiveness of potassium - XR femur: ( xray)
involve stress on the head and neck, such as gymnastics,
replacement. Monitor serum chloride because hypochloremia may occur if Cortical margins are intact. Alignment is anatomic. Fracture
diving, butterfly stroke in swimming, high jump, and soccer,
replacing potassium without concurrent chloride. or focal lesion is not seen.
should be evaluated radiologically for atlantoaxial Ketolorac 30 mg IV q 6 hrs SAFE
3. Treatment includes discontinuation of potassium, administration of sodium -Pelvis 1 view XR:Bone mineralization normal joint spaces
instability.Symptoms of the disorder include neck Indication:Short-term management of pain
bicarbonate to correct acidosis, dextrose and insulin to facilitate passage of symmetric acetabula normal. No fracture or intrinsic bone
pain, weakness, and torticollis. Side effects: STROKE, drowsiness, abnormal
potassium into cells, calcium salts to reverse ECG effects (in patients who are lesion.
not receiving digoxin), sodium polystyrene used as an exchange resin, and/or thinking, dizziness, euphoria, headache, nasal
- Abdomen XR: discomfort (spray), throat irritation
dialysis for patient with impaired renal function. Bowel gas. There is gas seen in normal caliber distal
Dextrose (spray).asthma, dyspnea. MYOCARDIAL
bowel. There is a moderate amount of stool in the colon. INFARCTION, edema, pallor, vasodilation.GI
1. Assess the hydration status of patients receiving IV dextrose. Monitor intake Peritoneum: no free air.
and output and electrolyte concentrations. Assess patient for dehydration or BLEEDING, abnormal taste, diarrhea, dry mouth,
- ***Spine cervical XR: dyspepsia, GI pain
edema. Pathophysiology: Cervical
Enteral subluxation of C1 over C2. In flexion atlantodens Contraindications: Hypersensitivity;
2. Assess nutritional status, function of gastrointestinal tract, and caloric needs vertebral subluxation means a
Priority #3: Ineffective health interval is 9mm. In extension it is 3mm. Cross-sensitivity with other NSAIDs may ex- ist;
of patient. misalignment exists within the
maintenance related to -MRI ordered 4/4/18 Preoperative use;
3. Lab Test Considerations: May cause an increase in serum glucose level seven uppermost vertebrae of the
alteration in cognitive Labs ordered 4/4/18 Nursing Implications:
spine. This is the cervical (upper)
functioning, decrease in fine spinal region, and because it 1.Patients who have asthma, aspirin-induced
motor skills, impaired decision bears the weight of the head and allergy, and nasal polyps are at increased risk for
making, perceptual impairment, is subject to a broad range of Potential Complications: developing hypersensitivity reactions. Assess for
unachieved developmental stress-inducing movement, it is loses of blood supply to the rhinitis, asthma, and urticaria.
tasks as evidenced by inability particularly vulnerable to the head, paralysis of arms and 2.Assess for rash periodically during therapy.
to take responsibility for development of issues. legs, neurological damage, May cause Stevens-Johnson syndrome or toxic
meeting basic health practices; Conditions can be caused by epidermal necrolysis. Discontinue therapy if
insufficient knowledge about traumatic injury related to the severe or if accompanied with fever, general
basic health practices Priority #1: Acute pain related to
aging process, muscle strain, malaise, fatigue, muscle or joint aches, blisters,
Signs and back injury and physical injury as
lifting, rheumatoid arthritis or oral lesions, conjunctivitis, hepatitis and/or
symptoms: neck pain, evidenced by expressive behavior,
Teaching: Nurse will tailor both the information provided infection. Medical treatments: Pain eosinophilia.
weakness,reduction in mobility, guarding, facial expressions,proxy
and the method of delivery of information to the specific
management, Tentative 3.Pain: Assess pain (note type, location, and
client and/or family. CEB: A systematic review of 27 joint pain or weakness, rotation of report of pain behavior/activity
studies related to medication adherence and diabetes posterior fusion surgery, intensity) prior to and 1?2hr following
the extremity, alteration in the changes (e.g., family member,
outcomes was not able to identify a specific Referral: Neurosurgery, administration.
intervention, but emphasized the need to tailor contour of the joint, Pt fell caregiver)
interventions to optimize management and Nutrition
improve outcomes . Pathophysiology: Down syndrome
The cause of Down syndrome is not known, but
Nurse will tailor both the information evidence from cytogenetic and epidemiologic studies
Nurse will use telehealth interventions to facilitate provided and the method of delivery of supports the concept of multiple causality.
self-care. EBN: A systematic review of 14 studies
Patient will follow mother information to the specific client and/or Approximately 95% of all cases of Down syndrome
supports telehealth as a positive factor in Community resources available for patient
and provider?s mutually family. CEB: A systematic review of 27 are attributable to an extra chromosome 21 (group G), Teaching: Nurse will demonstrate the use of
enabling self-care behaviors related to daily
thus the name nonfamilial trisomy 21 (National Down and family: Nurse will assume that pain is present if the client is unable to
weighing, medication management, exercise agreed on health care studies related to medication adherence and Nurse will assess for family appropriate nonpharmacological approaches
adherence, fluid and alcohol restriction, salt Syndrome Society, 2011b; Walker and Johnson, -**Down Syndrome Association of Jacksonville provide a self-report and has tissue injury, a pathological condition,
restriction, and stress reduction in clients with
maintenance plan diabetes outcomes was not able to identify a patterns, economic issues, in addition to pharmacological approaches
2006). Although children with trisomy 21 are born to -Hope Haven Children's Clinic and Family Center or has undergone a procedure that is thought to produce pain, and
heart failure (Radhakrishnan & Jacelon, 2012). specific intervention, but emphasized the spiritual, and cultural patterns to help control pain, such as application of
parents of all ages, there is a statistically greater risk - National Down Syndrome Society conduct an analgesic trial. CEB: Pain is associated with actual or
need to tailor interventions to optimize Goal:Patient will that influence compliance with heat and/or cold, distraction techniques,
in older women, particularly those older than 35 years - National Down Syndrome Congress potential tissue damage such as pathological conditions (e.g.,
management and improve outcomes meet goals for health a given medical regimen. relaxation breathing, visualization,
of age.However, the majority (?80%) of infants with rocking, stroking, listening to music, cancer) and procedures (e.g., surgery or trauma, fractures). In the
(Williams et al, 2014). care maintenance. CEB: A qualitative study (N = Down syndrome are born to women younger than age Patient will absence of self-report (e.g., anesthetized, critically ill, or cognitively
14) found that critical and watching television.
Nurse will discuss realistic goal setting for 35 years because younger women have higher fertility decrease in impaired client), the health care provider should use clinical
changes in health maintenance with the challenges to increasing rates. About 3% to 4% of the cases may be caused by Nurse will reinforce the importance of taking pain-related judgment and assume pain is present, then implement pain
client and family. EBN: An integrative physical activity among translocation of chromosomes 15 and 21 or 22. This pain medications to patient?s mother to behaviors management interventions accordingly (McCaffery et al, 2011).
review of 13 studies revealed that mutual low-income African American As with adults, nurse will use nonpharmacological analgesic
goal-setting between the client and the type of genetic aberration is usually hereditary and is maintain the comfort-function goal. CEB:
Provide a health promotion focus for the client with women included financial Patient?s mom will interventions to supplement, not replace, pharmacological
health care provider improves overall not associated with advanced parental age. From 1% Teaching clients to stay on top of their pain
disabilities, with the goals of reducing secondary conditions health behaviors and outcomes for older constraints (Harley et al, report patient?s ability to interventions in pediatric clients. EB: Heel pain associated with
(e.g., obesity, hypertension, pressure sores), maintaining to 2% of affected persons demonstrate mosaicism, and prevent it from getting out of control will
adults with chronic conditions (Anuruang et 2014). obtain sufficient amounts lancet heel sticks in preterm newborns was shown to provide
functional independence, providing opportunities for leisure al, 2014). which refers to a mixture of normal and abnormal cell improve the ability to accomplish the goals of
and enjoyment, and enhancing overall quality of life. CEB: A of rest and sleep greater reduction in pain scores when pharmacological methods
types. recovery (McCaffery et al, 2011).
retrospective analysis of data from a national survey (fentanyl injections) were combined with nonpharmacological
comparing health of adults with and without physical or
cognitive disabilities found that individuals living with techniques (sensory saturation) (Gitto et al, 2012). CEB:
physical disabilities or cognitive impairment receive fewer Complementary therapies such as relaxation, distraction,
preventive services and have higher rates of chronic illness Before the activity begins, hypnotics, art therapies, and imagery may play an important role Nurse will assess for the presence of pain using a valid and
(Reichard et al, 2011). A systematic review of 11 studies Nurse will refer the client to appropriate reliable pain scale based on age, cognitive development, and
found that community-based physical activity and medical and social services as needed, obtain any assistive devices in holistic pain management (Oakes, 2011). Nonpharmacological
Goal unmet; The patient?s BMI is Priority #2: Impaired Goal:Patient will the child's ability to provide a self-report. EBN: Scales that
educational programs provide fitness and psychosocial 64.8%. She started going to a weight providing adequate information on details needed for activity, such as interventions reduce procedure-related distress (Oakes, 2011).
benefits for individuals with intellectual disabilities (Heller et management facility at UF. Nurse
Teaching: Teach family members physical mobility related use adaptive depict faces at various levels of pain intensity are commonly
about the service, including scheduling. EBN: and caregivers to work with clients gait belt, weighted vest,
al, 2011). asked the patient?s mom about her to pain,body mass index equipment (e.g., used in young children and have been shown to be reliable
Goal met; Patient?s family A metasynthesis of 62 qualitative studies actively during self-care activities walker, cane, crutches, or
weight. Patient?s mother is overweight.
using a restorative care >75th percentile for age wheelchairs, walkers, During the initial assessment and interview, if the client and valid in children as young as 3 years old (Oakes, 2011).
discussed making small changes Social services can provide if financial concluded that client participation in services wheelchair, ergonomic
to transition the patient to have a problems are a contributing factor to ineffective
philosophy for eating, bathing, gait belts, weighted is experiencing pain, nurse will conduct and document a EB: Behavioral tools such as the FLACC Scale may be used
such as cardiac rehabilitation is most strongly grooming, dressing, and shower chairs, ceiling and
healthier lifestyle. For example, cutting health maintenance. Medical services can be walking vests) to comprehensive pain assessment, using appropriate pain to assess pain in infants and children who cannot provide a
down on salt and replacing juice with associated with perceptions of the nature, transferring to restore the floor-based lifts, and
utilized to figure out if her lipase levels are severely
client to maximum function increase mobility. assessment tools. CEB: Determining location, temporal self-report (Crellin et al, 2015).
water and natural juices. Patient does impairing her body?s ability to process fat. suitability, and scheduling, but not the benefits air-assisted lateral transfer
have a cognitive impairment and It is important to relay the information to the
and independence. Before activity, nurse will observe aspects, pain intensity, characteristics, and the impact of
of the rehabilitation program (Clark et al, devices. Assistive devices
needs more help with making family since they are the ones making food for and, if possible, treat pain with pain on function and quality of life are critical to
changes to health maintenance. can help increase mobility
decisions and taking care of the patient. It massage, heat pack to affected determine the underlying cause of pain and
would be important for the nurse to use (Hodgson et al, 2013).
short simple sentences when
area, or medication. Ensure that effectiveness of treatment (McCaffery, 1968; McCaffery Nurse will prevent pain by administering analgesia before
communicating to the patient in sign the client is not oversedated. Pain et al, 2011). The initial assessment includes all pain painful procedures whenever possible (e.g., endotracheal
language considering her cognitive limits mobility and if exacerbated by information that the client can provide for the suctioning, wound care, heel puncture, venipunctures, and
level.
specific movements should be development of the individualized pain management peripherally inserted intravenous catheters).EB: Adult clients
Goal:Patient will be temporarily avoided (ACSM, 2014). plan (McCaffery et al, 2011).Implement or request in the intensive care setting experience numerous sources of
free from complications of
orders to implement pain management interventions to Evaluation: Goal met; The procedural pain and chest tube removal, wound drain
immobility, as evidenced by Evaluation: Goal met. The patient?s mom reported her
patient?s mother used the achieve a satisfactory level of comfort. Components of removal, and arterial line insertion are identified as the most
intact skin, absence of daughter sleeping much better
Adults with disabilities should follow the adult guidelines; wheelchair to get the patient out of this initial assessment include location, quality, after the application of the cervical
painful procedures (Puntillo et al, 2014). The use of topical
thrombophlebitis, normal the bed and wheeled her around on
however, if not possible these persons should be as physically Nurse will monitor and record the client's onset/duration, temporal profile, intensity, aggravating spine collar. The patient was offered lidocaine 1% before removal of extremity vacuum-assisted
bowel pattern, and clear the pediatric floor. The student nurse coloring books and she declined. The
active as their abilities allow and avoid inactivity (U.S. Department ability to tolerate activity and use all four noticed the patient?s limited range of and alleviating factors, and effects of pain on function closure wound dressings results in reduced pain and opioid
breath sounds. student nurse offered a stuffed animal
of Health & Human Services, 2008). Use ?start low and go slow? extremities; note pulse rate, blood motion with her neck. The patient was and quality of life. to the patient which she sometimes
use (Christensen et al, 2013).
pressure, dyspnea, and skin color before hunched over when her mom get her out of took. When the patient was
approach for intensity and duration of physical activity if client bed to change her. She did not want to
and after activity. Refer to the care plan for agitated nothing seemed to
highly deconditioned, functionally limited, or has chronic roll with her right side down. There was work besides just leaving the
conditions affecting performance of physical tasks. When Activity intolerance. EB: Use valid and no change in skin color after she patient alone.
reliable screening procedures and tools to walked. The patient is prescribed
progressing client's activities, use an individualized and tailored a medication to treat moderate Evaluation of goal : Goal partially
approach based on client's tolerance and preferences (American assess the client's preparticipation in pain met; Patient has a subluxation of the
College of Sports Medicine [ACSM], 2014). exercise health screening and risk cervical spine and her pain is currently
stratification for exercise testing (low, being managed with Ketolorac. When she
was initially admitted to the ER the patient
moderate, or high risk) (ACSM, 2014).
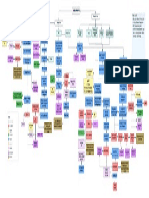
Key was given morphine. The student nurse looks at
her body language and her movements and
Medical Treatments Diagnostics
Pathophysiology reports from mom to assess the patient?s level of
Interventions
pain. The patient is unable to self-report. She
Teaching/Learning needs Physical
uses some signs but not extensive use of
asessesment sign language. The patient?s chart
Signs and symptoms Priority/ Nursing Diagnosis
indicates wound care will be doing a
Nurse will screen for mobility skills in the following dressing on the lesion for RLQ for
Community resource
order: (1) bed mobility; (2) supported and Evaluation of goal
Affects on multiple body abdomen.
systems
unsupported sitting; (3) transition movements such Nurse will assess the client for cause Developmental Assessment
as sit to stand, sitting down, and transfers; and (4) of impaired mobility. Determine History
Possible complications
standing and walking activities. CEB: Use a tool such whether cause is physical, Patient Goals
Medications
as the Assessment Criteria and Care Plan for Safe psychological, or motivational. Some Medical Diagnosis
Patient Handling and Movement (Sedlak et al, 2009). clients choose not to move because of Risk factors
EBN: Assess for low mobility, functional difficulties, Goal not met; The patient has
psychological factors such as fear of
cognitive impairment and multiple comorbidities that impaired skin integrity on her RLQ- falling or pain, an inability to cope, or
require both client safety and rehabilitation circular, red lesion. Patient also has a rash depression. EBN: Because fear of
near her anus. Patient?s mom uses diaper
interventions (Kneafsey et al, 2013). cream. X-rays were completed to find the cause
falling is associated with immobility and
of immobility. MRIs are also ordered for both hip functional dependence, it requires
and cervical spine. Patient is able to sit up on effective assessment and
her own when she is willing to cooperate.
Patient impairment that requires close
measurement (Greenberg, 2012).
supervision and bed rails up to promote
safety.
Você também pode gostar
- Blue Belt Level 01 - Fact Sheet - 0 PDFDocumento9 páginasBlue Belt Level 01 - Fact Sheet - 0 PDFShayma ShamoAinda não há avaliações
- My Way Nursing NoteDocumento79 páginasMy Way Nursing Noterauda AlsawwafiAinda não há avaliações
- Health Assessment FormDocumento12 páginasHealth Assessment Formmiha3la33Ainda não há avaliações
- 175P - FCardoso-BYLieve StudyDocumento1 página175P - FCardoso-BYLieve StudyΒΑΣΙΛΗΣ ΚΟΛΙΝΤΖΙΚΗΣAinda não há avaliações
- Education: Kennel TechnicianDocumento1 páginaEducation: Kennel Technicianapi-577979422Ainda não há avaliações
- Order of Worship November 14, 2010Documento2 páginasOrder of Worship November 14, 2010Robbie D GrahamAinda não há avaliações
- Classroom Daily Health Monitoring Tool For CovidDocumento3 páginasClassroom Daily Health Monitoring Tool For CovidLittle Baguio Elementary School (R III - Zambales)Ainda não há avaliações
- Surveilence Hais: Dr. Elsye Maria Rosa, M.KepDocumento9 páginasSurveilence Hais: Dr. Elsye Maria Rosa, M.KepEni MuchlisohAinda não há avaliações
- Chores + Adverbs of Frequency LessonDocumento1 páginaChores + Adverbs of Frequency LessonCharlotte PresleyAinda não há avaliações
- OB 1.03B Placental Hormones CasesDocumento3 páginasOB 1.03B Placental Hormones CasesCandice SongcoAinda não há avaliações
- A Practical Guide To Small-Sided & Conditioned Games (SSCG) in Football: Implications For Training DesignDocumento1 páginaA Practical Guide To Small-Sided & Conditioned Games (SSCG) in Football: Implications For Training DesignLukas ArenasAinda não há avaliações
- Thetahealing - Dig Deeper Practitioners Manual PDFDocumento11 páginasThetahealing - Dig Deeper Practitioners Manual PDFGislaine Maria100% (4)
- Case Study 2Documento4 páginasCase Study 2H MAinda não há avaliações
- NUR 115 - LAB ACTIVITY # 1bDocumento3 páginasNUR 115 - LAB ACTIVITY # 1bMoira Julianne Serognas BrigoliAinda não há avaliações
- Classical Musician Today TocDocumento4 páginasClassical Musician Today TocLuiz Antonio De Britto JuniorAinda não há avaliações
- Simo Häyhä: Strong Point Module: Riding Big WinnersDocumento8 páginasSimo Häyhä: Strong Point Module: Riding Big WinnersPao Pecadizo SalazarAinda não há avaliações
- Identify Your Values - Leigh Allen-ArredondoDocumento2 páginasIdentify Your Values - Leigh Allen-ArredondoLeighAinda não há avaliações
- Order of Worship Publisher August 22, 2010Documento2 páginasOrder of Worship Publisher August 22, 2010Robbie D GrahamAinda não há avaliações
- Vocabulary WorksheetsDocumento14 páginasVocabulary WorksheetsRaquel RomeroAinda não há avaliações
- EnglishFile4e Upp-Int TG PCM Comm COMPLETEDocumento25 páginasEnglishFile4e Upp-Int TG PCM Comm COMPLETEMariaAinda não há avaliações
- EnglishFile4e Upp-Int TG PCM Vocab COMPLETEDocumento14 páginasEnglishFile4e Upp-Int TG PCM Vocab COMPLETEMariaAinda não há avaliações
- Audit Iadp Bundle ChecklistDocumento5 páginasAudit Iadp Bundle ChecklistAyu Ngurah SuarminiAinda não há avaliações
- Duty CensusDocumento19 páginasDuty CensusJames MaravillasAinda não há avaliações
- Frozen Shoulder FinalDocumento3 páginasFrozen Shoulder FinalRatnaPrasadNalamAinda não há avaliações
- 10 Step Approach To Designing A Training ProgramDocumento2 páginas10 Step Approach To Designing A Training ProgramAbdu AbduAinda não há avaliações
- Code Status: MD: Diet: Isolation: Cna: Room Number:: None Cane/Walker WheelchairDocumento1 páginaCode Status: MD: Diet: Isolation: Cna: Room Number:: None Cane/Walker WheelchairVanessa FloresAinda não há avaliações
- One and One (Reprise)Documento11 páginasOne and One (Reprise)Tom CarronAinda não há avaliações
- The 3 Steps To Emotional Success HandbookDocumento19 páginasThe 3 Steps To Emotional Success Handbook4884 AlphaAinda não há avaliações
- The Last Goodbye (Solo Piano) by David BenoitDocumento9 páginasThe Last Goodbye (Solo Piano) by David BenoitFist GymAinda não há avaliações
- Bar Sample QsDocumento30 páginasBar Sample QsChristian Paul LugoAinda não há avaliações
- Bulletin 6000ADocumento1 páginaBulletin 6000AKala KingAinda não há avaliações
- Information Zur Anwendung Der Selbsttests Xiamen Boson Biotech - Rapid Sars-Cov-2 Antigen TestDocumento3 páginasInformation Zur Anwendung Der Selbsttests Xiamen Boson Biotech - Rapid Sars-Cov-2 Antigen TestmaxvaneykAinda não há avaliações
- Praxis Scores 2Documento3 páginasPraxis Scores 2api-477521933Ainda não há avaliações
- Austins Warmup March1Documento2 páginasAustins Warmup March1api-277906070Ainda não há avaliações
- Resume: K.AkhilaDocumento3 páginasResume: K.AkhilaAkhila KunamallaAinda não há avaliações
- O Church, Arise (D - Sheet Music)Documento2 páginasO Church, Arise (D - Sheet Music)Javier Castañeda Pineda100% (1)
- Daily Health Check Symptoms Record Month - YearDocumento1 páginaDaily Health Check Symptoms Record Month - YearfitchAinda não há avaliações
- ViviDocumento1 páginaViviMaria Vivienne CerilloAinda não há avaliações
- 4 - Seventh Chords IdeasDocumento1 página4 - Seventh Chords IdeasKatayoon GhomiAinda não há avaliações
- Osteoarthritis Concept MapDocumento1 páginaOsteoarthritis Concept MapJanselle H ArmaAinda não há avaliações
- Scorereport 2Documento3 páginasScorereport 2api-339203904Ainda não há avaliações
- Body Back Buddy ManualDocumento11 páginasBody Back Buddy ManuallyleAinda não há avaliações
- Form Audit BUNDLE VAP - NewDocumento1 páginaForm Audit BUNDLE VAP - NewYuanita ayuAinda não há avaliações
- Lakshmi Vilas Bank Initiating Coverage Dec 2015Documento14 páginasLakshmi Vilas Bank Initiating Coverage Dec 2015janmAinda não há avaliações
- The Boyfriend Test Book Part 1Documento25 páginasThe Boyfriend Test Book Part 1Edwina Madriz0% (1)
- NCM 114 Ethical Aspects of Care PromotionDocumento2 páginasNCM 114 Ethical Aspects of Care PromotionJane DiazAinda não há avaliações
- Following Symptoms: A Patient Suffering From The White Disease, Oblivious To The Seriousness of His ConditionDocumento1 páginaFollowing Symptoms: A Patient Suffering From The White Disease, Oblivious To The Seriousness of His ConditionDREAinda não há avaliações
- Do Not Forsake Health For Fear of Rejection!: Am I Too Fat?Documento1 páginaDo Not Forsake Health For Fear of Rejection!: Am I Too Fat?kaiteckAinda não há avaliações
- Emi Tesalonika - Rahametwau Askep Bahasa InggrisDocumento7 páginasEmi Tesalonika - Rahametwau Askep Bahasa InggrisSiva PutriAinda não há avaliações
- Praxis Scores-1Documento3 páginasPraxis Scores-1api-477521933Ainda não há avaliações
- Scorereport 1Documento3 páginasScorereport 1api-485931730Ainda não há avaliações
- Turkey Trot Bro2010Documento2 páginasTurkey Trot Bro2010track9060Ainda não há avaliações
- ScorereportDocumento3 páginasScorereportapi-575424000Ainda não há avaliações
- Heath Pe ContentDocumento3 páginasHeath Pe Contentapi-312882401Ainda não há avaliações
- All Will Be WellDocumento1 páginaAll Will Be WellCallumAinda não há avaliações
- PADocumento3 páginasPAaashika shresthaAinda não há avaliações
- ScorereportDocumento3 páginasScorereportapi-393899761Ainda não há avaliações
- Assignment 4 HLTH 101Documento3 páginasAssignment 4 HLTH 101api-622678802Ainda não há avaliações
- UntitledDocumento230 páginasUntitledSilvana RoccoAinda não há avaliações
- Menstruation and Bleeding Conditions in Women and AdolescentsDocumento123 páginasMenstruation and Bleeding Conditions in Women and AdolescentsBritanny NelsonAinda não há avaliações
- Approved Hospice Discharge Disposition Meditech v2Documento8 páginasApproved Hospice Discharge Disposition Meditech v2Britanny NelsonAinda não há avaliações
- Management of Preconceptual Care, Normal PregnancyDocumento233 páginasManagement of Preconceptual Care, Normal PregnancyBritanny NelsonAinda não há avaliações
- Approved Traumatic Brain Injury (TBI)Documento38 páginasApproved Traumatic Brain Injury (TBI)Britanny NelsonAinda não há avaliações
- Hca Retirement Readiness: Supporting Your Personal and Professional Goals While Promoting A Healthier, Happier LifeDocumento4 páginasHca Retirement Readiness: Supporting Your Personal and Professional Goals While Promoting A Healthier, Happier LifeBritanny NelsonAinda não há avaliações
- Introduction To Critical CareDocumento21 páginasIntroduction To Critical CareBritanny NelsonAinda não há avaliações
- Tele Safety Bundle - StandardsDocumento2 páginasTele Safety Bundle - StandardsBritanny NelsonAinda não há avaliações
- Final 48 HouCram FullDocumento106 páginasFinal 48 HouCram FullRadu Urcan50% (2)
- Ati Med SurgDocumento1 páginaAti Med SurgBritanny NelsonAinda não há avaliações
- Menopause Concept MapDocumento1 páginaMenopause Concept MapBritanny NelsonAinda não há avaliações
- Critical Care Notes Clinical Pocket Guide - (Gastro-Urinary)Documento1 páginaCritical Care Notes Clinical Pocket Guide - (Gastro-Urinary)Britanny Nelson100% (1)
- Critical Care Notes Clinical Pocket Guide - (Front Matter)Documento10 páginasCritical Care Notes Clinical Pocket Guide - (Front Matter)Britanny Nelson100% (1)
- Critical Care Notes Clinical Pocket Guide - (Hematology Oncology)Documento17 páginasCritical Care Notes Clinical Pocket Guide - (Hematology Oncology)Britanny NelsonAinda não há avaliações
- Pharmacology NCLEX ReviewDocumento128 páginasPharmacology NCLEX ReviewBritanny NelsonAinda não há avaliações
- Digestion and Absorption Study GuideDocumento6 páginasDigestion and Absorption Study GuideBritanny NelsonAinda não há avaliações
- R & C L W G: Esume Over Etter Riting UideDocumento15 páginasR & C L W G: Esume Over Etter Riting UideBritanny NelsonAinda não há avaliações
- Creating Study Guides Oregon StateDocumento5 páginasCreating Study Guides Oregon StateBritanny NelsonAinda não há avaliações
- ATI SecretsDocumento9 páginasATI SecretsBritanny Nelson100% (11)
- 5 Lead EKG PlacementDocumento1 página5 Lead EKG PlacementBritanny NelsonAinda não há avaliações
- Order of Lab Draws PDFDocumento1 páginaOrder of Lab Draws PDFBritanny Nelson100% (1)
- Sumit YadavDocumento85 páginasSumit Yadavanuj3026Ainda não há avaliações
- Trabajos de InglésDocumento6 páginasTrabajos de Inglésliztmmm35Ainda não há avaliações
- IRS McqsDocumento7 páginasIRS McqsIbrahimGorgageAinda não há avaliações
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocumento2 páginasNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comAinda não há avaliações
- Essay 1 John WatsonDocumento4 páginasEssay 1 John Watsonapi-259502356Ainda não há avaliações
- Dolphin Is An a-WPS OfficeDocumento3 páginasDolphin Is An a-WPS Officeinova ilhamiAinda não há avaliações
- Out To Lunch: © This Worksheet Is FromDocumento1 páginaOut To Lunch: © This Worksheet Is FromResian Garalde BiscoAinda não há avaliações
- Age of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Documento4 páginasAge of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Ughu RajaAinda não há avaliações
- Math - Gr6 - Q2 - Week-08 - Comparing and Arranging Integers On The Number LineDocumento37 páginasMath - Gr6 - Q2 - Week-08 - Comparing and Arranging Integers On The Number LineDiana TubigAinda não há avaliações
- Lpm2.1theoryDocumento85 páginasLpm2.1theoryvetprabu34Ainda não há avaliações
- Artikel Andi Nurindah SariDocumento14 páginasArtikel Andi Nurindah Sariapril yansenAinda não há avaliações
- My Cook BookDocumento66 páginasMy Cook BookAkshay KumariAinda não há avaliações
- QinQ Configuration PDFDocumento76 páginasQinQ Configuration PDF_kochalo_100% (1)
- Region 2Documento75 páginasRegion 2yoyiyyiiyiyAinda não há avaliações
- Homeless Class ActionDocumento36 páginasHomeless Class ActionMichael_Lee_RobertsAinda não há avaliações
- Fallout Unwashed Assets Monsters and NpcsDocumento4 páginasFallout Unwashed Assets Monsters and NpcsVeritas VeritatiAinda não há avaliações
- Enter Pre NaurDocumento82 páginasEnter Pre NaurNeha singhalAinda não há avaliações
- The Liberal Welfare Reforms 1906Documento5 páginasThe Liberal Welfare Reforms 1906Skye G-sAinda não há avaliações
- ERF 2019 0128 H160 Noise CertificationDocumento10 páginasERF 2019 0128 H160 Noise CertificationHelimanualAinda não há avaliações
- Unit 5 Performance ManagementDocumento20 páginasUnit 5 Performance Managementbhavisha_30kAinda não há avaliações
- Kinematic Tool-Path Smoothing For 6-Axis Industrial Machining RobotsDocumento10 páginasKinematic Tool-Path Smoothing For 6-Axis Industrial Machining RobotsToniolo LucaAinda não há avaliações
- Natureview Case StudyDocumento3 páginasNatureview Case StudySheetal RaniAinda não há avaliações
- Constitutional Law OutlineDocumento28 páginasConstitutional Law OutlineCasey HartwigAinda não há avaliações
- 2019 National Innovation PoliciesDocumento98 páginas2019 National Innovation PoliciesRashmi SinghAinda não há avaliações
- NMAT PRACTICE SET 0619 - Rationale - TEST D. ChemistryDocumento10 páginasNMAT PRACTICE SET 0619 - Rationale - TEST D. ChemistryMianella RosalesAinda não há avaliações
- BM - GoPro Case - Group 6Documento4 páginasBM - GoPro Case - Group 6Sandeep NayakAinda não há avaliações
- College Physics Global 10th Edition Young Solutions ManualDocumento25 páginasCollege Physics Global 10th Edition Young Solutions ManualSaraSmithdgyj100% (57)
- Manual GPS Trimble Portugues CFX-750 / FM-750Documento246 páginasManual GPS Trimble Portugues CFX-750 / FM-750José Luis Mailkut Pires100% (5)
- The Convergent Parallel DesignDocumento8 páginasThe Convergent Parallel Designghina88% (8)
- Drishti IasDocumento36 páginasDrishti Ias23010126269Ainda não há avaliações