Escolar Documentos
Profissional Documentos
Cultura Documentos
Prevalence of Urinary Incontinence and Its Association With Overweight Among Postpartum Patients
Enviado por
Baru Chandrasekhar RaoTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Prevalence of Urinary Incontinence and Its Association With Overweight Among Postpartum Patients
Enviado por
Baru Chandrasekhar RaoDireitos autorais:
Formatos disponíveis
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN: 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
http://doi.org/10.5281/zenodo.1225552
Available online at: http://www.iajps.com Research Article
PREVALENCE OF URINARY INCONTINENCE AND ITS
ASSOCIATION WITH OVERWEIGHT AMONG POSTPARTUM
PATIENTS
*1
Dr. Abu Bakar Khan, 2Dr. Muhammad Rumas Mahde, 3Dr. Muhammad Sohaib,
4
Ghazala Kiran
1
BHU Ganda, Mianwali.
2
Medical Officer BHU Chakki Pindigheb Attock.
3
Medical Officer BHU Mianwala Pindigheb Attock.
DPT, University of Lahore
Abstract:
Objective: To determine the prevalence of urinary incontinence among postpartum patients according to different
BMI group.
Method: A cross-sectional study was conducted on 190 postpartum women. Non-probability convenient sampling was
used to collect the data. Numerical data was measured in the form of mean and standard deviation, whereas
qualitative data was presented in the form of frequency and percentage. The prevalence of urinary incontinence find
out in overweight women were assessed by ICIQ-UI questionnaire
Result: Mean age of the subjects was 28.81 ± 5.03years. Out of 190, 26.9% of the women reported urinary
incontinence. 5(2.63%) were underweight women, 79 (41.5%) normal, overweight 105 (55.26%) and 1 obese women
(0.61%). Association of urinary incontinence with different BMI groups was determined using chi square test. P-value
of 0.05or less was considered as significant.
Conclusion: Urinary incontinence is a communal problem in overweight women. Urinary incontinence is more as
compared of normal and underweight women and the associated factors that are avertible, modifiable and overweight
and high BMI may have the greatest impact on the prevalence of urinary incontinence.
Keywords: Urinary incontinence, overweight, postpartum
Corresponding author:
Dr. Abu Bakar Khan, QR code
BHU Ganda,
Mianwali.
Please cite this article in press Abu Bakar Khan et al , Prevalence of Urinary Incontinence and Its Association with
Overweight among Postpartum Patients, Indo Am. J. P. Sci, 2018; 05(04).
www.iajps.com Page 2774
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
INTRODUCTION: (UI), (12) Among the different types of UI, stress UI is
Urinary incontinence is a communal and pricey the type most closely associated with
problematic issue in postpartum after first and BMI.(13) Overweight women have increased
multiple gestational surgery in over weighted intra-abdominal pressures, which adversely stress the
women.(1)Mostly researches on weight loss in pelvic floor and may contribute to the development of
perversely overweight women undergoing bariatric UI. Weight loss may relieve UI, but definitive therapy
surgery takes publicized a positive conclusion on the via operative procedures has been shown to be
symptoms of urinary incontinence. Over weight is a effective even in obese patients, and can be
forever-cumulative public health matter and the recommended with confidence.(14) Over weight is
particular supreme predominant health hazard amid rising at an alarming rate situation of worldwide. It
women.(2) Management of the pelvic organ and stances a major health problem that in turn places an
pelvic muscles prolapse and tension urinary enormous financial burden on health services.
incontinence involves surgical repair of site precise Medical conditions such as diabetes mellitus and
faults in pelvic floor.(3) Risk factors of the progress diseases of heart are commonly associated with
of stress incontinence consist of progression of age, obesity but less well documented is the association
multiple postpartum , bariatric surgery, gestational between overweight and urinary incontinence.(15)
diabetes, urinary tract infection , excessive fat on
abdominal area. (4) Over weight was deliberated a symbol of social status
and wealth in many beliefs. Till recently a moderately
Although urinary incontinence is common in older infrequent phenomenon, it was also connected with
women, risk factors are not well defined. It is known comfort and fertility. Enhanced appreciative of the
that the prevalence of urinary incontinence in older impression of overweight on health and the alarming
women increases with age.(5) Our investigation also rates of increase in its prevalence over the last two eras
established that the prevalence of urinary have raised the issue to a leading public health task. A
incontinence increased with increasing BMI, a finding huge quantity of medical conditions have been related
that has been reported previously.(6) Reductions in with overweight and obesity. Overweight is a great
urinary incontinence have been observed in morbidly impact on health is the result of moreover increased fat
in overweight women who have had theatrical mass and causes different diseases osteoarthritis,
weight loss after bariatric surgery.(7) The risk factors pelvic floor dysfunction or enlarged number of fat
of urinary incontinence such as obesity, hysterectomy, cells cause cancer, cardiovascular disease,
prolonged medical infections, excessive medications, non-alcoholic fatty liver disease. (16) Low birth
and excessive soft drink, tea and alcohol intake, have weight has been associated with an increased risk of
been assessed adequately. (8) With the passage of time hypertension, and high birth weight has been
more researches appraisal of an imperfect number of associated with increased adult body mass index Early
potential risk factors(9) An extended period of time life exposures affecting birth weight may be important
interval of obesity was concomitant with facial hairs in the development of hypertension and obesity in
and excessive hairs in the body Additional adults.(17)
investigation establish that teenage obesity was
greater risk of polycystic ovaries and Young, adult women appear to be at increased risk for
recommendation for surgery and after that urinary substantial weight gain. Pregnancy has frequently
incontinence s more after first postpartum and been cited as a contributor to overweight in women
moreover women having ovarian surgery for other Excessive postpartum weight retention seems to be
reasons. It is correspondingly support and connotation especially prevalent among minority women. Factors
of obesity with an ovulatory cycles. These findings such as pre pregnancy weight and excessive
showing evidence of abnormality in ovulation, gestational weight gain have the strongest support as
menstrual abnormalities and additional hair growth in risk factors for postpartum weight retention and could
obese women may an overtone among obesity and guide targeted intervention efforts. However, there are
hormonal imbalances.(10) few controlled studies of behavioral interventions to
prevent substantial pregnancy-related weight gain or
Advanced disinhibition is strappingly linked with postpartum weight retention. Weight loss methods
higher adult weight gain and higher ration of BMI, successful in promoting weight control in other
moreover dietary disturbances is play a mainly role in populations would likely also be effective with
increase rate of BMI. (11)Increasing weight is a pregnant or postpartum women, although
common condition among women in developed modifications for the needs of mothers may be
countries. The body mass index (BMI) is positively required.(18)
associated with the prevalence of urinary incontinence
www.iajps.com Page 2775
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
Weight gained during pregnancy and not lost maternal fat gain, pregnancy complications, and
postpartum may contribute to obesity in women of delivery problems and should be discouraged.
childbearing age. Breastfeeding was associated with Postpartum weight loss is essential to prevent
lower PPWR in all categories of pre pregnancy BMI. permanent weight increase. Smoking cessation during
These results suggest that, when combined with GWG pregnancy, reduced postpartum physical activity, and
values in kg, breastfeeding as recommended could other lifestyle changes can contribute to increased
eliminate weight retention by 6 month postpartum in postpartum weight. Health care providers can help to
many women.(19) Overweight causes significant reduce obesity risk by regularly monitoring women's
complications for the mother and fetus. Interventions weight; promoting appropriate pre pregnancy weight,
directed towards weight loss and prevention of pregnancy weight gain, and postpartum weight less;
excessive weight gain must begin in the and explicitly encouraging maintenance of an active
pre-conception period. Obstetrical care providers must postpartum lifestyle. Weight gain during pregnancy
counsel their obese patients regarding the risks and may contribute to obesity development. Concerns
complications conferred by obesity and the about possible adverse effects of pregnancy weight
importance of weight loss. Maternal and fetal gain on later maternal weight and on labor and
surveillance may need to be heightened during delivery must be rigorously evaluated in light of
pregnancy; a multidisciplinary approach is useful. possible benefits for fetal growth and development.
Women need to be informed about both maternal and Birth-weight rises with increased pregnancy weight
fetal complications and about the measures that are gain, and perinatal and neonatal mortality fall as
necessary to optimize outcome, but the most important birthweight increases in both preterm and term
measure is to address the issue of weight prior to infants.(24)
pregnancy.(20)
Previous studies have found that weight gain during
Although women should begin pregnancy at a healthy pregnancy is often associated with postpartum weight
weight and gain reasonably during gestation, not all retention and the subsequent development of
will. Pediatricians can help overweight women to long-term obesity and obesity-related illness. Relative
succeed at breastfeeding by targeting them for contact to women whose weight changed by less than 10
with a lactation consultant before discharge from the pounds between pregnancies, women who gained at
hospital to be sure that they have received optimal least 10 pounds had a 1.5-fold increased risk of
advice on breastfeeding techniques. In addition, early gestational diabetes in their next pregnancy, and
contact with the mother after discharge by calling her women who lost at least 10 pounds between
at home to offer her support and counseling for pregnancies had a 40% decreased risk. Weight gain
breastfeeding, by scheduling the first pediatric visit above the Institute of Medicine Recommendations for
earlier than for other patients, or by enlisting the pregnancy results in greater retained postpartum
assistance of public health nurses for a home visit if weight. Unfortunately, heavier women who gain
this is possible would help overweight women to excessive weight are more likely to retain it
continue to breastfeed. Being overweight or obese is postpartum compared with lighter women. We sought
negatively associated with the prolactin response to to estimate the incremental effect of gestational
suckling in the first week postpartum and, thus, may weight gain above the Institute of Medicine
contribute to early lactation failure.(21) The greatest recommendation for overweight women on
variation in rates of weight gain is seen in the first 1-2 postpartum weight retention at 1 year.(25)
years of life when infants may show significant Once a low-risk pregnancy has been established,
“catch-up” or “catch-down” growth. These variable walking in combination with nutritional control may
growth rates often compensate for intrauterine be effective in preventing excessive weight gain in
restraint or enhancement of fetal growth, and by two overweight and obese women. Maternal exercise
years of age growth usually follows the genetic prescription should use the Frequency, Intensity, Time
trajectory.(22) Excess weight gain and failure to lose spent and Type of exercise principle, with a frequency
weight after pregnancy are important and identifiable of three to four sessions per week as ideal. Intensity
predictors of long-term obesity. Breast-feeding and based on a target heart-rate zone of 110 to 131 beats
exercise may be beneficial to control long-term per minute for women 20 to 29 years of age and 108 to
weight.(23) 127 beats per minute for women 30 to 39 years of age,
coupled with use of the rating of perceived exertion
Weight gain that is optimal for the mother and the scale and the “Talk Test” is suggested. Dieting and
baby differs according to the mother's pre pregnancy exercise together are most effective in reducing
weight. Pregnancy weight gain exceeding current weight retention after childbirth and compliance may
recommendations is associated with increases in be improved by incorporating child-care and children
www.iajps.com Page 2776
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
into the exercise routine. After medical consultation, factor for incontinence in women. Only a few
postpartum women should begin exercise slowly, interventional studies have been carried out to assess
starting from 15 minutes, and building to at least 150 the effect of weight reduction on incontinence. Five
minutes of aerobic activity per week, with this activity studies report effect on incontinence after surgical
spread throughout the week.(26) weight reduction procedures, and one study after a
weight reduction program, thus giving some level 2
LITERATURE REVIEW documentation. There are three RCTs which all show
P.L.DWYER et al discussed in the study, 368 reducing incontinence by weight loss. The
incontinent women participated for assessment. The Conclusions of the study was epidemiological studies
conclusion of the study was 232 (63%) were document overweight and obesity as an important risk
diagnosed who have genuine stress incontinence and factor for urinary incontinence. There is now valid
136 (27%) as having detrusor instability. Obesity was documentation for weight reduction as a treatment for
knowingly more communal in women with genuine urinary incontinence in women.(28)
stress incontinence and detrusor instability than in the
normal population. In those with detrusor instability K. Mukherjee et al discussed in the study to determine
the body mass index was found to increase with age the effectiveness of the tension-free vaginal tape in
and parity. In women with genuine stress incontinence obese women with genuine stress incontinence , in
the body mass index increased with age and the whom obesity is often considered a relative
number of previous incontinence operations It was contraindication to surgical treatment by traditional
higher in nulliparous than in parous women. There approaches, e.g. Burch suspension and slings or
was no significant difference between obese and no injectable. Methodology was used for this study is
obese women in any of the urodynamic variables data on 242 consecutive women with uro dynamically
measured in the two incontinence groups (27) J. proven GSI were collected prospectively. The women
M. CummingsC. B. Rodning et al obesity is a were subdivided into three groups with a body mass
common disorder among women in urbanized index (BMI) of < 25, 25–29 and 30; obesity was
countries and has a major impact on stress urinary defined as a BMI of 30. All procedures were
incontinence. Women misery from obesity manifest performed under spinal anesthesia. The King's
increased intra-abdominal pressures, which adversely validated quality of life questionnaires (version 7)
stress the pelvic floor and may contribute to the were completed before and 6 months after surgery.
development of urinary incontinence. In addition, The subjective results were defined as a cure,
obesity may affect the neuromuscular function of the significant improvement or failure. The result of the
genitourinary tract, thereby also contributing to study was virtually 90% of the obese women with GSI
incontinence. Consequently, thorough evaluation of were cured, while the remaining 10% noted a
obese women must be performed prior to the considerable improvement in their symptoms. There
institution of treatment. Weight loss may relieve was no significant difference in cure rates among the
urinary incontinence, but definitive therapy via three groups. There was a highly significant
operative procedures is actual even in obese patients (P < 0.001) improvement in quality of life in all
and should be suggested with confidence.(14)Steinar groups. The conclusion of the study was TVT is at
Hunskar et al to appraisal epidemiological literature least as effective in obese women as in those with a
of urinary incontinence with respect to overweight and lower BMI. The TVT is a simple and minimally
obesity as a risk factor, and how the findings invasive procedure, with low morbidity even in the
eventually fulfill general criteria for being a causal obese group. TVT can be offered confidently to all
factor for the condition. Likewise to review all obese women with GSI.(29).
interventional studies assessing the effect of weight
reduction on incontinence. The author used the Leslee L. Subak, M.D et al discussed in the study
methodology of this study is Systematic searches until obesity is an recognized and adaptable risk factor for
June 2008 for publications of community based urinary incontinence, but conclusive evidence for a
prevalence studies with bivariate or multivariate beneficial effect of weight loss on urinary
analyses of the association between urinary incontinence is lacking. The methodology was used in
incontinence in women and overweigh/obesity. In this randomly assigned 338 overweight and obese
addition an attempt was made to identity and assess all women with at least 10 urinary-incontinence episodes
relevant longitudinal studies, prospective case series, per week to an intensive 6-month weight-loss program
and trials, whatever design. The results of the study that included diet, exercise, and behavior modification
was there is evidence 3 and some evidence 2 level data (226 patients) or to a structured education program
to support that in addition to BMI, waist-hip ratio and (112 patients). The result of the study was the mean
thus abdominal obesity may be an independent risk age of the participants was 53±11 years. The
www.iajps.com Page 2777
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
body-mass index (BMI) (the weight in kilograms associated with a lower risk of incontinence. Other
divided by the square of the height in meters) and the obstetric factors were not significantly associated with
weekly number of incontinence episodes as recorded the risk of incontinence 12 years later. Patients who
in a 7-day diary of voiding were similar in the were overweight before their first pregnancy were at
intervention group and the control group at baseline increased risk. The conclusion of the study was onset
(BMI, 36±6 and 36±5, respectively; incontinence of stress urinary incontinence during first pregnancy
episodes, 24±18 and 24±16, respectively). The or puerperal period carries an increased risk of
women in the intervention group had a mean weight long-lasting symptoms.(31)
loss of 8.0% (7.8 kg), as compared with 1.6% (1.5 kg)
in the control group (P<0.001). After 6 months, the Gisele Martins et al discussed in the study
mean weekly number of incontinence episodes physiological and anatomical changes of pregnancy
decreased by 47% in the intervention group, as are risk factors for lower urinary tract symptoms
compared with 28% in the control group (P=0.01). As (LUTS). This study aimed to evaluate the prevalence
compared with the control group, the intervention and risk factors for urinary incontinence (UI) in
group had a greater decrease in the frequency of healthy pregnant women. The methodology was used
stress-incontinence episodes (P=0.02), but not of a cross-sectional study was conducted in pregnant
urge-incontinence episodes (P=0.14). A higher Brazilian women who enrolled in the primary
proportion of the intervention group than of the health-care system in Sao Jose do Rio Prato, Brazil.
control group had a clinically relevant reduction of Face-to-face interview and completion of two-part
70% or more in the frequency of all incontinence questionnaire were administered and done which
episodes (P<0.001), stress-incontinence episodes evaluated the presence of LUTS pre- and during
(P=0.009), and urge-incontinence episodes (P=0.04). pregnancy. The data were analyzed by logistic
The conclusion of the study was 6-month behavioral regression. The result of the study was five hundred
intervention targeting weight loss reduced the pregnant women were enrolled ranging from first to
frequency of self-reported urinary-incontinence third trimester. LUTS present in 63.8% in these
episodes among overweight and obese women as women; the main associated risk factors were
compared with a control group. A decrease in urinary multiparty and pre -pregnancy LUTS as well as
incontinence may be another benefit among the smoking, constipation, and daily coffee intake. The
extensive health improvements associated with conclusion of the study was the prevalence of UI
moderate weight reduction.(30) during pregnancy is high, highlighting the presence
of the risk factors associated with UI during
Viktrup, Lars MD et al discussed the estimation the pregnancy.(32)
impact of onset of stress urinary incontinence in first
pregnancy or postpartum period, for the risk of Arnold T. M. Bernards et al stress urinary
symptoms 12 years after the first delivery. The incontinence (SUI) is the most common form of
methodology was used longitudinal cohort study, 241 incontinence impacting on quality of life (QOL) and is
women answered validated questions about stress associated with high financial, social, and emotional
urinary incontinence after first delivery and 12 years costs. The purpose of this study was to provide an
later. The result of the study was twelve years after update existing Dutch evidence-based clinical practice
first delivery the prevalence of stress urinary guidelines (CPGs) for physiotherapy management of
incontinence was 42% (102 of 241). The 12-year patients with stress urinary incontinence (SUI) in
incidence was 30% (44 of 146). The prevalence of order to support physiotherapists in decision making
stress urinary incontinence 12 years after first and improving efficacy and uniformity of care.
pregnancy and delivery was significantly higher Materials and methodology was used in this study was
(P<.01) in women with onset during first pregnancy a computerized literature search of relevant databases
(56%, 37 of 66) and in women with onset shortly after was performed to search for information regarding
delivery (78%, 14 of 18) compared with those without etiology, prognosis, and physiotherapy assessment
initial symptoms (30%, 44 of 146). In 70 women who and management in patients with SUI. Where no
had onset of symptoms during first pregnancy or evidence was available, recommendations were based
shortly after the delivery but remission 3 months on consensus. Clinical application of CPGs and
postpartum, a total of 40 (57%) had stress urinary feasibility were reviewed. The diagnostic process
incontinence 12 years later. In 11 women with onset of consists of systematic history taking and physical
symptoms during the first pregnancy or shortly after examination supported by reliable and valid
delivery but no remission 3 months postpartum, a total assessment tools to determine physiological potential
of 10 (91%) had stress urinary incontinence 12 years for recovery. Therapy is related to different problem
later. Cesarean during first delivery was significantly categories. SUI treatment is generally based on pelvic
www.iajps.com Page 2778
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
floor muscle exercises combined with patient and lifestyles are sedentary.
education and counseling. An important strategy is to
reduce prevalent SUI by reducing influencing risk
factors(21) MATERIALS AND METHODS
Study Design: Cross sectional
OBJECTIVES Setting Data was collected from different hospitals of
To determine the prevalence of urinary incontinence Lahore
among postpartum patients according to different BMI Duration of study was completed within 6 months
group. after the approval of synopsis
4. Operational definition Sample size: One hundred Ninety individuals
Urinary incontinence Sample Technique: Non-probability convenient
The loss of bladder control — is a common and often sampling
embarrassing problem. The severity ranges from Sample selection criteria
occasionally leaking urine when you cough or sneeze Inclusion Criteria:
to having an urge to urinate that’s so sudden and • Pre menopause
strong you don't get to a toilet in time • Postpartum
Exclusion Criteria:
BMI • Hysterectomy
BMI is a person's weight in kilograms (kg) divided by • Tumor
his or her height in meters squared. The National • Vaginal cyst or ovarian cyst
Institutes of Health (NIH) now defines normal weight, Methodology
overweight, and obesity according to BMI rather than A study was conducted in the different hospitals of
the traditional height/weight charts. Overweight is a Lahore. One hundred ninety postpartum women were
BMI of 27.3 or more for women and 27.8 or more for take part in this study. The women included,
men. postpartum, pre menopause, exclusion criteria is the
hysterectomy, tumor, vaginal cyst or ovarian cyst
Postpartum women. In cross sectional study 190 women
A postpartum (or postnatal) period begins participated to give data with consent, 5(2.63%) were
immediately after the birth of a child and extends for underweight women, 79 (41.5%) normal, overweight
about six weeks,[1] as the mother's body, 105 (55.26%). ICIQ-UI standardized questionnaire is
including hormone levels and uterus size, returns to a used to check the urinary incontinence with
non-pregnant state. Less frequently used are the demographic data. The BMI data will be taken from
terms puerperium or puerperal period. the participant’s weight in kg and height in feet and
after than feet converted into meters. All assessments
Overweight received ethical approval and all participants gave
Being overweight or fat is having more body fat than informed consent. Data was analyzed by SPSS version
is optimally healthy. Being overweight is especially 21.0
common where food supplies are plentiful
RESULTS:
www.iajps.com Page 2779
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
Mean age of the subjects was 28.81 ± 5.03years. Out of 190, 26.9% of the women reported urinary incontinence.
5(2.63%) were underweight women, 79 (41.5%) normal, overweight 105 (55.26%) and 1 obese women (0.61%).
Association of urinary incontinence with different BMI groups was determined using chi square test. P-value of 0.05or
less was considered as significant.
www.iajps.com Page 2780
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
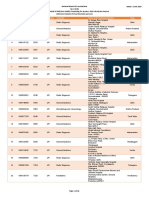
Body Mass Index * do you have Urinary Incontinence Crosstabulation
do you have Urinary Incontinence Total
no yes
Count 4 1 5
Under Weight
% within Body Mass Index 80.0% 20.0% 100.0%
Count 55 24 79
Normal
% within Body Mass Index 69.6% 30.4% 100.0%
Body Mass Index
Count 77 28 105
Over Weight
% within Body Mass Index 73.3% 26.7% 100.0%
Count 1 0 1
Obese
% within Body Mass Index 100.0% 0.0% 100.0%
Count 137 53 190
Total
% within Body Mass Index 72.1% 27.9% 100.0%
www.iajps.com Page 2781
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
www.iajps.com Page 2782
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
www.iajps.com Page 2783
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
www.iajps.com Page 2784
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
Body Mass Index
How often do you leak urine Under weight Normal Overweight Obese
never 3(2.30%) 59(45.00%) 68(51.90%) 1(0.80%)
About once a week or less a week 0(0.00%) 2(66.70%) 1(33.30%) 0(0.00%)
Two or three times a week 0(0.00%) 5(71.40%) 2(28.60%) 0(0.00%)
Once a day 0(0.00%) 5(33.30%) 10(66.70%) 0(0.00%)
Several times a day 0(0.00%) 16(61.50%) 10(38.50%) 0(0.00%)
Total 3(1.60%) 87(47.80%) 91(50.00%) 1(0.50%)
In this study leakage of urine also discussed the total percentage of underweight is (1.60%), (2.3%) normal (47.80%),
in overweight (50%) and in obese (0.50%). Fisher's exisure test is apply for this check to leaking of urine frequency
and maximum frequency found in overweight women
DISCUSSION: postpartum women is disturb and irritating. Fusilier et
In this study our population is postpartum women, we al discussed was obesity is very prevalent and is
assessed the prevalence of urinary incontinence and, associated with stress urinary incontinence. The
association among postpartum women. We found that determinations of this review are to assess the
urinary incontinence was very common in overweight pathophysiology of stress urinary incontinence in the
women due to excessive fat on the belly portion causes obese female and review the outcomes of weight loss
exert pressure on the urinary bladder. Daily routine of and anti-incontinence surgery in this population. The
www.iajps.com Page 2785
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
assumptions of the study was increased International Journal of Gynecology &
intra-abdominal pressure appears to be the common Obstetrics. 1993;43(2):235-.
pathophysiologic link between obesity and stress 5. Jolleys JV. Reported prevalence of urinary
urinary incontinence, neurogenic and metabolic incontinence in women in a general practice. Br
pathways. Both surgical and non-surgical weight loss Med J (Clin Res Ed). 1988;296(6632):1300-2.
continue to have supportive effects on however, 6. Kölbl H, Riss P. Obesity and stress urinary
long-term outcomes are largely absent. But in our incontinence: significance of indices of relative
study we discussed the urinary incontinence in women weight. Urologia internationalis.
and its association between with high BMI postpartum 1988;43(1):7-10.
women and overweight women and urinary 7. Bump RC, Sugerman HJ, Fantl JA, McClish DK.
incontinence is increased in overweight is more than Obesity and lower urinary tract function in
underweight and normal postpartum women .(33) women: effect of surgically induced weight loss.
DeFoor WR Jr et al was debated obesity has been American Journal of Obstetrics & Gynecology.
associated with daytime urinary incontinence, likely 1992;167(2):392-9.
due to enlarged intra-abdominal pressure. The author 8. Bump RC, McClish DK. Cigarette smoking and
assess symptoms of urinary incontinence in severely urinary incontinence in women. American
obese adolescents before and 3 years after bariatric Journal of Obstetrics & Gynecology.
surgery. The result of in females than in 1992;167(5):1213-8.
males. Incontinence status significantly improved by 9. CAMPBELL AJ, Reinken J, McCosh L.
6 months and was durable to 3 years after surgery, Incontinence in the elderly: prevalence and
signifying that bariatric surgery constructively affects prognosis. Age and Ageing. 1985;14(2):65-70.
anatomic or physiologic mechanisms of bladder 10. Hartz A, Barboriak PN, Wong A, Katayama KP,
control in both males and females.in this study author Rimm AA. The association of obesity with
check urinary incontinence in both gender male and infertility and related menstural abnormalities in
female and check association between urinary women. International journal of obesity.
incontinence after 3 years of surgery while in our 1979;3(1):57-73.
study we assess the postpartum women from recent to 11. Hays NP, Bathalon GP, McCrory MA, Roubenoff
6 years and above and check association between R, Lipman R, Roberts SB. Eating behavior
urinary incontinence in overweight women .(34) correlates of adult weight gain and obesity in
healthy women aged 55–65 y. The American
CONCLUSION: journal of clinical nutrition. 2002;75(3):476-83.
The firmness of the study was to determine urinary 12. Mommsen S, Foldspang A. Body mass index and
incontinence. It is a communal problem in overweight adult female urinary incontinence. World journal
women. Urinary incontinence is more as compared of of urology. 1994;12(6):319-22.
normal and underweight women and the associated 13. Foldspang A, Mommsen S. Overweight and
factors that are avertible, modifiable and overweight urinary incontinence in women. Ugeskrift for
and high BMI may have the greatest impact on the laeger. 1995;157(42):5848-51.
prevalence of urinary incontinence. Urinary 14. Cummings J, Rodning C. Urinary stress
incontinence is more due to intra-abdominal pressure incontinence among obese women: review of
and pelvic floor muscle weakness. pathophysiology therapy. International
Urogynecology Journal. 2000;11(1):41-4.
REFERENCES 15. Khong S-Y, Jackson S. Obesity and urinary
1. Brown JS, Seeley DG, Fong J, Black DM, Ensrud incontinence. Menopause international.
KE, Grady D, et al. Urinary incontinence in older 2008;14(2):53-6.
women: who is at risk? Obstetrics & Gynecology. 16. Christofi N, Hextall A. Obesity and urinary
1996;87(5):715-21. incontinence. SAGE Publications Sage UK:
2. Muennig P, Lubetkin E, Jia H, Franks P. Gender London, England; 2008.
and the burden of disease attributable to obesity. 17. Curhan GC, Chertow GM, Willett WC,
American Journal of Public Health. Spiegelman D, Colditz GA, Manson JE, et al.
2006;96(9):1662-8. Birth weight and adult hypertension and obesity
3. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, in women. Circulation. 1996;94(6):1310-5.
Clark AL. Epidemiology of surgically managed 18. Gore SA, Brown DM, West DS. The role of
pelvic organ prolapse and urinary incontinence. postpartum weight retention in obesity among
Obstetrics & Gynecology. 1997;89(4):501-6. women: a review of the evidence. Annals of
4. Bump RC. Racial comparisons and contrasts in Behavioral Medicine. 2003;26(2):149-59.
urinary incontinence and pelvic organ prolapse. 19. Baker JL, Gamborg M, Heitmann BL, Lissner L,
www.iajps.com Page 2786
IAJPS 2018, 05 (04), 2774-2787 Abu Bakar Khan et al ISSN 2349-7750
Sørensen TI, Rasmussen KM. Breastfeeding Gynecology. 2006;108(2):248-54.
reduces postpartum weight retention. The 32. Martins G, Soler ZA, Cordeiro JA, Amaro JL,
American journal of clinical nutrition. Moore KN. Prevalence and risk factors for
2008;88(6):1543-51. urinary incontinence in healthy pregnant
20. Arendas K, Qiu Q, Gruslin A. Obesity in Brazilian women. International urogynecology
pregnancy: pre-conceptional to postpartum journal. 2010;21(10):1271-7.
consequences. Journal of Obstetrics and 33. Fuselier A, Hanberry J, Lovin JM, Gomelsky A.
Gynaecology Canada. 2008;30(6):477-88. Obesity and Stress Urinary Incontinence: Impact
21. Rasmussen KM, Kjolhede CL. Prepregnant on Pathophysiology and Treatment. Current
overweight and obesity diminish the prolactin urology reports. 2018;19(1):10.
response to suckling in the first week postpartum. 34. DeFoor WR, Inge TH, Jenkins TM, Jackson E,
Pediatrics. 2004;113(5):e465-e71. Courcoulas A, Michalsky M, et al. Prospective
22. Ong KK, Ahmed ML, Emmett PM, Preece MA, evaluation of urinary incontinence in severely
Dunger DB. Association between postnatal obese adolescents presenting for weight loss
catch-up growth and obesity in childhood: surgery. Surgery for Obesity and Related
prospective cohort study. Bmj. Diseases. 2018;14(2):214-8.
2000;320(7240):967-71.
23. Rooney BL, Schauberger CW. Excess pregnancy
weight gain and long-term obesity: one decade
later. Obstetrics & Gynecology.
2002;100(2):245-52.
24. Lederman SA. Pregnancy weight gain and
postpartum loss: avoiding obesity while
optimizing the growth and development of the
fetus. Journal of the American Medical Women's
Association (1972). 2001;56(2):53-8.
25. Vesco KK, Dietz PM, Rizzo J, Stevens VJ, Perrin
NA, Bachman DJ, et al. Excessive gestational
weight gain and postpartum weight retention
among obese women. Obstetrics & Gynecology.
2009;114(5):1069-75.
26. Mottola MF. Exercise prescription for overweight
and obese women: pregnancy and postpartum.
Obstetrics and Gynecology Clinics.
2009;36(2):301-16.
27. Dwyer P, Lee E, Hay D. Obesity and urinary
incontinence in women. BJOG: An International
Journal of Obstetrics & Gynaecology.
1988;95(1):91-6.
28. Hunskaar S. A systematic review of overweight
and obesity as risk factors and targets for clinical
intervention for urinary incontinence in women.
Neurourology and urodynamics.
2008;27(8):749-57.
29. Mukherjee K, Constantine G. Urinary stress
incontinence in obese women: tension‐ free
vaginal tape is the answer. BJU international.
2001;88(9):881-3.
30. Subak LL, Wing R, West DS, Franklin F,
Vittinghoff E, Creasman JM, et al. Weight loss to
treat urinary incontinence in overweight and
obese women. New England Journal of Medicine.
2009;360(5):481-90.
31. Viktrup L, Rortveit G, Lose G. Risk of stress
urinary incontinence twelve years after the first
pregnancy and delivery. Obstetrics &
www.iajps.com Page 2787
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Assessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaDocumento7 páginasAssessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaBaru Chandrasekhar RaoAinda não há avaliações
- Chapter 14 Intravenous Solutions, Equipment, and CalculationsDocumento48 páginasChapter 14 Intravenous Solutions, Equipment, and CalculationsEn Ras100% (1)
- Neurology Assessment BlueprintDocumento7 páginasNeurology Assessment Blueprintidno1008Ainda não há avaliações
- 1979 Trevor L, P. Watts, Edwars C. Combe. Periodontal Dressing MaterialsDocumento13 páginas1979 Trevor L, P. Watts, Edwars C. Combe. Periodontal Dressing MaterialsAlejandro MorenoAinda não há avaliações
- The Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalDocumento11 páginasThe Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalBaru Chandrasekhar RaoAinda não há avaliações
- Dorothy Johnson (Report)Documento24 páginasDorothy Johnson (Report)mlbonthelineAinda não há avaliações
- Development of Cell Culture System From Selected Tissues of Pangaius HypopthalmusDocumento6 páginasDevelopment of Cell Culture System From Selected Tissues of Pangaius HypopthalmusBaru Chandrasekhar RaoAinda não há avaliações
- Development and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormDocumento11 páginasDevelopment and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormBaru Chandrasekhar RaoAinda não há avaliações
- Genetic Enhancment of Groundnut (Arachis Hypogaea L.) Through Induced Muiation.Documento5 páginasGenetic Enhancment of Groundnut (Arachis Hypogaea L.) Through Induced Muiation.Baru Chandrasekhar RaoAinda não há avaliações
- Formulation, Optimization and Evaluation Colon Targated Drug Delivery System For OrniadazoleDocumento9 páginasFormulation, Optimization and Evaluation Colon Targated Drug Delivery System For OrniadazoleBaru Chandrasekhar RaoAinda não há avaliações
- Analytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationDocumento8 páginasAnalytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationBaru Chandrasekhar RaoAinda não há avaliações
- Non-Adherence in Hyppertensive Patients of Peshawar, PakistanDocumento13 páginasNon-Adherence in Hyppertensive Patients of Peshawar, PakistanBaru Chandrasekhar RaoAinda não há avaliações
- Gastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsDocumento7 páginasGastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsBaru Chandrasekhar RaoAinda não há avaliações
- Knowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyDocumento8 páginasKnowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyBaru Chandrasekhar RaoAinda não há avaliações
- The Bordering Areas (Nine Areas of Panjgur District) Issue of Pakistan About Human Malaria Prevalence: A Cross-Sectional Research of Malaria Parasites Identification in Blood SlidesDocumento8 páginasThe Bordering Areas (Nine Areas of Panjgur District) Issue of Pakistan About Human Malaria Prevalence: A Cross-Sectional Research of Malaria Parasites Identification in Blood SlidesBaru Chandrasekhar RaoAinda não há avaliações
- Simultaneous Estimation of Rosuvastatin Calcium and Ezetimibe As Bulk Drug and in Tablet Dosage Form by RP-HPLC MethodDocumento6 páginasSimultaneous Estimation of Rosuvastatin Calcium and Ezetimibe As Bulk Drug and in Tablet Dosage Form by RP-HPLC MethodBaru Chandrasekhar RaoAinda não há avaliações
- A Brief Review On YawsDocumento7 páginasA Brief Review On YawsBaru Chandrasekhar RaoAinda não há avaliações
- Preparation of Silver Nanoparticles From Herbal PlantDocumento9 páginasPreparation of Silver Nanoparticles From Herbal PlantBaru Chandrasekhar RaoAinda não há avaliações
- Nephroprotective Activityof Acorus Calamus Leaves Extract Against Lithium Induced Nephrotoxicity in Wistar RatsDocumento12 páginasNephroprotective Activityof Acorus Calamus Leaves Extract Against Lithium Induced Nephrotoxicity in Wistar RatsBaru Chandrasekhar RaoAinda não há avaliações
- Relationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityDocumento4 páginasRelationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityBaru Chandrasekhar RaoAinda não há avaliações
- Role of Simvastatin in Addition To Metformin in Polycystic Ovarian Syndrome Patients, A Randomized Controlled Trial On Pakistani WomenDocumento4 páginasRole of Simvastatin in Addition To Metformin in Polycystic Ovarian Syndrome Patients, A Randomized Controlled Trial On Pakistani WomenBaru Chandrasekhar RaoAinda não há avaliações
- An Incidence of Hypertension Among People and Its Association To Consumption of Hard Water: A Cross-Sectional ResearchDocumento6 páginasAn Incidence of Hypertension Among People and Its Association To Consumption of Hard Water: A Cross-Sectional ResearchBaru Chandrasekhar RaoAinda não há avaliações
- An Epidemiological Survey About The Infections Caused by Dengue in The Perspective of Hematological, Clinical and Demographic Risk FactorsDocumento6 páginasAn Epidemiological Survey About The Infections Caused by Dengue in The Perspective of Hematological, Clinical and Demographic Risk FactorsBaru Chandrasekhar RaoAinda não há avaliações
- Review On: Inventory ManagementDocumento8 páginasReview On: Inventory ManagementBaru Chandrasekhar RaoAinda não há avaliações
- Association of Socioeconomic Status, Hypertension and Treatment Modality With Diabetic Amputation - A Case Control StudyDocumento4 páginasAssociation of Socioeconomic Status, Hypertension and Treatment Modality With Diabetic Amputation - A Case Control StudyBaru Chandrasekhar RaoAinda não há avaliações
- Pharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoDocumento7 páginasPharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoBaru Chandrasekhar RaoAinda não há avaliações
- Study of Clinical Profile of Transfused Thalassemic Childrens With Special Reference To Hepatitis B Profile and Liver Function.Documento6 páginasStudy of Clinical Profile of Transfused Thalassemic Childrens With Special Reference To Hepatitis B Profile and Liver Function.Baru Chandrasekhar RaoAinda não há avaliações
- After Acute Myocardial Infarction End Result of Cardiogenic Shock in Hospitalized PatientsDocumento4 páginasAfter Acute Myocardial Infarction End Result of Cardiogenic Shock in Hospitalized PatientsBaru Chandrasekhar RaoAinda não há avaliações
- Descriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreDocumento4 páginasDescriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreBaru Chandrasekhar RaoAinda não há avaliações
- C-Reactive Protein Levels Preoperatively and Postoperatively Effect On Cardiovascular Surgery ComplicationsDocumento5 páginasC-Reactive Protein Levels Preoperatively and Postoperatively Effect On Cardiovascular Surgery ComplicationsBaru Chandrasekhar RaoAinda não há avaliações
- An Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentDocumento6 páginasAn Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentBaru Chandrasekhar RaoAinda não há avaliações
- Isolation and Identification of Clostridium Perfringens Causing Enterotoxaemia in Bovine of Kacchi District Balochistan.Documento8 páginasIsolation and Identification of Clostridium Perfringens Causing Enterotoxaemia in Bovine of Kacchi District Balochistan.Baru Chandrasekhar RaoAinda não há avaliações
- Oppertunistic Hypertension Screening in Rural Health Population of Umar Abad Tehsil Kharezat Disrtrict Pishin Balochistan. A Cross Sectional StudyDocumento10 páginasOppertunistic Hypertension Screening in Rural Health Population of Umar Abad Tehsil Kharezat Disrtrict Pishin Balochistan. A Cross Sectional StudyBaru Chandrasekhar RaoAinda não há avaliações
- A Cross Sectional Survey Information About Weaning Process Among Mothers of Infants Above 6 Months of Age in Opd Pediatrics at Kishwer Fazal Teaching Hospital LahoreDocumento8 páginasA Cross Sectional Survey Information About Weaning Process Among Mothers of Infants Above 6 Months of Age in Opd Pediatrics at Kishwer Fazal Teaching Hospital LahoreBaru Chandrasekhar RaoAinda não há avaliações
- TVVP-CAS SPL NotificationDocumento10 páginasTVVP-CAS SPL NotificationKranthi RajAinda não há avaliações
- Bta Brochure 10-15 CompleteDocumento8 páginasBta Brochure 10-15 CompletePop IonAinda não há avaliações
- Review Article: Occlusal Schemes For Complete Dentures - A Review ArticleDocumento6 páginasReview Article: Occlusal Schemes For Complete Dentures - A Review ArticleoktikikiAinda não há avaliações
- Fixation of The Distal Tibiofibular Bone-Bridge in Transtibial Amputation PDFDocumento4 páginasFixation of The Distal Tibiofibular Bone-Bridge in Transtibial Amputation PDFThomas BowersAinda não há avaliações
- Jurnal DDHDocumento18 páginasJurnal DDHAulia RizkiAinda não há avaliações
- Dental Liaison Committee in The EUDocumento545 páginasDental Liaison Committee in The EUirinalully100% (1)
- Allotment Details of DNB Final Round Counseling for January 2019Documento48 páginasAllotment Details of DNB Final Round Counseling for January 2019Raghul KrishnasamyAinda não há avaliações
- Validation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent PlacentaDocumento2 páginasValidation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent PlacentaOmpAinda não há avaliações
- John Ioannidis' CVDocumento146 páginasJohn Ioannidis' CVFelipe BrandãoAinda não há avaliações
- MDocumento86 páginasMeheidariAinda não há avaliações
- Lupus NeonatalDocumento2 páginasLupus NeonatalFer45Ainda não há avaliações
- Down Syndrome: An Overview: March 2016Documento7 páginasDown Syndrome: An Overview: March 2016Hartotok VipnetAinda não há avaliações
- F1581 08 (2016)Documento4 páginasF1581 08 (2016)masoudAinda não há avaliações
- Patient Evaluation and Wound Assessment: Key Practice PointsDocumento6 páginasPatient Evaluation and Wound Assessment: Key Practice PointsFofiuAinda não há avaliações
- Clinic Ore Cases New TemplateDocumento68 páginasClinic Ore Cases New TemplateAnonymous StuglR6tQAinda não há avaliações
- Charles Burstone PDFDocumento2 páginasCharles Burstone PDFPaola Lolo100% (1)
- Jurnal Terapi CA ColonDocumento4 páginasJurnal Terapi CA ColonyopiAinda não há avaliações
- Independent/Advanced Practice NurseDocumento25 páginasIndependent/Advanced Practice NurseswethashakiAinda não há avaliações
- Intensive Management of Pediatric Acute Liver FailureDocumento11 páginasIntensive Management of Pediatric Acute Liver FailureAditya SeptiadinataAinda não há avaliações
- Sports DentistryDocumento11 páginasSports DentistryMaqbul AlamAinda não há avaliações
- Sudden Unexplained Early Neonatal Death or CollapsDocumento7 páginasSudden Unexplained Early Neonatal Death or CollapsMaria Alejandra ForeroAinda não há avaliações
- Lucas 1917Documento124 páginasLucas 1917abcd_9876Ainda não há avaliações
- Hearing Related Quality of Life Outcomes For 2016 European Annals of OtorhiDocumento6 páginasHearing Related Quality of Life Outcomes For 2016 European Annals of OtorhiElmoPranauskasAinda não há avaliações
- Ancient Egypt's Views on Light, Blindness, and Eye HealthDocumento18 páginasAncient Egypt's Views on Light, Blindness, and Eye HealthAdnan BuljubašićAinda não há avaliações
- SAFE Poster On PEWS - Evelina Children's HospitalDocumento1 páginaSAFE Poster On PEWS - Evelina Children's HospitalSepriwan ElidraAinda não há avaliações