Escolar Documentos
Profissional Documentos
Cultura Documentos
Adrenal Cortex DR - Gomez
Enviado por
vicbart11Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Adrenal Cortex DR - Gomez
Enviado por
vicbart11Direitos autorais:
Formatos disponíveis
Adrenal Cortex Physiology
Dr. Carina C. Gomez, February 21, 2017
Suprarenal – the adrenal glands are structures above the
kidneys.
Adrenal – adrenal glands adjacent to kidney.
Each adrenal gland weighs around 4 grams.
2 MAJOR DIVISIONS
Adrenal Medulla
o Inner part, 10-20%
o comprised of neurons that migrate from
neuroectodermal tissue to the abdominal cavity where
they are enclosed within the adrenal cortex that are
trapped inside (Neuroectodermal).
o The neurons lose their axons and become secretory cells,
secreting neurotransmitters directly into the blood, thus
are also considered hormones. (mediates
Neuroendocrine signaling)
o This includes the catecholamines primarily epinephrine
80%, norepinephrine 20% & dopamine in small amount.
Adrenal Cortex
o Outer part, 80-90%
o Mesodermal origin.
o These are secreting cells (not neurons).
o 3 major hormones are secreted here (corticosteroids)
these include: mineralocorticoids – prototype substance
is aldosterone; glucocorticoids – cortisol; androgens –
prototype substance is DHEA dehydroepiandrosterone.
*Although these are known as adrenal gland, these are 2 different
structures.
* 3 zones of the adrenal cortex, acronym = (G.F.R)
Zona glomerulosa, Zona fasciculata, Zona reticularis
*In the Zona reticularis DHEA is produced initially then it is
converted into testosterone & estrogen.
TRANS BY: TEAM PAGE 1 OF 13
Blood Supply
o from the aorta, renal and phrenic arteries
o Direction of blood flow from these vessels should always be
from the adrenal cortex to the medulla.
Why?
o Well because of the enzyme phenylethanolamine-N-
methyl transferase (PNMT) that converts norepinephrine
(NE) to epinephrine (E) (Dra. says a slightly different name
in the recording so I double checked on google! - ;))
o primarily found in the cortex of the adrenal gland
(although some books claim it can be found in other
organs).
o Blood flow from the cortex to the medulla will wash
out PNMT into the medulla where it is needed. Another acronym by Dra. (GFRSSS) – Glomerulosa, fasciculata,
o Conversion of NE to E is cortisol dependent. reticularis, salt, sugar, sex!
Layers of Adrenal Cortex Steroids are referred to as wonder drugs because they treat
many illnesses however they have massive side effects.
Adrenal Regulation
Zona Glomerulosa
o outermost layer
o 15% of the adrenal cortex.
o The only layer capable of secreting mineralocorticoid in the
form of aldosterone due to presence of aldosterone
synthase which is absent in other layers.
o Secretes substances important in salt metabolism. Regulation of adrenal cortex secretion is mainly via Negative
Zona Fasciculata Feedback.
o thickest layer o The initiating stimulus is always opposite the response;
o 75% of the adrenal cortex. ↑initiating stimulus ↓response.
o Secretes glucocorticoids in the form of cortisol & also Negative feedback is not always inhibitory. It can also be
corticosteroids. Androgen secretion also occurs but in stimulatory.
lesser amounts.
o Secretions important for sugar (glucose) metabolism. ↑Cortisol, ↑androgen = inhibitory effect to hypothalamus &
Zona Reticularis pituitary (ACTH dependent hormones).
o thinnest layer ↑Aldosterone has no inhibitory effect on hypothalamus &
o 10% of the adrenal cortex. pituitary because aldosterone is ACTH independent. It is
o Primarily secretes androgen in the form of DHEA which is regulated by RAAS. (ACTH increases Aldosterone, but
converted to testosterone & estrogen. Also secretes Aldosterone will not give feedback)
glucocorticoid but in lesser amounts.
o Secretions important for sex.
TRANS BY: TEAM PAGE 2 OF 13
What are the stimuli for adrenocortical hormone secretion? : Beta lipoproteins – substances with opioid-like action, pain
STRESS! Any type of stress, running, jogging, emotions, surgery, suppressing agents, analgesia system in the body.
hot weather, fever, psychosis, burns, lab manuals. 4 steps in pain transmission;
Sometimes on admission to hospital, blood sugar is high but this Transduction
does not mean one has diabetes. (That’s why Dra. resigned from Transmission
her many chairman positions, to avoid stress. And she will not be Perception
stressed by us, rather, we should be the one to be stressed ;) ) Pain modulation – this step is affected by beta
lipoproteins or endorphins (endogenous opioid
peptide).
MSH – secreted from the intermediate lobe in lower animals,
activates melanocytes in melanopores to cause skin
pigmentation.
*Humans have no MSH because we do not have intermediate
lobe we have no melanocortin activated by ACTH.
Stress activates the paraventricular nuclei to secrete CRH →
which acts on anterior pituitary (corticotropes) to release POMC
(Proopiomelanocortin – large structure with an N-Carboxy
terminal) → which is cleaved, one of the fragments is ACTH →
acts on adrenal cortex increasing secretion of aldosterone,
cortisol, androgen.
Pathways:
Zona Glomerulosa – Mineralocorticoid Pathway
And so on…
All of them come from CHOLESTEROL (that is why they are
called steroid hormones)
Rate-Limiting Step – Conversion of Cholesterol to
Pregnenolone (will not be converted back)
After conversion, it will now depend on what enzyme is
present on that layer to determine the path it will take.
CORTISOL SECRETION
PRIMARILY Negative feedback : Hypothalamic-
Pituitary Axis (CRH-ACTH axis)
Circadian rhythm – ↑morning ↓evening
TRANS BY: TEAM PAGE 3 OF 13
ANDROGEN SECRETION Effect of ACTH on Adrenal Cortical Cells
Hypothalamic-Pituitary Axis (CRH-ACTH Axis) CRH ACTH will bind either to Adrenocortical cells (Binds
Cortical Androgen-Stimulating Hormone with Melanocortin 2 Receptor, MC2R) or the skin (MC1R - will
Cortisol has a greater effect on HPA than androgen, cause skin pigmentation)
both are ACTH dependent hormones.
Also Developmental pattern of secretion Binding with MC2R Effects:
Immediate: Production of Hormones (Aldosterone, Cortisol,
ALDOSTERONE SECRETION Androgen) by activating all enzymes needed
ECF Potassium Ion Concentration ( K+) Subsequent/Intermediate: Enzyme/Protein Synthesis and
(Major mechanism regulating aldosterone) Gene Transcription (p450 dependent – occurs in mitochondria)
Hyperkalemia - activates aldosterone secretion thus
Long-Term: structural changes in adrenal cortex
increasing K secretion.
Hypokalemia – Inhibits aldosterone secretion, Hypertrophy – Size and functional complexity of organelles
decreasing K secretion. Hyperplasia – size and number of cells
Renin-Angiotensin-Aldosterone System (AII)
Angiotensin II
ECF Sodium Ion Concentration ( Na+)
Minor mechanism
Hypothalamic-Pituitary Axis (ACTH)
(has little effect on controlling the rate of secretion)
The Suprachiasmatic Nuclei in the hypothalamus controls the
Highest secretion of cortisol is at 8 in the morning, lowest at 8 in
set point of various body activities.
the evening – circadian rhythm.
Thirst – controlled by ventrolateral hypothalamus
Satiety – controlled by ventromedial hypothalamus
Temperature (hot) – controlled by anterior hypothalamus
Temperature (cold) – controlled by posterior
hypothalamus
Endocrine function – supraoptic, paraventricular, arcuate
For Adrenal Cortex - PARAVENTRICULAR
TRANS BY: TEAM PAGE 4 OF 13
Stimuli for release of renin;
Low arterial blood pressure/hypotension
low ECF volume/dehydration
low total blood volume
low renal blood flow/hypoperfusion
increased sympathetic discharge *Starts with Cholesterol Pregnenolone (ACTH Dependent –
= these will activate JG cells in afferent & efferent arterioles to Rate-Limiting Step)
*Angiotensin II (facilitates conversion of corticosterone to
secrete renin acts on angiotensinogen from the liver
converting it into angiotensin 1 converted to angiotensin 2 by Hydroxycorticosterone, thus, increasing Aldosterone Production
ACE in the lungs, angiotensin 3,4,5,6,7,8 are produced by *Blockage of a pathway will lead to increase production of other
steroids (blockage of androgen, increase aldosterone and cortisol
aminopeptidases in the blood… all are vasoconstrictors,
production.
increase total peripheral resistance increasing blood pressure
to corrected initiating stimuli.
Angiotensin 2,3,4,5,6,7,8 are all potent stimulators causing the
adrenal cortex to secrete aldosterone which ↑Na reabsorption, ↑
K secretion
TRANS BY: TEAM PAGE 5 OF 13
Major source of cholesterol is LDL (80%) circulating in the blood MINERALOCORTICOIDS
→ binds with LDL receptor → enters the cell (can also be
Regulation of Salt
synthesized within the cell from acetyl CoA) → stored or Aldosterone - principal mineralocorticoid
esterified (cholesterol esters are formed if hormone is not o accounts for about 90%
needed immediately), hydrolysis occurs if hormones are needed o 60% (protein-bound usually inactive), 40% (free form
→ cholesterol enters the mitochondria (because conversion of usually active)
cholesterol to pregnenolone is P450 dependent) this process is o Half-life – 20 minutes (longer half-life because it is
ACTH dependent → pregnenolone leaves the mitochondria & protein-bound, unlike in insulin which is in free form)
enters smooth ER → converted to progesterone, 17-OH- o destroyed mainly in the liver (bile/feces, 25%), mainly
progesterone, 11-deoxycortisol (non P450 dependent reactions excreted in the urine
in smooth ER) → 11-deoxycortisol returns to the mitochondria to mainly affect electrolytes (minerals K+/Na+) of the ECF.
be converted to cortisol (P450 dependent) thus mitochondria When you change sodium concentration, water follows.
release cortisol. (Refer to endocrine system diagram above!) Thus, its main purpose is to regulate ECF Volume and ABP
Deoxycorticosterone, Corticosterone, Cortisone, Cortisol and
Cimetidine – anti-ulcer drug, P450 inhibitor.
9α Fluorocortisol (synthetic). These substances have
mineralocorticoid activity. Why is cortisol included here? It
is a glucocorticoid with mineralocorticoid activity.
ALDOSTERONE
Mineralocorticoid
Maintain BP, water, and salt balance
Help kidney retain sodium and excrete potassium
Functions to maintain blood volume and stabilize BP. – One
involved in CVS Long term control
*Aldosterone and Cortisol, if present in the blood, can easily
enter the cell. Its receptor is present in the cytoplasm.
*At the start, the receptor is bind to an inhibitory protein
(chaperone). When aldosterone is present, the inhibitory protein
dissociates. You now form Mineralocorticoid-Aldosterone
Complex enter the nucleus act on gene (Same with Cortisol)
*Steroid hormones are not usually stored in the cell unlike
proteins, polypeptides & catecholamines which are stored.
Cortisol is not stored appreciably in the adrenocortical
cells. Hence, an acute need for increased amounts of
circulating cortisol requires rapid activation by ACTH. (Familiarize yourself with the diagram above ↑)
In women, the adrenal glands ultimately supply 50 –
60% of the androgenic hormone requirements. That is
*Aminopeptidases in the blood will convert Ang II to Ang III, IV,
why androgen levels are low in women, so no
masculinizing effects. and so on…
In males additional androgen are produced by the testes.
TRANS BY: TEAM PAGE 6 OF 13
BIOLOGIC EFFECTS
renal tubular reabsorption of sodium (late DCT and
primarily CD)
Late DCT is blocked by K sparing diuretics (aka aldosterone
antagonists e.g. Spironolactone which blocks aldosterone
thus Na reabsorption is inhibited which means water is not
reabsorbed = diuresis.
K sparing because K is not secreted.
Another K sparing mechanism involves ENac (epithelial Na
channel e.g. Amiloride)
Another electrolyte being secreted is hydrogen, thus one
can develop metabolic alkalosis.
renal tubular secretion of potassium (DCT and CD)
renal tubular secretion of hydrogen (DCT and CD)
maintenance of ECF volume (principal function)
same effect to sweat glands, salivary glands, intestinal
epithelial cells in colon (Sodium and Potassium Absorption)
Hyperaldosteronism
*Aldosterone & cortisol are steroids – they bind to cytoplasmic
receptors (mineralocorticoid receptors MR). These receptors are
bound to inhibitory proteins, when aldosterone binds with the
MR, the inhibitory protein dissociates forming an MR-
aldosterone complex which then enters the nucleus, to regulate
gene expression by increasing the activity of the Na/K pump.
*Na pump hypothesis - ↑Na/K pump activity → Na reabsorbed
into ECF in exchange with K this leads to ↓Na inside the cell
which favors reabsorption permeability (permeate hypothesis).
↑K in ECF favors secretion of K.
*Aldosterone also increases mitochondrial activity to produce
more ATP for the Na/K pump (metabolic hypothesis).
(Refer to image above) o Problem is in the adrenal cortex = primary
o Problem anywhere outside the adrenal cortex = secondary
The manifestation is the same in both types. So, what is the
difference between primary & secondary?
TRANS BY: TEAM PAGE 7 OF 13
In primary – adrenal cortex secretion of aldosterone is very BIOLOGIC EFFECTS
high, it follows a negative feedback - ↑ aldosterone ↓renin
In secondary, it could be a problem in the kidney e.g. a tumor
increasing renin secretion. Therefore ↑renin = ↑aldosterone (no
more negative feedback because the tumor will continuously
increase renin secretion)
In primary - ↑aldosterone, ↓renin
In secondary - ↑ aldosterone, ↑renin
Thus, to differentiate the two, the doctor requests for the level of
renin.
Primary Aldosteronism (Conn’s Syndrome)
caused by a tumor of the zona glomerulosa cells or
hyperplasia of the adrenal cortices (high aldosterone
secretion, inhibit renin secretion)
manifestation: (Hypertension and weakness – most important)
o hypokalemia
o ECFV (slight) - (muscle weakness)
o Increase plasma Na+ concentration (very slight because
there are other hormones affecting Na)
o Hypertension – (increased ECF volume &
vasoconstriction)
o muscle weakness – due to hypokalemia METABOLIC EFFECTS
Carbohydrates Metabolism (Diabetogenic Effect)
GLUCOCORTICOIDS HYPERGLYCEMIC effect
Cortisol (aka hydrocortisone) – principal glucocorticoid stimulates gluconeogenesis from CHON (either proteins
(with mineralocorticoid activity) from the liver) - MAIN/PRIMARY effect
accounts for about 95% of all glucocorticoid activity decreases glucose utilization by cells because it has anti-
90 - 95% (protein bound), 10 -15% (free form) insulin effect (Prevents transport of glucose into the cell)
mainly to globulin (cortisol binding globulin or increases:
transcortin) and albumin glucose-6-phosphatase (used in glycogenolysis)
half-life – 60 to 90 minutes (greater % gluconeogenic enzymes
of protein binding = greater half-life) critical for the survival during fasting
destroyed mainly in the liver (bile/feces, 25%), “adrenal diabetes” and
mainly excreted in the urine (water soluble) insulin secretion (Hyperinsulinemia – Same with GH)
Corticosterone, Cortisone (synthetic), Prednisone
(synthetic) most common in the market, causes high Protein Metabolism (Catabolic/Antianabolic)
appetite = obesity, Methyl prednisone (synthetic) o ↑ protein catabolism and ↓ protein synthesis
preferred option w/ lesser side effect, Dexamethasone o facilitate conversion of protein to glucose
(synthetic) used as topical, long term corticosteroid. o ↓ proteins in the body except liver and plasma
o increases plasma and liver proteins (thus, all the
CORTISOL proteins in the body will decrease except in the blood
Principal glucocorticoid and liver because proteins broken down will be
increases blood glucose level transported to the liver for gluconeogenesis via the
has slight mineralocorticoid activity bloodstream)
helps to resist physical, mental and other types of
stresses. Fat Metabolism (Catabolic/Antianabolic)
essential for life (without it, you die!) o (+) lipolysis (growth hormone and epinephrine) -
Thyroid hormones are not essential for life however one will extremities
suffer from the deficiency. o (+) lipogenesis (central portion of the body)
o That is why truncal obesity is present
When some doctors run out of ideas in treating a patient, they
o (+) ketogenesis
administer steroids and the patient improves. Don’t do that Lol
TRANS BY: TEAM PAGE 8 OF 13
Permissive action Effects on Connective Tissue
o cortisol may amplify the effect of another hormone on a (-) collagen synthesis (thinning of the skin and walls of the
process that it does not affect directly. capillaries)
o potentiates and extends the action of glucagon, leads to intracutaneous hemorrhage
epinephrine and growth hormone (greater effect on these That is why when you have high levels of cortisol, you have
hormones) micro-hemorrhages, gum bleeding, massive stretch marks
o *All of these are not direct effects of cortisol. It has If you are using topical steroids, only apply thinly into your
permissive action. It can only amplify the effect of other skin
hormone’s processes.
*COMPARED with Growth Hormone: Similar with Carbohydrate Osteoporosis
effect, opposite with Protein effect, in fats, it depends. Most devastating effect
Summary feared and sometimes devastating complication of
Cortisol has; (when stimulated by stress) glucocorticoid therapy that last for more than a few
Diabetogenic Effect (gluconeogenesis and anti-insulin weeks.
effect) That is why you only give your steroids for 2 weeks, if
Lipolytic (extremities), Lipogenetic (central body not, you are prone to osteoporosis
region) and Ketogenic Effect preventive treatment with Ca++ and vitamin D and
Proteolytic Effect diphosphanates that inhibits bone reabsorption is
Effects on Muscle advisable.
maintains the contractility and work performance of
Effects on the Cardiovascular System
skeletal and cardiac muscle (↑ Ach synthesis (skeletal) and
required for the maintenance of normal blood pressure
↑ Na+K+ ATPase and β-adrenergic receptors (cardiac) -----
maintains CO by sustaining myocardial performance
normal level
arteriolar tone (permits normal responsiveness of the
Is it beneficial for athletics to take steroids? It improves
arterioles to AII, E and NE), that is why you facilitate
muscle performance both skeletal and cardiac ONLY IN
vasoconstriction
NORMAL LEVELS.
production of vasodilator prostaglandin
muscle mass and strength (↑ muscle catabolism and ↓
endothelial permeability (helps maintain the blood
muscle protein synthesis) cortisol excess
volume) (One anti-inflammatory effect)
long term excessive intake of cortisol will cause protein
breakdown. Muscles are mainly made up of proteins. Then
Effects on the Kidney
it will decrease muscle mass resulting to its weakness.
glomerular filtration rate by ↓ preglomerular (afferent
↓ slow oxidative type I : fast glycolytic type II-B muscle
arteriole) resistance and ↑ glomerular plasma flow
fiber ratio
↑ free water clearance (diuresis)
Effects on Bones
required for generation of NH3 (acid load) - buffer
-most devastating effect of cortisol is here
↑ Ca++ and PO4- excretion
bone formation (most profound effect)
Cortisol increases afferent arteriolar vasodilation
o ↓ formation of mature osteoblasts
Increase GFR ↑ urine
o ↑ apoptosis of osteoblasts and osteocytes
o ↓ collagen synthesis
bone resorption/destruction Effects on the CNS
o ↑ osteoclasts formation and mRNA of collagenase modulates emotional tone (excitability, behavior and
(enzyme that destroys the organic matrix of the bone) mood) and wakefulness. (Type I and II GRs are present in
Ca++ absorption in the GIT (antagonizes the effect of 1,25 various areas of the brain)- In normal level
(OH)2D3 and (-) its synthesis) in excess level, you either enhance the depression or
PTH production(PTH removes the calcium out of the bone) enhance the excitability. That’s why psychiatric disorders
In longer usage of steroids, you must have a prophylactic are present with very high steroids.
vitamin D and Calcium ↓ REM sleep and ↑ NREM and the time spent awake)
2 components of bones: Collagen (The “steel”) and Calcium & The patients suffer insomnia by decreasing the REM sleep.
Phosphates (The “cement”) – PROVIDES THE TENSILE ↓ the ability to detect salty taste
STRENGTH (+) appetite center (↑ neuropeptide Y)
Construction of bones – Osteoblasts It increases appetite especially on pregnisol not more on
Breakdown of Bones – Osteoclasts methyl pregnisolone. By increasing the orexogenic
Vitamin D increases the absorption of Calcium and substance, neuropeptide YY which increases appetite, thus
Phosphates in the GIT it stimulates the appetite center.
TRANS BY: TEAM PAGE 9 OF 13
insomnia, elevate or depress moods, decrease memory stabilizes lysosomal membrane.
function and lower the threshold for seizure activity decreases capillary permeability.
(psychiatric disorders) cortisol excess decreases migration of WBC and neutrophils and
INFANTILE SPASM- a type of seizure where patients are recruitment of leukocytes into the inflamed area and
given steroids because they increases the threshold for phagocytosis of damaged cells.
seizure activity by inflammation. ↓ phagocytic and bactericidal activity of neutrophils.
(-) differentiation and proliferation of mast cells
Effects on the Fetus ↓ proliferation of fibroblast (causes keloid) and their
The beneficial effect of steroids can be found on the fetus synthesis and deposition of fibrils.
because it facilitates the maturation of the CNS If you have a keloid former, you can apply steroid
facilitates maturation of the fetus (maturation of the CNS, because you decreases the proliferation of fibroblast.
retina, skin GIT and lungs - PRIMARILY) suppresses febrile response to infection
one of the common cause of death in premature individuals reduces the releases of interleukin-1
is respiratory distress because of low level of surfactant thromboxane, prostaglandin, leukotrienes, nitric oxide
then steroids will increase the surfactant. The respiratory and PAF
membrane is thin, if it is thick, diffusion of oxygen is low. causes resolution of inflammation
Steroids make it thinner. that is why you are given steroids during inflammation
↑ synthesis of surfactant, flattening of alveolar cells,
thinning of the lung septa and ↑ the rate of dev’t of the Inhibits immune responses
laveoli (last weeks of gestation) this is one of the substances that actually reset the set point,
causing fever
Effects on blood cells if you have antigen and macrophage, thus, increasing your
eosinophils, basophils and lymphocytes by increasing IL-1, temperature increases. Thermostat should lower it
apoptosis down by excessive sweating, hyperventilation by activating
Since eosinophils and basophils mediate allergy, the anterior hypothalamus. Parasympathetic is being
steroids have a powerful anti-allergic effect. It activated.
decreases lymphocytes by increasing their apoptosis, If body is too cold, posterior hypothalamus is activated, and
therefore it is an immunosuppressant. shivering will occur normalizing the temperature.
For patients who underwent transplant or autoimmune Sympathetic is activated.
disorder they are given steroids to lower their immune In fever, you increase this. With steroids these are being
system. That’s why they suffer from immunodeficiency. blocked.
Sometimes, patients with anemia or dengue are ↓ circulating T lymphocyte (T helper)
challenged with steroids to increase platelet. Take note ↓ migration to antigenic stimulation and function.
that though they are increased, it doesn’t mean they (transplant rejection)
have increased protective function. (-) differentiation of monocytes to macrophages
red blood cells, neutrophils and platelets influenced the proliferation, differentiation and
For neutrophils, only the number is increased but its production of antibodies by the B cells. (blocked by
function is increased. steroids by decreasing lymphocytes)
Inhibits inflammatory responses (↓ eosinophils)
↓ IL-1, IL-2 and IL-6 but ↑ IL-4 (↑ IgE)
-another beneficial effect of steroids
Phospholipase A that acts on arachidonic acid produces
CARDINAL SYMPTOMS OF INFLAMMATION:
cyclooxygenase. COX will then produce prostaglandins,
Rubor- redness caused by vasodilation. steroids increases
bradykinins, thromboxane which causes vasodilation. This
tone
cascade is blocked by steroids.
Tumor- swelling due to increase permeability. Fluid goes
Thus this is a very powerful for maturation of fetus and for anti-
to the interstitium. Steroid causes vasoconstriction, thus
inflammation.
decreases permeability,
Again, there is decreased lymphocytes, decreased migration.
Calor (heat) and Dolor (pain) caused by inflammatory
Thus, very much used in patients who had transplant to
substances due to migration of inflammatory cells which is
suppress the immune system and decrease the migration of
decreased by steroids.
antigenic stimulation in transplant patients.
Therefore, all the steps of inflammation are inhibited by
steroids
Check the pictures below
Mast cells increases the inflammatory mediators when
they degranulate. This is stabilized by steroids, decreasing
their granulation.
TRANS BY: TEAM PAGE 10 OF 13
Immunodeficiency
increases the susceptibility to bacterial, fungal and viral
infection and allow their dissemination.
Cortisol is important in resisting stresses;
trauma of almost any type
infection
intense heat or cold
injection of E and NE, necrotizing substances
surgery
debilitating diseases
physical stress ex. Exercise
SUMMARY
our body cope with these stresses with the help of steroids.
Connective Tissue: decrease collagen synthesis. In high level-
gum bleeding, micro hemorrhages, skin thinning causing
stiae formation, tensile strength of bone
On inflammation: decreases lymphocytes, migration, IL and
all the responses for inflammation. It also decreases capillary
permeability, stabilizes lysosomal enzymes, decreases
migration of inflammatory cells, decreases fibroblasts
proliferation.
On the heart: increases arteriolar tone, facilitating
vasoconstriction, inhibits production of vasodilators which
increases cardiac performance. Thus, maintain cardiac
function and arterial blood pressure.
Fetus: maturation of CNS, retina, GIT, skin, primary in the
lungs concomitantly increasing the surfactant.
Kidney: diuresis, increases water clearance due to increase
GFR, increase renal blood flow because of afferent arteriolar
dilatation
It modulates emotional tone. Either elevate or decreased
Sleep duration decreased (↑ NREM ↓REM)
Appetite increase
On muscle: maintains performance, but since it has protein it
can facilitate protein weakness
Bone: decrease bone formation, increase bone resorption,
inhibit action of vit D, enhance action of PTH
TRANS BY: TEAM PAGE 11 OF 13
Hyperadrenalism (Cushing’s Syndrome) Hypoadrenalism (Addison’s Disease)
Cushing’s Syndrome: problem is anywhere in the body except due to atrophy of the adrenal cortex (autoimmunity),
pituitary. tuberculous destruction and cancer invasion of the adrenal
Cushing’s Disease: If it has something to do with functional cortex.
pituitary adenoma *tuberculous bacilli don’t only affect your lungs, it can also
*If you have the signs of cushing’s, we just call that cushing’s affect extrapulmonary structure like adrenal cortex.
syndrome, but if you can already pin point the problem, you call Because of these reasons, both glucocorticoid and
the cushing’s disease. mineralocorticoid levels are decreased.
characterized by;
Primary Hyperadrenalism Inability to maintain normal blood glucose level
Due to adrenal hypercortisolism (excessive secretion of Protohypoglycemia, but not necessarily
cortisol). hypoglycemia- because you still have glucagon,
Most commonly due to excessive intake of steroids. It can epinephrine, and norepinephrine. However, their
also be due to function is not amplified.
exogenous corticosteroids Inability to cope up stress
ACTH secreting tumor ( ACTH, Cortisol), Depression of most metabolic functions of the body
functional adrenal tumor in the adrenal medulla Skin hyperpigmentation (occurs in Secondary
functional pituitary adenoma which is called the Hypercoticolism and Primary hypocorticolism)
cushing’s disease. Due to ACTH level that binds with
caused by adrenal cortex adenoma, bilateral adrenal cortex melanocortex 1 receptor
hyperplasia and administration of large amount of cortisol Hypotension (due to mineralocorticoid activity)
PRIMARY: problem in adrenal cortex ( Cortisol, ACTH) ECF volume shock (due to mineralocorticoid
SECONDARY: problem in pituitary or hypothalamus ( activity)
ACTH, Cortisol) hyponatremia
manifested by; hyperkalemia
Buffalo hump hypertension (Lipogenesis at the mild acidosis
central) Decreased total peripheral resistance- cortisol
Moon face (Lipogenesis at the central) increases arteriolar tone and decreases
hypernatremia (Light mineralocorticoid activity) vasodilatation
Truncal obesity (Lipogenesis at the central) Weight loss due to decrease appetite and GI function
hypokalemia (Light mineralocorticoid activity) Water intoxication- water moves intracellularly. If
Purplish striae (collagen inhibition) you do not have cortisol water stays inside the cells.
mild alkalosis (slight mineralocorticoid activity) Muscle weakness- cortisol improves muscle
Weakness (mainly due to protein breakdown, slightly performance. if you have hypo and hyper cortisol,
by hypokalemia and mineralocorticoid activity) this manifest.
vertebral fractures (due to osteoporosis) Anemia- due to its effect on RBC
Osteoporosis Decrease GIT motility and secretion because they are
easy bruisability (collagen breakdown) sometimes promoted by cortisol.
Diabetes (hyperglycemic) There will be no excitement here unlike in
psychiatric disorders (effect on mood and behavior of hypercorticosolism. For hypocortisolism, there is
patient) depression.
immunodeficiency
Secondary Hypercorticolism
cortisol→→→ ACTH
pituitary adenoma
abnormal function of hypothalamus
ectopic secretion of ACTH
*To differentiate primary to secondary based on PE, skin
hyperpigmentation occurs with secondary because of ACTH.
TRANS BY: TEAM PAGE 12 OF 13
ANDROGENS
Secreted by zona reticularis
Dehydroepeandrosterone (DHEA) and androstenedione
- principal cortical androgens (in the peripheral circulation,
they should be converted to testosterone or estrogen
responsible for the early development of male sex
organs.
converted to testosterone (potent)
“masculinizing effect”
What will happen if there is androgen deficiency? This
will not be manifested by females and males. For males,
testis is still present to compensate.
Excess androgen is more common for females.
also secrete estrogen (estradiol) and progesterone
Androgenital Syndrome
AKA Virilism/hirsutism/female pseudohermaphroditism
Only in females!
develops intense musculinizing effects throughout the body
(virilism)
Growth of beard
Deeper voice
Baldness (baldness means excessive testosterone)
Musculine hair distribution
Growth of clitoris
Loss of regular of menses Regression of breast tissue
(excessive testosterone will decrease your GnRH.
Without GnRH no LH surge, loss of regular menses)
Additional:
* Excessive Stress – you are prone to infection (because of
immunosuppression)
* If you will be given high dose of steroids continuously and you
abruptly stop it, you will die.
Why? Because the high level of steroids will give negative
feedback to your hypothalamus, causing low CRH and low ACTH
cause the atrophy of the adrenal cortex.
*If there is abrupt cessation of intake, you cannot produce
cortisol (which is essential to life) because your cortex is still
atrophied.
*There should be gradual cessation of intake in dosage and in
duration (slightly increasing CRH, ACTH reviving your adrenal
cortex)
TRANS BY: TEAM PAGE 13 OF 13
Você também pode gostar
- ABS Endocrinology PDFDocumento59 páginasABS Endocrinology PDFMichael Olivier WAinda não há avaliações
- Adrenocortical Hormones: Learning ObjectivesDocumento3 páginasAdrenocortical Hormones: Learning ObjectivesMarlin Berliannanda TawayAinda não há avaliações
- Endocrine Pathophysiology Nursing NotesDocumento4 páginasEndocrine Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- Week 11. Endocrinology 3Documento17 páginasWeek 11. Endocrinology 3MACOB, ETHELHYN JHANEAinda não há avaliações
- Adrenal Glands Clinical Chemistry (Laboratory) : Lesson 7Documento5 páginasAdrenal Glands Clinical Chemistry (Laboratory) : Lesson 7Cherry Ann ColechaAinda não há avaliações
- AP 18 Endocrine OverviewDocumento19 páginasAP 18 Endocrine OverviewMARICRIS NEBIARAinda não há avaliações
- Adrnl StressDocumento43 páginasAdrnl StressPraveen ChowdharyAinda não há avaliações
- Functional Anatomy of The Adrenal GlandDocumento9 páginasFunctional Anatomy of The Adrenal GlandPaula SchaeferAinda não há avaliações
- Adrenal Gland: Dr. Fatimah Eliana, SPPD, KemdDocumento46 páginasAdrenal Gland: Dr. Fatimah Eliana, SPPD, KemdZahra AstriantaniAinda não há avaliações
- 1 Adrenal CortexDocumento15 páginas1 Adrenal CortexMarion Lawrence LaraAinda não há avaliações
- Adrenal GlandDocumento2 páginasAdrenal GlandAurelia AlexandraAinda não há avaliações
- Adrenal Gland - GlucocorticoidsDocumento16 páginasAdrenal Gland - GlucocorticoidsDongs McClureAinda não há avaliações
- Pharma NewestDocumento131 páginasPharma NewestPaolo Montańa EzparasAinda não há avaliações
- 17 Adrenal GlandDocumento33 páginas17 Adrenal GlandPande Indra PremanaAinda não há avaliações
- Endo 3 Notes PDFDocumento9 páginasEndo 3 Notes PDFDilAinda não há avaliações
- Adrenal Gland (Basic)Documento2 páginasAdrenal Gland (Basic)Nikhat GarimaAinda não há avaliações
- Study of The Endocrine SystemDocumento225 páginasStudy of The Endocrine SystemHuzaifa RashidAinda não há avaliações
- 3 - Steroid and Gonadal DrugsDocumento21 páginas3 - Steroid and Gonadal DrugsSoc Gerren TuasonAinda não há avaliações
- Summary & Mcqs of Adrenal Gland: Done byDocumento7 páginasSummary & Mcqs of Adrenal Gland: Done byHabib Ullah100% (1)
- ADRENALSDocumento60 páginasADRENALSJyoti ChadhaAinda não há avaliações
- The Adrenal GlandDocumento13 páginasThe Adrenal GlandardevanaAinda não há avaliações
- Chem+Path +adrenal+2021 H+VreedeDocumento39 páginasChem+Path +adrenal+2021 H+VreedeKamogelo AlbertAinda não há avaliações
- 1 - Biokimia ReproduksiDocumento56 páginas1 - Biokimia ReproduksiTarissa Kartika EdwinAinda não há avaliações
- 1 - Endocrine 1 (Introduction) - MedicineDocumento36 páginas1 - Endocrine 1 (Introduction) - MedicineBHUWAN BASKOTAAinda não há avaliações
- Endocrine Notes - All in One FileDocumento182 páginasEndocrine Notes - All in One FilekjAinda não há avaliações
- What Is A Hormone?: HormonesDocumento89 páginasWhat Is A Hormone?: HormonesMarkus van der WesthuizenAinda não há avaliações
- The Endocrine System Consists of Hormones Secreted by Glands Traveling Through The Blood To Target TissuesDocumento16 páginasThe Endocrine System Consists of Hormones Secreted by Glands Traveling Through The Blood To Target TissuesAljon AniesAinda não há avaliações
- Learning JournalDocumento82 páginasLearning JournalAnnapurna RavelAinda não há avaliações
- Phys 8Documento39 páginasPhys 8sakwork30Ainda não há avaliações
- Anfis Endokrin Idk-1 ElsDocumento60 páginasAnfis Endokrin Idk-1 ElsAuliya ArahmanAinda não há avaliações
- A&p - All Files in One PDFDocumento52 páginasA&p - All Files in One PDFSreejith Jagal KishoreAinda não há avaliações
- General Biology Lesson 13Documento13 páginasGeneral Biology Lesson 13GUCOR, LOVELY SHANE C.Ainda não há avaliações
- Chapter 34 - Introduction To The Endocrine SystemDocumento3 páginasChapter 34 - Introduction To The Endocrine Systemkdayeon018Ainda não há avaliações
- Adrenal GlandDocumento49 páginasAdrenal GlandRaphael AnajeAinda não há avaliações
- Chapter 6 The Endocrine SystemDocumento37 páginasChapter 6 The Endocrine SystemReikooAinda não há avaliações
- Endocrinology IntroductionDocumento43 páginasEndocrinology IntroductionDICKSONAinda não há avaliações
- Endocrine System: EndocrinologyDocumento10 páginasEndocrine System: EndocrinologyAnya IgnacioAinda não há avaliações
- Lecture 15 - Adrenal Gland BNS KUMDocumento17 páginasLecture 15 - Adrenal Gland BNS KUMabdulsaboor30Ainda não há avaliações
- Endocrinology Course OutllokDocumento59 páginasEndocrinology Course OutllokJeff ParkAinda não há avaliações
- Endocrine System-1Documento90 páginasEndocrine System-1markmuiruri581Ainda não há avaliações
- 19 SYNTHESIS OF ADRENALINEADRENERGIC RECEPTORS by COL AZMAT ALIDocumento53 páginas19 SYNTHESIS OF ADRENALINEADRENERGIC RECEPTORS by COL AZMAT ALIAhmed YTAinda não há avaliações
- Endocrine System HandoutsDocumento9 páginasEndocrine System HandoutsJosh ViñalonAinda não há avaliações
- Human Anatomy & Physiology: Autonomic Nervous SystemDocumento8 páginasHuman Anatomy & Physiology: Autonomic Nervous SystemBeth EchavezAinda não há avaliações
- Endocrine System: THE Adrenal GlandsDocumento50 páginasEndocrine System: THE Adrenal GlandsAbdel Aziz NazihAinda não há avaliações
- HormonesDocumento55 páginasHormonesAvinashAinda não há avaliações
- Regulasi Dan Mekanisme EndokrinDocumento121 páginasRegulasi Dan Mekanisme Endokrinluthfiyya syafiqaAinda não há avaliações
- Introduction To ANS PharmacologyDocumento34 páginasIntroduction To ANS PharmacologySebontu HasenAinda não há avaliações
- Adrenal Gland by DR Rajnee Ist PartDocumento29 páginasAdrenal Gland by DR Rajnee Ist Part9460106212Ainda não há avaliações
- Endocrine SystemDocumento4 páginasEndocrine Systemden mAinda não há avaliações
- Screenshot 2023-04-26 at 12.52.44 PMDocumento1 páginaScreenshot 2023-04-26 at 12.52.44 PMRenadAinda não há avaliações
- LEC 01 - Principles of EndocrinologyDocumento44 páginasLEC 01 - Principles of EndocrinologyIoana Cozma100% (1)
- Introduction To Autonomic PharmacologyDocumento44 páginasIntroduction To Autonomic PharmacologyZemburukaAinda não há avaliações
- Endo Adrenal ElhDocumento26 páginasEndo Adrenal Elhodiodi57Ainda não há avaliações
- Endocrine System of FishesDocumento5 páginasEndocrine System of FishesmonjitpaulAinda não há avaliações
- ENDOCRINE SYSTEM SCRIPT and Outlines ChurmeheDocumento13 páginasENDOCRINE SYSTEM SCRIPT and Outlines ChurmeheMIKAEL PATRICK DEIPARINEAinda não há avaliações
- CUSHINGSDocumento205 páginasCUSHINGSDaroo D.TAinda não há avaliações
- Adrenal Function: T. Creighton Mitchell, A. Wayne MeikleDocumento19 páginasAdrenal Function: T. Creighton Mitchell, A. Wayne MeikleWho KnowsAinda não há avaliações
- MD2 Pathology May 2018Documento13 páginasMD2 Pathology May 2018vicbart11Ainda não há avaliações
- Blood SupplyDocumento2 páginasBlood Supplyvicbart11Ainda não há avaliações
- Physiology Feedback: Finals Sem1 Ay 2017-2018: D. Both A & B (Phospagen andDocumento4 páginasPhysiology Feedback: Finals Sem1 Ay 2017-2018: D. Both A & B (Phospagen andvicbart11Ainda não há avaliações
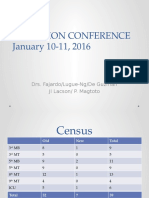
- Auf Im Adcon Jan1016-1Documento41 páginasAuf Im Adcon Jan1016-1vicbart11Ainda não há avaliações
- Physicochemical IncompatibilitiesDocumento20 páginasPhysicochemical Incompatibilitiesvicbart11Ainda não há avaliações
- GSJGFJ SPDocumento11 páginasGSJGFJ SPvicbart11Ainda não há avaliações
- Lectgiugdfiugsdsdkjasjure 9Documento9 páginasLectgiugdfiugsdsdkjasjure 9vicbart11Ainda não há avaliações
- Particle Size and Surface Area Are Important Parameters in The Development of A DrugDocumento8 páginasParticle Size and Surface Area Are Important Parameters in The Development of A Drugvicbart11Ainda não há avaliações
- Storage PolysaccharidesDocumento8 páginasStorage Polysaccharidesvicbart11Ainda não há avaliações
- WATER Is The Solvent of Choice For BiologicalDocumento15 páginasWATER Is The Solvent of Choice For Biologicalvicbart11Ainda não há avaliações
- Angeles University Foundation Angeles University Foundation: Number of Hours Number of HoursDocumento1 páginaAngeles University Foundation Angeles University Foundation: Number of Hours Number of Hoursvicbart11Ainda não há avaliações
- Retail Banking Black BookDocumento95 páginasRetail Banking Black Bookomprakash shindeAinda não há avaliações
- 5066452Documento53 páginas5066452jlcheefei9258Ainda não há avaliações
- Specifications (018-001) : WarningDocumento6 páginasSpecifications (018-001) : WarningRómulo Simón Lizarraga LeónAinda não há avaliações
- Analytical Chem Lab #3Documento4 páginasAnalytical Chem Lab #3kent galangAinda não há avaliações
- Kosher Leche Descremada Dairy America Usa Planta TiptonDocumento2 páginasKosher Leche Descremada Dairy America Usa Planta Tiptontania SaezAinda não há avaliações
- VMP 930 Veterinary Parasitology: Paragonimus KellicottiDocumento63 páginasVMP 930 Veterinary Parasitology: Paragonimus KellicottiRenien Khim BahayaAinda não há avaliações
- A Review of Service Quality ModelsDocumento8 páginasA Review of Service Quality ModelsJimmiJini100% (1)
- Cyclic MeditationDocumento8 páginasCyclic MeditationSatadal GuptaAinda não há avaliações
- HRMDocumento118 páginasHRMKarthic KasiliaAinda não há avaliações
- Battery Guide - 2021Documento27 páginasBattery Guide - 2021Mario LaurieAinda não há avaliações
- To Find Fatty Material of Different Soap SamplesDocumento17 páginasTo Find Fatty Material of Different Soap SamplesRohan Singh0% (2)
- Maritime Academy of Asia and The Pacific-Kamaya Point Department of AcademicsDocumento7 páginasMaritime Academy of Asia and The Pacific-Kamaya Point Department of Academicsaki sintaAinda não há avaliações
- Prospekt Puk U5 en Mail 1185Documento8 páginasProspekt Puk U5 en Mail 1185sakthivelAinda não há avaliações
- Komunikasi Sebagai Piranti Kebijakan Bi: Materi SESMABI Mei 2020Documento26 páginasKomunikasi Sebagai Piranti Kebijakan Bi: Materi SESMABI Mei 2020syahriniAinda não há avaliações
- COURTESY Reception Good MannersDocumento1 páginaCOURTESY Reception Good MannersGulzina ZhumashevaAinda não há avaliações
- Ilocos Norte Youth Development Office Accomplishment Report 2Documento17 páginasIlocos Norte Youth Development Office Accomplishment Report 2Solsona Natl HS MaanantengAinda não há avaliações
- Seabank Statement 20220726Documento4 páginasSeabank Statement 20220726Alesa WahabappAinda não há avaliações
- Question Answers of Chapter 13 Class 5Documento6 páginasQuestion Answers of Chapter 13 Class 5SuvashreePradhanAinda não há avaliações
- Babe Ruth Saves BaseballDocumento49 páginasBabe Ruth Saves BaseballYijun PengAinda não há avaliações
- Please Refer Tender Document and Annexures For More DetailsDocumento1 páginaPlease Refer Tender Document and Annexures For More DetailsNAYANMANI NAMASUDRAAinda não há avaliações
- Mozal Finance EXCEL Group 15dec2013Documento15 páginasMozal Finance EXCEL Group 15dec2013Abhijit TailangAinda não há avaliações
- Mathematics BQP 2022Documento43 páginasMathematics BQP 2022muhammadmansuri815Ainda não há avaliações
- Pulmonary EmbolismDocumento48 páginasPulmonary Embolismganga2424100% (3)
- BackgroundsDocumento13 páginasBackgroundsRaMinah100% (8)
- Asterisk NowDocumento82 páginasAsterisk Nowkambojk100% (1)
- Instant Download Ebook PDF Ecology Concepts and Applications 8th Edition PDF ScribdDocumento41 páginasInstant Download Ebook PDF Ecology Concepts and Applications 8th Edition PDF Scribdsteven.cross256100% (45)
- Facebook: Daisy BuchananDocumento5 páginasFacebook: Daisy BuchananbelenrichardiAinda não há avaliações
- Intelligent DesignDocumento21 páginasIntelligent DesignDan W ReynoldsAinda não há avaliações
- BIAN How To Guide Developing Content V7.0 Final V1.0 PDFDocumento72 páginasBIAN How To Guide Developing Content V7.0 Final V1.0 PDFميلاد نوروزي رهبرAinda não há avaliações
- A Medium-Rise Residential Building: A B C E D F G HDocumento3 páginasA Medium-Rise Residential Building: A B C E D F G HBabyjhaneTanItmanAinda não há avaliações