Escolar Documentos
Profissional Documentos
Cultura Documentos
Bioactive Glasses in Dentistry: A Review: Abbasi Z, Bahrololoom ME, Shariat MH, Bagheri R
Enviado por
Rajesh PuniaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Bioactive Glasses in Dentistry: A Review: Abbasi Z, Bahrololoom ME, Shariat MH, Bagheri R
Enviado por
Rajesh PuniaDireitos autorais:
Formatos disponíveis
Abbasi Z et al.
Journal of Dental Biomaterials. 2015;2(1)
Bioactive Glasses in Dentistry: A Review
a a a b
Abbasi Z , Bahrololoom ME , Shariat MH , Bagheri R
a. Department of Materials Science and Engineering, School of Engineering, Shiraz University, Shiraz, Iran
b. Department of Dental Materials and Biomaterial Research center, Shiraz University of Medical Sciences, Shiraz,
Iran
ARTICLE INFO Abstract
Article History Bioactive glasses are silicate-based and can form a strong chemical
Received: 2 October 2014 bond with the tissues. These biomaterials are highly biocompatible
Accepted: 2 January 2015 and can form a hydroxyapatite layer when implanted in the body or
soaked in the simulated body fluid. Due to several disadvantages,
Key words: conventional glass processing method including melting of glass
Bioglass components, is replaced by sol-gel method with a large number of
Hydroxyapatite benefits such as low processing temperature, higher purity and ho-
Sol-gel derived mogeneity and therefore better control of bioactivity. Bioactive
glasses have a wide range of applications, particularly in dentistry.
Corresponding Author: These glasses can be used as particulates or monolithic shapes and
Rafat Bagheri porous or dense constructs in different applications such as
Department of Dental Materials remineralization or hypersensitivity treatment. Some properties of
and Biomaterial Research cen- bioactive glasses such as antibacterial properties can be promoted by
ter, Shiraz University of Medi- adding different elements into the glass. Bioactive glasses can also
cal Sciences, Shiraz, Iran be used to modify different biocompatible materials that need to be
Tel: +98-71-36280119 bioactive. This study reviews the significant developments of bioac-
Fax : +98-71-36285276 tive glasses in clinical application, especially dentistry. Furthermore,
Email : bagherir@sums.ac.ir we will discuss the field of bioactive glasses from beginning to the
current developments, which includes processing methods, applica-
tions, and properties of these glasses.
Cite this article as: Abbasi Z, Bahrololoom ME, Shariat MH, Bagheri R. Bioactive Glasses in Dentistry: A Review. J Dent
Biomater, 2015;2(1):1-9.
1. Introduction of bioactive glass bioactivity increases with the amount of CaO in the
Bioactive glasses are a group of biomaterials which composition, because the dissolution of the calcium
are used in the fields of dentistry and orthopedics. ion from the glass plays an important role in formation
Forty five years ago, these glasses modified the func- of the chemical bond [5].
tions and capabilities of biomaterials from bioinert to Results of in vivo implantation of bioactive glasses
bioactive by stimulating a strong response after im- show that these materials produce no toxicity, no in-
planting in the human body (e.g. osteoproductivity) flammation, and no foreign-body response [6]. In fact,
[1]. A material can be classified as bioactive if the these glasses bond with the bone through formation of
above-mentioned biological response results in for- a hydroxyapatite (HAp) layer. The same HAp layer is
mation of a strong chemical bond between the im- formed on the surfaces of these materials after soaking
planted material and a soft or hard tissue [2]. Certain in the simulated body fluid (SBF) which has ion con-
compositions of the silicate-based glasses, with calci- centrations similar to the human blood plasma [7].
um and phosphorus in proportions identical to those of Hench at the University of Florida introduced the
natural bone, can form such a strong bond without an first bioactive glass in 1969 [3]. Those days, the avail-
intervening fibrous layer [3]. When the glass contains able implant materials (metals and polymers) designed
more than 60% SiO2, bonding to tissues is no longer to be bioinert had a problem; they initiated fibrous
observed [4]. On the other hand, it is expected that encapsulation after implantation, rather than forming a
Jdb.sums.ac.ir J Dent Biomater 2015; 2(1) 1
Bioactive Glasses in Dentistry: A Review
2 Jdb.sums.ac.ir J Dent Biomater 2015; 2(1)
Abbasi Z et al.
stable bond with the tissues. Hench began his work to In 1980, Hench showed that the in vivo formation
overcome this problem by finding a material that of the HAp layer can be reproduced in Tris buffer
could bond to the bone and survive the harsh envi- solution at pH 7.4. Later, Kokubo and Hench
ronment of the human body. He tried making a de- independently confirmed that apatite can form on the
gradable glass in the Na2O-CaO-SiO2-P2O5 system ®
surface of Bioglass in SBF. In 1991, it was suggested
with high calcium content [3]. He discovered such that a sim- ulated body fluid (SBF) which has the ion
glass with the composition of 46.1 mol.% SiO2, 24.4 concentra- tions equal to human blood plasma can
mol.% Na2O, 26.9 mol.% CaO and 2.6 mol.% P2O5 reproduce HAp formation [3]. Thin film X-ray
®
(later termed 45S5 and Bioglass ) which formed a diffraction (TF-XRD), Fourier transform infrared
bond with the bone so tightly that it could not be re- spectroscopy (FTIR), scan- ning electron microscopy
moved without breaking the bone. In fact, this glass (SEM) and transmission elec- tron microscopy (TEM)
bonds with bone rapidly and stimulates bone growth were used to confirm the simi-
away from the bone-implant interface. This bone larity of the composition and structure of HAp formed
bonding is the result of HAp layer formation on the in SBF to the bone mineral [12]. Hence, immersion in
surface of the glass, following initial glass dissolution SBF can be used for in vivo bone bioactivity prediction
[2]. This discovery was the introduction of the field of before animal testing; this reduces the number of ani-
bioactive ceramics and the beginning of the formation mals used and the duration of experiments and, there-
of many new materials such as synthetic hydroxyap- fore, increases the possibility of the development of
atite (HAp) and other calcium phosphates [8]. All new types of bioactive materials [3].
glasses, glass-ceramics and ceramics that are used as SBF is a solution that simulates human blood
implant materials are called “bioceramics” but plasma with ion compositions similar to human blood,
®
“Bioglass ” is referred to as the original 45S5 compo- but without any proteins, hormones, glucose, or vita-
sition and should not be used as a general term for mins [13]. During immersion in SBF, different pro-
bioactive glasses [9]. Table 1 presents the composi- cesses occur simultaneously which result in structural
tions of the bioactive glasses mentioned in this review. and chemical changes to the surface of the material.
These processes are leaching, degradation, and precip-
Table 1: Compositions of three types of bioactive glass- itation [14]. In the leaching process, through the ex-
es. + +
change of the cations H and H3O , metal ions like
Name Composition + 2+
Na and Ca are released and the pH at the interface
46.1 mol.% SiO2, 24.4 mol.% Na2O, 26.9
45S5 (Bioglass®) mol.% CaO and 2.6 mol.% P2O5 increases up to 7.4. In parallel, hydroxyl ions locally
break the silica-oxygen bonding. Then, silicon as silic-
58S (Sol-gel 60 mol.% SiO2, 36 mol.% CaO and 4 mol.% ic acid, Si(OH)4, is released into the solution. The hy-
derived) P2O5 drated silicic acid on the surface is surrounded by at
S53P4
53 mol.% SiO2, 23 mol.% Na2O, 20 mol.%
CaO and 4 mol.% P2O5
least one hydroxy group; subsequently, a silicic acid
gel layer forms. Simultaneously, the glass releases
calcium and phosphorus and an amorphous calcium
2. The mechanism of HAp layer formation on bio- phosphate-rich phase is formed on the surface. The
active glasses CaP phase then crystallizes into a hydroxyapatite
Hydroxyapatite is similar to the bone mineral and can (HAp) structure [14].
interact with collagen fibrils of damaged bone to bond
with it. Protein adsorption, incorporation of collagen 3. Processing methods
fibrils, attachment of bone progenitor cells, cell differ- For years, conventional glass technology has been
entiation, the excretion of bone extracellular matrix used to produce bioactive glasses. Mixture of oxides
and its mineralization are involved in the formation of or carbonates grains, as the glass components, are
HAp layer-bone bond. Osteogenesis, due to the disso- melted in a platinum crucible and homogenized at
lution products of the glass on osteoprogenitor cells, high temperatures up to 1250-1400°C. Then, to pro-
stimulates new bone growth [10]. duce a bulk implant, the molten glass is cast into steel
The mechanism of HAp layer formation on bioac- or graphite mold. For the required tolerance, a final
tive glasses has been widely studied in vitro and in grind and polish is often necessary. Sometimes, bioac-
vivo. This process involves different stages; calcium tive glass powders are required for some clinical ap-
ions dissolve from the bioactive glass into the body plications such as treatment of periodontal lesions. In
fluid while a silica-rich interlayer forms on the glass conventional glass technology, the molten glass is
surfaces. The nucleation of HAp is now possible be- poured into water or other liquid medium to produce
cause the surrounding fluid is supersaturated with re- small fragments. To achieve powders with specific
spect to HAp due to the dissolution of the calcium size ranges for periodontal treatment, subsequent
ions. In addition, silica-rich interlayer dissolves a con- grinding is necessary [4].
siderable amount of silicate ion and provides favorable Producing bioactive glasses by conventional glass
sites for the nucleation. The process of nucleation and technology has several disadvantages as listed below
growth of the HAp layer continues by the reactions of (A-D). A: Very high purity is necessary for optimal
the calcium, phosphate, and hydroxide ions. It is pos- bioactivity which is difficult to maintain in this meth-
sible that carbonate or fluoride anions incorporate in od due to the high temperatures of processing, the low
the reactions, as well [3,9,11].
Jdb.sums.ac.ir J Dent Biomater 2015; 2(1) 3
silica and high alkali conventional glass more rapid. The tive glass has been
content of the processing, which recognition that the conducted through sol-
traditional bioac- tive considerably reduces high surface-area is gel method [21]. Sol-
glass compositions. the costs due to favorable for the gel method allows the
Such glasses are very lowering the formation of the HAp production of other
reactive and can processing layer bonding led to glass ceramics such as
dissolve platinum and temperatures [4]. This application of the sol- SiO2–CaO–P2O5,
take other multiple process has be- come gel process to create SiO2–P2O5– Al2O3–
cat- ions as an attractive research bioactive glasses [5]. CaO–Na2O–K2O [22].
impurities [4]. Gross field during 1980s A ternary bioactive On the surface of these
and Strunz [15] have [18]. Mixing the metal glass with a starting glasses, the formation
shown that M , M ,
3+ 4+
alkoxides in the surface area greater and the rapid increase
2
and M
5+
impurity solution to synthe- size than 150 m /g was of the thickness of
cations in bio- active an inorganic network, produced by Li et al., HAp layer were
glasses have hydrolysis, gelation, [4] and used for bone observed as a result of
considerable effects on and low-temperature graft applications. contact with Tris
tissue bonding. firing are the steps for Greenspan et al. [20] buffer and simulated
Greenspan and producing a sol-gel demonstrated that body fluid (SBF). This
Hench [16] have derived glass [19]. bioactive glasses with is an indication of the
revealed how bone surface areas greater high bioactivity of the
The microscopic 2
bonding is sensitive to structure of such glass than 50 m /g could gel-derived glasses
3+
a small amount of A1 can be modified by bond to the bone and [23].
in bioactive glasses. controlling monomer soft tissue within 24 h Difficulty to obtain
Evaporation of P2O5 at precursor, reaction of in vitro experiment. crack-free bioactive
high temperatures temperatures, water to Production of a glass monoliths,
may also result in two (CaO and SiO2), greater than 1 cm in
alkoxide ratio, and
composition uncer- three (SiO2– CaO– diameter, is the disad-
catalyst [5]. In sol-gel
tainty in the P2O5 , SiO2–CaO– vantage of sol–gel
process, many disad-
conventional method Na2O , P2O5–CaO– synthesis. The large
vantages of
[17]. B: Bioactive Na2O) or even four shrinkage dur- ing
conventional method
powders are exposed (SiO2–CaO–P2O5– drying stage and the
can be eliminated and
to contaminants during Ag2O) component evaporation of the
the purity which is
the con- ventional bioac- liquid by- products are
resulted from
glass processing which two reasons of the
processing at low
exerts negative ef- cracking. The vapor
temperatures (600-
fects on bioactivity. must pass through the
C: Conventional 700ºC) can be
controlled. The interconnected pore
method imposes a network from inside to
compositional advantages of this
method include ease of the surface, which can
limitation on bioactive create capillary
glasses; this is because powder production, a
broader range and a stresses and, therefore,
of very high liquidus
better control of cracking. For powders,
temperature of SiO2
bioactivity, high these stresses are small
and very high viscosity
homogeneity, good because the path of
of silicate melts with
control of parti- cles evaporation is short
high SiO2 content. D:
size and morphology and the material can
The increased
and the easy accommodate the
production costs of
preparation of thin stresses. For
this method is
considerable which is films and coatings monoliths, the path
due to high- [4,5]. from the center to the
temperature The sol-gel derived surface is long and
processing in platinum bioactive glass has a twisty, and the drying
crucibles, multiple porous structure which stresses can lead to
handling steps, capital increases its specific fracture. Narrow
equipment, labor, surface area by two distribution pores
maintenance, quality orders of magnitude with increasing size
assurance, and quality compared to a melt- can reduce this
control [4]. derived glass of a problem [9].
Low-temperature similar composition.
sol-gel processing Therefore, the rate of 4. The
offers a favor- able the surface of HAp applic
alternative to formation for the sol- ations
gel based materials is
of be discussed. Table 2,
bioacti presents these products
ve and some of their
glass applications.
In 1986, a bioactive
glass was successfully * Medical Devices
used as middle ear with Monolithic
prosthesis to repair shape
conductive hearing In 1988, a simple
®,
loss cone of Bioglass
and it was the first termed the
clinical application of Endosseous Ridge
such materi- Maintenance Implant
®
al. In tooth (ERMI ), was the
®
extraction, bioactive commercial Bioglass
glasses have been device in dentistry. To
used to preserve the repair the tooth roots
height of the alveolar and to provide a stable
ridge [24]. Bioactive ridge for dentures,
glasses also have been such devices were
used for spinal fu- inserted into fresh
sion, reconstruction of tooth
the iliac crest extraction sites. They
following autograft were highly stable
harvesting, and for and much
filling bony defects in better than HAp tooth
a number of root implants.
orthopedic procedures. However, this product
These early clinical did not gain
applications confirmed commercial success
the benefits of this because sur- geons
material as highly prefer to be able to cut
compatible implants the implant to shape
[25]. More recent rather than be limited
applica- tion of to cones of fixed size.
bioactive glasses
include coatings for
orthope- dic metallic
implants, trabecular
coatings, bone re-
placement,
periodontology,
endodontology,
scaffolds for bone
tissue engineering,
regenerative
medicine, and
composite based
scaffolds [26,27].
Different forms of
bioactive glasses
including par- ticles,
porous scaffolds, or
dense constructs have
been used in clinical
applications, such as
dentistry [9]. In
the following section,
some applications and
products of the
®
original Bioglass , as
the first introduced
bioac- tive glass, will
Figure 1. SEM micrographs of human dentine (bar = 1 µm): (a) untreated, (b) immediately after application of NovaMin® in artifi-
®
cial saliva (AS); (c) 24 h after application of NovaMin in AS; (d) 5 days after application. SEM images are adapted from Earl et
al. [39].
Internationally, 3i, Palm Beach cyclic loading fatigue attach to the dentine.
products based on Gardens, Florida) and of the thin enamel near For in vitro trials,
® human dentine is
particles rather than BonAlive (BonAlive the cemento-enamel
monolithic shapes are Biomaterials, Turku, junction [35]. The lightly etched to reveal
in commercial use Finland) [9,34]. hydrodynamic theory the tubules. Figure 1-b
[24]. *Using Bioactive about DH mechanism shows the den- tine
* Particulates of Glass for Treatment of proposes that when ex- immediately after the
Bioactive Glass Hyper- sensitivity ternal stimuli such as application of
®
Surgeons and A very fine cold, hot, tactile or NovaMin . After 24 h,
®
dentists often prefer to Bioglass osmotic pres- sure are the particles are
use particles or particulate called applied to the exposed attached to the dentine
® and HAp layer covers
granules instead of NovaMin dentin, they cause
monoliths, as they (NovaMin fluid movement within the surface. This
®
can press them easily Technology, the dentinal tubules. shows that NovaMin
to fill a defect. In GlaxoSmithKline, These open tubules stimulates the
®
1993, Perio-Glas Florida, UK), with a allow the fluid to flow deposition of calcium
(NovaBone Products particle size of ~18 through the tubules, phos- phate over the
LLC, Alachua, µm is used as an ac- which may result in dentine tubules. In
Florida) as the first tive repair agent in pressure changes that fact, the glass disso-
particulate bioactive toothpaste. This excite the nerve lution products
glass with the particle material mineral- endings in the dental stimulate the
sizes of 90–710 µm izes tiny holes in the pulp and DH occurs mineralization.
was introduced for the dentine and reduces [36]. Dissolu- tion of the
repair of bony defects the sensitivi- When these glass in the mouth
of the jaw and bone ty of the tooth. Dentin kinds of toothpastes raises pH, which leads
loss arising from hypersensitivity (DH) ® to promotion of HAp
are used, Bioglass deposition [39].
perio- dontal disease. is an oral problem particles adhere to the
In vivo and clinical which is attributed to The sol-gel derived
dentine and form an
studies [28-30] the root surface expo- bioactive particles
HAp layer; therefore,
showed a great success sure due to periodontal are also us-
® blocking of the tubules
of Perio-Glas in disease, toothbrush relieves the pain for
treatments of defects abrasion or longer periods. In a
filled with new bone clinical trial of 100
compared to controls. volunteers who
The regenerative brushed twice daily
properties for infra- ®
with a NovaMin -
bony defects can be
containing toothpaste
enhanced with low-
over the 6-week
level laser therapy
period, gingival
post- operatively [31].
bleeding and plaque
Another application of
® growth reduced 58.8%
Perio-Glas is in and 16.4% respectively
“guided tissue in comparison with
regeneration”, which the control groups
has been used with who used normal
polymeric membranes toothpaste [37].
®
[32]. Perio-Glas can Another clinical trial
also be used to has shown improved
produce bioactive pain relief when
glass slurry with brushing with a
applica- tions in root ®
NovaMin -containing
canal sterilization toothpaste for 2-6
tools prior to insertion weeks compared to
of implants and raising brushing with a
pH to bactericidal toothpaste containing
levels in addition to its potassium nitrate [38].
bioactive properties Despite brushing
[33]. Other prod- ucts, only for a few minutes
which have been used ®
a day, the Bioglass
as bone graft in
particles stimulate
dentistry and
long-term repair,
orthopaedic, are
® which results from the
Biogran (BIOMET fact that these particles
ed in treatment of hypersensitivity. The trials have effective remineralizing agent as the effects of bioac-
shown that 24 h after using toothpaste containing the tive-containing products were investigated on
sol–gel and after washing with cola, juice, coffee and remineralization of artificial induced carious enamel
further brushing, the tubules remain occluded [40]. lesion [46].
Toothpaste is not the only dental care application *Bioactive Glass Coatings
® ®
of Bioglass ; NovaMin can repair the enamel sensi- As metals are bioinert, the metallic implants are
tivity due to bleaching treatments of the teeth [39]. For encapsulated with fibrous tissue after implantation and
whitening the teeth, dentists use air polishing using cannot attach to tissue which shows serious need of
particles as abrasives to remove the stains. Air polish- such implants to bioactive coatings. The hydroxyap-
®
ing with Bioglass can stimulate mineralization of the atite layer forms on bioactive glass coatings as a result
dentine tubules in a similar mechanism to that of of dissolution and improves the bonding of implants to
®
NovaMin -containing toothpaste, which resulted in the host bone. The problem is that a highly bioactive
44% reduction of tooth sensitivity compared to other coating may degrade over time and result in instability
air polishing powders, such as sodium bicarbonate. of the metallic implant in the long term. Perhaps, the
®
Teeth treated with the Bioglass were also whiter than dental field is the best application for bioactive glass
those coatings, e.g. on titanium implants with screw threads.
treated with sodium bicarbonate [41]. However, it should be noted that the thermal expan-
*Remineralization Using Bioactive Glass sion coefficient of the glass and the metal must match
Demineralization and remineralization are natural to prevent the glass pulling away from the metal dur-
processes which continuously occur for teeth. Physio- ing the processing [47]. For instance, the thermal ex-
®
logical processes as well as bacterial acids and foods pansion coefficient of the Bioglass and titanium
cause demineralization, while remineralization results don’t match. In order to address such problem, for
from the deposition of mineral (calcium and phospho- example, in the SiO2–CaO–MgO–Na2O–K2O–P2O5
rous) from saliva or oral fluid. Since natural system, the Na2O and CaO are replaced with K2O and
remineralization is not enough for having strong MgO, respectively to modify the thermal expansion
enamel, bioactive glasses are used to augment the pro- coefficient [48]. Another example is coating with the
cess. Bioactive glasses have unique remineralizing following composition (by weight): 53% SiO2, 6%
properties and are generally introduced into various Na2O, 22% CaO, 11% K2O, 5% MgO, 2% P2O5, and
dentifrices as very fine particles to provide calcium 1% B2O3 on titanium implants, which were first test-
and phosphorus to the tooth surface [42]. ed in rabbit femurs [49]. Compared to non-coated im-
The first study on dentin remineralization by a bio- plants, more bone grew on the coated implants. By
active glass was conducted by Wang et al. [43]. In this using appropriate compositions, the mismatch of
study, after artificial demineralization with EDTA thermal expansion coefficients doesn’t make any
(ethylene-diamine-tetraacetic acid), the treatment with problem and bioactive glasses can successfully be
nanoparticulate bioactive glass was compared to the used as coatings.
®
(PerioGlas ). The results showed that nanoparticulate Table 2: Name and application of some products of the
bioactive glass resulted in a noticeable increase in original Bioglass® and their applications
mineral content suggested a rapid remineralization of Product Applications
the samples. This result confirmed the critical role of ERMI® Repair of the tooth roots and providing a sta-
particle size and specific surface area. However, these ble ridge for dentures
samples are mechanically unstable, unless the precipi- Perio- Repair of bony defects of the jaw and bone
tated mineral forms a composite material with the col- Glas® loss arising from periodontal disease- Guided
tissue regeneration- Root canal sterilization
lagen matrix of the samples [43]. In addition, investi- tools
gations on bioactive glass-containing toothpaste show Biogran® Bone graft
significant reduction in dentine permeability and ex- BonAlive® Bone graft
cellent resistance to acid challenge which can be bene- NovaMin® Active repair agent in toothpaste for hypersen-
ficial for hypersensitivity and remineralization treat- sitivity treatment- Repair of the enamel sensi-
ments [44]. tivity due to bleaching treatments of the teeth-
In 2014, Mehta et al. showed that bioactive glass Remineralizing agent
®
(Novamin ) and casein phosphopeptide-amorphous
calcium phosphate (CPP-ACP) successfully 5. Antibacterial properties
remineralized early enamel caries. However, During dissolution of bioactive glass, the pH rises due
®
Novamin remineralized the carious lesion more ef- to cation release and such condition can kill the mi-
fectively. CPP-ACP had an amorphous nature and crobes [1]. For instance, an in vitro study showed that
couldn’t properly adhere to the enamel surface. This S53P4, as one kind of bioactive glass, can kill patho-
also led to lower hardness value for CPP-ACP, while gens connected with enamel caries (Streptococcus
®
Novamin showed higher values of hardness because mutans), root caries (Actinomyces naeslundii, S.
it attached to the surface more compactly [45]. In an- mutans) and periodontitis (e.g. Actinobacillus
other study, it was confirmed that bioactive glass is an actinomycetemcomitas) [50]. S53P4 and other compo-
sitions of bioactive toxic to human effect of en- dogenous with 2% zinc citrate
glass with osteoblasts [53]. growth factors, which have been used in the
concentrations higher Silver-containing sol- makes it a perfect treatment of poor
-1
than 50 mg ml in the gel glasses have a additive for blood gingival health [61].
broth cultures of 16 limitation in their vessel ingrowth [57].
different bacteria synthesis as it must be Cellular cop- per can 6
showed antibacterial conducted under be regarded as an .
properties due to the infrared radiation and angiogenic agent
pH increase [50]. It is the glass must be because of its M
postulated that an ideal stored in the dark to remarkable e
bioactive glass prevent the silver distributions in human c
material includes nitrate precursor and endothelial cells h
antibacterial elements Ag2O reducing to during their a
which prevent silver metal. This not angiogenesis. This ion n
infections and reduce only increases the cost can also stimulate the i
the post-operative of pro- duction, but endothelial cell c
sensi- tivity. The also complicates the proliferation and a
widely considered surgical procedures. suppress osteo- clast l
elements for this pur- Silver-doped melt- activity [58].
pose are metals which derived glasses have Moreover, elastin
have bioactivity also improved p
matrix deposition can
against micro- bactericidal properties r
be stimulated by this
organisms and can compared to silver-free o
metal because elastin
overcome the equiva- lent glasses. p
fibrils can aggregate
problems related with Nanoparticles of e
into mature fibers
the low stability of ®
Bioglass can kill En- r
when copper ions are
other organic terococcus faecalis, a t
released from
antimicrobial micro-organism i
nanoparticles [59].
compounds during the associated with failed e
Zinc is another
biomaterial processing root canal treatments s
metal which is thought
[51]. [54]. The application of
to have an- tibacterial bioactive glasses,
Silver is one of the Copper and its properties and
elements known as alloys, such as brass, due to their low
beneficial cellular mechanical strength
antimicro- bial. Silver bronz, copper- nickel response, but it can
ions can easily be and copper-nickel-zinc and inherent
also cause toxicity brittleness, has been
introduced into a glass can also be used in an- [60]. Because of anti- limited to non-load-
and then released timicrobial inflammatory and bearing parts such as
during dissolution. applications. The antimicrobial ossicles in the middle
The sol-gel- derived strong antimicrobial properties, dentifrices ear. Incorporation of
composition of 76 % ions of copper can be
SiO2, 19% CaO, 2% doped to different nitrogen into the sili-
P2O5 and 3% Ag2O matrices such as cate network can
(by weight) is the first address the problem of
polymers or ceramics
antibacteri- low strength in
[55,56]. Copper not
al glass which glasses. When oxygen
only is an excellent
contains silver [52]. is replaced by nitrogen
- antimicrobial agent but
Less than 1 mg ml in alumino-silicate
1 also has an essential
of this glass in glasses, elastic
role in bone
culture is needed to modulus and hardness
formation and
kill bacteria such as increase linearly with
healing. This metal
Escherichia coli, nitrogen content;
can also stimulate
Pseudomonas however, glass
wound healing
aeruginosa and transition temperature
responses and increases, as well.
Staphylococcus
improves the vascular Incorporation of
aureus, compared to
-1 density in and around nitrogen also results in
50 mg ml of silver-
subcutaneously greater slow crack
free glasses to be
implanted allografts growth resistance,
bactericidal. It is
and hyaluronan based modest gains in
noteworthy
hydrogel. Copper fracture resistance, and
that the low
sulfate can induce the increased viscosities
concentrations of the
formation of cord-like [62]. Addition of
sol-gel glass that can
and tubular structures both fluorine and
be bactericidal are not
and potentiate the
nitrogen can increase present in bioactive
the mechanical glasses as
properties as fluorine orthophosphate, aids in
induces considerable maintaining the
reductions in both network connectivity.
glass melting In fluoride-containing
temperatures (Tm) and glasses, the formation
glass transition of flourapatite at low
temper- atures (Tg) pH is favored by
while elastic modulus increasing P2O5 and
and hardness in- crease this is more favorable
with nitrogen for clinical
incorporation but they applications of
are unaf- fected by dentistry and
fluorine incorporation. orthopedics [65].
The dissolution of *Effect of fluoride
nitrogen into the glass Fluoride can inhibit
melt is also facilitated the demineralization of
by fluo- rine [63]. the enamel and dentin,
enhance
7. Effects of different remineralization, and
ion doping on other in- hibit bacterial
proper- ties of enzyme; hence, it
bioactive glass prevents dental decay
In addition to and improves the oral
antibacterial and health [66].
mechanical properties *Effect of zinc
of bioactive glass, Zinc is a
other properties can fundamental ion that
also be affected by improves bone-
adding different ions bonding of glass,
which make the inhibits bone
material more resorption, controls
compatible for cell growth,
different clinical differentiation, and
applications. development and
*Effect of strontium stimulates protein
Strontium is a synthesis. Slow
bone-seeking agent, skeletal growth and
able to impact bone alterations in bone
cells which can be calcification can result
substituted for from zinc deficiency
calcium in bioactive [60].
glass for better bone
bonding and osteoblast
stimulation, with
anabolic and anti-
catabolic proper-
ties. For treatment of
osteoporosis, strontium
ranelate and strontium
chloride can be used.
Osteoblast prolif-
eration can be
promoted by
strontium-substituted
®
Bioglass which also
decreases the
osteoclast activity in
the cell culture [64].
*Effect of phosphate
Increasing
phosphate which is
8. Modification of not bioactive. before, bioactive ceramic was coated by
dental ceramics with Consequently, if these glasses can restore a bioactive glass and
a bioactive glass ceramics would be osseous defects and after im- mersion in
Dental ceramics modified in a way that develop a new SBF, the growth of a
should have specific they could stimulate attachment on tooth well-attached apatite
properties, such bioactive behavior surfaces. The strong layer on the surface
as high strength, around the fixed and stable bonding was observed [70].
fracture toughness, restora- tions margins results from Moreover, it was
wear resistance, and provide a development of a reported that the
similarity with natural bioactive surface, hydroxyapatite layer, attachment and
tooth structure and through the tissue similar to that of the proliferation of human
long life in the oral regenerative bone, on the surface periodontal ligament
environment, in order techniques, they could after inclusion into cells can be supported
to be used in develop periodontal biological by dental ceramic–
restorative dentistry. tissue attachment and environment. bioactive glass
To successfully place create complete Sometimes, biological mixtures [71].
the fixed restorations sealing of the marginal apatites include traces As expected, sol-
in the oral gap. This sealing could of inorganic elements gel method can create
environment, it is prevent the failure of that can be substituted a more po- rous
necessary to keep fixed ceramic in the apatite lattice or surface which raises
perio- dontal tissues restorations by adsorbed on the apatite the dissolution rate and
healthy. Fixed eliminating secondary surface. Bioactive promotes apatite
restorations increase caries, materials can form this formation, so dental
the local plaque micropenetration of bio- logical apatite on ceramic- bioactive
accumulation, the oral bacteria and their surface in vitro glass mixture prepared
especially with poor their adhesion on under various soaking by such method can
oral hygiene, and lead cement surface [68]. conditions [7]. accelerate the onset of
to inflammation, loss It is expected that Development of HAp formation [72].
of attachment and utilization of guided apatite on the dental In 2010, two sol–gel
eventually periodontal tissue re- generation ceramic sur- faces derived materials were
tissue’s breakdown. techniques in the field through modification successfully pro-
Exist- ence of a of dental ceramics can with bioactive glasses duced for dental
marginal gap between provide solutions to has been tried by applications: a novel
the tooth and restora- address fixed several researchers. ceramic and a
tion which is exposed prosthetic resto- In 2003, a dental bioactive mixture
to oral bacteria results rations failure. This (ceramic 30 wt.%-
in pulp irritation or technique can result in bioactive glass
necrosis, secondary formation of new 58S 70 wt.%) with
caries and cement attachments on the better control of
dissolution, all being tooth surfaces (e.g. composition, mi-
the common reasons cementum) or on crostructure and
of fixed prosthetic implant surfaces properties due to high
restoration failure (Titanium, hydrox- homogeneity provided
[67]. yapatite, etc.). by the sol-gel method,
It is impossible for Therefore, if dental compared to melt-
ceramic materials to ceramics could exhibit derived ceramics [22].
develop new a cement-like In melting powder
attachment on their behavior, the preparation techniques,
surface. Therefore, in biological surface the sur- face reactivity
spite of the ability of required for of ceramics has been
fixed ceramic attachment of the cells weakened by high
restorations to would be provided and reaction temperature,
regenerate the tissue attachment which results in high
morphology and would be promoted. heteroge-
function of the Formation of apatite neity and loss of
damaged struc- ture, on the dental ceramic porosity and their
they cannot surface can enhance surface area de-
completely attach to the tissue attachment pends only on the
the periodontal tissue. because cementum particle size of the
In fact, conventional consists of biological powders [21]. On the
dental ceramics are hydroxyapatite [69]. other hand, the sol-gel
bio- compatible but As mentioned method provides
control over the are used for
textural properties hypersensitivity
(specific surface area treatment. One of the
and porosity) and most im- portant
crystal structure which properties of bioactive
develops an op- glasses is their ability
timized bioactive to exhibit antibacterial
surface and also activity, which creates
maintains the sur- face a bacte- ria-free
bioactivity over a environment while
wider composition healing and
range of silica content regenerating the defect
[73]. area. The promotion of
this ability is possi- ble
C by doping antibacterial
o elements, such as
n silver, copper or zinc
c to such glasses.
l Another property of
u bioactive glasses is
s mechanical property
i which can be improved
o by introducing
n nitrogen and fluorine
s to the silicate network
of the glasses. The
Bioactive glasses are other properties of
able to bond to both bioactive glasses can
soft and hard tissue also be altered by
and promote the bone incorporation of
growth. The bioac- different ions such as
tivity behavior of these strontium and
glasses is related to the phosphates. These
for- mation of a potentials of bioactive
biologically active glass make it a unique
hydroxyapatite layer material to be widely
on the surface of the used in dentistry. For
glasses. The example,
mechanism of bonding
of bioactive glasses to
tissues includes a
series of sur- face
reactions that occur
when the glass is
exposed to an aqueous
environment. These
glasses are produced
via two main methods,
melting and sol-gel
processing. The latter
has many advantages
which make it a fa-
vorable method in
order to provide
glasses with fine
porous textures and
enhanced bioactivity.
Bioactive glasses have
a wide range of
applications, such as
bone grafts, scaffolds,
coating materials, and
modification of dental Sol-Gel Processing. J Mater. 2013;29:1256- 20. Greenspan DC,
ceramics with sol-gel Appl Biomater. 1264. Zhong JP, LaTorre
1991;2:231-239. 14. Cerruti M, GP. The evaluation of
derives bioactive Greenspan D,
5. Laudisio G, Branda surface structure of
glasses is one of the Powers K. Effect of
F. Sol-gel synthesis bioactive glasses in-
most attractive and crystallisa- tion pH and ionic vitro. In Wilson J,
applica- tions of these strength on the Hench LL, Greenspan
of 3CaO.2SiO2
glasses in dentistry. reactivity of D, editors:
glassy powders.
Such materials can Thermochim Acta. Bioglass® 45S5. Bio- Bioceramics. Elsevier
materials. Science; 1995;8:477-
stimulate bioactive 2001;370:119-124.
2005;26:1665-1674.
behavior around the 6. Greenspan DC, 482.
15. Gross UM, Strunz V. 21. Sepulveda P, Jones
fixed restora- tions Zhong JP, Latorre
The anchoring of JR, Hench LL.
margins and provide a GP. Effect of surface
glass ceramics of Characterization of
area to volume ratio
bioactive surface. different solubility in melt-derived 45S5
on in vitro surface
There- fore, they can the femur of the rat. J and sol-gel-derived
reactions of bioac-
develop periodontal Biomed Mater Res. 58S bioactive glasses.
tive glass particulates.
tissue attachment and 1980;14:607-618. J Biomed Mater
Bioceramics.
16. Greenspan D, Hench Res (Appl
create complete 1994;7:28-35.
LL. Chemical & Biomater).
sealing of the marginal 7. Siriphannon P,
mechanical behav- ior
gap. This sealing can Kameshima Y, 2
Yasumori A, et al. of Bioglass coated 0
prevent the failure of alumina. J Biomed
For- mation of 0
fixed ceramic resto- hydroxyapatite on Mater Res. 1
rations by eliminating CaSiO3 powders in 1976;10:503-509. ;
the secondary caries, simulated body fluid. 17. Li J, Cai S, Xu G, et 5
micropenetration of J Eur Ceram Soc. al. In vitro 8
oral bacteria and their 2002;22:511-520. biocompatibility :
8. LeGeros RZ. study of calcium 7
adhesion on the
Properties of phosphate glass 3
cement surface. ceramic scaffolds
osteoconductive 4
biomaterials: with different trace -
R calcium phosphates. element doping. 7
e Clin Orthop Relat Mater Sci Eng C. 4
f Res. 2002;395:81- 2012;32:356-363. 0
e 98. 18. Sakka S. Glasses and .
r 9. Jones JR. Review of glass-ceramics from 22. Chatzistavrou X,
bioactive glass: From gels. J Non- Cryst Esteve D,
e
Hench to hy- brids. Solids. 1985;73:651- Hatzistavrou E, et al.
n 660.
Acta Biomater. Sol-gel based
c 19. Brinker CJ, Scherer
2013;9:4457-4486. fabrication of novel
e 10. Hench LL, Polak JM. GW. Sol-gel glass: I. glass-ceramics and
s Third-generation Gelation and gel composites for dental
biomedical mate- structurc. J Non- applications. Mater
1. Stoor P, Soderling E, rials. Science. Cryst Solids. Sci Eng C.
Salonen JI. 2002;295:1014-1017. 1985;70:301-322. 2010;30:730-
Antibacterial effects 11. Rahaman MN, Day 7
of a bioactive glass DE, Bal BS, et al. 3
paste on oral Bioactive glass in 9
microorganisms. Acta tissue engineering. .
Odontol Scand. Acta Biomater. 23. Laczka M, Cholewa
1998;56:161-165. 2011;7:2355-2373. K, Laczka-Osyczka
2. Hench LL, Splinter 12. Kokubo T, Kushitani A. Gel-derived
RJ, Allen WC, et al. H, Sakka S, et al. powders of CaO-
Bonding mecha- Solutions able to P2O5-SiO2 system as
nisms at the reproduce in vivo a starting material to
interface of ceramic surface-structure production of
prosthetic materials. change in bioactive bioactive ceramics. J
J glass-ceramic A-W. Alloys Compd.
Biomed Mater. J Biomed Mater Res. 1
1971;5:117-141. 1990;24:721- 9
3. Hench LL. The 734. 9
story of Bioglass®. J 13. Plewinski M, 7
Mater Sci: Mater Schickle K, Lindner ;
Med. 2006;17:967- M, et al. The effect of 2
978. crystallization of 4
4. Li R, Clark AE, bioactive bioglass 8
Hench LL. An 45S5 on apatite for- :
Investigation of Bioactive mation and 4
Glass Powders by degradation. Dent 2
- osteointegration of Bulman JS, et al.
5 prosthetic elements. J 2 Perceptions of
1 Mater Sci-Mater 0 dentine
. Med. 2012;23:2369- 0 hypersensitivity in a
24. Stanley HR, Hall 2380. 9 general practice
MB, Clark AE, et al. 28. Wilson J, Low SB. ; population. J Oral
Using 45S5 Bioactive ceramics 2 Rehabil.
Bioglass cones as for periodontal 4 1999;26:710-714.
endosseous ridge treatment- : 36. Kawabata M, Hector
maintenance implants comparative studies 3 MP, Davis GR, et al.
to prevent alveolar in the Patus monkey. 8 Diffusive tra- nsport
ridge resorption: A 5- J Appl Biomater. 7 within dentinal
year evaluation. Int J 1992;3:123-129. - tubules: an X-
Oral Maxillofac Impl. 29. Park JS, Suh JJ, Choi 3 ray
1997;12:95-105. SH, et al. Effects of 9 microtomographic
25. Zhong J, Greenspan pretreatment clinical 5 study. Arch Oral
DC. Processing and parameters on . Biol. 2008;53:736-
properties of sol- gel bioactive glass 32. Yadav VS, Narula 7
bioactive glasses. J implantation in SC, Sharma RK, et 4
Biomed Mater Res intrabony periodontal al. Clinical evalua- 3
(Appl defects. J Periodontol. tion of guided .
B 2001;72:730- tissue regeneration 37. Tai BJ, Bian Z, Jiang
i 7 combined with H, et al. Anti-
o 4 autogenous bone or gingivitis effect of a
m 0 autogenous bone dentifrice containing
a . mixed with bioac- bioactive glass
t 30. Norton MR, Wilson tive glass in (NovaMin) particu-
e J. Dental implants intrabony defects. J
r placed in extrac- tion Oral Sci.
) sites implanted with 2011;53:481-
. bioactive glass: 4
human histology 8
2 and clinical 8
0 outcome. Int J Oral .
0 Maxillofac Implants. 33. Waltimo T, Mohn D,
0 2 Paque F, et al. Fine-
; 0 tuning of bioac- tive
5 0 glass for root
3 2 canal disinfection. J
: ; Dent Res.
6 1 2
9 7 0
4 : 0
- 2 9
7 4 ;
0 9 8
1 - 8
. 3 :
26. Boccaccini AR, 5 2
Erol M, Stark WJ, 7 3
et al. Poly- . 5
mer/bioactive glass 31. AboElsaad NS, Soory -
nanocomposites for M, Gadalla LMA, et 2
biomedical appli- al. Effect of soft laser 3
cations: a review. and bioactive glass 8
Compos Sci on bone regeneration .
Technol. in the 34. Turunen T, Peltola J,
2010;70:1764- treatment of infra- Yli-Urpo A, et al.
1 bony defects (a Bioactive glass
7 clinical study). granules as a bone
7 Lasers adjunctive material in
6 M maxillary sinus floor
. e augmentation. Clin
27. Vitale-Brovarone C, d Oral Implants Res.
Baino F, Tallia F, et
2004;15:135-
al. Bioactive glass-
S 1
derived trabecular
c 4
coating: a smart
i 1
solution for en-
. .
hancing
35. Gillam DG, Seo HS,
late. J Clin an in vitro study. Aust embedded metal with embedded
Periodontol. Dent J. ions synthesized by copper metal or
2006;33:86-91. 2011;56:372–381. the sol-gel method J. copper oxide
38. Pradeep AR, Sharma 45. Mehta AB, Kumari Mater Sci Eng nanoparti- cles as a
A. Comparison of V, Jose R, et al. C. 2013;33:3795- novel plastic
clinical efficacy of a Remineralization 3801. antimicrobial agent.
dentifrice containing potential of 52. Bellantone M, Lett Appl Microbiol.
calcium sodium bioactive glass and Coleman NJ, Hench 2011;53:50-54.
phosphosilicate casein LL. Bacteriostatic 56. Abou Neel EA,
to a dentifrice phosphopeptide- action of a novel four Ahmed I, Pratten J, et
containing potassium amorphous calcium component bioactive al. Characterization of
nitrate and to a place- phosphate on initial glass. J Bio med antibacterial copper
bo on dentinal carious lesion: Mater Res. releasing degradable
hypersensitivity: a An in-vitro pH- 2000;51:484-490. phosphate
randomized clinical cycling study. J 53. El-Kady AM, Ali glass fibres.
tri- al. J Periodontol. Conserv Dent. AF, Rizk RA, et al. Biomaterials.
2010;81:1167-1173. 2014;17:3- Synthesis, charac- 2005;26:2247-2254.
39. Earl JS, Leary RK, 7. terization and 57. Gérard C, Bordeleau
Muller KH, et al. 46. Narayana SS, microbiological LJ, Barralet J, et al.
Physical and chemi- Deepa VK, Ahamed response of silver The stimulation of
cal characterization S, et al. doped angiogenesis and
of dentin surface, Remineralization bioactive glass collagen deposition
following treatment efficiency of nanoparticles. Ceram by copper. Bio-
with NovaMin bioactive glass on Int. 2012;38:177- materials.
technology. J Clin artifi- cially induced 188. 2010;31:824-831.
Dent. 2011;22:2-67. carious lesion an in- 54. Waltimo T, Brunner 58. Zhang JC, Huang JA,
40. Mitchell JC, Musanje vitro study. J Indian TJ, Vollenweider M, Xu SJ, et al. Effects of
L, Ferracane JL. Soc Pedod Prev et al. Antimi- crobial Cu2+ and pH
Biomimetic dentin Dent. 2014;32:19-25. effect of nanometric on osteoclastic bone
desensitizer based 47. Gomez-Vega JM, bioactive glass 45S5. resorption in vitro.
on nano-structured Saiz E, Tomsia AP, J Dent Prog Nat Sci.
bioactive glass. et al. Novel bioac- Res. 2007;86:754- 2003;13:266-270.
Dent Mater. tive functionally 757. 59. Kothapalli CR,
2011;27:386-393. graded coatings on 55. Delgado K, Quijada Ramamurthi A.
41. Banerjee A, Ti6Al4V. Adv R, Palma R, et al. Copper nanoparticle
Hajatdoost-Sani M, Mater. 2000;12:894- Polypropylene cues for biomimetic
Farrell S, et al. A 898. cellular assembly of
clinical evaluation 48. Gomez-Vega JM, crosslinked elastin fi-
and comparison of Saiz E, Tomsia AP, bers. Acta Biomater.
bioactive glass and et al. Bioactive glass 2009;5:541-553.
sodium coatings with 60. Aina V. Perardi A,
bicarbonate air- hydroxyapatite and Bergandi L, et al.
polishing powders. J Bioglass particles Cytotoxicity of zinc-
Dent. 2010;38:475- on Ti-based containing bioactive
479. implants. I glasses in contact
42. Madan N, Madan N, Processing. with human osteo-
Sharma V, et al. Biomaterials. blasts. Chem Biol
Tooth remineraliza- 2000;21:105-111. Interact.
tion using bio-active 49. Moritz N, Rossi S, 2007;167:207-218.
glass - A novel Vedel E, et al. 61. Saino E, Grandi S,
approach. J Acad Implants coated with Quartarone E, et al.
Adv Dent Res. bioactive glass by In vitro calcified
2011;2:45-50. CO2-laser, an in vivo matrix deposition
43. Vollenweider M, study. J Mater by human
Brunner TJ, Knecht Sci-Mater Med. osteoblasts onto a
S, et al. 2004;15:795-802. zinc-
Remineralization of 50. Zhang D, Lepparanta containing bioactive
human dentin using O, Munukka E, , et glass. Eur Cells Mater.
ultrafine bioac- tive al. Antibacterial 2011;21:59-
glass particles. Acta effects and 72.
Biomater. dissolution behavior 62. Bachar A, Mercier C,
2007;3:936–943. of six bioactive Tricoteaux A, et al.
44. Wang Z, Jiang T, glasses. J Biomed Effects of addi- tion
Sauro S, et al. The Mater Res. of nitrogen on
dentine 2010;93:475-483. bioglass properties
remineralization 51. Palza H, Escobar B, and structure. J
activity of a Bejarano J, et al. Non-Crys Solids.
desensitizing Designing antimi- 2012;358:693-701.
bioactive glass- crobial bioactive 63. Hanifi AR, Pomeroy
containing toothpaste: glass materials with MJ, Hampshire S.
Novel glass for- dynamic conditions.
mation in the Ca– Phys Status Solidi A.
Si–Al–O–N–F 2003;198:65-
system. J Am 75.
Ceram Soc. 71. Kontonasaki E,
2011;94:455-461. Papadopoulou L,
64. Gentleman E, Zorba T, et al.
Fredholm Y, Jell G, Apatite formation on
et al. The effects of dental ceramics
strontium-substituted modified by bioactive
bioactive glasses on glass. J Oral Rehabil.
osteoblasts and 2003;30:893-902.
osteoclasts, in vitro. 72. Kontonasaki E,
Biomaterials. Kantiranis N,
2010;31:3949-3956. Papadopoulou L, et
65. Brauer D, al. Mi- crostructural
Karpukhina N, characterization and
O’Donnell MD, et al. comparative
Fluoride- containing evaluation
bioactive glasses: of physical, mechanical
effect of glass design and biological
and structure on properties of three
degradation, pH and ceramics for metal
apatite formation in ceramic restorations.
sim- ulated body Dent
fluid. Acta Biomater. Mater. 2008;24:1362-
2010;6:3275-3282. 1373.
66. Brauer DS, 73. Salinas AJ, Vallet-
Karpukhina N, Regi M. The sol-gel
O’Donnell MD, et al. production of
Struc- ture of Bioceramics. Key Eng
fluoride-containing Mater. 2008;391:141-
bioactive glasses. J 158.
Mater Chem.
2009;19:5629-5636.
67. Wickens JL. Tooth
surface loss: Dealing with
failures.
Br Dent J.
1999;186:443-446.
68. Craig RG, LeGeros
RZ. Early events
associated with
periodontal
connective tissue
attachment formation
on ti-
tanium and
hydroxyapatite
surfaces. J Biomed
Mater Res.
1999;47:585-594.
69. Kokoti M,
Sivropoulou A,
Koidis P, et al.
Comparison of cell
proliferation on
modified dental
ceramics. J Oral
Rehabil. 2001;28:880-
887.
70. Papadopoulou L,
Kontonasaki E, Zorba
T, et al. Dental
ceramics coated with
bioactive glass:
Surface changes af-
ter exposure in a
simulated body fluid
under static and
Você também pode gostar
- Biomaterials Science: Processing, Properties and Applications IVNo EverandBiomaterials Science: Processing, Properties and Applications IVSusmita BoseAinda não há avaliações
- Biomaterials: Alexander Hoppe, Nusret S. Güldal, Aldo R. BoccacciniDocumento18 páginasBiomaterials: Alexander Hoppe, Nusret S. Güldal, Aldo R. Boccaccini林佳君Ainda não há avaliações
- Articulo Biomateriales CeramicosDocumento37 páginasArticulo Biomateriales CeramicosIran QuirozAinda não há avaliações
- Chronology of Bioactive Glass Development and Clinical ApplicationsDocumento7 páginasChronology of Bioactive Glass Development and Clinical ApplicationsNileshTipanAinda não há avaliações
- Bioglass Hench To HybridsDocumento30 páginasBioglass Hench To HybridsSreedhar PugalendhiAinda não há avaliações
- Bioceramic in Dental ImplantsDocumento5 páginasBioceramic in Dental ImplantsDeepalakshmi VenkatesanAinda não há avaliações
- A Study On The Crystallization of Hydroxyapatite On Hydroxyethyl Cellulose SpongesDocumento9 páginasA Study On The Crystallization of Hydroxyapatite On Hydroxyethyl Cellulose SpongesInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Bioglass: A Novel Biocompatible Innovation: Vidya Krishnan T. Lakshmi Author Information Go ToDocumento10 páginasBioglass: A Novel Biocompatible Innovation: Vidya Krishnan T. Lakshmi Author Information Go ToraieskhannitAinda não há avaliações
- Bioceramic-Based Root Canal Sealers: A Review: International Journal of Biomaterials January 2016Documento12 páginasBioceramic-Based Root Canal Sealers: A Review: International Journal of Biomaterials January 2016Ovy Prima DamaraAinda não há avaliações
- ch2 Melt-Derived Bioactive GlassDocumento15 páginasch2 Melt-Derived Bioactive GlasslilypaivaAinda não há avaliações
- Bioactive Materials: Jianhui Chen, Lei Zeng, Xiaofeng Chen, Tianshun Liao, Jiafu ZhengDocumento7 páginasBioactive Materials: Jianhui Chen, Lei Zeng, Xiaofeng Chen, Tianshun Liao, Jiafu ZhengKharisah AfifahAinda não há avaliações
- 1 JACS HenchDocumento40 páginas1 JACS Henchanon_789829405Ainda não há avaliações
- Bioceramic SealersDocumento4 páginasBioceramic SealersMonalisa DebbarmaAinda não há avaliações
- Bioactive Glass - Mechanism of Bone BondingDocumento5 páginasBioactive Glass - Mechanism of Bone Bondingcollin samuelAinda não há avaliações
- Calcium CarbonateDocumento13 páginasCalcium CarbonateAisah Cory PrasonoAinda não há avaliações
- Bioceramic Sealer ReviewDocumento11 páginasBioceramic Sealer ReviewArdelia RaissaAinda não há avaliações
- Review Article Bioceramics in Operative Dentistry and EndodonticsDocumento9 páginasReview Article Bioceramics in Operative Dentistry and EndodonticspoojaAinda não há avaliações
- Chemistry-Hydrothermally Synthesized Hydroxyapatite-Silica CompositesDocumento11 páginasChemistry-Hydrothermally Synthesized Hydroxyapatite-Silica Compositeseti apriyantiAinda não há avaliações
- Biomimetic Scaffolds From Hydroxyethyl CelluloseCalcium Phosphate For Bone Tissue Engineering ApplicationsDocumento6 páginasBiomimetic Scaffolds From Hydroxyethyl CelluloseCalcium Phosphate For Bone Tissue Engineering ApplicationsInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Nowatorski Bioaktywny Uszczelniacz Kanałowy Na Bazie Szkła W EndodoncjiDocumento8 páginasNowatorski Bioaktywny Uszczelniacz Kanałowy Na Bazie Szkła W EndodoncjiKarolina WójcikAinda não há avaliações
- Endodontic Sealers Based On Calcium Silicates: A Systematic ReviewDocumento16 páginasEndodontic Sealers Based On Calcium Silicates: A Systematic ReviewFedia AjiliAinda não há avaliações
- Bioactive Glasses: Where Are We and Where Are We Going?: Functional BiomaterialsDocumento26 páginasBioactive Glasses: Where Are We and Where Are We Going?: Functional BiomaterialsLucas AraujoAinda não há avaliações
- Materials Science and Engineering CDocumento10 páginasMaterials Science and Engineering CInesita de AlcobendillasAinda não há avaliações
- 7 & 8 - Bioactive GlassesDocumento41 páginas7 & 8 - Bioactive GlassesmahaAinda não há avaliações
- 63 PDFDocumento6 páginas63 PDFAngelAinda não há avaliações
- Articulo Materiales BioactivosDocumento8 páginasArticulo Materiales BioactivosIvette BustillosAinda não há avaliações
- Bjoernoey 2015Documento14 páginasBjoernoey 2015brouuorbAinda não há avaliações
- Dental Research Journal: A Review of Glass-Ionomers: From Conventional Glass-Ionomer To Bioactive Glass-IonomerDocumento10 páginasDental Research Journal: A Review of Glass-Ionomers: From Conventional Glass-Ionomer To Bioactive Glass-IonomerFRANCISCO JAVIER BRAVO RIVEROSAinda não há avaliações
- Bio GlassDocumento7 páginasBio GlassAndu1991100% (1)
- The Advent of Bioceramics in Dentistry: A ReviewDocumento5 páginasThe Advent of Bioceramics in Dentistry: A Reviewpooja100% (1)
- 97bioactivity Improvement of Poly (E-Caprolactone) Membrane With The Addition of Nanofibrous Bioactive GlassDocumento8 páginas97bioactivity Improvement of Poly (E-Caprolactone) Membrane With The Addition of Nanofibrous Bioactive Glassormlove09Ainda não há avaliações
- tmpB150 TMPDocumento21 páginastmpB150 TMPFrontiersAinda não há avaliações
- Mello Et Al - 2015 PDFDocumento10 páginasMello Et Al - 2015 PDFlorena amorimAinda não há avaliações
- Hidroxi Sol-Gel Ashuri 2012Documento10 páginasHidroxi Sol-Gel Ashuri 2012Tharcilla SouzaAinda não há avaliações
- UTS - Take Home PDFDocumento17 páginasUTS - Take Home PDFErna LumbantoruanAinda não há avaliações
- Bioceramics For Clinical Application in Regenerative DentistryDocumento8 páginasBioceramics For Clinical Application in Regenerative DentistrypoojaAinda não há avaliações
- BIOCERAMIC Implants 4-2Documento6 páginasBIOCERAMIC Implants 4-2sushilAinda não há avaliações
- Synthesis Characterization and Bioactivity of A Calcium Phosphate Glass-Ceramics Obtained by The Sol-Gel Processing MethodDocumento10 páginasSynthesis Characterization and Bioactivity of A Calcium Phosphate Glass-Ceramics Obtained by The Sol-Gel Processing MethodZino KamounAinda não há avaliações
- Bio Materials For MedicineDocumento6 páginasBio Materials For MedicineIan Anderson Konopczyk Maluf100% (1)
- Mechanisms of Bioactive Glass On Caries Management: A ReviewDocumento15 páginasMechanisms of Bioactive Glass On Caries Management: A Reviewmilagros falconAinda não há avaliações
- Biomaterials 2010 317 1465 DorozhkinDocumento22 páginasBiomaterials 2010 317 1465 DorozhkinAdam PrasetyaAinda não há avaliações
- Calcium Silicate-Based Root Canal SealersDocumento21 páginasCalcium Silicate-Based Root Canal SealersdoctorlupuAinda não há avaliações
- Dental Tissue Remineralization by Bioactive Calcium Phosphate Nanoparticles FormulationsDocumento16 páginasDental Tissue Remineralization by Bioactive Calcium Phosphate Nanoparticles FormulationsJade SanchezAinda não há avaliações
- Fibrous Silica-Hydroxyapatite Composite by ElectrospinningDocumento10 páginasFibrous Silica-Hydroxyapatite Composite by ElectrospinningareliAinda não há avaliações
- Vitreous Sio - Cao Coatings On Ti6Al4V Alloys: Reactivity in Simulated Body Uid Versus Osteoblast Cell CultureDocumento11 páginasVitreous Sio - Cao Coatings On Ti6Al4V Alloys: Reactivity in Simulated Body Uid Versus Osteoblast Cell CultureMario Misael Machado LòpezAinda não há avaliações
- Review Article Poly (Vinyl Alcohol) Hydrogels: The Old and New Functional MaterialsDocumento16 páginasReview Article Poly (Vinyl Alcohol) Hydrogels: The Old and New Functional MaterialsEngineer SohaibAinda não há avaliações
- A Review of Glass-Ionomers: From Conventional Glass-Ionomer To Bioactive Glass-IonomerDocumento23 páginasA Review of Glass-Ionomers: From Conventional Glass-Ionomer To Bioactive Glass-IonomerRodica IlincaAinda não há avaliações
- Bioactive Glass-Published ArticleDocumento4 páginasBioactive Glass-Published ArticleSara Loureiro da LuzAinda não há avaliações
- Phil. Trans. R. Soc. A-2012-Cerruti-1281-312 Silicate BioceramicaDocumento33 páginasPhil. Trans. R. Soc. A-2012-Cerruti-1281-312 Silicate BioceramicaMurillo MarcosAinda não há avaliações
- 291-Article Text-841-3-10-20191219Documento10 páginas291-Article Text-841-3-10-20191219UMT JournalsAinda não há avaliações
- Minerals 11 01028 v4Documento12 páginasMinerals 11 01028 v4sivaAinda não há avaliações
- Evolving Application of Biomimetic Nanostructured HydroxyapatiteDocumento20 páginasEvolving Application of Biomimetic Nanostructured HydroxyapatiteVishvanth SaravanakumarAinda não há avaliações
- Processing and Properties of Hydroxyapatite-Based Biomaterials For Use As Hard Tissue Replacement ImplantsDocumento24 páginasProcessing and Properties of Hydroxyapatite-Based Biomaterials For Use As Hard Tissue Replacement ImplantsValeAinda não há avaliações
- 1 s2.0 S0144861716303940 MainDocumento8 páginas1 s2.0 S0144861716303940 MainIbnu SalehAinda não há avaliações
- Journal of Asian Ceramic Societies: Sanjaya Kumar Swain, Debasish SarkarDocumento7 páginasJournal of Asian Ceramic Societies: Sanjaya Kumar Swain, Debasish SarkarAngga SaputraAinda não há avaliações
- In Vitro New Biopolymer For Bone Grafting and Bone Cement: April 2015Documento11 páginasIn Vitro New Biopolymer For Bone Grafting and Bone Cement: April 2015Jonathan RoaAinda não há avaliações
- Diamond As A Scaffold For Bone Growth: Please Do Not Remove This PageDocumento23 páginasDiamond As A Scaffold For Bone Growth: Please Do Not Remove This PageSozharajan BAinda não há avaliações
- In Situ Forming Hydrogels Based On Chitosan ForDocumento11 páginasIn Situ Forming Hydrogels Based On Chitosan ForЕгор ЛетовAinda não há avaliações
- Nanomaterials 14 00274 v2Documento26 páginasNanomaterials 14 00274 v2Jose Manuel Quintero RomeroAinda não há avaliações
- Development of Glass Ionomer Cement Modified With Seashell Powder As A Scaffold Material For Bone FormationDocumento5 páginasDevelopment of Glass Ionomer Cement Modified With Seashell Powder As A Scaffold Material For Bone Formationsiraj_khan_13Ainda não há avaliações
- Research PaperDocumento8 páginasResearch PaperRajesh PuniaAinda não há avaliações
- Testing Facilities Tribology Lab and Metrology Lab in Department of Mechanical EnggDocumento1 páginaTesting Facilities Tribology Lab and Metrology Lab in Department of Mechanical EnggRajesh PuniaAinda não há avaliações
- 16 5 201916may2019121243 PDFDocumento1 página16 5 201916may2019121243 PDFRajesh PuniaAinda não há avaliações
- FT IRAnalysisofMaterialsDocumento50 páginasFT IRAnalysisofMaterialsRajesh PuniaAinda não há avaliações
- Advertisement: Dr. Ambedkar Medhavi Chhattar YojnaDocumento1 páginaAdvertisement: Dr. Ambedkar Medhavi Chhattar YojnaRajesh PuniaAinda não há avaliações
- Aarti SangrhDocumento33 páginasAarti SangrhRajesh PuniaAinda não há avaliações
- Aboudzadeh 2010Documento9 páginasAboudzadeh 2010Rajesh PuniaAinda não há avaliações
- IJCS 18 36 - GhorbaniDocumento13 páginasIJCS 18 36 - GhorbaniRajesh PuniaAinda não há avaliações
- Teqip - IiiDocumento33 páginasTeqip - IiiRajesh PuniaAinda não há avaliações
- 10 - Chapter 5 PDFDocumento10 páginas10 - Chapter 5 PDFAnonymous zsxsPPEAinda não há avaliações
- Final 00387Documento4 páginasFinal 00387Rajesh PuniaAinda não há avaliações
- IJCS 18 36 - GhorbaniDocumento13 páginasIJCS 18 36 - GhorbaniRajesh PuniaAinda não há avaliações
- Ganita Darshan 1Documento4 páginasGanita Darshan 1Rajesh PuniaAinda não há avaliações
- Ant Colony OptimizationDocumento24 páginasAnt Colony OptimizationRajesh PuniaAinda não há avaliações
- Latex Quickguide PDFDocumento2 páginasLatex Quickguide PDFMalkavian KhaozAinda não há avaliações
- Jobs/Methods Utilized Under TEM/ Sem / Iem: Levy Charges For Different Facilities Provided atDocumento1 páginaJobs/Methods Utilized Under TEM/ Sem / Iem: Levy Charges For Different Facilities Provided atRajesh PuniaAinda não há avaliações
- Haryana Government Employee Holidays List 2019Documento3 páginasHaryana Government Employee Holidays List 2019Renuka SharmaAinda não há avaliações
- Sarkar 2016Documento4 páginasSarkar 2016Rajesh PuniaAinda não há avaliações
- IJCS 18 36 - GhorbaniDocumento13 páginasIJCS 18 36 - GhorbaniRajesh PuniaAinda não há avaliações
- Materials 11 00870Documento9 páginasMaterials 11 00870Rajesh PuniaAinda não há avaliações
- Lec 27Documento9 páginasLec 27Rajesh PuniaAinda não há avaliações
- Fischer 2002Documento8 páginasFischer 2002Rajesh PuniaAinda não há avaliações
- Welding MetallurgyDocumento37 páginasWelding Metallurgyhemant1886100% (4)
- Castanal 2Documento106 páginasCastanal 2Rajesh PuniaAinda não há avaliações
- (WWW - Entrance-Exam - Net) - PTU M.tech in Production Engineering Metal Casting Sample Paper 1Documento2 páginas(WWW - Entrance-Exam - Net) - PTU M.tech in Production Engineering Metal Casting Sample Paper 1Sreekumar RajendrababuAinda não há avaliações
- Lec 25Documento9 páginasLec 25Rajesh PuniaAinda não há avaliações
- Analysis of Controlled Air Cooling For Castings by Experiment and Simulation - Foundry-PlanetDocumento16 páginasAnalysis of Controlled Air Cooling For Castings by Experiment and Simulation - Foundry-PlanetRajesh PuniaAinda não há avaliações
- 166 Foundry Technology: Figure 3.43 Typical Architecture of A ComprehensiveDocumento3 páginas166 Foundry Technology: Figure 3.43 Typical Architecture of A ComprehensiveRajesh PuniaAinda não há avaliações
- ISFM 2018 BrochureDocumento5 páginasISFM 2018 BrochureRajesh PuniaAinda não há avaliações
- Lenovo S340-15iwl Compal LA-H101P SchematicDocumento53 páginasLenovo S340-15iwl Compal LA-H101P SchematicYetawa Guaviare100% (4)
- Evaluating Websites A Checklist - JOHN CARLO G. GAERLANDocumento3 páginasEvaluating Websites A Checklist - JOHN CARLO G. GAERLANMarvin CincoAinda não há avaliações
- Chapter 3.seed CertificationDocumento9 páginasChapter 3.seed Certificationalemneh bayehAinda não há avaliações
- Standalone Financial Results, Limited Review Report For December 31, 2016 (Result)Documento4 páginasStandalone Financial Results, Limited Review Report For December 31, 2016 (Result)Shyam SunderAinda não há avaliações
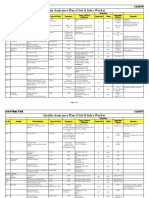
- Quality Assurance Plan - CivilDocumento11 páginasQuality Assurance Plan - CivilDeviPrasadNathAinda não há avaliações
- Body Temperature PDFDocumento56 páginasBody Temperature PDFBanupriya-Ainda não há avaliações
- PC300-8 New ModelDocumento22 páginasPC300-8 New Modeljacklyn ade putra100% (2)
- KPJ Healthcare Berhad (NUS ANalyst)Documento11 páginasKPJ Healthcare Berhad (NUS ANalyst)noniemoklasAinda não há avaliações
- Aluminium PasteDocumento11 páginasAluminium PasteGovindanayagi PattabiramanAinda não há avaliações
- Integrated Management System 2016Documento16 páginasIntegrated Management System 2016Mohamed HamedAinda não há avaliações
- 1 s2.0 S0378432004002465 MainDocumento20 páginas1 s2.0 S0378432004002465 MainMuhammad JameelAinda não há avaliações
- Reviewer CSCDocumento22 páginasReviewer CSCChristopher CocalAinda não há avaliações
- How Do I Predict Event Timing Saturn Nakshatra PDFDocumento5 páginasHow Do I Predict Event Timing Saturn Nakshatra PDFpiyushAinda não há avaliações
- Đề Anh DHBB K10 (15-16) CBNDocumento17 páginasĐề Anh DHBB K10 (15-16) CBNThân Hoàng Minh0% (1)
- Theory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)Documento15 páginasTheory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)International Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Project Success - Stakeholders 1 PDFDocumento7 páginasProject Success - Stakeholders 1 PDFMoataz SadaqahAinda não há avaliações
- 4.9 Design of Compression Members: L 4.7 UsingDocumento22 páginas4.9 Design of Compression Members: L 4.7 Usingctc1212100% (1)
- Old Man and The SeaDocumento10 páginasOld Man and The SeaXain RanaAinda não há avaliações
- Unix SapDocumento4 páginasUnix SapsatyavaninaiduAinda não há avaliações
- Embedded System Lab ManualDocumento67 páginasEmbedded System Lab Manualsaim100% (1)
- IRJ November 2021Documento44 páginasIRJ November 2021sigma gaya100% (1)
- Photoshoot Plan SheetDocumento1 páginaPhotoshoot Plan Sheetapi-265375120Ainda não há avaliações
- Diagnostic Test Everybody Up 5, 2020Documento2 páginasDiagnostic Test Everybody Up 5, 2020George Paz0% (1)
- SSC 211 ED Activity 4.1Documento4 páginasSSC 211 ED Activity 4.1bernard bulloAinda não há avaliações
- Characteristics: Our in Vitro IdentityDocumento4 páginasCharacteristics: Our in Vitro IdentityMohammed ArifAinda não há avaliações
- Module 17 Building and Enhancing New Literacies Across The Curriculum BADARANDocumento10 páginasModule 17 Building and Enhancing New Literacies Across The Curriculum BADARANLance AustriaAinda não há avaliações
- Evidence Based Practice in Nursing Healthcare A Guide To Best Practice 3rd Edition Ebook PDFDocumento62 páginasEvidence Based Practice in Nursing Healthcare A Guide To Best Practice 3rd Edition Ebook PDFwilliam.tavares69198% (50)
- LCP-027 VectraLCPDesignGuideTG AM 0613Documento80 páginasLCP-027 VectraLCPDesignGuideTG AM 0613Evert100% (1)
- Astm C119-16Documento8 páginasAstm C119-16Manuel Antonio Santos Vargas100% (2)
- EQUIP9-Operations-Use Case ChallengeDocumento6 páginasEQUIP9-Operations-Use Case ChallengeTushar ChaudhariAinda não há avaliações