Escolar Documentos
Profissional Documentos
Cultura Documentos
Gentamicin-Collagen Sponge For Infection Prophylaxis in Colorectal Surgery
Enviado por
Nurul ImaniarTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Gentamicin-Collagen Sponge For Infection Prophylaxis in Colorectal Surgery
Enviado por
Nurul ImaniarDireitos autorais:
Formatos disponíveis
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Gentamicin–Collagen Sponge for Infection
Prophylaxis in Colorectal Surgery
Elliott Bennett-Guerrero, M.D., Theodore N. Pappas, M.D.,
Walter A. Koltun, M.D., James W. Fleshman, M.D., Min Lin, Ph.D.,
Jyotsna Garg, M.S., Daniel B. Mark, M.D., M.P.H., Jorge E. Marcet, M.D.,
Feza H. Remzi, M.D., Virgilio V. George, M.D., Kerstin Newland, R.N.,
and G.R. Corey, M.D., for the SWIPE 2 Trial Group*
A BS T R AC T
BACKGROUND
From the Duke Clinical Research Institute Despite the routine use of prophylactic systemic antibiotics, surgical-site infection
(E.B.-G., M.L., J.G., D.B.M., K.N., G.R.C.) continues to be associated with significant morbidity and cost after colorectal sur-
and the Duke University Department of
Surgery (T.N.P.), Duke University Medi- gery. The gentamicin–collagen sponge, an implantable topical antibiotic agent, is
cal Center, Durham, NC; the Milton S. approved for surgical implantation in 54 countries. Since 1985, more than 1 million
Hershey Medical Center, Penn State Col- patients have been treated with the sponges.
lege of Medicine, Hershey, PA (W.A.K.);
Washington University School of Medi-
cine, St. Louis (J.W.F.); University of South METHODS
Florida, Tampa (J.E.M.); Cleveland Clinic, In a phase 3 trial, we randomly assigned 602 patients undergoing open or laparo-
Cleveland (F.H.R.); and Indiana Univer
sity School of Medicine, Indianapolis
scopically assisted colorectal surgery at 39 U.S. sites to undergo either the insertion
(V.V.G.). Address reprint requests to Dr. of two gentamicin–collagen sponges above the fascia at the time of surgical closure
Bennett-Guerrero at the Duke Clinical (the sponge group) or no intervention (the control group). All patients received
Research Institute, Duke University Med-
ical Center, Box 3094, Durham, NC 27710,
standard care, including prophylactic systemic antibiotics. The primary end point
or at elliott.bennettguerrero@duke.edu. was surgical-site infection occurring within 60 days after surgery, as adjudicated by
a clinical-events classification committee that was unaware of the study-group as-
*Members of the Surgical Wound Infec-
tion Prevention (SWIPE) 2 Trial Group
signments.
are listed in the Appendix.
RESULTS
This article (10.1056/NEJMoa1000837) was The incidence of surgical-site infection was higher in the sponge group (90 of 300
published on August 4, 2010, and last up-
dated on December 22, 2010, at NEJM.org. patients [30.0%]) than in the control group (63 of 302 patients [20.9%], P = 0.01).
Superficial surgical-site infection occurred in 20.3% of patients in the sponge group
N Engl J Med 2010;363:1038-49. and 13.6% of patients in the control group (P = 0.03), and deep surgical-site infec-
Copyright © 2010 Massachusetts Medical Society.
tion in 8.3% and 6.0% (P = 0.26), respectively. Patients in the sponge group were
more likely to visit an emergency room or surgeon’s office owing to a wound-related
sign or symptom (19.7%, vs. 11.0% in the control group; P = 0.004) and to be re-
hospitalized for surgical-site infection (7.0% vs. 4.3%, P = 0.15). The frequency of
adverse events did not differ significantly between the two groups.
CONCLUSIONS
Our large, multicenter trial shows that the gentamicin–collagen sponge is not ef-
fective at preventing surgical-site infection in patients who undergo colorectal sur-
gery; paradoxically, it appears to result in significantly more surgical-site infections.
(Funded by Innocoll Technologies; ClinicalTrials.gov number, NCT00600925.)
1038 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
P
ostoperative surgical-site infection Duke University coauthors wrote the study proto-
continues to be a significant problem after col, gathered and analyzed the data, vouch for the
general surgical procedures, especially co accuracy and integrity of the data and analysis,
lorectal surgery. Reported incidences of surgical- and wrote the manuscript. Institutional review
site infection among patients who undergo co boards at participating institutions approved the
lorectal surgery range from 8.2%1 to 26%,2 with study protocol, and the study was performed in
an incidence of approximately 18 to 20% in most accordance with it.
series.3-7 Postoperative surgical-site infection is
associated with a significant rate of complica- Patients
tions and cost.8-10 Thus, prevention of these fre- All patients provided written informed consent.
quent infections has been the focus of numerous A complete list of inclusion and exclusion crite-
strategies.2-7,11 ria, along with a detailed list of the surgical pro-
The gentamicin–collagen sponge was devel- cedures, is provided in the Supplementary Ap-
oped to prevent and treat wound infections by pendix, available with the full text of this article
providing high gentamicin concentrations lo- at NEJM.org. Inclusion criteria were an age of 18
cally, avoiding the high systemic concentrations years or older and having 1 of 13 types of colo
associated with nephrotoxicity. The sponge’s col- rectal surgery scheduled. Laparoscopically as-
lagen matrix biodegrades and disappears within sisted procedures requiring an incision of at least
days to weeks. Pharmacokinetic data show that 7 cm were allowed, a length that is consistent
implantation of one to five sponges (correspond- with the use of a laparotomy “hand port” in many
ing to a gentamicin dose of 130 to 650 mg) re- so-called laparoscopic colorectal procedures. Ex-
sulted in local-tissue gentamicin concentrations clusion criteria included the presence of a clini-
of 170 to 9000 μg per milliliter. These concen- cally significant concomitant surgical procedure,
trations exceed the minimum inhibitory concen- use of a laparoscopic or other minimally invasive
trations for many microorganisms. Systemic con- surgical approach involving a laparotomy inci-
centrations of gentamicin, however, remained sion shorter than 7 cm, laparotomy within the
below 2 μg per milliliter 24 hours after implan- 60-day period before the screening visit or a
tation.12 planned second laparotomy within the 60-day
The sponge received marketing approval in period after surgery, and a situation in which it
Germany in 1985 and is currently approved for was technically impossible to insert two sponges
use in another 53 countries. Since 1985, more above the fascia.
than 2 million sponges manufactured by Innocoll
Technologies (Gallowston, Ireland) have been Study Procedure
used to treat more than 1 million patients across Study Treatment and Randomization
a broad range of clinical indications. Several Each sponge (10 by 10 cm) contained 280 mg of
studies suggest that the sponge may be effective collagen and 130 mg of gentamicin. In patients
in the prevention and treatment of infections who were randomly assigned to receive a sponge,
after general surgery.6,13,14 In a single-center,two sponges were inserted anteriorly to the fas-
randomized trial, patients who underwent colo cia, along the full length of the incision, imme-
rectal surgery and received a sponge had a 70% diately before closure of the surgical wound. To
decrease in surgical-site infection, as compared facilitate placement in the wound, the sponges
with those who did not receive a sponge.6 The could be cut into strips while dry. No sponges
current phase 3 trial was designed to confirm were placed in control patients. Patients in the
these promising data and support regulatory ap- sponge group in whom reexploration of the sur-
proval in the United States. gical site was necessary within 1 week after the
first surgery had two new sponges inserted at the
Me thods time of closure. All participating surgeons un-
derwent a training and certification process that
study oversight included the viewing of a video outlining proper
Patients were enrolled at 39 sites in the United use of the study sponge.
States. The study was coordinated by the Duke Randomization occurred after the surgical
Clinical Research Institute (DCRI). The DCRI– incision had been made, with the use of a cen-
n engl j med 363;11 nejm.org september 9, 2010 1039
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
tral randomization system. Control patients did infection, including use of antibiotics, drainage of
not receive a placebo sponge (a sponge contain- pus under local anesthesia, wound débridement
ing collagen but not gentamicin), since bacteria under general anesthesia, isolation of bacteria,
might have grown on a sponge that did not con- prolonged postoperative hospitalization, and find-
tain the antibiotic. Therefore, surgeons could ings on daily examination of the wound.4,17,18 The
not be unaware of the study-group assignments, minimum score is 0, and there is no theoretical
but patients and members of the adjudication maximum score; higher scores indicate a worse
committee did remain unaware. infection. We assessed the change in the serum
creatinine level from baseline, reporting the peak
Administration of Antibiotics and Bowel level during the first 7-day postoperative period or
Preparation the period until hospital discharge if discharge
In accordance with published guidelines,15 the occurred before day 7. Patients assessed their pain
protocol called for initiation of one of the follow- and wound healing according to a structured
ing antibiotic regimens within 60 minutes before questionnaire administered 30 and 60 days after
incision: cefazolin plus metronidazole, cefoxitin, surgery. Data were recorded for death from any
or ciprofloxacin plus clindamycin or metronida- cause at 60 days, visits to the emergency depart-
zole. Dosing was based on body weight, and the ment or surgical office in association with wound-
drugs were not to be continued for more than 24 related signs or symptoms, rehospitalization for
hours after surgery. Preoperative oral antibiotics surgical-site infection, and serum gentamicin lev-
were not required but could be added to the sys- els at several sites. Blood samples were obtained at
temic antibiotic prophylaxis: oral neomycin plus baseline (after incision) and then at 2±0.5, 6±0.5,
oral erythromycin or oral neomycin plus oral 12±1, 24±2, and 48±2 hours after surgical-wound
metronidazole.15 The use of topical antibiotics, closure for the determination of serum gentami-
other than the gentamicin in the sponge, was cin levels.
prohibited in patients randomly assigned to re-
ceive the sponge. At least one of the following Clinical Events Committee
bowel-preparation regimens was required: use of The independent clinical events committee con-
a laxative (polyethylene glycol, sodium phosphate, sisted of three independent infectious disease ex-
or a magnesium citrate–based regimen) or a high- perts who were unaware of the study-group as-
volume enema. signments. All suspected wound-infection events
were reviewed independently by two of the three
Data Collection experts. Cases for which the two experts dis-
Standard preoperative demographic and intraop- agreed were reviewed by the third expert. Possi-
erative characteristics were recorded, and we also ble wound infections were identified by events
collected data on variables suspected to play a including signs of infection, administration of
role in surgical-site infection. The risk of infec- postoperative antibiotics, rehospitalization, and
tion was assessed with the use of the National death. After review of blinded medical rec
Nosocomial Infection Surveillance System.4,16 ords,4,17,18 the committee ascertained the pres-
ence or absence, extent, and severity of all infec-
Primary and Secondary End Points tions according to standardized criteria, including
The primary study end point was surgical-site in- those from the Centers for Disease Control and
fection within the laparotomy wound during the Prevention4,16,17,19 and Itani and colleagues2: super
period from surgery through postoperative day 60. ficial infections that involved the skin and super
Key secondary efficacy end points included the in- ficial fat but did not threaten the fascia, deep
cidence of deep surgical-site infections, superficial infections involving deeper soft tissue of the inci-
surgical-site infections, surgically treated surgical- sion and potentially threatening the fascia, and
site infections (defined as infection treated with organ-space infections below the fascia (which
any type of surgical intervention, including open- are usually manifested as abscess). Data for in-
ing of the wound), postoperative hospital length fections not considered to be related to laparotomy
of stay, and ASEPSIS score through 60 days after (e.g., perineal-incision infection, peristomal in-
colorectal surgery.4,17,18 The validated ASEPSIS fection, infection at the intravenous catheter site,
score assigns points for nine variables related to or pneumonia) were not included in the analysis.
1040 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
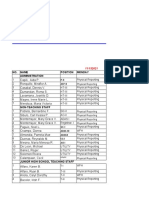
674 Patients were enrolled
72 Were excluded
54 Had a planned change in surgery or no
longer met eligibility criteria
7 Withdrew consent
6 Were enrolled but not studied because
trial sample size was reached
4 Had an unknown reason
1 Was withdrawn by investigator
602 Underwent randomization
300 Were assigned to receive gentamicin– 302 Were assigned not to receive
collagen sponges sponges (control)
281 Received 2 sponges 302 Received assigned intervention
15 Received only 1 sponge
4 Did not receive a sponge
5 Were lost to follow-up
3 Were lost to follow-up
300 Had data included in the intention- 302 Had data included in the intention-
to-treat analysis to-treat analysis
26 Were excluded from the per- 10 Were excluded from the per-
protocol analysis protocol analysis because
7 Did not meet eligibility criteria eligibility criteria were not met
15 Received only 1 sponge
4 Did not receive a sponge
Figure 1. Enrollment, Randomization, and Follow-up of the Patients, According to Study Group.
Statistical Analysis site interaction. In all secondary efficacy and sub
All analyses were performed by the statistical group analyses, a nominal two-sided P value of
team at the DCRI. Calculations during the plan- less than 0.05 was considered to indicate statis-
ning phase indicated that enrollment of 592 pa- tical significance, and the results were consid-
tients (296 per study group) would be required to ered to be descriptive.
detect a 50% relative reduction in the incidence Descriptive statistical comparisons between
of surgical-site infection in the sponge group as the two study groups were performed with the
compared with the control group, with a power of use of chi-square tests or Fisher’s exact test, as
at least 85% and a two-sided type I error rate of appropriate, for categorical secondary efficacy
0.05. On the basis of previous trials, we assumed end points and with the use of analysis-of-vari-
a 16% incidence of surgical-site infection. ance techniques or Wilcoxon rank-sum tests, as
The primary analysis was based on intention- appropriate, for continuous secondary efficacy
to-treat methods. We also performed a per-proto- end points. The log-rank tests were used to com-
col analysis, as a prespecified secondary analy- pare the time to first surgical-site infection be-
sis, which included all patients who completed tween two study groups. Kaplan–Meier survival
the study and had no major deviations from the estimates of the time to first surgical-site infec-
prespecified protocol. We compared the primary tion were also calculated.
end point between the two study groups by means No formal interim analysis was planned. An
of a two-sided chi-square test involving data independent data and safety monitoring com-
across all sites, after checking the treatment-by- mittee monitored the trial on an ongoing basis.
n engl j med 363;11 nejm.org september 9, 2010 1041
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
All statistical analyses were performed with the section primarily for colon or rectal carcinoma
use of SAS software (version 9.2). (in 307 of 602 patients [51.0%]) or diverticulitis
or inflammatory bowel disease (217 of 602 pa-
R e sult s tients [36.0%]). The study groups were balanced
with regard to baseline characteristics (Table 1)
Overall, 602 patients were enrolled at 39 U.S. as well as surgical preparation and intraopera-
sites between February 2008 and March 2009 tive characteristics (Table 2). Laparoscopically
(Fig. 1). Of the 300 patients randomly assigned to assisted surgery that was not converted to an
receive two sponges, 281 (93.7%), 15 (5.0%), and open procedure was performed in 51 of the 300
4 (1.3%) received two, one, and no sponges, re- patients (17.0%) in the sponge group and 58 of
spectively. A total of 8 of the 602 patients (1.3%; the 302 patients (19.2%) in the control group.
3 in the sponge group and 5 in the control group) Adjudicated surgical-site infection was more
were lost to follow-up at day 60. likely to occur in association with open surgery
Patients in both groups underwent bowel re- (139 of 493 patients [28.2%]) than with laparo-
Table 1. Baseline Characteristics of the Patients, According to Study Group.*
Gentamicin–Collagen Control
Characteristic Sponge (N = 300) (N = 302)
Age — yr
Median 57.8 58.0
IQR 45.5–67.7 47.4–67.0
White race — no. (%)† 272 (90.7) 273 (90.4)
American Society of Anesthesiologists score of 3 or 4 — no. (%)‡ 132 (44.0) 126 (41.7)
Weight — kg
Median 79.5 80.0
IQR 67.9–93.0 69.4–93.2
Body-mass index§
Median 26.8 27.2
IQR 23.8–30.8 24.0–30.8
Waist circumference — cm
Median 96.0 96.5
IQR 86.0–106.7 86.4–106.7
Male sex — no. (%) 181 (60.3) 158 (52.3)
Hypertension — no. (%) 140 (46.7) 122 (40.4)
Diabetes — no. (%) 37 (12.3) 47 (15.6)
Smoking status — no. (%)
Current or previous 142 (47.3) 147 (48.7)
Current 47 (15.7) 46 (15.2)
Chronic obstructive pulmonary disease — no. (%) 17 (5.7) 12 (4.0)
Peripheral vascular disease — no. (%) 12 (4.0) 13 (4.3)
Previous laparotomy — no./total no. (%) 131/300 (43.7) 124/301 (41.2)
Previous radiation to abdomen — no. (%) 42 (14.0) 45 (14.9)
Chemotherapy within 6 wk before surgery — no. (%) 22 (7.3) 17 (5.6)
Corticosteroid use within 1 mo before surgery — no. (%) 25 (8.3) 17 (5.6)
History of abdominal fistula — no. (%) 10 (3.3) 10 (3.3)
Renal insufficiency — no. (%)¶ 5 (1.7) 5 (1.7)
1042 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
Table 1. (Continued.)
Gentamicin–Collagen Control
Characteristic Sponge (N=300) (N=302)
Preoperative laboratory values
Serum albumin — g/dl
Median 4.0 4.0
IQR 3.6–4.3 3.7–4.4
Serum glucose — mg/dl
Median 99 96
IQR 89–111 89–109
Serum glycated hemoglobin — %
Median 5.5 5.6
IQR 5.2–6.0 5.3–6.0
Hematocrit — %
Median 39.0 40.0
IQR 36.0–42.5 36.0–43.0
Serum creatinine — mg/dl
Median 0.9 0.9
IQR 0.8–1.1 0.8–1.0
Preoperative core temperature — °C
Median 97.7 97.7
IQR 97.0–98.2 97.0–98.2
Preoperative hospital stay — days
Median 0.0 0.0
IQR 0.0–0.0 0.0–0.0
NNISS score — no. (%)‖
0 32 (10.7) 38 (12.6)
1 166 (55.3) 159 (52.6)
2 102 (34.0) 105 (34.8)
3 0 0
* To convert the values for glucose to millimoles per liter, multiply by 0.05551. To convert the values for creatinine to
micromoles per liter, multiply by 88.4. IQR denotes interquartile range.
† Race was self-reported.
‡ The American Society of Anesthesiologists physical status classification score can range from 0 to 6, with higher scores
representing a worse condition. A score of 3 or 4 represents severe systemic disease.
§ The body-mass index is the weight in kilograms divided by the square of the height in meters.
¶ Renal insufficiency was defined as a preoperative serum creatinine level of 2.5 mg per deciliter (221 μmol per liter) or
more.
‖ The National Nosocomial Infection Surveillance System (NNISS) score can range from 0 to 3 points, with a higher
score representing a higher risk of infection. One point is awarded for an American Society of Anesthesiologists physi-
cal status classification score of 3 or more, one point is awarded for a contaminated or nonsterile operation, and one
point is awarded for a duration of surgery of more than 2 hours.
scopically assisted surgery (14 of 109 patients ble 3). The incidence of superficial surgical-site
[12.8%]). infection was 20.3% in the sponge group, versus
In the primary analysis, surgical-site infec- 13.6% in the control group, and the incidence of
tions occurred more frequently in the sponge deep surgical-site infections was 8.3% versus
group (90 of 300 patients [30.0%]) than in the 6.0%. Patients in the sponge group were more
control group (63 of 302 [20.9%]) (P = 0.01) (Ta- likely than those in the control group to visit an
n engl j med 363;11 nejm.org september 9, 2010 1043
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 2. Characteristics of Surgical Preparation and Procedure, According to Study Group.*
Gentamicin–Collagen Control
Characteristic Sponge (N = 300) (N = 302)
Oral antibiotics administered preoperatively — no. (%) 44 (14.7) 38 (12.6)
Preoperative bowel preparation — no. (%)
Laxative use and complete bowel preparation 273 (91.0) 277 (91.7)
Enema 4 (1.3) 5 (1.7)
Other 9 (3.0) 12 (4.0)
None 17 (5.7) 16 (5.3)
Preoperative shower with chlorhexidine soap — no. (%) 39 (13.0) 44 (14.6)
Hair at operative site not removed — no./total no. (%) 61/299 (20.4) 82/302 (27.2)
Preincision skin preparation — no. (%)
With povidone–iodine 220 (73.3) 220 (72.8)
With alcohol 42 (14.0) 42 (13.9)
With chlorhexidine-based agent 110 (36.7) 117 (38.7)
IV antibiotics administered within 60 min before incision 284 (94.7) 289 (95.7)
Antibiotic administered before incision — no. (%)
Aztreonam 0 1 (0.3)
Cefotetan 4 (1.3) 2 (0.7)
Cefazolin 89 (29.7) 92 (30.5)
Cefoxitin 111 (37.0) 105 (34.8)
Clindamycin 6 (2.0) 6 (2.0)
Ciprofloxacin 83 (27.7) 88 (29.1)
Metronidazole 173 (57.7) 182 (60.3)
Other 6 (2.0) 8 (2.6)
Prophylactic IV antibiotics discontinued within 24 hr after incision — 262/296 (88.5) 267/301 (88.7)
no./total no. (%)
Surgical procedure performed — no. (%)
Left hemicolectomy 17 (5.7) 21 (7.0)
Transverse colectomy 12 (4.0) 11 (3.6)
Segmental (sleeve) left colon resection 1 (0.3) 6 (2.0)
Total abdominal colectomy with ileorectal anastomosis 12 (4.0) 14 (4.6)
Total abdominal colectomy with ileostomy 18 (6.0) 15 (5.0)
Total abdominal proctocolectomy 23 (7.7) 15 (5.0)
Low anterior resection 77 (25.7) 105 (34.8)
Sigmoid resection 65 (21.7) 60 (19.9)
Nonemergency Hartman’s procedure 7 (2.3) 4 (1.3)
Colotomy with polypectomy distal to hepatic flexure 0 1 (0.3)
Colostomy takedown through laparotomy incision 21 (7.0) 15 (5.0)
Ileal pouch anal anastomosis with or without stoma 40 (13.3) 29 (9.6)
Abdominal–perineal resection of the rectum 22 (7.3) 16 (5.3)
Other 7 (2.3) 11 (3.6)
Laparoscopically assisted surgery† 51 (17.0) 58 (19.2)
1044 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
Table 2. (Continued.)
Gentamicin–Collagen Control
Characteristic Sponge (N = 300) (N = 302)
Laparotomy incision length — cm
Median 16.0 14.0
IQR 9.3–23.0 9.0–20.0
Method to close laparotomy incision — no. (%)
Staples 239 (79.7) 219 (72.5)
Sutures 68 (22.7) 88 (29.1)
Glue 3 (1.0) 5 (1.7)
Duration of surgery — hr
Median 2.8 2.9
IQR 2.1–4.0 2.2–3.7
Abdominal surgical drain inserted — no. (%) 111 (37.0) 113 (37.4)
Crystalloid volume administered intraoperatively — liters
Median 3.0 3.0
IQR 2.3–4.0 2.4–4.0
Colloid volume administered intraoperatively — liters
Median 0.0 0.0
IQR 0.0–0.5 0.0–0.5
Nitrous oxide used — no. (%) 33 (11.0) 18 (6.0)
FiO2 during surgery — %
Lowest value
Median 53 52
IQR 46–70 47–65
Estimated average value
Median 60 60
IQR 54–87 52–77
Administered any dexamethasone in perioperative period — no. (%) 31 (10.3) 41 (13.6)
Peak serum glucose in first 24 hr after surgery — mg/dl
Median 140 142
IQR 119–167 116–173
Perioperative allogeneic red-cell transfusion — no. (%) 48 (16.0) 56 (18.5)
Core temperature at end of surgery — °C
Median 36.5 36.4
IQR 36.2–36.8 36.2–36.8
Core temperature at end of surgery ≥36°C — no./total no. (%) 264/297 (88.9) 250/297 (84.2)
* To convert the values for glucose to millimoles per liter, multiply by 0.05551. FiO2 denotes fraction of inspired oxygen,
IQR interquartile range, and IV intravenous.
† Laparoscopically assisted surgery did not include procedures in which the laparoscopic approach was abandoned
(i.e., conversion to open laparotomy).
n engl j med 363;11 nejm.org september 9, 2010 1045
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
emergency department or surgical office with a Given the increase in surgical-site infection
wound-related sign or symptom (19.7 vs. 11.0%, observed with the gentamicin–collagen sponge,
P = 0.004); rehospitalization for surgical-site in- a post hoc analysis was performed to investigate
fection occurred in 7.0% of patients in the sponge a possible mechanism for this effect. We specu-
group and 4.3% of patients in the control group lated that the presence of sponge mass (assum-
(P = 0.15). Times to surgical-site infection are ing two sponges were placed) may have been a
shown in Figure 2. mechanical barrier to early wound healing that
The frequency of adjudicated surgical-site in- promoted infection. However, no clear associa-
fection was 44.7% (134 of 300 patients) in the tion was seen between surgical-site infection and
sponge group, versus 34.4% (104 of 302 patients) incision length, waist circumference, or body-
in the control group, as assessed by the site in- mass index according to study group (results not
vestigators (which is similar to results on the basis shown). In addition, there was no overt differ-
of assessment by the clinical events committee). ence in the degree of wound healing between
Analyses performed in the per-protocol population the two groups at 30 or 60 days, on the basis
of 566 patients yielded results similar to those of data from a structured patient questionnaire
for the intention-to-treat population (Table 3). (Table 4 in the Supplementary Appendix).
Among patients in the per-protocol popula-
tion with adjudicated surgical-site infection, po- Discussion
tential pathogens were isolated in samples from
44 patients in the sponge group and 28 patients The gentamicin–collagen sponge, developed to
in the control group (Table 1 in the Supplemen- deliver a high local and wound concentration of
tary Appendix). The organisms found to be most gentamicin, has undergone testing throughout
frequently resistant to gentamicin include Entero- northern Europe. For example, a single-center,
coccus faecalis (in 3 of 9 isolates), Enterococcus faecium nonblinded study involving 221 patients under-
(1 of 3 isolates), Escherichia coli (1 of 9 isolates), going colorectal surgery showed a 70% relative
Proteus mirabilis (1 of 5 isolates), and Staphylococcus reduction of the incidence of surgical-site infec-
epidermidis (9 of 12 isolates) (Table 2 in the Sup- tion with the use of the sponge (18.4%, vs. 5.6%
plementary Appendix). All but 2 of the 15 resis- with no sponge; P<0.01).6 These results served as
tant isolates were cultured from patients in the strong preliminary data for our trial. However,
sponge group. the results of our large, randomized clinical trial
Peak serum gentamicin levels ranged from showed that use of the sponge, as compared with
0.9 to 4.7 μg per milliliter (mean, 2.4) and de- no sponge, did not reduce the incidence of surgi-
creased to a mean (±SD) of 0.4±0.4 μg per mil- cal-site infection in patients undergoing colo
liliter by 48 hours after sponge insertion (Fig. 1 rectal surgery. Contrary to initial expectations,
in the Supplementary Appendix). The mean per- patients randomly assigned to undergo sponge
cent increase from baseline in the peak serum placement, as compared with those who did not
creatinine level was similar in the two groups undergo sponge placement, had a higher inci-
(14.8±42.6% in the sponge group and 15.4±45.1% dence of surgical-site infection, were more likely
in the control group). to visit an emergency room or surgical office for
Eighteen patients required reexploration of a wound-related sign or symptom, and more fre-
the surgical wound: 11 patients in the sponge quently underwent rehospitalization for surgical-
group and 7 patients in the control group. Exclu- site infection. These results raise important new
sion of data from these patients from the primary questions about the best method for reducing the
analysis did not change the overall results (with risk of this important complication, which still
a rate of adjudicated surgical-site infection of affects about one in five patients undergoing colo
29.4% in the sponge group vs. 21.4% in the con- rectal surgery, despite skin decontamination
trol group, P = 0.03). Six patients had died by day and administration of systemic antibiotics.3-7
60 (1 patient in the sponge group and 5 patients Our data do not allow us to identify with
in the control group). No significant differences certainty the cause of the lack of efficacy we
were found between the two groups regarding observed. However, we can speculate that sev-
serious adverse events (Table 3 in the Supple- eral factors may have been operational. First,
mentary Appendix). though the microorganisms cultured from in-
1046 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
Table 3. Surgical-Site Infection (SSI) and Other Postoperative End Points through Postoperative Day 60, According to
Study Group.*
Gentamicin–Collagen Control
Characteristic Sponge (N = 300) (N = 302) P Value
Intention-to-treat analysis
SSI — no. of patients (%)
Any (primary end point) 90 (30.0) 63 (20.9) 0.01
Surgically treated 71 (23.7) 49 (16.2) 0.02
Superficial 61 (20.3) 41 (13.6) 0.03
Deep 25 (8.3) 18 (6.0) 0.26
Organ space 4 (1.3) 4 (1.3) 1.00
ASEPSIS score† 0.17
Median 0.0 0.0
IQR 0.0–10.0 0.0–4.0
Rehospitalization for SSI — no. of patients (%) 21 (7.0) 13 (4.3) 0.15
Visit to ER or physician for wound-related sign or symptom 57 (19.7) 31 (11.0) 0.004
— no. of patients/total no. (%)
Postoperative hospital length of stay — days 6.0 (5.0–8.0) 6.0 (4.0–8.0) 0.44
Median
IQR
Gentamicin–Collagen Control
Sponge (N = 274) (N = 292)
Per-protocol analysis
SSI — no. of patients (%)
Any (primary end point) 83 (30.3) 62 (21.2) 0.01
Surgically treated 68 (24.8) 48 (16.4) 0.01
Superficial 56 (20.4) 41 (14.0) 0.04
Deep 23 (8.4) 18 (6.2) 0.31
Organ space 4 (1.5) 3 (1.0) 0.72
ASEPSIS score† 0.19
Median 0.0 0.0
IQR 0.0–10.0 0.0–5.0
Rehospitalization for SSI — no. of patients (%) 20 (7.3) 12 (4.1) 0.10
Visit to ER or physician for wound-related sign or symptom 53/265 (20.0) 30/272 (11.0) 0.004
— no. of patients/total no. (%)
Postoperative hospital length of stay — days 0.48
Median 6.0 6.0
IQR 5.0–8.0 4.0–8.0
* ER denotes emergency room, and IQR interquartile range.
† The ASEPSIS score reflects nine variables related to the infection, including use of antibiotics, drainage of pus under lo-
cal anesthesia, wound débridement under general anesthesia, isolation of bacteria, prolonged postoperative hospital-
ization, and findings on daily examination of the wound. The minimum score is 0, and there is no theoretical maximum
score; higher scores indicate a worse infection. The mean (±SD) score was 6.1±10.4 in the sponge group and 5.2±11.0
in the control group in the intention-to-treat population and 6.0±10.2 and 5.3±11.1, respectively, in the per-protocol
population.
n engl j med 363;11 nejm.org september 9, 2010 1047
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
infection. Third, the collagen used to construct
0.5 the sponges we used could have stimulated a
deleterious local effect. An additional possibility
0.4
is that the collagen may have been a mechanical
P=0.02
barrier to rapid and effective closure of the
Probability of SSI
Gentamicin–collagen sponge wound, thus providing additional time for bacte-
0.3
rial penetration to occur. Arguing against this
hypothesis is the fact that our post hoc analyses
0.2
No sponge (control)
showed no clear association between treatment
effect and wound length or surrogates for wound
0.1 depth (waist circumference and body-mass index).
If the sponge is not effective, why did results
0.0 of an earlier study by Rutten and Nijhuis6 sug-
0 10 20 30 40 50 60
gest such a strong treatment benefit? In the
Days after Surgery previous study, the duration of follow-up was not
reported; duration could be a factor, since evi-
Figure 2. Kaplan–Meier Estimates of the Number of Days from Surgery
dence of harm became apparent in our study
to Surgical-Site Infection (SSI) within the 60-Day Postoperative Period,
According to Study Group. only 3 weeks after surgery. In addition, the pre-
vious study used a lower dose of gentamicin (one
sponge containing 130 mg of gentamicin) than
was used in our study (two sponges, each con-
fected surgical wounds were similar in distribu- taining 130 mg of gentamicin). However, it is
tion between the two study groups (Table 1 in unclear why our use of a higher dose of gen-
the Supplementary Appendix), cultures from the tamicin would yield such different results, un-
sponge group contained significantly more re- less harm was mediated by a mechanical effect
sistant bacteria than cultures from the control of the sponge. An important difference between
group. These findings may be partly explained the study by Rutten and Nijhuis and ours is that
by the results of the time-kill testing (which they did not use several quality-control measures
measures the antimicrobial activity of a drug) (e.g., verification of data from on-site monitor-
independently performed by the sponsor with ing and source documents, central adjudication
doses of 100 μg and 300 μg of gentamicin sul- of end points by an independent committee that
fate per milliliter (Prior D: personal communica- was unaware of the group assignments, and the
tion). Regrowth of S. aureus, coagulase-negative inclusion of a large number of surgical sites [1, vs.
staphylococci, and enterococcus was found at 24 39 in our study] and patients). The discrepancy
hours. These results are consistent with the con- in results may be related to the fact that findings
clusion by Tam and colleagues20 that gentamicin from positive single-center trials are often not
should be administered every 8 hours to elimi- confirmed in larger multicenter trials.22 Further-
nate staphylococci and enterococci, in contrast to more, differences among races and ethnic groups
administration every 24 hours, which is effective and among regions may have resulted in the dif-
against gram-negative bacilli. Second, gentami- ferent results between our U.S.-based trial and
cin may elute too rapidly to increase the efficacy previous studies.23
of systemic preoperative antibiotics. In support A limitation of our trial is that it was de-
of this hypothesis are data showing low wound signed to study the prevention of infection, so its
and local levels of gentamicin 12 hours after results cannot be used to address whether the
sponge insertion.21 We found what appeared to sponge is effective for the treatment of infec-
be a transient early benefit of the sponge (Fig. 2), tion.13 Another limitation of our trial is that it
with a subsequent reversal in that effect, which did not address the efficacy of sponge placement
may be consistent with the failure of the sponge below the fascia.
to provide a sustained local level of gentamicin. In conclusion, our large, multicenter trial
A sponge with depleted antibiotic levels could shows that the gentamicin–collagen sponge is
harbor bacteria and thereby increase the risk of not effective at preventing surgical-site infection
1048 n engl j med 363;11 nejm.org september 9, 2010
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Gentamicin– Collagen Sponge and Infection
in patients undergoing colorectal surgery and, Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
as compared with the placement of no sponges,
We thank the DCRI coordinating center and staff, Susan Cu-
appears to result in significantly more surgical- sack (Regulatory Affairs), and members of the data and safety
site infections. monitoring board (Daniel Sexton, M.D., chair, Jose G. Guillem,
Supported by Innocoll Technologies. M.D., and Shein Chung Chow, Ph.D.).
Appendix
Members of the SWIPE 2 trial group are as follows: R. Bailey (Methodist Hospital, Houston), C. Bellows (Tulane University Health Sci-
ence Center), S. Bergese (Ohio State University), R. Billingham (Northwest Colon and Rectal Clinic), S. Binderow (Atlanta Colon and
Rectal Surgery), J. Charchaflieh (University Hospital of Brooklyn), M. Choti (Johns Hopkins Hospital), K. Deck (Saddleback Memorial
Medical Center), N. Ellis (University of South Alabama), Y. Fayiga (University of Texas Southwestern Medical Center), P. Fleshner (Ce-
dars–Sinai Medical Center), B. Gemlo (Colon and Rectal Surgical Associates), D. Herzig (Oregon Health and Science University) N.
Hyman (University of Vermont–Fletcher Allen Health Care), A. Kaiser (University of Southern California, University Hospital), K. Kwong
(Portland Veterans Affairs Medical Center), E. Lee (Albany Medical College), N. Mahmoud (University of Pennsylvania Health System),
C. Mantyh (Duke University), M. McCarter (University of Colorado), D. Newman (Vital re:Search), E. Moore (Denver Health Medical
Center), R. Muldoon (Vanderbilt University Medical Center), V. Ohaju (St. Mary’s Duluth Clinic Health System), H. Papaconstantinou
(Scott and White Memorial), J. Rafferty (University of Cincinnati), C. Reickert (Henry Ford Hospital), M. Rodriguez-Bigas (M.D. Ander-
son Cancer Center), A. Segura-Vasi (Shoals Clinical Research Associates), A. Shelton (Stanford University Medical Center), V. Stowell
(Multicare Health System), A. Turan (University of Louisville Hospital), J. Viola (New York University Medical Center), S. Wexner (Cleve-
land Clinic), and Hongqiu Yang (Duke Clinical Research Institute).
References
1. Greif R, Akça O, Horn EP, Kurz A, pitalization, and extra costs. Infect Con- wound class, operative procedure, and pa-
Sessler DI. Supplemental perioperative trol Hosp Epidemiol 1999;20:725-30. tient risk index. Am J Med 1991;91:152S-
oxygen to reduce the incidence of surgi- 9. Walz JM, Paterson CA, Seligowski JM, 157S.
cal-wound infection. N Engl J Med 2000; Heard SO. Surgical site infection follow- 17. Wilson AP, Gibbons C, Reeves BC, et
342:161-7. ing bowel surgery: a retrospective analy- al. Surgical wound infection as a perfor-
2. Itani KM, Wilson SE, Awad SS, Jensen sis of 1446 patients. Arch Surg 2006; mance indicator: agreement of common
EH, Finn TS, Abramson MA. Ertapenem 141:1014-8. definitions of wound infection in 4773
versus cefotetan prophylaxis in elective 10. Smith RL, Bohl JK, McElearney ST, et patients. BMJ 2004;329:720.
colorectal surgery. N Engl J Med 2006; al. Wound infection after elective colorec- 18. Wilson AP, Weavill C, Burridge J,
355:2640-51. tal resection. Ann Surg 2004;239:599- Kelsey MC. The use of the wound scoring
3. Belda FJ, Aguilera L, Garcia de la 607. method ‘ASEPSIS’ in postoperative wound
Asuncion J, et al. Supplemental periopera- 11. Kurz A, Sessler DI, Lenhardt R. Peri- surveillance. J Hosp Infect 1990;16:297-
tive oxygen and the risk of surgical wound operative normothermia to reduce the in- 309.
infection: a randomized controlled trial. cidence of surgical-wound infection and 19. Haley RW, Culver DH, Morgan WM,
JAMA 2005;294:2035-42. shorten hospitalization. N Engl J Med White JW, Emori TG, Hooton TM. Identi-
4. Fleischmann E, Lenhardt R, Kurz A, 1996;334:1209-15. fying patients at high risk of surgical
et al. Nitrous oxide and risk of surgical 12. Ruszczak Z, Friess W. Collagen as a wound infection: a simple multivariate
wound infection: a randomised trial. Lan- carrier for on-site delivery of antibacterial index of patient susceptibility and wound
cet 2005;366:1101-7. drugs. Adv Drug Deliv Rev 2003;55:1679- contamination. Am J Epidemiol 1985;
5. Pryor KO, Fahey TJ III, Lien CA, Gold- 98. 121:206-15.
stein PA. Surgical site infection and the 13. Guzmán Valdivia Gomez G, Guerrero 20. Tam VH, Kabbara S, Vo G, Schilling
routine use of perioperative hyperoxia in a TS, Lluck MC, Delgado FJ. Effectiveness AN, Coyle EA. Comparative pharmacody-
general surgical population: a random- of collagen-gentamicin implant for treat- namics of gentamicin against Staphylo-
ized controlled trial. JAMA 2004;291:79- ment of “dirty” abdominal wounds. World coccus aureus and Pseudomonas aerugi-
87. J Surg 1999;23:123-7. nosa. Antimicrob Agents Chemother 2006;
6. Rutten HJ, Nijhuis PH. Prevention of 14. Nowacki MP, Rutkowski A, Oledzki J, 50:2626-31.
wound infection in elective colorectal sur- Chwalinski M. Prospective, randomized 21. Friberg O, Jones I, Sjöberg L, Söder-
gery by local application of a gentamicin- trial examining the role of gentamycin- quist B, Vikerfors T, Kallman J. Antibiotic
containing collagen sponge. Eur J Surg containing collagen sponge in the reduc- concentrations in serum and wound fluid
Suppl 1997;578:31-5. tion of postoperative morbidity in rectal after local gentamicin or intravenous di-
7. Meyhoff CS, Wetterslev J, Jorgensen cancer patients: early results and surpris- cloxacillin prophylaxis in cardiac surgery.
LN, et al. Effect of high perioperative oxy- ing outcome at 3-year follow-up. Int J Co Scand J Infect Dis 2003;35:251-4.
gen fraction on surgical site infection and lorectal Dis 2005;20:114-20. 22. Bellomo R, Warrillow SJ, Reade MC.
pulmonary complications after abdomi- 15. Bratzler DW, Houck PM. Antimicro- Why we should be wary of single-center
nal surgery: the PROXI randomized clini- bial prophylaxis for surgery: an advisory trials. Crit Care Med 2009;37:3114-9.
cal trial. JAMA 2009;302:1543-50. statement from the National Surgical In- 23. Glickman SW, McHutchison JG, Pe-
8. Kirkland KB, Briggs JP, Trivette SL, fection Prevention Project. Clin Infect Dis terson ED, et al. Ethical and scientific im-
Wilkinson WE, Sexton DJ. The impact of 2004;38:1706-15. plications of the globalization of clinical
surgical-site infections in the 1990s: at- 16. Culver DH, Horan TC, Gaynes RP, et research. N Engl J Med 2009;360:816-23.
tributable mortality, excess length of hos- al. Surgical wound infection rates by Copyright © 2010 Massachusetts Medical Society.
n engl j med 363;11 nejm.org september 9, 2010 1049
The New England Journal of Medicine
Downloaded from nejm.org by linda mahardhika on May 25, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Você também pode gostar
- Maybury ManualDocumento55 páginasMaybury ManualFriends of MayburyAinda não há avaliações
- NCLEX Practice Test For OncologyDocumento26 páginasNCLEX Practice Test For OncologyDizerine Mirafuentes Rolida100% (4)
- Adderall-Safer Than AspirinDocumento2 páginasAdderall-Safer Than AspirinChristopher RhudyAinda não há avaliações
- 001 Hipoglucemia NeonatalDocumento6 páginas001 Hipoglucemia NeonatalErick Lozada OlivaAinda não há avaliações
- Predictors of Surgical Site InfectionsDocumento7 páginasPredictors of Surgical Site InfectionsMageAinda não há avaliações
- Prospective Randomized Evaluation of Prophylactic Antibiotic Usage in Patients Undergoing Tension Free Inguinal HernioplastyDocumento6 páginasProspective Randomized Evaluation of Prophylactic Antibiotic Usage in Patients Undergoing Tension Free Inguinal HernioplastyYai El BaRcaAinda não há avaliações
- Does An Antimicrobial Incision Drape Prevent.15Documento9 páginasDoes An Antimicrobial Incision Drape Prevent.15Jimenez-Espinosa JeffersonAinda não há avaliações
- Prospective Study of Preincisional Single-Dose Ceftriaxone in Reducing Postoperative Wound Infection in High Risk of Infection PatientsDocumento5 páginasProspective Study of Preincisional Single-Dose Ceftriaxone in Reducing Postoperative Wound Infection in High Risk of Infection PatientsoopsadhitAinda não há avaliações
- Hybrid Minimally Invasive Esophagectomy For Esophageal CancerDocumento11 páginasHybrid Minimally Invasive Esophagectomy For Esophageal CancerLuca BellaioAinda não há avaliações
- Surgical Site InfectionDocumento8 páginasSurgical Site Infection1234chocoAinda não há avaliações
- 10 1155@2019@1438793Documento7 páginas10 1155@2019@1438793bouchra8blsAinda não há avaliações
- Cirugía y CirujanosDocumento6 páginasCirugía y CirujanosDidit SatmokoAinda não há avaliações
- The Immunoscore: Colon Cancer and BeyondDocumento24 páginasThe Immunoscore: Colon Cancer and BeyondcollianairaAinda não há avaliações
- Efficacy of Triclosan-Coated Sutures For Reducing Risk of Surgical Site Infection in Adults: A Meta-Analysis of Randomized Clinical TrialsDocumento13 páginasEfficacy of Triclosan-Coated Sutures For Reducing Risk of Surgical Site Infection in Adults: A Meta-Analysis of Randomized Clinical TrialsJose Manuel Luna VazquezAinda não há avaliações
- 4147 15918 1 PBDocumento7 páginas4147 15918 1 PBI Made AryanaAinda não há avaliações
- Surgical Site Infections: Epidemiology, Microbiology and PreventionDocumento8 páginasSurgical Site Infections: Epidemiology, Microbiology and Preventionm8wyb2f6ngAinda não há avaliações
- Thyroglossal Duct Infections and Surgical OutcomesDocumento4 páginasThyroglossal Duct Infections and Surgical OutcomesKitaFankiAinda não há avaliações
- Medical Problem That Needs Antibiotic ProphylaxisDocumento6 páginasMedical Problem That Needs Antibiotic ProphylaxisPing KyAinda não há avaliações
- Extending The Interval For Port-A-Cath Maintenance: Eugenia Girda, Rebecca Phaeton, Gary L. Goldberg, Dennis KuoDocumento4 páginasExtending The Interval For Port-A-Cath Maintenance: Eugenia Girda, Rebecca Phaeton, Gary L. Goldberg, Dennis KuoJane PengAinda não há avaliações
- Acute Management of Open Fractures An Evidence Based Review PDFDocumento9 páginasAcute Management of Open Fractures An Evidence Based Review PDFSusPa Naraha100% (1)
- Ultrasound-Guided Drainage Vs Surgical Drainage ofDocumento7 páginasUltrasound-Guided Drainage Vs Surgical Drainage ofAbigail Ruiz hernándezAinda não há avaliações
- Revista Brasileira DE AnestesiologiaDocumento7 páginasRevista Brasileira DE AnestesiologiaPutriRahayuMoidadyAinda não há avaliações
- 1 s2.0 S0039606007003480 MainDocumento8 páginas1 s2.0 S0039606007003480 MainAna MîndrilăAinda não há avaliações
- Journal Homepage: - : IntroductionDocumento10 páginasJournal Homepage: - : IntroductionIJAR JOURNALAinda não há avaliações
- Post-Operative Wound Infection: A Surgeon'S Dilemma: Original ArticleDocumento7 páginasPost-Operative Wound Infection: A Surgeon'S Dilemma: Original ArticlePetit-Paul WedlyAinda não há avaliações
- 1 s2.0 S1078588413007946 Main 2Documento7 páginas1 s2.0 S1078588413007946 Main 2Saffa AzharaaniAinda não há avaliações
- 10 1016@j Jamcollsurg 2020 02 031Documento34 páginas10 1016@j Jamcollsurg 2020 02 031Residentes Cirugia Udea 2016Ainda não há avaliações
- Low Lying Fistula-In-Ano - Fistulotomy or FistulectomyDocumento4 páginasLow Lying Fistula-In-Ano - Fistulotomy or FistulectomyApjhs ApjhsAinda não há avaliações
- 2007, Besselink. Timing of InterventionDocumento8 páginas2007, Besselink. Timing of Interventionalvaro9101Ainda não há avaliações
- Burden of Adhesions in Abdominal and Pelvic SurgeryDocumento15 páginasBurden of Adhesions in Abdominal and Pelvic SurgeryDian AdiAinda não há avaliações
- UntitledDocumento9 páginasUntitledherdian ariebowoAinda não há avaliações
- Chlorhexidine-Impregnated SpongesDocumento11 páginasChlorhexidine-Impregnated Spongeshector nuñezAinda não há avaliações
- Surgical Site InfectionDocumento7 páginasSurgical Site InfectionCaxton ThumbiAinda não há avaliações
- 10 1016@j Ejca 2019 07 028Documento7 páginas10 1016@j Ejca 2019 07 028Ferdian PriantoAinda não há avaliações
- Delmarmariscal Cazalla2020Documento9 páginasDelmarmariscal Cazalla2020Andi Muhammad Imam RAinda não há avaliações
- Ni Hms 792438Documento16 páginasNi Hms 792438Fino GunnersAinda não há avaliações
- Operative Management of Anastomotic Leaks After Colorectal SurgeryDocumento6 páginasOperative Management of Anastomotic Leaks After Colorectal SurgeryJorge OsorioAinda não há avaliações
- Surgical Site Infection PreventionDocumento9 páginasSurgical Site Infection PreventionRachmat HasanAinda não há avaliações
- Predictors of Mesh Infection and Explantation After Abdominal Wall Hernia RepairDocumento8 páginasPredictors of Mesh Infection and Explantation After Abdominal Wall Hernia RepairOtto NaftariAinda não há avaliações
- Screenshot 2022-09-26 at 20.14.44Documento8 páginasScreenshot 2022-09-26 at 20.14.44Sutama ArtaAinda não há avaliações
- A Multicenter, Prospective Randomized Trial of Negative Pressure Wound Therapy For Infrainguinal Revascularization With A Groin IncisionDocumento12 páginasA Multicenter, Prospective Randomized Trial of Negative Pressure Wound Therapy For Infrainguinal Revascularization With A Groin IncisionburhanAinda não há avaliações
- The American Journal of SurgeryDocumento8 páginasThe American Journal of Surgerypolomska.kmAinda não há avaliações
- Soria 2019Documento7 páginasSoria 2019Dr. Alexandre SatoAinda não há avaliações
- Trial of Short-Course Antimicrobial Therapy For Intraabdominal InfectionDocumento10 páginasTrial of Short-Course Antimicrobial Therapy For Intraabdominal InfectionMeygan CórdovaAinda não há avaliações
- Christensen 2020Documento11 páginasChristensen 2020Francisco ChourioAinda não há avaliações
- A Proposed Protective Protocol Predicting Reduction of Shunt InfectionDocumento9 páginasA Proposed Protective Protocol Predicting Reduction of Shunt InfectionRamon VenturaAinda não há avaliações
- Jurnal PlastiksDocumento5 páginasJurnal PlastiksbdhAinda não há avaliações
- Quilting After Mastectomy Significantly Reduces Seroma FormationDocumento5 páginasQuilting After Mastectomy Significantly Reduces Seroma Formationbeepboop20Ainda não há avaliações
- Comparing The Efficacy of Modified Continuoussmead-Jones Versus Conventional Closure Ofmidline LaparotomywoundDocumento12 páginasComparing The Efficacy of Modified Continuoussmead-Jones Versus Conventional Closure Ofmidline LaparotomywoundIJAR JOURNALAinda não há avaliações
- Articles: BackgroundDocumento12 páginasArticles: BackgroundCésar Aguirre RomeroAinda não há avaliações
- Green-Tsui2013 Article ImpactOfAnesthesiaForCancerSurDocumento22 páginasGreen-Tsui2013 Article ImpactOfAnesthesiaForCancerSurNataAinda não há avaliações
- 1 s2.0 S1473309923007569 MainDocumento12 páginas1 s2.0 S1473309923007569 Mainbarrientosgerman321Ainda não há avaliações
- Risk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialDocumento9 páginasRisk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialsaryindrianyAinda não há avaliações
- Jce80002 2413 2422Documento10 páginasJce80002 2413 2422Erwin CandraAinda não há avaliações
- Surgical InfectionDocumento108 páginasSurgical InfectionodayfarmaaAinda não há avaliações
- 10 1 1 577 9465 PDFDocumento6 páginas10 1 1 577 9465 PDFRiwanda OktavianiAinda não há avaliações
- Surgical Site Infection After Groin Hernia RepairDocumento7 páginasSurgical Site Infection After Groin Hernia Repairيحيى الجبليAinda não há avaliações
- Study of Incidence and Risk Factors For Surgical Site Infection After Cesarean Section at First Referral UnitDocumento3 páginasStudy of Incidence and Risk Factors For Surgical Site Infection After Cesarean Section at First Referral UnitFaozan FikriAinda não há avaliações
- Stan Nard 2006Documento6 páginasStan Nard 2006Lavonia Berlina AdzalikaAinda não há avaliações
- Prognostic FactorDocumento8 páginasPrognostic FactorMarno TakaAinda não há avaliações
- 11 DJMCJ v5 I1 74 Maksuda CeftriaxoneDocumento4 páginas11 DJMCJ v5 I1 74 Maksuda Ceftriaxonenurul wahyuniAinda não há avaliações
- Diagnostics 13 01362Documento10 páginasDiagnostics 13 01362ela.sofiaAinda não há avaliações
- Case Studies of Postoperative Complications after Digestive SurgeryNo EverandCase Studies of Postoperative Complications after Digestive SurgeryAinda não há avaliações
- Pre and Post Conception Risk Factors in PROM: Research ArticleDocumento5 páginasPre and Post Conception Risk Factors in PROM: Research ArticleNurul ImaniarAinda não há avaliações
- Ekwo 1993Documento10 páginasEkwo 1993Nurul ImaniarAinda não há avaliações
- JURDING I Role of Iron Sucrose Infusion in Correction of Iron Deficiency Anemia During Pregnancy PDFDocumento4 páginasJURDING I Role of Iron Sucrose Infusion in Correction of Iron Deficiency Anemia During Pregnancy PDFNurul ImaniarAinda não há avaliações
- Jurnal Saraf 1Documento5 páginasJurnal Saraf 1Nurul ImaniarAinda não há avaliações
- Atrial FibrillationDocumento60 páginasAtrial FibrillationNurul ImaniarAinda não há avaliações
- Intracellular AccumulationsDocumento19 páginasIntracellular AccumulationsWajiha106Ainda não há avaliações
- Reckettsia and ChlamediaDocumento37 páginasReckettsia and ChlamediaMuqtadir “The Ruler” KuchikiAinda não há avaliações
- Lassa Fever: What You Need To Know AboutDocumento2 páginasLassa Fever: What You Need To Know AboutMoses AyoadeAinda não há avaliações
- No. Name Position Monday Administration: Alternative Work Arrangement Jose C. Payumo Jr. Memorial High SchoolDocumento35 páginasNo. Name Position Monday Administration: Alternative Work Arrangement Jose C. Payumo Jr. Memorial High SchoolJeremy Desoyo TorresAinda não há avaliações
- Annex D Health Declaretion FormDocumento2 páginasAnnex D Health Declaretion FormJoseph SadiaAinda não há avaliações
- Mcqs FinalDocumento4 páginasMcqs FinalJats_Fru_1741Ainda não há avaliações
- Maria's First Love and Tooth No. 29Documento2 páginasMaria's First Love and Tooth No. 29Doreene Andres0% (1)
- Hypertention and HypotentionDocumento46 páginasHypertention and HypotentionAmanuel MaruAinda não há avaliações
- DipSlide For Environmental Monitoring in HospitalDocumento6 páginasDipSlide For Environmental Monitoring in HospitalIwan RidwantoAinda não há avaliações
- Safety Data Sheet: Section 1. Chemical Product and Company IdentificationDocumento17 páginasSafety Data Sheet: Section 1. Chemical Product and Company IdentificationEngr Qaisar NazeerAinda não há avaliações
- Vanjaarsveld MelodyM 1111992 PatientReportDocumento2 páginasVanjaarsveld MelodyM 1111992 PatientReportmelodyvanjaasveldAinda não há avaliações
- Health Benefits of Bicycle RidingDocumento3 páginasHealth Benefits of Bicycle RidingPeter JohnsonAinda não há avaliações
- CDC 26714 DS1Documento383 páginasCDC 26714 DS1Joyce AngobungAinda não há avaliações
- Original Studies: Originalni Naučni RadoviDocumento8 páginasOriginal Studies: Originalni Naučni RadoviMiroslav JovanovicAinda não há avaliações
- Tugas 1 Writing 4-Bing4309Documento1 páginaTugas 1 Writing 4-Bing4309DitaSariKusumaAinda não há avaliações
- Prenatal Substance Dependence AbuseDocumento13 páginasPrenatal Substance Dependence AbuseLei Ortega100% (1)
- E Coli-PowerpointDocumento29 páginasE Coli-PowerpointThrina Gynae CondezAinda não há avaliações
- Antibiotic Decision Making in IcuDocumento11 páginasAntibiotic Decision Making in IcumalvindersahiAinda não há avaliações
- Treatment of Hyperprolactinemia A.7Documento4 páginasTreatment of Hyperprolactinemia A.7Leyni fanny guerrero limaAinda não há avaliações
- Heparin - ClinicalKeyDocumento85 páginasHeparin - ClinicalKeydayannaAinda não há avaliações
- AsepsisDocumento20 páginasAsepsisErSandeepVermaAinda não há avaliações
- Understanding The Different Routes of Drug AdministrationDocumento3 páginasUnderstanding The Different Routes of Drug AdministrationMark Russel Sean LealAinda não há avaliações
- Dental AuxillaryDocumento125 páginasDental AuxillaryAME DENTAL COLLEGE RAICHUR, KARNATAKAAinda não há avaliações
- Clinical Genetics: General Aspects and Laboratory DiagnosticsDocumento14 páginasClinical Genetics: General Aspects and Laboratory DiagnosticsKinga-Borbála GagyiAinda não há avaliações
- @ (White Paper Cut-Off) QUS 0202 FinalDocumento13 páginas@ (White Paper Cut-Off) QUS 0202 FinalHajjab AnasAinda não há avaliações
- Journal Reading: Stase Ilmu THT RS Umum Daerah Sayang Cianjur Universitas Muhammadiyah Jakarta 2019Documento15 páginasJournal Reading: Stase Ilmu THT RS Umum Daerah Sayang Cianjur Universitas Muhammadiyah Jakarta 2019dwi purwantiAinda não há avaliações
- Feline Chronic Kidney Disease - Integrated ApproachDocumento12 páginasFeline Chronic Kidney Disease - Integrated ApproachClara SanchezAinda não há avaliações