Escolar Documentos
Profissional Documentos
Cultura Documentos
Carbamazepine Intoxication
Enviado por
Riccardo GuglielmoDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Carbamazepine Intoxication
Enviado por
Riccardo GuglielmoDireitos autorais:
Formatos disponíveis
Pharmacological Reports Copyright © 2010
2010, 62, 398404 by Institute of Pharmacology
ISSN 1734-1140 Polish Academy of Sciences
Short communication
Carbamazepine intoxication in alcohol dependent
epileptic patients
Wojciech Piekoszewski1, Ewa Florek2, Dorota Szpak3, Lucyna Kramer4,
Wojciech Jawieñ5
Department of Analytical Chemistry, Jagiellonian University, Ingardena 3, PL 30-060 Kraków, Poland
Laboratory of Environmental Research, Department of Toxicology, University of Medical Sciences, Dojazd 30,
PL 60-631 Poznañ, Poland
!
Toxicology Clinic, Jagiellonian University, Z³otej Jesieni 1, PL 31-826 Kraków, Poland
"
Department of Computer Sciences, University of Medical Sciences, D¹browskiego 79, PL 60-529 Poznañ, Poland
#
Department of Pharmacokinetics and Physical Pharmacy, Jagiellonian University, Medyczna 9,
PL 30-688 Kraków, Poland
Correspondence: Wojciech Piekoszewski, e-mail: wpiekosz@tlen.pl
Abstract:
Carbamazepine is frequently administrated to alcohol addict patients. The aim of this study was to evaluate the influence of alcohol
addiction on carbamazepine pharmacokinetics and severity of drug intoxication. The total of 158 carbamazepine intoxicated patients
participated in the study (76 non-alcohol-dependent, and 82 alcohol-dependent subjects). The results of the study indicate that the
level of unconsciousness depends on carbamazepine concentration. The frequency of anticholinergic toxidrome was higher in
alcohol-dependent patients (88.6% – alcohol-abused subjects, and 78.3% – alcoholics in abstinency) comparing to non-alcohol-
dependent epileptics (67.1%). The average biological half-life of carbamazepine in non-addicted epileptics was 41.5 h, 43.5 h for
alcohol-dependent patients during abstinency, and 38.6 in abused patients. It may be concluded that ethanol doesn’t influence the
pharmacokinetic and pharmacodynamic of carbamazepine in acute drug intoxication.
Key words:
carbamazepine, alcohol abuse, interaction
Introduction withdrawal syndrome [15, 23], and it is an alternative
to benzodiazepines [2]. Its application in the with-
drawal syndrome is related to the anti-convulsant,
Carbamazepine, apart from many therapeutic applica- anxiety-relieving, sedative, and mood-stabilizing ac-
tions, especially to control generalized tonic-clonic tion [9].
seizures and partial seizures in children and adults, is Although on the basis of the experiences gained so
broadly applied in the detoxification therapy for far, the intoxication resulting from the overdose of
alcohol-dependent patients and in the treatment of carbamazepine alone rarely constitutes a life threat,
398 Pharmacological Reports, 2010, 62, 398404
Carbamazepine and alcohol intoxication
Wojciech Piekoszewski et al.
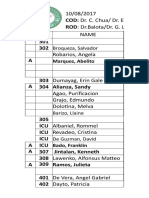
however, it is a problem due to the frequency of the Tab. 1. Demographic data of studied patients
phenomenon. The mixed intoxications with carba-
mazepine and ethanol are particularly dangerous from Parameter Group I Group II Group III
the toxicological point of view. Number 76 35 47
During intoxication, the absorption of carba- of patients
mazepine from the gastrointestinal tract is slowed Sex Male Female Male Female Male Female
down even up to 72 h, which may be a consequence
28 48 32 3 38 9
of its poor water solubility and a weaker bowel move-
Age [year] 27.3 ± 13.4 42.9 ± 8.9 38.7± 9.3
ment related to its anticholinergic action [3]. (mean ± SD)
As a result of carbamazepine biotransformation,
more than 30 metabolites are produced, including Group I non-alcohol-dependent epileptics with carbamazepine in-
10,11-epoxide, an active metabolite [10]. For clinical toxication. Group II alcohol-dependent epileptics with carba-
purpose, carbamazepine can be measured in saliva and mazepine intoxication (abstinent at the admission to the hospi-
tal).Group III alcohol-dependent epileptics with carbamazepine in-
genotype has no effect on its secretion to saliva [6]. toxication (abused at the admission to the hospital)
The simultaneous administration of carbamazepine
with other drugs or after the consumption of alcohol
may lead to interactions which may have dangerous performed and additionally a standard resting electro-
effects. This problem is particularly important among cardiogram was recorded. The level of consciousness
alcohol-dependent patients. Because the medical use disturbances was assessed on the basis of the
of carbamazepine among the alcohol addicted is very Matthew-Lawson Coma Scale.
frequent, a great risk of occurrence of such interac- After regaining the consciousness, the psychologi-
tions exist. cal examination with the application of the Self-
The aim of this paper was to evaluate the impact of al- Administered Alcohol Screening Test (SAAST) [19]
cohol acute intoxication and alcohol abuse on the course was carried out in all patients.
of carbamazepine intoxication in patients with epilepsy. At the moment of admission to the hospital, a blood
sample was collected in order to estimate the activity
of selected enzymes and concentrations of sodium
(Synchrone CX7 analyzer, Beckman Co.), ethanol
Materials and Methods and carbamazepine (AxSYME, Abbott Co.). The col-
lected samples of urine were used to perform a stan-
dard toxicological analysis for various drugs in urine
The total of 158 patients treated at the Toxicology (amphetamine derivatives, cannabinols, benzodi-
Clinic of the Jagiellonian University in Kraków, Po- azepines, barbiturates and phenytoin), and determina-
land participated in the study. All patients were di- tion of carbamazepine in serum and ethanol in whole
vided into three groups. Group I – patients intoxicated blood was performed. Carbamazepine was addition-
with carbamazepine and non-alcohol-dependent, ally determined in serum samples collected 2–6 times
groups II and III included alcohol-dependent patients, during hospitalization.
who overdosed carbamazepine. Patients from group II All patients with known enzyme inducers, (e.g.
were abstinent and in group III alcohol was detected barbiturates, phenytoin), and drugs impacting their
in blood at the admission to the clinic (Tab. 1). The clinical condition (e.g., benzodiazepies) detected in
cause of carbamazepine overdosing (accidental or at- urine were excluded from the study.
tendants to commit suicide) were not established.
All medical procedures in this study were carried
out in concordance with ethical standards and the Hel- Statistical and pharmacokinetic calculations
sinki Declaration (1975 with revision of 2000).
The results were assessed by the variance analysis
Patients and procedures method. Correlations between the respective variables
were indicated on the basis of Spearman coefficient.
At the admission to the hospital, a standardized medi- The pharmacokinetic calculations were carried out by
cal history and general physical examination were the statistical moment’s analysis.
Pharmacological Reports, 2010, 62, 398404 399
conductivity in three patients (rSr in V1). The sinus
Results
rate acceleration was observed in 18% of the studied
group. In one case, supraventricular tachycardia was
The age of the patients in group I was lower compared recorded. Among alcohol addicts, a block of the left
with patients in two other groups. The gender struc- bundle branch was observed, and among three of
ture was statistically different (Tab. 1). them – rSr’ in V1 was recorded. The non-specific
abnormalities of ST-T were present in six patients. In
General medical examination one case, the sinusal bradycardia 55/min occurred.
The supraventricular tachycardia was recorded in two
The arterial systolic and diastolic blood pressure (Tab. patients. The sinus rate acceleration was present in
2) was statistically significantly lower in the group of almost 30% of the studied group.
non-alcohol-dependent subjects than in both groups
of alcohol-dependent patients. Laboratory tests
The heart rate was higher in the group of alcohol-
dependent patients regardless of the presence of alco- The mean value of activity of AlAT in all studied
hol in blood tests in comparison with the group of groups was below upper limit of reference value (40 U/l).
non-addicts (Tab. 2). The concentration of carba- On the other hand, the activity of AspAT was higher
mazepine had no impact on the heart rate. than reference value (40 U/l) in both groups of ad-
In the electrocardiograms of the subjects who were dicted patients and statistically higher comparing with
not alcohol-dependent, no abnormalities were found non-alcohol-dependent patients (Tab. 2). The mean
except for the disturbances in the intraventricular values of concentration of sodium in plasma were in
the normal range (135–145 mM/l) and did not differ
between studied groups (data not shown).
Tab. 2. Results of medical examination and biochemical tests
Parameter Group I Group II Group III Tab. 3. Results of the toxicological and pharmacokinetic examination
of carbamazepine
Systolic blood 125.8 142 140
pressure [mmHg] ± 20.7 ± 20.5* ± 20.6*
Parameter Group I Group II Group III
Diastolic blood 80.8 89.8 87.5
pressure [mmHg] ± 14.7 ± 12.8* ± 16.1*
Estimated dose 8.3 9.6 9.5
Heart rate 91 98 100 of carbamazepine [g] ± 5.1 ± 6.7 ± 6.6
[beats/min] ± 17 ± 18* ± 16*
Cholinolytic syndrome [%] 67.1 78.4* 88.5* Time from drug 6.5 7.2 6.0
taking [h] ± 6.3 ± 4.8 ± 4.2
Physostigmine application [%] 19.7 21.7 27.0*
AlAT activity [U/] 25.2 32.2 31.0 Time of 6.8 5.8 7.5
± 23.4 ± 29.0 ± 30.6 hospitalization [day] ± 6.3 ± 3.8 ± 5.3
AspAT activity [U/] 35.9 56.6 47.33 Maximum carbamazepine 30.2 34.7 29.5
± 54.9 ± 86.9* ± 75.9* concentration [mg/] ± 10.9 ± 11.8 ± 12.4
Degree of coma 0 22.06 11.43 23.92
Biological half-live [h] 41.5 43.4 38.6
during admission to
I 23.38 48.57 15.21
the hospital [%]
Clearance [l/h/kg] 0.067 0.0701 0.0693
II 35.07 22.86 39.13
± 0.005 ± 0.006 ± 0.004
III 14.29 17.14 19.57
Volume of 3.71 3.86 3.89
IV 5.20 0 2.17
distribution [l/kg]
Group I non-alcohol-dependent epileptics with carbamazepine in-
toxication. Group II alcohol-dependent epileptics with carba- Group I non-alcohol-dependent epileptics with carbamazepine in-
mazepine intoxication (abstinent at the admission to the hospital). toxication. Group II alcohol-dependent epileptics with carba-
Group III alcohol-dependent epileptics with carbamazepine intoxi- mazepine intoxication (abstinent at the admission to the hospital).
cation (abused at the admission to the hospital). Data are the mean Group III alcohol-dependent epileptics with carbamazepine intoxi-
± SD, number of patients is presented in Table 1. * Differences statis- cation (abused at the admission to the hospital). Data are the mean
tically significant from group I; p < 0.05 ± SD, number of patients is presented in Table 1
400 Pharmacological Reports, 2010, 62, 398404
Carbamazepine and alcohol intoxication
Wojciech Piekoszewski et al.
Toxicological tests
The mean doses of carbamazepine used by patients,
established on the basis of a medical interview, were
similar in all study groups (Tab. 3).
The largest group was formed by patients who took
s
an intoxicating dose below 10 grams of carba-
mazepine (81.82% in group I; 68,57% in group II and
c
73,91% in group III). Also, the time that expired from
the moment of drug administration to the moment of
admission to the hospital did not differ between the
studied groups (Tab. 3).
The toxicological tests demonstrated that the mean
of maximum concentration of carbamazepine in stud-
ied groups ranged from 29.5 to 34.7 mg/l. Despite the
highest concentration of carbamazepine in the group
of abused patients, the differences in drug concentra- Fig. 1. Relationship between carbamazepine concentration and
tion in comparison to the remaining groups were not score in Matthew-Lawson coma scale. Group I epileptics non-
alcohol dependent with carbamazepine intoxication. Group II
statistically significant. alcohol-dependent epileptics intoxicated with carbamazepine (ab-
The statistical analysis indicates that there is a rela- stinent at the admission to the hospital). Group III alcohol-
dependent epileptics with carbamazepine intoxication (abused at
tionship between the maximal carbamazepine concen- the admission to the hospital). Data presented are the mean ± SD,
tration and the dose of the drug taken by the patient. number of patients is presented in Table 1
Within the group of patients admitted to the hospi-
tal and intoxicated with alcohol, the concentrations of
alcohol ranged from 0.5 to 3.0 g/l, but in almost 50% third studied groups were 0.5399, 0.5817 and 0.6982,
of cases, the concentration of ethanol ranged from 1.1 respectively, and were statistically significant (p <
to 2.0 g/l, and the mean concentration of alcohol was 0.05) (Fig. 1).
1.4 ± 0.8 g/l. With regard to the percentage, the cholinolytic syn-
It was not demonstrated that the differences in du- drome occurred most frequently within the group of
ration of hospitalization within the respective groups alcohol-dependent persons and intoxicated with it
were statistically significant (Tab. 3), however, the (88.5%). More seldom (78.4%), this syndrome was
time of hospitalization depended on concentration of observed in the group of addicts, in whose case, no
carbamazepine, and when the concentration was presence of alcohol was detected, whereas in the
higher than 30 mg/l, the time of hospitalization was group of non-addicts, occurred only in 67.11% (Tab.
longer than 7 days. 2). The frequency of occurrence of the cholinolytic
A parameter proving the severity of intoxication syndrome depended on the concentration of carba-
evaluated in the conducted tests was the degree of mazepine. In the case of 35 out of 158 patients, the in-
coma. The distribution of the degrees of coma in the tesity of the symptoms of cholinolytic syndrome
studied groups in the first day of hospitalization is caused the necessity of administering physostigmine
presented in Table 2. salicylate (Tab. 2). The necessity for its administra-
During the subsequent days, the degree of coma in tion did not occur more often within the group of
the studied subiects was lowered and in the second alcohol-dependent persons comparing to the group of
day the number of patients with the consciousness non-addicted patients.
disturbance lowered to 105 persons. On the fifth day, The symptoms of respiratory insufficiency ob-
the number of patients with consciousness distur- served among patients were indication for intubations
bance decreased to about 5%. and mechanical ventilation in 2.3% of patients in
The degree of consciousness disturbance at the first group I, 3.5% in group II and 1.4% in group III. The
day of hospitalization correlated with the concentra- mean time of mechanical ventilation was three days in
tion of carbamazepine in blood and the Spearman’s the first group, two days in the second group and as
coefficients of correlation for the first, second and much as five days in the third group.
Pharmacological Reports, 2010, 62, 398404 401
Pharmacokinetic analysis within the studied groups, it was observed that it was
higher within the group of alcohol-dependent persons,
The obtained results prove that the majority of pa- and the differences were statistically significant. This
tients came to the clinic after complete absorption of may result from a direct toxic impact of alcohol on the
the drug. Within the group of non-addicted persons, myocardium, secondary electrolytic disorders, and the
this amounted to 100%, whereas in group II of alco- presence of cardiotoxic acetic aldehyde [14, 21].
hol addicts, who were not intoxicated with it, the ab- Statistically significant differences in the values of
sorption process was not completed in 9.21% of pa- the arterial blood pressure were also observed within
tients, and in group III, it was 24.44%. The basic the studied groups. The described impact of carba-
pharmacokinetic parameters are presented in Table 3. mazepine on the cardiovascular system indicates a
possibility of occurrence of both hypotension and hy-
Psychological test pertension [13, 17]. The statistical analysis demon-
strated that both the systolic and diastolic pressure
The alcohol dependence was diagnosed basing on were significantly higher in the group of alcohol-
ICD-10 criteria and additionally it was evaluated with dependent persons. As noticed by Bannan et al., the
the SAAST test. The differences between scores systolic and diastolic arterial blood pressure is related
achieved by alcohol-dependent subjects (21.3 ± 4.46) to the seriousness of withdrawal syndrome [1].
and non-dependent persons (2.31 ± 2.8) were statisti- The rhythm and conductivity disorders resulting
cally significant. from the cardiotoxic action of carbamazepine occur
fairly seldom. Within the studied group, this type of
carbamazepine action was not observed. The lack of
such disorders in this study may result from the fact
that high concentrations of carbamazepine in the stud-
Discussion
ied patients exceeding 50 mg/l occurred rarely,
whereas heart disorders described in the literature
It is a well-known fact that carbamazepine increases show high concentrations of carbamazepine exceed-
its own metabolism [8, 18]. Therefore, a long period ing these values [20].
(at least one year) of carbamazepine administration The consciousness disturbance within the studied
was a condition for qualifying a patient to the study groups of patients during admitting to the hospital
group. was observed in 81.1% of persons in the group of
On the basis of the medical history, it was found non-addicts, 88.6% of sober alcohol-dependent pa-
that the mean time from drug administration in the tients and 76.6% of drunk alcohol-dependent persons
groups studied was similar and ranged between poisoned by carbamazepine. The intensity of con-
6.0–7.2 h, with the mean estimated dose of carba- sciousness disturbance correlated with the carba-
mazepine 8.3–9.6 g. The mean maximum concentra- mazepine concentration in blood. The correlation be-
tions of carbamazepine within the studied groups tween the degree of coma and the level of carba-
were 30.2 ± 10.9 mg/l in group I, 34.7 ± 11.8 mg/l in mazepine in blood confirmed the results of Feldman
group II and 29.5 ± 12.4 mg/l in group III. In many of et al. [4].
cases the carbamazepine concentrations were within The cases of liver damage as a result of toxic car-
the toxic range (20–40 mg/l). bamazepine action are described in the literature. In
In this study, no impact of age on the elimination the studied groups, the mean values of AlAT activity
and toxicity of carbamazepine were confirmed as were in the range of the reference value. The activity
suggested in some papers. This can be explained by of AspAT, was above reference value in both groups
the fact that only adults participated in the study, of alcohol-dependent patients, but not in non-alcohol
whereas the suggested differences typically can be dependend patients with carbamazepine intoxication.
seen between adults, children and older persons [7]. Both carbamazepine and alcohol may cause symp-
The sinusal tachycardia occurring in carba- toms of cholinolytic toxidrome [10]. However, the
mazepine intoxications is a frequent symptom re- cholinolytic toxidrome occurred most often within the
ported in the literature, as a result of the vagolytic ac- group of addicted persons, who were intoxicated with
tion of carbamazepine [16]. Evaluating the heart rate alcohol. The statistical analysis demonstrated a good
402 Pharmacological Reports, 2010, 62, 398404
Carbamazepine and alcohol intoxication
Wojciech Piekoszewski et al.
correlation of its occurrence with the carbamazepine The reports concerning pharmacokinetics of carba-
concentration in blood. In cases of intensified choli- mazepine in acute intoxications are not frequent, and
nolytic symptoms, the physostigmine salicylate is rec- the presented results are not unambiguous. In the
ommended. In spite of the undeniable relationship be- study based on a relatively small group of intoxicated
tween the occurrence of the cholinolytic symptoms patients, Hundt showed that the elimination of carba-
and the carbamazepine concentration in blood, the ap- mazepine takes place in accordance with the linear ki-
plication of physostigmine salicylate was most often netics [5]. On the other hand, in other studies, it was
indicated within the group of alcohol-dependent pa- demonstrated that the elimination of carbamazepine
tients with ethanol present in blood, and the differ- occurs in accordance with zero order kinetics, and the
ences between the groups of addicted and non- rate of elimination ranges from 0.5 to 0.8 mg/l/h [22].
alcohol-dependent persons with regard to the drug ad- The results most similar to presented in this paper
ministration were statistically significant. This fact were obtained by Montoya-Cabrera et al. (t0.5 18–54 h)
may be explained by the presence of alcohol, which [12].
also has a cholinolytic action. Our study showed an increase of arterial blood
Most authors emphasize the correlation between pressure and heart rate in alcohol-dependent persons
the concentrations of carbamazepine with its toxicity. but it was not fairly elevated by carbamazepine
Montogomery et al. observed the symptoms of respi- intoxication. Other obtained results did not confirmed an
ratory insufficiency with the carbamazepine concen- impact of alcohol addiction and the level of intoxication
trations exceeding 40 mg/l [11]. Among the persons on pharmacodynamics and pharmacokinetics of carba-
subjected to the study, the necessity for intubations mazepine.
and mechanical ventilation was necessary in few
cases. The carbamazepine concentrations observed at
that time was 40–60 mg/l. Within group I, 3 (2.9%)
References:
patients required intubations, whereas the mechanical
ventilation was implemented in 2 cases (1.5%).
Within the group of alcohol-dependent patients, intu- 1. Bannan LT, Potter JF, Beeverse DG, Saunders JB, Wal-
bation was required in 5 patients (4%) of which 4 ters JR, Ingram MC: Effects of alcohol withdrawal on
were inebriated with alcohol. The mechanical ventila- blood pressure, plasma renin activity, aldosterone, corti-
sol and dopamine beta hydroxylase. Clin Sci, 1984, 66,
tion in this group was applied in 4 patients (3.2%) of 659–663.
whom three were inebriated with alcohol. 2. Bayard M, McIntyre J, Hill KR, Woodside J Jr: Alcohol
In the studies of Spiller et al. [16], the indications withdrawal syndrome. Am Fam Physician, 2004, 69,
for artificial ventilation occurred among patients with 1443–1450.
3. Desphande G, Meert KL, Valentini, RP: Repeat charcoal
the carbamazepine concentration ranging between
hemoperfusion treatments in life threatening carba-
20–59 mg/l and the time of mechanical ventilation mazepine overdose. Pediatr Nephrol, 1999, 13, 775–777.
was 12–23 h. Within the studied group, the time was 4. Feldman R, Burda PR, Glinska-Serwik M, Kotlarska M,
longer, and ranged from 2 days (group II) to 5 days Szajewski J: Correlation of carbamazepine level in blood
(group III). A clearly longer period of mechanical with clinical, intoxication status, evaluated with the help
of the APACHE II system and the Metthew coma scale.
ventilation in the group studied by us was most proba- Przegl Lek, 1997, 54, 411–415.
bly related to higher concentrations of carbamazepine 5. Hundt HK, Aucamp AK, Muller PO: Pharmacokinetic
in blood as they exceeded the levels given by Spiller, aspects of carbamazepine and its two major metabolites
where the concentration higher than 50 mg/l were re- in plasma during overdose. Human Toxicol, 1983, 2,
607–614.
corded only in one case [16].
6. Kurzawski M, Bartnicka L, DroŸdzik A, Bia³ecka M,
When analyzing the duration of stay in the hospital, DroŸdzik M: Effect of ABCB1 (MDR1) 3435C >T poly-
it was proved that it was dependent on the carba- morphism on salivary secretion of carbamazepine. Phar-
mazepine concentration in blood. The time of hospi- macol Rep, 2007, 59, Suppl 1, 275–279.
talization in carbamazepine intoxication assessed by 7. Lanchote VL, Bonato PS, Campos GM, Rodrigues I:
Factors influencing plasma concentration of carba-
Spiller demonstrated that the prolonged time of hospi- mazepine and carbamazepine 10,11-epoxide in epileptic
tal stay correlate with carbamazepine concentration in children and adults. Ther Drug Metabol, 1995, 17,
blood [16]. 47–52.
Pharmacological Reports, 2010, 62, 398404 403
8. Liu H, Delgedo MR: The influence of polytherapy on the tion. Results from an open clinical study. Eur Arch Psy-
relationships between serum carbamazepine and its me- chiatry Clin Neurosci, 2002, 252, 197–200.
tabolites in epileptic children. Epilepsy Res, 1994, 17, 16. Spiller AH, Krenzelok EP, Cookinks DE: Carba-
257–269. mazepine overdose: prospective study of serum levels
9. Lucht M, Kuehn KU, Armbruster J, Abraham G, Gaen- and toxicity. Clin Toxicol, 1990, 28, 445–456.
sicke M, Barnow S, Tretzel H, Freyberger HJ: Alcohol 17. Spiller F, Carlisle FM: Carbamazepine and NMS.
withdrawal treatment in intoxicated and non-intoxicated Br J Psychiatry, 2002, 158, 434–435.
patients: a controlled open-label study with tiapride/car- 18. Spina E, Pisani F, Perucca E: Clinically significant phar-
bamazepine, clomethazole and diazepam. Alcohol Alco- macokinetic drug interaction with carbamazepine. Clin
holism, 2003, 38, 168–175. Pharmacokinet, 1996, 31, 198–214.
19. Swenson WM, Morse RM: The use of a self-
10. Maggs JL, Pirmohamed M, Kitteringham NR, Park BK:
administered alcoholism screening test (SAAST) in a
Characterisation of the metabolites of carbamazepine in
medical center. Mayo Clin Proc, 1975, 50, 2048.
patient urine by liquid chromatography/mass spectrome- 20. Tibbals J: Acute intoxication to carbamazepine: clinical
try. Drug Metab Dispos, 1997, 25, 275–279. effects and serum concentrations. J Pediatr, 1992, 12,
11. Montgomery VL, Richman BJ, Goldsmith LJ, Rodgers 295–299.
GC Jr: Severity and carbamazepine levels at time initial. 21. Wickramansinghe SN, Hasan R, Knapey Z: Differences
Poisoning centre contact correlate with outcome in car- in the serum levels of acetaldehyde and cytotoxic acetal-
bamazepine poisoning. Clin Toxicol, 1995, 33, 311–323. dehyde albumin complexes after the consumption of red
12. Montoya-Cabrera MA, Sauceda-Garcia JM, Escalante- and white wine: in vitro effects of flavonoids, vitamin E
Galindo P, Flores-Alvarez E, Ruiz-Gómez A: Carba- and other dietary antioxidants on cytotoxic complexes.
mazepine poisoning in adolescent suicide attempters. Ef- Alcohol Clin Exp Res, 1996, 20, 799–806.
fectives of multiple dose activated charcoal in enhancing 22. Winnicka RI, Topaciñski B, Szymczak WM, Szymañska
carbamazepine elimination. Arch Med Res, 1996, 7, B: Carbamazepine poisoning: elimination kinetics and
485–489. quantitative response. Clin Toxicol, 2002, 40, 759–765.
13. Mordel A, Sivilotti MLA, Linden CH: Fatal TCA-like 23. Zilker T: Alcohol withdrawal syndrome and delirium
cardiotoxicity following carbamazepine overdose. Clin tremens. Diagnosis and therapy. MMW Fortschr Med,
Toxicol, 1998, 36, 472–476. 2004, 141, 26–30.
14. Opolski G, Torbicki A: Auricular fibrillation (in Polish).
Urban & Partner, Wroc³aw. 2000.
15. Soyka M, Morhart-Klute V, Horak M: A combination of Received:
carbamazepine/tiapride in outpatient alcohol detoxifica- July 13, 2009; in revised form: October 1, 2009.
404 Pharmacological Reports, 2010, 62, 398404
Você também pode gostar
- Basic Toxicology Manual ModifiedDocumento63 páginasBasic Toxicology Manual ModifiedEmilia DuncaAinda não há avaliações
- Critical Issues in Alcohol and Drugs of Abuse TestingNo EverandCritical Issues in Alcohol and Drugs of Abuse TestingAinda não há avaliações
- 5.thyroid Gland LectureDocumento96 páginas5.thyroid Gland Lecturesdsher100% (3)
- NCP Ineffective Cerebral Tissue PerfusionDocumento2 páginasNCP Ineffective Cerebral Tissue PerfusionAngelo ︻╦̵̵͇̿̿̿̿╤── Bulacan50% (6)
- Severe Carbamates IntoxicationDocumento3 páginasSevere Carbamates IntoxicationFrancieudo SampaioAinda não há avaliações
- The Influence of CYP2D6 Phenotype On The Pharmacokinetic Profile of Atomoxetine in Caucasian Healthy SubjectsDocumento8 páginasThe Influence of CYP2D6 Phenotype On The Pharmacokinetic Profile of Atomoxetine in Caucasian Healthy SubjectsAlina RotariAinda não há avaliações
- CarbamazepinaDocumento15 páginasCarbamazepinaNataliaPalacínBernalAinda não há avaliações
- The PK/PD Index (C /mic) For Ciprofloxacin in Patients With Cystic FibrosisDocumento7 páginasThe PK/PD Index (C /mic) For Ciprofloxacin in Patients With Cystic Fibrosisefra maneAinda não há avaliações
- Retrospective Review of Vancomycin-Induced Nephrotoxicity in Patients With LeukemiaDocumento6 páginasRetrospective Review of Vancomycin-Induced Nephrotoxicity in Patients With LeukemiaAdisak DuangthumAinda não há avaliações
- CarbamateDocumento7 páginasCarbamateJulianHCardenasAinda não há avaliações
- Tubulointerstitial Injury and Drugs of AbuseDocumento6 páginasTubulointerstitial Injury and Drugs of AbuseHadsfrv KajdgygAinda não há avaliações
- Screening For Drugs of Abuse. II Cannabinoids, Lysergic Acid Diethylamide, Buprenorphine, Methadone, Barbiturates, Benzodiazepines and Other DrugsDocumento51 páginasScreening For Drugs of Abuse. II Cannabinoids, Lysergic Acid Diethylamide, Buprenorphine, Methadone, Barbiturates, Benzodiazepines and Other DrugsRafal RogalewiczAinda não há avaliações
- Laprosy Research Paper (Ahmed Tanjimul Islam)Documento7 páginasLaprosy Research Paper (Ahmed Tanjimul Islam)AHMED TANJIMUL ISLAMAinda não há avaliações
- (25!11!15) Artigo Management of Exogenous Intoxication PublicadoDocumento6 páginas(25!11!15) Artigo Management of Exogenous Intoxication PublicadoSydney LeãoAinda não há avaliações
- Comparative Pharmacokinetics of The Three Echinocandins in ICU PatientsDocumento8 páginasComparative Pharmacokinetics of The Three Echinocandins in ICU PatientsAris DokoumetzidisAinda não há avaliações
- Jurnal NorvascDocumento8 páginasJurnal NorvascYoung AjjaAinda não há avaliações
- Different Behaviour of Plasma Antioxidant Status After Red Wine Giammanco M, Et Al.Documento8 páginasDifferent Behaviour of Plasma Antioxidant Status After Red Wine Giammanco M, Et Al.Marco GiammancoAinda não há avaliações
- Valproic Acid in Epilepsy: Clinical and Pharmacological EffectsDocumento6 páginasValproic Acid in Epilepsy: Clinical and Pharmacological EffectsadityaAinda não há avaliações
- Amoniaco NeurotoxicidaDocumento8 páginasAmoniaco NeurotoxicidaJOHANNA CATHERINE RUIZ CASTILLOAinda não há avaliações
- Meta-Analysis: The Safety and Ef Ficacy of Vaptans (Tolvaptan, Satavaptan and Lixivaptan) in Cirrhosis With Ascites or HyponatraemiaDocumento8 páginasMeta-Analysis: The Safety and Ef Ficacy of Vaptans (Tolvaptan, Satavaptan and Lixivaptan) in Cirrhosis With Ascites or HyponatraemiaHadi KuriryAinda não há avaliações
- Patisiran Pharmacokinetics, Pharmacodynamics, and Exposure-Response Analyses in The Phase 3 APOLLO Trial in Patients With Hereditary Transthyretin-Mediated (hATTR) AmyloidosisDocumento13 páginasPatisiran Pharmacokinetics, Pharmacodynamics, and Exposure-Response Analyses in The Phase 3 APOLLO Trial in Patients With Hereditary Transthyretin-Mediated (hATTR) AmyloidosisMihaela BerindeieAinda não há avaliações
- Winnicka 2002Documento8 páginasWinnicka 2002Hamida MidaAinda não há avaliações
- Correlation of Serum Amylase With Serum Cholinesterase in Assessing The Severity of Acute Organophosphorus PoisoningDocumento5 páginasCorrelation of Serum Amylase With Serum Cholinesterase in Assessing The Severity of Acute Organophosphorus PoisoningInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Smoking 15Documento6 páginasSmoking 15Clara CurcaAinda não há avaliações
- Sangviroon 2010Documento8 páginasSangviroon 2010uciAinda não há avaliações
- Medi 95 E2881Documento5 páginasMedi 95 E2881Betari YoscarAinda não há avaliações
- Phase I Pharmacokinetic and Pharmacodynamic StudyDocumento10 páginasPhase I Pharmacokinetic and Pharmacodynamic StudyPriyanka ParikhAinda não há avaliações
- Clinchem 1565Documento4 páginasClinchem 1565ghfkhgfjhfgAinda não há avaliações
- Bauch-Atrial Natriuretic Peptide As A MarDocumento6 páginasBauch-Atrial Natriuretic Peptide As A MarSzendeAinda não há avaliações
- Quantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsDocumento6 páginasQuantification of Pregabalin Using Hydrophilic Interaction HPLC-High-Resolution MS in Postmortem Human Samples: Eighteen Case ReportsLuisa Fernanda Velásquez QuijanoAinda não há avaliações
- Jur DingDocumento4 páginasJur DingerwinAinda não há avaliações
- Journal of Antimicrobial Chemotherapy Volume Issue 2016Documento7 páginasJournal of Antimicrobial Chemotherapy Volume Issue 2016Ulima Mazaya GhaisaniAinda não há avaliações
- Carnahan2006 (ADS)Documento7 páginasCarnahan2006 (ADS)arslaneAinda não há avaliações
- Aprillyanti 009Documento10 páginasAprillyanti 009Muhammad Mariadi FirdausAinda não há avaliações
- Acetaminophen-Cysteine Adducts During Therapeutic Dosing and Following OverdoseDocumento9 páginasAcetaminophen-Cysteine Adducts During Therapeutic Dosing and Following OverdoseLuifer AgudeloAinda não há avaliações
- Updates On Acetaminophen Toxicity: Adam K. Rowden, DO, Jeffrey Norvell, MD, David L. Eldridge, MD, Mark A. Kirk, MDDocumento15 páginasUpdates On Acetaminophen Toxicity: Adam K. Rowden, DO, Jeffrey Norvell, MD, David L. Eldridge, MD, Mark A. Kirk, MDAnumolu GoparajuAinda não há avaliações
- 1 s2.0 S0753332221008386 MainDocumento7 páginas1 s2.0 S0753332221008386 MainIsaura MendezAinda não há avaliações
- Research PaperDocumento3 páginasResearch PaperMalik Shehr YarAinda não há avaliações
- A Rational Use of Clozapine Based On Adverse Drug Reactions, Pharmacokinetics, and Clinical PharmacopsychologyDocumento15 páginasA Rational Use of Clozapine Based On Adverse Drug Reactions, Pharmacokinetics, and Clinical PharmacopsychologyDian GbligAinda não há avaliações
- High-Performance Liquid Chromatographic Analysis of Drugs of Abuse in Biologic SamplesDocumento6 páginasHigh-Performance Liquid Chromatographic Analysis of Drugs of Abuse in Biologic SamplesPutra SpAinda não há avaliações
- 2 - Paracetamol Toxicity Spring 2022Documento40 páginas2 - Paracetamol Toxicity Spring 2022mariamkhaledd777Ainda não há avaliações
- Dosing of Gentamicin in Patients With End-Stage Renal Disease Receiving HemodialysisDocumento10 páginasDosing of Gentamicin in Patients With End-Stage Renal Disease Receiving HemodialysisLuciana OliveiraAinda não há avaliações
- Acute Toxicity of RopivacaineDocumento7 páginasAcute Toxicity of RopivacaineAmilkar VazquezAinda não há avaliações
- A Pharmacokinetic and Pharmacodynamic Drug Interaction Study of Acamprosate and NaltrexoneDocumento12 páginasA Pharmacokinetic and Pharmacodynamic Drug Interaction Study of Acamprosate and NaltrexoneAldora OktavianaAinda não há avaliações
- Cocaine Metabolites DeterminationDocumento24 páginasCocaine Metabolites Determinationmohd firdosAinda não há avaliações
- Clinicopathologic Features of Agranulocytosis in The Setting of Levamisole-Tainted CocaineDocumento7 páginasClinicopathologic Features of Agranulocytosis in The Setting of Levamisole-Tainted Cocaineal jaynAinda não há avaliações
- Propylene Glycol Toxicity: A Severe Iatrogenic Illness in ICU Patients Receiving IV BenzodiazepinesDocumento8 páginasPropylene Glycol Toxicity: A Severe Iatrogenic Illness in ICU Patients Receiving IV BenzodiazepinesjongwoonieAinda não há avaliações
- L. CanabinoidDocumento10 páginasL. CanabinoidRoxana StanAinda não há avaliações
- 1471 2369 14 191 PDFDocumento9 páginas1471 2369 14 191 PDFhanifahrafaAinda não há avaliações
- Pharmacokinetics of Mycophenolate Mofetil Metabolites in Older Patients On The Seventh Day After Renal TransplantationDocumento4 páginasPharmacokinetics of Mycophenolate Mofetil Metabolites in Older Patients On The Seventh Day After Renal TransplantationMISS KIMAinda não há avaliações
- PIIS0007091217320603Documento10 páginasPIIS0007091217320603amjedsenoussiAinda não há avaliações
- Fmed 07 00440Documento9 páginasFmed 07 00440ERICK JHOVANI GUADALUPE GARCIA HERNANDEZAinda não há avaliações
- HCN 153Documento9 páginasHCN 153Suck my dickAinda não há avaliações
- 10 1097MD 0000000000000587Documento3 páginas10 1097MD 0000000000000587abbasamiri135103Ainda não há avaliações
- Articulo 9Documento9 páginasArticulo 9fabiana huatuco oréAinda não há avaliações
- ACBR - Manuscript - 008 CorrectedDocumento10 páginasACBR - Manuscript - 008 CorrectedFabian PitkinAinda não há avaliações
- Metabolism, Excretion, and Pharmacokinetics of Selumetinib, An MEK1/2 Inhibitor, in Healthy Adult Male SubjectsDocumento33 páginasMetabolism, Excretion, and Pharmacokinetics of Selumetinib, An MEK1/2 Inhibitor, in Healthy Adult Male SubjectsAndi wahyuniAinda não há avaliações
- Basic Toxicology Manual Modified PDFDocumento63 páginasBasic Toxicology Manual Modified PDFduncaemiliaAinda não há avaliações
- JCMayo2022 PDFDocumento10 páginasJCMayo2022 PDFAle López CastroAinda não há avaliações
- Revisión SistemáticaDocumento9 páginasRevisión SistemáticaavmolanoAinda não há avaliações
- The Relationship Between Blood Lactate and Survival Following The Use of Adrenaline in The Treatment of Septic ShockDocumento7 páginasThe Relationship Between Blood Lactate and Survival Following The Use of Adrenaline in The Treatment of Septic ShockGoran CucicAinda não há avaliações
- Limfoma Kutis Pada Pasien Yang Semula Di DiagnosisDocumento34 páginasLimfoma Kutis Pada Pasien Yang Semula Di DiagnosisChris MulyoAinda não há avaliações
- Prevalence of Depression, Anxiety, and Associated Factors in Residents From Hospital Centers During COVID-19 PandemicDocumento6 páginasPrevalence of Depression, Anxiety, and Associated Factors in Residents From Hospital Centers During COVID-19 PandemicMericia Guadalupe Sandoval ChavezAinda não há avaliações
- Abdominal Assessment: Jonalyn S. Esco,.Rn.,ManDocumento77 páginasAbdominal Assessment: Jonalyn S. Esco,.Rn.,ManClifford Subagan Patil-aoAinda não há avaliações
- Malaria: Health Education HFT 201 By: Sophia Kol, MDDocumento10 páginasMalaria: Health Education HFT 201 By: Sophia Kol, MDTith SeavmeyAinda não há avaliações
- Hip Interventions Project - Harris SvorinicDocumento3 páginasHip Interventions Project - Harris Svorinicapi-620069244Ainda não há avaliações
- Pre & Post Operative TracheostomyDocumento2 páginasPre & Post Operative TracheostomyHantu Kak Limah100% (2)
- Clinical Medical Reviews and Case Reports CMRCR 5 227Documento8 páginasClinical Medical Reviews and Case Reports CMRCR 5 227Juan BacelarAinda não há avaliações
- Doctor'S Order and Progress NotesDocumento3 páginasDoctor'S Order and Progress NotesDienizs LabiniAinda não há avaliações
- Chapter 7-Brief Psychodynamic Therapy: BackgroundDocumento54 páginasChapter 7-Brief Psychodynamic Therapy: BackgroundKarenHAinda não há avaliações
- ClindamycinDocumento3 páginasClindamycinWinter KimAinda não há avaliações
- Hypertensión Ese - Spin - Brochure - Rev. - 03 - LowDocumento12 páginasHypertensión Ese - Spin - Brochure - Rev. - 03 - LowVICTOR losanAinda não há avaliações
- Maternal and Child ReviewerDocumento330 páginasMaternal and Child ReviewerMiles Brianne Lymer A. OlvidoAinda não há avaliações
- Chapter 6 Water Safety - Recognition and ResponseDocumento41 páginasChapter 6 Water Safety - Recognition and ResponsemaligayamicadaleAinda não há avaliações
- Harjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCDocumento7 páginasHarjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCSofia PerezAinda não há avaliações
- Hyperparathyroidism A Forgotten Cause of Musculoskeletal PainDocumento3 páginasHyperparathyroidism A Forgotten Cause of Musculoskeletal PainPhuoc TranAinda não há avaliações
- Form Ringkasan Perawatan Pasien Pulang (Resume Medis)Documento1 páginaForm Ringkasan Perawatan Pasien Pulang (Resume Medis)gandi mahardika muktiAinda não há avaliações
- Census FormatDocumento35 páginasCensus Formatkolintang1Ainda não há avaliações
- Awareness of Medication-Related Fall Risk A Survey of Communitydwelling Older Adults PDFDocumento7 páginasAwareness of Medication-Related Fall Risk A Survey of Communitydwelling Older Adults PDFRenaldiPrimaSaputraAinda não há avaliações
- FARMASAINS Vol. Xx. No. XX, Bulan TahunDocumento9 páginasFARMASAINS Vol. Xx. No. XX, Bulan TahunShonia FatwaAinda não há avaliações
- Notices About Filtered ResultsDocumento5 páginasNotices About Filtered ResultsJoshua TerceñoAinda não há avaliações
- Leave Letter MedicalDocumento1 páginaLeave Letter MedicalAdrian EdryAinda não há avaliações
- History Taking Form in Gynecology Obstetrics - CompressDocumento8 páginasHistory Taking Form in Gynecology Obstetrics - CompresskeightAinda não há avaliações
- Pulmonaryrehabilitation 180412172759Documento44 páginasPulmonaryrehabilitation 180412172759IvanAinda não há avaliações
- Antibiotic Sensitivity FINAL V4 Sheet1Documento1 páginaAntibiotic Sensitivity FINAL V4 Sheet1JHAinda não há avaliações
- Anaphylactic Death FinalDocumento73 páginasAnaphylactic Death Finalkhaled eissaAinda não há avaliações
- 4.A.3.3 Ramos v. CA (1999 and 2002)Documento4 páginas4.A.3.3 Ramos v. CA (1999 and 2002)Soraya Salubo Laut100% (1)
- Comorbidity GuidelinesDocumento231 páginasComorbidity Guidelinesgavinbuzz100% (1)
- Medgears: We Have Been Pioneers at Manufacturing, Exporting and Wholesaling A Wide Assortment of High-QualityDocumento24 páginasMedgears: We Have Been Pioneers at Manufacturing, Exporting and Wholesaling A Wide Assortment of High-QualitySubhasis MallikAinda não há avaliações