Escolar Documentos
Profissional Documentos
Cultura Documentos
Form Reconciliation PDF
Enviado por
bella sobaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Form Reconciliation PDF
Enviado por
bella sobaDireitos autorais:
Formatos disponíveis
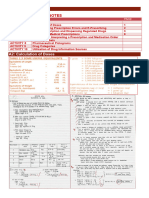
MEDICATION
RECONCILIATION
FORM
PATIENT IDENTIFICATION
DATE: TIME:
FAXED: YES NO
DRUG ALLERGIES:
( mg, ml, Medications Home Medications
microgram, Ordered Continued
( List only those Medications currently being taken )
grams, units ) on Admission? at Discharge?
MEDICATION NAME DOSE FREQUENCY ROUTE YES NO YES NO
RN SIGNATURE / TITLE: DATE:
RN SIGNATURE / TITLE: DATE:
PHYSICIAN INSTRUCTIONS: 1. Physician will clarify all medications not continued and document in Progress Notes.
2. Physician will review the above list, which has been completed to the best of your knowledge;
afterwards add signature, date and time, as indicated.
PHYSICIAN SIGNATURE / TITLE: DATE:
PART OF THE MEDICAL RECORD
8850526 Rev. 04/06 Medication Reconciliation Form_Nursing Pharmacy Committee_MEDICAL AFFAIRS PAGE 1 of 2
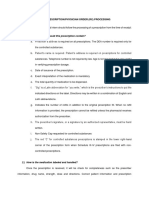
TITLE: GUIDELINES FOR COMPLETING THE MEDICATION RECONCILIATION FORM
PURPOSE: To assure that each patient's medication history is documented by staff upon admission and reconciled by
the physician. Upon discharge, the form will be used to assure that all medications have been addressed.
NATURE OF The MEDICATION RECONCILIATION FORM is a legal document that documents the safe and effective
THE FORM: medication management of the patient's medication. The form will be used to identify the patient's current
medications, dosages and scheduling. Medication reconciliation will be performed to clarify any
discrepancies between the patient's actual medication regime and the most recent record of prescribed
medication. This will allow for medical practitioners to review the information and order the appropriate
medication and dosages for patients upon admission and discharge from Providence Hospital. Patients
will have all medication reconciled within 24 hours of admission. The MEDICATION RECONCILIATION
FORM is a one-sided form, to be completed in black ink, and should be the first form placed in the medical
record.
RESPONSIBLE The RN / LPN, Physician or Pharmacist may complete the form.
PERSON:
INSTRUCTIONS: 1. Upon initiating this form, the patient's identification label will be placed in the upper
right corner of this form.
2. Complete the date and time lines, as indicated
3. Complete the drug allergies line, as appropriate, indicating the actual drug, food &
environmental allergies, or "NKDA".
4. The medication history will be obtained from the patient and/or family members present
at time of admission to the hospital. Medications will be obtained from patient's
transfer summary for nursing / group home patients.
5. Complete the name, dose, frequency and route of each medication.
6. Check the "Yes" or "No" checkbox to indicate if home medications were ordered on
admission.
7. Form must be signed by the RN /LPN completing this form on admission. (Note:
two signature lines are available, if more than one nurse is completing this form).
8. Physician must sign and date this form to ensure the reconciliation process has
taken place and all needed medications have been ordered.
9. After completing this form and within 24 hours of admission, this form must be
faxed to the Pharmacy Department. Check the "Yes" box (top of Pg 1) once the
form has been faxed to the Pharmacy Department.
10. Upon discharge, check the "Yes" or "No" checkbox for home medications that are
being continued after discharge home.
8850526 Rev. 04/06 Medication Reconciliation Form_Nursing Pharmacy Committee_MEDICAL AFFAIRS PAGE 2 of 2
Você também pode gostar
- Medication SafetyDocumento35 páginasMedication SafetybabychelleAinda não há avaliações
- Arizona Pharmacy Board Regulations and RequirementsDocumento5 páginasArizona Pharmacy Board Regulations and Requirementseze24Ainda não há avaliações
- ASHP Pharmaceutical Care PDFDocumento3 páginasASHP Pharmaceutical Care PDFCella Mboeik IIAinda não há avaliações
- Sample Case ScenarioDocumento10 páginasSample Case ScenarioKarilee Salcedo AyunayunAinda não há avaliações
- Medication Therapy Management - A Focus On HypertensionDocumento31 páginasMedication Therapy Management - A Focus On Hypertensionchdx21479100% (1)
- Chapter 7. The Care PlanDocumento19 páginasChapter 7. The Care PlanLouise TheunisAinda não há avaliações
- Module 16 - Pharmacotherapy For Psychiatric DisordersDocumento157 páginasModule 16 - Pharmacotherapy For Psychiatric Disordersgeekay79Ainda não há avaliações
- Chapter 01Documento14 páginasChapter 01flaviamarottaAinda não há avaliações
- 11-24 First Draft 1 5Documento3 páginas11-24 First Draft 1 5api-242283963Ainda não há avaliações
- Walgreens MTM PresentationDocumento28 páginasWalgreens MTM Presentationtomoe hotaruAinda não há avaliações
- Introduction PC 2017Documento20 páginasIntroduction PC 2017ChristinaAinda não há avaliações
- Medication ManagementDocumento34 páginasMedication ManagementRhodora BenipayoAinda não há avaliações
- Professional Competencies For Canadian Pharmacy Technicians at Entry To PracticeDocumento26 páginasProfessional Competencies For Canadian Pharmacy Technicians at Entry To PracticeAnonymous jVZOuTAinda não há avaliações
- Pharmacoeconomics LceDocumento118 páginasPharmacoeconomics LceHope GemidaAinda não há avaliações
- HOME MEDICATION REVIEW OPTIMIZATIONDocumento31 páginasHOME MEDICATION REVIEW OPTIMIZATIONFaiz MustaffaAinda não há avaliações
- Medication History InterviewDocumento2 páginasMedication History InterviewShaik SameenaAinda não há avaliações
- Core Elements in Medication Therapy ManagementDocumento24 páginasCore Elements in Medication Therapy ManagementFaishalMahdiAinda não há avaliações
- Pharmacy Law & Ethics Regulations StandardsDocumento62 páginasPharmacy Law & Ethics Regulations Standardsaberhaneth1163Ainda não há avaliações
- General Consent Form English 29-IV-09Documento3 páginasGeneral Consent Form English 29-IV-09rubenguzAinda não há avaliações
- Medication ErrorDocumento22 páginasMedication ErrorSulastri LastriAinda não há avaliações
- Hospital Formulary-Lecture NotesDocumento7 páginasHospital Formulary-Lecture NotesPatras BhattiAinda não há avaliações
- Introduction to Clinical PharmacyDocumento54 páginasIntroduction to Clinical PharmacySajid Hassan GhafoorAinda não há avaliações
- New Concept of Pharmacy PracticeDocumento21 páginasNew Concept of Pharmacy PracticeSaddamix AL OmariAinda não há avaliações
- Ward Round Participation - Introduction - : Prepared By: Dr. C. Suhas ReddyDocumento25 páginasWard Round Participation - Introduction - : Prepared By: Dr. C. Suhas Reddysuhas reddyAinda não há avaliações
- Medication Errors Paper 2019Documento6 páginasMedication Errors Paper 2019api-485472556100% (1)
- 5 Morisky Medication Adherence-Scale PDFDocumento1 página5 Morisky Medication Adherence-Scale PDFDellAinda não há avaliações
- Policies and Procedures For Sound-Alike and Look-Alike MedicationsDocumento6 páginasPolicies and Procedures For Sound-Alike and Look-Alike Medicationsrelena badrAinda não há avaliações
- Hospital Formulary DR MotghareDocumento50 páginasHospital Formulary DR MotghareNaveen Kumar50% (2)
- Community Pharmacy Rutter PDF DownloadDocumento2 páginasCommunity Pharmacy Rutter PDF DownloadNicole50% (4)
- Drug Utilization Review (DUR)Documento8 páginasDrug Utilization Review (DUR)Rinta MoonAinda não há avaliações
- Narcotic Controlled and Semi-Controlled Medications ManagementDocumento11 páginasNarcotic Controlled and Semi-Controlled Medications Managementshajahanputhusseri100% (1)
- Medication Therapy ManagementDocumento4 páginasMedication Therapy ManagementAlexandru TibaAinda não há avaliações
- Clinical Pharmacist in ICUDocumento26 páginasClinical Pharmacist in ICUCosmina GeorgianaAinda não há avaliações
- JNC 8 Guideline Algorithm for Treating HypertensionDocumento2 páginasJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- Take As Directed: Your Prescription for Safe Health Care in CanadaNo EverandTake As Directed: Your Prescription for Safe Health Care in CanadaNota: 3.5 de 5 estrelas3.5/5 (14)
- The Nurse Practitioner in UrologyNo EverandThe Nurse Practitioner in UrologyMichelle LajinessAinda não há avaliações
- Contemporary Research Methods in Pharmacy and Health ServicesNo EverandContemporary Research Methods in Pharmacy and Health ServicesAinda não há avaliações
- Lexicon of Pharmacy: A Concise up-to-date referenceNo EverandLexicon of Pharmacy: A Concise up-to-date referenceAinda não há avaliações
- Social and Administrative Aspects of Pharmacy in Low- and Middle-Income Countries: Present Challenges and Future SolutionsNo EverandSocial and Administrative Aspects of Pharmacy in Low- and Middle-Income Countries: Present Challenges and Future SolutionsNota: 1 de 5 estrelas1/5 (1)
- NURSING THE CHILDBEARING FAMILY: Passbooks Study GuideNo EverandNURSING THE CHILDBEARING FAMILY: Passbooks Study GuideAinda não há avaliações
- Manual for Iv Therapy Procedures & Pain Management: Fourth EditionNo EverandManual for Iv Therapy Procedures & Pain Management: Fourth EditionAinda não há avaliações
- Medication Reconciliation Form: Part of The Medical RecordDocumento2 páginasMedication Reconciliation Form: Part of The Medical Recordbella sobaAinda não há avaliações
- New Discharge PolicyDocumento4 páginasNew Discharge PolicywLiAinda não há avaliações
- SB Toledo: (A) Policy StatementDocumento2 páginasSB Toledo: (A) Policy StatementSofie DyahAinda não há avaliações
- Responsibilities and Principles of Drug AdministrationDocumento3 páginasResponsibilities and Principles of Drug AdministrationJessica RogersAinda não há avaliações
- Medication Errors: Causes, Types & PreventionDocumento4 páginasMedication Errors: Causes, Types & PreventionJoyce TanAinda não há avaliações
- Kwhs Medication Test Final Revision Feb 11Documento8 páginasKwhs Medication Test Final Revision Feb 11api-2424364910% (1)
- Pharmaceutics 1 (Chapter 7 To 11) BOOKDocumento58 páginasPharmaceutics 1 (Chapter 7 To 11) BOOKshahida hassanAinda não há avaliações
- Interpreting prescriptions and medication orders at Al-Mustaqbal University CollegeDocumento16 páginasInterpreting prescriptions and medication orders at Al-Mustaqbal University Collegejbbhh nbbbvvgAinda não há avaliações
- Good Dispensing Practice On PharmacyDocumento23 páginasGood Dispensing Practice On PharmacySamantha Revantad100% (1)
- Core Assignment 4 PDFDocumento5 páginasCore Assignment 4 PDFGoAinda não há avaliações
- Mar ChecklistDocumento18 páginasMar ChecklistMin MawAinda não há avaliações
- (Dispensing 1 Laboratory) Review NotesDocumento12 páginas(Dispensing 1 Laboratory) Review NotesZen HeartAinda não há avaliações
- Prescription Writing - HandoutDocumento3 páginasPrescription Writing - HandouthabbouraAinda não há avaliações
- JD Pharmacy TechnologistDocumento3 páginasJD Pharmacy Technologistpeter mulilaAinda não há avaliações
- Writing Medical Orders, Transcribing MedicationDocumento3 páginasWriting Medical Orders, Transcribing MedicationAgus IsmailAinda não há avaliações
- Core Standards For Handling Medicines in Community Teams - Version 4 - April 17Documento11 páginasCore Standards For Handling Medicines in Community Teams - Version 4 - April 17Liza GomezAinda não há avaliações
- If The Bladder Is Not Completely Emptied ..Documento1 páginaIf The Bladder Is Not Completely Emptied ..Christian RobbyAinda não há avaliações
- Brochure Splash MaticDocumento2 páginasBrochure Splash MaticChristian RobbyAinda não há avaliações
- EvakuasiDocumento4 páginasEvakuasiRima DinaAinda não há avaliações
- Guideline TBC AustraliaDocumento145 páginasGuideline TBC AustraliaChristian RobbyAinda não há avaliações
- Pediatric Protokol EmergencyDocumento19 páginasPediatric Protokol EmergencyChristian RobbyAinda não há avaliações
- Drug in Pregnancy InfoDocumento3 páginasDrug in Pregnancy InfoChristian RobbyAinda não há avaliações
- Obat Pada Kehamilan Dan LaktasiDocumento11 páginasObat Pada Kehamilan Dan LaktasiChristian RobbyAinda não há avaliações
- Drug in Pregnancy InfoDocumento3 páginasDrug in Pregnancy InfoChristian RobbyAinda não há avaliações
- Drug in Pregnancy InfoDocumento3 páginasDrug in Pregnancy InfoChristian RobbyAinda não há avaliações
- Developing Nursing Care Plans: Continuing Professional DevelopmentDocumento10 páginasDeveloping Nursing Care Plans: Continuing Professional DevelopmentHilal NorAinda não há avaliações
- Antithrombotic Treatment GuidelinesDocumento9 páginasAntithrombotic Treatment GuidelinesAnh NguyenAinda não há avaliações
- 2018 ESMO Handbook of Interpreting Oncological Study PublicationsDocumento219 páginas2018 ESMO Handbook of Interpreting Oncological Study PublicationsAlex Lugli100% (1)
- Rogelio P. Nogales Et Al vs. CMC, Dr. Oscar Estrada Et Al - gr142625Documento5 páginasRogelio P. Nogales Et Al vs. CMC, Dr. Oscar Estrada Et Al - gr142625Dani EsequeAinda não há avaliações
- RSP20110601Documento64 páginasRSP20110601Abhinav SinghalAinda não há avaliações
- Guidelines Rh D Immunoglobulin Use ObstetricsDocumento3 páginasGuidelines Rh D Immunoglobulin Use Obstetricsbenjamin890333Ainda não há avaliações
- Maternal-Newborn Nursing AbbreviationsDocumento7 páginasMaternal-Newborn Nursing AbbreviationsPallaviAinda não há avaliações
- Virginity and DeflorationDocumento11 páginasVirginity and DeflorationNehru Valdenarro Valera0% (1)
- Obesity and Diabetes Genetic Variants Associated With Gestational Weight GainDocumento17 páginasObesity and Diabetes Genetic Variants Associated With Gestational Weight GainEgie Nugraha Fitriyan ApriyadiAinda não há avaliações
- Cervical Cancer Diagnosis and ManagementDocumento128 páginasCervical Cancer Diagnosis and Managementnicewan0% (1)
- 1-Mini-implant-miniscrews in Orthodontics-oussama Sandid- Mohamad Aboualnaser-Awatef Shaar-maria Doughan-miniscrews Mini-implant en Orthodontie- Beirut- Lebanon- France- Usa -Dentist - Orthodontist-dentistry school beirut arab university zaarourieh zaarourieDocumento129 páginas1-Mini-implant-miniscrews in Orthodontics-oussama Sandid- Mohamad Aboualnaser-Awatef Shaar-maria Doughan-miniscrews Mini-implant en Orthodontie- Beirut- Lebanon- France- Usa -Dentist - Orthodontist-dentistry school beirut arab university zaarourieh zaarourieAnonymous oD9H6T8p100% (2)
- Thermage: The Non Ablative Radiofrequency For RejuvenationDocumento6 páginasThermage: The Non Ablative Radiofrequency For RejuvenationJosé GálvezAinda não há avaliações
- DR K Chan - Ecg For SVT Made EasyDocumento66 páginasDR K Chan - Ecg For SVT Made Easyapi-346486620Ainda não há avaliações
- Logiq c5 BrochureDocumento2 páginasLogiq c5 BrochureFabio PappalardoAinda não há avaliações
- 641 1769 1 PBDocumento8 páginas641 1769 1 PBHira DamayantiAinda não há avaliações
- Chapter 32 - Labor and Birth ComplicationsDocumento14 páginasChapter 32 - Labor and Birth ComplicationsJill Hill100% (6)
- Grossing Uterus Presentation1Documento19 páginasGrossing Uterus Presentation1jayesh saha100% (1)
- Maternity Magazine 2012 - 2013 PDFDocumento212 páginasMaternity Magazine 2012 - 2013 PDFMaria Carolina LowenAinda não há avaliações
- Diagnosing Cephalopelvic Disproportion: A Review of Clinical Assessment TechniquesDocumento12 páginasDiagnosing Cephalopelvic Disproportion: A Review of Clinical Assessment TechniquesArjun RameshAinda não há avaliações
- Vaginal Examination Wit RationaleDocumento1 páginaVaginal Examination Wit RationaleAna Maria Teresa H RollanAinda não há avaliações
- CPT ComprehensiveDocumento14 páginasCPT Comprehensivesha100% (1)
- Acute Cholecystitis CaseDocumento16 páginasAcute Cholecystitis CaseZharif Fikri100% (3)
- HANDLING DELIVERIESDocumento396 páginasHANDLING DELIVERIESTrishaAinda não há avaliações
- Therapy LasersDocumento12 páginasTherapy LasersFrenchySan JinAinda não há avaliações
- AIIMS and All India PGMEE: Review QuestionsDocumento11 páginasAIIMS and All India PGMEE: Review QuestionsAnonymous RnGlkT53100% (1)
- Uterinefibroids 130120064643 Phpapp02Documento73 páginasUterinefibroids 130120064643 Phpapp02Tharun KumarAinda não há avaliações
- Labor & DeliveryDocumento28 páginasLabor & DeliveryVenice Joy Toledo-Malonzo,RN100% (1)
- De Ocampo, Pinky Rose Mojica: Lpu - St. Cabrini College of Allied Medicine, Inc ODC Form 5Documento1 páginaDe Ocampo, Pinky Rose Mojica: Lpu - St. Cabrini College of Allied Medicine, Inc ODC Form 5Pinky TenshiAinda não há avaliações
- Catalog Seturi MedicaleDocumento239 páginasCatalog Seturi MedicaleVasile GabrielAinda não há avaliações
- RN To BSN PlanDocumento5 páginasRN To BSN Planapi-251976678Ainda não há avaliações