Escolar Documentos
Profissional Documentos
Cultura Documentos
Proliferative Diabetic Retinopathy in Type 2 Diabetes Is Related To Coronary Artery Calcium in The Veterans Affairs Diabetes Trial (VADT)
Enviado por
cyneuronDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Proliferative Diabetic Retinopathy in Type 2 Diabetes Is Related To Coronary Artery Calcium in The Veterans Affairs Diabetes Trial (VADT)
Enviado por
cyneuronDireitos autorais:
Formatos disponíveis
Pathophysiology/Complications
O R I G I N A L A R T I C L E
Proliferative Diabetic Retinopathy in Type
2 Diabetes Is Related to Coronary Artery
Calcium in the Veterans Affairs Diabetes
Trial (VADT)
PETER D. REAVEN, MD1 KATHY GLANDER, BBA4 ship appears to be present in both type 1
NICHOLAS EMANUELE, MD2 WILLIAM DUCKWORTH, MD1 and type 2 diabetes (4 –11). Importantly,
THOMAS MORITZ, PHD3 CARLOS ABRAIRA, MD5 most (4,5,7–11), but not all (9), of these
RONALD KLEIN, MD4 FOR THE VETERANS AFFAIRS DIABETES studies have indicated that retinopathy
MATHEW DAVIS, MD4 TRIAL (VADT)* may be independently associated with
CVD events or mortality even after taking
into account standard cardiovascular risk
OBJECTIVE — Increasing evidence suggests that macrovascular disease and retinopathy may factors, diabetes duration, and/or glyce-
be more closely linked than previously believed. We determined the relationship between mic control. Results from these studies
retinopathy and coronary atherosclerosis as measured by computed tomography– detectable suggest that there may be shared risk fac-
coronary artery calcium (CAC).
tors or mechanisms underlying both reti-
RESEARCH DESIGN AND METHODS — The cross-sectional association between nopathy and clinical CVD and that the
CAC and retinopathy was assessed on a Veteran Affairs Diabetes Trial subsample of 204 subjects relationship does not appear to be ex-
with a mean duration of type 2 diabetes of 12.3 ⫾ 8.3 years. plained by standard cardiovascular risk
factors or glycemic control. This raises the
RESULTS — Retinopathy was correlated with CAC (r ⫽ 0.19, P ⫽ 0.006). Median CAC possibility that other novel risk factors or
increased across retinopathy categories: 197 in those with no retinopathy, 229 in those with disease pathways may contribute to both
microaneurysms only, 364 in those with mild nonproliferative diabetic retinopathy (NPDR), 300 retinopathy and CVD.
in those with moderate to severe NPDR, and 981 in those with proliferative diabetic retinopathy Because studies to date have been
(PDR). Stepwise multivariable linear regression analysis was performed to find a parsimonious generally limited to understanding the re-
subset of relevant risk factors to include along with PDR in predicting CAC. After adjustment for
lationship of retinopathy to CVD clinical
either this subset of standard factors (P ⫽ 0.047) or a more extensive panel of risk factors (P ⫽
0.035), PDR was significantly associated with CAC. Moreover, using logistic regression, indi- events, it is unclear whether these shared
viduals with PDR were approximately sixfold more likely to have CAC ⬎400 than those with no risk factors or disease mechanisms con-
PDR, even after adjustment for other CVD risk factors. tribute to these events through thrombo-
sis, plaque instability, or atherosclerosis.
CONCLUSIONS — These data indicate an important relationship between retinopathy and Better understanding of these events will
extent of CAC and suggest the potential to identify and treat shared risk factors for these common not only provide direction toward identi-
micro- and macrovascular complications. fying the novel factors underlying the
relationship between micro- and macro-
Diabetes Care 31:952–957, 2008 vascular disease but may also provide
insight into how to best use the rela-
T
here is increasing evidence that in- has been well described (1–3), studies tively easily assessed microvascular dis-
dividuals with microvascular com- now suggest that retinopathy may also be ease to predict risk of macrovascular
plications of diabetes are also at associated with cardiovascular disease disease.
increased risk for clinical complications (CVD). In fact, retinopathy, especially Thus, in this study we sought to in-
of macrovascular diseases such as myo- proliferative diabetic retinopathy (PDR), vestigate the association of retinopathy
cardial infarctions and cardiovascular is associated with incident coronary heart with a direct measure of coronary athero-
mortality. Although the relationship of disease events, CVD events, and cardio- sclerosis burden (by measuring coronary
microalbuminuria with vascular disease vascular mortality (4 –11). This relation- artery calcium [CAC]) in a subset of well-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● characterized individuals with type 2 di-
abetes that are participating in the Veteran
From the 1Carl T. Hayden VA Medical Center, Phoenix, Arizona; the 2Edward Hines, Jr., VA Hospital, Hines,
Illinois; the 3Cooperative Studies Program Coordinating Center, Edward Hines, Jr., VA Hospital, Hines, Affairs Diabetes Trial (VADT) of tight gly-
Illinois; the 4University of Wisconsin, Madison, Wisconsin; and the 5Miami VA Medical Center, Miami, cemic control.
Florida.
Corresponding author: Peter Reaven, MD, Phoenix VAMC, 650 E. Indian School Road (111E), Phoenix, RESEARCH DESIGN AND
AZ 85012-1892. E-mail: peter.reaven@va.gov.
Received for publication 9 October 2007 and accepted in revised form 10 February 2008. METHODS — Data for this study de-
Published ahead of print at http://care.diabetesjournals.org on 3 March 2008. DOI: 10.2337/dc07-1926. rive from baseline examinations of partic-
*A complete list of participating investigators is available in the APPENDIX. ipants in the Risk Factors, Atherosclerosis
Abbreviations: CAC, coronary artery calcium; CVD, cardiovascular disease; NPDR, nonproliferative and Clinical Events in Diabetes (RACED)
diabetic retinopathy; PDR, proliferative diabetic retinopathy; VADT, Veterans Affairs Diabetes Trial.
© 2008 by the American Diabetes Association.
study (12), a seven-site substudy of the
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby VADT. A detailed description of the
marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. VADT with exclusion and inclusion crite-
952 DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008
Reaven and Associates
ria has been previously described (13). blinded to the demographic and clinical ble 1 are characteristics of the population
Approximately 95% of all subjects who information, performed calcium scoring. across categories of retinopathy. Age,
were recruited into the VADT study, at A threshold of 4 pixels and 130 BMI, history of smoking, hypertension,
sites participating in the RACED study, Hounsfield units was used for identifica- and CVD history, as well as values of A1C
also agreed to receive coronary calcium tion of calcified lesions. Each focus ex- and LDL and HDL cholesterol, were not
scans. ceeding the minimum volume criteria was significantly different between groups.
The VADT baseline examination in- scored using the algorithm developed by While total cholesterol and triglyceride
cluded a medical history, physical exam- Agatston et al. (18). Total coronary cal- levels did vary between groups, only du-
ination, and collection of blood for cium scores were determined by sum- ration of diabetes and insulin use showed
measurement of traditional cardiovascu- ming individual lesion scores from each a clear increasing trend across categories
lar risk factors. Height and weight were of four anatomic sites (left main, left an- (from no retinopathy to PDR).
measured to the nearest 0.1 cm and 0.5 terior descending, circumflex, and right To investigate the potential relation-
kg, respectively, and BMI (weight in kilo- coronary arteries). A calibration phantom ship between retinopathy and CAC, we
grams divided by the square of height in was scanned under the chests of each par- first determined that retinopathy (Early
meters) was calculated. Information re- ticipant at each scanning center to allow Treatment of Diabetic Retinopathy Study
garding current medical health status in- calibration of the images to identical stan- scores) was significantly correlated with
cluding history of diabetes, hypertension, dards, as previously described (12,17). CAC (r ⫽ 0.19, P ⫽ 0.006). We then ex-
prior CVD, and medication use was col- amined the median CAC score across ret-
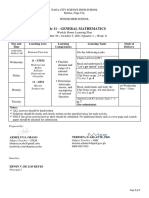
lected by a questionnaire administered by Statistical analyses inopathy categories (Fig. 1). For those
research staff as previously described Statistical analyses were performed with with no retinopathy, the median CAC
(13). A non-Hispanic white variable was the SAS statistical package (release 8.2; score was 197; for microaneurysm only,
generated because this race-ethnicity SAS Institute, Cary, NC). For the descrip- 229; for mild NPDR, 364; and for moder-
grouping effectively identifies those with tion of the data parameters with a normal ate to severe NPDR, 300. Most striking
greater CAC in this and other cohorts distribution, means ⫾ SD are reported. was the significantly higher CAC values in
(12,14,15). All laboratory assays, includ- Parameters with a skewed distribution are individuals with PDR: 981 (P ⬍ 0.01).
ing plasma total cholesterol, triglycerides, reported as medians (interquartile range), To determine whether the association
HDL cholesterol concentrations, and and proportions are given for categorical between PDR and CAC was independent
A1C, were measured in the central labo- variables. Significant differences between of other standard risk factors for these
ratory at Tufts University. Lipid values the levels of retinopathy were assessed us- conditions, we first performed multivari-
were assayed using standard enzymatic ing one-way ANOVA or the Kruskal- able linear regression analyses. To avoid
methods, and LDL cholesterol was calcu- Wallis where appropriate. Linear and over-fitting of the models, we chose to
lated using the Friedewald equation. A1C logistic regression models were used to initially limit the number of variables in-
was measured using an immunoaffinity investigate the association of CAC with cluded to those with evidence of relevant
method that was referenced against the risk factors, including retinopathy. The model effects. Therefore, stepwise vari-
national standard methodology as de- log of CAC ⫹ 1 was used to include pa- able selection was initially performed to
rived from the Diabetes Control and tients with a score of zero in the linear find a parsimonious subset of risk factors
Complications Trial (13). Urinary protein regression models. Univariate linear re- to include along with PDR in predicting
and creatinine were measured on random gression analysis was applied to examine CAC. After adjustment for these factors
morning urine samples, and an albumin- the association of CAC with each covari- (age, non-Hispanic white status, HDL
to-creatinine ratio was calculated. ate. Stepwise regression models were cholesterol, insulin use, and prior CVD
created to find appropriate and parsimo- events), PDR was significantly (P ⫽
Assessment of retinopathy nious subsets of traditional risk factors to 0.047) associated with CAC (Table 2).
Patients consented to a set of seven-field include in the initial multivariate linear This translated into an ⬃3.2-fold increase
standard 30° stereoscopic color photo- (and logistic) regression analyses in order in individuals’ CAC scores if PDR was
graphs of both eyes at the baseline exam to investigate the independent association present. Interestingly, the  coefficients
according to the Diabetes Retinopathy of retinopathy with CAC. Subsequent re- and P values for the other variables
Study protocol (13). The Fundus Photo- gression analyses contained additional changed very little (data not shown) when
graph Reading Center of the University of risk factors to provide more complete PDR was included in the model, suggest-
Wisconsin assessed the photographs us- models for presentation. ing that the association between PDR and
ing the Early Treatment Diabetic Retinop- CAC does not appear to be mediated
athy Study modification of the Airlie RESULTS — Our study population in- through these other risk factors. The ad-
House classification and severity scale; cluded 204 subjects with type 2 diabetes dition of variables such as BMI, smoking,
the score from the eye with the most se- with a mean diabetes duration of 12.3 ⫾ hypertension history, A1C, diabetes du-
vere retinopathy was used (16). 8.3 years and had characteristics very ration, lipid levels, and albumin-to-
similar to those of the overall VADT co- creatinine ratio in the models was found
Assessment of CAC scores hort (38). The majority of subjects were to not contribute to the extent of CAC and
CAC was determined by electron-beam male (95%) and non-Hispanic white increased the strength of the PDR-CAC
computed tomography cardiac scanning (70%), with a mean age of 62.0 ⫾ 9.2 relationship (Table 2).
using Imatron C150XL scanners (GE years. Prevalence of hypertension (80%) We also explored the relationship of
Imatron, South San Francisco, CA) as pre- and a prior history of smoking (70%) was PDR with common clinical categories of
viously described (12,17). Readers at the high in this population, and 39% had CAC (0 –10, 11–100, 101– 400, and
centralized reading center, which were some prior history of CVD. Shown in Ta- ⬎400), recognizing that prior studies
DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008 953
Diabetic retinopathy and atherosclerosis
Table 1—Subject characteristics by retinopathy category
Mild Moderate to
Total No retinopathy Microaneurysms NPDR severe NPDR PDR P
n 204 68 37 49 35 15
Age (years) 62.0 60.0 60.6 64.7 63.3 62.4 0.07
BMI (kg/m2) 31.4 31.5 31.5 30.7 32.1 31.2 0.67
Diabetes duration (years) 12.3 8.9 11.2 13.3 15.0 21.3 0.01
Smoker (%) 16 19 21 8 17 8 0.33
Non-Hispanic white (%) 70 71 60 63 83 80 0.19
Hypertension (%) 80 78 74 80 89 93 0.34
A1C (%) 9.2 9.2 8.9 9.2 9.3 9.6 0.63
Total cholesterol (mg/dl) 176 187 176 171 162 173 0.01
Median triglycerides (mg/dl) 157 184 151 141 138 179 0.01
LDL cholesterol (mg/dl) 102 110 99 102 93 97 0.06
HDL cholesterol (mg/dl) 36 36 36 38 36 37 0.80
Insulin use (%) 60 53 42 71 69 87 0.005
Median urinary albumin-to-creatinine ratio 16.5 15.5 8.0 13.0 40.5 39.0 0.01
(g/mg)
CVD (%) 30 24 32 27 37 60 0.07
Data are means except where indicated.
have demonstrated that individuals with tors assessed in these models, age, non- tive model was used that included many
CAC ⬎400 are at very high risk for prev- Hispanic white status, prior CVD events, additional risk factors (Table 3).
alent and incident CVD. Impressively, in and PDR were all significantly associated
80% of the subjects with PDR, CAC was with CAC ⬎400 (Table 3). In fact, indi-
⬎400 (P ⫽ 0.001), and 100% of the sub- CONCLUSIONS — Our data show a
viduals with PDR were over sixfold more rather striking relationship between dia-
jects with PDR had CAC scores ⬎250. likely to have CAC ⬎400 than those with
To determine whether this strong as- betic retinopathy, especially PDR, and
no PDR, even after adjustment for other coronary calcium deposition, a reliable
sociation between PDR and the highest CVD risk factors. Similar or higher odds
risk category of CAC scores was explained estimate of coronary atherosclerosis. This
ratios for PDR were also present in models relationship was present whether CAC
by factors other than retinopathy, we per- that excluded women or all subjects with
formed multivariable logistic regression was assessed as a continuous outcome or
known CVD disease or when a less selec- in clinical categories. In fact, in this cohort
analyses. Of the many standard risk fac-
of 204 patients, 80% of the individuals
who had PDR had CAC scores ⬎400.
Thus, the presence of PDR was associated
with a greater than sixfold increased risk
of having CAC ⬎400, a value that is in-
creasingly recognized as placing individ-
uals at a particularly high risk for future
clinical cardiovascular events (19,20).
Because of the moderate sample size
of this substudy, variable selection proce-
dures were initially used in order to dis-
card less statistically important factors
and thus identify relevant factors that
could be included, along with PDR, in
models to predict CAC. In these analyses
and in subsequent more complete mod-
els, it did not appear that BMI, hyperten-
sion, lipid levels (other than HDL
cholesterol), A1C, smoking history, or
even the more novel risk factors plasmin-
ogen activator inhibitor-1 or fibrinogen
(data not shown) were useful in predict-
ing CAC. Although plasma cholesterol
levels and blood pressure abnormalities
Figure 1—CAC scores by retinopathy category. Median (25th-75th percentile range) values are have been associated with CAC in some
presented. Differences between the levels of retinopathy were assessed using Kruskal-Wallis. NL, but not all studies (21–27), these associ-
no retinopathy; MA, microaneurysms; M/S, moderate to severe. P ⬍ 0.01. ations may be more difficult to identify in
954 DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008
Reaven and Associates
Table 2—Multivariate linear regression model with the dependent variable log (CAC ⴙ 1) been proposed to account for diabetic ret-
inopathy, including polyol accumulation,
 SE of  P oxidative damage, formation of advanced
glycation end products, stimulation of ac-
Age (per 10 years) 0.440 0.07 ⬍0.001 tivation pathways such as PKC, and in-
Non-Hispanic white vs. other 0.312 0.141 0.028 creased levels of various growth factors
HDL cholesterol (per 5 mg/dl) ⫺0.090 0.035 0.007 (33–35). Each of these pathways has also
Insulin use (yes/no) 0.395 0.135 0.004 been implicated in the initiation and/or
CVD at baseline (yes/no) 0.761 0.145 ⬍0.001 progression of atherosclerosis. In addi-
PDR (yes/no) 0.497 0.249 0.047 tion, ischemia of small retinal vessels is
PDR (yes/no)* 0.608 0.287 0.035 believed to be particularly relevant for the
*Adjusted for the above-shown variables as well as BMI, duration of diabetes, smoking, A1C, total choles- development of new vessel proliferation
terol, triglycerides, history of hypertension, and urinary albumin-to-creatinine ratio. For this more complete
model, n ⫽ 195 (PDR ⫽ 15) instead of the original 204, as not all measures were available.
in the retina (36). Similarly, recent studies
have also implicated the contribution of
plaque ischemia and small vessel angio-
an older cohort of subjects with diabetes Our study has several unique advan- genesis in progression of atherogenesis
that receives numerous medications for tages compared with previous studies. (37). Thus, there are clearly several novel
these conditions. Consistent with other Whereas many of the prior studies only pathways that may contribute to both ret-
reports (12,17,27–29), age, HDL choles- used opthalmoscopic exams or one- or inopathy and atherosclerosis and may
terol, race-ethnicity status, and prior CVD two-field retinal photographs of one or help explain our demonstration of a close
were each significantly related to CAC. In- occasionally both eyes, the current study relationship between PDR and atheroscle-
terestingly, baseline use of insulin, possi- used the gold standard seven-field stereo-
rosis. Measurement of novel risk factors
bly because it indicates long-standing and scopic color photographs of both eyes to
that will reflect activity of these pathways
complicated diabetes, was also a signifi- provide a more sensitive and comprehen-
and processes are needed in future studies
cant predictor of coronary atherosclerosis sive assessment of retinopathy. In addi-
to provide further insight into the specific
burden. However, PDR remained associ- tion, the fundus photographs were
mechanisms that underlay the association
ated with CAC, even after adjusting for centrally analyzed at the Retinopathy
these factors. Thus, the relationship be- Reading Center at the University of Wis- of retinopathy with atherosclerosis.
tween PDR and CAC score could not fully consin, a facility with extensive experi- Several limitations of this study de-
be accounted for by traditional historical ence in retinopathy assessment for many serve mention. Because this is a cross-
or laboratory-measured cardiovascular landmark clinical studies of retinopathy. sectional study, and the subcohort of the
risk factors. These data, therefore, pro- Moreover, this study clearly demonstrates VADT has a relatively modest number of
vide additional support for the hypothesis that there is a direct relationship of reti- subjects with PDR that are predominantly
that PDR and CAC share a common un- nopathy, and PDR in particular, not just male, we recognize that these novel find-
derlying pathophysiology that may be with CVD events as previously shown, ings need confirmation in larger cohorts
mediated, at least in part, by nontradi- but also with the burden of coronary ath- with greater female representation and in
tional risk factors. erosclerosis. Of note, this association re- prospective studies. Importantly, this
One potential implication of a strong mained robust and significant using subset of subjects with coronary calcium
and independent relationship between several different approaches to analyze scans appears to have demographic and
retinopathy, especially PDR, and severe CAC. Only one other study, comprised of risk factor characteristics similar to those
coronary atherosclerosis is that the non- a small group of patients preselected for of the entire diabetic cohort of the VADT
invasive measurement of PDR, in combi- suspected CVD, has explored the rela- (38). Similarly, the percentages of indi-
nation with standard risk factors, may tionship between retinopathy and coro- viduals in this cohort with mild or moder-
provide a relatively useful assessment of nary atherosclerosis and demonstrated a ate/severe NPDR and PDR are essentially
clinically relevant atherosclerosis. This relationship between retinopathy, as- the same as those recently reported in the
possibility deserves evaluation in addi- sessed during opthalmoscopic fundus ex- overall VADT population (39). For these
tional studies. ams, and coronary angiogram severity reasons, and because the substudy is being
These results are consistent with sev- (32). conducted at seven sites around the coun-
eral prior studies demonstrating that mi- Several biochemical pathways have try, we believe that the results from these
crovascular disease is related to both
macrovascular disease events and overall Table 3—Multivariate logistic regression model with the dependent variable CAC >400
mortality (2,3). In fact, substantial evi-
dence now exists that both microalbu-
minuria and retinopathy are independent OR CI P
risk factors for CVD events and mortality Age (per 10 years) 2.2 1.4–3.4 0.0003
(2–5,7–11,30). Although the studies in Non-Hispanic white vs. other 2.8 1.2–6.5 0.02
type 1 diabetes are limited in number CVD at baseline (yes/no) 14.8 6.4–33.8 ⬍0.001
(9,31), this relationship between retinop- PDR (yes/no) 6.2 1.3–29.2 0.022
athy and CVD is present in both type 1 PDR (yes/no)* 9.0 1.7–49.2 0.011
and type 2 diabetic populations and ap- *Adjusted for the above-shown variables as well as BMI, duration of diabetes, smoking, A1C, total choles-
pears strongest for proliferative retinopa- terol, triglycerides, history of hypertension, and urinary albumin-to-creatinine ratio. For this more complete
thy (4,5,7–11). model, n ⫽ 195 (PDR ⫽ 15) instead of the original 204, as not all measures were available.
DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008 955
Diabetic retinopathy and atherosclerosis
individuals are representative of the larger cardiovascular disease. J Am Soc Nephrol glycemic control and complications in di-
VA population. 17:2100 –2105, 2006 abetes mellitus type 2: Veterans Affairs
In summary, these data indicate a sur- 2. Yuyun MF, Adler AI, Wareham NJ: What Diabetes Trial. J Diabetes Complications
prising relationship between retinopathy is the evidence that microalbuminuria 17:314 –322, 2003
is a predictor of cardiovascular disease 14. Reaven PD, Thurmond D, Domb A, Ger-
and the extent of CAC and, if confirmed
events? Curr Opin Nephrol Hypertens 14: kin R, Budoff MJ, Goldman S: Compari-
in other studies, suggest that identifying 271–276, 2005 son of frequency of coronary artery
type 2 diabetic patients with PDR may 3. Valmadrid CT, Klein R, Moss SE, Klein calcium in healthy Hispanic versus non-
help ascertain who is at uniquely high risk BE: The risk of cardiovascular disease Hispanic white men by electron beam
for clinical CVD, indicating that it may be mortality associated with microalbumin- computed tomography. Am J Cardiol 92:
possible to identify and treat shared risk uria and gross proteinuria in persons with 1198 –1200, 2003
factors for these common micro- and ma- older-onset diabetes mellitus. Arch Intern 15. Bild DE, Detrano R, Peterson D, Guerci A,
crovascular complications. Med 160:1093–1100, 2000 Liu K, Shahar E, Ouyang P, Jackson S,
4. Hiller R, Sperduto RD, Podgor MJ, Ferris Saad MF: Ethnic differences in coronary
FL 3rd, Wilson PW: Diabetic retinopathy calcification: the Multi-Ethnic Study of
APPENDIX
and cardiovascular disease in type II dia- Atherosclerosis (MESA). Circulation 111:
betics: the Framingham Heart Study and 1313–1320, 2005
Additional Participating the Framingham Eye Study. Am J Epide- 16. Emanuele N, Klein R, Abraira C, Colwell
Investigators miol 128:402– 409, 1988 J, Comstock J, Henderson WG, Levin S,
Christian Meyer, MD, John Matchette, 5. Miettinen H, Haffner SM, Lehto S, Ronne- Nuttall F, Sawin C, Silbert C, Lee HS,
PA, Dawn Schwenke, PhD, Phoenix maa T, Pyorala K, Laakso M: Retinopathy Johnson-Nagel N: Evaluations of retinop-
VAMC; Jayendrah H. Shah, MD, South- predicts coronary heart disease events in athy in the VA Cooperative Study on Gly-
ern Arizona VA Health Care System; NIDDM patients. Diabetes Care 19:1445– cemic Control and Complications in Type
Sundar Muduliar, MD, Robert Henry, 1448, 1996 II Diabetes (VA CSDM): a feasibility
MD, VA San Diego Healthcare System; 6. Klein R, Marino EK, Kuller LH, Polak JF, study. Diabetes Care 19:1375–1381,
Tracy RP, Gottdiener JS, Burke GL, Hub- 1996
Moti Kayshap, MD, Long Beach VAMC;
bard LD, Boineau R: The relation of ath- 17. Reaven PD, Sacks J: Coronary artery and
Jennifer B. Marks, MD, Hermes Florez, erosclerotic cardiovascular disease to abdominal aortic calcification are associ-
Miami VAMC; R. Harsha Rao, MD, VA retinopathy in people with diabetes in the ated with cardiovascular disease in type 2
Pittsburgh Healthcare System; Nasrin Cardiovascular Health Study. Br J Oph- diabetes. Diabetologia 48:379 –385, 2005
Azad, MD, Lily Agrawal, MD, Hines VA thalmol 86:84 –90, 2002 18. Agatston AS, Janowitz WR, Hildner FJ,
Hospital; Steven Goldman, MD, Southern 7. Cheung N, Wang JJ, Klein R, Couper DJ, Zusmer NR, Viamonte M Jr, Detrano R:
Arizona VA Health Care System; Michael Sharrett AR, Wong TY: Diabetic retinop- Quantification of coronary artery calcium
Criqui, MPH, MD, University of Califor- athy and the risk of coronary heart disease: using ultrafast computed tomography.
nia, San Diego; Robert Detrano, MD, Uni- the Atherosclerosis Risk in Communities J Am Coll Cardiol 15:827– 832, 1990
versity of California, Irvine; Mathew Study. Diabetes Care 30:1742–1746, 2007 19. Rumberger JA, Brundage BH, Rader DJ,
Budoff, MD, Harbor UCLA Medical Cen- 8. Rajala U, Pajunpaa H, Koskela P, Kein- Kondos G: Electron beam computed to-
anen-Kiukaanniemi S: High cardiovascu- mographic coronary calcium scanning: a
ter; Michael Wright, MD, University of lar disease mortality in subjects with review and guidelines for use in asymp-
California, San Diego; George Kondos, visual impairment caused by diabetic ret- tomatic persons. Mayo Clin Proc 74:243–
MD, University of Illinois, Chicago Med- inopathy. Diabetes Care 23:957–961, 252, 1999
ical Center; Steven Reis, MD, University 2000 20. Greenland P, Bonow RO, Brundage BH,
of Pittsburgh Medical Center; and Joseph 9. van Hecke MV, Dekker JM, Stehouwer Budoff MJ, Eisenberg MJ, Grundy SM,
Horgan, MD, Health Test Scan Center. CD, Polak BC, Fuller JH, Sjolie AK, Kofi- Lauer MS, Post WS, Raggi P, Redberg RF,
nis A, Rottiers R, Porta M, Chaturvedi N: Rodgers GP, Shaw LJ, Taylor AJ, Wein-
Diabetic retinopathy is associated with traub WS: ACCF/AHA 2007 clinical ex-
Acknowledgments — Financial support was mortality and cardiovascular disease inci- pert consensus document on coronary
provided by the Department of Veterans Af- dence: the EURODIAB prospective com- artery calcium scoring by computed to-
fairs Cooperative Studies Program of the VA plications study. Diabetes Care 28:1383– mography in global cardiovascular risk
Office of Research and Development, National 1389, 2005 assessment and in evaluation of patients
Institutes of Health Grant RO1067690, the 10. Juutilainen A, Lehto S, Ronnemaa T, with chest pain. J Am Coll Cardiol 49:378 –
Kronos Research Institute, and a clinical re- Pyorala K, Laakso M: Retinopathy pre- 402, 2007
search award from the American Diabetes As- dicts cardiovascular mortality in type 2 21. Bild DE, Folsom AR, Lowe LP, Sidney S,
sociation. diabetic men and women. Diabetes Care Kiefe C, Westfall AO, Zheng ZJ, Rum-
We acknowledge the contributions of the 30:292–299, 2007 berger J: Prevalence and correlates of cor-
Hines VA Cooperative Studies Program Coor- 11. Rius Riu F, Salinas Vert I, Lucas Martin A, onary calcification in black and white
dinating Center, the Tufts Lipid Metabolism Romero Gonzalez R, Sanmarti Sala A: A young adults: the Coronary Artery Risk
Laboratory, and the Harbor UCLA EBCT prospective study of cardiovascular dis- Development in Young Adults (CARDIA)
Reading Center. ease in patients with Type 2 diabetes. 6.3 Study. Arterioscler Thromb Vasc Biol 21:
Results from this study were presented in years of follow-up. J Diabetes Complica- 852– 857, 2001
abstract form at the 67th annual meeting of the tions 17:235–242, 2003 22. Kuller LH, Matthews KA, Sutton-Tyrrell
American Diabetes Association, Chicago, Illi- 12. Reaven PD, Sacks J: Reduced coronary ar- K, Edmundowicz D, Bunker CH: Coro-
nois, 22–26 June 2007. tery and abdominal aortic calcification in nary and aortic calcification among
Hispanics with type 2 diabetes. Diabetes women 8 years after menopause and their
Care 27:1115–1120, 2004 premenopausal risk factors: the healthy
References 13. Abraira C, Duckworth W, McCarren M, women study. Arterioscler Thromb Vasc
1. de Zeeuw D, Parving HH, Henning RH: Emanuele N, Arca D, Reda D, Henderson Biol 19:2189 –2198, 1999
Microalbuminuria as an early marker for W: Design of the cooperative study on 23. Reilly MP, Wolfe ML, Localio AR, Rader
956 DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008
Reaven and Associates
DJ: Coronary artery calcification and car- W, Kronmal RA: Distribution of coronary 34. Hardy P, Beauchamp M, Sennlaub F, Go-
diovascular risk factors: impact of the an- artery calcium by race, gender, and age: beil F Jr, Tremblay L, Mwaikambo B,
alytic approach. Atherosclerosis 173:69 – results from the Multi-Ethnic Study of Lachapelle P, Chemtob S: New insights
78, 2004 Atherosclerosis (MESA). Circulation 113: into the retinal circulation: inflammatory
24. Valdes AM, Wolfe ML, Tate HC, Gefter 30 –37, 2006 lipid mediators in ischemic retinopathy.
W, Rut A, Rader DJ: Association of tradi- 29. Folsom AR, Evans GW, Carr JJ, Stillman Prostaglandins Leukot Essent Fatty Acids 72:
tional risk factors with coronary calcifica- AE: Association of traditional and nontra- 301–325, 2005
tion in persons with a family history of ditional cardiovascular risk factors with 35. Lee TS, MacGregor LC, Fluharty SJ, King
premature coronary heart disease: the coronary artery calcification. Angiology GL: Differential regulation of protein ki-
study of the inherited risk of coronary 55:613– 623, 2004 nase C and (Na, K)-adenosine triphos-
atherosclerosis. J Investig Med 49:353– 30. Agardh CD, Agardh E, Torffvit O: The phatase activities by elevated glucose
361, 2001 prognostic value of albuminuria for the levels in retinal capillary endothelial cells.
25. Wolfe ML, Iqbal N, Gefter W, Mohler ER, development of cardiovascular disease J Clin Invest 83:90 –94, 1989
3rd, Rader DJ, Reilly MP: Coronary artery and retinopathy: a 5-year follow-up of 36. Arjamaa O, Nikinmaa M: Oxygen-depen-
calcification at electron beam computed 451 patients with type 2 diabetes melli- dent diseases in the retina: role of hypox-
tomography is increased in asymptomatic tus. Diabetes Res Clin Pract 32:35– 44,
ia-inducible factors. Exp Eye Res 83:473–
type 2 diabetics independent of tradi- 1996
483, 2006
tional risk factors. J Cardiovasc Risk 9: 31. Klein BE, Klein R, McBride PE, Cruicks-
37. Moreno PR, Purushothaman KR, Zias E,
369 –376, 2002 hanks KJ, Palta M, Knudtson MD, Moss
26. Mazzone T, Meyer PM, Kondos GT, Da- SE, Reinke JO: Cardiovascular disease, Sanz J, Fuster V: Neovascularization in
vidson MH, Feinstein SB, D’Agostino RB, mortality, and retinal microvascular char- human atherosclerosis. Curr Mol Med
Sr, Perez A, Haffner SM: Relationship of acteristics in type 1 diabetes: Wisconsin 6:457– 477, 2006
traditional and nontraditional cardiovas- Epidemiologic Study of Diabetic Retinop- 38. Meyers CD, McCarren M, Wong ND,
cular risk factors to coronary artery cal- athy. Arch Intern Med 164:1917–1924, Abraira C, Duckworth WC, Kashyap ML:
cium in type 2 diabetes. Diabetes 56:849 – 2004 Baseline achievement of lipid goals and
855, 2007 32. Norgaz T, Hobikoglu G, Aksu H, Guveli usage of lipid medications in patients with
27. Arad Y, Newstein D, Cadet F, Roth M, A, Aksoy S, Ozer O, Bolca O, Narin A: diabetes mellitus (from the Veterans Af-
Guerci AD: Association of multiple risk Retinopathy is related to the angiographi- fairs Diabetes Trial). Am J Cardiol 98:63–
factors and insulin resistance with in- cally detected severity and extent of coro- 65, 2006
creased prevalence of asymptomatic cor- nary artery disease in patients with type 2 39. Emanuele N, Sacks J, Klein R, Reda D,
onary artery disease by an electron-beam diabetes mellitus. Int Heart J 46:639 –646, Anderson R, Duckworth W, Abraira C:
computed tomographic study. Arterio- 2005 Ethnicity, race, and baseline retinopathy
scler Thromb Vasc Biol 21:2051–2058, 33. Fong DS, Aiello LP, Ferris FL 3rd, Klein R: correlates in the Veterans Affairs Diabe-
2001 Diabetic retinopathy. Diabetes Care 27: tes Trial. Diabetes Care 28:1954 –1958,
28. McClelland RL, Chung H, Detrano R, Post 2540 –2553, 2004 2005
DIABETES CARE, VOLUME 31, NUMBER 5, MAY 2008 957
Você também pode gostar
- Enf Art PerifericaDocumento6 páginasEnf Art PerifericaGIOVANNI ANDRES CADENA CASTAÑEDAAinda não há avaliações
- Lacunar Strokes in Patients With Diabetes Mellitus: Risk Factors, Infarct Location, and PrognosisDocumento6 páginasLacunar Strokes in Patients With Diabetes Mellitus: Risk Factors, Infarct Location, and PrognosisNicole Carolina Quintero RomeroAinda não há avaliações
- MASLD - A Systemic Metabolic Disorder With Cardiovascular and Malignant Complications 2024Documento12 páginasMASLD - A Systemic Metabolic Disorder With Cardiovascular and Malignant Complications 2024draanalordonezv1991Ainda não há avaliações
- Cells 11 04136 v2Documento3 páginasCells 11 04136 v2ayunda rinataAinda não há avaliações
- Left Ventricular Mass As A Predictor of Cardiovascular DiseaseDocumento19 páginasLeft Ventricular Mass As A Predictor of Cardiovascular DiseaseerikafebriyanarAinda não há avaliações
- Ioi60144 2388 2394Documento7 páginasIoi60144 2388 2394orangeshibuya99Ainda não há avaliações
- Heart and Rheumatic DiseasesDocumento6 páginasHeart and Rheumatic DiseasesSergio CerpaAinda não há avaliações
- 08 Tarr Et Al 2012Documento13 páginas08 Tarr Et Al 2012abbhyasa5206Ainda não há avaliações
- Metabolic Syndrome Is An Independent Predictor of Cardiovascular Events in High-Risk Patients With Occlusive and Aneurysmatic Peripheral Arterial DiseaseDocumento6 páginasMetabolic Syndrome Is An Independent Predictor of Cardiovascular Events in High-Risk Patients With Occlusive and Aneurysmatic Peripheral Arterial DiseaseGono GenieAinda não há avaliações
- Diabetes, Pancreatogenic Diabetes, and Pancreatic CancerDocumento8 páginasDiabetes, Pancreatogenic Diabetes, and Pancreatic CancerTeodoraManAinda não há avaliações
- The Relationship Between Retinal Microvascular Abnormalities and Coronary Heart DiseaseDocumento7 páginasThe Relationship Between Retinal Microvascular Abnormalities and Coronary Heart DiseaseMaria Camila RestrepoAinda não há avaliações
- Relationship Between Measures of Adiposity, Arterial Inflammation, and Subsequent Cardiovascular EventsDocumento8 páginasRelationship Between Measures of Adiposity, Arterial Inflammation, and Subsequent Cardiovascular EventsAlejandra MendozaAinda não há avaliações
- BMJDRC 2019 000726Documento11 páginasBMJDRC 2019 000726Pawan MishraAinda não há avaliações
- Malfd AbelDocumento23 páginasMalfd AbelAriel VediaAinda não há avaliações
- Cardiovascular Kidney Metabolic Health SyndromeDocumento4 páginasCardiovascular Kidney Metabolic Health Syndromevali.levo7Ainda não há avaliações
- A Correlation Study of Arterial Stiffness, Cardiac Autonomic Neuropathy and Lipid Profile in Type 2 Diabetes Mellitus PatientsDocumento6 páginasA Correlation Study of Arterial Stiffness, Cardiac Autonomic Neuropathy and Lipid Profile in Type 2 Diabetes Mellitus PatientsvanathyAinda não há avaliações
- Diabetic Retinopathy Screening Update: Epidemiology Pathophysiology and ClassificationDocumento6 páginasDiabetic Retinopathy Screening Update: Epidemiology Pathophysiology and ClassificationAulia Eka PurwaniAinda não há avaliações
- Cardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthDocumento8 páginasCardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthABAinda não há avaliações
- 998 FullDocumento7 páginas998 FullsilviaAinda não há avaliações
- Chapter 4 Other Complications of CKD CVD Medication Dosa 2013 Kidney InteDocumento21 páginasChapter 4 Other Complications of CKD CVD Medication Dosa 2013 Kidney IntewardaninurindahAinda não há avaliações
- Prevalence of Chronic Kidney Disease in Patients With or at A High Risk of Cardiovascular DiseaseDocumento4 páginasPrevalence of Chronic Kidney Disease in Patients With or at A High Risk of Cardiovascular DiseasenuvitaAinda não há avaliações
- Noninvasive Assessment of Plaque Characteristics With Multislice Computed Tomography Coronary Angiography in Symptomatic Diabetic PatientsDocumento7 páginasNoninvasive Assessment of Plaque Characteristics With Multislice Computed Tomography Coronary Angiography in Symptomatic Diabetic PatientscyneuronAinda não há avaliações
- Charytan 2017Documento9 páginasCharytan 2017Andrew E P SunardiAinda não há avaliações
- Aterosclerosis SubclinicaDocumento4 páginasAterosclerosis SubclinicaEnzo GonzalezAinda não há avaliações
- Dysglycemia and Cardiovascular Risk in The General PopulationDocumento4 páginasDysglycemia and Cardiovascular Risk in The General PopulationKevin WewengkangAinda não há avaliações
- 4.-Genetics of Diabetes Mellitus and Diabetes ComplicationsDocumento14 páginas4.-Genetics of Diabetes Mellitus and Diabetes ComplicationsOscar ClementeAinda não há avaliações
- Coutinho 1999Documento8 páginasCoutinho 1999DR VENKATARAMANA MurthyAinda não há avaliações
- Hypertensive Retinopathy Revisited: Some Answers, More QuestionsDocumento9 páginasHypertensive Retinopathy Revisited: Some Answers, More QuestionsPaito MartinezAinda não há avaliações
- CKD Ska2Documento14 páginasCKD Ska2Maya RustamAinda não há avaliações
- Cardiovascular Risk Assessment and Screening in Diabetes: Yanglu ZhaoDocumento6 páginasCardiovascular Risk Assessment and Screening in Diabetes: Yanglu ZhaoEward Rod SalAinda não há avaliações
- Clinical Use of Carotid Intima-Media Thickness: Review of The LiteratureDocumento8 páginasClinical Use of Carotid Intima-Media Thickness: Review of The LiteraturehardianAinda não há avaliações
- Diabetic RetinopathyDocumento11 páginasDiabetic RetinopathyShell PatelAinda não há avaliações
- Guideline Myocarditis AHA ACCDocumento16 páginasGuideline Myocarditis AHA ACCAle PanjaitanAinda não há avaliações
- Diabetes, The Metabolic Syndrome, and Ischemic Stroke: Epidemiology and Possible MechanismsDocumento10 páginasDiabetes, The Metabolic Syndrome, and Ischemic Stroke: Epidemiology and Possible MechanismsFelia AlyciaAinda não há avaliações
- Diabetes, Glucose Level, and Risk of Sudden Cardiac DeathDocumento6 páginasDiabetes, Glucose Level, and Risk of Sudden Cardiac DeathDino DanielAinda não há avaliações
- Metabolic Dysfunction Associated Steatotic Liver Disease Increa 2023 EClinicDocumento11 páginasMetabolic Dysfunction Associated Steatotic Liver Disease Increa 2023 EClinicronaldquezada038Ainda não há avaliações
- Joc05039 1610 1616 PDFDocumento7 páginasJoc05039 1610 1616 PDFDubster OneXAinda não há avaliações
- A1C and Cardiovascular Outcomes in Type 2 Diabetes: A Nested Case-Control StudyDocumento7 páginasA1C and Cardiovascular Outcomes in Type 2 Diabetes: A Nested Case-Control StudysamuelAinda não há avaliações
- Independent Causal Effect of Remnant Cholesterol On Atherosclerotic Cardiovascular Outcomes - A Mendelian Randomization Study (Navarese, 2023)Documento8 páginasIndependent Causal Effect of Remnant Cholesterol On Atherosclerotic Cardiovascular Outcomes - A Mendelian Randomization Study (Navarese, 2023)MNAinda não há avaliações
- Medical Comorbidity in Alzheimer's 2 Disease: A Nested Case-Control StudyDocumento9 páginasMedical Comorbidity in Alzheimer's 2 Disease: A Nested Case-Control StudyOncología CdsAinda não há avaliações
- 1 s2.0 S000291491730807X MainDocumento11 páginas1 s2.0 S000291491730807X MainEndru AngelAinda não há avaliações
- How I Diagnose and Treat Venous Thromboembolism in Sickle Cell DiseasDocumento9 páginasHow I Diagnose and Treat Venous Thromboembolism in Sickle Cell DiseassamuelAinda não há avaliações
- Dom 13550Documento12 páginasDom 13550mandaAinda não há avaliações
- PIIS2468024919314652Documento4 páginasPIIS2468024919314652adri20121989Ainda não há avaliações
- Diabetic Vascular Diseases: Molecular Mechanisms and Therapeutic StrategiesDocumento29 páginasDiabetic Vascular Diseases: Molecular Mechanisms and Therapeutic StrategiesBBD BBDAinda não há avaliações
- Cardiothoracic Ratio Values and Trajectories Are Associated With Risk of Requiring Dialysis and Mortality in Chronic Kidney DiseaseDocumento8 páginasCardiothoracic Ratio Values and Trajectories Are Associated With Risk of Requiring Dialysis and Mortality in Chronic Kidney Diseaseapi-652909147Ainda não há avaliações
- Retinopatía DiabéticaDocumento7 páginasRetinopatía DiabéticaDIANE EDITH LUNA TOPETEAinda não há avaliações
- How Common Is Pre-Existing Cardiovascular Disease in Cancer Patients (2022)Documento4 páginasHow Common Is Pre-Existing Cardiovascular Disease in Cancer Patients (2022)DanielAinda não há avaliações
- Asssociation of Glycaemia With Macrovascular and Microvascular ComplicationsDocumento8 páginasAsssociation of Glycaemia With Macrovascular and Microvascular ComplicationsMartha CoradoAinda não há avaliações
- Impacts of Anemia On 3-Year Ischemic Events in Patients Undergoing Percutaneous Coronary Intervention: A Propensity-Matched StudyDocumento9 páginasImpacts of Anemia On 3-Year Ischemic Events in Patients Undergoing Percutaneous Coronary Intervention: A Propensity-Matched StudysarahAinda não há avaliações
- Riaz 2018 Oi 180176Documento9 páginasRiaz 2018 Oi 180176César Gonzalvo DíazAinda não há avaliações
- A Comparative Study of Platelet Indices in Acute Coronary SyndromeDocumento4 páginasA Comparative Study of Platelet Indices in Acute Coronary SyndromeMarcellia AngelinaAinda não há avaliações
- Sigaliptin 2Documento8 páginasSigaliptin 2trinda ireneAinda não há avaliações
- Moulson N Et Al. Circulation, 2021Documento11 páginasMoulson N Et Al. Circulation, 2021Anonymous 9aq7eNvOAinda não há avaliações
- Genetics of Dilated CardiomyopathyDocumento12 páginasGenetics of Dilated CardiomyopathyPhạm Quang LongAinda não há avaliações
- 216 FullDocumento7 páginas216 FullEduardo Paglomutan Jr.Ainda não há avaliações
- Hypertensive Disorders of Pregnancy and Longterm Risk of Maternal StrokeDocumento21 páginasHypertensive Disorders of Pregnancy and Longterm Risk of Maternal StrokenskhldAinda não há avaliações
- Human C-Reactive Protein and The Metabolic SyndromeDocumento13 páginasHuman C-Reactive Protein and The Metabolic SyndromeEmir SaricAinda não há avaliações
- Managing Cardiovascular Complications in DiabetesNo EverandManaging Cardiovascular Complications in DiabetesAinda não há avaliações
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesNo EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesAinda não há avaliações
- POWEV2434234Documento461 páginasPOWEV2434234John M. HemsworthAinda não há avaliações
- Unit5 v1.0022101210Documento52 páginasUnit5 v1.0022101210Lily KkAinda não há avaliações
- Financial Management - Risk and Return Assignment 2 - Abdullah Bin Amir - Section ADocumento3 páginasFinancial Management - Risk and Return Assignment 2 - Abdullah Bin Amir - Section AAbdullah AmirAinda não há avaliações
- TTG Basic Rules EngDocumento1 páginaTTG Basic Rules Engdewagoc871Ainda não há avaliações
- Autoregressive-Moving Average (ARMA) ModelsDocumento34 páginasAutoregressive-Moving Average (ARMA) Modelsflaviorochaavila100% (1)
- Michelle Kommer Resignation LetterDocumento1 páginaMichelle Kommer Resignation LetterJeremy TurleyAinda não há avaliações
- Leadership PaperDocumento6 páginasLeadership PaperSTANCIU VALENTINAinda não há avaliações
- The Holy See: Benedict XviDocumento4 páginasThe Holy See: Benedict XviAbel AtwiineAinda não há avaliações
- Aqeedah TahawiyyahDocumento151 páginasAqeedah Tahawiyyahguyii86100% (1)
- Sanjay Seth - Once Was Blind But Now Can See Modernity and The Social SciencesDocumento16 páginasSanjay Seth - Once Was Blind But Now Can See Modernity and The Social SciencesQuelen GuedesAinda não há avaliações
- Grade 3 MathematicsDocumento3 páginasGrade 3 Mathematicsailaine grace alapAinda não há avaliações
- Slides - Simple Linear RegressionDocumento35 páginasSlides - Simple Linear RegressionJarir AhmedAinda não há avaliações
- Sedition ActDocumento11 páginasSedition ActYei TengAinda não há avaliações
- MATH3161 MATH5165 T1 2023 OutlineDocumento10 páginasMATH3161 MATH5165 T1 2023 OutlineDouglusAinda não há avaliações
- Vocabulary ListDocumento2 páginasVocabulary List謝明浩Ainda não há avaliações
- Amnesty - Protest SongsDocumento14 páginasAmnesty - Protest Songsimusician2Ainda não há avaliações
- Longman Communication 3000Documento37 páginasLongman Communication 3000irfanece100% (5)
- Metric Schnorr Lock Washer SpecDocumento3 páginasMetric Schnorr Lock Washer SpecGatito FelinoAinda não há avaliações
- Curriculum Vitae: Lungnila Elizabeth School of Social Work, Senapati, Manipur August 2016-June 2018Documento4 páginasCurriculum Vitae: Lungnila Elizabeth School of Social Work, Senapati, Manipur August 2016-June 2018Deuel khualAinda não há avaliações
- Chapter 15 NegotiationsDocumento16 páginasChapter 15 NegotiationsAdil HayatAinda não há avaliações
- Jurnal Q1 PDFDocumento29 páginasJurnal Q1 PDFSepti DamayantiAinda não há avaliações
- Coursera Qs-Ans For Financial AidDocumento2 páginasCoursera Qs-Ans For Financial AidMarno03Ainda não há avaliações
- 1st Annual Charity Golf Tournament For ChloeDocumento2 páginas1st Annual Charity Golf Tournament For ChloeM.G. PerezAinda não há avaliações
- Ujt and PutDocumento35 páginasUjt and Putisraeljumbo100% (1)
- Spanish Web PDFDocumento36 páginasSpanish Web PDFSergio SayagoAinda não há avaliações
- General Mathematics - Module #3Documento7 páginasGeneral Mathematics - Module #3Archie Artemis NoblezaAinda não há avaliações
- الاستراتيجية الامنية الأمريكيةDocumento141 páginasالاستراتيجية الامنية الأمريكيةAhmedZEMMITAinda não há avaliações
- Teresa of Avila - The Life of ST Teresa, A Carmelite Nun Reprint 1912Documento674 páginasTeresa of Avila - The Life of ST Teresa, A Carmelite Nun Reprint 1912WaterwindAinda não há avaliações
- RBG - CRM BRD - Marketing - v4.1Documento68 páginasRBG - CRM BRD - Marketing - v4.1Manvi Pareek100% (2)
- Introduction PDFDocumento7 páginasIntroduction PDFJalal NhediyodathAinda não há avaliações