Escolar Documentos
Profissional Documentos
Cultura Documentos
Safety of Donors in Live Donor Liver Transplantation Using Right Lobe Grafts 2014
Enviado por
hoangducnamDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Safety of Donors in Live Donor Liver Transplantation Using Right Lobe Grafts 2014
Enviado por
hoangducnamDireitos autorais:
Formatos disponíveis
ORIGINAL ARTICLE
Safety of Donors in Live Donor Liver Transplantation
Using Right Lobe Grafts
Sheung-Tat Fan, MS, MD, FRCS(Glasg and Edin); Chung-Mau Lo, MS, FRACS, FRCS(Edin);
Chi-Leung Liu, MBBS, FRCS(Edin); Boon-Hun Yong, MBBS, MRCP; John Ka-Fat Chan, MBBS, DMRD, FRCR;
Irene Oi-Lin Ng, MD, FRCPath
Hypothesis: Right lobe donation was advocated for adult- Results: The median blood loss was 719 mL (range, 200-
to-adult live donor liver transplantation but the safety of 1600 mL). Only one donor, who had thalassemia, re-
the donor is still a major concern. We hypothesize that ceived 1 U of homologous blood transfusion. Postopera-
right lobe donation is safe if the lowest limit of volume tive complications included wound infection, incision
of liver remnant that can support donor survival is known. hernia, and cholestasis in 1 donor whose liver showed
20% fatty change and who had a left lobe–total liver vol-
Design: Retrospective analysis of data collected pro- ume of 0.34. Another donor with 15% fatty change in the
spectively. liver and a left lobe–total liver volume ratio of 0.27 de-
veloped prolonged cholestasis. Two other donors with
Setting: Tertiary hepatobiliary surgery referral center. left lobe–total liver volume ratios of 0.27 but with mild
steatosis (,5%) did not develop postoperative cholesta-
Patients: Twenty-two live donors involved in adult-to- sis. Postoperative complications also included 1 case of
adult right lobe liver transplantation from May 1996 to biliary stricture and 1 case of small bowel obstruction.
June 1999. Both complications were adequately treated. There was
no donor mortality. All donors are well and have re-
Interventions: The right lobe grafts were obtained by turned to their previous occupations.
transecting the liver on the left side of the middle he-
patic vein. Liver transection was performed by using an Conclusion: Live donation of right lobe graft for adult-
ultrasonic dissector, without using the Pringle maneu- to-adult liver transplantation is safe provided that the re-
ver. The left lobe volume was measured by computed to- sidual liver volume exceeds 30% of the total liver vol-
mographic volumetry and the ratio of left lobe volume ume and the liver itself is normal or only mildly affected
to the total liver volume was calculated. by steatosis.
Main Outcome Measures: Hospital mortality rate
and complication rate. Arch Surg. 2000;135:336-340
L
IVE DONOR liver transplanta- cular clamp applied to the junction of the
tion using extended right middle and left hepatic vein during the har-
lobe graft was advocated to vesting procedure accidentally occluded
treat adult patients who the left hepatic vein and resulted in con-
could not receive a timely ca- gestion of the liver remnant. The mistake
daveric graft.1 Since donation hepatec- was recognized only after division of the
tomy is complicated, lengthy, and in- middle hepatic vein and was rectified af-
volves resection of 60% to 70% of the total ter suturing of the middle hepatic vein ori-
volume of the donor’s liver, the safety of fice. For the other donors, the operations
the donor is the major concern. In this re- were uneventful.
port, we analyzed the data of the donors The duration of the donor operation
of our first 22 live donor liver transplan- was 8.3 to 15.5 hours (median, 11.8
tations using right lobe grafts to deter- hours). The median blood loss of the op-
mine the criteria of selection of donors so eration (including blood loss from the graft
that potential donors who are at risk of during harvesting) was 719 mL (range,
From the Center of Liver liver failure would not be subject to do- 200-1600 mL) (Table). The first and sec-
Diseases, Departments of nor hepatectomy. ond donors received 500 mL of autolo-
Surgery (Drs Fan, Lo, and Liu),
Anesthesiology (Dr Yong),
gous blood. For the other donors, only do-
Diagnostic Radiology RESULTS nor 13, who had thalassemia, received 1
(Dr Chan), and Pathology U of homologous blood. At the time of
(Dr Ng), The University of Intraoperatively, mishap occurred to do- blood transfusion, her hemoglobin level
Hong Kong, Hong Kong. nor 2. At the time of harvesting, the vas- was 69 g/L. Blood collected in the cell saver
ARCH SURG/ VOL 135, MAR 2000 WWW.ARCHSURG.COM
336
©2000 American Medical Association. All rights reserved.
Downloaded From: by a Vinmec International Hospital – Ha Noi City User on 06/16/2018
PATIENTS AND METHODS The liver was transected at a plane on the left of the
middle hepatic vein by using an ultrasonic dissector. The
transection plane was demarcated on the liver surface by
From May 1996 to June 1999, 22 live donor liver trans- temporary occlusion of the right hepatic artery and right
plantations using right lobe grafts were performed at Queen portal vein. Inflow vascular occlusion was not used dur-
Mary Hospital, Hong Kong. The ages of the donors ranged ing liver transection. When the transection of liver ap-
from 18 to 51 years (median, 35.5 years). They were fathers proached the liver hilum, the right hepatic duct together
(n = 2), spouses (n = 8), daughters (n = 3), son (n = 1), broth- with the surrounding Glissonian sheath was encircled.
ers (n = 3), sister (n = 1), aunt (n = 1), uncle (n = 1), nephew After identification of the confluence of the right and left
(n = 1), and brother-in-law (n = 1) of the recipients. All do- hepatic ducts, the right hepatic duct was divided near to
nors received psychological counseling before the donor the confluence of the hepatic ducts by scissors. The di-
operations. They were screened by laboratory tests includ- vided end at the confluence of the hepatic duct was closed
ing complete blood cell count, liver and renal biochemis- transversely together with the surrounding Glissonian sheath
try values, and viral serologic studies. The blood types of by continuous 5-0 polydioxanone monofilament absorb-
all donors were matched or compatible with the recipi- able suture. The liver transection was carried on down to
ents. Autologous blood collection was made in the first 2 the junction of the middle hepatic vein with the left he-
donors but not in the subsequent donors. Computed to- patic vein or inferior vena cava.
mography (CT), CT volumetry, and hepatic arteriogra- At the time of harvesting, the right portal vein was
phy were routinely performed. The hepatic vein anatomy clamped and cannulated by a catheter connected to cold
was carefully studied on the CT scan, particularly in the plasma solution. The right hepatic artery, right hepatic
region of middle hepatic vein (Figure 1). vein(s), and middle hepatic veins were clamped at the junc-
The donors were prepared on the operating table with tion with the main trunks and divided. Blood that escaped
care to avoid sores at the pressure points. Heparin was given from the graft was recovered and collected in a red cell saver.
subcutaneously in 2 female donors who had a history of The stumps of the right hepatic artery, right portal vein,
taking oral contraceptive pills. In 3 donors (2 with slightly and hepatic veins were closed by continuous nonabsorb-
abnormal liver biochemistry results [alanine aminotrans- able surgical sutures. Methylene blue was injected into the
ferase level greater than the upper limit of normal] and 1 common bile duct via the cystic duct cannula to detect bile
with a CT scan finding of splenomegaly), laparoscopy and leakage from the right hepatic duct stump and transection
liver biopsy were performed before laparotomy. surface. The falciform ligament was sutured to the ante-
The laparotomy was performed via bilateral subcos- rior abdominal wall to prevent rotation of the left lobe into
tal incision with an upward midline extension. Intraop- the right subphrenic cavity. A drain (Reliavac; Davol, CR
erative ultrasonography was performed to identify the pres- Bard Inc, Covington, Mexico) was inserted into the right
ence of a large right inferior hepatic vein (accessory right subphrenic cavity before wound closure.
hepatic vein) and to study the junction of the middle he- The donors were cared for in the intensive care unit
patic vein with the inferior vena cava. Operative cholan- with attention to adequate tissue oxygenation and perfu-
giography via cystic duct cannulation was performed to sion. Parenteral nutrition consisting of a mixture of
study the bile duct anatomy. Hilar dissection was then per- branched-chain amino acid–enriched solution, dextrose,
formed to isolate the right hepatic artery and right portal and medium- and long-chain triglycerides was adminis-
vein. All portal vein branches to the caudate process were tered in all except the first 2 donors immediately after the
divided and ligated. The right lobe of the liver was then hepatectomy to stimulate liver regeneration. Once paren-
rotated toward the left side for division of right triangular teral nutrition was started, no other intravenous fluid was
ligament and tiny venous branches between the anterior given, and the central venous pressure was maintained as
surface of the inferior vena cava and posterior surface of low as possible to avoid congestion of the liver remnant.
paracaval portion of the caudate lobe. The rotation was in- Oral nutrition was encouraged once bowel activity re-
termittent to avoid prolonged twisting of the inflow and turned and the parenteral nutrition was stopped. Chest phys-
outflow vascular pedicles of the left lobe. The right he- iotherapy and incentive spirometry were routinely given.
patic vein and the right inferior hepatic vein larger than 5 All data were recorded prospectively by a single research
mm were preserved until the time of harvesting. assistant.
was returned to donors 2 and 6 only. The volume of blood end of the first week. The peak serum bilirubin level of do-
returned was 300 mL and 750 mL, respectively. None of nor 2 was 203 µmol/L on postoperative day 3. The peak se-
the donors received platelet and fresh frozen plasma in- rum bilirubin level of donor 8 was 318 µmol/L on postop-
fusion intraoperatively, but donors 3 and 5 received 1040 erative day 23. The postoperative international normalized
mL and 540 mL exogenous fresh frozen plasma, respec- ratio and the platelet count data are shown in Figure 3.
tively, in the postoperative period. The median dura- The international normalized ratio of the donors returned
tion of postoperative hospital stay was 11.5 days (range, rapidly to the normal level at the end of the first week.
6-38 days). Five donors volunteered to stay longer than Mild fatty change of liver (,5%) was found on liver
2 weeks to take care of the recipients and their duration histological evaluation in 12 donors (55%) (Table).
of hospital stay was included in the calculation. Moderate fatty change was seen in donor 2 (20%) and
Data on the postoperative serum bilirubin, alanine ami- donor 8 (15%). These 2 donors developed postopera-
notransferase, and aspartate aminotransferase levels are tive cholestasis.
shown in Figure 2. The serum bilirubin level of all donors, The ratio of the left lobe volume to the total vol-
except donors 2 and 8, returned to the normal level at the ume of the liver of the donor was calculated on CT volu-
ARCH SURG/ VOL 135, MAR 2000 WWW.ARCHSURG.COM
337
©2000 American Medical Association. All rights reserved.
Downloaded From: by a Vinmec International Hospital – Ha Noi City User on 06/16/2018
metry.2 The remnant left lobes were 27% to 43% of the rotomy. She was well after biliary enteric anastomosis
total liver volume (median, 33%). Donors 8, 16, and 17 constructed at segment III duct. On review of the pre-
had left lobe volume of 27% of the total volume. Only operative hepatic arteriogram, excessive dissection of the
donor 8, whose liver showed 15% steatosis, developed right hepatic artery to the left might have been respon-
postoperative cholestasis (Table). sible for ischemia of the common hepatic duct. Donor 8
There was no donor mortality. Donor 2 developed developed cholestasis for 4 weeks. He was otherwise well
wound infection due to methicillin-resistant Staphylo- and eventually free from jaundice. Donor 17 had tran-
coccus aureus and cholestasis. He subsequently devel- sient left peroneal nerve palsy. Donor 18 returned to the
oped an incision hernia that required repair. Donor 3 de- hospital 34 days after discharge because of a small bowel
veloped obstructive jaundice 2 months after discharge obstruction. Laparotomy showed a single adhesion band
from the hospital. Endoscopic retrograde cholangiopan- beneath the right subcostal wound. All donors are well
creatography showed that she had stricture at the con- and have returned to their previous occupations.
fluence. Fibrosis was found at the liver hilum at lapa-
COMMENT
Live donor liver transplantation is performed on the
premise that the remnant liver in the donor will regen-
erate quickly and the donor will not be harmed by
the operation. To ensure that the remnant liver will re-
3
4 generate quickly after the operation, intraoperative trauma
to the liver remnant must be minimal. Thus, we ex-
ercised careful and intermittent rotation of the right
8 2 lobe during mobilization,3 exerted no Pringle maneuver
during liver transection, reconstructed the falciform
ligament to prevent left lobe rotation into the right
subphrenic cavity,4 and initiated immediate postopera-
tive parenteral nutritional support to stimulate liver
Figure 1. Computed tomographic scan showing the hepatic vein anatomy in regeneration.5,6
the region of the middle hepatic vein. The segment IV hepatic vein (4) joined
the segment III hepatic vein (3) and was vulnerable to injury when
In live donor liver transplantation using the right
transection was performed on the left side of the middle hepatic vein. The lobe, the volume of the remnant liver is a major con-
segment VIII hepatic vein (8) joined the middle hepatic vein near the inferior cern. There were, however, insufficient data in the lit-
vena cava. Two orifices would be expected at the transection plane of the erature to guide the surgeons in choosing the appropri-
middle hepatic vein. The segment II hepatic vein (2) is separated from the
segment III hepatic vein (3). The dotted line indicates the boundary of the ate candidates for right lobe donation. In animal
right lobe. experiments, it was demonstrated that 10% of viable liver
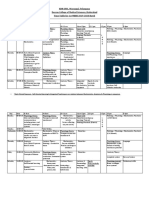
Donor Data and Postoperative Complications
Donor Blood Fresh Frozen Total Parenteral Left Lobe Left Lobe–Total Fatty
No. Loss, mL Plasma, mL Nutrition, d Volume, mL Volume Ratio Change, % Complication(s)
1 1300 0 0 423 0.36 ,5 None
2 738 0 0 586 0.34 20 Cholestasis, MRSA*
wound infection, incision hernia
3 900 1040 4 291 0.32 0 Biliary stricture
4 1000 0 3 231 0.34 ,5 None
5 800 540 3 472 0.33 0 None
6 1600 0 5 394 0.40 0 None
7 700 0 3 406 0.34 0 None
8 500 0 3 368 0.27 15 Cholestasis
9 1200 0 3 391 0.32 ,5 None
10 1000 0 4 365 0.31 ,5 None
11 600 0 2 350 0.34 ,5 None
12 400 0 2 446 0.43 0 None
13 1200 0 4 306 0.35 0 None
14 300 0 4 466 0.32 ,5 None
15 400 0 2 405 0.38 0 None
16 800 0 3 292 0.27 ,5 None
17 200 0 5 224 0.27 ,5 Transient left peroneal nerve palsy
18 500 0 3 407 0.41 ,5 Small bowel obstruction
19 800 0 4 217 0.29 ,5 None
20 500 0 3 322 0.31 0 None
21 300 0 3 221 0.32 1 None
22 200 0 2 436 0.39 1 None
*MRSA indicates methicillin-resistant Staphylococcus aureus.
ARCH SURG/ VOL 135, MAR 2000 WWW.ARCHSURG.COM
338
©2000 American Medical Association. All rights reserved.
Downloaded From: by a Vinmec International Hospital – Ha Noi City User on 06/16/2018
Total Bilirubin AST ALT Platelet INR
50 230 220 1.8
190 200
Total Bilirubin, µmol/L
Platelet Count, ×109/L
40 1.6
AST and ALT, U/L
150 180
INR
30 1.4
110 160
20 1.2
70 140
10 30 120 1.0
0 1 2 3 4 5 6 7 0 1 2 3 4 5 6 7
Postoperative Day Postoperative Day
Figure 2. Median values of serum total bilirubin, aspartate aminotransferase Figure 3. Median values of platelet count and international normalized ratio
(AST), and alanine aminotransferase (ALT) levels of the donors during the (INR) of the donors during the first postoperative week.
first postoperative week.
mass was adequate for spontaneous recovery after ma- The speed of recovery of the donor depends on ad-
jor hepatectomy.7 In human situations, many patients sur- equate regeneration of the liver remnant. After hepatec-
vived major hepatectomy of large tumors because the con- tomy, liver regeneration in humans is not immediate.
tralateral lobe of liver had undergone hypertrophy before There may be 3 to 5 days between the resection and the
the operation or only a small portion of nontumorous initial regenerative events.16 Before adequate regenera-
liver was removed together with the large tumor. Before tion occurs and before oral nutrition can stimulate in-
the era of CT volumetry, Stone et al8 estimated that re- creased portal blood flow necessary for liver regenera-
moval of 70% of the total volume of the liver was well tion,17,18 we give the donors parenteral nutrition, because
tolerated in patients with normal liver. Recently, Kubota in addition to providing nutrients and stimuli for liver
et al,9 using CT volumetry, showed that individuals with regeneration, the parenteral nutritional mixture can also
normal liver function could tolerate resection of up to serve as an efficient metabolic vehicle for resolving acute
60% of the nontumorous liver. The present data, albeit electrolyte and acid-based disturbances19 and has been
limited, indicated that residual liver volume that is 27% shown to prevent deterioration of liver function.20
of the total volume is the lowest limit that can support The most important risk to the donor during hepa-
survival, provided that the liver itself is not fatty. To al- tectomy is bleeding, which can be serious at the deeper
low a safety margin, residual liver volume of 30% of the plane of transection near to the middle hepatic vein. Se-
total volume is probably the lowest limit. In this regard, vere bleeding is associated with a decrease in hepatic blood
CT volumetry is necessary for preoperative documenta- flow and ischemic injury.21 The bleeding volume can be
tion because the volume of the left lateral segment could reduced if the central venous pressure is low22 and the
be quite variable. patient is placed in a slightly Trendelenburg position.23
The incidence of fatty liver was surprisingly high Bleeding during transection of liver parenchyma can be
among live donors in our locality. Liver grafts with mild reduced by using the Pringle maneuver24 or hemihe-
degree of fatty change can be used for liver transplanta- patic vascular occlusion25 but it is uncertain whether in-
tion without ill effect but liver grafts with moderate or flow vascular occlusion can be safely utilized in donor
severe degree of fatty change will lead to primary graft hepatectomy. Theoretically, inflow vascular occlusion can
dysfunction in the recipients.10 The acceptable upper limit damage hepatocytes but it was also shown that hepatic
of fatty change in a liver graft was 30%.11 In partial hep- venous back-perfusion could maintain viability of hepa-
atectomy, a trend toward increased mortality was also re- tocytes during the Pringle maneuver.26 Before more data
ported for patients with moderate to severe steatosis are available, we would continue the present practice of
(.30% of hepatocytes containing fat).12 Although fatty transecting the liver without the Pringle maneuver.
liver may not have serious liver function impairment, fatty Another risk to the donor is injury to the bile duct
livers are probably more vulnerable to injury by general resulting in biliary stricture or leakage. Ischemia due to
anesthesia13 and ischemia-reperfusion.14,15 Although we excessive right hepatic artery dissection is probably re-
did not use the Pringle maneuver during liver transec- sponsible for such complication in one of our donors.
tion, the left lobe of the liver may sustain ischemic in- To avoid such a complication, we consider that the dis-
jury during right lobe mobilization because of twisting section of the right hepatic artery should be confined to
of the inflow and outflow vascular pedicles. In donor 2, the right side of the common hepatic duct. It is also im-
whose liver showed 20% steatosis, the period of liver con- portant not to isolate the right hepatic artery too far into
gestion induced by accidental left hepatic vein clamp- the right side of the liver hilum to avoid devasculariza-
ing might aggravate the injury. Therefore, based on the tion of the right hepatic duct. The length of the right he-
data of the present series and those reported in the lit- patic artery available for the right lobe graft might be short
erature on similar subjects, we consider that liver with but usually was sufficiently long for subsequent micro-
steatosis of 20% or more, especially when the liver rem- vascular anastomosis.
nant was less than 30% of the total volume, should not To protect the donor from contracting viral infec-
be selected for right lobe donor hepatectomy. tion, avoidance of exogenous blood or blood product
ARCH SURG/ VOL 135, MAR 2000 WWW.ARCHSURG.COM
339
©2000 American Medical Association. All rights reserved.
Downloaded From: by a Vinmec International Hospital – Ha Noi City User on 06/16/2018
transfusion is the goal. In the present series, one donor patic functional reserve as a guide to decision-making in resectional surgery for
hepatic tumors. Hepatology. 1997;26:1176-1181.
received homologous blood transfusion intraopera-
10. D’Alessandro AM, Kalayoglu M, Sollinger HW, et al. The predictive value of do-
tively and 2 donors received fresh frozen plasma post- nor liver biopsies for the development of primary non-function after orthotopic
operatively. The transfusion arose out of lack of com- liver transplantation. Transplantation. 1991;51:157-163.
munication. With expansion of activities of the liver 11. Marsman WA, Wiesner RH, Rodriguez L, et al. Use of fatty donor liver is asso-
transplant program in our hospital and awareness of po- ciated with diminished early patient and graft survival. Transplantation. 1996;
62:1246-1251.
tential harmful effect of exogenous blood transfusion by 12. Behrns KE, Tsiotos GG, DeSouza NF, Krishna MK, Ludwig J, Nagorney DM. He-
all members of the team, the risk of exogenous blood and patic steatosis as a potential risk factor for major hepatic resection. J Gastro-
blood product transfusion were completely eliminated intest Surg. 1998;2:292-298.
in the later part of this series. 13. Friedman LS, Maddrey WC. Surgery in the patient with liver disease. Med Clin
North Am. 1987;71:453-476.
In conclusion, the live donation of right lobe graft
14. Hui AM, Kawasaki S, Makuuchi M, Nakayama J, Ikegami T, Miyagawa J. Liver
for adult-to-adult liver transplantation is safe provided injury following normothermic ischemia in steatotic rat liver. Hepatology. 1994;
that the residual liver volume of the donor exceeds 30% 20:1287-1293.
of the total liver volume, the liver itself is not fatty, and 15. Hakamada K, Sasaki M, Takahashi K, Umehara Y, Konn M. Sinusoidal flow block
there is no injury to the liver remnant. after warm ischemia in rats with diet-induced fatty liver. J Surg Res. 1997;70:
12-20.
16. Francavilla A, Panella C, Polimeno L, et al. Hormonal and enzymatic parameters
This study was supported by the Hong Kong Oriental Press of hepatic regeneration in patients undergoing major liver resections. Hepatol-
Charitable Fund Association. ogy. 1990;12:1134-1138.
Corresponding author: Sheung-Tat Fan, MS, MD, 17. Fischer JE. Cirrhosis and jaundice. In: Wilmore DW, Brennan MF, Harken AH,
FRCS, Department of Surgery, The University of Hong Kong, Holcroft JW, Meakins JL, eds. Scientific American Surgery. Vol 2. New York, NY:
Scientific American; 1998.
Queen Mary Hospital, 102 Pokfulam Rd, Hong Kong 18. Kameoka N, Nimura Y, Sato T, et al. Postprandial responses of liver blood flow
(e-mail: hrmsfst@hkucc.hku.hk). prior to and following hepatectomy in conscious dogs. J Surg Res. 1996;61:
437-443.
19. Driscoll DF, Palombo JD, Bistrian BR. Nutritional and metabolic considerations of
REFERENCES the adult liver transplant candidate and organ donor. Nutrition. 1995;11:255-263.
20. Fan ST, Lo CM, Lai ECS, Chu KM, Liu CL, Wong J. Perioperative nutritional sup-
1. Lo CM, Fan ST, Liu CL, et al. Adult-to-adult living donor liver transplantation us- port in patients undergoing hepatectomy for hepatocellular carcinoma. N Engl J
ing extended right lobe graft. Ann Surg. 1997;226:261-270. Med. 1994;331:1547-1552.
2. Higashiyama H, Yamaguchi T, Mori K, et al. Graft size assessment by preopera- 21. Rosenberg PM, Friedman LS. The liver in circulatory failure. In: Schiff ER, Sor-
tive computed tomography in living related partial liver transplantation. Br J Surg. rell MF, Maddrey WC, eds. Schiff’s Diseases of the Liver. 8th ed. Philadelphia,
1993;80:489-492. Pa: Lippincott-Raven; 1999:1215-1227.
3. Fan ST. Technique of hepatectomy. Br J Surg. 1996;83:1490-1491. 22. Johnson M, Mannar R, Wu AVO. Correlation between blood loss and inferior vena
4. Poon RTP, Chan J, Fan ST. Left hepatic vein kinking after right trisegmentec- caval pressure during liver resection. Br J Surg. 1998;85:188-190.
tomy—a potential cause of postoperative liver failure. Hepatogastroenterology. 23. Blumgart LH. Liver resection—liver and biliary tumours. In: Blumgart LH, ed.
1998;45:508-509. Surgery of the Liver and Biliary Tract. Edinburgh, Scotland: Churchill Living-
5. Chiba T, Kawai K, Ikenaka K, et al. Effect of an exogenous energy source and stone; 1994:1495-1537.
amino acids on DNA synthesis in regenerating rat liver. Biochim Biophys Acta. 24. Man K, Fan ST, Ng IOL, Lo CM, Liu CL, Wong J. Prospective evaluation of Prin-
1983;755:420-427. gle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg.
6. McGowan J, Atryzek V, Fausto N. Effects of protein-deprivation on the regen- 1997;226:704-713.
eration of rat liver after partial hepatectomy. Biochem J. 1979;180:25-35. 25. Makuuchi M, Mori T, Gunven P, Yamazaki S, Hasegawa H. Safety of hemihe-
7. Ganb J, Inversen J. Rat liver regeneration after 90% partial hepatectomy. Hepa- patic vascular occlusion during resection of the liver. Surg Gynecol Obstet. 1987;
tology. 1984;4:902-904. 164:155-158.
8. Stone HH, Long WD, Smith RB III, Haynes CD. Physiological consideration in 26. Kim YI, Ishii T, Aramaki M, Nakashima K, Yoshida T, Kobayashi M. The Pringle
major hepatic resection. Am J Surg. 1969;117:78-84. maneuver induces only partial ischemia of the liver. Hepatogastroenterology. 1995;
9. Kubota K, Makuuchi M, Kusaka K, et al. Measurement of liver volume and he- 42:169-171.
ARCH SURG/ VOL 135, MAR 2000 WWW.ARCHSURG.COM
340
©2000 American Medical Association. All rights reserved.
Downloaded From: by a Vinmec International Hospital – Ha Noi City User on 06/16/2018
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Lover CompleteDocumento18 páginasThe Lover Completehoangducnam100% (1)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Hosa Practice Questions 1Documento12 páginasHosa Practice Questions 1rohitmital0% (1)
- IELTS Listening - Reading Answer SheetsDocumento2 páginasIELTS Listening - Reading Answer Sheetsntnam11383% (12)
- Lower Extremity Venous Protocol 14Documento3 páginasLower Extremity Venous Protocol 14api-276847924Ainda não há avaliações
- Updated Bastyr Materia MedicaDocumento491 páginasUpdated Bastyr Materia MedicaAmanda Luu100% (1)
- Anatomy of The Lymphatic SystemDocumento27 páginasAnatomy of The Lymphatic SystemAntonio Lima Filho100% (2)
- Best VideoDocumento16 páginasBest VideohoangducnamAinda não há avaliações
- Fong1997 - Useful Stapling Techniques in Liver SurgeryDocumento8 páginasFong1997 - Useful Stapling Techniques in Liver SurgeryhoangducnamAinda não há avaliações
- Alvarez2016 - Parenchymal-Sparing Liver Surgery in Patients With Colorectal Carcinoma Liver Metastases PDFDocumento18 páginasAlvarez2016 - Parenchymal-Sparing Liver Surgery in Patients With Colorectal Carcinoma Liver Metastases PDFhoangducnamAinda não há avaliações
- Chouillard2010 - Vascular Clamping in Liver Surgery - Physiology, Indications and TechniquesDocumento12 páginasChouillard2010 - Vascular Clamping in Liver Surgery - Physiology, Indications and TechniqueshoangducnamAinda não há avaliações
- Helling2014 - Ton That Tung's LiversDocumento8 páginasHelling2014 - Ton That Tung's Livershoangducnam100% (1)
- Anatomical Laparoscopic Right Posterior SectionectomyDocumento7 páginasAnatomical Laparoscopic Right Posterior SectionectomyhoangducnamAinda não há avaliações
- Hepatic Manifestations in Hematological Disorders 2013Documento14 páginasHepatic Manifestations in Hematological Disorders 2013hoangducnamAinda não há avaliações
- Split RevisionDocumento13 páginasSplit RevisionhoangducnamAinda não há avaliações
- The Associating Liver Partition and Portal Vein Ligation For Staged Hepatectomy Approach Using Only Segments I and IV As Future Liver RemnantDocumento5 páginasThe Associating Liver Partition and Portal Vein Ligation For Staged Hepatectomy Approach Using Only Segments I and IV As Future Liver RemnanthoangducnamAinda não há avaliações
- Cholangiocarcinoma diagnosis and treatment advancesDocumento12 páginasCholangiocarcinoma diagnosis and treatment advanceslimbert manuelAinda não há avaliações
- IntJAppBasicMedRes64237-2646592 072105Documento4 páginasIntJAppBasicMedRes64237-2646592 072105hoangducnamAinda não há avaliações
- Factor Analysis in SPSSDocumento9 páginasFactor Analysis in SPSSLoredana IcsulescuAinda não há avaliações
- IELTS Reading Answer SheetDocumento1 páginaIELTS Reading Answer Sheetskuppal50% (2)
- Classification, Diagnosis, and Management of Cholangiocarcinoma - Razumilava2013Documento10 páginasClassification, Diagnosis, and Management of Cholangiocarcinoma - Razumilava2013hoangducnamAinda não há avaliações
- SAS BigData FinalDocumento37 páginasSAS BigData FinalDevika RadjkoemarAinda não há avaliações
- Combined Liver-Kidney Transplantation in Patients With Cirrhosis and Chronic Kidney DiseaseDocumento8 páginasCombined Liver-Kidney Transplantation in Patients With Cirrhosis and Chronic Kidney DiseasehoangducnamAinda não há avaliações
- Academic Test 1 Question PaperDocumento21 páginasAcademic Test 1 Question PaperPeach Peach Lynn0% (2)
- Dumortier2016 - EVEROLIMUSDocumento10 páginasDumortier2016 - EVEROLIMUShoangducnamAinda não há avaliações
- Blood Vessels Lecture Slides PDFDocumento32 páginasBlood Vessels Lecture Slides PDFRaluca AlexandraAinda não há avaliações
- Chapter 15: Cardiovascular System: Shier, Butler, and Lewis: Hole's Human Anatomy and Physiology, 13Documento26 páginasChapter 15: Cardiovascular System: Shier, Butler, and Lewis: Hole's Human Anatomy and Physiology, 13Elvin MoletaAinda não há avaliações
- Transportation Systems in Animals and PlantsDocumento6 páginasTransportation Systems in Animals and PlantsMidhun Bhuvanesh.B 7AAinda não há avaliações
- 2 - Vascular InjuryDocumento6 páginas2 - Vascular Injuryمحمد عماد عليAinda não há avaliações
- A Study To Evaluate Effectiveness of Cold Application and Magnesium Sulphate Application On Superficial Thrombophlebitis Among Patients Receiving Intravenous Therapy in Selected Hospitals Amritsar.Documento25 páginasA Study To Evaluate Effectiveness of Cold Application and Magnesium Sulphate Application On Superficial Thrombophlebitis Among Patients Receiving Intravenous Therapy in Selected Hospitals Amritsar.Navjot Brar71% (14)
- DMC College Foundation Inc. College of Nursing A Case Study OnDocumento41 páginasDMC College Foundation Inc. College of Nursing A Case Study OnTiffany AdriasAinda não há avaliações
- Urbn159 Paper 9Documento5 páginasUrbn159 Paper 9Mutiara Khairunnisa SuhardiAinda não há avaliações
- Biology and Chemistry ReviewDocumento11 páginasBiology and Chemistry ReviewAngel Louise VillondoAinda não há avaliações
- Pediatric Echocardiogram GuidelinesDocumento18 páginasPediatric Echocardiogram GuidelinesNorhafizah AhmadAinda não há avaliações
- Live Donor Liver Transplantation: Caq CornerDocumento12 páginasLive Donor Liver Transplantation: Caq CornerBarbara ZabraAinda não há avaliações
- Body Fluids and CirculationsDocumento14 páginasBody Fluids and CirculationsNikhil SharmaAinda não há avaliações
- Sustainable Design of Mobile Transilluminator Vein Finder DeviceDocumento12 páginasSustainable Design of Mobile Transilluminator Vein Finder DeviceTohid TalefifuAinda não há avaliações
- Respiratory and Circulatory SystemDocumento243 páginasRespiratory and Circulatory Systemfiroz77Ainda não há avaliações
- Paper 1 MCQDocumento8 páginasPaper 1 MCQmarwaAinda não há avaliações
- 2 Circulation SystemDocumento29 páginas2 Circulation SystemPERTUNIA KORABIAinda não há avaliações
- Intra-Abdominal Hypertension GuideDocumento40 páginasIntra-Abdominal Hypertension GuideBayu Surya Dana100% (1)
- Transesophageal Echocardiography: M. Elizabeth Brickner, MDDocumento9 páginasTransesophageal Echocardiography: M. Elizabeth Brickner, MDHilario. Hayascent.Reign.M.Ainda não há avaliações
- BioMedical Book Full Text NewDocumento329 páginasBioMedical Book Full Text NewSu Rya ReddyAinda não há avaliações
- Physical Diagnosis Case SampleDocumento3 páginasPhysical Diagnosis Case SampleHerlene Lyneth Zalameda100% (2)
- Basic IV TherapyDocumento23 páginasBasic IV TherapyBea Flor Rapisura-PegadAinda não há avaliações
- (NS) Week 11 SBL Fractures QuestionsDocumento16 páginas(NS) Week 11 SBL Fractures QuestionsJoei “Jojo” GohAinda não há avaliações
- NMC Exam Review for Medical Nursing 01Documento61 páginasNMC Exam Review for Medical Nursing 01Kumah WisdomAinda não há avaliações
- Human Circulatory SystemDocumento3 páginasHuman Circulatory SystemMir Rehan Mushtaq100% (1)
- PATIENT POSITIONING AND ANAESTHESIA SAFETYDocumento24 páginasPATIENT POSITIONING AND ANAESTHESIA SAFETYGrishma KothariAinda não há avaliações
- Histology of The Circulatory SystemDocumento24 páginasHistology of The Circulatory SystemFatima Zehra YusefAinda não há avaliações
- KNRUHS 1st MBBS Time Table 2019-2020 DCMS - CumulativeDocumento42 páginasKNRUHS 1st MBBS Time Table 2019-2020 DCMS - CumulativeAnime FanAinda não há avaliações