Escolar Documentos
Profissional Documentos
Cultura Documentos
The Diagnosis of Appendicitis in Children: Outcomes of A Strategy Based On Pediatric Surgical Evaluation
Enviado por
AndikaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Diagnosis of Appendicitis in Children: Outcomes of A Strategy Based On Pediatric Surgical Evaluation
Enviado por
AndikaDireitos autorais:
Formatos disponíveis
The Diagnosis of Appendicitis in Children: Outcomes of a Strategy Based
on Pediatric Surgical Evaluation
Ann M. Kosloske, MD, MPH*‡储; C. Lance Love, MD*; James E. Rohrer, PhD§; Jane F. Goldthorn, MD*‡储;
and Stuart R. Lacey, MD*‡储
ABSTRACT. Objective. To determine the accuracy of dectomy (5%) and perforation (17%) were achieved with-
a protocol for diagnosis of appendicitis in children based out the potential costs and radiation exposure of excess
on clinical evaluation by a pediatric surgeon with selec- imaging. Pediatrics 2004;113:29 –34; appendicitis, appen-
tive use of diagnostic imaging studies. We performed dectomy, pediatric surgeon, CT, computed tomography.
this study because 1) current reports in the medical, pe-
diatric, emergency medical, and surgical literature advo-
cate imaging, particularly computed tomography (CT), as ABBREVIATIONS. CT, computed tomography; US, ultrasound;
WBC, white blood cell.
the gold standard for diagnosis of appendicitis, and 2)
the value of pediatric surgical evaluation early in the
management of the child with possible appendicitis has
A
cute appendicitis is the most common surgi-
rarely been emphasized. cal emergency in children and adolescents in
Methods, Design, Setting, and Participants. Retro-
spective review of 356 children (mean age: 9.6 years;
the United States. In 1999, an estimated
range: 1–18 years) referred to a regional pediatric surgical 59 000 children ⬍15 years old were diagnosed with
center for possible appendicitis from 1999 through 2001. appendicitis.1 Despite its frequency, however, the
Interventions. Initial pediatric surgical evaluation diagnosis of appendicitis in a child is sometimes
consisted of history, physical examination, white blood difficult. Recent reports recommended imaging, par-
cell count, differential count, and urinalysis. Children ticularly computed tomography (CT) with rectal con-
diagnosed with appendicitis underwent appendectomy trast, as the optimal diagnostic study in both adults2
without additional studies; those with equivocal find- and children.3,4 One protocol used imaging (usually
ings received intravenous fluids, rest, and reevaluation both ultrasound [US] and CT scan with rectal con-
after 4 to 6 hours. Imaging was used selectively by the trast) in 78.5% of children with possible appendici-
pediatric surgeon.
Outcome Measures. Sensitivity, specificity, positive
tis.3,5 CT scanning was calculated as cost-effective in
predictive value, negative predictive value, and accuracy children based on a negative appendectomy rate of
of the protocol based on final diagnoses; rate of appen- 23%.6 Because in our west Texas pediatric surgical
diceal perforation; and rate of negative appendectomy. practice we rely on a clinically based strategy with
Results. Of 356 children evaluated for appendicitis, selective use of imaging, and because we considered
220 (62%) had an appendectomy. Two-hundred nine a 23% rate of negative appendectomy to be unaccept-
(95%) had histologically proven appendicitis, and 11 (5%) ably high, we undertook the present study. We re-
had a normal appendix. Of the 209 children with appen- viewed the outcomes of 356 children and adolescents
dicitis, 139 (66%) had acute appendicitis, 34 (16%) had referred to us for possible appendicitis over a 3-year
advanced appendicitis without perforation, and 36 (17%) period and calculated the accuracy of our diagnostic
had advanced appendicitis with perforation. Appendec-
tomy was performed after initial evaluation in 195 (89%)
strategy compared with the accuracy of imaging.
of the 220 children and after a period of supportive care
and observation in 25 (11%) of 220. One hundred thirty- METHODS
six children (38%) did not have an appendectomy and The pediatric surgeon authors (A.M.K., J.F.G., and S.R.L.) prac-
were discharged with other diagnoses. The sensitivity of tice in a west Texas city of 204 000 population, with a referral area
this protocol was 99%, specificity was 92%, positive pre- consisting of 62 primarily rural counties in west Texas and eastern
New Mexico. The total population served is 1.4 million. No other
dictive value was 95%, and negative predictive value was pediatric surgeon practiced in this area during the study period.
99%. The accuracy was 97% compared with an accuracy of Children and adolescents with possible appendicitis were referred
82% for ultrasound alone and 90% for CT scan alone. to the pediatric surgeon by a pediatrician, a family practitioner, or
Conclusions. These data show that a protocol based an emergency department physician. Patients were treated at 2
on clinical evaluation by a pediatric surgeon with selec- hospitals: Texas Tech University Hospital, a 325-bed teaching
tive use of imaging was highly accurate for the diagnosis hospital with an 88-bed pediatric hospital located on one floor,
of appendicitis in children. Low rates of negative appen- and Covenant Children’s Hospital, a 73-bed pediatric hospital that
is a separate wing of a 400-bed community hospital. The study
was approved by the institutional review boards of both hospitals.
From the Departments of *Surgery, ‡Pediatrics, and §Health Services Re- Residents in general surgery (Post-Graduate Year 4 or Post-Grad-
search, Texas Tech University, Health Sciences Center, Lubbock, Texas; and uate Year 2) assisted the 3 pediatric surgeons in the diagnosis and
储Covenant Children’s Hospital, Lubbock, Texas. treatment of all patients. The “diagnostic call,” however, was
Received for publication Mar 3, 2003; accepted Apr 10, 2003. made by the attending pediatric surgeon. Radiographic studies
Reprint requests to (A.M.K.) 1273 Par View Drive, Sanibel, FL 33957. E-mail: were performed by general radiologists at each hospital; there
akosloske@hotmail.com were no specialty-trained pediatric radiologists at either institu-
PEDIATRICS (ISSN 0031 4005). Copyright © 2004 by the American Acad- tion.
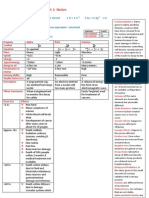
emy of Pediatrics. The strategy for diagnosis of appendicitis (Fig 1), agreed on by
PEDIATRICS Vol. 113 No. 1 January 2004
Downloaded from www.aappublications.org/news by guest on July 23, 2018
29
the 3 pediatric surgeons (who were associated for ⬎20 years), was not referred and thus were excluded from this patient population.)
as follows: initial pediatric surgical evaluation consisted of his- Incidental appendectomies performed as part of another proce-
tory, physical examination, white blood cell (WBC) count, differ- dure were excluded. A standardized data collection tool was used
ential count, and urinalysis. This was usually done in the emer- that included age, gender, duration of symptoms, county of resi-
gency department or occasionally on the ward or in the office. dence, imaging (US or CT scan), physician ordering imaging stud-
When the diagnosis of appendicitis (without perforation) was ies, results of imaging studies (positive, negative, or equivocal),
made, the child was prepared for operation. No additional labo- interval (hours) from arrival to pediatric surgical consultation,
ratory or radiographic tests were done. Children with perforated interval (hours) from arrival to appendectomy, operative diagno-
appendicitis received more intensive preparation with intrave- sis, and pathologic diagnosis. Pathologic criteria for acute appen-
nous hydration and antibiotics before operation. If a nonsurgical dicitis were mucosal and intramural inflammation. The presence
condition was suspected, eg, streptococcal pharyngitis or pneu- of advanced appendicitis, eg, right lower quadrant peritonitis
monia, appropriate diagnostic studies were done, and manage- with or without gross appendiceal perforation was based on the
ment was continued by the pediatrician or family practitioner. If surgeon’s operative note. The presence of perforation was based
the diagnosis remained uncertain, eg, gastroenteritis or early ap- on the pathologist’s report. In children who did not have appen-
pendicitis, we preferred that imaging (usually US in girls or CT dicitis, the discharge diagnosis was recorded. Children who im-
scan in boys) be ordered by the pediatric surgeon. The child proved under observation were discharged; those who did not
received intravenous hydration, nothing by mouth, and was al- return to the hospital were presumed not to have appendicitis.
lowed to rest, sometimes with sedation. Two reviewers (including A.M.K.) performed ⬎95% of chart re-
A second pediatric surgical evaluation was conducted 4 to 6 views, and 2 individuals (including A.M.K.) performed all the
hours later consisting of physical examination, usually repeat data entry. Outliers were double-checked by a second review of
WBC count and differential, and radiographic studies as deter- the original record. The data were entered into a computer pro-
mined by the pediatric surgeon. If appendicitis was diagnosed, the gram (Epi Info 2002, Centers for Disease Control and Prevention,
child was prepared for appendectomy. If the diagnosis remained Atlanta, GA) for analysis. Significance tests were performed to
in doubt, the child received hydration and rest for another 4 to 6 compare differences between groups. Means were tested by using
hours, after which a third pediatric surgical evaluation was done. the Student t or the Kruskal-Wallace test. 2 tests were used for
If appendicitis remained a possibility after the third evaluation, comparison of categorical variables. Sensitivity, specificity, posi-
appendectomy was done; otherwise, a nonsurgical diagnosis was tive predictive value, and negative predictive value were calcu-
made, and management was conducted in collaboration with the lated by standard epidemiologic methods.7 Accuracy was calcu-
attending pediatrician or family practitioner. lated by number of patients with correct diagnoses/total number
The medical records of 356 children and adolescents referred of patients. Reports from US or CT which were diagnostically
for possible appendicitis from January 1999 through December equivocal were not included in the calculation of accuracy. The
2001 were reviewed. Patients were identified from our practice study did not attempt to analyze separate aspects of the pediatric
database by using the diagnoses of appendicitis, perforated ap- surgical evaluation (history, physical examination, WBC count,
pendicitis, and abdominal pain/possible appendicitis. (Children differential count, or urinalysis) for determination of rank of im-
with abdominal pain who did not have possible appendicitis were portance in the diagnostic process.
Fig 1. Algorithm for diagnosis of appendicitis.
30 DIAGNOSIS OF APPENDICITIS BY PEDIATRIC SURGICAL EVALUATION
Downloaded from www.aappublications.org/news by guest on July 23, 2018
RESULTS referring physician in the 356 children (33%) before
The mean age of the 356 patients was 9.6 years pediatric surgical evaluation. An additional 60 stud-
(standard deviation ⫾ 3.83 years; range: 1–18 years). ies (17%) were ordered by the pediatric surgeon.
There were 144 females and 212 males. Of the 356 (The physician ordering 5 other imaging studies
children, 220 (62%) underwent appendectomy. Of could not be determined.) US alone was performed
these 220 children, 209 (95%) had pathologic confir- in 96 patients; CT scan alone was performed in 54
mation of appendicitis, and 11 (5%) had a normal patients, and both US and CT scan were performed
(negative) appendix. Of the 209 children with appen- in 16 patients. The sensitivity, specificity, positive
dicitis, 139 (66%) had acute appendicitis, 34 (16%) predictive value, negative predictive value, and ac-
had advanced appendicitis without perforation, and curacy of the pediatric surgical protocol for US alone
36 (17%) had advanced appendicitis with perfora- and CT scan alone for diagnosis of appendicitis are
tion. There were no significant changes from year to included in Table 2. We did not calculate accuracy of
year across the 3-year period in the proportion of sequential US and CT scan because only 16 (4.5%) of
patients with perforation or with a negative appen- 356 children had both studies. Fourteen (12.5%) of a
dix. total of 112 US examinations and 8 (11.4%) of a total
Disposition of the patients after initial pediatric of 70 CT examinations were equivocal and omitted
surgical consultation was: operation in 195 (55%) of from the calculations. The accuracy of diagnosis was
the 356 patients; observation in 152 patients (43%); similar in the children with prereferral diagnostic
and discharge home in 9 patients (2%). Of the 152 imaging studies (102 [94%] of 109) and children who
children who were observed, 25 were subsequently did not receive such studies (235 [95%] of 247; P ⫽
operated on for appendicitis, and 127 improved un- .5452). Table 3 compares the results of 3 recent re-
der observation (with hydration and supportive ther- ports for diagnosis of appendicitis based on imag-
apy) and were discharged from the hospital with a ing3,8,9 with our series based on clinical evaluation
diagnosis other than appendicitis. One of these 127 and selective imaging.
children returned to the hospital 6 days later with Of the 25 children who had appendectomy after a
perforated appendicitis and was considered a case of period of observation, 8 had acute appendicitis, 6
missed appendicitis. The diagnoses of 146 children had advanced appendicitis without perforation, 8
who did not have appendicitis are listed in Table 1. had perforated appendicitis, and 3 had a normal
The sensitivity of this protocol for the diagnosis of appendix. The proportion of children with advanced
appendicitis was 99%, the specificity was 92%, the or perforated appendicitis was greater in the 25 chil-
positive predictive value was 95%, the negative pre- dren who had appendectomy after observation com-
dictive value was 99%, and the accuracy was 97% pared with 195 children who had appendectomy
(Table 2). after initial evaluation (14 [56%] of 25 vs 57 [29%] of
Duration of symptoms before arrival at the hospi- 195; P ⫽ .0070). These 25 children, in additional
tal was significantly longer for children with ad- comparisons with the 195 children with appendec-
vanced/perforated appendicitis than for those with tomy after initial evaluation, were similar in age (9.28
early acute appendicitis (mean: 58.2 vs 26.0 hours; vs 10.18 years; P ⫽ .2394) and duration of symptoms
P ⱕ .0001). Median time from arrival at the hospital before admission (36.40 vs 36.22 hours; P ⫽ .9795)
to appendectomy in the 195 children diagnosed with but had higher rates of imaging (27 studies [100%] in
appendicitis at the initial pediatric surgical evalua- 25 patients vs 95 [49%] of 195; P ⬍ .0001), incorrect or
tion was 5 hours. Median time to appendectomy in equivocal interpretation of imaging (14 [52%] of 27 vs
the 25 children who had appendectomy after a pe- 26 [24%] of 95; P ⫽ .0168), and negative appendec-
riod of observation was 18 hours. tomy (3 [12%] of 25 vs 8 [4%] of 194; P ⫽ .1158).
Despite our preference that pediatric surgical eval- Nearly 40% (39.6%) of children were referred from
uation be conducted before imaging, 117 imaging rural counties outside of Lubbock County. Although
studies (67 US and 50 CT scans) were ordered by the mean duration of symptoms was greater in patients
from rural counties than in those from Lubbock
County (46.0 vs 35.1 hours; P ⫽ .0993, using a 1-tailed
TABLE 1. Diagnoses of 146 Children and Adolescents Who
Did Not Have Appendicitis
test), the rate of advanced/perforated appendicitis
was not different in rural children than in those from
Diagnosis No. of Patients Lubbock County (35.8% vs 29.5%; P ⫽ .3328). Com-
Gastroenteritis 54 plications (wound infection, intraabdominal abscess,
Constipation 31 and prolonged ileus) occurred in 8 (11%) of 70 chil-
Abdominal pain 23 dren with advanced/perforated appendicitis and in
Viral syndrome 9
Ovarian cyst 7 1 child (wound infection) of 150 (0.7%) with a non-
Pneumonia 6 perforated appendix. All children survived.
Pharyngitis/strep 4
Mesenteric lymphadenitis 2 DISCUSSION
Pancreatitis 2
Pyelonephritis/urinary tract infection 2
In many centers, imaging for possible appendicitis
Other* 6 has become routine. Reports advocating the CT scan
Total 146 with rectal contrast as the gold standard for diagno-
* 1 each: abdominal wall strain, diabetic ketoacidosis, dysmenor- sis of appendicitis have appeared in the medical,2,3
rhea, infectious mononucleosis, vomiting (unspecified), and not pediatric,4 – 6 radiologic,8 emergency medical,10 and
recorded. even the surgical11 literature and have had an enor-
Downloaded from www.aappublications.org/news by guest on July 23, 2018
ARTICLES 31
TABLE 2. Epidemiologic Measures of Pediatric Surgical Protocol and of Imaging Techniques for
Diagnosis of Appendicitis in This Series
Basis of No. of Sensitivity Specificity PPV NPV Accuracy
Diagnosis Patients (%) (%) (%) (%) (%)
Pediatric surgical 356 99.5 92.5 95.0 99.3 96.6
protocol
US 112 76.5 88.4 88.6 76.0 81.9
CT scan 70 87.2 80.0 93.2 66.7 90.3
PPV indicates positive predictive value; NPV, negative predictive value.
TABLE 3. A Comparison of Protocols for Diagnosis of Appendicitis
Study Basis of No. of Age* Sensitivity Specificity PPV NPV Accuracy Negative
Diagnosis Patients (y) (%) (%) (%) (%) (%) Appendix
(%)
Rao8 CT scan 100 28 98 98 98 98 98 13
Weyant et al9 CT scan 625 35 96 16 90 NS 88 12
Peña et al3 US ⫹ CT 139 3–21 94 94 90 97 94 12
Present study Clinical ⫹ selective 356 9.6 99 92 95 99 97 5
imaging
PPV indicates positive predictive value; NPV, negative predictive value.
* Mean age of patients (except in the Peña study, in which the mean age was not stated; the range of ages is shown).
mous influence on practice. Few reports have ques- after a period of observation represented a small
tioned the accuracy or wisdom of CT scanning for proportion of children who were observed (25 [16%]
appendicitis.9,12 Parents of a child with possible ap- of 152) and of children who underwent appendec-
pendicitis may request a CT scan because they have tomy (25 [11%] of 220). Although their rate of ad-
read about it in the lay press as the definitive test.13 vanced or perforated appendicitis was higher than
Evaluation by a pediatric surgeon early in the course that of our 195 children with appendectomy after
of a child with possible appendicitis has rarely been first evaluation (56% vs 29%; P ⫽ .0070), it could not
emphasized. be concluded that the period of observation was
Our data, however, support a diagnostic strategy responsible for the higher rate of advanced disease.
based primarily on the clinical acumen of a pediatric Many confounding factors could have influenced the
surgeon rather than imaging. Our sensitivity (99%), outcome in these 25 children. For example, the 25
specificity (93%), diagnostic accuracy (97%), and children may have represented a subgroup selected
negative appendectomy rate (5%) compare favorably by greater complexity of their clinical presentations.
with recent reports of imaging-based strategies in This hypothesis is supported by their high rates of
both adults and children (Table 3). Our rate of per- imaging studies, of incorrect or equivocal interpreta-
forated appendicitis (17%) compares favorably to tion of imaging studies, and of negative appendec-
other large pediatric series since 1995, the rates of tomy. Theoretically, the outcome of the observed
which have ranged from 15.5% to 47%.4,14 –18 Many patients might have been improved by more timely
different factors are associated with the perforation surgical decision making and more accurate inter-
rate, which in general varies inversely with age and pretation of imaging studies. Such refinements might
directly with duration of illness. Surprisingly, our shorten the period of observation and lower the rate
large proportion of children (40%) from rural coun- of advanced/perforated disease.
ties did not have an increased rate of perforation Because a missed diagnosis often leads to perfora-
compared with local children, despite their longer tion and complications, rates of negative appendec-
duration of symptoms. tomy of 12% to 18% are considered acceptable in
Because appendicitis is an evolving pathologic children.15,19 A recent nationwide study of ⬎261 000
process, and because early appendicitis may be im- appendectomies in both adults and children reported
possible to differentiate from other causes of abdom- a 15.3% rate of negative appendectomy20 and em-
inal pain in children, clinical reevaluation after a phasized the potential for enormous cost savings by
period of observation and supportive care may be a decrease in this rate. Our clinically based approach,
necessary. Cost analyses, however, may be biased with its low rate of negative appendectomy (5%),
toward testing to make the diagnosis at first encoun- may be more cost-effective than other diagnostic
ter; if appendicitis can be ruled out (by testing), the strategies. We did not perform a cost-effectiveness
patient may be sent home from the emergency de- analysis in this study because we did not have a
partment. In an urban setting, this strategy may be comparison group of children who did not receive
successful, especially if intravenous fluid resuscita- pediatric surgical evaluation early in their manage-
tion has been completed during the period of testing. ment for possible appendicitis.
In our rural west Texas population, however, dis- Protocols from tertiary medical centers may not be
charge home from the emergency department was generalizable. For example, an imaging protocol for
rarely an option. childhood appendicitis (US followed by CT with rec-
The 25 children who underwent appendectomy tal contrast) that originated from a large, urban, uni-
32 DIAGNOSIS OF APPENDICITIS BY PEDIATRIC SURGICAL EVALUATION
Downloaded from www.aappublications.org/news by guest on July 23, 2018
versity children’s hospital (Children’s Hospital, Bos- population that is prescreened to exclude patients
ton, MA) depended on a coterie of pediatric with abdominal pain who have no suspicion of ap-
radiologists with special interest and expertise in the pendicitis is therefore appropriate and was used by
radiographic diagnosis of pediatric appendicitis.3– 6 Peña et al3– 6 in several recent studies on diagnosis of
The cost of imaging (US ⫹ CT, in 1997 dollars) was pediatric appendicitis. Selection bias, which typically
reported as $907 per patient.6 Other tertiary centers occurs when nonrandomized groups with different
have chosen opposite strategies with successful out- characteristics are compared (incorrectly), is not a
comes. One large, urban, university children’s hos- factor if an entire population is selected for an obser-
pital (Children’s Hospital Medical Center, Cincin- vational study such as ours and those of Peña et al.
nati, OH), for example, used a clinical, evidence- Childhood CT is not innocuous; recent reports in
based pathway for appendicitis in which pediatric the radiologic literature have warned of a significant
surgical evaluation was conducted before any tests increase in lifetime radiation risk. Investigators from
were ordered. Imaging was done in doubtful cases. Columbia University, alarmed by a rapidly increas-
Quality of care, using as indicators the rates of ap- ing number of pediatric CT examinations, estimated
pendiceal perforation (25%) and negative appendec- that 500 individuals currently ⬍15 years old might
tomy (12%), was unchanged with this pathway, and ultimately die from cancer attributable to the CT
hospital costs were reduced significantly.19 A diag- radiation.22 A study from Belfast documented that
nostic strategy that depends on the clinical acumen ⬃50% of pediatric CT examinations at general hos-
of a pediatric surgeon may be more generalizable pitals failed to adjust the technique for patient age,
than one that requires the technologic skill and ex- thus exposing children to an unnecessarily high ra-
pertise unique to pediatric radiologists. diation dose.23 Donnelly et al,24 from Cincinnati, out-
Improved technology does not always translate lined a strategy for adjustment of standard adult CT
into improved diagnosis and patient outcomes. Wey- protocols to control the radiation dose in children.
ant et al9 studied 625 patients with appendicitis but The risk is not theoretical but is based on Japanese
found no correlation between CT findings and data on actual excess cancer in those who were irra-
pathologically proven appendiceal disease. A popu- diated as children in 1945.25 Because children are 10
lation-based study from the state of Washington an- times more sensitive than adults to the induction of
alyzed 63 707 appendectomies performed during a cancer, Hall26 estimated that an abdominal helical CT
12-year period (1987–1998), during which great im- scan in a young girl results in a risk of fatal cancer
provements in CT, US, and laparoscopy occurred. later in life that amounts to about 1 in 1000. The
Contrary to expectation, however, the incidence of public health problem becomes significant when the
negative appendectomies (15.5%) and perforation small individual risk is multiplied by the 2.7 million
(25.8%) did not change with the availability of ad- of such procedures performed annually.26 Thus a
vanced diagnostic testing.21 strategy that relies on careful history and physical
A limitation of our investigation is its retrospective examination and minimizes radiation exposure may
format. Despite our preference that imaging studies be inherently safer than one that relies on routine
be ordered by the pediatric surgeon, a CT scan, imaging. Future investigations should consider the
which some authors now consider as the definitive risk of radiation exposure against possible benefits in
imaging study,4 was ordered in 50 (14%) of 356 chil- cost effectiveness or diagnostic accuracy for this
dren by the referring physician before pediatric sur- common pediatric condition.
gical evaluation. We could not determine retrospec-
tively whether such prereferral imaging was helpful
or superfluous in making the diagnosis of appendi- ACKNOWLEDGMENTS
citis; however, the data suggest that it may have been We are grateful to Christy Ratheal, RN, for keeping our practice
superfluous, because the accuracy of diagnosis of database and for assistance with data entry; Catherine Lovett, RN,
BS, for assistance with data collection; and John Griswold, MD, for
appendicitis was no better with prereferral imaging encouragement and expert advice.
(94%) than without it (95%).
Because the children in our study population were
prescreened by another physician before referral, REFERENCES
they were more likely to have appendicitis than an 1. Popovic JR. 1999 National Hospital Discharge Survey: annual summary
unscreened population of children with the initial with detailed diagnosis and procedure data. Vital Health Stat 13. 2001;
presentation of abdominal pain. Selection thus (151):i–v, 1–206
2. Rao PM, Rhea JT, Novelline RA, Mostafave AA, McCabe CJ. Effect of
would account for our relatively high proportion of computed tomography of the appendix on treatment of patients and use
children with confirmed appendicitis (62%). Selec- of hospital resources. N Engl J Med. 1998;338:141–146
tion by prescreening, however, does not affect the 3. Peña BM, Mandl KD, Kraus SJ, et al. Ultrasonography and limited
study outcomes, ie, the perforation rate or negative computed tomography in the diagnosis and management of appendi-
citis in children. JAMA. 1999;282:1041–1046
appendectomy rate, because the denominator of 4. Peña BM, Taylor GA, Fishman SJ, Mandl KD. Effect of an imaging
these outcomes is the number of children who actu- protocol on clinical outcomes among pediatric patients with appendi-
ally undergo operation. Further, selection by pre- citis. Pediatrics. 2002;110:1088 –1093
screening does not affect the epidemiologic measures 5. Peña BM, Taylor GA, Fishman SJ, Mandl KD. Costs and effectiveness of
(sensitivity, specificity, positive predictive value, ultrasonography and limited computed tomography for diagnosing
appendicitis in children. Pediatrics. 2000;106:672– 676
negative predictive value, and accuracy), because 6. Peña BM, Taylor GA, Lund DP, Mandl KD. Effect of computed tomog-
these measures are based on correct diagnoses, not raphy on patient management and costs in children with suspected
on the proportion of subjects with appendicitis. A appendicitis. Pediatrics. 1999;104:440 – 446
Downloaded from www.aappublications.org/news by guest on July 23, 2018
ARTICLES 33
7. Gordis L. Epidemiology. 2nd ed. Philadelphia, PA: Saunders; 2000:64 –75 diagnosed in a pediatric emergency department. Pediatr Emerg Care.
8. Rao PM. CT for suspected appendicitis. AJR Am J Roentgenol. 1999;172: 2000;16:233–237
1447–1448 18. Gadomski A, Jenkins P. Ruptured appendicitis among children as an
9. Weyant MJ, Eachempati SR, Maluccio MA, et al. Interpretation of com- indicator of access to care. Health Serv Res. 2001;36:129 –142
puted tomography does not correlate with laboratory or pathologic 19. Warner BW, Kulick RM, Stoops MM, Mehta S, Stephan M, Kotagal UR.
findings in surgically confirmed acute appendicitis. Surgery. 2000;128: An evidence-based clinical pathway for acute appendicitis decreases
145–152 hospital duration and cost. J Pediatr Surg. 1998;33:1371–1375
10. Rao PM. Plain abdominal radiography in clinically suspected 20. Flum DR, Koepsell T. The clinical and economic correlates of misdiag-
appendicitis: diagnostic yield, resource use, and comparison with CT. nosed appendicitis: nationwide analysis. Arch Surg. 2002;137:799 – 804
Am J Emerg Med. 1999;17:325–328 21. Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of
11. Rao PM, Rhea JT, Rattner DW, Venus LG, Novelline RA. Introduction of
appendicitis decreased over time? A population-based analysis. JAMA.
appendiceal CT: impact on negative appendectomy and appendiceal
2001;286:1748 –1753
perforation rates. Ann Surg. 1999;229:344 –349
22. Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-
12. Karakas SP, Guelfguat M, Leonidas JC, Springer S, Singh SP. Acute
induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:
appendicitis in children: comparison of clinical diagnosis with ultra-
289 –296
sound and CT imaging. Pediatr Radiol. 2000;30:94 –98
23. Paterson A, Frush DP, Donnelly LF. Helical CT of the body: are settings
13. Lawrence J. Computed tomography in diagnosing suspected appendi-
citis [letter]. Pediatrics. 2001;107:1231–1232 adjusted for pediatric patients? AJR Am J Roentgenol. 2001;176:
14. Emil S, Laberge J-M, Mikhail P, et al. Appendicitis in children: a 297–301
ten-year update of therapeutic recommendations. J Pediatr Surg. 2003; 24. Donnelly LF, Emery KH, Brody AS, et al. Minimizing radiation dose for
38:236 –242 pediatric body application of single-detector helical CT: strategies at a
15. Pearl RH, Hale DA, Molloy M, Schutt DC, Jaques DP. Pediatric appen- large Children’s Hospital. AJR Am J Roentgenol. 2001;176:303–306
dectomy. J Pediatr Surg. 1995;30:173–181 25. Berdon WE, Slovis TL. Where we are since ALARA and the series of
16. O’Toole SJ, Karamanoukian HL, Allen JE, et al. Insurance-related dif- articles on CT dose in children and risk of long-term cancers: what has
ferences in the presentation of pediatric appendicitis. J Pediatr Surg. changed? Pediatr Radiol. 2002;32:699
1996;31:1032–1034 26. Hall EJ. Lessons we have learned from our children: cancer risks from
17. Nelson DS, Bateman B, Bolte RG. Appendiceal perforation in children diagnostic radiology. Pediatr Radiol. 2002;32:700 –706
GOING AFTER THE UNINSURED
“The charges issues has become a focus of healthcare advocates, who have
flagged a major inequity in the billing system: While hospitals negotiate discounts
with insurers and HMOs that require payment of only a fraction of the listed
charges, they ask the uninsured to pay the full rates and then pursue them
aggressively to collect.”
Lagnado L. Hospitals urged to end harsh tactics for billing uninsured. Wall Street Journal, July 7, 2003
Submitted by Student
34 DIAGNOSIS OF APPENDICITIS BY PEDIATRIC SURGICAL EVALUATION
Downloaded from www.aappublications.org/news by guest on July 23, 2018
The Diagnosis of Appendicitis in Children: Outcomes of a Strategy Based on
Pediatric Surgical Evaluation
Ann M. Kosloske, C. Lance Love, James E. Rohrer, Jane F. Goldthorn and Stuart R.
Lacey
Pediatrics 2004;113;29
DOI: 10.1542/peds.113.1.29
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/113/1/29
References This article cites 25 articles, 4 of which you can access for free at:
http://pediatrics.aappublications.org/content/113/1/29#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Gastroenterology
http://www.aappublications.org/cgi/collection/gastroenterology_sub
Surgery
http://www.aappublications.org/cgi/collection/surgery_sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news by guest on July 23, 2018
The Diagnosis of Appendicitis in Children: Outcomes of a Strategy Based on
Pediatric Surgical Evaluation
Ann M. Kosloske, C. Lance Love, James E. Rohrer, Jane F. Goldthorn and Stuart R.
Lacey
Pediatrics 2004;113;29
DOI: 10.1542/peds.113.1.29
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/113/1/29
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,
60007. Copyright © 2004 by the American Academy of Pediatrics. All rights reserved. Print ISSN:
1073-0397.
Downloaded from www.aappublications.org/news by guest on July 23, 2018
Você também pode gostar
- Defining Child Abuse TypesDocumento14 páginasDefining Child Abuse TypesAndreas Springfield GleasonAinda não há avaliações
- Orthopedics Prometric Mcq1 SamplesDocumento7 páginasOrthopedics Prometric Mcq1 SamplesshaifAinda não há avaliações
- Meningocele Case StudyDocumento70 páginasMeningocele Case StudyKyssel Seyer100% (2)
- A1 Gluten Free Materials LonghurstDocumento23 páginasA1 Gluten Free Materials LonghurstWarriorLast100% (1)
- Drug StudyDocumento9 páginasDrug StudyKatrina Mae RamirezAinda não há avaliações
- Snake BiteDocumento206 páginasSnake BiteElviraThaherAinda não há avaliações
- Concepts of Physical FitnessDocumento5 páginasConcepts of Physical FitnessNilo Golosino III100% (1)
- Frozen Shoulder ExercisesDocumento7 páginasFrozen Shoulder ExercisesSumon PhysioAinda não há avaliações
- Psychopathy NotesDocumento10 páginasPsychopathy Notesjsoldinger15100% (1)
- Chronic Apical Periodontitis.Documento24 páginasChronic Apical Periodontitis.Alina EsanuAinda não há avaliações
- Psychiatric Disorders in PregnancyDocumento30 páginasPsychiatric Disorders in PregnancyAnusha Verghese100% (1)
- IjnnjjiiDocumento8 páginasIjnnjjiiSelvyani PasombaAinda não há avaliações
- Article ApendicitisDocumento7 páginasArticle ApendicitisXerexAinda não há avaliações
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocumento6 páginasSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedAinda não há avaliações
- US en EndometritisDocumento7 páginasUS en EndometritisRubí FuerteAinda não há avaliações
- Use of White Blood Cell Count and Negative Appendectomy RateDocumento8 páginasUse of White Blood Cell Count and Negative Appendectomy RatePremaKurniaAinda não há avaliações
- E37 FullDocumento10 páginasE37 FullAtika RahmahAinda não há avaliações
- To Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongDocumento6 páginasTo Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongIkki DongAinda não há avaliações
- RheumatologyDocumento3 páginasRheumatologyluizamgoAinda não há avaliações
- Comparison of Ultrasound Versus Computed Tomography For The Detection of Kidney Stones in The Pediatric Population A Clinical Effectiveness StudyDocumento11 páginasComparison of Ultrasound Versus Computed Tomography For The Detection of Kidney Stones in The Pediatric Population A Clinical Effectiveness StudyLalu Editia SubihardiAinda não há avaliações
- Pediatric NAR Trend, Predictors and DifferentialsDocumento5 páginasPediatric NAR Trend, Predictors and DifferentialsBariša KiršnerAinda não há avaliações
- Amniocentesis Results and Retrospective Analysis Performed in The University ClinicDocumento6 páginasAmniocentesis Results and Retrospective Analysis Performed in The University ClinicCindy Denti PratikasariAinda não há avaliações
- 1 s2.0 S002234681930301X 2Documento5 páginas1 s2.0 S002234681930301X 2suyudi kimikoAinda não há avaliações
- Perforated Appendicitis PDFDocumento8 páginasPerforated Appendicitis PDFMuhammad AkrimAinda não há avaliações
- Comparison Between Small and Large Bowel Intussusception in ChildrenDocumento3 páginasComparison Between Small and Large Bowel Intussusception in ChildrenParamartha KesumaAinda não há avaliações
- Classifying Patients Suspected of Appendicitis With Regard To LikelihoodDocumento6 páginasClassifying Patients Suspected of Appendicitis With Regard To LikelihoodabybmusAinda não há avaliações
- Laparotomy in Children in A Tertiary Hospital in A Developing CountryDocumento5 páginasLaparotomy in Children in A Tertiary Hospital in A Developing CountryWorld Journal of Clinical SurgeryAinda não há avaliações
- Misdiagnosed Appendicitis in ChildrenDocumento7 páginasMisdiagnosed Appendicitis in ChildrenMusyawarah MelalaAinda não há avaliações
- Appendicitis NaddlerDocumento6 páginasAppendicitis NaddlerMedardo ApoloAinda não há avaliações
- Functional Outcome of Anorectal Malformations and Associated Anomalies in Era of Krickenbeck ClassificationDocumento4 páginasFunctional Outcome of Anorectal Malformations and Associated Anomalies in Era of Krickenbeck ClassificationdarmiAinda não há avaliações
- Febrile Urinary Tract Infections in 0-To 3-Month-Old Infants: A Prospective Follow-Up StudyDocumento4 páginasFebrile Urinary Tract Infections in 0-To 3-Month-Old Infants: A Prospective Follow-Up StudyMark Vertiz CernaAinda não há avaliações
- Apendicitis y EmbarazoDocumento6 páginasApendicitis y EmbarazoBernardo RomeroAinda não há avaliações
- Use of The Skeletal Survey in The Evaluation of Child MaltreatmentDocumento3 páginasUse of The Skeletal Survey in The Evaluation of Child MaltreatmentAprilia DhammashintaAinda não há avaliações
- Acute Appendicitis in Children - Diagnostic Imaging - UpToDateDocumento28 páginasAcute Appendicitis in Children - Diagnostic Imaging - UpToDateHafiz Hari NugrahaAinda não há avaliações
- Our Experience With Adnexal Masses in The Pediatric Age Group and Review of LiteratureDocumento6 páginasOur Experience With Adnexal Masses in The Pediatric Age Group and Review of LiteratureEdwin CalleAinda não há avaliações
- Original ContributionsDocumento8 páginasOriginal ContributionsDaniyRosaAinda não há avaliações
- Current Success in The Treatment of Intussusception in ChildrenDocumento9 páginasCurrent Success in The Treatment of Intussusception in ChildrenOby RomdhoniAinda não há avaliações
- HydrocephalusDocumento8 páginasHydrocephaluscaliptra36Ainda não há avaliações
- Hefler Et Al., 2009Documento4 páginasHefler Et Al., 2009Jonathan LucisAinda não há avaliações
- The Role of Physical Examination in Establishing The Diagnosis of PneumoniaDocumento4 páginasThe Role of Physical Examination in Establishing The Diagnosis of PneumoniaCarlos GuiterizAinda não há avaliações
- 1 Sttri 3Documento6 páginas1 Sttri 3parkfishyAinda não há avaliações
- Schallert 2019Documento7 páginasSchallert 2019Dian Putri NingsihAinda não há avaliações
- Acute Appendicitis in Children - Diagnostic Imaging - UpToDateDocumento33 páginasAcute Appendicitis in Children - Diagnostic Imaging - UpToDateლელა ნიშნიანიძეAinda não há avaliações
- A Study of Inguinal Hernia in ChildrenDocumento5 páginasA Study of Inguinal Hernia in ChildrenrhmathidayatAinda não há avaliações
- Pi Is 0022347618300465Documento8 páginasPi Is 0022347618300465debbyrahmadiniAinda não há avaliações
- Cytology Anat 30 JulyDocumento11 páginasCytology Anat 30 JulySamir ShinnawiAinda não há avaliações
- Aydin 2017Documento7 páginasAydin 2017Berry BancinAinda não há avaliações
- The American Journal of Surgery: J. Quinn Gentles, Gabriela Meglei, Leo Chen, Cameron J. Hague, Adrienne L. MelckDocumento5 páginasThe American Journal of Surgery: J. Quinn Gentles, Gabriela Meglei, Leo Chen, Cameron J. Hague, Adrienne L. Melcksuyudi kimikoAinda não há avaliações
- emil2006Documento5 páginasemil2006mia widiastutiAinda não há avaliações
- Consequences of Prenatal Ultrasound Diagnosis: A Preliminary Report On Neonates With Congenital MalformationsDocumento8 páginasConsequences of Prenatal Ultrasound Diagnosis: A Preliminary Report On Neonates With Congenital MalformationsSafinaz InazAinda não há avaliações
- Screening of Asymptomatic Children For Tuberculosis:: Is A Lateral Chest Radiograph Routinely Indicated?Documento7 páginasScreening of Asymptomatic Children For Tuberculosis:: Is A Lateral Chest Radiograph Routinely Indicated?jayyidahafifahAinda não há avaliações
- 2013 Different Guidelines For Imaging After First UTI in Febrile Infants - Yield, Cost and RadiationDocumento9 páginas2013 Different Guidelines For Imaging After First UTI in Febrile Infants - Yield, Cost and RadiationAnneCanapiAinda não há avaliações
- ApendicitisDocumento5 páginasApendicitisAtziri LoeraAinda não há avaliações
- Dream 2020Documento4 páginasDream 2020Karlito Dela CruzAinda não há avaliações
- Rumination Syndrome in Children and Adolescents: Diagnosis, Treatment, and PrognosisDocumento7 páginasRumination Syndrome in Children and Adolescents: Diagnosis, Treatment, and PrognosisryselAinda não há avaliações
- Use and Accuracy of Diagnostic Imaging by Hospital Type in Pediatric AppendicitisDocumento2 páginasUse and Accuracy of Diagnostic Imaging by Hospital Type in Pediatric AppendicitisdionesophiaAinda não há avaliações
- Low-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticleDocumento10 páginasLow-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticleNia MidfordAinda não há avaliações
- Usg Acute AppendicitisDocumento10 páginasUsg Acute AppendicitisAtika RahmahAinda não há avaliações
- Clinical CharacteristicsDocumento9 páginasClinical CharacteristicsManusama HasanAinda não há avaliações
- Combination of Alvarado Score and Ultrasound Findings in Diagnosis of Acute Appendicitis in ChildrenDocumento30 páginasCombination of Alvarado Score and Ultrasound Findings in Diagnosis of Acute Appendicitis in ChildrenMaya Astuti SaphiraAinda não há avaliações
- J Neurosurg Pediatr Article p52Documento10 páginasJ Neurosurg Pediatr Article p52Audhrey BAinda não há avaliações
- Bladder Management in Children With Transverse MyelitisDocumento6 páginasBladder Management in Children With Transverse Myelitisdipan diratuAinda não há avaliações
- Yeung TeenagersDocumento5 páginasYeung TeenagersAnonymous YyLSRdAinda não há avaliações
- Low-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticleDocumento10 páginasLow-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticlePra YudhaAinda não há avaliações
- Jurnal Pediatri 2Documento10 páginasJurnal Pediatri 2Fluffyyy BabyyyAinda não há avaliações
- Elkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialDocumento6 páginasElkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialModou NianeAinda não há avaliações
- Neutropenic Colitis in Children 2011Documento4 páginasNeutropenic Colitis in Children 2011IRINA SULEY TIRADO PEREZAinda não há avaliações
- Radiography: G. Ogunmefun, M. Hardy, S. BoynesDocumento8 páginasRadiography: G. Ogunmefun, M. Hardy, S. BoynesDian J PutraAinda não há avaliações
- Early appendectomy significantly reduces costs for perforated appendicitis in childrenDocumento8 páginasEarly appendectomy significantly reduces costs for perforated appendicitis in childrenLestari Chye PouedanAinda não há avaliações
- Fa Lomo 2018Documento6 páginasFa Lomo 2018Mateus CespedesAinda não há avaliações
- Upper Tract Urothelial CarcinomaNo EverandUpper Tract Urothelial CarcinomaShahrokh F. ShariatAinda não há avaliações
- FST Annual Conference 2023 Abstract GuidelinesDocumento3 páginasFST Annual Conference 2023 Abstract GuidelinesAndikaAinda não há avaliações
- Accepted Manuscript: 10.1016/j.jpedsurg.2018.03.021Documento23 páginasAccepted Manuscript: 10.1016/j.jpedsurg.2018.03.021AndikaAinda não há avaliações
- Laplant 2018Documento14 páginasLaplant 2018AndikaAinda não há avaliações
- Euro Guideline 2001 Balanoposthitis PDFDocumento5 páginasEuro Guideline 2001 Balanoposthitis PDFrahmaAinda não há avaliações
- 10 1016@j Jpedsurg 2019 01 040Documento14 páginas10 1016@j Jpedsurg 2019 01 040AndikaAinda não há avaliações
- Factors Linked to Rectal Prolapse After AnorectoplastyDocumento5 páginasFactors Linked to Rectal Prolapse After AnorectoplastyAndikaAinda não há avaliações
- Snakebite in Indonesia: Randy Adiwinata, Erni J. NelwanDocumento8 páginasSnakebite in Indonesia: Randy Adiwinata, Erni J. NelwanSalma KarimahAinda não há avaliações
- 10 1016@j Jpedsurg 2019 01 040Documento14 páginas10 1016@j Jpedsurg 2019 01 040AndikaAinda não há avaliações
- Saluja 2017Documento6 páginasSaluja 2017AndikaAinda não há avaliações
- Jadwal Dokter Oktober 17Documento2 páginasJadwal Dokter Oktober 17Juarendra Ramadhani Jr.Ainda não há avaliações
- Guidelines on Paediatric Urology DiseasesDocumento14 páginasGuidelines on Paediatric Urology DiseasesEndang Yulia AngrainiAinda não há avaliações
- Bulan Pebruari 2008 Bulan Maret 2008 No Tanggal Nama Umur Diagnosis Ket No Tanggal Nama Umur Diagnosis KetDocumento38 páginasBulan Pebruari 2008 Bulan Maret 2008 No Tanggal Nama Umur Diagnosis Ket No Tanggal Nama Umur Diagnosis KetAndikaAinda não há avaliações
- 2020 2360 Moesm1 EsmDocumento1 página2020 2360 Moesm1 EsmAndikaAinda não há avaliações
- Functional Outcomes of Patients With Short-Segment Hirschsprung Disease After Transanal Endorectal Pull-ThroughDocumento6 páginasFunctional Outcomes of Patients With Short-Segment Hirschsprung Disease After Transanal Endorectal Pull-ThroughAndikaAinda não há avaliações
- Management of Fecal Incontinence: Andrea Bischoff January 21, 2021Documento32 páginasManagement of Fecal Incontinence: Andrea Bischoff January 21, 2021AndikaAinda não há avaliações
- Feeding Alternative for Gastrostomy PatientsDocumento3 páginasFeeding Alternative for Gastrostomy PatientsAndikaAinda não há avaliações
- Effective ImagingDocumento10 páginasEffective ImagingAndikaAinda não há avaliações
- Radial Neck Fractures in ChildrenDocumento4 páginasRadial Neck Fractures in ChildrenAndikaAinda não há avaliações
- Retroperitoneal Teratomas in Children: Amit Chaudhary, Samir Misra, Ashish Wakhlu, R.K. Tandon and A.K. WakhluDocumento3 páginasRetroperitoneal Teratomas in Children: Amit Chaudhary, Samir Misra, Ashish Wakhlu, R.K. Tandon and A.K. WakhluAndikaAinda não há avaliações
- A Comparison of Circumumbilical and Transverse AbdominalDocumento5 páginasA Comparison of Circumumbilical and Transverse AbdominalTammie YoungAinda não há avaliações
- App in Children PDFDocumento9 páginasApp in Children PDFAndikaAinda não há avaliações
- Impact App PDFDocumento7 páginasImpact App PDFAndikaAinda não há avaliações
- Hambraeus 2016Documento20 páginasHambraeus 2016AndikaAinda não há avaliações
- Anorectal Malf Wo Fistula PDFDocumento4 páginasAnorectal Malf Wo Fistula PDFAndikaPurbaAinda não há avaliações
- App in Children PDFDocumento9 páginasApp in Children PDFAndikaAinda não há avaliações
- Gastrostomy Feeding ProcedureDocumento5 páginasGastrostomy Feeding ProcedureRohini RaiAinda não há avaliações
- Petitioner Vs Vs Respondents: Third DivisionDocumento9 páginasPetitioner Vs Vs Respondents: Third DivisionRamon DyAinda não há avaliações
- MSI22 OnlinedistributionDocumento28 páginasMSI22 Onlinedistributionsunnyn1Ainda não há avaliações
- Group 6 Case Study Pancreatic CancerDocumento20 páginasGroup 6 Case Study Pancreatic CancerMarcel TabucolAinda não há avaliações
- Philippine Supreme Court Rules in Favor of Worker's Compensation ClaimDocumento5 páginasPhilippine Supreme Court Rules in Favor of Worker's Compensation ClaimShash BernardezAinda não há avaliações
- Water Borne Disease Signs, Symptoms and PreventionDocumento5 páginasWater Borne Disease Signs, Symptoms and PreventionRoxie SilvanoAinda não há avaliações
- The Art of Ageing WellDocumento3 páginasThe Art of Ageing WellDrhaidee BassAinda não há avaliações
- مهم للمزاولةDocumento13 páginasمهم للمزاولةbelal nurseAinda não há avaliações
- Euthanasia and Physician Assisted Suicide ExplainedDocumento22 páginasEuthanasia and Physician Assisted Suicide ExplainedSANA SAFDARAinda não há avaliações
- Patofisio DemamDocumento29 páginasPatofisio DemamJanet UngAinda não há avaliações
- Health Hazard EvalutionDocumento13 páginasHealth Hazard Evalutionshintia febrianiAinda não há avaliações
- Diet Analysis ProjectDocumento7 páginasDiet Analysis ProjectBrittany DiamondGurl ColbertAinda não há avaliações
- Introduction To MicrobesDocumento10 páginasIntroduction To MicrobesAngela WeaslyAinda não há avaliações
- 2922radioactivity Summary Cheat Sheet..Aidan MatthewsDocumento3 páginas2922radioactivity Summary Cheat Sheet..Aidan MatthewsSyed Mairaj Ul HaqAinda não há avaliações
- SX - Surgical Clinical Skills - Update2 VERY GOOD FOR OSCEDocumento158 páginasSX - Surgical Clinical Skills - Update2 VERY GOOD FOR OSCEamanda deonananAinda não há avaliações
- Skin Integrity and Wound CareDocumento55 páginasSkin Integrity and Wound Caremango47Ainda não há avaliações
- Inake Forms AJD Complete Nov 07 - Rev 09072009Documento19 páginasInake Forms AJD Complete Nov 07 - Rev 09072009adruckerAinda não há avaliações
- Unit 3. Digestive SystemDocumento46 páginasUnit 3. Digestive SystemNURIA VAZQUEZAinda não há avaliações
- Ocular InfectionsDocumento129 páginasOcular Infectionsnorma paulina carcausto lipaAinda não há avaliações
- Urinary System15Documento47 páginasUrinary System15Michael John PaderesAinda não há avaliações