Escolar Documentos
Profissional Documentos
Cultura Documentos
Atherosclerosis-A Brief Review: Biochemistry For Medics WWW - Namrata.co
Enviado por
Muhammad Tariq Raza100%(1)100% acharam este documento útil (1 voto)
117 visualizações46 páginaspathology
Título original
Atherosclerosis
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentopathology
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
100%(1)100% acharam este documento útil (1 voto)
117 visualizações46 páginasAtherosclerosis-A Brief Review: Biochemistry For Medics WWW - Namrata.co
Enviado por
Muhammad Tariq Razapathology
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 46
Atherosclerosis- A Brief Review
Biochemistry for Medics
www.namrata.co
11/15/2012 Biochemistry for Medics 1
Normal Blood Vessel Wall
• Vessel walls are
organized into three
concentric layers:
intima, media, and
adventitia
• These are present to
some extent in all
vessels but are most
apparent in larger
arteries and veins.
11/15/2012 Biochemistry for Medics 2
Normal Blood Vessel Wall
Blood vessel walls
1. The three tunics:
a) Tunica intima
(1) Endothelium
(2) Subendothelial layer
b) Tunica media
(1) Smooth muscle
(2) Elastin
c) Tunica adventitia (externa)
(1) CT(Connective tissue) surrounding TM(Tunica Media)
(2) Arterioles in larger vessels
11/15/2012 Biochemistry for Medics 3
Normal Blood Vessel Wall
11/15/2012 Biochemistry for Medics 4
Normal Blood Vessel Wall
• Arterial walls are
thicker than
corresponding
veins at the same
level of branching
to accommodate
pulsatile flow and
higher blood
pressure.
11/15/2012 Biochemistry for Medics 5
Classes of Arteries
Arteries
a) Elastic arteries – large arteries near heart
b) Muscular (distributing) arteries – thick tunica
media
c) Arterioles- Diameter regulated by
vasoconstriction/dilation
Atherosclerosis affects mainly elastic and muscular
arteries and hypertension affects small muscular
arteries and arterioles.
11/15/2012 Biochemistry for Medics 6
Atherosclerosis
Atherosclerosis is a disease of large and
medium-sized muscular arteries and is
characterized by –
endothelial dysfunction,
vascular inflammation, and
the buildup of lipids, cholesterol, calcium, and
cellular debris within the intima of the vessel
wall.
11/15/2012 Biochemistry for Medics 7
Atherosclerosis
It is characterized by
intimal lesions called
atheromas (also called
Atheromatous or
atherosclerotic
plaques), that
protrude into vascular
lumina.
11/15/2012 Biochemistry for Medics 8
Atheromatous plaque
An Atheromatous plaque consists of a
raised lesion with a soft, yellow, grumous core
of lipid (mainly cholesterol and cholesterol
esters) covered by a firm, white fibrous cap.
Besides obstructing blood
flow, atherosclerotic plaques weaken the
underlying media and can themselves
rupture, causing acute thrombosis.
11/15/2012 Biochemistry for Medics 9
Atheromatous plaque
Atherosclerosis or Arteriosclerosis is a slow and
progressive building up of plaque, fatty
substances, cholesterol, cellular waste
products, calcium andBiochemistry
11/15/2012 fibrinforin the inner lining of
Medics 10
Atherosclerosis
Atherosclerosis primarily affects elastic
arteries (e.g., aorta, carotid, and iliac arteries)
Large and medium-sized muscular arteries
(e.g., coronary and popliteal arteries).
In small arteries, atheromas can gradually
occlude lumina, compromising blood flow to
distal organs and cause ischemic injury.
11/15/2012 Biochemistry for Medics 11
Atherosclerosis
Atherosclerosis also takes a toll through other
consequences of acutely or chronically diminished arterial
perfusion, such as mesenteric occlusion, sudden cardiac
death, chronic IHD, and ischemic encephalopathy.
11/15/2012 Biochemistry for Medics 12
Risk Factors for Atherosclerosis
Major risk factors (Non Modifiable)-
Increasing Age
Male gender
Family history
Genetic abnormalities
11/15/2012 Biochemistry for Medics 13
Risk Factors for Atherosclerosis
Lesser, Uncertain, or Nonquantitated Risks-
Obesity
Physical Inactivity
Postmenopausal estrogen deficiency
High carbohydrate intake
Lipoprotein(a)
Hardened (trans)unsaturated fat intake
Chlamydia pneumoniae infection
11/15/2012 Biochemistry for Medics 14
Risk Factors for Atherosclerosis
Potentially Controllable-
Hyperlipidemia
Hypertension
Cigarette smoking
Diabetes
C-reactive protein
11/15/2012 Biochemistry for Medics 15
Age as a risk factor
Age is a dominant influence.
Although the accumulation of atherosclerotic
plaque is typically a progressive process, it does
not usually become clinically manifest until
lesions reach a critical threshold and begin to
precipitate organ injury in middle age or later.
Thus, between ages 40 and 60, the incidence of
myocardial infarction in men increases fivefold
Death rates from IHD rise with each decade even
into advanced age.
11/15/2012 Biochemistry for Medics 16
Gender
Premenopausal women are relatively protected
against atherosclerosis and its consequences
compared with age-matched men
Myocardial infarction and other complications of
atherosclerosis are uncommon in premenopausal
women unless otherwise predisposed by
diabetes, hyperlipidemia, or severe hypertension.
After menopause, the incidence of
atherosclerosis-related diseases increases and
with greater age exceeds that of men.
11/15/2012 Biochemistry for Medics 17
Genetics
The familial predisposition to atherosclerosis
and IHD is multifactorial.
In some instances it relates to familial
clustering of other risk factors, such as
hypertension or diabetes
In others it involves well-defined genetic
derangements in lipoprotein metabolism, such
as familial hypercholesterolemia that result in
excessively high blood lipid levels.
11/15/2012 Biochemistry for Medics 18
Hyperlipidemia
Hyperlipidemia-more
specifically, hypercholesterolemia-is a major risk
factor for atherosclerosis;
Even in the absence of other risk
factors, hypercholesterolemia is sufficient to
stimulate lesion development.
The major component of serum cholesterol
associated with increased risk is low-density
lipoprotein (LDL) cholesterol ("bad cholesterol")
11/15/2012 Biochemistry for Medics 19
Hyperlipidemia
LDL cholesterol has an essential physiologic role
delivering cholesterol to peripheral tissues.
In contrast, high-density lipoprotein (HDL, "good
cholesterol") mobilizes cholesterol from
developing and existing atheromas and
transports it to the liver for excretion in the bile.
Consequently, higher levels of HDL correlate with
reduced risk.
11/15/2012 Biochemistry for Medics 20
Factors affecting plasma lipid levels
High dietary intake of cholesterol and saturated
fats (present in egg yolks, animal fats, and
butter, for example) raises plasma cholesterol
levels.
Diets low in cholesterol and/or with higher ratios
of polyunsaturated fats lower plasma cholesterol
levels.
Omega-3 fatty acids (abundant in fish oils) are
beneficial, whereas (trans)unsaturated fats
produced by artificial hydrogenation of
polyunsaturated oils (used in baked goods and
margarine) adversely affect cholesterol profiles.
11/15/2012 Biochemistry for Medics 21
Factors affecting plasma lipid levels
Exercise and moderate consumption of
ethanol both raise HDL levels, whereas obesity
and smoking lower it.
Statins are a class of drugs that lower
circulating cholesterol levels by inhibiting
hydroxy methylglutaryl coenzyme A
reductase, the rate-limiting enzyme in hepatic
cholesterol biosynthesis.
11/15/2012 Biochemistry for Medics 22
Hypertension
On its own, hypertension can increase the risk
of IHD by approximately 60% in comparison
with normotensive populations
Left untreated, roughly half of hypertensive
patients will die of IHD or congestive heart
failure, and another third will die of stroke.
11/15/2012 Biochemistry for Medics 23
Cigarette Smoking
Cigarette smoking is a well-established risk factor
in men
An increase in the number of women who smoke
probably accounts for the increasing incidence
and severity of atherosclerosis in women.
Prolonged (years) smoking of one pack of
cigarettes or more daily increases the death rate
from IHD by 200%.
Smoking cessation reduces that risk substantially.
11/15/2012 Biochemistry for Medics 24
Diabetes Mellitus
Diabetes mellitus induces
hypercholesterolemia as well as a markedly
increased predisposition to atherosclerosis.
Other factors being equal, the incidence of
myocardial infarction is twice as high in
diabetic as in Nondiabetic individuals.
There is also an increased risk of strokes and a
100-fold increased risk of atherosclerosis-
induced gangrene of the lower extremities.
11/15/2012 Biochemistry for Medics 25
Additional Risk Factors
Despite the identification of
hypertension, diabetes, smoking, and
hyperlipidemia as major risk factors, as many
as 20% of all cardiovascular events occur in
the absence of any of these.
other "nontraditional" factors contribute to
risk.
11/15/2012 Biochemistry for Medics 26
Lipoprotein a or Lp(a)
Lipoprotein a or Lp(a), is an altered form of
LDL that contains the apolipoprotein B-100
portion of LDL linked to apolipoprotein A;
Increased Lp(a) levels are associated with a
higher risk of coronary and cerebro vascular
disease, independent of total cholesterol or
LDL levels.
11/15/2012 Biochemistry for Medics 27
Additional Risk Factors
Stressful lifestyle ("type A" personality);
Obesity - Due to
o Hypertension
o Diabetes
o Hypertriglyceridemia and
o Decreased HDL.
11/15/2012 Biochemistry for Medics 28
Pathogenesis of Atherosclerosis
The contemporary view of atherogenesis is
expressed by the response-to-injury hypothesis.
This model views atherosclerosis as a chronic
inflammatory response of the arterial wall to
endothelial injury.
Lesion progression occurs through interactions of
modified lipoproteins, monocyte-derived
macrophages, T lymphocytes, and the normal
cellular constituents of the arterial wall.
11/15/2012 Biochemistry for Medics 29
Pathogenesis of Atherosclerosis
1) Endothelial Injury
Initial triggering event in the development of
Atherosclerotic lesions
Causes ascribed to endothelial injury in include
mechanical trauma, hemodynamic
forces, immunological and chemical
mechanisms, metabolic agents like chronic
hyperlipidemia, homocystine, circulating toxins
from systemic infections, viruses, and tobacco
products.
11/15/2012 Biochemistry for Medics 30
Pathogenesis of Atherosclerosis
2. Intimal Smooth Muscle Cell Proliferation
Endothelial injury causes adherence aggregation and
platelet release reaction at the site of exposed sub
endothelial connective tissue.
Proliferation of intimal smooth muscle cells is
stimulated by various mitogens released from
platelets adherent at the site of endothelial injury.
These mitogens include platelet derived growth
factor (PDGF), fibroblast growth factor, TNF-ά.
Proliferation is also facilitated by nitric oxide and
endothelin released from endothelial cells.
11/15/2012 Biochemistry for Medics 31
Pathogenesis of Atherosclerosis
3) Role of Blood Monocytes
Though blood monocytes do not possess
receptors for normal LDL, LDL does appear in the
monocyte cytoplasm to form foam cell.
Plasma LDL on entry into the intima undergoes
oxidation.
Oxidized LDL formed in the intima is readily taken
up by scavenger receptor on the monocyte to
transform it to a lipid laden foam cell.
11/15/2012 Biochemistry for Medics 32
11/15/2012 Biochemistry for Medics 33
Pathogenesis of Atherosclerosis
Oxidized LDL stimulates the release of growth
factors, cytokines, and chemokines by
endothelial cells (EC)and macrophages that
increase monocyte recruitment into lesions.
Oxidized LDL is cytotoxic to ECs and smooth
muscle cells (SMCs )and can induce
Endothelial dysfunction.
11/15/2012 Biochemistry for Medics 34
Pathogenesis of Atherosclerosis
4) Role of Hyperlipidemia
Chronic hyperlipidemia in itself may initiate
endothelial injury and dysfunction by causing
increased permeability.
Increased serum concentration of LDL and
VLDL promote formation of foam cells, while
high serum concentration of HDL has anti-
atherogenic effect.
11/15/2012 Biochemistry for Medics 35
11/15/2012 Biochemistry for Medics 36
Progression of Atherosclerosis
Fatty Streaks- Fatty streaks are composed of lipid-filled
foam cells but are not significantly raised and thus do
not cause any disturbance in blood flow
Fatty streaks can appear in the aortas of infants
younger than 1 year and are present in virtually all
children older than 10 years, regardless of
geography, race, sex, or environment.
The relationship of fatty streaks to atherosclerotic
plaques is uncertain; although they may evolve into
precursors of plaques, not all fatty streaks are destined
to become advanced atherosclerotic lesions.
11/15/2012 Biochemistry for Medics 37
Progression of Atherosclerosis
Atherosclerotic Plaque-The key processes in
atherosclerosis are intimal thickening and lipid
accumulation Atheromatous plaques (also
called fibrous or fibro fatty plaques) impinge
on the lumen of the artery and grossly appear
white to yellow
Plaques vary from 0.3 to 1.5 cm in diameter but
can coalesce to form larger masses.
11/15/2012 Biochemistry for Medics 38
Components of Atherosclerotic
plaque
Atherosclerotic plaques have three principal
components:
Cells, including SMCs, macrophages, and T cells
ECM, including collagen, elastic fibers, and
proteoglycans and
Intracellular and extracellular lipid
These components occur in varying proportions
and configurations in different lesions.
11/15/2012 Biochemistry for Medics 39
Changes in Atherosclerotic Plaque
Atherosclerotic plaques are susceptible to the following
pathologic changes with clinical significance:
Rupture, ulceration, or erosion
Hemorrhage
Atheroembolism
Aneurysm formation
Atherosclerosis is a slowly evolving lesion usually requiring
many decades to become significant.
However, acute plaque changes
(e.g., rupture, thrombosis, or hematoma formation) can
rapidly precipitate clinical sequelae (the so-called "clinical
horizon“)
11/15/2012 Biochemistry for Medics 40
Progression of Atherosclerosis
11/15/2012 Biochemistry for Medics 41
Atherosclerosis- Symptoms
Symptomatic atherosclerotic disease most
often involves the arteries supplying the
heart, brain, kidneys, and lower extremities.
Myocardial infarction (heart attack), cerebral
infarction (stroke), aortic aneurysms, and
peripheral vascular disease (gangrene of the
legs) are the major consequences of
atherosclerosis.
11/15/2012 Biochemistry for Medics 42
Prevention of Atherosclerotic Vascular
Disease
Primary prevention aims at either delaying
atheroma formation or encouraging
regression of established lesions in persons
who have not yet suffered a serious
complication of atherosclerosis
Secondary prevention is intended to prevent
recurrence of events such as myocardial
infarction or stroke in symptomatic patients
11/15/2012 Biochemistry for Medics 43
Prevention of Atherosclerotic
Vascular Disease
Primary prevention of atherosclerosis
Cessation of cigarette smoking
Control of hypertension
Weight loss
Exercise, and lowering total and LDL blood cholesterol
levels while increasing HDL (e.g., by diet or through
statins).
Statin use may also modulate the inflammatory state of
the vascular wall.
Risk factor stratification and reduction should even
begin in childhood.
11/15/2012 Biochemistry for Medics 44
Prevention of Atherosclerotic
Vascular Disease
Secondary prevention involves use of –
Aspirin (anti-platelet agent),
Statins, and beta blockers (to limit cardiac
demand),
Surgical interventions (e.g., coronary artery
bypass surgery, carotid endarterectomy).
These can successfully reduce recurrent
myocardial or cerebral events.
11/15/2012 Biochemistry for Medics 45
Summary
Atherosclerosis is an intima-based lesion organized into
a fibrous cap and an atheromatous (gruel-like) core and
composed of SMCs, ECM, inflammatory
cells, lipids, and necrotic debris.
Atherogenesis is driven by an interplay of inflammation
and injury to vessel wall cells.
Atherosclerotic plaques accrue slowly over decades but
may acutely cause symptoms due to
rupture, thrombosis, hemorrhage, or embolization.
Risk factor recognition and reduction can reduce the
incidence and severity of atherosclerosis-related
disease.
11/15/2012 Biochemistry for Medics 46
Você também pode gostar
- Atherosclerosis, (Vascular Thickening) A Simple Guide To The Condition, Treatment And Related ConditionsNo EverandAtherosclerosis, (Vascular Thickening) A Simple Guide To The Condition, Treatment And Related ConditionsAinda não há avaliações
- Musculoskeletal Pathology Notes PDFDocumento20 páginasMusculoskeletal Pathology Notes PDFvevestephaniAinda não há avaliações
- Understand Cancer & Reduce Cancer Risk - Based On The Teachings Of Dr. Andrew Huberman: Empowering You To Safeguard Against ItNo EverandUnderstand Cancer & Reduce Cancer Risk - Based On The Teachings Of Dr. Andrew Huberman: Empowering You To Safeguard Against ItAinda não há avaliações
- Synovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandSynovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNo EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionAinda não há avaliações
- Lipid Lowering DrugsDocumento15 páginasLipid Lowering Drugsmwaithira71682Ainda não há avaliações
- Hematopoietic System PathologyDocumento78 páginasHematopoietic System PathologyNuhu SibaAinda não há avaliações
- Skin Path NotesDocumento15 páginasSkin Path NoteszeeathrAinda não há avaliações
- Electrolyte Imbalance, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandElectrolyte Imbalance, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNota: 1 de 5 estrelas1/5 (1)
- Lung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyNo EverandLung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyPhilip FarrellAinda não há avaliações
- Anaerobic Infections in HumansNo EverandAnaerobic Infections in HumansSydney FinegoldNota: 5 de 5 estrelas5/5 (1)
- Metabolic Syndrome DR - Yunus, SPPDDocumento15 páginasMetabolic Syndrome DR - Yunus, SPPDMariaEllyNobetaHutabarat100% (1)
- Hemodynamic PathologyDocumento9 páginasHemodynamic PathologyjoeAinda não há avaliações
- Arthritis, Infectious, BacterialDocumento6 páginasArthritis, Infectious, BacterialHarry IsraAinda não há avaliações
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Atlas of Clinical Vascular MedicineNo EverandAtlas of Clinical Vascular MedicineMichael R. JaffAinda não há avaliações
- Genetic Diseases of the KidneyNo EverandGenetic Diseases of the KidneyRichard P. LiftonAinda não há avaliações
- Cirrhosis Jol 2009Documento54 páginasCirrhosis Jol 2009SaaraAlleyahAlAnazi100% (1)
- Practical Gastroenterology and Hepatology Board Review ToolkitNo EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultAinda não há avaliações
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Inflamed Blood Vessels (Vasculitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandInflamed Blood Vessels (Vasculitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Current treatment concepts for primary CNS lymphomaNo EverandCurrent treatment concepts for primary CNS lymphomaAinda não há avaliações
- Inflammation and Obesity: A New and Novel Approach to Manage Obesity and its ConsequencesNo EverandInflammation and Obesity: A New and Novel Approach to Manage Obesity and its ConsequencesRaman MehrzadAinda não há avaliações
- The Ideal Multiple Myeloma Cookbook; The Superb Diet Guide To Fighting And Reversing Multiple Myeloma For A Vibrant Health With Nutritious RecipesNo EverandThe Ideal Multiple Myeloma Cookbook; The Superb Diet Guide To Fighting And Reversing Multiple Myeloma For A Vibrant Health With Nutritious RecipesAinda não há avaliações
- A Simple Guide to Acalculous Cholecystopathy, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Acalculous Cholecystopathy, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Mediterranean Diet Cookbook for Beginners: Unlock the Health Benefits of the Mediterranean Diet with Easy and Delicious Recipes for Everyday Eating!No EverandMediterranean Diet Cookbook for Beginners: Unlock the Health Benefits of the Mediterranean Diet with Easy and Delicious Recipes for Everyday Eating!Ainda não há avaliações
- Fatty Liver (1) - General PathologyDocumento22 páginasFatty Liver (1) - General PathologyDarien LiewAinda não há avaliações
- Vegetarian Nutrition 101: The Science Behind a Plant-Based Diet: The Vegetarian Kitchen Series, #3No EverandVegetarian Nutrition 101: The Science Behind a Plant-Based Diet: The Vegetarian Kitchen Series, #3Ainda não há avaliações
- Night Sweats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandNight Sweats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Carcinoid Syndrome, A Simple Guide To The Condition, Treatment And Related DiseasesNo EverandCarcinoid Syndrome, A Simple Guide To The Condition, Treatment And Related DiseasesAinda não há avaliações
- Numerical Aberrations: Meiotic NondisjunctionDocumento36 páginasNumerical Aberrations: Meiotic NondisjunctionHemanth_Prasad_2860Ainda não há avaliações
- Presented by T. V. L. Sahithi Ist Year PG Dept of PeriodonticsDocumento49 páginasPresented by T. V. L. Sahithi Ist Year PG Dept of Periodonticslakshmi sahithi natakalaAinda não há avaliações
- Immunoregulation in Health and Disease: Experimental and Clinical AspectsNo EverandImmunoregulation in Health and Disease: Experimental and Clinical AspectsMiodrag L. LukicAinda não há avaliações
- LEUKEMIA ProjectDocumento17 páginasLEUKEMIA ProjectNayak Alok Ranjan100% (1)
- Multiple Myeloma-My NotesDocumento8 páginasMultiple Myeloma-My NotesMitra Sadrameli100% (1)
- PPTDocumento61 páginasPPTRheal P EsmailAinda não há avaliações
- Parathyroid Glands: Serum PTH Levels Are Inappropriately Elevated For The LevelDocumento4 páginasParathyroid Glands: Serum PTH Levels Are Inappropriately Elevated For The LevelNada MuchAinda não há avaliações
- Pathology of LiverDocumento15 páginasPathology of Liverערין גבאריןAinda não há avaliações
- Aspirin OverdoseDocumento3 páginasAspirin OverdoseSaputra BismaAinda não há avaliações
- CHR InflammationDocumento33 páginasCHR InflammationAlnzeer6Ainda não há avaliações
- Molecular Basis of CancerDocumento6 páginasMolecular Basis of CancerguptaamitalwAinda não há avaliações
- Exam 2 Study Guide - Cellular Response To InjuryDocumento7 páginasExam 2 Study Guide - Cellular Response To InjuryWendy SuhAinda não há avaliações
- Obesity What Is Obesity?Documento9 páginasObesity What Is Obesity?Aleena KhanAinda não há avaliações
- Atherosclerosis 1Documento45 páginasAtherosclerosis 1MoonAIRAinda não há avaliações
- AtherosclerosisDocumento23 páginasAtherosclerosisPoonam soniAinda não há avaliações
- Pathology of Digestive SystemDocumento28 páginasPathology of Digestive SystemDianNursyifaRahmahAinda não há avaliações
- Management of Diabetes Emergencies''Documento85 páginasManagement of Diabetes Emergencies''Princewill SeiyefaAinda não há avaliações
- Chap1 Introduction To Nutritional AssessmentDocumento32 páginasChap1 Introduction To Nutritional AssessmentAbdi Khalaq Ali Hashi100% (1)
- Valvular Heart DiseasesDocumento29 páginasValvular Heart Diseasesbpt2Ainda não há avaliações
- Alport SyndromeDocumento49 páginasAlport SyndromemuslimAinda não há avaliações
- 4 Circulation Disorders PDFDocumento69 páginas4 Circulation Disorders PDFSetiawan SukmadjaAinda não há avaliações
- Liver Tests SlidesDocumento65 páginasLiver Tests SlidesDokter MuhammadAinda não há avaliações
- Lecture 28 - Pathology of DiabetesDocumento34 páginasLecture 28 - Pathology of Diabetesapi-3703352100% (4)
- 02 HemoglobinDocumento78 páginas02 HemoglobinpixiedustAinda não há avaliações
- Digital Marketing: 2.9 Conceptual FrameworkDocumento1 páginaDigital Marketing: 2.9 Conceptual FrameworkMuhammad Tariq RazaAinda não há avaliações
- 5 GoutDocumento2 páginas5 GoutMuhammad Tariq RazaAinda não há avaliações
- Preformulatioon Studies: Process of DissolutionDocumento5 páginasPreformulatioon Studies: Process of DissolutionMuhammad Tariq RazaAinda não há avaliações
- List of StudiesDocumento1 páginaList of StudiesMuhammad Tariq RazaAinda não há avaliações
- Drugs For Asthma and CopdDocumento1 páginaDrugs For Asthma and CopdMuhammad Tariq RazaAinda não há avaliações
- Acid Base Titrations PDFDocumento31 páginasAcid Base Titrations PDFMuhammad Tariq RazaAinda não há avaliações
- Acid Base Titrations PDFDocumento31 páginasAcid Base Titrations PDFMuhammad Tariq RazaAinda não há avaliações
- Almquist Ashir Brannstroem Guide 1.0.1 PDFDocumento343 páginasAlmquist Ashir Brannstroem Guide 1.0.1 PDFMuhammad Tariq RazaAinda não há avaliações
- Name of Disease Are FollowingDocumento1 páginaName of Disease Are FollowingMuhammad Tariq RazaAinda não há avaliações
- 18225-Article Text-81558-1-10-20170301 PDFDocumento274 páginas18225-Article Text-81558-1-10-20170301 PDFMuhammad Tariq RazaAinda não há avaliações
- Mass Spectrometry: Ev MVDocumento12 páginasMass Spectrometry: Ev MVMuhammad Tariq RazaAinda não há avaliações
- Field of TitrationDocumento1 páginaField of TitrationMuhammad Tariq RazaAinda não há avaliações
- 11 Chapter 2Documento8 páginas11 Chapter 2Muhammad Tariq RazaAinda não há avaliações
- Annex 1 Glossary of TermsDocumento6 páginasAnnex 1 Glossary of TermsMuhammad Tariq RazaAinda não há avaliações
- Aerosols: Prashant Pandey M.Pharm (Pharmaceutics)Documento43 páginasAerosols: Prashant Pandey M.Pharm (Pharmaceutics)Muhammad Tariq RazaAinda não há avaliações
- Anti EpiDocumento27 páginasAnti EpiMuhammad Tariq RazaAinda não há avaliações
- Lightning Arrester Lightningcontroller MC 125-B/Npe: Operation and Fields of ApplicationDocumento2 páginasLightning Arrester Lightningcontroller MC 125-B/Npe: Operation and Fields of ApplicationAnas BasarahAinda não há avaliações
- Common Core Content and Training Objectives For Basic AIS Training - Phase 2 - SpecialistDocumento82 páginasCommon Core Content and Training Objectives For Basic AIS Training - Phase 2 - SpecialistjlferreiraAinda não há avaliações
- Sla At&tDocumento2 páginasSla At&tCésar Lainez Lozada TorattoAinda não há avaliações
- Create A Visual DopplerDocumento1 páginaCreate A Visual DopplerRahul GandhiAinda não há avaliações
- Modular Q1 WK3-4Documento3 páginasModular Q1 WK3-4JENIFFER DE LEONAinda não há avaliações
- Unit 1 Module 3 Rep in PlantsDocumento26 páginasUnit 1 Module 3 Rep in Plantstamesh jodhanAinda não há avaliações
- SilmaDocumento12 páginasSilmanobleconsultantsAinda não há avaliações
- OT Initial Assessment (OTIA) 2022-11-15Documento2 páginasOT Initial Assessment (OTIA) 2022-11-15funtikarAinda não há avaliações
- CG Photo Editing2Documento3 páginasCG Photo Editing2Mylene55% (11)
- 4th Sept - Marathon Series Lecture 8 - General AwarenessDocumento208 páginas4th Sept - Marathon Series Lecture 8 - General AwarenessManbir ArinAinda não há avaliações
- VRPIN 01843 PsychiatricReportDrivers 1112 WEBDocumento2 páginasVRPIN 01843 PsychiatricReportDrivers 1112 WEBeverlord123Ainda não há avaliações
- Maya Deren PaperDocumento9 páginasMaya Deren PaperquietinstrumentalsAinda não há avaliações
- Toh736 - 84000 The Dharani of Parnasavari PDFDocumento24 páginasToh736 - 84000 The Dharani of Parnasavari PDFJames LeeAinda não há avaliações
- GPP Calendar of Activities 2022 23 SdoDocumento5 páginasGPP Calendar of Activities 2022 23 SdoRomel GarciaAinda não há avaliações
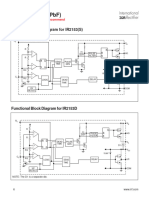
- IR2153 Parte6Documento1 páginaIR2153 Parte6FRANK NIELE DE OLIVEIRAAinda não há avaliações
- Computer System Validation - Definition and Requirements - MustRead PDFDocumento3 páginasComputer System Validation - Definition and Requirements - MustRead PDFtraining validAinda não há avaliações
- Healthy Apps Us New VarDocumento9 páginasHealthy Apps Us New VarJESUS DELGADOAinda não há avaliações
- Safety Bulletin 09 - Emergency Escape Breathing Device - Product RecallDocumento2 páginasSafety Bulletin 09 - Emergency Escape Breathing Device - Product RecallMuhammadAinda não há avaliações
- Information Systems and Supply Chain ManagementDocumento2 páginasInformation Systems and Supply Chain Managementvipinkandpal86Ainda não há avaliações
- Tuma Research ManualDocumento57 páginasTuma Research ManualKashinde Learner Centered Mandari100% (1)
- SCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Documento104 páginasSCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Athulya ThondangattilAinda não há avaliações
- Module 5 What Is Matter PDFDocumento28 páginasModule 5 What Is Matter PDFFLORA MAY VILLANUEVAAinda não há avaliações
- OM CommandCenter OI SEP09 enDocumento30 páginasOM CommandCenter OI SEP09 enGabriely MuriloAinda não há avaliações
- Genil v. Rivera DigestDocumento3 páginasGenil v. Rivera DigestCharmila SiplonAinda não há avaliações
- Engleza Referat-Pantilimonescu IonutDocumento13 páginasEngleza Referat-Pantilimonescu IonutAilenei RazvanAinda não há avaliações
- CA21159 MG 8 Digital BookletDocumento5 páginasCA21159 MG 8 Digital BookletcantaloupemusicAinda não há avaliações
- Federalist Papers 10 51 ExcerptsDocumento2 páginasFederalist Papers 10 51 Excerptsapi-292351355Ainda não há avaliações
- W.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueDocumento2 páginasW.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueParth PatelAinda não há avaliações
- Praise and Worship Songs Volume 2 PDFDocumento92 páginasPraise and Worship Songs Volume 2 PDFDaniel AnayaAinda não há avaliações
- Test Physics Chapter# 12,13,14 (2 Year) NameDocumento1 páginaTest Physics Chapter# 12,13,14 (2 Year) NameStay FocusedAinda não há avaliações