Escolar Documentos
Profissional Documentos
Cultura Documentos
Except VRE: Antibiotics
Enviado por
BenHanson0 notas0% acharam este documento útil (0 voto)
11 visualizações3 páginas1. Vancomycin is effective against all gram-positive bacteria except VRE. It has limited gram-negative coverage. It is not as bactericidal as beta-lactams and requires monitoring of trough levels during prolonged therapy.
2. Penicillins such as penicillin, oxacillin, ampicillin are effective against various gram-positive cocci but have more limited gram-negative coverage. Combinations with beta-lactamase inhibitors like sulbactam or clavulanic acid provide broader gram-positive and gram-negative coverage. Piperacillin-tazobactam has broad coverage similar to carbapenems.
3. Carbapen
Descrição original:
aa
Título original
aa
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documento1. Vancomycin is effective against all gram-positive bacteria except VRE. It has limited gram-negative coverage. It is not as bactericidal as beta-lactams and requires monitoring of trough levels during prolonged therapy.
2. Penicillins such as penicillin, oxacillin, ampicillin are effective against various gram-positive cocci but have more limited gram-negative coverage. Combinations with beta-lactamase inhibitors like sulbactam or clavulanic acid provide broader gram-positive and gram-negative coverage. Piperacillin-tazobactam has broad coverage similar to carbapenems.
3. Carbapen
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
11 visualizações3 páginasExcept VRE: Antibiotics
Enviado por
BenHanson1. Vancomycin is effective against all gram-positive bacteria except VRE. It has limited gram-negative coverage. It is not as bactericidal as beta-lactams and requires monitoring of trough levels during prolonged therapy.
2. Penicillins such as penicillin, oxacillin, ampicillin are effective against various gram-positive cocci but have more limited gram-negative coverage. Combinations with beta-lactamase inhibitors like sulbactam or clavulanic acid provide broader gram-positive and gram-negative coverage. Piperacillin-tazobactam has broad coverage similar to carbapenems.
3. Carbapen
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 3
Antibiotics
1. Vancomycin (IV only)
a. CLASS: Glycopeptides
b. Coverage
i. ALL GRAM POSITIVES!!! – except VRE
1. Staphs and Vanc SENSITIVE Enterococci
2. Streps (including Strep. pneumo)
3. Gram positive rods (GPRs)
a. NOTE: C. dif is the ONLY time PO Vanc is used!
ii. NO Gram negative coverage
c. NOT as bactericidal as the beta-lactams (womp, womp)
d. If prolonged therapy – monitor trough level (measure before 4th dose)
i. Serious infections – trough goal is 15-20
ii. Continuous infusion – trough goal is 20-30
e. S/E:
i. Red Man Syndrome – TRUE allergic rxn is not very common
ii. Nephrotoxicity – primarily occurs when used w/ other nephrotoxins
2. PCNs
a. PCN G (IV) or PCN VK (PO)
i. Reliably kills Strep (EXCEPT SOME Strep. pneumo!)
ii. Neisseria meningitidis (meningitis), Treponema pallidum (syphilis)
iii. Resistance will NOT develop DURING therapy
iv. Therefore, if the organism is sensitive to PCN G, USE IT!!!
1. CHEAP and ‘CIDAL!
b. Oxacillin/Nafcillin (IV) or Dicloxacillin (PO)
i. Ox/Naf achieve higher serum concentration than Diclox
ii. NARROW SPECTRUM – destroys Staph and Strep
1. MISSES: MRSA, GRAM NEGS!
iii. MOST ‘cidal agent against SUSCEPTIBLE Staph. aureus (MSSA)
iv. DOC for endocarditis, osteomyelitis (if these are caused by MSSA)
c. Ampicillin (IV) or Amoxicillin (PO)
i. Susceptibile to beta-lactamase :/ womp womp!
ii. BROADER SPECTRUM than PCN G and Oxacillin
1. Covers CERTAIN Gram negs
2. Misses Staph 95% of the time
a. NOTE: If Staph is RES to PCN, then IT IS RES to Amp/Amox!
3. Use for: Otitis media, bronchitis, sinusitis, UTI (uncomplicated)
4. DOC for Enterococcus (if it’s sensitive)
5. Do NOT use empirically for COPD exacerbation
d. Unasyn AKA Amp/Sulbactam (IV) and Augmentin AKA Amox/Clavulanic Acid (PO)
i. BROADER SPECTRUM due to beta-lactamase INHIBITOR (Sul and Clav)
1. Covers MANY Gram pos, Gram negs, AND ANAEROBES!
2. MISSES: MRSA, Pseudomonas (GNR), Atypicals, and RES Gram negs :/
e. Piperacillin/Tazobactam AKA Zosyn (IV ONLY!)
i. About AS BROAD AS YOU CAN GET!
ii. Covers: Gram pos, Gram neg (INCLUDING PSEUDOMONAS), Anaerobes
1. AND Enterococcus (IF susceptible to Amp)
iii. MISSES: MRSA, VRE, Atypicals and ESBL Gram negs
1. NOTE: ESBL=extended spectrum beta-lactamases
3. Carbapenems (IV ONLY!): some cross rxn w/ PCN allergic pts (avoid if possible!)
a. Meropenem/Imipenem
i. Almost same coverage as Zosyn, but a little LESS resistance
ii. BUT tends to PROMOTE RESISTANCE so use Zosyn if possible
iii. “Ace in the hole” abx – save it until needed!
iv. Imipenem can cause seizures! (LOWERS THE THRESHOLD! STEP 1 QUESTION!!!)
4. Aztreonam (IV ONLY!)
a. Monobactam, expensive $$$!
b. OK to use in PCN allergic pts (this is its ONLY use)
i. NOTE: UNLESS allergy is to Ceftazidime (then can’t use)
c. Covers: ONLY Gram negatives (INCLUDING PSEUDOMONAS)
i. So basically only use this when you need to cover Pseudo in a PCN allg pt!
5. Cephalosporins
a. 1st gen: Cefazolin (Ancef) and Cephalexin (Keflex)
i. Similar to Ox/Diclox
1. REMEMBER??? NARROW SPECTRUM – destroys Staph and Strep
a. MISSES: MRSA, GRAM NEGS!
2. MOST ‘cidal agent against SUSCEPTIBLE Staph. aureus (MSSA)
3. DOC for endocarditis, osteomyelitis (if these are caused by MSSA)
ii. Cefazolin (Ancef)=mainly a surgical prophylactic abx
b. 2nd gen:
i. Cefuroxime: similar to Amox
1. REMEMBER??? BROADER SPECTRUM than PCN G and Oxacillin
a. Covers CERTAIN Gram negs
b. Misses Staph 95% of the time
i. NOTE: If Staph is RES to PCN, then IT IS RES to Amp/Amox!
c. Use for: Otitis media, bronchitis, sinusitis, UTI (uncomplicated)
d. DOC for Enterococcus (if it’s sensitive)
ii. Cefotetan and Cefoxitin: also kills anaerobes (surg ppx w/ abd surgs)
c. 3rd gen:
i. Cefotaxime and Ceftriaxone AKA Rocephin (IV)
1. Covers: Gram pos (Strep. pneumo), more Gram neg than 1st and 2nd gens
2. Does NOT cover: MRSA, Enterococcus, Pseudomonas, Anaerobes, or Atyps
3. Penetrate the BBB!!!
4. Use for: Pna (in combo w/ Azithro), pyelo, gonorrhea, and meningitis
ii. Ceftazidime: KILLS PSEUDOMONAS (but use Cefepime due to resistance)
d. 4th gen: Here’s your Cefepime!!! (IV)
i. VERY BROAD SPECTRUM COVERAGE!!!
1. Covers: Gram pos, Gram neg, PSEUDOMONAS
2. MISSES: Enterococcus, Anaerobes, Atypicals
3. Use for: NEUTROPENIC FEVER!!! Gram negs, and PSEUDOMONAS!!!
e. 5 gen: CEFTAROLINE (IV) AKA ONLY beta-lactam that covers MRSA!!!
th
i. Use for: cellulitis and CAP (MRSA community acquired pneumonia)
6. Fluoroquinolones (IV and PO)
a. ALWAYS try to use PO – near 100% bioavailability
b. NOT GOOD FOR: Staph. aureus
c. Moxifloxacin
i. Excellent for Strep. pneumo, most Gram negs, and Atypicals
ii. Just OK for other Gram pos
iii. MISSES: Pseudomonas, MRSA, anaerobes
iv. Does NOT penetrate URINE well so DO NOT use for UTI or pyelo!!!
d. Levofloxacin AKA Levaquin
i. Similar to Moxi except THIS ONE COVERS PSEUDOMONAS at 750mg daily!
e. Ciprofloxacin
i. Not as good for S. pneumo, Gram pos
ii. Best FQ for Pseudomonas, Gram neg, and URINE INFXNS!!!
7. Macrolides
a. Azithromycin (PO/IV)
i. Very long half life – stays therapeutic for up to 7 days after tx stopped (Zpack)
ii. Covers: S. pneumo, some Gram negs, and Atypicals
iii. Use for: bronchitis, otitis media, urethritis, and pna (w/ 3rd gen cefs)
b. Clarithromycin – similar, just BID
8. Clindamycin (PO/IV)
a. Covers: OK for Anaerobes and Gram pos (Staph, Strep)
b. MISSES: Gram negs
c. Use for: Aspiration pna, abdominal infxns
d. INTERESTING FACT: may decrease toxin production in severe Staph/Strep infections
(cellulitis, and particularly Fournier’s gangrene)
9. Aminoglycosides (Gentamicin, Tobramycin, Amikacin)
a. Covers: Gram negs, PSEUDOMONAS; and Staph and Enterococcus when used w/ PCN
(synergy)
i. ***Tobra is MOST active against Pseudomonas!***
b. MISSES: Gram pos and anaerobes
c. S/E: ototoxicity and nephrotoxicity (reduced w/ once daily dosing)
10. Bactrim (TMP/SMX)
a.
Você também pode gostar
- Infectious Disease - Antibiotic Ladder PDFDocumento2 páginasInfectious Disease - Antibiotic Ladder PDFVaishali PrasharAinda não há avaliações
- Pance Prep Pearls AntibioticsDocumento14 páginasPance Prep Pearls Antibioticskat100% (4)
- Adult Infectious Disease Bulletpoints HandbookNo EverandAdult Infectious Disease Bulletpoints HandbookNota: 4.5 de 5 estrelas4.5/5 (9)
- Adhesive Capsulitis Presentation May 2009Documento29 páginasAdhesive Capsulitis Presentation May 2009cm4100% (1)
- Antiobitic Infection TX ChartDocumento8 páginasAntiobitic Infection TX ChartTLAinda não há avaliações
- 90+% of S. Aureus Are Resistant To PCN: Clinical PearlsDocumento6 páginas90+% of S. Aureus Are Resistant To PCN: Clinical PearlsJessica WoeppelAinda não há avaliações
- Antibiotics - Who Kills WhatDocumento1 páginaAntibiotics - Who Kills WhatBenHansonAinda não há avaliações
- Print Antibiotics ReviewDocumento6 páginasPrint Antibiotics ReviewtiuwangAinda não há avaliações
- Antibiotic Class by CoverageDocumento3 páginasAntibiotic Class by Coverageayy1Ainda não há avaliações
- Antibiotic Management Chalk Talk NotesDocumento3 páginasAntibiotic Management Chalk Talk NotesMarl KarxAinda não há avaliações
- Pharmacology II 352 CDocumento15 páginasPharmacology II 352 CMustafa SaßerAinda não há avaliações
- Veterinary Antimicrobial DrugsDocumento5 páginasVeterinary Antimicrobial DrugsLaureece Salm ApduhanAinda não há avaliações
- O DOC For Syphillis (Benzathine Penicillin), o DOC in Strep Infections, Especially To Prevent Rheumatic Fever o DOC For Susceptible PneumococciDocumento5 páginasO DOC For Syphillis (Benzathine Penicillin), o DOC in Strep Infections, Especially To Prevent Rheumatic Fever o DOC For Susceptible PneumococciIndu BhavanaAinda não há avaliações
- Penicillins - KatzungDocumento6 páginasPenicillins - KatzungKarl CAinda não há avaliações
- Antibioticsforyear3medics PDFDocumento13 páginasAntibioticsforyear3medics PDFShonaMalhanAinda não há avaliações
- Antibacterial DR Mostafa Alfishawy AntibioticDocumento64 páginasAntibacterial DR Mostafa Alfishawy Antibioticramzi MohamedAinda não há avaliações
- Introduction To AntibioticsDocumento6 páginasIntroduction To AntibioticsMuslimAinda não há avaliações
- HCC Exam 4Documento20 páginasHCC Exam 4Sheri BarlingAinda não há avaliações
- The Beta-Lactam Antibiotics: Cell Wall Active AgentsDocumento32 páginasThe Beta-Lactam Antibiotics: Cell Wall Active Agentsjayaprakashr72616Ainda não há avaliações
- Opportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaDocumento4 páginasOpportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaPinay YaunAinda não há avaliações
- Antibiotic TableDocumento1 páginaAntibiotic Tablebob someoneAinda não há avaliações
- Case 1: Toxacara CatiDocumento4 páginasCase 1: Toxacara Catiseo82087Ainda não há avaliações
- Antimicrobial PANCE ReviewDocumento40 páginasAntimicrobial PANCE ReviewFlora LawrenceAinda não há avaliações
- Topic - Neutropenic Fever OutlineDocumento5 páginasTopic - Neutropenic Fever Outlineapi-549451092Ainda não há avaliações
- Sketchy Pharm - AntimicrobialsDocumento32 páginasSketchy Pharm - AntimicrobialsDennis Torres SchelamaussAinda não há avaliações
- 1a Antiinfective DrugsDocumento4 páginas1a Antiinfective DrugsMaria Donabella OngueAinda não há avaliações
- Cephalosporins Quick ReviewDocumento19 páginasCephalosporins Quick ReviewErinson Custodio PlasenciaAinda não há avaliações
- Tropical Medicine Lecture Edited-1Documento96 páginasTropical Medicine Lecture Edited-1inspiredwriter617Ainda não há avaliações
- Antibiotic Summary - DraftDocumento10 páginasAntibiotic Summary - DraftStrept Pneumonia100% (1)
- Supporting Document of How To Choose Empirical Antibiotics in ICU Video LectureDocumento7 páginasSupporting Document of How To Choose Empirical Antibiotics in ICU Video LectureNeha AgrawalAinda não há avaliações
- Clinical Pharmacology - Rationale Behind Antibiotics PrescriptionDocumento12 páginasClinical Pharmacology - Rationale Behind Antibiotics PrescriptionhalesAinda não há avaliações
- Antibiotics: Lecture 6: Antibiotics For Anaerobic InfectionsDocumento12 páginasAntibiotics: Lecture 6: Antibiotics For Anaerobic InfectionsMuath AlqarniAinda não há avaliações
- InfectionDocumento96 páginasInfectionBassem Georguos LabibAinda não há avaliações
- BDS and NUR Two Antiprotozoal MarchDocumento68 páginasBDS and NUR Two Antiprotozoal MarchElvis KiprotichAinda não há avaliações
- Microbiology Summary DocumentDocumento7 páginasMicrobiology Summary DocumentKAinda não há avaliações
- Pharm: Antibacteria/Antiviral/AntifungalDocumento19 páginasPharm: Antibacteria/Antiviral/AntifungalNathan BarrerasAinda não há avaliações
- 2011 PK-PD AntibiotikDocumento88 páginas2011 PK-PD AntibiotikUniatimelindaAinda não há avaliações
- Antibacterials For Respiratory Tract Infections: Cecilia C. Maramba-Lazarte, MD, MscidDocumento29 páginasAntibacterials For Respiratory Tract Infections: Cecilia C. Maramba-Lazarte, MD, MscidCecile Maramba-LazarteAinda não há avaliações
- Infectious Diseases of The Dog and CatDocumento52 páginasInfectious Diseases of The Dog and CatHikmat UllahAinda não há avaliações
- Bacteriology SummaryDocumento35 páginasBacteriology SummarykevinAinda não há avaliações
- Antibiotics: Penicillium-Terrestrial Mold Cephalosporium - Marine Mold Bacillus - Bacteria Streptomyces - BacteriaDocumento9 páginasAntibiotics: Penicillium-Terrestrial Mold Cephalosporium - Marine Mold Bacillus - Bacteria Streptomyces - BacteriavexicaAinda não há avaliações
- Classification of Clinically Significant Bacteria by GenusDocumento2 páginasClassification of Clinically Significant Bacteria by GenusSEAN BUIAinda não há avaliações
- Classification of Clinically Significant Bacteria by GenusDocumento2 páginasClassification of Clinically Significant Bacteria by GenusBrhmcmicroAinda não há avaliações
- Bacteria: Gram + CoverDocumento2 páginasBacteria: Gram + CoverPhil St Flour NPMT Central CoastAinda não há avaliações
- 4 IGP Basics of Antimicrobial TherapyDocumento11 páginas4 IGP Basics of Antimicrobial TherapyTin NatividadAinda não há avaliações
- DR Lie Khie Chen - Management of MDR Infection in Sepsis Jade 2016Documento33 páginasDR Lie Khie Chen - Management of MDR Infection in Sepsis Jade 2016Astria PermanaAinda não há avaliações
- Common Antibiotic UseDocumento40 páginasCommon Antibiotic UseKittiphat ChaikuntaAinda não há avaliações
- Rangkuman UkaiDocumento15 páginasRangkuman Ukaimaxifarma2023Ainda não há avaliações
- USMLE Step 3 Lecture Notes 2017-2018Documento74 páginasUSMLE Step 3 Lecture Notes 2017-2018kaelenAinda não há avaliações
- 7fa8e6ac-47db-4f0f-90f3-bb6e1ece863cDocumento18 páginas7fa8e6ac-47db-4f0f-90f3-bb6e1ece863cSatendra SrivastavaAinda não há avaliações
- Rapid Review AntibioticsDocumento82 páginasRapid Review AntibioticsObaroAinda não há avaliações
- Group I: Penicillin G (Benzylpenicillin), Penicillin V (Phenoxymethylpenicillin)Documento16 páginasGroup I: Penicillin G (Benzylpenicillin), Penicillin V (Phenoxymethylpenicillin)jhk451Ainda não há avaliações
- AntibacterialsDocumento8 páginasAntibacterialslisalynnleeAinda não há avaliações
- Parasites and Parasitism (Parasitology)Documento3 páginasParasites and Parasitism (Parasitology)Joraine Nichole Roquero VillajuanAinda não há avaliações
- Antimicrobials IDocumento40 páginasAntimicrobials IclarkfunAinda não há avaliações
- Antibiotics: Faculty of Dentistry 22 September 2014Documento61 páginasAntibiotics: Faculty of Dentistry 22 September 2014gamalsolimanAinda não há avaliações
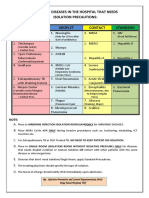
- Diseases That Needs Isolation PrecautionsDocumento1 páginaDiseases That Needs Isolation Precautionsjerimiah_manzonAinda não há avaliações
- DermatologyDocumento29 páginasDermatologykeyur patelAinda não há avaliações
- 2.fahad Khaliq.... Febrile Neutro - pptx-1Documento38 páginas2.fahad Khaliq.... Febrile Neutro - pptx-1dr FAHADKHALIQSIALAinda não há avaliações
- Wound CX: NGTD Day 1, Upon D/C Long Term Abx IV Vs PO - Given History of Recurrently UTI, Will Get CT Abd/pelvis To R/o Underlying PathologyDocumento2 páginasWound CX: NGTD Day 1, Upon D/C Long Term Abx IV Vs PO - Given History of Recurrently UTI, Will Get CT Abd/pelvis To R/o Underlying PathologyBenHansonAinda não há avaliações
- Usmle Step 1 240, Step 2 244 Comlex Level 1 604, Level 2 618 Class Rank Top Quartile Ecs/Research Were WeakDocumento5 páginasUsmle Step 1 240, Step 2 244 Comlex Level 1 604, Level 2 618 Class Rank Top Quartile Ecs/Research Were WeakBenHansonAinda não há avaliações
- Visiting Student Application Service (VSAS)Documento10 páginasVisiting Student Application Service (VSAS)BenHansonAinda não há avaliações
- Cardiology - ACLS Easy PDFDocumento1 páginaCardiology - ACLS Easy PDFrolpf garriAinda não há avaliações
- USMLE Step 1 Study Plan 2Documento3 páginasUSMLE Step 1 Study Plan 2BenHansonAinda não há avaliações
- MATUCOL 3 Meses Seguridad Efectividad de Metodos de InduccionDocumento11 páginasMATUCOL 3 Meses Seguridad Efectividad de Metodos de InduccionMitsury Jacqueline Flores C.Ainda não há avaliações
- Burns SeminarDocumento66 páginasBurns SeminarPratibha Thakur100% (1)
- Lesson 4Documento6 páginasLesson 4doldol ocampoAinda não há avaliações
- Drug StudyDocumento3 páginasDrug StudySherlyn Delos ReyesAinda não há avaliações
- Urinary Tract Infection (UTI) : Pharmacotherapeutics II YrDocumento20 páginasUrinary Tract Infection (UTI) : Pharmacotherapeutics II YrpawannnnAinda não há avaliações
- Muscular System FunctionDocumento2 páginasMuscular System FunctionLachlan PalmerAinda não há avaliações
- Chapter 46 Antianginal AgentsDocumento14 páginasChapter 46 Antianginal AgentsJewel SantosAinda não há avaliações
- Grade 6: The Heart and Circulatory SystemDocumento18 páginasGrade 6: The Heart and Circulatory SystemEstanislao Villanueva ElemAinda não há avaliações
- Open Heart Surgery CaabgDocumento6 páginasOpen Heart Surgery CaabgGopi KrishnanAinda não há avaliações
- Desvenlafaxine Venlafaxine: StructureDocumento6 páginasDesvenlafaxine Venlafaxine: StructureAndrew PanickerAinda não há avaliações
- HPV Template MasterlistDocumento1 páginaHPV Template Masterlistmarialovella.gonzagaAinda não há avaliações
- 10.master Rotation Plan M. Sc. Nursing 1st YearDocumento4 páginas10.master Rotation Plan M. Sc. Nursing 1st YearNaresh JeengarAinda não há avaliações
- Gastrointestinal System Practice ExamDocumento53 páginasGastrointestinal System Practice Examcarina.pldtAinda não há avaliações
- J1-T5 Anemia FerropénicaDocumento12 páginasJ1-T5 Anemia FerropénicaGoblin HunterAinda não há avaliações
- Physiotherapy Management of TMJ PainDocumento4 páginasPhysiotherapy Management of TMJ Painakheel ahammed100% (1)
- Metastases Bone DiseaseDocumento59 páginasMetastases Bone Diseasemuhammad rustamAinda não há avaliações
- 9c5ff54e-92aa-4393-8350-218e91c128d2Documento6 páginas9c5ff54e-92aa-4393-8350-218e91c128d2Zarbakht AliAinda não há avaliações
- Tarife AnalizeDocumento1 páginaTarife AnalizeVincze Alina ClaudiaAinda não há avaliações
- Ischemic Optic NeuropathyDocumento10 páginasIschemic Optic NeuropathyScerbatiuc CristinaAinda não há avaliações
- User Guide For The Participant Use Data File: American College of Surgeons National Surgical Quality Improvement ProgramDocumento40 páginasUser Guide For The Participant Use Data File: American College of Surgeons National Surgical Quality Improvement Programbobobobo12341212Ainda não há avaliações
- ADAT Practice TestDocumento54 páginasADAT Practice TestRyan GrossAinda não há avaliações
- Case PresentationDocumento10 páginasCase Presentationapi-402129690Ainda não há avaliações
- Rachel Costa ResumeDocumento2 páginasRachel Costa ResumeracrnAinda não há avaliações
- Cir 0000000000000549Documento120 páginasCir 0000000000000549MSAinda não há avaliações
- Medstar ObGyn 2nd EditionDocumento570 páginasMedstar ObGyn 2nd EditionMerahit Abera100% (2)
- Respiratory MCQs LJDocumento7 páginasRespiratory MCQs LJfjghAinda não há avaliações
- Kanker PayudaraDocumento2 páginasKanker PayudaraIndrawati SyarifAinda não há avaliações
- AAST Renal Injury ScaleDocumento11 páginasAAST Renal Injury ScaleyuenkeithAinda não há avaliações
- GGT enDocumento2 páginasGGT enKaoueche OmarAinda não há avaliações