Escolar Documentos
Profissional Documentos
Cultura Documentos
Cistostomia Artigo
Enviado por
Diego FélixTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cistostomia Artigo
Enviado por
Diego FélixDireitos autorais:
Formatos disponíveis
The n e w e ng l a n d j o u r na l of m e dic i n e
videos in clinical medicine
summary points
Suprapubic Bladder Aspiration
Jennifer R. Marin, M.D., Nader Shaikh, M.D., Steven G. Docimo, M.D.,
Robert W. Hickey, M.D., and Alejandro Hoberman, M.D.
The following text summarizes information provided in the video.
Overview
This summary reviews suprapubic bladder aspiration in children, both with and From the Departments of Pediatrics
without the use of ultrasound guidance. Familiarity with this procedure is impor- (J.R.M., N.S., S.G.D., R.W.H., A.H.) and
Emergency Medicine (J.R.M.), University
tant when neither a clean-catch urine sample nor a specimen from a urethral cath- of Pittsburgh, Pittsburgh. Address re-
eter can be obtained. print requests to Dr. Marin at Children’s
Hospital of Pittsburgh, 4401 Penn Ave.,
AOB, Suite 2400, Pittsburgh, PA 15224,
Indications or at jennifer.marin@chp.edu.
Suprapubic bladder aspiration is performed to obtain a sterile urine sample from
N Engl J Med 2014;371:e13.
children when the urethra cannot be adequately visualized, such as in girls with DOI: 10.1056/NEJMvcm1209888
labial adhesions or labial edema, in uncircumcised boys with unretractable fore- Copyright © 2014 Massachusetts Medical Society.
skins, in children with conditions such as severe, protracted diarrhea that may
make it difficult to obtain a sterile specimen, in children in whom multiple unsuc-
cessful attempts have been made to obtain urine through urethral catheterization,
and in children with a history of urethral or introital surgery in whom it may be
difficult to perform catheterization.
Before the procedure is performed, its purpose and its risks and benefits should
be explained to a family member or guardian, and that person should be given the
opportunity to ask questions. Some institutions may require written documenta-
tion of informed consent.
Contraindications
Contraindications to suprapubic bladder aspiration include major genitourinary
abnormalities, infections of the abdominal wall, clinically significant bleeding dis-
orders, and massive organomegaly.
Equipment
To perform suprapubic bladder aspiration, you will need topical anesthetic cream
and an adhesive bandage, 1% lidocaine (with or without epinephrine), a 25-gauge
5/8-in. or 1-in. needle, a 22-gauge or 23-gauge 1.5-in. needle, two sterile 5-ml sy-
ringes, sterile gloves, a sterile drape or towel, antiseptic solution with sterile gauze,
a sterile specimen container, and a bandage.
Analgesia
Apply the topical anesthetic to the skin 1 to 2 cm superior to the pubic symphysis
and cover with an adhesive bandage. The anesthetic will be most effective if applied
approximately 20 to 30 minutes before the procedure begins.
If you are performing the procedure in an infant, dip a pacifier into an oral
sucrose solution and allow the infant to suck the pacifier during the procedure to
decrease discomfort. Alternatively, the care provider can dip a finger into the solu-
n engl j med 371;10 nejm.org september 4, 2014 e13(1)
The New England Journal of Medicine
Downloaded from nejm.org at UNIFOR on June 11, 2015. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
tion. In older children, who have thicker abdominal walls, use a subcutaneous
injection of lidocaine.
Anatomy
To perform the procedure safely and successfully, you must have a clear under-
standing of pelvic anatomy. The bladder lies posterior to the pubic symphysis and
anterior to the uterus in girls and anterior to the rectum in boys.
Procedure
The procedure can be performed with or without ultrasound guidance. Both ap-
proaches are described.
Without Ultrasound Guidance
Place the child on his or her back, in the frog-leg position. You will need one as-
sistant positioned at the child’s head to maintain control of the arms and a second
assistant to restrain the legs.
Wash your hands with soap and water, and don sterile gloves. Cleanse the
child’s skin from the umbilicus to the pubic symphysis, using an antiseptic solu-
tion. You may choose to leave the diaper on during the procedure to capture
spontaneous urination. Drape the area to avoid contamination.
Next, infiltrate the subcutaneous tissues approximately 1 to 2 cm above the
pubic symphysis with 1 ml of lidocaine. Use the 1.5-in. needle to perform bladder
Figure 1. First Attempt at Bladder aspiration. The needle should be placed at an angle that is perpendicular to the
Aspiration.
ICM AUTHOR Marin RETAKE 1st abdominal wall, which means the needle will be approximately 10 to 20 degrees
REG F FIGURE 1 2nd
In the
CASE first
TITLE
attempt at bladder aspira-
Revised
3rd from true vertical (Fig. 1).
tion,Enonthe needle should
EMail Line be 4-C placed at
SIZE Penetrate the skin and immediately apply negative pressure to the syringe as
ARTIST: mst H/T H/T
an angle that is perpendicular to the
16p6
FILL Combo
you advance the needle through the skin until urine is visible. You may feel a
abdominal wall,
AUTHOR, which means the
PLEASE NOTE:
Figure has been redrawn and type has been reset.
needle will bePlease approximately
check carefully. 10 to change in resistance as the needle penetrates the bladder wall.
20 degrees
JOB: 37110 from true vertical. ISSUE: 9-4-14 If no urine is obtained after the initial attempt, withdraw the needle to the edge
of the needle tip, but do not remove the needle from the skin. Then change the
angle of needle entry so that the needle tip is more caudad. The needle should be
oriented in a true vertical position (Fig. 2). Once you have collected sufficient urine
in the syringe, immediately transfer the urine to a sterile container.
With Ultrasound Guidance
Ultrasonography is increasingly used for diagnostic and procedural guidance. The
use of ultrasonography to assess bladder volume and to guide aspiration can in-
crease the likelihood that the procedure will be successful.1-3
The most common reason for failing to obtain urine with suprapubic bladder
Figure 2. Second Attempt at Bladder aspiration is a lack of sufficient urine in the bladder, which may be the case if the
Aspiration.
ICM AUTHOR Marin RETAKE 1st child has urinated within the past hour or if the child is dehydrated. Performing
REG F FIGURE 2
If no
CASEurine
TITLEis obtained after the
2nd
initial
3rd ultrasonographic evaluation of the bladder to ensure an adequate urine volume
Revised
attempt,
Enon
withdraw the
ARTIST: mst
Line needle
H/T
4-C
H/T
toSIZEthe before attempting the procedure can increase the likelihood that urine will be
edgeFILLof the needle Combo tip, but do 16p6 not obtained. A high-frequency (5- to 10-MHz) linear-array transducer is ideal for
remove the needle from the skin. Then
AUTHOR, PLEASE NOTE:
Figure has been redrawn and type has been reset. imaging the superficial pediatric bladder. Obtain a transverse view and measure
change the angle of needle entry so
Please check carefully.
thatJOB:
the 37110
needle tip is more ISSUE:caudad.
9-4-14
the size of the bladder. Measurements of at least 2 cm in each dimension will
The needle should be oriented in a provide sufficient volume for analysis.2
true vertical position. If there is an inadequate amount of urine in the bladder, provide the patient
with oral or intravenous hydration, as appropriate to the patient’s clinical state,
and try using ultrasound guidance to locate the bladder 30 minutes afterward. The
amount of fluid you administer will depend on the size of the patient, the level of
dehydration, if present, and whether there is any known cardiac or renal disease.
e13(2) n engl j med 371;10 nejm.org september 4, 2014
The New England Journal of Medicine
Downloaded from nejm.org at UNIFOR on June 11, 2015. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Supr apubic Bladder Aspir ation
Once there is sufficient urine in the bladder, you may begin the procedure.
Prepare a small amount of sterile gel and put on sterile gloves. Cleanse the skin
with antiseptic solution, and place a sterile cover on the ultrasound probe.
Locate the bladder again. If you are not using ultrasonography for real-time
Needle
guidance of bladder aspiration, use a sterile pen to mark the skin site where the
bladder is best visualized and proceed with bladder aspiration (as described above).
When performing real-time ultrasound guidance, leave the probe on the abdo- Patient’s
right
Patient’s
left
men and insert the needle midline and just inferior to the edge of the probe at an
angle that is perpendicular to the abdominal wall. You should see the needle tip
clearly on the ultrasound screen as it advances through the skin and into the an-
terior wall of the bladder. Once you see the needle in the bladder, aspirate the urine
(Fig. 3). The procedure can also be performed with the transducer positioned along
the long axis of the needle, such that the length of the needle is visualized (Fig. 4). Figure 3. Transverse Sonographic
View through the Bladder.
Complications In this view, the patient’s right side
Complications of suprapubic bladder aspiration are rare. They include gross hema- can be seen on the left side of the
screen, and the patient’s left side
turia, cellulitis of the abdominal wall, and perforation of the bowel, which may
appears on the right side of the screen.
occur when a loop of bowel overlies the bladder. The use of ultrasound guidance Once the needle is visualized in the
decreases the likelihood of bowel perforation. bladder, the urine can be aspirated.
If you suspect bowel perforation, withdraw the needle and reattempt the proce-
dure with a fresh needle and syringe. Intestinal penetration is usually not clini-
cally significant and generally requires no follow-up.
Summary
Knowing how to perform suprapubic bladder aspiration is important for clinicians
who care for children who are not toilet-trained or who are unable to provide a Needle
clean-catch urine specimen. When a sterile urine specimen from a patient is re-
quired and the performance of urethral catheterization is difficult or unfeasible, Patient’s
head
suprapubic bladder aspiration is the next preferred method. Patient’s
feet
Dr. Hoberman reports receiving fees for providing expert testimony in a neonatal hypoglycemia case. No
other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
Figure 4. Longitudinal Sonographic
View through the Bladder.
In this view, the left side of the screen
is oriented to the patient’s head and
the right side of the screen is oriented
to the patient’s feet.
References
1. Chen L, Hsiao AL, Moore CL, Dziura
JD, Santucci KA. Utility of bedside blad-
der ultrasound before urethral catheter-
ization in young children. Pediatrics
2005;115:108-11.
2. Gochman RF, Karasic RB, Heller MB.
Use of portable ultrasound to assist urine
collection by suprapubic aspiration. Ann
Emerg Med 1991;20:631-5.
3. Witt M, Baumann BM, McCans K.
Bladder ultrasound increases catheteriza-
tion success in pediatric patients. Acad
Emerg Med 2005;12:371-4.
Copyright © 2014 Massachusetts Medical Society.
n engl j med 371;10 nejm.org september 4, 2014 e13(3)
The New England Journal of Medicine
Downloaded from nejm.org at UNIFOR on June 11, 2015. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Você também pode gostar
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Electrostimulatoare Denas MsDocumento43 páginasElectrostimulatoare Denas MsDanOlteanuAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Acid Base WorkshopDocumento71 páginasAcid Base WorkshopLSU Nephrology Transplant Dialysis AccessAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- ECAM2015 324369 PDFDocumento6 páginasECAM2015 324369 PDFLuiz Otavio CostaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- False Memories in Therapy and Hypnosis Before 1980Documento17 páginasFalse Memories in Therapy and Hypnosis Before 1980inloesAinda não há avaliações
- Movie ReviewDocumento5 páginasMovie ReviewVangeline MandiitAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Questions DRDocumento8 páginasQuestions DRRosalie Valdez EspirituAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Worksheet For Nervous Systems-KeyDocumento5 páginasWorksheet For Nervous Systems-KeyNazarine Torres100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Diabetic FootDocumento47 páginasDiabetic FootadhikarisamirAinda não há avaliações
- Laboratory Test Report: Test Name Result Biological Reference Interval Fasting Plasma Glucose: 102Documento3 páginasLaboratory Test Report: Test Name Result Biological Reference Interval Fasting Plasma Glucose: 102Ramesh KumarAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- PR Ke-2Documento2 páginasPR Ke-2Maulia IsnainiAinda não há avaliações
- Dental AssistantDocumento2 páginasDental Assistantapi-78993102Ainda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Research Sa Chem Trabaho'a Na!Documento14 páginasResearch Sa Chem Trabaho'a Na!NoellhaJeanetteGabeLiwagonAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Chakra Dancing Teacher Prospectus 2011 PDFDocumento3 páginasChakra Dancing Teacher Prospectus 2011 PDFGavin ElderAinda não há avaliações
- Guía Clínica HTA 2011Documento310 páginasGuía Clínica HTA 2011marcelagarciavAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Askep CKD Bhs InggrisDocumento15 páginasAskep CKD Bhs InggrisFitri MulyaAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Afifa Humaira's Career PlanDocumento1 páginaAfifa Humaira's Career Planca2afifa13Ainda não há avaliações
- Republic of Kenya: Application For Registration of A Health InstitutionDocumento13 páginasRepublic of Kenya: Application For Registration of A Health InstitutionianAinda não há avaliações
- Bowen Family TheoryDocumento320 páginasBowen Family Theorytonifieraru100% (14)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Grand Halad Sa Kapamilya: List of ServicesDocumento2 páginasGrand Halad Sa Kapamilya: List of ServicesLeo LastimosaAinda não há avaliações
- Bulacan State University College of Nursing City of Malolos, BulacanDocumento2 páginasBulacan State University College of Nursing City of Malolos, BulacanVIRGINIA M. SANTOSAinda não há avaliações
- Formation of Faeces and DefaecationDocumento15 páginasFormation of Faeces and Defaecationzurich100% (5)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Chapter 32 - Stop-Controlled Intersections Supp - 600Documento74 páginasChapter 32 - Stop-Controlled Intersections Supp - 600Ana María Lira CastroAinda não há avaliações
- BooksDocumento5 páginasBooksDanijela VukcevicAinda não há avaliações
- Sieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsDocumento18 páginasSieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsMelissa Viana100% (1)
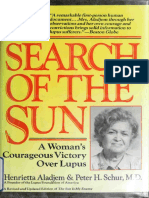
- Aladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Documento310 páginasAladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Anonymous gwFqQcnaX100% (1)
- Fascial Manipulation Practical Part PDFDocumento2 páginasFascial Manipulation Practical Part PDFBrandi0% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Supervision ToolsDocumento5 páginasSupervision ToolsYaya Taeh Baruh PykAinda não há avaliações
- Daftar Pustaka OaDocumento2 páginasDaftar Pustaka OaCut Naja SoviaAinda não há avaliações
- Lab Scientist Job DescriptionDocumento3 páginasLab Scientist Job DescriptionRajeev PareekAinda não há avaliações
- 1000 Calorie ChallengesDocumento25 páginas1000 Calorie ChallengesFrancesco Iavarone100% (3)