Escolar Documentos
Profissional Documentos
Cultura Documentos
Drug Use
Enviado por
HNNTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Drug Use
Enviado por
HNNDireitos autorais:
Formatos disponíveis
2017
SYRINGE EXCHANGE PROGRAM
ANNUAL REPORT
677 Ala Moana Blvd. Suite 226
Honolulu, HI 96813
(808) 521-2437
www.hhhrc.org
ALMOST THIRTY YEARS OF SYRINGE EXCHANGE
IN HAWAI`I
The Hawaiʻi State Department of Health (DOH) started a pilot syringe exchange project in
1989 in response to the growing Acquired Immunodeficiency Syndrome (AIDS) crisis. The project
involved training ex-persons who inject drugs (PWID) and other individuals knowledgeable about the
drug-using population to serve as peer educators for PWID who were at high risk for acquiring
and/or transmitting the Human Immunodeficiency Virus (HIV). In 1990, former Hawai`i Governor
John Waihe`e signed into law Act 280, enabling DOH to establish a two-year pilot Syringe Exchange
Program (SEP). The first Hawai`i SEP site was operated out of the Rubber Room in Honolulu by
members of the Life Foundation, the largest and oldest AIDS organization in the Pacific (which in July
2018 merged with Community Health Outreach Work to Prevent AIDS (The CHOW Project) to create
the Hawai`i Health & Harm Reduction Center). Following the two-year pilot period, during which the
SEP’s safety and efficacy were assessed, the State Legislature created the Needle Exchange Program
in Act 152 (1992), which was codified in chapter 325, Part VII, of the Hawai`i Revised Statutes (HRS).
(See, Needle Exchange Program, section 325-111 through 325-117, HRS). This legislation enabled the
DOH to operate the SEP for as long as necessary to accomplish its intended purposes: preventing the
transmission of HIV, hepatitis B virus (HBV), hepatitis C virus (HCV), and other blood-borne
pathogens; and providing PWID with referrals to appropriate health and social services. HRS §325-
115 requires the DOH to appoint an oversight committee to monitor the progress and effectiveness
of the SEP and to examine available data compiled by the program. HRS §325-116 requires the DOH
to report annually to the oversight committee, including the number and demographics of
participants, the impact of the program on HIV infection, an assessment of the cost-effectiveness of
the program, the strengths and weaknesses of the program, the advisability of its continuation, and
ways to improve the SEP.
In 1993, the legislature named Community Health Outreach Work to Prevent AIDS (The CHOW
Project) as the coordinating agency for the statewide SEP. By 1994, The CHOW Project extended the
SEP services beyond O`ahu to the islands of Kaua`i, Maui, and Hawai`i island. The CHOW Project
continues to operate the SEP under its new title, the Hawai`i Health & Harm Reduction Center
(HHHRC), and has expanded services to meet the growing needs of people who inject drugs in
Hawai`i. In the SEP year 2017 (January 1 – December 31) HHHRC was still known as CHOW and will be
referred to as such for the remainder of this report. In 2017 CHOW exchanged 1,068,621 syringes
statewide, which is an almost 3,000% increase since 1993 when it exchanged only 35,365 syringes.
The CHOW Project operates five mobile vans which cover each of Hawai`i's counties and
provides a variety of services beyond syringe exchange. Outreach workers attempt to establish
contact and trust with the target population in an effort to encourage safer behaviors among PWID.
Activities include conducting health education; offering HIV and HCV testing and counseling; linkages
to housing navigation and other services; wound care; overdose prevention education, including
naloxone training and distribution; as well as handing out harm reduction supplies such as condoms,
2017 Syringe Exchange Program Annual Report P A G E 2
hygiene kits, health education materials, and pipe covers (used to prevent cuts and burns from
smoking substances with a glass pipe). Currently, the Hawai`i statewide SEP is one of the larger
programs in the United States (U.S.) and was the first program in the U.S. to be fully state-funded to
offer coordinated services statewide.
SEP OPERATIONS
Hawaii's SEP began in a fixed location which provided the opportunity for The CHOW Project
to offer comprehensive services to participants accessing the SEP. After the building was sold, CHOW
relocated offices to a building that currently does not allow participants to access syringe exchange
services onsite. The SEP is currently entirely run through mobile sites and Syringe Exchange
Appointments (SEA) where outreach workers meet participants at locations convenient for the
participant. While this model provides flexibility, it limits the services that may be provided, such as
HIV and HCV counseling, testing, and referral (CTR), wound care, and other activities, although CHOW
continues to find innovative ways to provide these services in the field. The SEP continues to seek a
fixed site that would be appropriate for participants in Honolulu in order to provide more
comprehensive services; Neighbor Island sites will continue to be run through the mobile vans. The
downtown Honolulu mobile exchange has a regular schedule with the van parked in the same
location five days a week, and most of the Neighbor Islands have a fixed schedule where the vans are
parked at a location regularly in addition to SEA visits.
In 2016, the SEP began a collaborative relationship with the Hawai`i Island HIV/AIDS
Foundation (HIHAF) in Kailua-Kona. HIHAF conducts syringe exchange out of their office on Palani
Road. Hawaiian Ocean View Estates (HOVE) continues to be served by CHOW outreach workers from
Hilo. Starting in 2017, Mālama Pono Health Services provided syringe exchange services on Kaua`i,
hoping to provide more services to PWID who may not have normally contact with the SEP.
From January 2017 to December 2017, the SEP operated in the following areas:
Island Exchange Site Area of Operation
CHOW O`ahu Mobile Exchange Island-wide
O`ahu CHOW Downtown Mobile Exchange Downtown Honolulu
CHOW Hawai`i Mobile Exchange East-Hawai`i
Hawai`i CHOW/HIHAF Kailua-Kona Fixed Site Kailua-Kona
Maui CHOW Maui Mobile Exchange Island-wide
CHOW Kaua`i Mobile Exchange Island-wide
Kaua`i Mālama Pono Health Services Lihue
2017 Syringe Exchange Program Annual Report P A G E 3
As of May 2015, there were a total of 228 known SEPs operating in 35 states, the District of
Columbia, and Puerto Rico.1 SEP sizes range from small (<10,000 syringes exchanged a year) to very
large (>500,000 syringes exchanged per year) with only 21% falling in the category of very large. For
SEP2017, the Hawai`i SEP continued to be classified as “very large.”
PREVALENCE OF INJECTION DRUG USE AND
OTHER RISK BEHAVIORS
Nationally the prevalence of injection drug usage among youth has remained steady over the
last several years with 1.5% of high school youth reporting that they have ever injected an illegal drug
in 2017.2 Locally in Hawai`i, 2.8% of public high school students and 7.1% of public middle school
students reported ever injecting any illegal drugs in 2017.3
1200 Public High School Students In Hawai`i have ever injected
any illegal drug in 2017
2000 Public Middle School Students
Vulnerable populations, including sexual and gender minorities, disproportionately report
injection drug usage. Recent data from Hawai`i State Department of Health’s Sexual and Gender
Minority Health Report show that almost 1 in 10 (8.9%) lesbian, gay, and bisexual (LGB) youth
reported ever injecting an illegal drug.4 Additionally, 12.2% of high school youth and 6.8% of middle
school students in 2017 reported misusing prescription pain medication, which has been associated
with future injection drug use.3,5 These troubling statistics show that the number of youth in Hawai`i
at risk for injection drug use is high.
Limited data sources exist for adult prevalence of injection drug usage in Hawai`i. State level
surveillance, as well as monitoring at SEP, are important for identifying populations at risk and
developing culturally appropriate and tailored services and interventions.
OVERDOSES IN HAWAI`I
In Hawai`i, poisoning is the leading cause of self-injury-related deaths, with drugs causing
upwards of 90% of these deaths in 2014.6 Additionally, overdose deaths have been increasing over
the past decade, surpassing motor vehicle traffic deaths in 2008 to take the number one spot.
Examining the types of drugs that are leading to these high rates, at least 35% of these deaths were
found to be caused by opioids including oxycodone and hydrocodone. While there has been
increased federal regulation of prescription opioids nationally, many persons still addicted have
moved over to the illegal drug market where supplies have been found to be tainted with the
2017 Syringe Exchange Program Annual Report P A G E 4
cheaper and stronger drug Fentanyl.7 In response to this growing crisis, CHOW began offering
trainings and education on overdose prevention (see Naloxone and Naloxone Refill Databases).
PROGRAM EFFECTIVENESS
To ascertain the effectiveness of the SEP, it is important to look at cases of HIV and AIDS
among PWID in Hawai`i and to compare this data with national HIV/AIDS surveillance. Historically,
both national and local data have been available only for AIDS cases since HIV was not a reportable
condition for the first two decades of the epidemic. This creates limitations because some individuals
with HIV may take many years to progress to an AIDS diagnosis (if at all) – especially in the age of
combination anti-retroviral therapy. Thus, the picture created by looking only at AIDS cases may not
reflect the current trends in HIV infection. Despite these limitations, AIDS data can help determine
the epidemiology of HIV/AIDS, especially when it comes to risk factors linked to acquisition of the
disease.
As of 2016, there have been 1,232,346 reported cases in the United States that met the AIDS
diagnosis criteria established by the Centers for Disease Control and Prevention (CDC).8
Approximately 675,000 (57.7%) of persons who have ever been diagnosed with AIDS have died9. In
2016, 13% of incident AIDS cases in the United States were directly attributable to injection drug use
(IDU) or combined MSM/IDU.10 In Hawai`i, the incidence rate of AIDS is 2.5 per 100,000 persons
annually. Of these cases with an AIDS diagnosis, 14% were directly attributable to IDU, with none
reporting combined MSM/IDU risk. Since reporting began in 1983, 15% of all incident AIDS cases in
Hawai`i were attributable to IDU or MSM/IDU.11
In alignment with nationwide moves to report HIV cases by name, in 2008 Hawaii amended its
administrative rules to require named HIV reporting. This provided more accurate HIV data (including
AIDS cases) and provided a more precise picture of those living with HIV in Hawai`i. As of 2016, there
were 1,100,000 persons living with HIV in the United States, with an estimated 15% unaware of their
status.12 In Hawai`i, there are 2,519 persons living with diagnosed HIV infections, with an annual
incidence rate of 6.3 cases per 100,000 persons.11 Nationally, 9% of incident HIV infections were
directly related to IDU or MSM/IDU risk.13 In 2016, only 1% of incident HIV infections in Hawai`i were
attributable to IDU, and an additional 3% were attributable to MSM/IDU. Cumulatively, 9% of total
reported incident HIV diagnoses ever in the state were attributable to IDU or MSM/IDU.11 While
Hawai`i is comparable to the rest of the nation in incident AIDS cases attributable to IDU or MSM/IDU,
a significantly smaller proportion of annual incident HIV cases are related to injection drug use,
presumably due to the proactive efforts to implement a SEP in Hawai`i resulting in a lower overall
seropositive prevalence among this population.14
Results of CHOW’s HIV seroprevalence studies of the past ten years found a HIV+
seroprevalence between 0.0% and 5.8% among CHOW’s study cohorts. These low numbers, coupled
with the HIV/AIDS data above, is evidence that access to sterile syringes and other injection-related
2017 Syringe Exchange Program Annual Report P A G E 5
equipment is keeping the HIV prevalence low among PWID which simultaneously decreases the risk
of HIV in their sexual partners and children. Not only has the HIV prevalence among PWID accessing
the SEP continued to be low, having lower numbers of active PWID living with HIV decreases the risk
for other PWID (and their partners) to become infected. Access to sterile syringes and other
equipment decreases HIV-related risk behaviors, such as sharing used needles,15 but does not erase
injection-related risk completely. Maintaining a low prevalence of HIV among PWID lowers their risk
for HIV infection in the event they engage in high risk activities such as sharing equipment.
Additional factors likely contribute to maintaining a low prevalence of HIV among the
population, including services which allow the SEP to reach participants who do not directly come
into contact with SEP staff.
Secondary syringe exchange, also known as “gatekeeping,” is the practice
of a participant exchanging syringes for someone other than themselves. With a large proportion
of SEP’s participants reporting gatekeeping for other individuals, this practice increases clean
syringe access to PWID in Hawai`i who may otherwise not have contact with the SEP, whether it
be due to barriers around access, issues with confidentiality, or lack of trust among other
reasons.
In addition to providing access to clean syringes and related equipment, CHOW distributes
condoms to clients to prevent the spread of sexually transmitted infections, including HIV, HBV, and
HCV to their partners.
An unfortunate truth is that the effectiveness of syringe exchange services is often highlighted
by the seroprevalence of populations who do not have access to clean syringes. In the spring of 2015,
news sources reported an outbreak of HIV in a rural southeastern town in Indiana, with a majority of
cases being linked to injection drug use and the sharing of injection drug equipment. As of May 2016,
the Indiana State Department of Health has reported 217 confirmed HIV positives linked to this
outbreak.16
In addition to helping prevent the spread of HIV, syringe exchange programs have been found
to also decrease the spread of other blood borne pathogens, such as HCV.17 National and local data
on the prevalence of HCV were not available, but results from previous seroprevalence evaluations
have found that 65% to 89% of clients have screened positive since testing began in 2007.
METHODS AND DATA SOURCES
The timeframe for the annual report is January 1, 2017 through December 31, 2017.
The CHOW Project collects data through a variety of sources and maintains six databases: the
Daily Log database which captures CHOW services and participant demographics; the Survey
2017 Syringe Exchange Program Annual Report P A G E 6
database which compiles data from the annual survey results; the Participant Card database which
collects basic demographic data and selected risk factors on participants who have received a
participant card; the Naloxone database which collects information on trained participants who have
received naloxone and overdose prevention education from CHOW; the Naloxone Refill database
which contains data on overdose events and reasons for refills; and the Seroprevalence databases
which include HIV and HCV counseling and testing data. Data from these sources are combined to
create a picture of CHOW’s services and the participants who access them. For SEP2017, the annual
survey was not conducted on 100 clients (unlike previous years) due to limited staffing capacity
caused by the merge of Life Foundation and The CHOW Project. Despite this, the data presented
herein is a snapshot of the SEP services and resulting impact, and still provides valuable process and
outcome data to show the effectiveness of the SEP. Additionally, this is the first year that participants
have been linked across databases to examine engagement across multiple services provided by
CHOW.
Daily Logs
Data from the daily logs includes operational information collected by CHOW staff each time
a participant exchanges syringes or accesses harm reduction supplies. This includes the number and
type of syringes exchanged, and other outreach activities such as contraceptive distribution. This
database is the foundation for the data reported in the section on Syringe Exchange Program activity
for the SEP year. Additionally, the Daily Logs Database was used to identify the participants (through
participant ID/card number; see next section) who were in touch with the SEP and other services in
2017.
Participant Card Log
Started in 2012, every person who exchanges syringes with the SEP is offered a participant
card with a unique number which identifies that person as a participant with the program.
Participants remain anonymous and may choose not to register. A member of the outreach team
creates a unique identifier for the participant (herein referred to as participant ID) and collects basic
demographic data and some injection drug practices on the participant.
The card has been well received, as it also summarizes the law allowing participants to carry
syringes to and from the exchange printed on the back (“The person bearing this card has registered
2017 Syringe Exchange Program Annual Report P A G E 7
with the Hawai`i Health & Harm Reduction Center, a statewide syringe exchange program funded by the
Hawai`i Department of Health. This participant is carrying syringes to and from the exchange because it
has been proven to prevent the transmission of HIV, hepatitis, and other blood-borne pathogens. Hawai`i
Revised Statutes §325-114 provides that exchanges under this program shall not constitute an offense for
the participant.”). The participant card has been reported to offer participants limited amnesty when
they are stopped by police and allows them to keep syringes they have in their possession.
At the end of 2015, the outreach team also began collecting the participant card number of
the people who exchange on the daily log (see above). In response to this, staff increased their
efforts and began encouraging more persons to register. Persons were still allowed to opt out if they
did not want to register. This information allows the SEP to have an idea of how many unique
individuals exchange in any given year. SEP2016 saw 1,085 unique participant cards. While this
number does not include participants who refused a card, this is the second year that the SEP has
been able to measure the number of individual participants served. Any time ‘SEP2017’ data is listed
below, it refers specifically to individuals who exchanged syringes in 2017, registered for a participant
card, and were captured on the Daily Log (see above).
Naloxone and Naloxone Refill Databases
In September 2016, CHOW rolled out their naloxone program which consisted of individual
and group trainings on injectable naloxone. At first these trainings were primarily offered to PWID,
and occurred both at the syringe exchange sites and during outreach. After some time, the trainings
were expanded to include social service providers, law enforcement, librarians, and friends and
families of PWID. During the training some information is collected on the participant, including
socio-demographics, and overdose risk factors and history if applicable. In the event the participant
uses their naloxone (or if it is stolen, lost, or expired), the participant can get a refill and SEP staff
collects some additional information at that time.
Testing and Linkage & LUTHER Databases
In addition to access to syringe exchanges and other harm reduction supplies, CHOW also
offers HIV and HCV counseling, testing, and referral services for all participants. On O`ahu, these
services are offered on a regular basis at the Honolulu site while participants access other services.
Additionally, CHOW held health fairs where clients were screened and, if positive, referred to
appropriate medical care. For sites on Neighbor Islands, SEP staff refer participants to DOH testing
centers. This data is collected in the State’s LUTHER database which collects demographic
information as well as data on various risk factors for HIV and HCV infections. Unfortunately, there
was no way to identify neighbor island referrals from CHOW outreach workers in the database,
although this is being addressed at the time of this publication so that neighbor island screenings
could be included in reports in future years.
2017 Syringe Exchange Program Annual Report P A G E 8
Statistical Analyses
Univariate and bivariate analyses were conducted to calculate frequencies, prevalence
estimates, and measures of association. T-tests and Chi Square tests of independence were
conducted to look for significant differences between groups when applicable. Participants were
allowed to choose several race/ethnicity groups, although methodology was borrowed from the
Hawai`i State Department of Health to code all persons who identify as Native Hawaiian as “Native
Hawaiian/Part Native Hawaiian.”18 If participants identified with one or more other groups, other
than Native Hawaiian, then they were coded as multiracial. Moving forward, data collection forms will
be revised so that folks can be classified as a single race/ethnicity to align with the State. All analyses
were conducted in SAS 9.4 (Cary, NC). Significance was set at an alpha level of 0.05.
SYRINGE EXCHANGE ACTIVITY
In 2017, the SEP exceeded its program high by exchanging a total of 1,068,621 syringes,
maintaining its status as a very large SEP for the eighth year in a row (Figure 1). The month of May
was the busiest month with over 1,200 visits and 100,000 syringes exchanged statewide.
Figure 1. The total number of syringes exchanged statewide from 1993-2017.
1,068,621
1,000,000
800,000
# Syringes
600,000
468,379
400,000
173,761
200,000
0
1993 1995 1997 1999 2001 2003 2005 2007 2009 2011 2013 2015 2017
There were a total of 12,543 participants visits in 2017, which represents a 12.8% increase
from the 11,120 visits observed in 2016 (Table 1). On average, a participant exchanged 83 syringes
per visit. Of all these visits, 3,696 (29.5%) reported gatekeeping 707,715 syringes and injection drug
equipment for an additional 10,072 people. Of note, one participant reported gatekeeping for an
additional 100 people in a single visit. Compared to 2016, gatekeepers exchanged for an additional
2017 Syringe Exchange Program Annual Report P A G E 9
6,671 people, representing an increase of over 50%. This dramatic increase underscores the
importance of the SEP providing gatekeeping services to reach persons who may not have contact
with its services otherwise.
There were 135 new clients in 2017, of whom only 19 were youth. Despite this, CHOW has
received feedback from many neighbor island sites that report an increase in youth participants
accessing services. Kaua`i had the greatest proportion of first visits (6%).
The average number of syringes exchanged per visit on O`ahu has been decreasing for
several years. In 2014 the average number of syringes exchanged was approximately 86 per visit,
which is nearly twice as high as in 2017 (47 syringes). This may, in part, be explained by the large
increase in the number of visits to the O`ahu exchange. There was a 21% increase alone in the
number of visits between 2016 and 2017. East Hawai`i saw a decrease in both the number of visits
and syringes exchanged. This was due in part to delays in hiring a new outreach worker. Despite this,
March was one of the busiest months for that site in terms of the total number of syringes
exchanged (>20,000). Had hiring delays not occurred, the total number of syringes exchanged may
have been even higher.
In addition to syringes, many of the visits consisted of providing equipment and services to
participants. Condoms were distributed in 2,214 (17.7%) of visits, other syringe equipment such as
pipe covers were distributed in 1,242 (9.9%) of visits, and hygiene kits in 1,644 (13.1%) of visits.
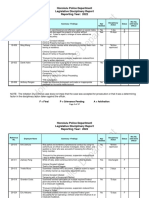
Table 1. Number of participant exchange visits, first visits, syringes exchanged, and average number of syringes exchanged
by site during SEP2016 and SEP2017.
Syringes Average Number of Syringes
Total Visits First Visits
Exchange Site Exchanged Exchanged Per Visit
N (%)* N (%)*
N (%)* N**
Statewide 12,967 135 (<1%) 1,068,621 83
11,120 133 (1%) 1,020,286 92
10,401 (80%) 60 (<1%) 487,041 (46%) 47
O`ahu
8,591 (77%) 41 (<1%) 455,022 (45%) 53
526 (4%) 13 (2%) 188,824 (18%) 339
East Hawai`i
636 (6%) 8 (1%) 220,220 (22%) 347
1,024 (8%) 10 (<1%) 139,139 (13%) 136
West Hawai`i
836 (8%) 34 (4%) 113,266 (11%) 136
505 (4%) 22 (4%) 170,669 (16%) 338
Maui
690 (6%) 31 (5%) 159,114 (16%) 231
511 (4%) 30 (6%) 83,908 (7%) 165
Kaua`i
367 (3%) 19 (5%) 72,264 (7%) 197
*Percents reflect column percentages, except for the “first visits” column, which represents the percent of total visits that were
first visits. **The average number of syringes have been rounded up to the nearest whole integer.
2017 Syringe Exchange Program Annual Report P A G E 10
DEMOGRAPHICS AND SELECTED RISK FACTORS
Of the 12,543 visits in 2017, a participant card number or participant ID was recorded for
11,687 visits (93.2%), resulting in potentially 1,536 unique participants. Over 82% (1,274) of these
potentially unique individuals on the daily log were able to be matched back to the participant card
database based on either of these identifiers; these were reconciled to avoid repeat participants
based on separate IDs.
The remainder of data in this section are on these 1,274 unique participants (noted as
SEP2017) unless otherwise stated. Comparison data is provided on individuals who previously
registered for a participant card but were not captured in the 2017 Daily Log database (n=1,050).
Participant Card Number versus Participant ID
Anecdotally, many of the participants forget to bring their participant card with them to the
SEP and often do not remember their card number, so staff try to collect their participant ID
instead, which is based on their father and mother’s name, and month and day of their birth.
The Participant Card Database contains clients’ participant card number and participant ID.
Consolidating and merging the daily log back to this database allows for the identification and
elimination of potentially duplicated clients. There are some limitations: while participant card
numbers are unique there is the possibility that two clients have the same participant ID.
Additionally, there is the possibility participants never registered for a participant card in the
first place because they have the right to refuse. Third, it could have been recorded incorrectly.
Finally, participants may have registered multiple times making older card numbers obsolete.
SEP2017 participants visited the SEP a range of one to 179 visits, with a median of three visits.
These participants exchanged a total of 1,021,395 syringes. SEP2017 visits on average exchanged 87
syringes per visit compared to 38 syringes for visits where no identifier was provided. Similarly, visits
with recorded participant card numbers/IDs on average provided gatekeeping services to more
people than visits where no identifier was reported. Over a course of a year, SEP2017 participants
exchanged a total of 261 syringes on average.
Five hundred and three people registered for a participant card in 2017. These clients and 771
from previous years make up the 1,274 unique participants who visited the SEP in 2017. Of note, 35
participants with participants cards accessed SEP services at multiple sites. Surprisingly only 9 (26%)
of these participants visited both East and West Hawai`i sites. The majority of these participants
primarily accessed services on Kaua`i and Maui, and sporadically on O`ahu.
2017 Syringe Exchange Program Annual Report P A G E 11
SEP2017
White 47.1%
Other 4.4%
Multiracial 13.3%
Black 1.6%
Other Pacific Islander 1.5% Native Hawaiian/Part Native Hawaiian 23.7%
Native American/American Indian 2.0%
Asian 6.5%
Figure 2. Race/ethnicity breakdown for participants who were in contact with the SEP in 2017
Most clients who accessed the SEP in 2017 (42.5%) had registered for a participant card their
first time accessing the SEP’s services, while close to 1 in 5 (19.5%) had been a client for five or more
years before registering. Hopefully as time goes on, more ‘first timers’ will register for a card so that
participants can be better tracked over time as they access SEP services.
The ages of participants ranged from 18 to 81 years. The average age of a client in 2017 was
43 years, which was no different than registered participants who were not in contact with the SEP in
2017 (43 years; p=0.45). Traditionally the SEP population has been an aging population, but many of
the sites anecdotally report an increase in youth participants. SEP2017 participants were diverse in
terms of their self-described gender, with 66.4% identifying as male, 31.5% as female, and 2.1% as
transgender or gender non-conforming. SEP2017 clients were significantly more likely to be male
than those not in contact with the SEP (p=0.03). The majority of SEP2017 identified as White (47.2%),
followed by Native Hawaiian/Part Native Hawaiian (23.7%), multiracial (23.7%), and Asian (6.5%;
Figure 2). SEP2017 were only marginally statistically different (p=0.06) in terms of race/ethnicity
distribution than participants who were not in contact with the SEP in 2017, with SEP2017
participants less likely to be white and more likely to be Native Hawaiian/Part Native Hawaiian. The
majority of SEP2017 clients were born in other states or overseas, with only 42.0% of clients
reporting being born in Hawai`i. Of note, 16.7% were born in California, the most common birthplace
after Hawai`i.
Housing continues to be an issue for a majority of SEP participants. More than one third
(37.3%) reported being homeless, and an additional 22.2% reported having temporary/unstable
housing situations. Only 2 in 5 (40.5%) reported having permanent housing. SEP2017 clients were
significantly more likely to be homeless and have unstable housing compared to those who did not
access the SEP (p=0.0031). Since 2014, CHOW has collaborated with other social service organizations
for outreach and case management to get more SEP participants into housing. Due to the stigma
faced by PWID, many people who were homeless were not accessing other social services. Once SEP
2017 Syringe Exchange Program Annual Report P A G E 12
staff began assisting their participants in accessing other social service organizations for housing,
they were more likely to engage because of their trust in CHOW.
Syringe Access as a Bridge to Other Services
The CHOW Project has recognized its role as the only social and health service many
participants regularly access. Previous evaluations have found that clients face many negative
social determinants of health, have poor health outcomes, and would likely benefit from
assistance. Through syringe access, CHOW has enabled many other services for participants,
including overdose prevention education, HIV/HCV counseling, testing and referral services, wound
care, and housing assistance (outreach workers secured permanent housing for 25 participants in
2017). Through its non-judgmental and low-threshold approach, CHOW reaches people who are
vulnerable and marginalized, and who have often been stigmatized for their drug use. Through
collaborating with CHOW, other agencies have learned to better work with PWID.
64.4% of clients reported not being employed. Among those who were employed, the largest
proportion reported working in construction (15.6%), followed by professional/office (9.6%) and then
restaurant/service industry (9.4%). The clear majority of clients reported having some form of health
insurance (82.1%). Despite this, previous evaluations have found high emergency room services
utilization and low preventive and regular health checkups.19 In response to this alarming trend,
CHOW began offering wound care services to clients in 2016, as open wounds are a major issue for
SEP participants. SEP wound care program evaluation findings show tremendous cost savings
compared to treatment at a hospital; every nickel spent at CHOW was equal to one dollar spent at
the emergency department.20
More than 2 in 5 (41.5%) SEP2017 participants reported their most frequent injectable drug
was heroin, followed by meth/ice (27.8%), and prescription opioids (20.5%). Participants in contact
with the SEP in 2017 were significantly more likely to inject heroin or meth, but less likely to inject
opioid pills (p<0.0001). Of note, 3.4% of clients reported only gatekeeping and no injection drug use.
Among SEP2017 clients, 233 (18.3%) were trained on overdose prevention highlighting the need to
continue to reach all clients, especially those at increased risk for overdose.
NALOXONE TRAINING AND REFILLS
Since September 2016, CHOW has trained 458 people on overdose prevention, including
rescue breathing and naloxone administration. In the year 2017 alone, 308 persons were trained
(Table 2). Among those trained included PWID, friends of family of PWID, community partners, law
enforcement, and the general public. The majority of persons trained in 2017 were male (52.3%),
followed by female (45.1%) and transgender (1.6%) The majority of persons identified as White
(55.5%), followed by Native Hawaiian/Part Native Hawaiian (21.8%), and multiracial (9.4%).
2017 Syringe Exchange Program Annual Report P A G E 13
Table 2. 2017 Naloxone training participants and selected Several questions are asked to
demographics and risk factors. screen trainees at risk for overdose.
Trainee One of these questions is on current
substance use. More than two thirds
N (%)
(70.0%) of persons reported using
Total 308 substances in the last thirty days. The
Demographics most commonly used substance was
Male 52.3% heroin (65.3%), followed by
Female 45.1% methamphetamine (57.4%), opiates
Transgender 1.6% (41.7%), benzodiazepines (32.4%),
alcohol (37.0%), methadone (25.0%)
Race/Ethnicity
crack/cocaine (13.9%), Suboxone
White 55.5%
(16.7%), and other substances (13.5%)
Native Hawaiian 21.8%
including marijuana, Fentanyl, and
Other Pacific Islander 2.6%
Clonidine (0.3%). Only 1 in 4 (24.5%)
Asian 5.5%
reported mono-drug use, with most
Native American 1.3%
persons (75.5%) reporting polydrug use.
Other 3.6%
Polydrug use has been associated with
Multiracial 9.7%
an increased risk for overdose, and is
Current Substance Use (Past 30 days) responsible for the majority of
Heroin 65.3% overdoses in the United States.21 More
Methamphetamine 57.4% than two thirds (68.8%) of participants
Prescription Opiates 41.7% who reported current substance use
Alcohol 37.0% also reported current injection drug
Benzodiazepines 32.4% use.
Methadone 25.0%
Among participants who were
Suboxone 16.7%
injecting drugs, close to half (49.5%) of
Crack/Cocaine 13.9%
these participants reported always
Other 13.5%
injecting in a private location, such as
Injection Drug Use* an apartment, hotel room, or house. An
Yes 68.8% additional 8.5% reported always using
Injection Practices** out in public, such as parks, public
Always inject in Private Location 49.5% bathrooms, on the streets, or in a car. In
8.5% terms of injecting practices, 83.5%
Always inject in Public Location
reported injecting alone, with 1 in 5
Always inject alone 20.3%
(20.3%) reporting always injecting alone.
Time off from using substances (past year)** While injecting alone may not increase
Yes 58.9% one’s risk for overdose, it may make it
*Among participants who reported using substances in the less likely that a person would survive
last thirty days. an overdose if it were to happen.
**Among participants who report injecting drugs.
2017 Syringe Exchange Program Annual Report P A G E 14
More than half (58.9%) of participants who were currently injecting drugs reported taking
time off from using during the last year, for reasons that include going to treatment, incarceration, or
simply cutting down on use. This is alarming since tolerance decreases during times of non-use
which can consequently increase one’s risk for overdose.22,23 Based on these data, an overwhelming
number of persons trained were at risk for overdose.
Overdose History
CHOW also collected data on overdose history, including on the participant themselves and if
they’ve ever witnessed someone else overdose (Table 3). Almost 1 in 3 (31.4%) trainees reported
ever overdosing one or more times. The majority identified as male (55.7%) and white (55.2%).
Participants overdosed a range of one to 50 times, with the median being two times. Many trainees
did not report a known reason for overdosing. Among those who did know, participants reported
that stronger drugs (32.1%), mixing substances (22.6%), low tolerance due to incarceration or
treatment (19.0%), and that they took too much (16.7%) were the most common known reasons.
Interestingly, many participants speculated that their substances were mixed with Fentanyl. While an
overdose can be accidental in nature, over 3% of participants reported that they were trying to kill
themselves. Participants were asked to recall if someone had ever administered naloxone to them
during one or more previous overdose events. Only 18.1% reported that naloxone had been ever
administered one or more times when they overdosed. The majority of these participants were
administered naloxone by an EMT (41.2%), followed by medical personnel at the emergency room
(41.2%), and non-medical persons (17.6%).
Participants were also asked to recall the drug or drugs used that led to their last overdose, as
well as their location and how they were revived. Almost half (46.7%) reported using heroin, followed
by other prescription opioids/benzodiazepines (15.5%). Almost a third (32.6%) reported polydrug use.
Of note, 7.2% reported using Fentanyl although many participants may have been inadvertently
exposed using other substances as reports have found local supplies of substances tainted.7 Despite
this, 95.9% of trainees who previously overdosed reported current substance use. Trainees were also
asked to describe what actions were taken when they last overdosed, if they could recall. Almost one
fifth (18.8%) of trainees who overdosed reported that naloxone was used to revive them the last time
they overdosed. In addition, 15.6% of participants reported being put into a cold shower or ice was
used to help revive them, more than 1 in 10 (10.4%) reported that they came to on their own, and
12.5% reported that they were physically hit or slapped. Of note, more than a third (34.3%) did not
know how they were revived.
The majority reported overdosing either at home (30.3%), or in public, in both unsheltered
locations (28.1%) such as in the streets, a park, or beach, or sheltered locations (10.1%) like public
bathrooms or bars/clubs. Additionally, 7.9% reported overdosing in a car and 4.5% reported
overdosing in a hotel. An additional 16.9% reported overdosing in another private residence, like a
friend’s or family member’s house. Less than 1% did not remember where they overdosed.
2017 Syringe Exchange Program Annual Report P A G E 15
In addition to experiencing overdoses, an overwhelming majority (65.2%) of trainees have
witnessed someone else overdose. The number of overdoses ranged from one to over 200; the
median number of overdoses a trainee witnessed was two. Nearly all (94.0%) could recall which
drug(s) were used prior to the last overdose they witnessed. The most common was heroin (55.2%),
followed by other prescription opioids/benzodiazepines (6.7%), and Fentanyl (5.5%). Over a quarter
(27.5%) reported poly-drug use. Among those who reported polydrug use, many of the participants
reported the person who overdosed was mixing heroin or meth with prescription medications, such
as benzodiazepines, opiates, and barbiturates. Less than half (41.8%) of participants reported that
naloxone was used to help revive the last person they saw overdose.
Table 3. Participants who experienced one or more overdoses, and participants who witnessed one or more overdoes, by
select demographics, risk factors, and protective actions.
Trainee -Previously Trainee-Witnessed
Overdosed Overdose
N (%) N (%)
Total 97 (31.4%) 201 (65.2%)
(%) (%)
Demographics
Female 43.8% 47.5%
Male 55.2% 51.3%
Transgender 1.0% 1.3%
Race/Ethnicity
White 55.2% 52.5%
Native Hawaiian 21.9% 22.5%
Asian 4.2% 5.0%
Other Pacific Islander 2.1% 2.5%
Native American/American Indian 1.0% 1.3%
Other 6.3% 5.6%
Multiracial 9.4% 10.6%
Drug(s) Used
Heroin (alone or with another substance) 46.4% 55.2%
Other Prescription opioids or benzos
15.5% 6.7%
(alone or with another substance)
Fentanyl (alone or with another substance) 7.2% 5.5%
Meth (alone or with another substance 5.2% 4.5%
Multiple 32.6% 22.9%
Naloxone Use
Yes 18.8% 41.8%
Other Actions
Cold Shower/Ice 15.6% 22.5%
Physically Hit/slapped 12.5% 23.7%
Unknown 34.3% 0.0%
2017 Syringe Exchange Program Annual Report P A G E 16
Among these, only 9.7% of trainees reported that they dispensed the naloxone themselves,
which may explain the need for training among many of the participants. Almost half (47.2%) were
dispensed by EMT, followed by other non-medical persons such as a friend, partner, or stranger
(27.8%). Of note, three trainees reported that they witnessed CHOW staff administer naloxone on
somebody who was overdosing. In addition to naloxone use, 22.5% reported that the person was put
into a cold shower, 23.7% physically hit/slapped, 29.9% reported rescue breathing was performed,
followed by 24.4% who reported that CPR was used to help revive the person. Only 2% reported that
nothing was done when they witnessed someone overdosing. 2.5% reported that the person was
unable to be successfully revived, although this number might be much higher.
Finally, participants were also asked if they knew anybody at risk of overdose. Almost all
(91.9%) trainees said they knew at least one person at risk. Among those, 61.3% said a friend, 9.2%
said a partner, 26.4% said a client, and less than 1% said themselves. This data shows that
participants are underestimating their own risk for overdose, despite reporting activities that
increase their risk (e.g. injection drug usage, polydrug use, time off from using substances).
Naloxone Refills
Participants are given two doses of naloxone after they complete training. In the event
something happens to their naloxone doses or if they expire, they are able to get a refill from CHOW.
CHOW collects some additional information from the participant at that time (Table 4).
In 2017, 158 participants received a refill of their naloxone dose(s), representing 34.5% of all
persons who have been trained on overdose prevention since 2016. Slightly less than half (48.7%)
reported that they had lost their naloxone or that someone had stolen it. Many participants reported
that their naloxone was lost in the homeless encampment “sweeps.” The remaining 51.3% reported
either using one or both of their doses at 86 overdose events. These participants were asked to recall
if they had witnessed any overdoses since being trained; the range of overdoses was 0 to 10, with a
median of two overdoses. The majority of participants who used their naloxone were female (74.1%),
followed by male (24.7%) and transgender (1.2%). Additionally, the majority of were under the age of
40 years (64.6%).
In a similar trend to previous sections, the majority (87.7%) of participants reported that
heroin was the drug used prior to the overdose event (or latest overdose event if they used both
doses). The next most used drug was prescription opiates (16.1%), followed by meth (13.6%). Almost
half (46.9%) reported that the participant overdosed in a private residence. The remainder reported
that the person overdosed in public, including a park (24.7%), car or boat (24.7%), or on the streets
(3.7%). Other than administration of naloxone, 50.6% reported doing sternum rubs, 43.2% performed
rescue breathing, 42.0% called 911, and 35.4% reported doing other actions, including putting the
person in a cold shower, screaming, or physically hitting the person. Only 51.9% of participants
reported using just one dose of their naloxone at the overdose event. The average duration it took
to use the naloxone was one to three minutes (33.8%), followed by greater than five minutes (31.2%).
2017 Syringe Exchange Program Annual Report P A G E 17
Participants reported issues using their naloxone. These reasons included personal physical
limitations, such as disabilities, being anxious or confused, or had trouble finding it when needed.
An overwhelming 81% reported that the person overdosing woke up
because of their help, saving 66 persons!
Table 4. Overdose prevention-trained participants who got a refill of naloxone in 2017, by selected demographics, risk
factors, and overdose prevention actions.
Trainee One eighth (12.7%) reported that
N the paramedics came and helped revive
Total 158 the person. Only 2.5% of participants
Demographics (%) reported that the person died. Despite
Male 24.7% saving at least 66 lives, participants
Female 74.1% reported some negative consequences
Transgender 1.2% of reversing the overdose. Almost 1 in 4
Reason for Refill (24.7%) reported that the person became
Lost/stolen 48.1% dopesick, and 11.1% vomited. Twenty
Used one or more one percent reported that the person
51.9%
dose became angry. Only 3.7% of participants
Drug used before overdose
reported that the person was harassed
Heroin 87.7%
by the police, and 1.2% were arrested.
Opioids 16.1%
Meth 13.6%
Overdose location
Private residence 46.9%
Public 53.1%
Other Actions Taken
Sternum rub 50.6%
Call 911 42.0%
Rescue breathing 43.2%
Duration of Naloxone Use
<1 minute 14.3%
1 to 3 minutes 33.8%
3 to 5 minutes 20.8%
>5 minutes 31.2%
Outcome of Overdose
Woke up because of
81.0%
trainee
Woke up because of
12.7%
health professional
Died 2.5%
2017 Syringe Exchange Program Annual Report P A G E 18
HIV AND HCV TESTING, COUNSELING, AND
REFERRAL SERVICES
In 2017, 101 persons were screened for HIV and 34 were screened for HCV, with 31 persons
screened for both infections.
HIV
Among the 101 persons screened for HIV in 2017, the majority were youth under the age of
30 years (27.7%), followed by participants aged 30 to 39 years (24.8%), and aged 40 to 49 years
(22.8%). Despite the SEP serving an older population, the majority of participants screened for HIV
are younger, highlighting a need to screen older persons who have had more time to engage in
behaviors which increase their risk for HIV infection. Almost 2 in 5 identified as White (39.6%),
followed by those who identified with more than one race (22.8%), and Native Hawaiian or Other
Pacific Islander (17.8%). The majority screened identified as male (53.5%), followed by female (32.7%),
and transgender (13.8%). Only three quarters (76.2%) of participants reported being previously
screened for HIV, although among these, 96.1% knew their status. Among those that knew their
status, 100% reported their last test result was negative.
Many of the participants reported engaging in behaviors placing them at increased risk for
HIV infection. More than 1 in 8 (14.9%) identified as MSM. Almost three quarters (71.3%) reported
usually having sex without a condom. In addition to this, 22.8% reported ever having sex with a
PWID. Only 33.7% of participants reported injecting drugs, but 44.1% of these participants reported
sharing injection drug equipment.
Despite engaging in these high-risk activities, none of the SEP2017 participants screened
positive for HIV, providing further evidence that the prevalence of HIV among PWID population is
low, and can be likely attributed to the proactive efforts of Hawai`i to fund a statewide syringe
exchange program.
Expanded testing efforts to reach older adults and more participants in general will ensure
the seroprevalence is low among all age groups and demographics.
HCV
Thirty-four persons were screened for HCV onsite. Ten persons who were being screened for
HIV and offered HCV testing declined. An additional 11 accepted a referral for offsite testing. Among
those who were screened, the majority were 40 years of age or older (54.8%), which is older than the
population screened for HIV. A third of participants identified as White (32.3%) and multiracial
(32.3%), followed by Native Hawaiian or other Pacific Islander (16.1%). The majority identified as male
(48.4%), followed by female (32.2%) and transgender (19.4%). More than half (58.1%) of participants
2017 Syringe Exchange Program Annual Report P A G E 19
reported previously being screened for HCV. Among these, only one person (3.2%) reported being
chronically infected with HCV. The remainder reported being negative (51.6%), or unsure of their
status (3.3%). Previous screening data was unavailable for 41.9% of participants.
In terms of risk factors, only 6.5% identified as MSM. Close to half (48.4%) reported using
injection drugs and ever having sex with a PWID. One third (33.3%) of participants who reported
using injection drugs reported sharing equipment.
Despite the high prevalence of risky behaviors, only four (12.9%) participants screened
positive for HCV. All clients who screened positive were referred to appropriate medical care.
Additionally, all were referred to and accepted confirmatory testing, except for the one participant
who previously reported having chronic HCV infection. The resulting sample size was too small to
examine by various demographics.
While the proportion of participants who screened positive for HCV is lower than what has
been found in previous evaluations, this data may not be representative of all persons who access
CHOW due to both a small sample size (n=34) and the relatively small proportion who reported
injection drug usage (48.4%). Future years and increased efforts to screen the population will help
monitor the seroprevalence of the SEP population to ensure they are referred to confirmatory testing
and appropriate medical care if they screen positive.
COST/BENEFIT ANALYSIS OF HAWAI`I SEP
While there are many difficulties in conducting a cost/benefit analysis of any HIV prevention
program, costs associated with treating HIV infection are known, and the cost has increased with the
advent of highly active anti-retroviral treatment (HAART). According to a 2010 analysis,24 the average
lifetime cost of treating someone living with HIV is $379,668. The same analysis estimates that the
state of Hawai`i spends on average $26,000,000 annually on healthcare costs associated with HIV.
Additionally, a very close linkage exists between HIV infection among PWID and heterosexual
transmission of HIV in the United States.25 Based on the national data, preventing an average of
three HIV infections per year among PWID would then prevent an average of 1.2 additional HIV
infections among non-drug injecting heterosexual partners of PWID for a total of slightly more than
four infections prevented per year. The combined SEP/CHOW Project would provide a cost savings to
the State of Hawai`i if it prevented as few as two HIV infections per year.
CONCLUSIONS
HIV/AIDS among PWID is a major public health problem in many countries throughout the
world. It is a particular problem in the United States, where approximately one third of all reported
AIDS cases have been related to injection drug use. Hawai`i acted early to establish HIV prevention
programs for PWID which has kept the newly diagnosed HIV cases related to injection drug use at
2017 Syringe Exchange Program Annual Report P A G E 20
about half the national average. The CHOW HIV testing study conducted over the past ten years
found both a low prevalence and a low incidence (likely to be less than 1% per year) among PWID
participating in the SEP.26 Given that the program is relatively large, and a large number of clients
provide gatekeeping services, clean syringes likely reach a high percentage of PWID in the state, and
it is unlikely that prevalence or incidence are very different among PWID not participating in the SEP.
The continuing success in limiting HIV transmission among injecting drug users in Hawai`i is notable
given indications of a resurgence of HIV infections among some high-risk populations in Hawai`i and
in other parts of the United States.11,12
Despite a low prevalence for SEP2017, the prevalence of chronic HCV among participants is
thought to be high. The CHOW HCV testing study conducted for the first time in 2007 showed a high
prevalence of 88.7% and the prevalence for SEP2016 was 68%. These findings fall within the world-
wide range of 60% to 80% among PWID.27 It is unclear if many of the participants became infected
with HCV before the syringe exchange became fully established. Ongoing and increased monitoring
of the youth SEP population, including engagement in risky behaviors, is necessary to better
understand the trajectory of SEP youth and the risk for HCV infection. Nonetheless, the notable trend
of high HCV+ seropositivity prevalence among SEP participants supports the importance of syringe
exchange services in combatting the rise of other prevalent bloodborne pathogens.
Previous evaluations have found a steady increase in methamphetamine use among the SEP
community, and over a quarter of SEP2017 participants reported that methamphetamine is their
most frequently used injectable drug. Additionally, among participants who were trained for
overdose prevention, over half reported current methamphetamine use. Data from Hawai`i’s Youth
Risk Behavior Survey (YRBS) shows that 4.8% of public high school students in 2017 have ever used
methamphetamine at least one time, with the prevalence increasing over the past several years.3 It is
widely acknowledged that the use of methamphetamine, alone or in conjunction with other
substances, significantly interferes with activities of daily living. The rise in the use of
methamphetamine also coincides with the increase in homelessness in the SEP community. This
decrease in stability has had far reaching implications, including increased interpersonal violence and
a decrease in personal care. Moving forward with this subset of SEP participants will be challenging,
but the SEP will continue to seek guidance from other harm reduction organizations and the
participants themselves on the needs of this part of our community.
Despite high methamphetamine use among participants, it only causes a fraction of reported
overdose events, with the majority being caused by heroin either alone or in combination with other
substances. Increased resources are needed so that drug testing kits are available for participants to
ensure they are not consuming any potential contaminants such as Fentanyl. Additionally, the high
overdose risk profiles of the subset of SEP participants who have been trained show that expanded
efforts will positively impact the PWID population. The naloxone refill data presented herein only
represents participants who have received a refill, and anecdotally many trainees reported being
trained and giving their naloxone to PWID who may not otherwise be in contact with the SEP.
Therefore, the number of reversed overdoses is predicted to be much higher.
2017 Syringe Exchange Program Annual Report P A G E 21
The Hawai`i SEP provides multiple health and social services to its participants. The strong
linkage of the Hawai`i program to other services is notable among SEPs in the United States.
While the present data systems do not permit an exact count of the number of PWID who use
the Hawai`i SEP, the participant card data is able to give a broad estimate. As of March 2018, the SEP
had generated 2,324 participant cards for individual SEP participants. The program is one of the
larger programs in the United States based on the annual numbers of syringes exchanged with
SEP2017 having the largest number since the program’s inception. Given the upwards trend in
number of syringes exchanged, it seems unlikely that the annual number of syringes exchanged has
stabilized and monitoring of the numbers of syringes exchanged should be continued. Participants in
the SEP report moderate rates of injection risk behavior; and based on their drug injection
frequencies, participants in the SEP would be at very high risk for HIV infection if they did not have a
legal source of sterile injection equipment and other needed educational and support services. Given
the considerable costs of medical treatment for HIV infection and the consistent evidence for low
rates of HIV infection among PWID in Hawai`i, there is great certainty that the investment in the
integrated SEP/CHOW Project produces a substantial cost savings for the State of Hawai`i.
RECOMMENDATIONS
The Hawai`i SEP has become an effective statewide program and has contributed to the low
prevalence of HIV among PWID in Hawai`i. The highest priority must be given to maintaining quality
and quantity of the services provided, in particular to preventing transmission of HIV and HCV by
exchanging syringes and distributing clean cottons, cookers, and sterile water used for drug injection.
As resources allow, the SEP should expand services to include activities identified as best practices
among SEPs such as overdose prevention, access to Naloxone, and basic wound care. The SEP
should also continue to seek a fixed site for providing comprehensive services to participants in
Honolulu. While HIV prevalence is quite low in Hawai`i among PWID, the SEP should continue
offering HIV prevention interventions beyond syringe access. HIV counseling, testing, and referral
services is available to all participants, and should be encouraged more among all participants. The
SEP should work to ensure that those PWID who test positive for HIV have sufficient access to a full
range of prevention services, including partner notification, sterile syringes, and condoms to avoid
transmission behaviors, and access to HIV case management, care and treatment.
HCV prevalence is very high among SEP participants and every effort should be made to
increase the availability of sterile injection equipment for PWID at the time of drug injection. Extra
efforts should be made to support SEP participants who are negative to stay negative and to link
participants with HCV to medical care and to engage in liver wellness activities. Additionally, more
targeted efforts toward youth are needed to increase screening rates, education, and awareness.
Injection drug usage is high among Hawai`i’s youth population with subpopulations such as
sexual minorities experiencing disproportionately high prevalence. Tailored and culturally
2017 Syringe Exchange Program Annual Report P A G E 22
appropriate interventions aimed at both the prevention and treatment level are needed to address
this growing issue. Ongoing and consistent surveillance is needed to monitor the prevalence of
injection drug usage among youth in Hawai`i.
While there were a number of young injectors identified in this year’s report, PWID in Hawai`i
are an aging population. They already have substantial health problems, and these will undoubtedly
increase with age. Efforts need to be continued to assist participants accessing health care and social
services, such as housing. There are several structural barriers to increasing the health of PWID in
Hawai`i that need to be addressed.
Methadone treatment services should be expanded to West Hawai`i and Kaua`i and access
to buprenorphine should be expanded statewide as alternatives to injection drug use. More options
for substance use treatment are needed for people when the traditional abstinence model is not
effective, including harm reduction-based counseling services.
Following the lead of national overdose prevention strategies, CHOW should investigate
purchasing fentanyl test strips to give to syringe exchange participants to test their drugs and to
continue expanding its overdose prevention and response training program to reach more PWID and
service providers who work with them.
Citation: Holmes JR, Lusk HM, Maxera L, Des Jarlais DC. 2017 Syringe Exchange Program Annual
Report. Honolulu: The CHOW Project, Hawai`i Health & Harm Reduction Center. 2018.
2017 Syringe Exchange Program Annual Report P A G E 23
REFERENCES
1. North American Syringe Exchange Network, The Facts. North American Syringe Exchange
Network, 2017. (Accessed 4/26/2018, at https://nasen.org/.)
2. 1991-2015 High School Youth Risk Behavior Survey Data. The Centers for Disease Control and
Prevention.
3. Hawai`i School Health Survey : Hawai`i Youth Risk Behavior Survey Module, 2017. Hawai`i
Health Data Warehouse, State of Hawai`i.
4. Holmes JR, Ching LK, Tomita KK, et al. Hawai`i Sexual and Gender Minority Health Report.
Honolulu, HI: Hawai`i State Department of Health, Chronic Disease Prevention and Health
Promotion Division; 2017.
5. Suryaprasad AG, White JZ, Xu F, Eichler BA, Hamilton J, Patel A. Emerging epidemic of hepatitis C
virus infections among young nonurban persons who inject drugs in the United States, 2006-
2012. Clinical Infectious Diseases: an official publication of the Infectious Diseases Society of
America 2014;59:1411-9.
6. Hawai`i State Department of Health. Drug Overdose Deaths among Hawai`i Residents, 1999-
2014. 2015.
7. Heroin use skyrockets on Kaua`i after prescription crackdown. Star Advertiser 2018 3/2/2018.
8. HIV in the United States: At a Glance. The Centers for Disease Control and Prevention, 2017.
(Accessed 4/26/2018, at https://www.cdc.gov/hiv/statistics/overview/ataglance.html.)
9. CDC Fact Sheet: Today's HIV/AIDS Epidemic. The Centers for Disease Control and Prevention,
August 2016. (Accessed 4/26/2018, at
https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf.)
10. HIV Among People Who Inject Drugs. The Centers for Disease Control and Prevention. (Accessed
4/26/2018, at https://www.cdc.gov/hiv/group/hiv-idu.html.)
11. HIV/AIDS Surveillance Annual Report, Cases to December 31, 2016. Hawai`i State Department of
Health, September 30,2017. (Accessed 4/26/2018, at
https://health.hawaii.gov/harmreduction/files/2013/05/Surveillance_Rep_2017_rev20171115.pdf.
)
12. HIV Surveillance Report, Statistics Overview. The Centers for Disease Control and Prevention,
2017. (Accessed 4/26/2018, at https://www.cdc.gov/hiv/statistics/overview/index.html.)
13. U.S. Statistics. US Department of Health & Human Services. (Accessed 4/26/2018, at
https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics.)
14. Des Jarlais DC, Hagan H, Friedman SR, et al. Maintaining low HIV seroprevalence in populations
of injecting drug users. JAMA 1995;274:1226-31.
2017 Syringe Exchange Program Annual Report P A G E 24
15. Ksobiech K. A meta-analysis of needle sharing, lending, and borrowing behaviors of needle
exchange program attenders. . AIDS edcation and prevention 2003;15:257-68.
16. HIV Outbreak in Southeastern Indiana. Indiana State Department of Health.
17. Hagan H, Jarlais DC, Friedman SR, Purchase D, Alter MJ. Reduced risk of hepatitis B and hepatitis
C among injection drug users in the Tacoma syringe exchange program. American Journal of
Public Health 1995;85:1531-7.
18. Hawai`i Health Data Warehouse Race-Ethnicity Documentation. State of Hawai`i, August 2011.
at http://www.hhdw.org/wp-content/uploads/HHDW-Race-Ethnicity-Documentation-Report.pdf.)
19. Des Jarlais DC, Lenze SM, Lusk HM, Holmes JR. 2016 Syringe Exchange Program Evaluation
Report. Honolulu, HI: The CHOW Project; 2017.
20. Gralapp S, Barile J, Lusk HM, Wang C, Seto J. Wound Care: A Need Identified by a Community of
Interest in Hawai`i. Hawai`i-Pacific Evaluation Association. Hawai`i. 2016.
21. Darke S, Hall W. Heroin overdose: research and evidence-based intervention. Journal of urban
health 2003;80:189-200.
22. Krinsky CS, Lathrop SL, Brown P, Nolte KB. Drugs, detention, and death: a study of the mortality
of recently released prisoners. Am J Forensic Med Pathol 2009;30:6-9.
23. Strang J, McCambridge J, Best D, et al. Loss of tolerance and overdose mortality after inpatient
opiate detoxification: follow up study. the bmj 2003;326:959-60.
24. HIV Cost-Effectivness. 2017. at http://www.cdc.gov/hiv/prevention/ongoing/costeffectiveness/. .)
25. Schackman BR, Gebo KA, Walensky RP, et al. The lifetime cost of current human
immunodeficiency virus care in the United States. Medical Care 2006;44:990-7.
26. Salek TP, Katz AR, Lenze SM, Lusk HM, Li D, D.C. DJ. Seroprevalence of HCV and HIV infection
among clients of the nation's longest-standing statewide syringe exchange program: A cross-
sectional study of Community Health Outreach Work to Prevent AIDS (CHOW). International
Journal of Drug Policy 2017;48:34-43.
27. Nelson PK, Mathers BM, Cowie B, et al. Global Epidemiology of hepatitis B and hepatitis C in
people who inject drugs: results of systematic reviews. The Lancet 2011;378:571-83.
2017 Syringe Exchange Program Annual Report P A G E 25
Você também pode gostar
- Oral Effect of Drugs AbbuseDocumento23 páginasOral Effect of Drugs AbbusefunkybananaAinda não há avaliações
- Addiction: Epidemiology and TheoriesDocumento3 páginasAddiction: Epidemiology and TheoriestabonAinda não há avaliações
- The Democracy of Knowledge-Bloomsbury Academic (2013)Documento220 páginasThe Democracy of Knowledge-Bloomsbury Academic (2013)Sandra MalagónAinda não há avaliações
- Swearing Study The Killing PDFDocumento109 páginasSwearing Study The Killing PDFStella KoutsiAinda não há avaliações
- An Evidence-Based and Occupational Perspective of Interventions For Persons With Substance-Use DisordersDocumento17 páginasAn Evidence-Based and Occupational Perspective of Interventions For Persons With Substance-Use DisordersChel FrancesAinda não há avaliações
- Acid Trip Cure Your OCDDocumento12 páginasAcid Trip Cure Your OCDClement FarahAinda não há avaliações
- Carlin Smith Child Abuse FinalDocumento12 páginasCarlin Smith Child Abuse FinalCarlin SmithAinda não há avaliações
- Midterm Exam Study GuideDocumento6 páginasMidterm Exam Study GuideDel KenzieAinda não há avaliações
- How HipHop and Rap Affects YouthsDocumento4 páginasHow HipHop and Rap Affects YouthsSayyid Muhammad Aqeed AabidiAinda não há avaliações
- Educating Students About Drug Use and Mental HealthDocumento16 páginasEducating Students About Drug Use and Mental Healthtoshir01Ainda não há avaliações
- The Natural History of Antisocial Personality Disorder PDFDocumento6 páginasThe Natural History of Antisocial Personality Disorder PDFGustavo FigueroaAinda não há avaliações
- The Truth About InhalantsDocumento24 páginasThe Truth About InhalantsofficialdfwAinda não há avaliações
- Addiction Trajectories Edited by Eugene Raikhel and William GarriottDocumento42 páginasAddiction Trajectories Edited by Eugene Raikhel and William GarriottDuke University Press50% (2)
- Understanding Drugs Alcohol and CrimeDocumento202 páginasUnderstanding Drugs Alcohol and CrimeMihaiAinda não há avaliações
- Drugs The Straight Facts, Alcohol OptimizedDocumento104 páginasDrugs The Straight Facts, Alcohol OptimizedDeathbedeli100% (1)
- Invisible CrisesDocumento198 páginasInvisible CrisesrjmarisAinda não há avaliações
- Malaysia Drugs AddictDocumento8 páginasMalaysia Drugs AddictBotaz ChinAinda não há avaliações
- Research PaperDocumento16 páginasResearch Paperapi-559296640Ainda não há avaliações
- Chapter 2Documento2 páginasChapter 2Melissa Jean HintonAinda não há avaliações
- Drugs AddictionDocumento18 páginasDrugs AddictionReader100% (2)
- Taylor Sowell Drug Report 2017Documento9 páginasTaylor Sowell Drug Report 2017api-457709071Ainda não há avaliações
- Drugs The Straight Facts, Inhalants OptimizedDocumento105 páginasDrugs The Straight Facts, Inhalants OptimizedDeathbedeli100% (5)
- Types of AbsusesDocumento2 páginasTypes of AbsusesKARAN GAIKWADAinda não há avaliações
- There's Something About Mary-JaneDocumento5 páginasThere's Something About Mary-JaneMichelle WebsterAinda não há avaliações
- Psychological Disorder (Schizophrenia)Documento31 páginasPsychological Disorder (Schizophrenia)Farah Bashir0% (1)
- Drug Abuse, Addiction, and The BrainDocumento3 páginasDrug Abuse, Addiction, and The BrainArum ArysandiAinda não há avaliações
- Let's Call It What It Is A Matter of ConscienceDocumento33 páginasLet's Call It What It Is A Matter of ConscienceDinh Son MYAinda não há avaliações
- Drug Policy and Human Nature Psychological Perspectives On The Prevention, Management, and Treatment of Illicit Drug Abuse by John L. Falk (Auth.), Warren K. Bickel, Richard J. DeGrandpre (Eds.) PDFDocumento330 páginasDrug Policy and Human Nature Psychological Perspectives On The Prevention, Management, and Treatment of Illicit Drug Abuse by John L. Falk (Auth.), Warren K. Bickel, Richard J. DeGrandpre (Eds.) PDFpredelmAinda não há avaliações
- Parental Influence On ChildrenDocumento6 páginasParental Influence On ChildrenDaka DobranićAinda não há avaliações
- Drug 7 PDFDocumento295 páginasDrug 7 PDFNatsu DragneelAinda não há avaliações
- Drug AbuseDocumento15 páginasDrug AbuseGlenn BanlaygasAinda não há avaliações
- (2008) Abuse and Dependence Liability of Benzodiazepine-Type DrugsDocumento28 páginas(2008) Abuse and Dependence Liability of Benzodiazepine-Type Drugssharp8787Ainda não há avaliações
- Sugar The Bitter Truth ADocumento4 páginasSugar The Bitter Truth AFlorentino Rodriguez ChaviraAinda não há avaliações
- Drug Use Among Young PeopleDocumento16 páginasDrug Use Among Young Peoplelovebooks1980Ainda não há avaliações
- Introduction To Pharmacology DefinitionDocumento4 páginasIntroduction To Pharmacology DefinitionMaicha PestañoAinda não há avaliações
- Bipolar EditDocumento23 páginasBipolar EditIda LailaAinda não há avaliações
- UNICEF Youth Review InvestmentDocumento94 páginasUNICEF Youth Review InvestmentamadpocrcAinda não há avaliações
- Drugs and Substance AbuseDocumento15 páginasDrugs and Substance AbuseEve Lexy MutituAinda não há avaliações
- The Role of Dost Welfare Foundation in Rehabilitation of Drug Addicts (Noor Ahmed)Documento31 páginasThe Role of Dost Welfare Foundation in Rehabilitation of Drug Addicts (Noor Ahmed)KHAN_EROS67% (3)
- Psychoactive Drugs: The Proper Way of Using Drugs and What Effect It My Bring To UsDocumento14 páginasPsychoactive Drugs: The Proper Way of Using Drugs and What Effect It My Bring To Usathena villaAinda não há avaliações
- Violent Video Games Effects On Children and AdolescentsDocumento199 páginasViolent Video Games Effects On Children and AdolescentsCrima CrinaAinda não há avaliações
- The Impact of Social Support and Self-Esteem On Adolescent Substance Abuse Treatment OutcomeDocumento17 páginasThe Impact of Social Support and Self-Esteem On Adolescent Substance Abuse Treatment OutcomeThe Stacie Mathewson FoundationAinda não há avaliações
- Sexual Offences and Juveniles.Documento25 páginasSexual Offences and Juveniles.Sujana KoiralaAinda não há avaliações
- "Lava Jato", The Brazilian TrapDocumento22 páginas"Lava Jato", The Brazilian TrapMarcelo CordeiroAinda não há avaliações
- Internet Addiction Test: Dr. Kimberly S. YoungDocumento11 páginasInternet Addiction Test: Dr. Kimberly S. Youngvinita singh0% (1)
- Techniques of Neutralization - Sykes & MatzaDocumento4 páginasTechniques of Neutralization - Sykes & MatzaAnna KasapoglouAinda não há avaliações
- Measuring Violence-Related Attitudes, Behaviors, and Influences Among Youths - Assessment ToolDocumento373 páginasMeasuring Violence-Related Attitudes, Behaviors, and Influences Among Youths - Assessment ToolStacie Martin100% (1)
- I-502 Evaluation Plan and Preliminary Report On Implementation FINALDocumento54 páginasI-502 Evaluation Plan and Preliminary Report On Implementation FINALJake B EllisonAinda não há avaliações
- Theories of AggressionDocumento4 páginasTheories of AggressionJael100% (1)
- The Impact of Social Media On Depression in 18-34-Year-Olds in The United StatesDocumento66 páginasThe Impact of Social Media On Depression in 18-34-Year-Olds in The United StatesRODLI AKBAR RAHARJA AULIAAinda não há avaliações
- Contemporary Psychoanalysis and HomosexualityDocumento11 páginasContemporary Psychoanalysis and HomosexualityVarun ViswanathanAinda não há avaliações
- 3.alcohol Gender Drinking Problems2005Documento241 páginas3.alcohol Gender Drinking Problems2005kevin100% (1)
- Novotny Grant 2016 To 2021Documento3 páginasNovotny Grant 2016 To 2021The Nutrition CoalitionAinda não há avaliações
- Final Press Release V 4 9-11-17Documento1 páginaFinal Press Release V 4 9-11-17api-300187650Ainda não há avaliações
- 12-24 Doctor ShortageDocumento18 páginas12-24 Doctor ShortageHawaii News NowAinda não há avaliações
- Kobayashi Medical Practice Business PlanDocumento26 páginasKobayashi Medical Practice Business Planzahoor80Ainda não há avaliações
- Adolescent Health and Development ProgramDocumento16 páginasAdolescent Health and Development ProgramEmbrmrie ParkAinda não há avaliações
- SC 10Documento16 páginasSC 10khamilatusyAinda não há avaliações
- Development and Validation of A Sociodemographic ADocumento14 páginasDevelopment and Validation of A Sociodemographic AvusAinda não há avaliações
- Modelos de Transmisión VIH BelizeDocumento85 páginasModelos de Transmisión VIH BelizeDennis ValvertAinda não há avaliações
- HMSA RulingDocumento24 páginasHMSA RulingHNNAinda não há avaliações
- Hawaii Supreme Court Ruling On BLNRDocumento21 páginasHawaii Supreme Court Ruling On BLNRHNNAinda não há avaliações
- Letter To Police CommissionDocumento3 páginasLetter To Police CommissionHNNAinda não há avaliações
- MFD After-Action ReportDocumento84 páginasMFD After-Action ReportHNNAinda não há avaliações
- Maui County Releases Herman Andaya's EmailsDocumento276 páginasMaui County Releases Herman Andaya's EmailsHNNAinda não há avaliações
- 2024-18 Hawai I Attorney General Anne Lopez Releases First Phase Objective, Science-Based Facts Related To The Maui Fire InvestigationDocumento3 páginas2024-18 Hawai I Attorney General Anne Lopez Releases First Phase Objective, Science-Based Facts Related To The Maui Fire InvestigationHNNAinda não há avaliações
- Tax Guidance On Red Hill ReimbursementsDocumento5 páginasTax Guidance On Red Hill ReimbursementsHNNAinda não há avaliações
- NTSB Releases Final Report in July 2021 Plane Crash Off OahuDocumento45 páginasNTSB Releases Final Report in July 2021 Plane Crash Off OahuHNNAinda não há avaliações
- EOC Sign-In SheetDocumento7 páginasEOC Sign-In SheetHNN100% (3)
- Top Five List Moving On To Final BallotDocumento4 páginasTop Five List Moving On To Final BallotHNN100% (1)
- Supreme Court DecisionDocumento13 páginasSupreme Court DecisionHNNAinda não há avaliações
- Kealoha FilingDocumento32 páginasKealoha FilingHNNAinda não há avaliações
- 2018 Maui Wildfires After-Action ReportDocumento66 páginas2018 Maui Wildfires After-Action ReportHNN0% (1)
- AFFF Investigation DocumentsDocumento312 páginasAFFF Investigation DocumentsHNNAinda não há avaliações
- DOH Recommendations On Lead at Shooting RangeDocumento5 páginasDOH Recommendations On Lead at Shooting RangeHNNAinda não há avaliações
- Hawaii Department of Health MemoDocumento18 páginasHawaii Department of Health MemoHonolulu Star-AdvertiserAinda não há avaliações
- Final Report On Ambulance FireDocumento18 páginasFinal Report On Ambulance FireHNNAinda não há avaliações
- Public Safety BriefingDocumento23 páginasPublic Safety BriefingHNNAinda não há avaliações
- Conduct Commission ReportDocumento396 páginasConduct Commission ReportHNNAinda não há avaliações
- HPD Discipline ReportDocumento17 páginasHPD Discipline ReportHNNAinda não há avaliações
- CDC SurveyDocumento1 páginaCDC SurveyHNNAinda não há avaliações
- CDC Survey PresentationDocumento38 páginasCDC Survey PresentationHNNAinda não há avaliações
- H-1 Freeway ClosureDocumento1 páginaH-1 Freeway ClosureHNNAinda não há avaliações
- IRS Red Hill - Hawaii Delegation LetterDocumento2 páginasIRS Red Hill - Hawaii Delegation LetterHNNAinda não há avaliações
- Koko Head TestingDocumento6 páginasKoko Head TestingHNNAinda não há avaliações
- Miske DocumentsDocumento14 páginasMiske DocumentsHNN100% (1)
- Motion of Preliminary InjunctionDocumento170 páginasMotion of Preliminary InjunctionHNNAinda não há avaliações
- Miske DocumentsDocumento42 páginasMiske DocumentsHNN100% (1)
- Miske DocumentsDocumento37 páginasMiske DocumentsHNNAinda não há avaliações
- Miske DocumentsDocumento31 páginasMiske DocumentsHNNAinda não há avaliações
- The Lancet Microbe.: Priya VenkatesanDocumento1 páginaThe Lancet Microbe.: Priya Venkatesankayegi8666Ainda não há avaliações
- Vaccination CentersDocumento30 páginasVaccination CentersAnil Kumar NallaAinda não há avaliações
- Who Immunization-Routine-Table2Documento11 páginasWho Immunization-Routine-Table2Frances Jean T. DoblasAinda não há avaliações
- Eyecheck Announces FDA IND Clearance of STRI Formula, The First-Ever Food-Based, Combination Product in The STRI Phase 2 Clinical Trial For COVID-19 SymptomsDocumento3 páginasEyecheck Announces FDA IND Clearance of STRI Formula, The First-Ever Food-Based, Combination Product in The STRI Phase 2 Clinical Trial For COVID-19 SymptomsPR.comAinda não há avaliações
- Health Programs Activities Timeframe Expected Output Child CareDocumento3 páginasHealth Programs Activities Timeframe Expected Output Child CareC SamAinda não há avaliações
- The Commonwealth The Commonwealth: CC CC CDocumento25 páginasThe Commonwealth The Commonwealth: CC CC COmkar SathaleAinda não há avaliações
- Bahasa Inggris Bu YuliDocumento8 páginasBahasa Inggris Bu YuliNova FitriaAinda não há avaliações
- Romania WHO Country ProfileDocumento4 páginasRomania WHO Country Profileoctavia2Ainda não há avaliações
- 50 QuestionsDocumento12 páginas50 QuestionsDhon ProkopyoAinda não há avaliações
- Coronavirus (COVID-19) RecordsDocumento1 páginaCoronavirus (COVID-19) RecordsMohammad Tayyab KhanAinda não há avaliações
- Letter To Deputy Director Education Department For Pulse Polio Programme (East District) On 10th December To 15th December 2023Documento2 páginasLetter To Deputy Director Education Department For Pulse Polio Programme (East District) On 10th December To 15th December 2023AAMIR KHANAinda não há avaliações
- High Power CommitteeDocumento9 páginasHigh Power CommitteeNissy Biju Varghese67% (3)
- Universal Health Care - EditedDocumento2 páginasUniversal Health Care - Editedronald wafulaAinda não há avaliações
- Everybody's Business: Strengthening Health Systems To Improve Health OutcomesDocumento56 páginasEverybody's Business: Strengthening Health Systems To Improve Health OutcomesEllen LicupAinda não há avaliações
- FlyerDocumento1 páginaFlyersaggittarianAinda não há avaliações
- Upaya Pencegahan TB ParuDocumento13 páginasUpaya Pencegahan TB Parurizka shofiyaniAinda não há avaliações
- Communicable Disease NursingDocumento9 páginasCommunicable Disease NursingMaybelyn JoradoAinda não há avaliações
- Premises & Plant Design Layouts PrincipleDocumento31 páginasPremises & Plant Design Layouts PrincipleArghya Pratim BhattacharjeeAinda não há avaliações
- Biopharmaceuticals Availability, Diffusion, Sustainability: Massimo Riccaboni University of Florence & CERM, RomeDocumento28 páginasBiopharmaceuticals Availability, Diffusion, Sustainability: Massimo Riccaboni University of Florence & CERM, RomeNoor hossainAinda não há avaliações
- EngDocumento40 páginasEngSebastian Gonzalez MazoAinda não há avaliações
- 116 Shivani NairDocumento20 páginas116 Shivani NairShivani NairAinda não há avaliações
- Jamie Stang HHS GrantsDocumento1 páginaJamie Stang HHS GrantsThe Nutrition CoalitionAinda não há avaliações
- School Based Mental Health and Psychosocial WellnessDocumento89 páginasSchool Based Mental Health and Psychosocial WellnessOliv KrisAinda não há avaliações
- IDSP BelgaumDocumento36 páginasIDSP BelgaumJ Nuchin100% (1)
- Jurnal - Pendampingan Perencanaan Kehamilan SehatDocumento6 páginasJurnal - Pendampingan Perencanaan Kehamilan SehatElly Naila Fauziah100% (1)
- Community Health Nursing Exam 1 - 198 TermsDocumento80 páginasCommunity Health Nursing Exam 1 - 198 TermsCharaAinda não há avaliações
- Pharmaceutical Benefits Under State Medical Assistance Programs, 1983Documento375 páginasPharmaceutical Benefits Under State Medical Assistance Programs, 1983National Pharmaceutical CouncilAinda não há avaliações
- Lecture 8 Surveillance FinalDocumento55 páginasLecture 8 Surveillance FinalKhalil UllahAinda não há avaliações
- NOH2005 2010may15Documento311 páginasNOH2005 2010may15Jamil Lorca100% (4)
- FP10 Toolkit (V1) 01.2020Documento12 páginasFP10 Toolkit (V1) 01.2020Armando KasinoAinda não há avaliações