Escolar Documentos
Profissional Documentos
Cultura Documentos
Guideline Trauma Anak 2018
Enviado por
nonasucirahayuDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Guideline Trauma Anak 2018
Enviado por
nonasucirahayuDireitos autorais:
Formatos disponíveis
SPECIAL ISSUE ARTICLE
Traumatic Brain Injury in the
Pediatric Intensive Care Unit
Elora Hussain, MD
CLINICAL INJURY SEVERITY
ABSTRACT TBI severity has classically been
Head trauma is a leading cause of brain injury in children, and it can have profound life- defined by using the Glasgow Coma
long physical, cognitive, and behavioral consequences. Optimal acute care of children with Scale (GCS)4 or Pediatric GCS on ad-
traumatic brain injury (TBI) requires rapid stabilization and early neurosurgical evaluation mission.5 A GCS of 13 to 15 is consid-
by a multidisciplinary team. Meticulous attention is required to limit secondary brain injury ered mild TBI; 9 to 12 is considered
after the initial trauma. This review discusses pathophysiology, acute stabilization, and mon- moderate; and GCS less than 9 is con-
itoring, as well as supportive and therapeutic measures to help minimize ongoing brain sidered severe. Frequent repeated as-
injury and optimize recovery in children with TBI. [Pediatr Ann. 2018;47(7):e274-e279.] sessments of the patient’s neurologic
examination and GCS are fundamental
T
raumatic brain injury (TBI) is a MECHANISMS OF BRAIN INJURY to understanding the severity and pro-
leading cause of morbidity and The distribution of damage after TBI gression of illness, and to guide clinical
mortality in children. In the may be focal or diffuse. Focal injury is management.6
United States, approximately 475,000 produced by direct impact forces act-
children younger than age 14 years ing on the skull, resulting in compres- PATHOPHYSIOLOGY
suffer from TBI annually.1 Financial sion of brain tissue at the site of impact Cerebral pathology from TBI occurs
burden can be significant, with pedi- (coup) or opposite the site of impact by two mechanisms: primary (or im-
atric inpatients accounting for over $1 (contrecoup). Focal injuries may cause mediate) brain injury and secondary (or
billion in total charges for TBI-associ- parenchymal contusions, intraparen- delayed) brain injury. Primary injury is
ated hospitalizations.2 chymal hemorrhage, subdural and epi- the immediate parenchymal injury that
Injury patterns due to TBI vary by dural hematomas, and subarachnoid occurs from the trauma itself. Preven-
age. In infants, inflicted or nonacci- hemorrhage. tion is the only measure that can affect
dental injury must always be consid- Diffuse injury is more widely dis- primary injury.
ered. Falls are the primary mechanism tributed, involving the axons and vas- In the minutes to days after primary
of TBI-related emergency department cular structures, and can be associated injury, the brain is particularly vulnera-
visits in children (age 0 to 4 years). with hypoxic ischemic injury and ce- ble to secondary injury due to increased
In school-age children, falls decrease rebral edema. It is typically caused by metabolic demands and compromised
with age, with a rise in bicycle acci- rapid acceleration-deceleration move- cerebral perfusion. A complex cascade
dents. In adolescents, there is a dra- ments of the head. Diffuse axonal in- of cellular, biochemical, and meta-
matic rise in TBI due to motor vehicle jury is caused by widespread insult to bolic processes is initiated, which can
accidents, sports-related injuries, and cerebral white matter and may result in lead to ongoing neuronal damage and
violence.1 extended loss of consciousness.3 cell death. Both cytotoxic and vaso-
genic edema may occur, with cytotoxic
Elora Hussain, MD, is the Medical Director of Neurocritical Care, Division of Pediatric Critical Care edema from cellular swelling, and va-
Medicine, Helen DeVos Children’s Hospital; and an Assistant Professor, Department of Pediatrics and sogenic edema from disruption of the
Human Development, Michigan State University College of Human Medicine. blood-brain barrier and vascular integ-
Address correspondence to Elora Hussain, MD, Helen DeVos Children’s Hospital, 100 Michigan Street rity.7 This phase of injury can be further
NE, MC 117, Grand Rapids, MI 49503; email: elora.hussain@helendevoschildrens.org. exacerbated by physiologic derange-
Disclosure: The author has no relevant financial relationships to disclose. ments including hypoxia, hypotension,
doi:10.3928/19382359-20180619-01 and hyperthermia.8,9 Management strat-
e274 Copyright © SLACK Incorporated
SPECIAL ISSUE ARTICLE
egies in the acute period after TBI are After initial stabilization, patients ICP monitoring, it does highlight the
primarily focused on minimizing and with moderate or severe TBI warrant need for additional investigation re-
preventing secondary brain injury. emergent neuroimaging with computed garding the role of ICP monitoring in
tomography without contrast to assess the management of severe TBI.12
EVALUATION for lesions requiring emergent neuro- Invasive and noninvasive tissue
Details of the patient’s medical his- surgical intervention. A full trauma as- oximeters may be used in combina-
tory, timing and mechanism of the trau- sessment by a multidisciplinary trauma tion with ICP monitors, with studies
ma, and resuscitation efforts prior to team is also necessary to evaluate for suggesting that reduced brain tissue
presentation are essential. On physical and treat extracranial insults. oxygen tension is associated with poor
examination, adequacy of the patient’s outcomes in severe pediatric TBI.13
respiratory and cardiovascular status, INVASIVE NEUROMONITORING Oxygenation parameters and manage-
as well as neurologic examination, must An intracranial pressure (ICP) ment targets, however, are largely ex-
be rapidly assessed. Cervical spine sta- monitor is often placed by a neuro- trapolated from adult data.
bilization should be maintained to avoid surgeon after stabilization in children
cervical spine injury. GCS should be with severe injury (GCS ≤8) for ICP ONGOING MANAGEMENT
determined, and life-threatening signs monitoring and potential treatment of After initial stabilization and resus-
of impending herniation rapidly identi- intracranial hypertension. This can al- citation, ongoing physiologic monitor-
fied. These may include altered level of low for early detection of patients at ing and management should continue
consciousness, pupillary dysfunction, risk for cerebral herniation and may in a pediatric intensive care unit (ICU)
lateralizing extremity weakness, or allow for therapeutic drainage of cere- to avoid secondary insults such as hy-
Cushing’s triad (systemic hypertension, brospinal fluid (CSF) if needed. Cur- poxia, hypotension, and hyperthermia.
bradycardia, irregular respirations). rent recommendations in pediatrics are In 2012, the revised Guidelines for the
The presence of Cushing’s triad is a late for treatment of intracranial pressure Acute Medical Management of Severe
and ominous sign of herniation.7 ≥20 mm Hg.10 Traumatic Brain Injury in Infants, Chil-
Invasive ICP monitoring is the cur- dren, and Adolescents were published
INITIAL STABILIZATION rent standard of care for children with by the Brain Trauma Foundation.10
If a child has normal mentation, re- concern for intracranial hypertension. These guidelines focus on minimizing
spiratory effort, and favorable hemody- However robust evidence supporting secondary brain injury after pediatric
namics, advanced airway management this practice is lacking, with only class TBI and are based on best-available
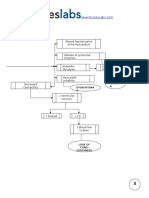
may not be required. However, in pa- III evidence available.10 The BEST current evidence. Figure 1 shows an
tients with signs of airway obstruction, TRIP trial published in 2012 is the example of a clinical management
inadequate oxygenation or ventilation, only large-scale, high-quality random- pathway for severe pediatric TBI. It
or shock, rapid stabilization and resus- ized multicenter controlled trial on this should be noted, however, that high
citation by a multidisciplinary team is subject to date, and created significant quality evidence in this field remains
required. controversy regarding ICP monitoring lacking; these consensus guidelines
In patients with decreasing level in severe TBI.11 This trial randomized include no level I recommendations,
of consciousness (and/or GCS ≤8), pediatric and adult patients in South and most recommendations are level
advanced airway support with endo- America to receive either invasive ICP III evidence.9
tracheal intubation is indicated while monitoring or treatment based on im-
maintaining stabilization of the cervical aging and clinical examination alone.11 INTRACRANIAL PRESSURE AND
spine. Strict avoidance of hypotension, There was no significant difference be- CEREBRAL AUTOREGULATION
hypoxemia, and intracranial hyperten- tween groups in morbidity or mortal- One of the most severe consequenc-
sion are necessary during intubation. ity measured at 6 months postinjury. es of TBI is intracranial hypertension
Fluid resuscitation with isotonic so- The degree to which these results can reflected by an elevated ICP. With a
lutions to reverse hypovolemic shock be generalized to clinical practice in space-occupying lesion, such as an ex-
may be necessary and to replenish in- North America is controversial, due to panding hematoma or cerebral edema,
travascular volume. Hypotonic fluid is potential differences in prehospital care initial compensatory mechanisms can
contraindicated in the initial resusci- and resuscitation. Although the BEST prevent elevated ICP to a limited ex-
tation as this may exacerbate cerebral TRIP trial may not warrant a change in tent. Once these mechanisms are ex-
edema and cell death.7 the current clinical practice of invasive hausted, even small increases in intra-
PEDIATRIC ANNALS • Vol. 47, No. 7, 2018 e275
SPECIAL ISSUE ARTICLE
Figure 1. Clinical pathway for the management of severe pediatric traumatic brain injury. CPP, cerebral perfusion pressure; CSF, cerebrospinal fluid; CT, com-
puted tomography; EEG, electroencephalogram; EVD, external ventricular drain; ICP, intracranial pressure; IV, intravenous; GCS, Glasgow Coma Scale; MAP,
mean arterial pressure; TBI, traumatic brain injury.
e276 Copyright © SLACK Incorporated
SPECIAL ISSUE ARTICLE
cranial volume can lead to intracranial oxygenation.16 Data in pediatrics are of etomidate may be considered for
hypertension, which can compromise lacking; however, the same manage- control of severe intracranial hyper-
cerebral perfusion and lead to cerebral ment is applied to children. Internal tension; however, the risk of adrenal
ischemia, and even herniation.8 jugular catheterization is often avoided suppression must be considered. Bar-
Under normal conditions, cerebral in these patients to maintain venous biturates may also be used for control
autoregulation allows the cerebral patency and optimize cerebral venous of intracranial hypertension but may
arterioles to vasodilate and vasocon- drainage. Care should be taken to en- cause myocardial depression and sys-
strict to maintain constant cerebral sure that cervical collars do not impede temic hypotension.10
blood flow (CBF) over a wide range venous drainage. Neuromuscular blockade is some-
of blood pressures. In the clini- times used to prevent cough, shivering,
cal setting, cerebral perfusion pres- Sedation, Analgesia, and and patient-ventilator dysynchrony.
sure (CPP) is used as a surrogate for Neuromuscular Blockade Paralytics reduce metabolic demand
CBF.14 CPP is the difference between Moderate to deep sedation is of- and may result in improved chest-wall
mean arterial pressure (MAP) and ICP ten necessary to ensure comfort and compliance, causing reduction in intra-
(CPP = MAP – ICP). In healthy adults, patient compliance with mechanical thoracic pressure to promote improved
MAP between 50 and 170 mm Hg pro- ventilation and treatment goals after cerebral venous drainage. However,
duces little to no change in CBF. In TBI. Pain, agitation, and anxiety can routine use of neuromuscular blockade
healthy infants and children, there are also increase ICP and cerebral meta- does not improve overall outcome and
few studies on the physiologic range bolic demand. Pediatric data on the is associated with prolonged ICU stay
of cerebral autoregulation. ideal medication regimen for sedation and nosocomial pneumonia and should
In moderate and severe TBI, the and analgesia are lacking; however, therefore only be reserved for limited
normal mechanisms for cerebral au- continuous infusions of narcotics and clinical situations.20
toregulation are often compromised, benzodiazepines are often used in the
causing CBF to become dependent pediatric ICU. These medications may Cerebrospinal Fluid Drainage
on MAP. Decreased CPP and cere- cause further respiratory depression If an external ventricular drain is
bral ischemia may occur due to ei- and hypotension, so the lowest pos- placed, CSF removal may be used as a
ther decreased MAP or increased sible doses needed for comfort and therapeutic maneuver to decrease ICP
ICP. Conversely, increased MAP and ICP management should be used. Pre- in patients with intracranial hyperten-
decreased ICP may result in cerebral medication with lidocaine may be used sion. Placement of such catheters may
hyperemia.7-9 Impaired cerebral au- prior to potentially noxious therapies be technically difficult in patients with
toregulation in children is associated such as suctioning of the endotracheal diffuse cerebral edema and compres-
with worse outcomes.15 Thus, many tube; however, whether lidocaine use sion of the lateral ventricles.8
therapeutic interventions after TBI are effects clinical outcomes is unclear.17
targeted at lowering ICP, augment- The use of ketamine has been de- Hyperosmolar Therapy
ing MAP to ensure adequate CPP, bated in the setting of TBI due to early Mannitol and hypertonic saline are
and maintaining euvolemia. Pediatric studies demonstrating an association used as hyperosmolar therapies for de-
guidelines recommend a minimum with increased ICP. More recent stud- creasing ICP. Insufficient evidence cur-
CPP threshold of 40 to 50 mm Hg to ies suggest that when administered rently exists to support the use of one
prevent cerebral hypoperfusion and in conjunction with other anesthetic therapy over the other. Mannitol has
ischemia. However, the optimal CPP agents, ICP does not increase and may had longstanding clinical acceptance
in pediatric TBI is unknown.10,14 even improve.18 Further studies of ket- and is commonly used in both pedi-
amine are needed to determine safety atric and adult TBI cases. However,
INTRACRANIAL PRESSURE in the setting of pediatric TBI. Propo- there are no controlled clinical trials of
LOWERING THERAPIES fol is often used in adult TBI for con- mannitol use in children. Hypertonic
Patient Positioning tinuous sedation; however, it is not rec- saline, however, is gaining more ac-
Maintaining the head in a neutral, ommended in children due to reports ceptance and is currently supported by
midline position and elevating the of metabolic acidosis, organ failure, class II evidence for acute treatment of
head of the bed to 30 degrees has been and death, leading to safety warnings intracranial hypertension in children,
shown in adults to reduce ICP with- from the US Food and Drug Admin- and class III evidence to support its use
out compromising CPP and cerebral istration.19 Single-dose administration as a continuous infusion.10
PEDIATRIC ANNALS • Vol. 47, No. 7, 2018 e277
SPECIAL ISSUE ARTICLE
Mannitol is typically given in bolus ric TBI.9 However, pediatric clinical tri- shown there may be benefit in survival
doses of 0.25 to 1 g/kg and works via als have not demonstrated benefit, with and neurologic outcomes,30,31 but both
rapid reduction of blood viscosity and one trial showing a trend toward worse adult and pediatric trials have thus far
osmotic diuresis, thereby improving outcomes.24,25 Therefore, prophylactic been heterogeneous in both trial design
CBF and decreasing cerebral blood vol- therapeutic hypothermia is not currently and results, making it difficult to draw
ume. Risks of mannitol administration recommended for management of intra- definitive conclusions regarding benefit
include hypotension and renal failure, cranial hypertension. It may be reserved from this procedure.9
particularly when serum osmolality is only as a temporizing measure for pa-
>320 mOsm/L. Hypertonic saline is typ- tients with refractory intracranial hyper- OUTCOMES
ically limited to 3% saline in children, tension unresponsive to other medical Long-term outcomes of children with
but higher concentrations are often used interventions.8 TBI are quite heterogeneous, ranging
in adults. Optimal dosing is not well from near return to baseline to varying
studied, but bolus dosing ranges between Seizure Control degrees of disability or death. Many
6.5 and 10 mL/kg, with a higher serum Post-traumatic seizures have been children continue to have significant
osmolar threshold of 360 mOsm/L. The shown to cause persistent cerebral meta- neurologic impairment at the time of dis-
mechanisms of hypertonic saline also bolic crisis and increased ICP.26 In chil- charge.9 In addition to physical disabili-
include improved CBF and providing dren younger than age 2 years, abusive ties, neuropsychological sequelae from
an osmotic gradient to reduce ICP. It is head trauma, and presence of subdural TBI may influence vital development
also thought to have theoretical benefits hemorrhage have been associated with in children, such as learning, emotional
of inhibiting inflammation, restoring increased risk of post-traumatic sei- awareness, and social functioning.2 On-
normal resting cellular membrane po- zures.27 Seizures can be convulsive or going management, rehabilitation, and
tential, and enhancing cardiac output.10 nonconvulsive, with nonconvulsive sei- anticipatory guidance for a potentially
Potential risks include rebound in ICP, zures only detected by electroencepha- new seizure disorder, or newly acquired
central pontine myelinolysis, and renal logram monitoring. There is a paucity physical, behavioral, and/or cognitive
impairment.21 of data to guide clinicians on treatment disability are important for follow-up
of post-traumatic seizures; the current care.
Hyperventilation pediatric guidelines suggest that routine
Carbon dioxide (CO2) has a profound seizure prophylaxis for the first 7 days CONCLUSIONS
and reversible effect on CBF, such that after severe TBI is reasonable to reduce Care of children with TBI should
hypercapnia causes dilation of cerebral the incidence of early post-traumatic focus on rapid stabilization and early
arteries and arterioles and increased seizures.10 neurosurgical evaluation, with ongo-
CBF, whereas hypocapnia causes vaso- ing management focused on prevention
constriction and decreased CBF. Thus, Decompressive Craniectomy of secondary cerebral insults. Careful
hyperventilation can rapidly reduce ICP. Surgical decompressive craniectomy physiologic monitoring, with optimiza-
It may be used as a brief temporizing with duraplasty, leaving the bone flap tion of CPP and treatment of intracranial
measure for acute impending herniation, out, may be considered for pediatric hypertension are critical. The paucity of
pending definitive therapy. However patients who have refractory intracra- high-quality literature in pediatric TBI
prophylactic, chronic hyperventilation nial hypertension unresponsive to other highlights the need for further research
in children should be avoided due to therapies.10 One randomized adult study, to advance our understanding of patho-
risks of hypoperfusion and cerebral isch- the DECRA trial, showed that decom- physiology and to aid in the neurologic
emia, and normocarbia with pCO2 of 35 pressive craniectomy decreased ICP and recovery of children with TBI.
to 40 mm Hg should be targeted.10,22 ICU length of stay, but was associated
with more unfavorable outcomes.28 An- REFERENCES
Temperature Control other recent adult study, the RESCUEicp 1. Langlois J, Rutland-Brown W, Thomas K.
Brain Injury in the United States: Emergen-
Fever in the setting of neurologic (Randomized Evaluation of Surgery cy Department Visits, Hospitalizations, and
illness is associated with worse out- with Craniectomy for Uncontrollable Deaths. Atlanta, GA: Centers for Disease
comes.23 Animal models and early adult Elevation of Intracranial Pressure) trial, Control and Prevention, National Center for
Injury Prevention and Control; 2004:1-32.
studies have demonstrated benefit from resulted in lower mortality but higher 2. Schneier AJ, Shields BJ, Hostetler SG,
therapeutic hypothermia, making it a po- rates of severe disability and vegetative Xiang H, Smith GA. Incidence of pediat-
tential neuroprotective therapy in pediat- state.29 Small studies in pediatrics have ric traumatic brain injury and associated
e278 Copyright © SLACK Incorporated
SPECIAL ISSUE ARTICLE
hospital resource utilization in the Unites Treatment of Intracranial Pressure Trial. fect of hyperventilation on regional cerebral
States. Pediatrics. 2006;118(2):483-492. J Neurotrauma. 2015;32(22):1722-1724. blood flow in head-injured children. Crit
doi:10.1542/peds.2005-2588. doi:10.1089/neu.2015.3976. Care Med. 1997:25(8):1402-1409.
3. Andriessen TM, Jacobs B, Vos PE. Clini- 13. Figaji AA, Zwane E, Thompson C, et 23. Greer DM, Funk SE, Reaven NL, Ou-
cal characteristics and pathophysiological al. Brain tissue oxygen tension monitor- zounelli M, Uman GC. Impact of fever
mechanisms of focal and diffuse brain inju- ing in pediatric severe traumatic brain in- on outcome in patients with stroke and
ry. J Cell Mol Med. 2010;14(10):2381-2392. jury. Part 1: relationship with outcome. neurologic injury: a comprehensive meta-
doi:10.1111/j.1582-4934.2010.01164.x. Childs Nerv Syst. 2009;25(10):1325-1333. analysis. Stroke. 2008;39(11):3029-3035.
4. Teasdale G, Jennett B. Assessment of coma doi:10.1007/s00381-009-0822-x. doi:10.1161/STROKEAHA.108.521583.
and impaired consciousness. A practical 14. Udomphorn Y, Armstead WM, Vavilala 24. Adelson PD, Ragheb J, Kanev P, et al. Phase
scale. Lancet. 1974;2(7872):81-84. MS. Cerebral blood flow and autoregu- II clinical trial of moderate hypothermia af-
5. Holmes JF, Palchak MJ, MacFarlane T, lation after pediatric traumatic brain in- ter severe traumatic brain injury in children.
Kuppermann N. Performance of the pe- jury. Pediatr Neurol. 2008;38(4):225-234. Neurosurgery. 2005;56(4):740-754.
diatric Glasgow Coma Scale in children doi:10.1016/j.pediatrneurol.2007.09.012. 25. Hutchison JS, Ward RE, Lacroix J, et
with blunt head trauma. Acad Emerg 15. Vavilala MS, Lee LA, Boddu K, et al. Ce- al. Hypothermia therapy after traumatic
Med. 2005;12(9):814-819. doi:10.1197/j. rebral autoregulation in pediatric trau- brain injury in children. N Engl J Med.
aem.2005.04.019. matic brain injury. Pediatr Crit Care Med. 2008;358(23):2447-2456. doi:10.1056/
6. Friedland D, Hutchinson P. Classification 2004;5(3):257-263. NEJMoa0706930.
of traumatic brain injury. Adv Clin Neuro- 16. Ng I, Lim J, Wong HB. Effects of head pos- 26. Vespa PM, Miller C, McArthur D, et
sci Rehab. http://www.acnr.co.uk/2013/07/ ture on cerebral hemodynamics: its influ- al. Nonconvulsive electrographic sei-
classification-of-traumatic-brain-injury/. ences on intracranial pressure, cerebral per- zures after traumatic brain injury result
Published July 27, 2013. Accessed June, 19, fusion pressure, and cerebral oxygenation. in a delayed, prolonged increase in in-
2018. Neurosurgery. 2004;54(3):593-597. tracranial pressure and metabolic crisis.
7. Kochanek PM, Bell MJ, Bayir H, et al. Se- 17. Bilotta F, Branca G, Lam A, Cuzzone Crit Care Med. 2007;35(12):2830-2836.
vere traumatic brain injury in infants and V, Doronzo A, Rosa G. Endotracheal li- doi:10.1097/01.ccm.0000295667.66853.bc.
children. In: Furhman BP, Zimmerman JJ, docaine in preventing endotracheal suc- 27. Bennett KS, DeWitt PE, Harlaar N,
eds. Pediatric Critical Care. Philadelphia, tioning-induced changes in cerebral he- Bennett TD. Seizures in children with
PA: Mosby; 2011:849-870. modynamics in patients with severe head severe traumatic brain injury. Pedi-
8. Freiss SH, Kilbaugh TJ, Huh J. Traumatic trauma. Neurocrit Care. 2008;8(2):241-246. atr Crit Care Med. 2017;18(1):54-63.
brain injury. In: Abend NS, Helfaer MA, eds. doi:10.1007/s12028-007-9012-4. doi:10.1097/PCC.0000000000000948.
Pediatric Neurocritical Care. New York, NY: 18. Bar-Joseph G, Guilburd Y, Tamir A, Guil- 28. Cooper DJ, Rosenfeld JV, Mur-
Demos; 2013:104-113. burd JN. Effectiveness of ketamine on ray L, et al. Decompressive craniec-
9. Guilliams K, Wainwright MS. Patho- decreasing intracranial pressure in chil- tomy in diffuse traumatic brain injury.
physiology and management of moderate dren with intracranial hypertension. J N Engl J Med. 2011;364(16)1493-1502.
and severe traumatic brain injury in chil- Neurosurg Pediatr. 2009;4(1):40-46. doi:10.1056/NEJMoa1102077.
dren. J Child Neurol. 2016;31(1):35-45. doi:10.3171/2009.1.PEDS08319. 29. Hutchinson PJ, Kolias AG, Timofeev IS,
doi:10.1177/0883073814562626. 19. Wysowski DK, Pollack ML. Reports of death et al. Trial of decompressive craniectomy
10. Kochanek PM, Carney N, Adelson PD, et al. with use of propofol (Diprivan) for nonproc- for traumatic intracranial hypertension.
Guidelines for the acute medical management edural (long-term) sedation and literature N Engl J Med. 2016;375(12):1119-1130.
of severe traumatic brain injury in infants, review. Anesthesiology. 2006;105(5):1047- doi:10.1056/NEJMoa1605215.
children, and adolescents--second edition. 1051. 30. Taylor A, Butt W, Rosenfeld J, et al. A ran-
Pediatr Crit Care Med. 2012;13(suppl):S1- 20. Hsian JK, Chestnut RM, Crisp CB, Klauber domized trial of very early decompressive
S82. doi:10.1097/PCC.0b013e31823f435c. MR, Blunt BA, Marshall LF. Early, routine craniectomy in children with traumatic brain
11. Chestnut RM, Temkin N, Carney N, paralysis for intracranial pressure control in injury and sustained intracranial hyperten-
et al. A trial of intracranial-pressure severe head injury: is it necessary? Crit Care sion. Childs Nerv Syst. 2001;17(3):154-162.
monitoring in traumatic brain injury. N Med. 1994;22(9):1471-1476. doi:10.1007/s003810000410.
Engl J Med. 2012;367(26):2471-2481. 21. Qureshi AI, Suarez JI. Use of hypertonic sa- 31. Cho DY, Wang YC, Chi CS. De-
doi:10.1056/NEJMoa1207363. line solutions in treatment of cerebral edema compressive craniectomy for acute
12. Chestnut RM, Bleck TP, Citerio G, et al. A and intracranial hypertension. Crit Care shaken/impact baby syndrome. Pedi-
consensus-based interpretation of the Bench- Med. 2000;28(9):3301-3313. atr Neurosurg. 1995;23(4):192-198.
mark Evidence from South American Trials: 22. Skippen P, Seear M, Poskitt K, et al. Ef- doi:10.1159/000120958.
PEDIATRIC ANNALS • Vol. 47, No. 7, 2018 e279
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- MeningomyeloceleDocumento34 páginasMeningomyelocelerajan kumarAinda não há avaliações
- Joshis External Stabilisation System Jess For Recurrent Ctev Due To Irregular Follow Up PDFDocumento5 páginasJoshis External Stabilisation System Jess For Recurrent Ctev Due To Irregular Follow Up PDFshankarAinda não há avaliações
- Myocardial Infarction Pathophysiology Schematic DiagramDocumento3 páginasMyocardial Infarction Pathophysiology Schematic Diagramnursing concept mapsAinda não há avaliações
- Mike McKendrickDocumento61 páginasMike McKendrickVikas AgrawalAinda não há avaliações
- NCP For PostpartumDocumento1 páginaNCP For PostpartumMary Hope BacutaAinda não há avaliações
- Encefalitis LimbicaDocumento11 páginasEncefalitis LimbicaRandy UlloaAinda não há avaliações
- IFU Intense - LFT06 Rev.02Documento9 páginasIFU Intense - LFT06 Rev.02Ana ČolovićAinda não há avaliações
- Diabetes and It's Oral ManifestationsDocumento28 páginasDiabetes and It's Oral ManifestationsYashpreetsingh BhatiaAinda não há avaliações
- Microbiology Question PapersDocumento100 páginasMicrobiology Question Papersprinceej92% (13)
- 7nutrition SupportDocumento17 páginas7nutrition Supportaklilu ewunetuAinda não há avaliações
- Renal and Perinephric AbscessDocumento11 páginasRenal and Perinephric AbscessYusak DpAinda não há avaliações
- (Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDocumento490 páginas(Contemporary Clinical Neuroscience) Giuliana Grimaldi, Mario Manto (auth.), Giuliana Grimaldi, Mario Manto (eds.)-Mechanisms and Emerging Therapies in Tremor Disorders-Springer-Verlag New York (2013).pdfDanalachi Adrian100% (2)
- Spanish Medical Words and PhrasesDocumento22 páginasSpanish Medical Words and PhrasesAnushkaAinda não há avaliações
- Respiratory Distress Syndrome (Hyaline Membrane Disease)Documento98 páginasRespiratory Distress Syndrome (Hyaline Membrane Disease)Miraf MesfinAinda não há avaliações
- Week 8 Hepato Biliary 2Documento94 páginasWeek 8 Hepato Biliary 2طفوف محمد.Ainda não há avaliações
- Motor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistDocumento36 páginasMotor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistJim Jose Antony100% (1)
- Proximal Humerus FracturesDocumento4 páginasProximal Humerus FracturesParidhi MittalAinda não há avaliações
- Cervical DystociaDocumento22 páginasCervical DystociaBaldau TiwariAinda não há avaliações
- L17. Askep Kritis Dan Gadar Pasien Dengan Ggguan Sistem Pernafan NontraumatikDocumento75 páginasL17. Askep Kritis Dan Gadar Pasien Dengan Ggguan Sistem Pernafan NontraumatikSepto KristianaAinda não há avaliações
- Thesis Statement Examples For Eating DisordersDocumento6 páginasThesis Statement Examples For Eating Disordersjenniferontiveroskansascity100% (2)
- Hernia HiatalDocumento4 páginasHernia HiatalFabrizioSanchezZegarraAinda não há avaliações
- Case Study About Rectal CADocumento11 páginasCase Study About Rectal CACantiga Vhadz0% (1)
- AceDocumento14 páginasAceJustice Ace DaprozaAinda não há avaliações
- DKA CME 23.08.2023 Edited FinalleDocumento20 páginasDKA CME 23.08.2023 Edited FinalleDeborah ChemutaiAinda não há avaliações
- Mycobacterium Tuberculosis: Paper Esm MicrobiologyDocumento15 páginasMycobacterium Tuberculosis: Paper Esm MicrobiologyMuhammad KurniawanAinda não há avaliações
- Wim Hof Basic Technique 2017PDFDocumento3 páginasWim Hof Basic Technique 2017PDFKaveh EbadiAinda não há avaliações
- Acupuncture 123Documento3 páginasAcupuncture 123Romi Brener83% (6)
- Buy Augmentin 1000 - AllDayGenericDocumento7 páginasBuy Augmentin 1000 - AllDayGenericBonitaAinda não há avaliações
- Office: of The SecretaryDocumento7 páginasOffice: of The SecretaryFidelis MaximusAinda não há avaliações
- Chapter 4 of 10 - Kelsey HillDocumento3 páginasChapter 4 of 10 - Kelsey HillspiritualbeingAinda não há avaliações